Abstract
There is growing literature suggesting a link between Vitamin D deficiency and asthma in children, but systematic reviews are lacking. The aim of this study is to evaluate the prevalence of Vitamin D deficiency in asthmatic children and to assess the correlations of Vitamin D levels with asthma incidence, asthma control, and lung functions. PubMed, EMBASE, and Cochrane Library were searched for observational studies on asthma and Vitamin D. Two authors independently extracted data. Meta-analysis was performed using the Review Manager Software. A total of 23 (11 case–control, 5 cohort, and 7 cross-sectional) studies enrolling 13,160 participants were included in the review. Overall, Vitamin D deficiency and insufficiency were prevalent in 28.5% and 26.7% children with asthma, respectively. The mean 25-hydroxyvitamin D (25(OH)D) levels (10 studies) were significantly lower in asthmatic children as compared to nonasthmatic children with a mean difference of −9.41 (95% confidence interval [CI] −16.57, −2.25). The odds ratio of Vitamin D deficiency (eight case–control studies) was significantly higher among asthmatic children as compared to nonasthmatic children (odds ratio 3.41; 95% CI 2.04, 5.69). Correlations between Vitamin D levels and incidence of asthma, lung functions, and control of asthma had mixed results. To conclude, asthmatic children had lower 25(OH)D levels as compared to nonasthmatic children, but the correlations between 25(OH)D and asthma incidence, asthma control, and lung functions were varied. Well-designed randomized controlled trials are required to determine if children with asthma can benefit from Vitamin D supplementation.
KEY WORDS: Asthma, children, meta-analysis, observational studies, Vitamin D
INTRODUCTION
Bronchial asthma is one of the most common diseases affecting the children worldwide.[1] Several observational studies suggest that serum Vitamin D deficiency is also common in children.[2,3,4] Vitamin D is an immunomodulator[5] and Vitamin D receptors (VDRs) are present in cells of the immune system such as macrophages, dendritic cells, monocytes, and activated T- and B-cells.[6] VDRs regulate the transcription of various genes implicated in inflammation and immunomodulation of respiratory epithelium.[7] Vitamin D suppresses the proinflammatory cytokines interleukin-17 (IL-17) and IL-13 and promotes the anti-inflammatory cytokines such as IL-10. Further, Vitamin D shifts the balance of T lymphocyte response from Th1 phenotype to Th2 phenotype.[8,9] Studies on Vitamin D and asthma in children had mixed results. The low maternal 25-hydroxyvitamin D (25(OH)D) levels[10,11] and low cord blood 25(OH)D levels[12] had been associated with increased risk of early childhood wheezing. However, in another study, higher Vitamin D levels during pregnancy were associated with increased risk of eczema at age of 9 months and asthma at age of 9 years in offspring.[13] Vitamin D deficiency has been associated with increased incidence[14] and severity[15] of childhood asthma. A few observational studies suggested association between low serum Vitamin D levels and poor asthma control and reduced lung function in children.[15,16,17] Whereas some other studies had adverse effects of Vitamin D in asthma.[13,18] In a study, Vitamin D supplementation during 1st year of life was associated with higher prevalence of allergic rhinitis, atopy, and asthma at age of 31 years of life.[18] The question of whether or not Vitamin D deficiency is a risk factor for pediatric asthma needs to be clarified. We conducted a systematic review and meta-analysis to evaluate the prevalence of Vitamin D deficiency in asthmatic children and to determine the correlation between Vitamin D levels and asthma incidence, asthma control, and lung functions in children.
MATERIALS AND METHODS
We searched the literature from PubMed, EMBASE, and Cochrane Library. The PubMed database was searched using MeSh terms for asthma and Vitamin D without any filters. The EMBASE database was searched with keywords “‘vitamin d’/exp and ‘asthma’/exp” without any filter. The Cochrane Library was searched with keywords “asthma” and “vitamin d” in title and abstract without any other filter. The last search for PubMed, EMBASE, and Cochrane was repeated on July 27, 2015. Reference list of eligible studies was hand searched for additional studies.
Inclusion criteria
Type of studies: Observational studies - cross-sectional studies, case–control studies, and cohort studies; population - children up to 18 years of age; content of study - related to asthma and Vitamin D.
Exclusion criteria
Randomized controlled trials (RCTs) assessing effect of Vitamin D supplementation on asthma as this was not the objective of the review
Studies comparing maternal serum level of Vitamin D with incidence of asthma in children.
The outcome measures of review were (1) mean Vitamin D levels among asthmatic and nonasthmatic children; (2) prevalence of Vitamin D deficiency and insufficiency among asthmatic and nonasthmatic children; and (3) relation between Vitamin D levels and incidence, lung functions, and control of asthma in children. Serum 25(OH)D levels of <20 ng/ml, between 20 and 30 ng/ml, and levels of 30–40 ng/ml are defined as Vitamin D deficient, Vitamin D insufficient, and Vitamin D sufficient levels in the review based on previously published studies, respectively.[19,20,21,22] Prevalence of Vitamin D deficiency and insufficiency was assessed using these definitions. Definition of incidence, lung functions, and asthma control were used as described by included studies.
Two authors independently assessed the title and abstract of electronic search results for potential eligible studies. The full texts of potential eligible studies were obtained and studies were selected for inclusion in the review as per inclusion criteria above. Two authors independently retrieved data in a predefined data collection proforma.
Quality assessment methods
The Newcastle–Ottawa Scale[23] (NOS) was used for assessing quality of nonrandomized studies (cohort and case–control studies).
Statistical methods
We analyzed dichotomous outcomes by calculating odds ratio (OR). Continuous outcome data were analyzed as mean differences (MDs). We presented overall results with 95% confidence intervals (CIs). Meta-analysis was performed using Cochrane RevMan 5.1. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2011.[24] Meta-analysis was only performed on studies of similar design and outcome measures and that comparison of different study types and outcomes are simply presented in the text.
The review was performed as per preferred reporting items for systematic reviews and meta-analyses statement for reporting systematic reviews and meta-analyses wherever applicable.
RESULTS
Study selection
The flow diagram for study selection is shown in Figure 1. The electronic database search revealed a total of 1822 records. Sixty potential eligible studies were identified after screening for titles and abstracts of all records. Full texts of 60 potential eligible studies were assessed for final inclusion in the review. One additional study was identified by reviewing references of included studies. Thirty-eight studies were excluded as per the reasons given in Figure 1 and remaining 23 studies were included in the review.
Figure 1.
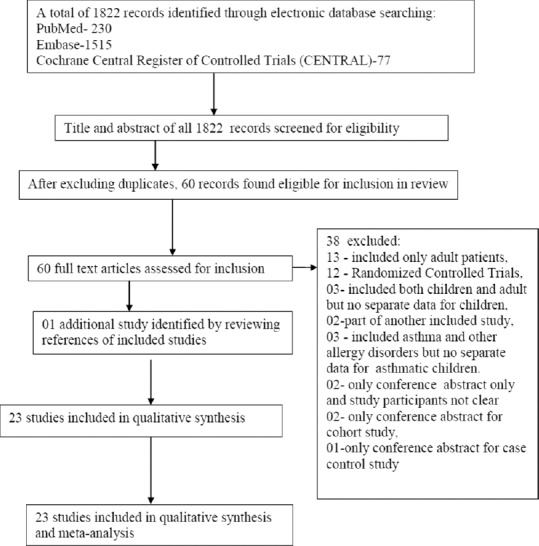
Study selection flow diagram
Included studies
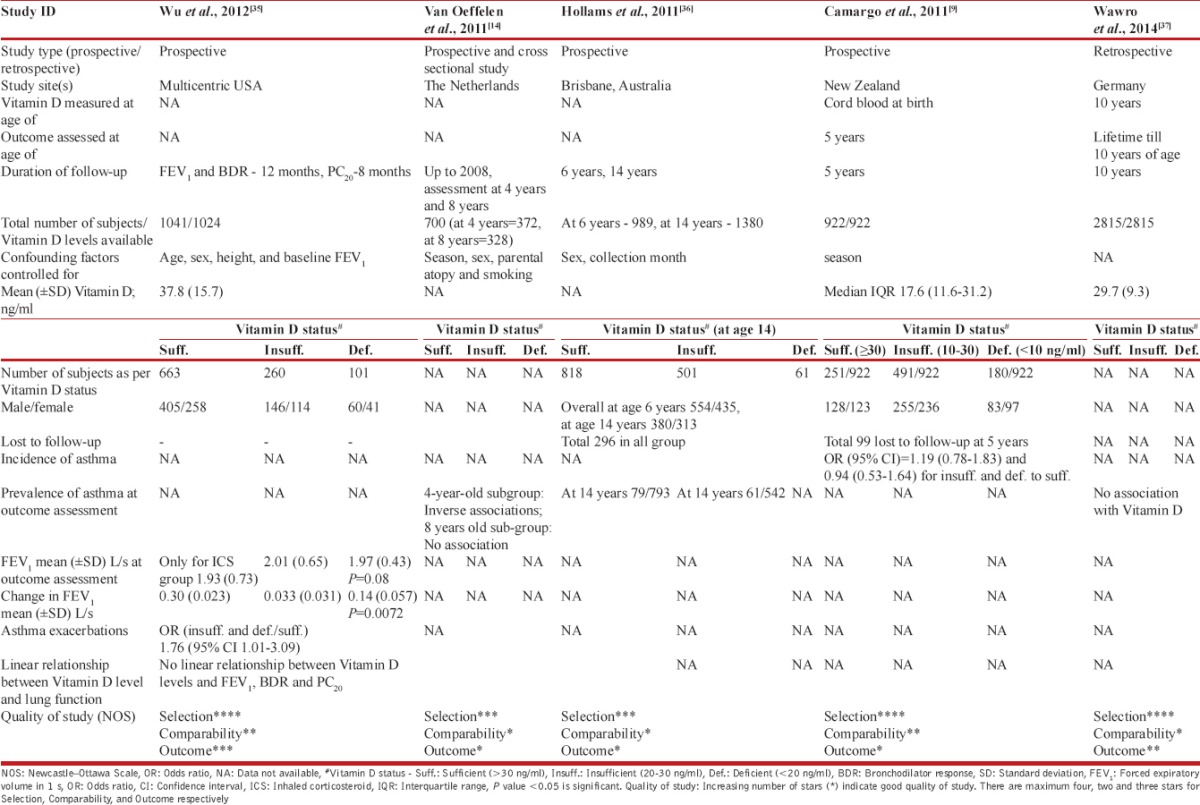
The data extractions from 23 included studies are shown in Tables 1–3. There were 11 case–control studies[16,25,26,27,28,29,30,31,32,33,34] [Table 1], 5 cohort studies[9,14,35,36,37] [Table 2], and 7 cross-sectional studies[1,5,38,39,40,41,42,43] [Table 3]. A total of 13,160 subjects were enrolled in included studies: Case–control studies, 2979; cohort studies, 7830; and cross-sectional studies, 2351. Included studies were both from developed and developing countries: USA (n = 4), Italy (n = 2), Turkey (n = 2), one each from UK, Qatar, China, Tunisia, Iran, USA, Costa Rica, Egypt, The Netherlands, Australia, New Zealand, Canada, Germany, and Thailand. Origin of country was not known for a few studies where only conference abstracts were available.
Table 1.
Case–control studies for asthma and Vitamin D in children
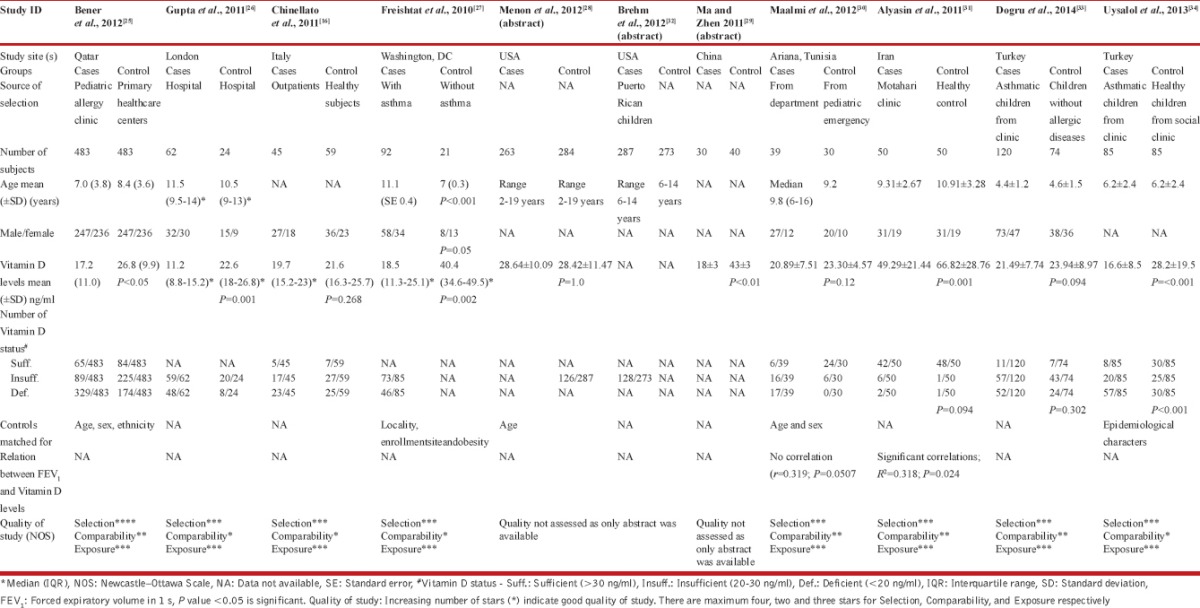
Table 3.
Cross-sectional studies for asthma and Vitamin D in children
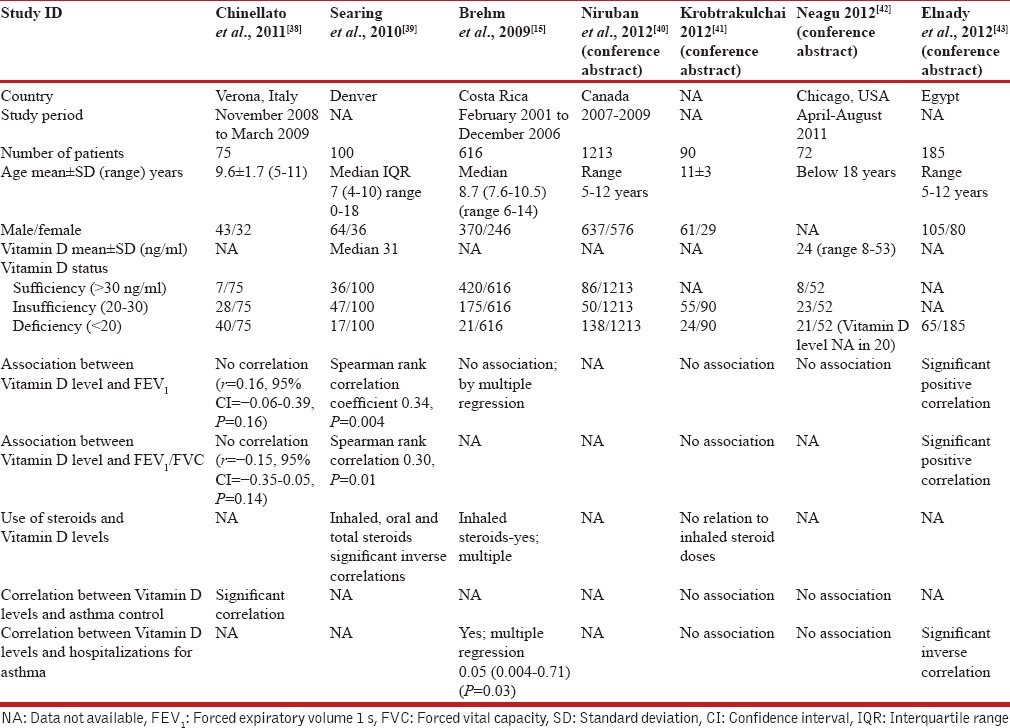
Table 2.
Cohort studies for asthma and Vitamin D in children
Quality of studies
Assessment of quality of case–control and cohort studies using NOS is shown in last row of Tables 1 and 2, respectively. A majority of studies were of moderate to high quality.
Outcomes
Meta-analysis of included studies was performed using Review Manager and results are shown in Table 4 and Figures 2–4. There was significant heterogeneity among studies; therefore, random effect model was used for meta-analysis.
Table 4.
Meta-analysis of Vitamin D levels in asthmatic and nonasthmatic children
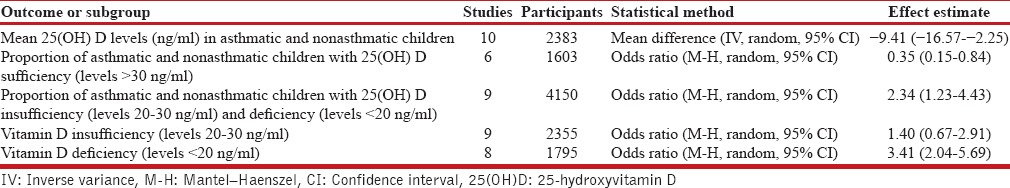
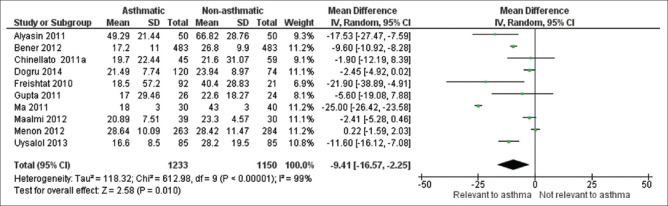
Figure 2.
Forest plot of comparison of mean 25-hydroxyvitamin D levels in asthmatic and nonasthmatic children
Figure 4.
Forest plot of proportion of asthmatic and nonasthmatic children with Vitamin D sufficiency
Mean Vitamin D levels among asthmatic and nonasthmatic children
Mean 25(OH)D levels were available from 10 case–control studies enrolling 2383 participants. Five studies[25,27,29,31,34] had significantly lower mean 25(OH)D levels in asthmatic children as compared to nonasthmatic children [Figure 2]. In other five studies,[19,26,28,30,33] mean 25(OH)D levels were not different between the groups. After pooling data from the 10 studies, the mean 25(OH)D levels were significantly lower in asthmatic children as compared to nonasthmatic children with MD of −9.41 (95% CI −16.57, −2.25) [Table 4 and Figure 2].
Prevalence of Vitamin D deficiency and insufficiency among asthmatic and nonasthmatic children
Vitamin D status was extracted from cohort and case–control studies. Prevalence of Vitamin D deficiency and insufficiency varied markedly between different studies ranging from 3.4% to 77.4% and 4.1% to 85.8%, respectively [Tables 1 and 3]. Overall, on an average, 28.5% and 26.7% children were Vitamin D deficient and insufficient, respectively.
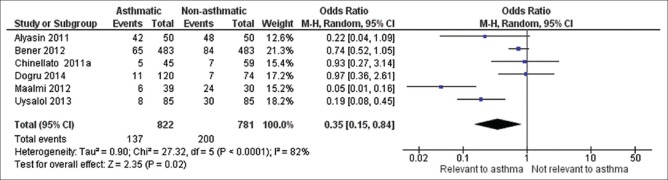
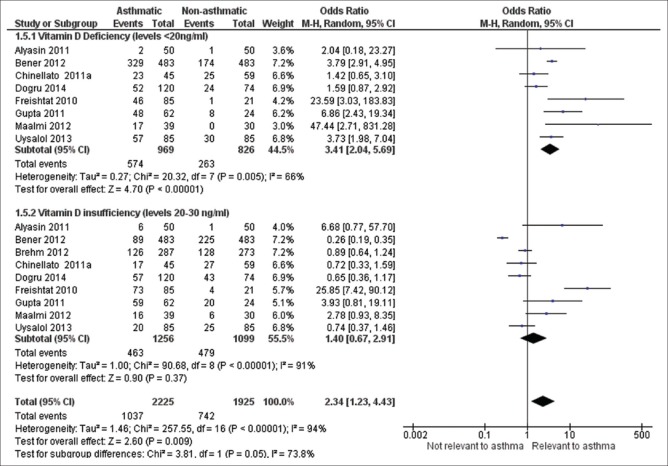
Data regarding proportion of children having Vitamin D deficiency among asthmatic versus nonasthmatic children were available from eight case–control studies enrolling 1795 patients. After pooling data, OR of asthmatic children being Vitamin D deficient (levels <20 ng/ml) was 3.41 (95% CI 2.04, 5.69) [Table 4 and Figure 3]. OR of asthmatic children having Vitamin D levels below 30 ng/ml (after combining subjects with both insufficiency and deficiency) was 2.34 (95% CI 1.23, 4.43) [Table 4 and Figure 3].
Figure 3.
Forest plot of proportion of asthmatic and nonasthmatic children with Vitamin D deficiency and insufficiency
Children without asthma had Vitamin D levels more sufficient as compared to asthmatic children [Figure 4].
Relation between Vitamin D levels and incidence of asthma
Four cohort studies reported relation of Vitamin D levels with incidence and prevalence. van Oeffelen et al.[14] assessed relation between serum micronutrient concentrations including Vitamin D and prevalence of asthma in children and found that there was inverse associations between serum Vitamin D concentrations and asthma and severe asthma at age of 4 years with OR of 0.49, 95% CI: 0.25–0.95, although there was no association between serum Vitamin D concentrations and severe asthma at 8 years of age in the same study.[14] Camargo et al.[9] assessed association between cord blood Vitamin D levels and respiratory outcome at 5 years of age and found that there was increased incidence of cumulative wheezing (OR [95% CI] = 1.63 [1.17, 2.26] and 2.15 [1.39, 3.33]) for insufficiency and deficiency, respectively, as compared to sufficiency at 5 years of age but there was no association between cord blood Vitamin D levels and incidence of asthma at 5 years of age with OR of 1.19 (95% CI 0.78, 1.83) and 0.94 (95% CI 0.53, 1.64) for insufficiency and deficiency as compared to sufficiency, respectively.[9] In a West Australian pregnancy cohort study by Hollams et al.,[36] asthma at age of 14 years was not related to Vitamin D levels with OR of 0.39 [95% CI 0.09, 1.62; P = 0.1930].
Relation between Vitamin D levels and lung functions
Five studies[26,16,31,39,43] reported significant association between Vitamin D levels and lung functions in asthmatic children including forced expiratory volume in 1 s (FEV1),[16,26,31,39,43] FEV1/forced vital capacity (FVC),[31,39,43] bronchodilator response,[26] and exercise-induced bronchoconstriction[16] in asthmatic children. On the other side, there was no correlation between Vitamin D levels and FEV1 and FEV1/FVC in asthmatic children in the study by Brehm et al.,[15] Maalmi et al.,[30] Wu et al.,[35] Chinellato et al.,[38] Krobtrakulchai,[41] and Neagu.[42]
Relation between Vitamin D levels and control of asthma in children
A few studies reported correlation of Vitamin D levels with asthma control. A positive relationship was found between 25(OH)D level and childhood asthma control in the study by Gupta et al.[26] (r = 0.6, P = 0.001), Chinellato et al.,[38] and Uysalol et al.[34] No association between Vitamin D levels and asthma control was reported in study by Menon et al.,[28] Krobtrakulchai,[41] and Neagu.[42] Daily doses of inhaled steroids were inversely related to serum Vitamin D levels in the study by Brehm et al.,[15] Gupta et al.,[26] and Searing et al.,[39] but there was no association between Vitamin D levels and inhaled steroid doses in the study by Krobtrakulchai[41] Brehm et al.,[32] Gupta et al.,[26] and Wu et al.[35] Uysalol et al.[34] reported association between increased acute asthma exacerbations and lower serum 25(OH)D levels, but again no association between Vitamin D levels and asthma exacerbation in the study by Krobtrakulchai[41] and Neagu.[42] No associations were reported between Vitamin D level and eosinophil counts, duration of disease, and the number of hospitalization or unscheduled visits in a year (P > 0.05) by Alyasin et al.[31] Four studies[25,26,29,43] evaluated association between Vitamin D levels and total IgE in asthmatic children and found inverse correlation.
DISCUSSION
This systematic review of 23 observational studies found that mean Vitamin D levels were significantly lower in asthmatic children compared to nonasthmatic children, but correlation between Vitamin D levels with incidence/prevalence of asthma, lung functions, and control of asthma was not uniform among the studies. Wide range of Vitamin D deficiency may be explained by variation in nutritional status, difference in sun exposure, fortification of food items, use of supplements, geographical location of country, and many other factors in different countries. Vitamin D deficiency and asthma may be linked by reverse causation because Vitamin D is synthesized by sun exposure and it is likely that asthmatic children may spend less time outdoor due to sickness by asthma. Brehm et al.[32] evaluated correlation between Vitamin D levels and asthma exacerbations in children after adjusting for time spent outdoors and racial ancestry and found that there was still a strong association between Vitamin D deficiency and asthma exacerbations after adjusting these factors. Therefore, this reverse causation seems to be less plausible. A recent review of observational studies by Cassim et al.[44] included both children and adult patients and identified 23 studies (12 cohort, 9 cross-sectional, and 2 case–control studies) and reported that higher Vitamin D levels were associated with decreased risk of acute exacerbations of asthma. Similar to our review, they also reported mixed results for association of Vitamin D levels with prevalence, incidence, and severity of asthma.[44] This review also included studies where Vitamin D levels were measured during pregnancy.[44] We excluded such studies, therefore number of cohort studies were less in our review. Yadav and Mittal[45] conducted a randomized controlled trial of oral Vitamin D3 (cholecalciferol) supplementation of 60,000 IU per month for 6 months in children and reported better peak expiratory flow rate improvement, better asthma control, and reduced need of emergency visit and oral steroids use in Vitamin D group compared to placebo group. However, the Vitamin D levels were not measured in the study.[45] In another pediatric RCT, 500 units of Vitamin D supplementation daily for 6 months showed decreased asthma exacerbation in Vitamin D group though Vitamin D levels did not change before and after supplementation and lung function improved significantly in both arms.[46] The Vitamin D assessment (VIDA) trial randomized 408 adults with poorly controlled asthma to supplement with high-dose Vitamin D or placebo.[47] Vitamin D supplementation did not alter the rate of first treatment failure during 28 weeks. In a subgroup analysis, subjects with a rise in Vitamin D levels >30 ng/ml had decreased rate of treatment failure and acute asthma exacerbations compared to placebo.[47] These trials suggest that Vitamin D supplementation will not be of help in all asthmatic children but in certain group of children.
Strength of the review includes broad search strategy, rigorous data extraction, and analysis. There are some limitations of review. First, we could not find full text of seven included studies (three case–control and four cross-sectional studies). Second, there was significant heterogeneity among included studies. Vitamin D levels were measured by different methods in different studies, e.g., radioimmunoassay method in Brehm et al.,[15] Chinellato et al.,[16] Bener et al.,[25] Maalmi et al.,[30] Alyasin et al.,[31] and Wu et al.;[35] enzyme-linked immunosorbent assay in van Oeffelen et al.,[14] Freishtat et al.,[27] and Hollams et al.;[36] high-performance liquid chromatography system–tandem mass spectrometry in Gupta et al. 2011;[26] and chemiluminescence immunoassay by Camargo et al.,[9] Chinellato et al.,[38] and Searing et al.[39] Finally, VIDA levels at different ages, diagnosis of asthma at variable ages, and partial control for confounders in some studies make results of the review difficult to rely upon. Large randomized clinical trials of Vitamin D supplementation with emphasis on timing and dosage are needed before recommending Vitamin D to children with asthma. It may be possible that Vitamin D supplementation may be beneficial in selected children who are Vitamin D deficient and dosages are sufficient enough to raise Vitamin D levels to normal range. It would be helpful if could identify asthmatic children who will benefit from Vitamin D supplementation in a particular dose for a particular duration.
CONCLUSIONS
Prevalence of Vitamin D deficiency varied from country to country. Asthmatic children had significantly lower Vitamin D levels as compared to nonasthmatic children. Correlation between Vitamin D levels and incidence of asthma, lung functions, and control of asthma had mixed results. There is need of large well-conducted randomized trials of Vitamin D supplementation with different doses and different duration of supplementation to assess the efficacy of Vitamin D on lung function and asthma control in children.
Note
The abstract was presented at the International Congress of Pediatrics 2013 (ICP), the 27th Congress of International Pediatric Association, held at Melbourne, Australia, from 24-29 August 2013.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to acknowledge Dr. S.K. Kabra and Dr. Rakesh Lodha (both from Department of Pediatrics, All India Institute of Medical Sciences, New Delhi, India) for their intellectual input in the final manuscript.
REFERENCES
- 1.Akinbami LJ, Moorman JE, Bailey C, Zahran HS, King M, Johnson CA, et al. Trends in asthma prevalence, health care use, and mortality in the United States, 2001-2010. NCHS Data Brief. 2012;94:1–8. [PubMed] [Google Scholar]
- 2.Holick MF. Vitamin D deficiency in 2010: Health benefits of Vitamin D and sunlight: A D-bate. Nat Rev Endocrinol. 2011;7:73–5. doi: 10.1038/nrendo.2010.234. [DOI] [PubMed] [Google Scholar]
- 3.Gordon CM, Feldman HA, Sinclair L, Williams AL, Kleinman PK, Perez-Rossello J, et al. Prevalence of Vitamin D deficiency among healthy infants and toddlers. Arch Pediatr Adolesc Med. 2008;162:505–12. doi: 10.1001/archpedi.162.6.505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kumar J, Muntner P, Kaskel FJ, Hailpern SM, Melamed ML. Prevalence and associations of 25-hydroxyvitamin D deficiency in US children: NHANES 2001-2004. Pediatrics. 2009;124:e362–70. doi: 10.1542/peds.2009-0051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Damera G, Fogle HW, Lim P, Goncharova EA, Zhao H, Banerjee A, et al. Vitamin D inhibits growth of human airway smooth muscle cells through growth factor-induced phosphorylation of retinoblastoma protein and checkpoint kinase 1. Br J Pharmacol. 2009;158:1429–41. doi: 10.1111/j.1476-5381.2009.00428.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Adams JS, Hewison M. Unexpected actions of Vitamin D: New perspectives on the regulation of innate and adaptive immunity. Nat Clin Pract Endocrinol Metab. 2008;4:80–90. doi: 10.1038/ncpendmet0716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Raby BA, Lazarus R, Silverman EK, Lake S, Lange C, Wjst M, et al. Association of Vitamin D receptor gene polymorphisms with childhood and adult asthma. Am J Respir Crit Care Med. 2004;170:1057–65. doi: 10.1164/rccm.200404-447OC. [DOI] [PubMed] [Google Scholar]
- 8.Litonjua AA, Weiss ST. Is Vitamin D deficiency to blame for the asthma epidemic? J Allergy Clin Immunol. 2007;120:1031–5. doi: 10.1016/j.jaci.2007.08.028. [DOI] [PubMed] [Google Scholar]
- 9.Camargo CA, Jr, Ingham T, Wickens K, Thadhani R, Silvers KM, Epton MJ, et al. Cord-blood 25-hydroxyvitamin D levels and risk of respiratory infection, wheezing, and asthma. Pediatrics. 2011;127:e180–7. doi: 10.1542/peds.2010-0442. [DOI] [PubMed] [Google Scholar]
- 10.Camargo CA, Jr, Rifas-Shiman SL, Litonjua AA, Rich-Edwards JW, Weiss ST, Gold DR, et al. Maternal intake of sitamin D during pregnancy and risk of recurrent wheeze in children at 3 y of age. Am J Clin Nutr. 2007;85:788–95. doi: 10.1093/ajcn/85.3.788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Devereux G, Litonjua AA, Turner SW, Craig LC, McNeill G, Martindale S, et al. Maternal Vitamin D intake during pregnancy and early childhood wheezing. Am J Clin Nutr. 2007;85:853–9. doi: 10.1093/ajcn/85.3.853. [DOI] [PubMed] [Google Scholar]
- 12.Camargo CA, Jr, Ingham T, Wickens K, Thadhani R, Silvers KM, Epton MJ, et al. Cord-blood 25-hydroxyvitamin D levels and risk of respiratory infection, wheezing, and asthma. Pediatrics. 2011;127:e180–7. doi: 10.1542/peds.2010-0442. [DOI] [PubMed] [Google Scholar]
- 13.Gale CR, Robinson SM, Harvey NC, Javaid MK, Jiang B, Martyn CN, et al. Maternal Vitamin D status during pregnancy and child outcomes. Eur J Clin Nutr. 2008;62:68–77. doi: 10.1038/sj.ejcn.1602680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.van Oeffelen AA, Bekkers MB, Smit HA, Kerkhof M, Koppelman GH, Haveman-Nies A, et al. Serum micronutrient concentrations and childhood asthma: The PIAMA birth cohort study. Pediatr Allergy Immunol. 2011;22:784–93. doi: 10.1111/j.1399-3038.2011.01190.x. [DOI] [PubMed] [Google Scholar]
- 15.Brehm JM, Celedón JC, Soto-Quiros ME, Avila L, Hunninghake GM, Forno E, et al. Serum Vitamin D levels and markers of severity of childhood asthma in Costa Rica. Am J Respir Crit Care Med. 2009;179:765–71. doi: 10.1164/rccm.200808-1361OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chinellato I, Piazza M, Sandri M, Peroni DG, Cardinale F, Piacentini GL, et al. Serum Vitamin D levels and exercise-induced bronchoconstriction in children with asthma. Eur Respir J. 2011;37:1366–70. doi: 10.1183/09031936.00044710. [DOI] [PubMed] [Google Scholar]
- 17.Brehm JM, Schuemann B, Fuhlbrigge AL, Hollis BW, Strunk RC, Zeiger RS, et al. Serum Vitamin D levels and severe asthma exacerbations in the childhood asthma management program study. J Allergy Clin Immunol. 2010;126:52–8. doi: 10.1016/j.jaci.2010.03.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hyppönen E, Sovio U, Wjst M, Patel S, Pekkanen J, Hartikainen AL, et al. Infant Vitamin D supplementation and allergic conditions in adulthood: Northern Finland birth cohort 1966. Ann N Y Acad Sci. 2004;1037:84–95. doi: 10.1196/annals.1337.013. [DOI] [PubMed] [Google Scholar]
- 19.Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357:266–81. doi: 10.1056/NEJMra070553. [DOI] [PubMed] [Google Scholar]
- 20.Thomas MK, Lloyd-Jones DM, Thadhani RI, Shaw AC, Deraska DJ, Kitch BT, et al. Hypovitaminosis D in medical inpatients. N Engl J Med. 1998;338:777–83. doi: 10.1056/NEJM199803193381201. [DOI] [PubMed] [Google Scholar]
- 21.Heaney RP, Dowell MS, Hale CA, Bendich A. Calcium absorption varies within the reference range for serum 25-hydroxyvitamin D. J Am Coll Nutr. 2003;22:142–6. doi: 10.1080/07315724.2003.10719287. [DOI] [PubMed] [Google Scholar]
- 22.Vieth R, Bischoff-Ferrari H, Boucher BJ, Dawson-Hughes B, Garland CF, Heaney RP, et al. The urgent need to recommend an intake of Vitamin D that is effective. Am J Clin Nutr. 2007;85:649–50. doi: 10.1093/ajcn/85.3.649. [DOI] [PubMed] [Google Scholar]
- 23.Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality if nonrandomized studies in meta-analyses. [Last accessed on 2015 Sep 17]. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm .
- 24.The Nordic Cochrane Centre. The Cochrane Collaboration. Review Manager (RevMan). 5.1. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration; 2011. [Google Scholar]
- 25.Bener A, Ehlayel MS, Tulic MK, Hamid Q. Vitamin D deficiency as a strong predictor of asthma in children. Int Arch Allergy Immunol. 2012;157:168–75. doi: 10.1159/000323941. [DOI] [PubMed] [Google Scholar]
- 26.Gupta A, Sjoukes A, Richards D, Banya W, Hawrylowicz C, Bush A, et al. Relationship between serum Vitamin D, disease severity, and airway remodeling in children with asthma. Am J Respir Crit Care Med. 2011;184:1342–9. doi: 10.1164/rccm.201107-1239OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Freishtat RJ, Iqbal SF, Pillai DK, Klein CJ, Ryan LM, Benton AS, et al. High prevalence of Vitamin D deficiency among inner-city African American youth with asthma in Washington, DC. J Pediatr. 2010;156:948–52. doi: 10.1016/j.jpeds.2009.12.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Menon J, Maranda L, Nwosu BU. Serum 25-hydroxyvitamin D levels do not correlate with asthma severity in a case-controlled study of children and adolescents. J Pediatr Endocrinol Metab. 2012;25:673–9. doi: 10.1515/jpem-2012-0143. [DOI] [PubMed] [Google Scholar]
- 29.Ma XL, Zhen YF. Serum levels of 25-(OH)D (3) and total IgE in children with asthma. Zhongguo Dang Dai Er Ke Za Zhi. 2011;13:551–3. [PubMed] [Google Scholar]
- 30.Maalmi H, Sassi FH, Berraies A, Ammar J, Hamzaoui K, Hamzaoui A. Association of Vitamin D receptor gene polymorphisms with susceptibility to asthma in Tunisian hildren: A case control study. J Asthma Allergy. 2012;5:11–9. doi: 10.1016/j.humimm.2012.11.005. [DOI] [PubMed] [Google Scholar]
- 31.Alyasin S, Momen T, Kashef S, Alipour A, Amin R. The relationship between serum 25 hydroxyvitamin D levels and asthma in children. Allergy Asthma Immunol Res. 2011;3:251–5. doi: 10.4168/aair.2011.3.4.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Brehm JM, Acosta-Pérez E, Klei L, Roeder K, Barmada M, Boutaoui N, et al. Vitamin D insufficiency and severe asthma exacerbations in Puerto Rican children. Am J Respir Crit Care Med. 2012;186:140–6. doi: 10.1164/rccm.201203-0431OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dogru M, Kirmizibekmez H, Yesiltepe Mutlu RG, Aktas A, Ozturkmen S. Clinical effects of Vitamin D in children with asthma. Int Arch Allergy Immunol. 2014;164:319–25. doi: 10.1159/000366279. [DOI] [PubMed] [Google Scholar]
- 34.Uysalol M, Mutlu LC, Saracoglu GV, Karasu E, Guzel S, Kayaoglu S, et al. Childhood asthma and Vitamin D deficiency in Turkey: Is there cause and effect relationship between them? Ital J Pediatr. 2013;39:78. doi: 10.1186/1824-7288-39-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wu AC, Tantisira K, Li L, Fuhlbrigge AL, Weiss ST, Litonjua A, Childhood Asthma Management Program Research Group Effect of Vitamin D and inhaled corticosteroid treatment on lung function in children. Am J Respir Crit Care Med. 2012;186:508–13. doi: 10.1164/rccm.201202-0351OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hollams EM, Hart PH, Holt BJ, Serralha M, Parsons F, de Klerk NH, et al. Vitamin D and atopy and asthma phenotypes in children: A longitudinal cohort study. Eur Respir J. 2011;38:1320–7. doi: 10.1183/09031936.00029011. [DOI] [PubMed] [Google Scholar]
- 37.Wawro N, Heinrich J, Thiering E, Kratzsch J, Schaaf B, Hoffmann B, et al. Serum 25(OH) D concentrations and atopic diseases at age 10: Results from the GINIplus and LISAplus birth cohort studies. BMC Pediatr. 2014;14:286. doi: 10.1186/s12887-014-0286-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chinellato I, Piazza M, Sandri M, Peroni D, Piacentini G, Boner AL. Vitamin D serum levels and markers of asthma control in Italian children. J Pediatr. 2011;158:437–41. doi: 10.1016/j.jpeds.2010.08.043. [DOI] [PubMed] [Google Scholar]
- 39.Searing DA, Zhang Y, Murphy JR, Hauk PJ, Goleva E, Leung DY. Decreased serum Vitamin D levels in children with asthma are associated with increased corticosteroid use. J Allergy Clin Immunol. 2010;125:995–1000. doi: 10.1016/j.jaci.2010.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Niruban SJ, Alagiakrishnan K, Beach J, Senthilselvan A. Association of Vitamin D with current asthma and lung function in children: Results from the Canadian health measures survey. Am J Epidemiol. 2012;176:1. [Google Scholar]
- 41.Krobtrakulchai W. The effect of Vitamin D status on pediatric asthma in a university hospital, Thailand. J Allergy Clin Immunol. 2012;129(2 Suppl):1. doi: 10.4168/aair.2013.5.5.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Neagu F. Hypovitaminosis D is very frequent but not associated with asthmacontrol in a low-income pediatric population seen in an allergy and immunology clinic. J Allergy Clin Immunol. 2012;129(2 Suppl):1. [Google Scholar]
- 43.Elnady HG, Abdel Hameed E, Fouda E, Abdel Shaheed A, Refaat E, Badawy E. Serum Vitamin D levels and markers of childhood asthma severity in Greater Cairo. Intensive Care Med. 2011;37(Suppl 2):S355–6. [Google Scholar]
- 44.Cassim R, Russell MA, Lodge CJ, Lowe AJ, Koplin JJ, Dharmage SC. The role of circulating 25 hydroxyvitamin D in asthma: A systematic review. Allergy. 2015;70:339–54. doi: 10.1111/all.12583. [DOI] [PubMed] [Google Scholar]
- 45.Yadav M, Mittal K. Effect of Vitamin D supplementation on moderate to severe bronchial asthma. Indian J Pediatr. 2014;81:650–4. doi: 10.1007/s12098-013-1268-4. [DOI] [PubMed] [Google Scholar]
- 46.Majak P, Olszowiec-Chlebna M, Smejda K, Stelmach I. Vitamin D supplementation in children may prevent asthma exacerbation triggered by acute respiratory infection. J Allergy Clin Immunol. 2011;127:1294–6. doi: 10.1016/j.jaci.2010.12.016. [DOI] [PubMed] [Google Scholar]
- 47.Castro M, King TS, Kunselman SJ, Cabana MD, Denlinger L, Holguin F, et al. Effect of Vitamin D3 on asthma treatment failures in adults with symptomatic asthma and lower Vitamin D levels: The VIDA randomized clinical trial. JAMA. 2014;311:2083–91. doi: 10.1001/jama.2014.5052. [DOI] [PMC free article] [PubMed] [Google Scholar]