Abstract
Objective
The effective components of interventions for reducing excessive gestational weight gain (GWG) remain to be identified. This study investigated the socio-demographic, physical, psychosocial, and environmental correlates of online GWG tracking and its independent association GWG outcomes.
Methods
898 women in the intervention arms of a randomized trial assessing the effectiveness of an integrated online and mobile phone behavioral intervention to decrease the prevalence of excessive GWG were included in this secondary analysis. Data were analyzed using chi-square analysis and modified Poisson and linear regression approaches.
Results
Only 16.5% of low income (Medicaid eligible) women consistently tracked GWG as did 34.2% of not-low income women. More highly educated, older, and white women were more likely to be consistent weight gain trackers. Among not-low income women, consistent weight gain tracking was associated with 2.35 kg less GWG (95% CI: −3.23 to −1.46 kg; p <0.0001) and a reduced risk of excessive GWG (RR 0.73; 95% CI: 0.59 to 0.89; p = 0.002).
Conclusion
Electronic tracking of GWG is an effective component of e- and m-health interventions aiming to decrease the prevalence of excessive GWG in not-low income women. Income-group specific motivators are needed to increase the prevalence of weight gain tracking.
Keywords: Weight tracking, gestational weight gain, pregnancy, online intervention
Introduction
Maternal obesity and excessive gestational weight gain (GWG) are associated with many adverse pregnancy and birth outcomes. In addition, they increase the risk of obesity in both mother and baby (1–3). A recent Cochrane review found diet and/or exercise interventions during pregnancy reduced the risk of excessive GWG by 20% (4).
Electronic health (e-Health) interventions have been shown to be efficacious across cognitive, some behavioral, and emotional outcomes (5). However, several recent metaanalyses of e-learning and web-based weight management interventions have yielded mixed results. Harris et al. (6) concluded that e-learning interventions did not have a significant positive effect on body mass index (BMI) or body weight. Arem and Irwin (7) in their review of internet-delivered weight loss and maintenance programs found intervention results ranging from no weight loss to an average loss of 7.6 kg. Kodama et al. (8) concluded from their metaanalysis that the intervention effects were inconsistent, and depended on the type of usage of the internet and the time period of use.
The recent Cochrane review mentioned above suggested that e-health interventions hold potential for addressing maternal obesity and excessive GWG (4). However, there is currently limited knowledge on the effectiveness of e-health interventions in preventing excessive GWG and even less is known about the effectiveness of specific intervention components (9). Self-monitoring is generally considered to be an important component of behavioral weight management interventions. Self-weighing is recommended as part of the AHA/ACC/TOS Guidelines for Managing Overweight and Obesity in Adults from the National Heart, Lung and Blood Institute (10). A recent systematic review of longitudinal studies of self-weighing and weight outcomes found more frequent self-weighing was associated with greater weight loss, less weight regain, and better weight gain prevention (11). Electronic self-monitoring has been found to be related to greater adherence to self-monitoring over a 6 month time period compared to paper monitoring, but not to better weight outcomes (12).
Several studies have been undertaken in Great Britain and Australia to encourage pregnant women to weigh themselves at time intervals between the first and last prenatal care visits, which are the only times they are measured by health care providers (13–15). Harrison and colleagues (13) found a significant difference in GWG at 28 weeks between women who engaged in self-weighing and those who did not in a randomized trial sample of women who were overweight and obese (5.66 ± 2.6 kg vs. 7.03 ± 3.56 kg, p = 0.02). Jeffries and colleagues (14) conducted a randomized controlled trial of self-weighing and weight tracking at 16, 20, 24, 28, 30, 32, 34 weeks gestation and found no overall positive effect. In a randomized controlled trial with pregnant women who were overweight and obese, with serial self-weighing and simple dietary advice as the intervention, there was no difference in mean GWG between treatment groups (−0.9 kg, 95% CI −2.0 to 0.24) (15).
A recent paper that used data from the trial reported here examined latent class-derived usage patterns of all intervention and control group features and their relationship to GWG (16). No significant associations were found between usage patterns and GWG in the control group. In the intervention group and among higher income women only, the combined group of super users (who had high use of all features) plus consistent weight trackers gained significantly less during pregnancy than the other use groups combined (normal BMI: −1.49 kg, p = 0.002; overweight and obese BMI: −2.17 kg, p = 0.003) (16). The common component across the two high use groups was consistent use of the weight gain tracker, indicating a need to better understand who used the online GWG tracking tool and the relationship of use to weight gain outcomes.
The aim of this study is to examine the relationship between electronic weight gain tracking and weight gain outcomes in a sample of pregnant women in the US. More specifically, this paper addresses the following questions: (1) What are the socio-demographic, physical, psychosocial, and environmental characteristics of pregnant women who use electronic weight gain tracking during pregnancy and (2) What is the relationship between weight gain tracking and GWG outcomes independent of the characteristics that predict tracking?
Methods
Sample
Data for this study come from a large randomized controlled effectiveness trial of an integrated mobile phone and online intervention aimed at preventing excessive GWG and postpartum weight retention (17–18). Pregnant women were eligible for the trial if they were 18–35 years of age, had normal to obese class I body mass index (BMI), and were relatively healthy without weight-affecting medical conditions. In addition, participants had to (1) consent at or before 20 weeks’ gestation, (2) be available for a 24 month intervention, (3) plan to carry their pregnancy to term and keep the baby, (4) read and understand English, and (5) have an email address. Upon consent, women were electronically randomized via computer to two identical intervention arms and one control arm within two income (low defined by Medicaid eligibility during pregnancy and not-low) and two BMI (normal BMI and overweight plus obese class 1 BMI) groups (four strata).
The sample includes women in the intervention arms who met study eligibility criteria and participated during pregnancy as indicated by at least 1 website login or completion of the baseline questionnaire. Among this group, only those who had a singleton pregnancy that lasted at least 20 weeks were included in the analysis, n=898. The study protocol was approved by the University of Rochester Research Subject Review Board and the Cornell University Institutional Review Board.
The intervention
All study participants were sent an email describing the study and the features and tools available on the study website. E-mail, postcard, and telephone reminders were used as prompts to encourage participants to visit the website the first time. A $5 incentive was also given for the first visit to the study website.
Fishbein and Yzer’s Integrative Model of Behavioral Prediction (19) and Fogg’s Behavior Model for Persuasive Design (20) were the guiding theoretical frameworks for the intervention. The website featured blogs, local resources, articles, frequently asked questions (FAQs), and event reminders that were available to women in the intervention and control arms (21). In addition, intervention arm participants had access to a weight gain tracker and diet and physical activity goal-setting and self-monitoring tools which were hypothesized to be the active ingredients of the intervention. The GWG tracker was based in the Institute of Medicine (IOM) GWG guidelines (2). It used a woman’s weight and height at recruitment for determining prepregnancy BMI and the appropriate GWG goal and graph for each women. Women could enter weights via text message or online, with each weight plotted on the women’s personal graph. After each weight entry, the woman was informed through her device if her weight was on or off track. The diet and physical activity goal setting tools were each multi-component tools that included assessment of problem or need for change, setting a goal, identification of personal strategies and barriers, self-monitoring, and rewards. Intervention participants were emailed weekly from randomization until delivery with reminders to login to see new content and reminders to use the weight gain tracker, diet and physical activity goal setting tools.
Measures and data collection
Use of the online features was automatically captured by the website. For some features, amount of use in relation to expected use was incorporated into the usage measure. Consistent use was expected for entry of weights into the weight gain tracker, an a priori decision. We expected women to track their weight in 30-day intervals based on the standard schedule for prenatal care visits. However, to allow for possible delays in the scheduling of appointments, we used 45-day intervals from time of enrollment to delivery. If a woman entered a weight during each of the 45-day intervals that she participated in the study she was categorized as a consistent tracker. If she entered a weight during at least of half of the intervals, she was categorized as an almost consistent tracker. If a woman entered weights in less than half of the intervals or she never entered a weight during pregnancy, she was categorized as an inconsistent tracker.
Socio-demographic, behavioral, psychosocial, and environmental data were collected through an online survey at baseline. Figure 1 shows the predictors of weight tracking from the Integrative Model of Behavioral Prediction (19) that were included in this study. Questions from the EARLY trials consortium were used for measuring socio-demographic characteristics, in-home access to a scale, and frequency of self-weighing (17). Items for measuring the other constructs predicting the behavior of weight tracking came from previous research on gestational weight gain (22) and all were pre-tested in the population for this project.
Figure 1.
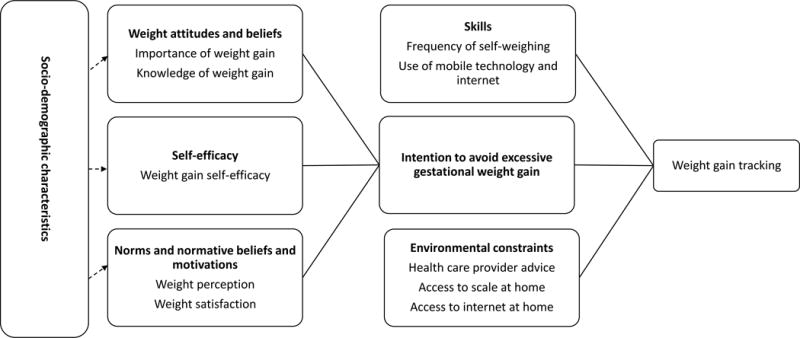
Variables from the Integrative Model of Behavioral Prediction (19) considered for models of consistent tracking and weight outcomes.
GWG data were obtained through an audit of the participant’s prenatal, labor and delivery, and 6 week postpartum medical record. Health data were abstracted from the medical record.
Statistical analysis
Total GWG was calculated as the difference between the first weight and the last weight in pregnancy. Overall, 13% of the sample did not have sufficient weight information in the medical record to yield a valid measure of GWG. Sufficient weight information required having both a measured weight < 14 weeks and ≥ 37 weeks gestation. Missing data were handled using multiple imputation to address issues of bias (23) that may result from analyzing only complete cases, using SAS Proc MI and MIANALYZE. Sixty imputed data sets were created for the primary analysis and the models presented below. Next, the binary outcome of excessive total GWG was calculated using the Institute of Medicine (IOM) guidelines for each BMI group as determined at randomization. For each of the three BMI groups, the cut-off values for excessive total GWG are as follows: normal BMI - > 16 kg (35 pounds); overweight BMI - > 11.5 kg (25 pounds); and obese class 1 BMI - > 9 kg (20 pounds).
Among participants with measured (not imputed) GWG data, chi-square analysis was used to identify the socio-demographic, physical, psychosocial and environmental predictors of consistent weight gain tracking. A modified Poisson regression approach (24) was used to identify the independent predictors of consistent tracking from the variables identified in the binary analyses using the imputed data. All analyses were conducted separately in low and not-low income groups.
The Mantel-Haenszel chi-square statistic was used to evaluate the association between consistency of tracking and the binary outcome of prevalence excessive total GWG, and for total GWG in kg, the Kruskal Wallis test was used for this purpose. Least-squares multiple regression models assessed the mean difference in total GWG (kg) between consistent weight gain trackers compared to non-consistent trackers (all the other categories combined) within income groups, controlling for the earlier identified predictors of consistent tracking. Similarly, a modified Poisson regression approach (24) was used to estimate the relative risk (RR) for the categorical outcome variable, proportion of women with excessive total GWG. All weight outcome models used the imputed data sets and were adjusted for the following covariates: BMI, age, race, and parity, as well as pregnancy timing variables including gestational age at delivery, the weeks between the first and last pregnancy weight, and the weeks between the last pregnancy weight and delivery. Significance level was set at p-value of < 0.05.
Results
Predictors of weight gain tracking
In this sample from a large randomized effectiveness trial, more than twice as many not-low income women (34.2%) compared to low income (Medicaid eligible) women (16.5%) tracked their weight gain consistently during pregnancy (Table 1). Of the socio-demographic and physical characteristics considered in the bivariate analyses, age, race, and education were significantly (p < 0.05) associated with consistent weight gain tracking in both income groups. Marital status was significantly associated with consistent tracking in the not-low income women, while there was a trend (p = 0.06) toward an association in low income women. Early pregnancy body mass index (BMI) and parity were not significantly associated with weight gain tracking in either income group.
Table 1.
Characteristics of participants by consistency of weight gain tracking within income groups
| Low income womena | Not low income women | ||||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Characteristic | Total sample (N=898) | Low income sample (N=351) | Consistent trackers N=58 (16.5%) | Non-consistent trackers N=293 (83.5%) | P-value b | Not-low income sample (N=547) | Consistent trackers N=187 (34.2%) | Non-consistent trackers N=360 (65.8%) | P-value b |
|
Socio-demographic and physical characteristics
| |||||||||
| Body mass index (BMI) | 0.79 | 0.25 | |||||||
| Normal | 480 (53.5)c | 173 (49.3) | 29 (16.8) | 144 (83.2) | 307 (56.1) | 114 (37.1) | 193 (62.9) | ||
| Overweight | 278 (31.0) | 120 (34.2) | 18 (15.0) | 102 (85.0) | 158 (28.9) | 47 (29.8) | 111 (70.3) | ||
| Obese | 140 (15.6) | 58 (16.5) | 11 (19.0) | 47 (81.0) | 82 (15.0) | 26 (31.7) | 56 (68.3) | ||
| Age at entry | 0.003 | 0.01 | |||||||
| Less than 25 y | 259 (28.8) | 188 (53.6) | 24 (12.8) | 164 (87.2) | 71 (13.0) | 13 (18.3) | 58 (81.7) | ||
| 25 to 29 y | 303 (33.7) | 102 (29.1) | 15 (14.7) | 87 (85.3) | 201 (36.8) | 72 (35.8) | 129 (64.2) | ||
| 30 y and older | 336 (37.4) | 61 (17.4) | 19 (31.2) | 42 (68.9) | 275 (50.3) | 102 (37.1) | 173 (62.9) | ||
| Race | 0.001 | 0.001 | |||||||
| White | 607 (72.1) | 141 (46.1) | 33 (23.4) | 108 (76.6) | 466 (86.9) | 173 (37.1) | 293 (62.9) | ||
| Black (African American) | 178 (21.1) | 142 (46.4) | 11 (7.8) | 131 (92.3) | 36 (6.7) | 3 (8.3) | 33 (91.7) | ||
| All other races | 57 (6.8) | 23 (7.5) | 4 (17.4) | 19 (82.6) | 34 (6.3) | 8 (23.5) | 26 (76.5) | ||
| Missing (n) | 56 | 45 | 10 | 35 | 11 | 3 | 8 | ||
| Marital status | 0.06 | 0.02 | |||||||
| Single, including divorced | 136 (15.3) | 116 (33.6) | 13 (11.2) | 103 (88.8) | 20 (3.7) | 2 (10.0) | 18 (90.0) | ||
| Married and cohabitating | 756 (84.8) | 229 (66.4) | 44 (19.2) | 185 (80.8) | 527 (96.3) | 185 (35.1) | 342 (64.9) | ||
| Missing (n) | 6 | 6 | 1 | 5 | 0 | 0 | 0 | ||
| Parity | 0.80 | 0.52 | |||||||
| Nulliparous | 416 (46.4) | 148 (42.2) | 26 (17.6) | 122 (82.4) | 268 (49.1) | 86 (32.1) | 182 (67.9) | ||
| Primi-parous | 298 (33.2) | 106 (30.2) | 18 (17.0) | 88 (83.0) | 192 (35.2) | 68 (35.4) | 124 (64.6) | ||
| Multi-parous | 183 (20.4) | 97 (27.6) | 14 (14.4) | 83 (85.6) | 86 (15.8) | 33 (38.4) | 53 (61.6) | ||
| Missing (n) | 1 | 0 | 0 | 0 | 1 | 0 | 1 | ||
| Education | 0.002 | 0.002 | |||||||
| High school or less | 185 (22.4) | 145 (48.7) | 16 (11.0) | 129 (89.0) | 40 (7.6) | 9 (22.5) | 31 (77.5) | ||
| Some college | 235 (28.5) | 115 (38.6) | 29 (25.2) | 86 (74.8) | 120 (22.8) | 30 (25.0) | 90 (75.0) | ||
| College graduate | 405 (49.1) | 38 (12.8) | 12 (31.6) | 26 (68.4) | 367 (69.6) | 149 (40.3) | 219 (59.7) | ||
| Missing (n) | 53 | 1 | 52 | 20 | 0 | 20 | |||
|
Intention | |||||||||
| Intended amount of GWG d | 0.97 | 0.03 | |||||||
| > IOM guidelines e | 191 (22.7) | 72 (23.1) | 12 (16.7) | 60 (83.3) | 119 (22.5) | 37 (31.1) | 82 (68.9) | ||
| Within IOM guidelines | 559 (66.4) | 196 (62.8) | 35 (17.9) | 161 (82.1) | 363 (68.5) | 139 (38.3) | 224 (61.7) | ||
| < IOM guidelines | 92 (10.9) | 44 (14.1) | 8 (18.2) | 36 (81.8) | 48 (9.1) | 10 (20.8) | 38 (79.2) | ||
| Missing (n) | 56 | 39 | 3 | 36 | 17 | 1 | 16 | ||
|
Skills | |||||||||
| Self-weighing | |||||||||
| Frequency of weighing | 0.004 | 0.15 | |||||||
| Once a year or less | 134 (15.7) | 62 (19.2) | 8 (12.8) | 54 (87.1) | 72 (13.5) | 27 (37.5) | 45 (62.5) | ||
| Every couple of months | 131 (15.3) | 50 (15.5) | 5 (10.0) | 45 (90.0) | 81 (15.2) | 23 (28.4) | 58 (71.6) | ||
| About once a month | 243 (28.4) | 112 (34.7) | 15 (13.4) | 97 (86.6) | 131 (24.6) | 43 (32.8) | 88 (67.2) | ||
| About once a week | 263 (30.7) | 79 (24.5) | 21 (26.6) | 58 (73.4) | 184 (34.5) | 63 (34.2) | 121 (65.8) | ||
| About once a day or more | 85 (9.9) | 20 (6.2) | 8 (40.0) | 12 (60.0) | 65 (12.2) | 31 (47.7) | 34 (52.3) | ||
| Missing (n) | 42 | 28 | 1 | 27 | 14 | 0 | 14 | ||
| Mobile/web technology usage | |||||||||
| Type of cell phone | 0.98 | 0.001 | |||||||
| Smart phone | 552 (64.6) | 195 (60.4) | 35 (18.0) | 160 (82.0) | 357 (67.1) | 106 (29.7) | 251 (70.3) | ||
| Cell phone and no internet | 251 (29.4) | 87 (26.9) | 16 (18.4) | 71 (81.6) | 164 (30.8) | 78 (47.6) | 86 (52.4) | ||
| Do not own a cell phone | 52 (6.1) | 41 (12.7) | 7 (17.1) | 34 (82.9) | 11 (2.1) | 1 (9.1) | 10 (90.9) | ||
| Missing (n) | 43 | 28 | 0 | 28 | 15 | 2 | 13 | ||
| Frequency of sending or receiving text messages | 0.24 | 0.08 | |||||||
| A few times a week or less | 127 (14.9) | 35 (10.8) | 4 (11.4) | 31 (88.6) | 92 (17.3) | 36 (39.1) | 56 (60.9) | ||
| A couple of times a day | 226 (26.4) | 61 (18.9) | 15 (24.6) | 46 (75.4) | 165 (31.0) | 67 (40.6) | 98 (59.4) | ||
| Many times a day | 450 (52.6) | 186 (57.6) | 32 (17.2) | 154 (82.8) | 264 (49.6) | 81 (30.7) | 183 (69.3) | ||
| Do not own a cell phone | 52 (6.1) | 41 (12.7) | 7 (17.1) | 34 (82.9) | 11 (2.1) | 1 (9.1) | 10 (90.9) | ||
| Missing (n) | 43 | 28 | 0 | 28 | 15 | 2 | 13 | ||
| Use any pregnancy apps or websites | 0.12 | 0.55 | |||||||
| Yes | 447 (49.8) | 126 (35.9) | 26 (20.6) | 100 (79.4) | 321 (58.7) | 113 (35.2) | 208 (64.8) | ||
| No | 451 (50.2) | 25 (64.1) | 32 (14.2) | 193 (85.8) | 226 (41.3) | 74 (32.7) | 152 (67.3) | ||
| Number of pregnancy apps or websites used | 0.29 | 0.08 | |||||||
| 0 | 451 (50.2) | 225 (64.1) | 32 (14.2) | 193 (85.8) | 226 (41.3) | 74 (32.7) | 152 (67.3) | ||
| 1 | 307 (34.2) | 90 (25.6) | 18 (20.0) | 72 (80.0) | 217 (39.7) | 85 (39.2) | 132 (60.8) | ||
| ≥ 2 | 140 (15.6) | 36 (10.3) | 8 (22.2) | 28 (77.8) | 104 (19.0) | 28 (26.9) | 76 (73.1) | ||
|
Environmental constraints | |||||||||
| Received weight advice from health care provider | 0.22 | 0.04 | |||||||
| Yes | 297 (34.3) | 102 (31.1) | 22 (31.6) | 80 (78.4) | 195 (36.3) | 57 (29.2) | 138 (70.8) | ||
| No | 568 (65.7) | 226 (68.9) | 36 (15.9) | 190 (84.1) | 342 (63.7) | 130 (38.0) | 212 (62.0) | ||
| Missing (n) | 33 | 23 | 0 | 23 | 10 | 0 | 10 | ||
| Access to scale at home | 0.11 | 0.77 | |||||||
| Yes | 527 (61.5) | 142 (44.1) | 31 (21.8) | 111 (78.2) | 385 (72.0) | 136 (35.3) | 249 (64.7) | ||
| No | 330 (38.5) | 180 (55.9) | 27 (15.0) | 153 (85.0) | 150 (28.0) | 51 (34.0) | 99 (66.0) | ||
| Missing (n) | 41 | 29 | 0 | 29 | 12 | 0 | 12 | ||
| Frequency of accessing the internet from home | 0.003 | 0.99 | |||||||
| A few times a week or less | 237 (27.7) | 126 (39.0) | 12 (9.5) | 114 (90.5) | 111 (20.8) | 39 (35.1) | 72 (64.9) | ||
| Most days of the week | 178 (20.8) | 61 (18.9) | 11 (18.0) | 50 (82.0) | 117 (21.9) | 40 (34.2) | 77 (65.8) | ||
| Everyday | 442 (51.6) | 136 (42.1) | 35 (25.7) | 101 (74.3) | 306 (57.3) | 106 (34.6) | 200 (65.4) | ||
| Missing (n) | 41 | 28 | 0 | 28 | 13 | 2 | 11 | ||
|
Psychosocial predictors of intention | |||||||||
| Weight attitudes and beliefs | |||||||||
| Importance of intended GWG d | 0.57 | 0.70 | |||||||
| Very important | 146 (17.3) | 69 (22.0) | 11 (15.9) | 58 (84.1) | 77 (14.5) | 23 (29.9) | 54 (70.1) | ||
| Important | 372 (44.1) | 122 (39.0) | 26 (21.3) | 96 (78.7) | 250 (47.2) | 91 (36.4) | 159 (63.6) | ||
| Neutral | 267 (31.7) | 97 (31.0) | 14 (14.4) | 83 (85.6) | 170 (32.1) | 60 (35.3) | 110 (64.7) | ||
| Unimportant | 58 (6.9) | 25 (8.0) | 4 (16.0) | 21 (84.0) | 33 (6.2) | 10 (30.3) | 23 (69.7) | ||
| Missing (n) | 55 | 38 | 3 | 35 | 17 | 3 | 14 | ||
| Knowledge of appropriate GWG d | 0.65 | 0.02 | |||||||
| > IOM guidelines e | 226 (27.1) | 86 (28.0) | 17 (19.8) | 69 (80.2) | 140 (26.6) | 41 (21.3) | 99 (70.7) | ||
| Within IOM guidelines | 539 (64.6) | 189 (61.6) | 33 (17.5) | 156 (82.5) | 350 (66.4) | 138 (39.4) | 212 (60.6) | ||
| < IOM guidelines | 69 (8.3) | 32 (10.4) | 4 (12.5) | 28 (87.5) | 37 (7.0) | 8 (21.6) | 29 (78.4) | ||
| Missing (n) | 64 | 44 | 4 | 40 | 20 | 0 | 20 | ||
| Self-efficacy | |||||||||
| Able to control GWG d | 0.001 | 0.54 | |||||||
| Sure | 341 (39.8) | 153 (47.5) | 16 (10.5) | 137 (89.5) | 188 (35.2) | 71 (37.8) | 117 (62.2) | ||
| Neutral | 289 (33.8) | 102 (31.7) | 22 (21.6) | 80 (78.4) | 187 (35.0) | 65 (34.8) | 122 (65.2) | ||
| Unsure | 226 (26.4) | 67 (20.8) | 20 (29.9) | 47 (70.1) | 159 (29.8) | 51 (32.1) | 108 (67.9) | ||
| Missing (n) | 42 | 29 | 0 | 29 | 13 | 0 | 13 | ||
| Norms and normative beliefs and motivations | |||||||||
| Weight perception | 0.95 | 0.96 | |||||||
| About right and too low | 540 (62.3) | 225 (68.6) | 40 (17.8) | 185 (82.2) | 315 (58.4) | 109 (34.6) | 206 (65.4) | ||
| Too high | 327 (37.7) | 103 (31.4) | 18 (17.5) | 85 (82.5) | 224 (41.6) | 78 (34.8) | 146 (65.2) | ||
| Missing (n) | 31 | 23 | 0 | 23 | 8 | 0 | 8 | ||
| Weight satisfaction | 0.15 | 0.06 | |||||||
| Very satisfied | 247 (28.5) | 104 (31.6) | 19 (18.3) | 85 (81.7) | 143 (26.5) | 59 (41.3) | 84 (58.7) | ||
| Somewhat satisfied | 370 (42.6) | 146 (44.4) | 20 (13.7) | 126 (86.3) | 224 (41.6) | 66 (29.5) | 158 (70.5) | ||
| Unsatisfied | 251 (28.9) | 79 (24.0) | 19 (24.1) | 60 (76.0) | 172 (31.9) | 62 (36.1) | 110 (64.0) | ||
| Missing (n) | 30 | 22 | 0 | 22 | 8 | 0 | 8 | ||
Low income is defined as eligible for Medicaid during pregnancy.
The p-value is for the chi-square test of association between the characteristic and consistency of weight gain tracking within income group.
Table entries are frequencies and column percentages.
GWG, gestational weight gain.
IOM, Institute of Medicine; GWG within IOM guidelines is 11.5 to 16 kg for women with normal early pregnancy BMI, 7 to 11.5 kg for women with overweight early pregnancy BMI and 5 to 9 kg for women with an obese class 1 early pregnancy BMI.
As shown in Figure 1, intention to avoid excessive pregnancy weight gain, is the most proximal predictor of weight tracking. Overall, 22.7% of women intended to gain more weight during pregnancy than recommended by the IOM, 66.4% intended to gain within the guidelines, and 10.9% intended to gain less than recommended by the IOM (Table 1). Among low income women who intended to gain within the IOM guidelines, 17.9% were consistent trackers and among not-low income women who intended to gain within the IOM guidelines, 38.3% were consistent trackers. The intended amount of GWG was significantly associated with consistent weight gain tracking in not-low income women (p = 0.03), but not in low income women (p = 0.97).
Among the skills examined in bivariate analyses, frequency of self-weighing was significantly associated with consistent weight tracking among low income women (p = 0.004), but not in not-low income women (p = 0.15). Among not-low income women, usage of mobile and web technology was associated with consistent tracking (p < 0.001). Women who had a cell phone and no internet were more likely to be consistent trackers than women who used other electronic communication technologies (Table 1).
Among environmental factors, receiving advice about GWG from a health care provider was considered as a potential facilitator of weight gain tracking. Among low income women, there was no relationship. In not-low income women, among those who did not get advice, 38.0% were consistent trackers compared to 29.2% among those who did get weight gain advice (p = 0.04), the opposite of what was expected. There was a trend for access to a scale at home to be associated with weight tracking in low income women only (p = 0.11). Accessing the internet frequently at home was strongly and significantly associated with consistent tracking among low income women (p = 0.003), but not in higher income women (p = 0.99) where daily use of the internet at home was much more common (57.3% vs. 42.1%).
Among the psychosocial predictors of intention, knowledge of the appropriate amount of weight gain was positively associated with consistent tracking among not-low income women in bivariate analyses (p = 0.02). In addition, self-efficacy was significantly associated with consistent weight tracking among low income women (p = 0.001). Low income women who were unsure of their ability to control their weight gain during pregnancy were more likely to be consistent weight trackers (29.9%) that those who were neutral or sure (10.5% and 21.6% respectively).
Each of the significant factors from the bivariate analyses was then included in a multivariate model predicting consistent weight gain tracking in each of the two income groups separately. Among low income women, the following factors were significantly associated (p < 0.05) with consistent weight tracking: age 30 years or older, some college education or more, weighing self once or more per week, accessing the internet daily from home, unsure weight gain self-efficacy, and BMI (Table 2). Among not-low income women and in the reduced model, not black race, completing college, receiving no GWG advice from a health care provider, and not owning a smart phone were positively and significantly associated (p < 0.05) with consistent weight gain tracking (Table 3).
Table 2.
Full and reduced regression models of consistent weight gain tracking in low income (Medicaid eligible) women a
| Full model b | Reduced model c | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| RR d | 95% CI | P-value | RR | 95% CI | P-value | |
| Age ≥ 30 y | 1.55 | 0.97, 2.47 | 0.06 | 1.74 | 1.12, 2.72 | 0.01 |
| Not-black race | 1.71 | 0.90, 3.24 | 0.10 | |||
| Not-single marital status | 1.16 | 0.65, 2.08 | 0.62 | |||
| Some college education or more | 1.76 | 0.98, 3.16 | 0.06 | 1.93 | 1.10, 3.38 | 0.02 |
| Weigh self ≥ once per week | 1.67 | 1.03, 2.71 | 0.04 | 1.84 | 1.16, 2.92 | 0.01 |
| Access web every day from home | 1.79 | 1.12, 2.84 | 0.01 | 1.89 | 1.19, 3.00 | 0.007 |
| Unsure self-efficacy for gestational weight gain | 2.25 | 1.42, 3.55 | 0.0005 | 2.23 | 1.43, 3.47 | 0.0004 |
| Body mass index | 0.93 | 0.88, 0.99 | 0.03 | 0.94 | 0.88, 0.99 | 0.03 |
Poisson regression models were used to calculate relative risk (RR), 95% CI, and p-values shown in table.
The full model includes all variables significantly (p < 0.05) associated with consistent tracking in chi-quare analysis.
The reduced model excludes variables from full model that had a p-value ≥ 0.10.
RR, relative risk
Table 3.
Full and reduced regression models of consistent weight gain tracking in not-low income (not-Medicaid elibigle) women a
| Full model b | Reduced model c | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| RR d | 95% CI | P-value | RR | 95% CI | P-value | |
| Age ≥ 25y | 1.19 | 0.79, 2.03 | 0.52 | |||
| Not-black race | 2.02 | 0.92, 4.45 | 0.08 | 2.17 | 1.00, 4.68 | 0.05 |
| Completed college | 1.44 | 1.05, 1.98 | 0.02 | 1.56 | 1.15, 2.11 | 0.004 |
| Not single marital status | 1.68 | 0.48, 5.94 | 0.42 | |||
| Unsatisfied with weight | 1.19 | 0.89, 1.60 | 0.25 | |||
| No weight advice from health care provider | 1.27 | 0.98, 1.64 | 0.07 | 1.31 | 1.02, 1.68 | 0.04 |
| Does not own a smart phone | 1.37 | 1.09, 1.73 | 0.008 | 1.48 | 1.16, 1.82 | 0.001 |
| Intend to gain ≤ IOM recommendation | 1.11 | 0.82, 1.50 | 0.49 | |||
| Use < 2 pregnancy websites or apps | 1.29 | 0.93, 1.80 | 0.13 | |||
| Send less than many text messages sent per day | 1.10 | 0.87, 1.40 | 0.42 | |||
| Body mass index | 0.98 | 0.94, 1.02 | 0.29 | 0.99 | 0.96, 1.02 | 0.40 |
Poisson regression models were used to calculate relative risk (RR), 95% CI, and p-values shown in table.
The full model includes all variables significantly (p < 0.05) associated with consistent tracking in chi-quare analysis.
The reduced model excludes variables from full model that had a p-value ≥ 0.10.
RR, relative risk.
Association of weight gain tracking with weight gain outcomes
The second research question of this paper was whether consistent weight tracking was associated with two weight outcomes: total amount of GWG in kg and the proportion of women with excessive GWG as defined by the IOM. In the unadjusted analysis for the sample with complete weight data shown in Figure 2, there was no association between consistency of weight gain tracking and the total amount of weight gained during pregnancy in low income (Medicaid eligible) women (p = 0.21). Among not-low income women, the more consistent the weight tracking, the less women gained and this relationship was significant (p ≤ 0.001). The results for the prevalence of excessive total GWG were similar to those for total GWG in kg (Figure 3). There was no association between the consistency of weight tracking and the prevalence of excessive GWG in low income women (p = 0.47), and there is a highly significant association in not-low income women (p ≤ 0.0001). In this income group, 36.4% of the consistent trackers gained excessively compared to 58.8% of inconsistent trackers (Figure 3).
Figure 2.
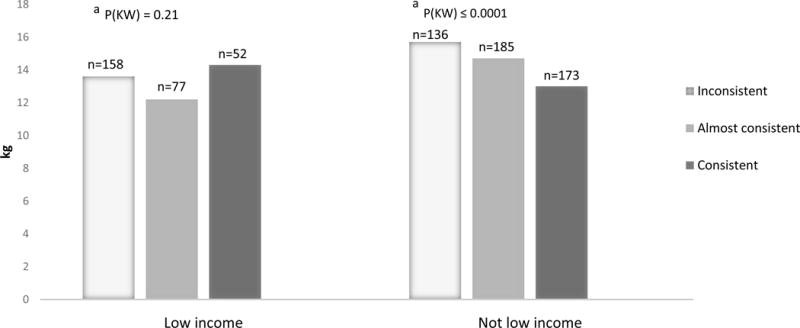
Total gestational weight gain (GWG) in kg by consistency of use of weight gain tracker among low (Medicaid eligible) and not- low income women.
a (KW) is the level of significance for the Kruskal-Wallis chi-square test assessing whether the total amount of gestational weight gain varies by consistency of use of the weight gain tracker.
Figure 3.
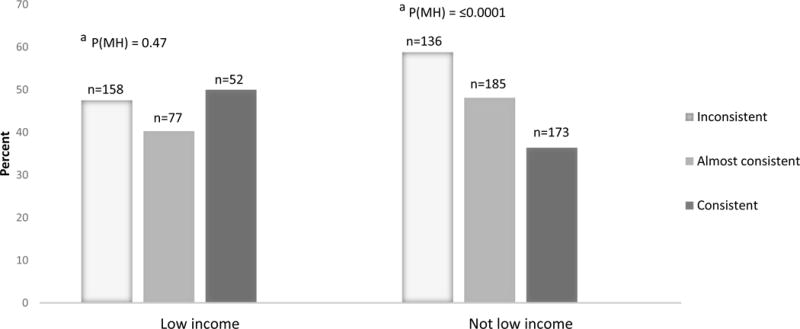
Percent with excessive total gestational weight gain (GWG) by consistency of use of weight gain tracker among low (Medicaid eligible) and not-low income women.
a P(MH) is the level of significance for the Mantel-Haenszel chi-square test assessing whether the rate of excessive total gestational weigh gain is linearly related to the consistency of use of the tracker
To assess the independent effect of weight gain tracking on weight outcomes in each income group, the GWG outcome models were adjusted for covariates associated with weight tracking. This analysis should inform answering the question: Is weight gain tracking associated with weight outcomes or does the association result from the characteristics of the women who choose to track?
Among low income women, consistent tracking was not significantly related to either total GWG or the proportion of women with excessive GWG (Table 4). In this income group, self-weighing once a week or more was associated with 1.57 kg greater weight gain (95% CI: 0.09 to 3.04; p = 0.04). Among not-low income women, consistent tracking was associated with an average of 2.35 kg less GWG (95% CI: −3.23 to −1.46; p <0.0001) controlling for other variables associated with consistent tracking (Table 5). Similarly, consistent trackers in this income group were at significantly reduced risk of gaining excessively (RR 0.73; 95% CI: 0.59 to 0.89; p = 0.002) (Table 5).
Table 4.
Multivariable regression models of gestational weight gain (GWG) outcomes by consistent tracking and its predictors among low income (Medicaid eligible) women a
| Total GWG in kg b | % with excessive total GWG c | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Estimate (kg) | 95% CI | P-value | RR d | 95% CI | P-value | |
| Consistent weight tracking | 0.59 | −1.23, 2.41 | 0.53 | 1.11 | 0.83, 1.48 | 0.49 |
| Age ≥30 y | −0.92 | −2.66, 0.83 | 0.30 | 0.85 | 0.62, 1.17 | 0.32 |
| Some college education or more | 0.49 | −0.93, 1.90 | 0.50 | 1.00 | 0.77, 1.28 | 0.97 |
| Weigh self ≥ once per week | 1.57 | 0.09, 3.04 | 0.04 | 1.25 | 0.99, 1.59 | 0.06 |
| Access web every day from home | 0.43 | −0.92, 1.77 | 0.53 | 1.08 | 0.86, 1.36 | 0.49 |
| Unsure self-efficacy for gestational weight gain | 0.12 | −1.52, 1.76 | 0.88 | 1.09 | 0.84, 1.41 | 0.50 |
Covariates in the model include body mass index (BMI), race, parity, gestational age at delivery, the number of weeks between the first and last pregnancy weight, and the number of weeks between the last pregnancy weight and delivery.
Least squares multiple regression models used to calculate the estimate, 95% CI and p-values shown in table.
A modified Poisson regression approach was used to calculate relative risk (RR), 95% CI, and p-values shown in table.
RR, relative risk.
Table 5.
Multivariable regression models of gestational weight gain (GWG) outcomes by consistent tracking and its predictors among not-low income (not-Medicaid eligible) women a
| Total GWG in kg b | % with excessive total GWG c | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Estimate (kg) | 95% CI | P-value | RR d | 95% CI | P-value | |
| Consistent weight tracking | −2.35 | −3.23, −1.46 | <0.0001 | 0.73 | 0.59, 0.89 | 0.002 |
| Not black race | 1.45 | −0.12, 3.02 | 0.07 | 1.17 | 0.87, 1.56 | 0.30 |
| Completed college | −0.53 | −1.48, 0.41 | 0.27 | 1.01 | 0.84, 1.22 | 0.92 |
| No weight advice from health care provider | 0.08 | −0.80, 0.96 | 0.86 | 1.02 | 0.85, 1.22 | 0.86 |
| Does not own a smart phone | −0.51 | −1.39, 0.38 | 0.26 | 0.87 | 0.72, 1.06 | 0.16 |
Covariates in the models include body mass index (BMI), age, parity, gestational age at delivery, the number of weeks between the first and last pregnancy weight, and the number of weeks between the last pregnancy weight and delivery.
Least squares multiple regression models used to calculate the estimate, 95% CI and p-values shown in table.
A modified Poisson regression approach was used to calculate relative risk (RR), 95% CI, and p-values shown in table.
RR, relative risk.
Discussion
The results of this study support weight gain tracking as an intervention feature in electronic intervention programs for avoiding excessive weight gain during pregnancy among not-low income (not-Medicaid eligible) women. Among women in this income group, consistent trackers gained 2.35 kg less weight during pregnancy and were at significantly reduced risk of gaining excessively compared to women who were not consistent weight gain trackers, controlling for predictors of tracking behavior.
The prevalence of consistent weight tracking during pregnancy was overall quite low, especially among the low income group where only 16.5% were consistent trackers. Among not-low income women, 34.2% were consistent trackers. While this number is double the proportion of low income women, it is not the majority of women.
Generally speaking, the socio-demographic factors positively associated with consistent tracking were similar among low and not-low income women: older age, white race, and higher education. In the multivariate analysis, early pregnancy BMI was significantly and negatively associated with weight gain tracking in low income women only. The psychosocial and environmental factors from the Integrative Model of Behavior Prediction (19; Figure 1) that were significantly associated with tracking varied by income group. Several important environmental constraints and skills were significantly associated with weight tracking among low income women, but not among not-low income women. This finding is consistent with the idea of a “digital divide” meaning that low income women have less access to the devices and technology for e-health interventions. The digital divide also includes an individual’s usual style of learning and the availability of supports that facilitate benefiting from access to the electronic communications technology.
For the design of future intervention trials, it is important to better understand how to encourage more women to track their weights electronically during pregnancy. The results support taking a different approach for women in each income group. Among low income women, increased access to and familiarity with using the e-health technologies and greater availability and use of the tools for weight monitoring (scales) need to be addressed. Among not-low income women, the intervention should focus on addressing the psycho-social factors that contribute directly to forming an intention to gain appropriately. Interestingly, among higher income women, those who did not recall getting advice from a health care provider were more likely to consistently track. This raises the question of how to involve health care providers in an online self-care weight gain prevention intervention such as the one described here. In this income group, women who did not own a smartphone were more likely to consistently track weight gain. We hypothesize that these women may have had less access to and possibly less interest in other pregnancy websites and apps and thus used the study website more frequently. The two ownership groups may have differed in characteristics not controlled in the analysis.
This study has several limitations. It is a secondary, post hoc analysis of data from a relevant subgroup of intervention arm participants in a randomized trial. The cross sectional analysis examines associations between weight tracking and weight outcomes and it is not possible to make a causal inference based on the study design. A second limitation is the small proportion of women who consistently tracked GWG. A strength is that this study includes a large and diverse sample from an effectiveness trial. This increases the applicability of the results to real-world e- and m-health applications.
Conclusion
Consistent weight tracking was associated with significantly less weight gain during pregnancy and a significantly reduced risk of gaining excessively in not-low income women. This relationship was independent of other variables that were associated with consistent tracking. Weight tracking by pregnant women themselves appears to be an effective component of interventions to reduce excessive GWG among not-low income women.
What is already known about this subject?
Frequent self-weighing is positively associated with weight outcomes in non-pregnant individuals.
In pregnant women, frequent self-weighing and weight gain tracking are not consistently associated with better weight outcomes in the 3 studies that have addressed the issue.
E-health interventions with electronic weight gain monitoring currently show better adherence to weight monitoring, but not better weight outcomes.
What does this study add?
The prevalence of consistent weight gain tracking during pregnancy is 16.5% among low income and 34.2% of not-low income women in a socioeconomically and racially/ethnically diverse trial sample from the US.
More highly educated, older, and white women are more likely to track their gestational weight gain than other women.
Among not-low income women, consistent weight gain tracking is associated with a 25% reduction in the risk of excessive gestational weight gain independent of sociodemographic, psychosocial, and environmental factors associated with tracking.
Acknowledgments
FUNDING: National Heart, Lung and Blood Institute and the Eunice Kennedy Shriver National Institute of Child Health and Human Development, Grant No. HL096760
Footnotes
CLINICAL TRIAL REGISTRATION: NCT01331564, www.clinicaltrials.gov
DISCLOSURE: None of the authors have any conflicts of interest to disclosure.
AUTHOR CONTRIBUTIONS: CMO, MSS and MLG designed the study. MSS and MLG conducted the research. MSS analyzed the data. CMO wrote the paper and has primary responsibility for the final content. All authors reviewed and edited the manuscript and approved the final version.
References
- 1.Grivell RM, O’Brien CM, Dodd JM. Managing obesity in pregnancy: A change in focus from harm minimization to prevention. Seminars in Reproductive Medicine. 2016;34(2):e-38–48. doi: 10.1055/s-0036-1583532. [DOI] [PubMed] [Google Scholar]
- 2.IOM (Institute of Medicine), National Research Council (NRC) Weight Gain During Pregnancy: Reexamining the Guidelines. Washington, D.C.: The National Academies Press; 2009. [PubMed] [Google Scholar]
- 3.Viswanathan M, Siega-Riz AM, Moos M-K, Deierlein A, Mumford A, Knaack J, et al. Outcomes of Maternal Weight Gain. Rockville, MD: Agency for Healthcare Research and Quality; 2008. (Evidence Report/Technology Assessment No 168). [PMC free article] [PubMed] [Google Scholar]
- 4.Muktabhant B, Lawrie T, Lumbiganon P, Laopaiboon M. Diet or exercise, or both, for preventing excessive weight gain in pregnancy. Cochrane Database of Systematic Reviews. 2015:CD007145. doi: 10.1002/14651858.CD007145.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Murray E. Web-based interventions for behavior change and self-management: potential, pitfalls, and progress. Medicine 2.0. 2012;1:e3. doi: 10.2196/med20.1741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Harris J, Felix L, Miners A, Murray E, Michie S, et al. Adaptive e-learning to improve dietary behaviour: a systematic review and cost-effectiveness analysis. Health Technol Assess. 2011;15 (37):1–160. doi: 10.3310/hta15370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arem H, Irwin J. A review of web-based weight loss interventions in adults. Obes Rev. 2011;12(5):e256–42. doi: 10.1111/j.1467-789X.2010.00787.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kodama S, Saito K, Tanaka S, Horikawa C, Fujiwara K, Hirasawa R, et al. Effect of web-based lifestyle modification on weight control: a meta-analysis. Int J Obes. 2012;36:675–685. doi: 10.1038/ijo.2011.121. [DOI] [PubMed] [Google Scholar]
- 9.Soltani H, Arden MA, Duxbury AMS, Fair FJ. An analysis of behaviour change techniques used in a sample of gestational weight management trials. (Ariticle No 1085916).J Preg. 2016 doi: 10.1155/2016/1085916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jensen MD, Ryan DH, Donato KA, Apovian CM, Ard JD, Comuzzie AG, et al. Guidelines (2013) for managing overweight and obesity in adults. Obesity. 2014;22(S2):S1–S410. [Google Scholar]
- 11.Zheng Y, Klem ML, Sereika SM, Danford CA, Eving LJ, Burke LE. Welf-weighing in weight management: a systematic literature review. Obesity. 2015;23(2):256–265. doi: 10.1002/oby.20946. [DOI] [PubMed] [Google Scholar]
- 12.Burke LE, Conroy MB, Sereika SM, Elci OU, Styn MA, Acharya SD, et al. The effect of electronic self-monitoring on weight loss and dietary intake: a randomized behavioral weight loss trial. Obesity. 2011;19(2):338–344. doi: 10.1038/oby.2010.208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Harrison CL, Teede HJ, Lombard CB. How effective is self-weighing in the setting of a lifestyle intervention to reduce gestational weight gain and pospartum weight retention? Aust NZ J Obstet Gynaecol. 2014;54(4):382–5. doi: 10.1111/ajo.12207. [DOI] [PubMed] [Google Scholar]
- 14.Jeffries K, Shub A, Walker SP, Hiscock R, Permezel M. Reducing excessive weight gain in pregnancy: a randomised controlled trial. Med J Aust. 2009;191:429–433. doi: 10.5694/j.1326-5377.2009.tb02877.x. [DOI] [PubMed] [Google Scholar]
- 15.McCarthy EA, Walker SP, Ugoni A, Lappas J, Leong O, Shub A. Self-weighing and simple dietary advice for overweight and obese pregnant women to reduce obstetric coomplications without impact on quality of life: a randomised trial. BJOG. 2016;123:965–973. doi: 10.1111/1471-0528.13919. [DOI] [PubMed] [Google Scholar]
- 16.Graham ML, Strawderman MS, Demment M, Olson CM. Does usage of an ehealth intervention reduce the risk of excessive gestational weight gain? Secondary analysis from a randomized controlled trial. J Med Internet Res. 2017;19(1):e6. doi: 10.2196/jmir.6644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lytle LA, Svetkey LP, Patrick K, Belle SH, Fernandez ID, Jakicic JM, et al. The EARLY trials: a consortium of studies targeting weight control in young adults. Transl Behav Med. 2014;4:304–313. doi: 10.1007/s13142-014-0252-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fernandez I, Groth S, Reschke J, Graham M, Strawderman M, Olson C. Electronically-mediated weight interventions for pregnant and postpartum women. Study design and baseline characteristics. Contemp Clin Trials. 2015;43:63–74. doi: 10.1016/j.cct.2015.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fishbein M, Yzer MC. Using theory to design effective health behavior interventions. Communication Theory. 2003;13:164–183. [Google Scholar]
- 20.Fogg B. Persuasive Technology Using computers to change what we think and do. San Francisco, CA: Morgan Kaufmann; 2002. [Google Scholar]
- 21.Graham M, Uesegi K, Niederdeppe J, Gay G, Olson CM. The theory, development, and implementation of an e-Intervention to prevent excessive gestational weight gain: e-Moms Roc. Telemed J E Health. 2014;20:1–8. doi: 10.1089/tmj.2013.0354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kendall A, Olson CM, Frongillo EA., Jr Evaluation of psychosocial measures for understanding weight-related behaviors in pregnant women. Ann Behav Med. 2001;23(2):50–58. doi: 10.1207/S15324796ABM2301_8. [DOI] [PubMed] [Google Scholar]
- 23.Graham J. Missing data analysis: making it work in the real world. Ann Rev Psychol. 2009;60:549–576. doi: 10.1146/annurev.psych.58.110405.085530. [DOI] [PubMed] [Google Scholar]
- 24.Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidem. 2004;159:702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]


