Abstract
Filtering facepiece respirators (FFRs) and elastomeric half-mask respirators (EHRs) are commonly used by workers for protection against potentially hazardous particles, including engineered nanoparticles. The purpose of this study was to evaluate the performance of these types of respirators against 10–400 nm particles using human subjects exposed to NaCl aerosols under simulated workplace activities. Simulated workplace protection factors (SWPFs) were measured for eight combinations of respirator models (2 N95 FFRs, 2 P100 FFRs, 2 N95 EHRs, and 2 P100 EHRs) worn by 25 healthy test subjects (13 females and 12 males) with varying face sizes. Before beginning a SWPF test for a given respirator model, each subject had to pass a quantitative fit test. Each SWPF test was performed using a protocol of six exercises for 3 min each: (i) normal breathing, (ii) deep breathing, (iii) moving head side to side, (iv) moving head up and down, (v) bending at the waist, and (vi) a simulated laboratory-vessel cleaning motion. Two scanning mobility particle sizers were used simultaneously to measure the upstream (outside the respirator) and downstream (inside the respirator) test aerosol; SWPF was then calculated as a ratio of the upstream and downstream particle concentrations. In general, geometric mean SWPF (GM-SWPF) was highest for the P100 EHRs, followed by P100 FFRs, N95 EHRs, and N95 FFRs. This trend holds true for nanoparticles (10–100 nm), larger size particles (100–400 nm), and the ‘all size’ range (10–400 nm). All respirators provided better or similar performance levels for 10–100 nm particles as compared to larger 100–400 nm particles. This study found that class P100 respirators provided higher SWPFs compared to class N95 respirators (P<0.05) for both FFR and EHR types. All respirators provided expected performance (i.e. fifth percentile SWPF > 10) against all particle size ranges tested.
Keywords: elastomeric half-mask respirators, filtering facepiece respirators, nanoparticle, N95 respirators, P100 respirators, simulated workplace protection factors
INTRODUCTION
Aerosolized nanoparticles generated by a variety of natural and industrial processes exhibit unique properties (e.g. chemistry and toxicity) due to their greater surface area and may be inhaled, ingested, or absorbed through skin (Baroli et al., 2007). Inhalation of nanoparticles is believed to be the primary route of exposure and is of the greatest concern (Birch et al., 2011; Dahm et al., 2013). Recent studies have reported the adverse effects of known mass concentrations of nanomaterial exposures on pulmonary and systemic functions in several systems (Shvedova et al., 2009; Brooks et al., 2010). Exposure to nanoparticles also has been shown to increase the incidence of pneumoconiosis among workers (Byrne and Baugh, 2008).
Filtering facepiece respirators (FFRs) and elastomeric half-mask respirators (EHRs) are commonly used by workers for protection against potentially hazardous particles, including engineered nanoparticles (Dahm et al., 2011). Respirator performance is dependent on many variables, such as filter penetration, face seal leakage (FSL), and leakage through other respirator components (i.e. exhalation valves). The filter penetration of particles is dependent on particle diameter, particle charge state, filter fiber charge, fiber packing density, and filtration velocity, while FSL is dependent on the fit of the respirator to the face and work activity (Liu et al., 1993; Han et al., 2005; Grinshpun et al., 2009).
Although numerous research studies have measured laboratory filtration performance against particles (Wilkes, 2002; Rengasamy et al., 2009; Vo et al., 2013), only a few of them have used human subjects exposed to particles for evaluating respirator performance. The respirator performance study of Lawrence et al. (2006) was focused only on N95 FFRs and EHRs and the respiratory performance level was determined based on the total particle counts using a PortaCount without the N95-Companion accessory. The respirator performance study of Grinshpun et al. (2009) was targeted toward testing N95 FFRs and surgical masks. Grinsphun et al. found higher levels of inward leakage for particles < ~200 nm. Zhuang et al. (2013) reported a laboratory FSL evaluation of N95 FFRs against nanoparticles in the laboratory. In that study, Zhuang et al. concluded that FSL for negatively charged ~40–60 nm nanoparticles is not greater than the FSL for the larger distribution of charged and uncharged 20 to > 1000 nm particles. This finding contradicts that of Grinshpun et al. (2009) which found greater leakage for nanoparticles in that size range.
The recommended process for selecting respirators for protection against various workplace hazards can be found in the 2004 NIOSH Respirator Selection Logic (NIOSH, 2005–100) and elsewhere (BS EN 529, 2005; CSA Standard Z94.4–11). As nanoparticles and engineered nanomaterials in particular have found increasing use in workplaces, questions have been raised about whether the 2004 NIOSH Respirator Selection Logic can also be applied to nanoparticles. NIOSH research (prior to December 2008) to address this question was reviewed by Shaffer and Rengasamy (2009). It was noted that the employer should take particle size into account when making a respirator selection decision. In addition, the Occupational Safety and Health Administration (OSHA) has recommended to use the 100 efficiency level filters (e.g. class P100 respirators) when exposed to potentially harmful levels of engineered nanomaterials (OSHA, FS-3634). However, no test data for class P100 respirators using human subjects exposed to aerosols under simulated workplace activities are available to validate this recommendation. Thus, there is a need for evaluating and comparing the performance of class N95 respirators (containing a most common filter with a 95% filtration efficiency) and class P100 respirators (containing a filter with a 99.97% filtration efficiency) in the two most common respirator types (FFRs and EHRs) using human subjects under simulated workplace activities. There is also a need for evaluating respirator performance as a function of particle size to further assist respiratory protection program managers in the respirator selection process.
The aim of this study was to evaluate the performance of class N95 and class P100 respirators for both FFR and EHR types against 10–400 nm particles using human subjects exposed to NaCl aerosols under simulated workplace activities. This study was conducted to achieve three specific research objectives: (i) measure simulated workplace protection factors (SWPFs) for both FFR and EHR types as a function of particle size; (ii) determine if individual models within each type provide the expected level of performance; and (iii) compare SWPF levels between class N95 and class P100 respirators and between FFR and EHR types. This was the first study to measure respirator performance against nanoparticles under simulated workplace conditions and to determine performance differences between respirators with different filter series (N versus P) and different filter efficiency levels (95 versus 100).
MATERIALS AND METHODS
Equipment and supplies
Respirator selection and test subjects
Eight NIOSH-approved respirator models (Table 1) were randomly selected from among models previously tested (Vo et al., 2012; Rengasamy et al., 2013) in our laboratory. Each respirator filter had a multilayer structure with the main layers of these filters composed of electrostatically charged polypropylene fibers; however, each filter had different characteristics, such as the number of layers, thickness, and hydrophilic/hydrophobic fiber materials.
Table 1.
Summary GM-SWPF and fifth percentile values by respirator model
| Respirator type | Class of filter | Respirator model | Respirator features | GM_SWPFa (± GSD) |
Fifth percentile |
|---|---|---|---|---|---|
| FFRs | N95 | N95-A | Cup, nonadjustable straps, metal nosepiece, one size | 103 ± 3.3 | 14 |
| N95-B | Cup, nonadjustable straps, metal nosepiece, one size | 94 ± 2.0 | 30 | ||
| P100 | P100-A | Cup, adjustable straps, exhalation valve, metal nosepiece, one size | 6586 ± 2.8 | 1207 | |
| P100-B | Cup, adjustable straps, exhalation valve, metal nosepiece, one size | 3200 ± 5.2 | 213 | ||
| EHRs | N95 | N95-A | S, M, L sizes, adjustable straps, exhalation valve | 136 ± 1.9 | 47 |
| N95-B | S, M, L sizes, adjustable straps, exhalation valve | 257 ± 1.9 | 88 | ||
| P100 | P100-A | S, M, L sizes, adjustable straps, exhalation valve | 8157 ± 2.9 | 1388 | |
| P100-B | S, M, L sizes, adjustable straps, exhalation valve | 9923 ± 2.9 | 1759 |
Total number of observations (n) of each respirator-model GM-SWPF data point = 75 (n = 1 model × 3 replicates × 25 subjects).
Twenty-five subjects (13 females and 12 males) participated in this study (Fig. 1). The age of the panel members ranged from 19 to 65 years. The NIOSH bivariate panel was used for placement of test subjects in specific face length by face width cells (Zhuang et al., 2007). This study was approved by the NIOSH Institutional Review Board (IRB) and all subjects gave written consent to participate.
Figure 1.
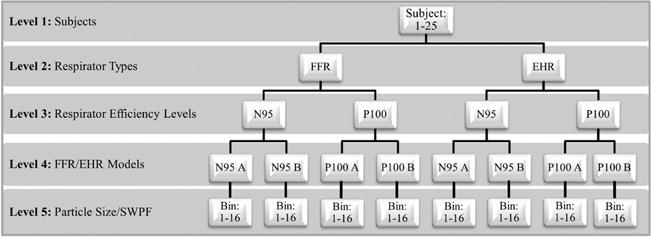
Schematic diagram of experimental study design for simulated workplace protection factors (SWPF) test.
Equipment and supplies for the fit test and SWPF test
Aerosol generator solutions: Two NaCl solutions in distilled water were used as generator solutions. The solution concentrations for the fit test generator and the SWPF test atomizer were 2 and 0.2%, respectively. These different solution concentrations were chosen to ensure that adequate particle concentrations were generated for the standard fit test as described by Lawrence et al. (2006) and the SWPF test as described by Vo and Zhuang (2013).
Fit test
A particle generator (Model 8026, TSI, Shoreview, MN) and a PortaCount Plus (Model 8038; TSI) were used for the fit test.
SWPF test
An aerosol chamber testing system (ACTS) consisting of an aerosol generation set, an exposure chamber system, and a particle detector component was used for the SWPF test (Fig. 2). The aerosol generation set has a six-jet atomizer (Model 9306, TSI), a Kr-85 aerosol neutralizer (Model 3054, TSI), and an ultrafine condensation particle counter (UCPC, model 3776, TSI) to track the particle concentration in the testing chamber. A compressed air supply for the generator was filtered with a high efficiency particulate air (HEPA) filter (Model 2074B, TSI). The chamber testing system consisted of an exposure chamber (Model 222–6, Dynatech, Albuquerque, NM, USA), a humidity/temperature sensor (Model RHXL3SD, Omega Engineering, Stamford, CT, USA), circulation fans, and a 14-cm diameter exhaust port. The exposure chamber height, width, and depth were 2.5 × 2.5 × 1.5 m, respectively. The chamber contained sufficient space for a human subject, with a respirator, to perform a SWPF test inside comfortably. The particle detector component consisted of two scanning mobility particle sizers (SMPSs, Model 3080 with Model-3772 CPCs, TSI). Two SMPSs were used simultaneously to measure the upstream (outside the respirator) and downstream (inside the respirator) test aerosol (Fig. 2).
Figure 2.
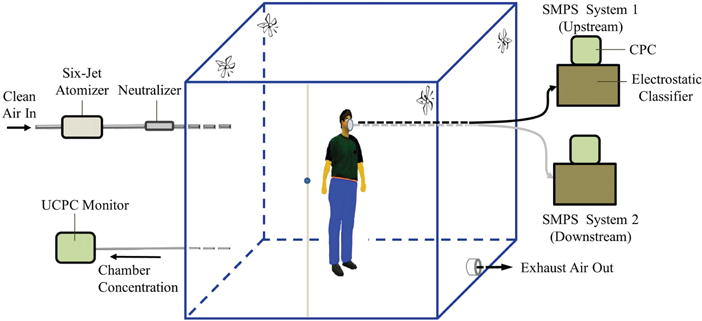
Schematic diagram of an aerosol chamber testing system: including an aerosol generator system with a particle concentration monitor, exposure chamber with an exhaust port, and particle detector systems [scanning mobility particle sizer (SMPS)].
Fit test and SWPF test procedures
The fit test procedure
A fit test was conducted under laboratory conditions for each subject and each respiratory protective device prior to the start of a SWPF test. A particle generator (Model 8026, TSI) was used to keep room concentration levels between 3000 and 8000 particles cm−3 for the fit test. When the laboratory particle concentrations reached the designated level, subjects trained by a test operator (the training included demonstrating how to don a respirator using the manufacturer’s user instructions) donned the FFR or EHR and connected the PortaCount sample line to the respirator. The fit test was initiated after the test operator assured that the respirator was properly donned by the test subject, including performance by the subject of the standard respirator user seal check. Subjects performed the eight exercises described in the OSHA standard fit test (OSHA, 2002). The eight exercises were performed in the following order: (i) normal breathing, (ii) deep breathing, (iii) turning head side to side, (iv) moving head up and down, (v) talking out loud, (vi) reaching for floor and ceiling, (vii) grimacing, and (viii) normal breathing. The fit factor (FF) was determined by the PortaCount Plus based on the ratio of the upstream and downstream concentrations of each exercise. A harmonic mean of the FFs measured for these exercises, except the grimace exercise (the grimace exercise was excluded from the overall FF calculation), was also obtained directly from the PortaCount. If the subject received a FF value of ≥100, the fit test was considered a pass. If the subject received a FF value of <100, the fit test was considered a failure. If the subject did not pass the fit test during the first trial, to ensure they passed, a test operator was required to help them don the respirator, adjust its head straps, and reshape its metal nosepiece (if equipped). Once a proper fit was achieved, the subject continued to don the respirator with the connector tube sealed using a clamp, and was escorted to the exposure chamber for the SWPF test.
The SWPF test procedure
A NaCl solution was aerosolized using the single jet mode of the six-jet atomizer at a dispersion of 30l min−1. The output aerosol was dried with 30% dilution air in an atomizer self-contained dilution system, followed by neutralizing with the Kr-85 charging source before entering into the exposure testing chamber (Fig. 2). The aerosol in the exposure chamber was mixed using four internal fans positioned on the top of four inner corners of the chamber (Fig. 2). Throughout the experiment, an UCPC tracked the total particle concentration at 1.5l min−1, and the climate conditions were tracked by a humidity/temperature sensor (Fig. 2). During particle generation and sampling, NaCl aerosol particles were continuously dispersed into the chamber, while the exhaust port was in the open position to remove excess air and maintain neutral pressure. When the NaCl aerosol concentration in the chamber stabilized at the exposure level of ~2 × 105 particles cm−3, the subject pre-donned with the respirator entered into the exposure chamber for the SWPF test.
After connecting the SMPS sample line to the respirator, the clamp on the connector tube was removed by the test operator to allow aerosol flow. The SWPF test was then performed using six exercises for 3 min each: (i) normal breathing, (ii) deep breathing, (iii) moving head side to side, (iv) moving head up and down, (v) bending at the waist, and (vi) a simulated laboratory-vessel cleaning motion. The simulated laboratory-vessel cleaning motion involved the subject moving their arms forward-down and backward-up in a shovel-scooping-like fashion, with a distance of about 30 cm at a rate of approximately one completed motion every 5 s to simulate a common workplace activity observed by Dahm et al. (2011). Test data was recorded and each individual exercise SWPF was calculated as a ratio of the upstream and downstream particle concentrations as in (1):
| (1) |
where SWPF, simulated workplace protection factor for a given exercise; i, exercise number; Cout, upstream particle concentration; Cin, downstream particle concentration
An overall SWPF for each respirator model obtained from the six individual SWPF exercises was derived from (2):
| (2) |
After completing testing with each respirator model, the subject removed the respirator and gave it to the test operator. The subject then donned the next respirator model and repeated the fit test and the SWPF test for all eight respirator models. This procedure was conducted three times for each respirator model for each subject on three different days.
DATA ANALYSIS
The data analysis was performed using an analysis of variance (ANOVA) model provided by the Statistical Analysis System version 9.3 (SAS Institute Inc., Cary, NC, USA). The ANOVA was also used for analyzing statistical computations, including overall SWPF, geometric mean (GM) SWPFs, and all pairwise SWPF comparisons. P < 0.05 were considered significant. The fifth percentile SWPF was computed from the formula GM/GSD1.645, where GSD equals the geometric standard deviation (Lenhart and Campbell, 1984).
RESULTS
Based on the particle size range of interest for this respirator performance study against nanoparticles, the size distribution range of 10–400 nm was measured. Within this size range, 96% of particles were centered between 28 and 350 nm with a mode of 82 nm, a count median diameter (CMD) of 60 nm, and GSD of 2.88 (Fig. 3).
Figure 3.
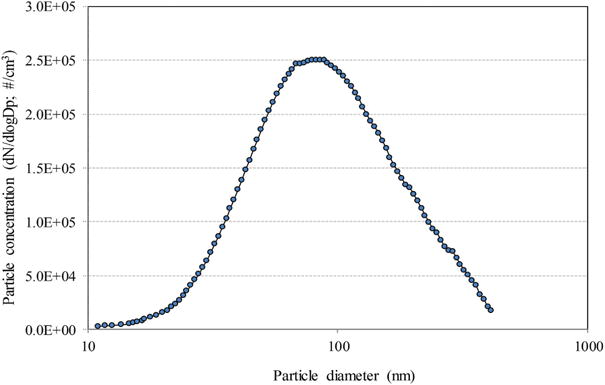
Size distribution of the NaCl aerosols in the exposure chamber measured using the SMPS.
All subjects passed the fit test with all FF values ≥100 with all N95 and P100 EHR models. All subjects also passed the fit test with two P100 FFR models; however, some subjects failed the fit test during the first trial with two N95 FFR models. Therefore, a test operator helped these test subjects with donning the N95 FFRs and reshaping the metal nosepiece to ensure the subjects passed their fit test with N95 FFRs before performing an SWPF test.
Table 1 is a summary of the respirator performance statistics (i.e. GM-SWPF, GSD, and fifth percentile) for the eight respirator models across the size range of 10–400 nm. The results show the GM-SWPF values for both N95 FFR models were the lowest level of performance with the GM-SWPF range of 94–103 and the SWPF fifth percentile range of 14–30 (Table 1). The two N95 EHR models had GM-SWPF values in the range of 136–257 and SWPF fifth percentiles in the range of 47–88 (Table 1). The GM-SWPF values of the two P100 FFR models provided the better level of performance with a GM-SWPF range of 3200–6586 and a SWPF fifth percentile range of 213–1207 (Table 1). Both P100 EHR models provided the greatest level of performance with a GM-SWPF range of 8157–9923 and a SWPF fifth percentile range of 1388–1759 (Table 1). In general, all class P100 respirators provided significantly higher SWPF values compared to class N95 respirators (all P < 0.05) for both FFR and EHR types (Table 1).
The average SWPF values of different respirator models (models A and B) within each class respirator (N95 or P100) across the particle size range of 10–400 nm are shown in Table 1. The results show that the SWPFs were not statistically different between the N95-A FFRs (GM-SWPF = 103) and the N95-B FFRs (GM-SWPF = 94) with P = 0.06; however, the SWPFs were statistically different between the P100-A FFRs (GM-SWPF = 6586) and the P100-B FFRs (GM-SWPF = 3200), the N95-A EHRs (GM-SWPF = 136) and the N95-B EHRs (GM-SWPF = 257), or the P100-A EHRs (GM-SWPF = 8157) and the P100-B EHRs (GM-SWPF = 9923) with all P < 0.05 (Table 1).
The respirator performance statistics for the different respirator filter classes (N95 and P100) for both EHR and FFR types as determined by the SWPF testing across the nanoparticle size range (10–100 nm) were determined and compared to the larger size range of 100–400 nm (Table 2). The results show that the GM-SWPFs for nanoparticles were significantly larger than those of larger particles (100–400 nm) (all P < 0.05), except N95 EHRs (P = 0.06). In general, the GM-SWPFs in both ranges had a similar trend order with the highest for the P100 EHRs, followed by P100 FFRs, N95 EHRs, and N95 FFRs (Table 2). All class P100 respirators in both ranges provided significantly higher SWPF values compared to class N95 respirators (all P < 0.05) for both EHR and FFR types (Table 2). The results also show that P100 and N95 EHRs exhibited better performance than P100 and N95 FFRs (all P < 0.05), respectively (Table 2).
Table 2.
GM-SWPF and fifth percentile values: nanoparticles versus larger particle range
| Respirator type | Class of filter | Size range: 10–100 nm
|
Size range: 100–400 nm
|
||
|---|---|---|---|---|---|
| GM_SWPF (± GSD) |
Fifth percentile | GM_SWPF (± GSD) |
Fifth percentile | ||
| FFR | N95 | 112 ± 2.5 | 45 | 83 ± 3.0 | 14 |
| P100 | 6595 ± 4.2 | 1574 | 3439 ± 4.5 | 292 | |
| EHRs | N95 | 196 ± 2.7 | 72 | 202 ± 1.9 | 68 |
| P100 | 11 800 ± 3.1 | 3777 | 6780 ± 2.9 | 1199 | |
Total number of observations of each respirator series GM-SWPF data point = 150 (n = 2 models in each series × 3 replicates × 25 subjects).
The average SWPF values as a function of particle diameter for the four combinations of filter classes and respirator types (N95 FFRs, P100 FFRs, N95 EHRs, and P100 EHRs) are shown in Fig. 4. These results show that the average SWPFs were the highest for the P100 EHRs, followed by P100 FFRs, N95 EHRs, and N95 FFRs (Fig. 4). All class P100 respirators provided significantly higher SWPF values compared to class N95 respirators (all P < 0.05) for both FFR and EHR types (Fig. 4). For all four combinations of filter classes and respirator types, the average SWPFs decreased with increasing particle diameter.
Figure 4.
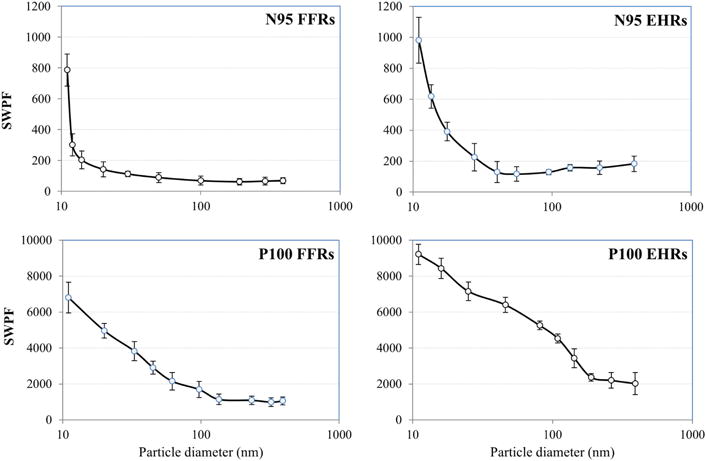
The average SWPF values (n = 150; 2 respirator models × 3 replicates × 25 subjects) as a function of particle diameter for the four combinations of filter classes and respirator types.
DISCUSSION
In general, all eight respirator models provided different values of SWPFs: EHR-P100 model-B > EHR-P100 model-A > FFR-P100 model-A > FFR-P100 model-B > EHR-N95 model-B > EHR N95 model-A > N95 FFR model-B > N95 FFR model-A. A possible explanation for the different values of SWPFs among eight respirator models is that these respirator models had different design features, such as sizes, shapes, and other different characteristics [i.e. a foam face seal (an additional foam piece attached to the surface perimeter of a respirator to create a seal against the wearer’s face) versus nonfoam face seal; metal nosepieces versus no metal nosepieces]. The performance levels of all eight models were also compared based on their fifth percentile SWPF values. The results revealed that the fifth percentile SWPFs for all models were different and had a similar trend as the GM SWPF values. All these respirators provided the expected levels of performance (fifth percentile SWPF > 10).
Class P100 respirators provided significantly higher SWPF values compared to class N95 respirators (all P < 0.05) for both FFR and EHR types. For the FFR type, the main reasons that the P100 FFRs performed better than N95 FFRs would be: (i) P100 FFRs had a foam face seal against the wearer’s face while N95 FFRs did not have a foam face seal and (ii) P100 FFRs contained a 100 efficiency level filter while N95 FFRs contained a 95 efficiency level filter. For the EHR type, although both P100 and N95 EHRs had the half-mask shape, P100 EHRs contained a 100 efficiency level filter while N95 EHRs contained a 95 efficiency level filter. Therefore, respirators with 100 efficiency level filters provided a high level of efficiency against the 10–400 nm NaCl particles used in the SWPF tests.
For a given filter type (N95 or P100), the results show that EHRs always performed better than FFRs (all P < 0.05). Differences in design features, such as sizes (three different sizes for EHRs versus one size for FFRs), shapes (half-mask shape for EHRs versus cup shape for FFRs), and metal nosepieces (no metal nosepiece for EHRs versus metal nosepieces for FFRs) could be the reason EHRs provided a higher performance than the FFRs. It should be noted that all FFRs used in this study had metal nosepieces (Table 1), so the wearer may not have remolded the nosepiece the same way during each donning, causing different SWPF values between tests. For class N95 respirators, the EHRs were equipped with adjustable head straps, whereas the N95 FFRs had only nonadjustable straps (Table 1). Adjustable head straps may allow a better customized seal because they can be tightened to a high degree of accuracy for fitting a wider variety of users and they may allow users to maintain a secure tight and comfortable seal of the respirators. Thus, having adjustable head straps could have contributed to the assessment that the N95 EHRs had a higher performance than the N95 FFRs. For both N95 and P100 classes used in this study, the FFRs came in one configuration, cup-shaped and one size, while the EHRs came in three different sizes (large, medium, and small sizes) (Table 1). Therefore, EHRs with different sizes provided a better fit against the different face sizes of the human subjects, resulting in greater performance.
When comparing the average SWPF values as a function of particle diameter for the four combinations of filter classes and respirator types (N95 FFRs, P100 FFRs, N95 EHRs, and P100 EHRs), it was found that the average SWPFs decreased with increasing particle diameters for all four combination groups. A possible explanation for it is that NaCl particles are hygroscopic. With the relative humidity (RH) inside the respirator at ~99%, the particles could have absorbed moisture and either grew or agglomerated, decreasing the particle concentrations of small particles and increasing the particle concentrations of larger particles inside the respirator. It must be noted that some inhaled NaCl particles which were not adsorbed by the body would return to the downstream sample area (inside the respirator) during exhalation; therefore, the inhaled NaCl particles returned from the body during exhalation would also increase the particle concentrations of larger particles inside the respirator. Interestingly, Rengasamy and co-workers reported that the most penetrating particle size (MPPS) through the class N95 and class P100 respirators was around 30–60 nm when these respirator classes were tested against a monodisperse NaCl (20–400 nm) at 85 l min−1 (Rengasamy et al., 2009). The MPPS range of 30–60 nm (Rengasamy et al., 2009) does not show in the results of our study. The main reason for the differences is that in our study FSL is the dominant cause of leakage into the class N95 and P100 respirators tested.
This study had several limitations as follows. A limited number of respirator models were tested, where other models that are also used in the workplace may perform better or worse than those selected. Although the SWPF exercise regime used in this study consisted of six exercises, these test exercises were centered around protection achieved in a working situation where respirator wear time was very short and associated with a single repetitive task at a relatively low metabolic rate; therefore, this SWPF exercise regime may not be representative of work activities in actual work environments. Another limitation might be the SWPF test was performed using NaCl aerosols, neutralized aerosols, and the particles were focused in the range of 10–400 nm, which may not be representative of actual workplace particles.
CONCLUSIONS
This study has shown there is a difference in the level of performance provided by class N95 and class P100 respirators. All class P100 respirators provided significantly higher SWPF values compared to class N95 respirators for both FFR and EHR types. In general, the levels of performance were the highest for the P100 EHRs, followed by P100 FFRs, N95 EHRs, and N95 FFRs. All these respirators provided expected levels of performance (fifth percentile were >10). This trend holds true for nanoparticles (10–100 nm), larger size particles (100–400 nm), and the ‘all size’ range (10–400 nm). All respirators provided better or similar performance levels for nanoparticles as compared to larger particles in the 100–400 nm size range. Results from this study also revealed that the levels of performance increased with decreasing particle diameters.
Acknowledgments
The authors thank Dr Mark Hoover (NIOSH/DRDS, Morgantown, WV, USA), Dr Peter A. Jaques (URS Corp., Pittsburgh, PA, USA), Mr Michael Bergman, and Dr Ron Shaffer (NIOSH/NPPTL, Pittsburgh, PA, USA), for their valuable review comments on the manuscript. The authors also want to thank Mr Lee Portnoff (URS Corp., Pittsburgh, PA, USA) for his valuable contributions to the project.
FUNDING
Funding for this study was provided as part of employment with the Centers for Disease Control and Prevention (CDC).
Footnotes
DISCLAIMER
The findings and conclusions in this manuscript are those of the authors and do not necessarily represent the views of the National Institute for Occupational Safety and Health (NIOSH). Mention of company names or products does not constitute endorsement by NIOSH.
References
- Baroli B, Ennas MG, Loffredo F, et al. Penetration of metallic nanoparticles in human full thickness skin. J Invest Dermatol. 2007;127:1701–12. doi: 10.1038/sj.jid.5700733. [DOI] [PubMed] [Google Scholar]
- Birch ME, Ku BK, Evans DE, et al. Exposure and emissions monitoring during carbon nanofiber production. Part I: elemental carbon and iron-soot aerosols. Ann Occup Hyg. 2011;55:1016–36. doi: 10.1093/annhyg/mer073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- British Standard EN 529. Respiratory Protective Devices - Recommendations for Selection, Use, Care and Maintenance - Guidance Document. 2005 Available at http://products.ihs.com/Ohsis-SEO/768159.html. Accessed 1 October 2014.
- Brooks RD, Rajagopalan S, Arden Pope C, III, et al. Particulate matter air pollution and cardiovascular disease: An update to the scientific statement from the American Heart Association. Circulation. 2010;121:2331–78. doi: 10.1161/CIR.0b013e3181dbece1. [DOI] [PubMed] [Google Scholar]
- Byrne JD, Baugh JA. The significance of nanoparticles in particle-induced pulmonary fibrosis. Mcgill J Med. 2008;11:43–50. [PMC free article] [PubMed] [Google Scholar]
- CSA (Canadian Standards Association) CAN/CSA-Z94.4-11: Selection, use, and care of respirators. Available at http://www.ccohs.ca/products/csa/27016392011. Accessed 1 October 2014.
- Dahm MM, Evans DE, Schubauer-Berigan MK, et al. Occupational exposure assessment in carbon nanotube and nanofiber primary and secondary manufacturers: mobile direct-reading sampling. Ann Occup Hyg. 2013;57:328–44. doi: 10.1093/annhyg/mes079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahm M, Yencken M, Schubauer-Berigan MK. Exposure control strategies in the carbonaceous nanomaterial industry. Journal of Occupational and Environmental Medicine. 2011;53:S68–S73. doi: 10.1097/JOM.0b013e31821b1d3b. [DOI] [PubMed] [Google Scholar]
- Grinshpun SA, Haruta H, Eninger RM, et al. Performance of an N95 filtering facepiece particulate respirator and a surgical mask during human breathing: two pathways for particle penetration. J Occup Environ Hyg. 2009;6:593–603. doi: 10.1080/15459620903120086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han DH, Lee J. Evaluation of particulate filtering respirators using inward leakage (IL) or total inward leakage (TIL) testing–Korean experience. Ann Occup Hyg. 2005;49:569–74. doi: 10.1093/annhyg/mei034. [DOI] [PubMed] [Google Scholar]
- Lawrence RB, Duling MG, Calvert CA, et al. Comparison of performance of three different types of respiratory protection devices. J Occup Environ Hyg. 2006;3:465–74. doi: 10.1080/15459620600829211. [DOI] [PubMed] [Google Scholar]
- Lenhart SW, Campbel DL. Assigned protection factors for two respirator types based upon workplace performance testing. Ann Occup Hyg. 1984;28:173–82. doi: 10.1093/annhyg/28.2.173. [DOI] [PubMed] [Google Scholar]
- Liu BYH, Lee J-K, Mullins H, et al. Respirator leak detection by ultrafine aerosols: a predictive model and experimental study. Aerosol Sci Tech. 1993;19:15–26. [Google Scholar]
- NIOSH (National Institute for Occupational Safety and Health) (NIOSH Publication No. 2005-100).NIOSH Respirator Selection Logic 2004. Available at http://www.cdc.gov/niosh/docs/2005–100. Accessed 1 October 2014.
- Occupational Safety and Health Administration (OSHA) (DTSEM FS-3634, 04/2013).OSHA Fact Sheet: Working Safely with Nanomaterials. Available at https://www.osha.gov/Publications/OSHA_FS-3634.pdf. Accessed 2 October 2014.
- OSHA. “Respiratory Protection,” Code of Federal Regulations Title 29, Part 1910.134. 2002:434–440. [Google Scholar]
- Rengasamy S, Eimer B, Shaffer RE. Comparison of nanoparticle filtration performance of NIOSH-approved and CE marked filtering facepiece respirators. Ann Occup Hyg. 2009;53:117–28. doi: 10.1093/annhyg/men086. [DOI] [PubMed] [Google Scholar]
- Rengasamy S, Miller A, Vo E, et al. Filter performance degradation of electrostatic N95 and P100 filtering face-piece respirators by dioctyl phthalate aerosol loading. J Eng Fibers Fabrics. 2013;8:62–9. [Google Scholar]
- Shaffer RE, Rengasamy S. Respiratory protection against airborne nanoparticles: a review. J Nanopart Res. 2009;11:1661–72. [Google Scholar]
- Shvedova AA, Kisin ER, Porter D, et al. Mechanism of pulmonary toxicity and medical applications of carbon nanotubes: two faces of Janus? Pharmacol Ther. 2009;121:192–204. doi: 10.1016/j.pharmthera.2008.10.009. [DOI] [PubMed] [Google Scholar]
- Vo E, Shaffer RE. Development and characterization of a new test system to challenge personal protective equipment with virus-containing particles. J Int Soc Respir Protect. 2012;29:13–29. [Google Scholar]
- Vo E, Zhuang Z. Development of a new test system to determine penetration of multi-walled carbon nanotubes through filtering facepiece respirators. J Aerosol Sci. 2013;61:50–9. doi: 10.1016/j.jaerosci.2013.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkes AR. Comparison of two techniques for measuring penetration of sodium chloride particles through breathing system filters. Br J Anaesth. 2002;89:541–45. doi: 10.1093/bja/aef231. [DOI] [PubMed] [Google Scholar]
- Zhuang Z, Bergman M, Eimer B, et al. Laboratory face seal leakage evaluation of N95 filtering facepiece respirators against nanoparticles and “all size” particles. J Occup Environ Hyg. 2013;10:496–504. doi: 10.1080/15459624.2013.818237. [DOI] [PubMed] [Google Scholar]
- Zhuang Z, Bradtmiller B, Shaffer RE. New respirator fit test panels representing the current U.S. civilian workforce. J Occup Environ Hyg. 2007;4:647–59. doi: 10.1080/15459620701497538. [DOI] [PubMed] [Google Scholar]


