Abstract
Our surroundings affect our mood, our recovery from stress, our behavior, and, ultimately, our mental health. Understanding how our surroundings influence mental health is central to creating healthy cities. However, the traditional observational analyses now dominant in the psychiatric epidemiology literature are not sufficient to garner such an understanding. Alternative strategies, such as randomizing people to place, randomizing places to change, or harnessing natural experiments that mimic randomized experiments each have their strengths and weaknesses. We discuss these strengths and weaknesses with respect to (1) defining the most relevant scale and characteristics of context, (2) disentangling the effects of context from the effects of individuals’ preferences and prior health, and (3) generalizing causal effects beyond the study setting. Promising alternative strategies include creating many small-scale randomized place-based trials, using the deployment of place-based changes over time as natural experiments, and using fluctuations in the changes in our surroundings in combination with emerging data collection technologies to better understand how surroundings influence mood, behavior, and mental health. Improving existing research strategies will require interdisciplinary partnerships between those specialized in mental health, those advancing new methods for place effects on health, and those who seek to optimize the design of local environments.
Keywords: Place, spatiotemporal, causal models, change-point, case study
Introduction: Context as a determinant of mental health
Interdisciplinary partnerships between urban studies and public health have revolutionized our understanding of the psychosocial and contextual determinants of physical health [1,2]. Perhaps ironically, relatively less attention has been given to the relationship between these psychosocial influences and mental health [3–5]. Particularly lacking in the existing literature on the influence of one’s surroundings on mental health are studies that employ causal methods [6,7]. This is especially problematic because studies of context are easily confounded -- those with poor mental health tend to have lower incomes and so have less ability to choose what many might consider to be healthy surroundings [8]. Likewise, communities with a high prevalence of mental illness may be less likely to have the characteristics that facilitate recovery from mental illness, such as social capital or access to green space [9,10]. Therefore, it is particularly difficult to disentangle cause from effect and nearly impossible to remove confounders from observational analyses through adjustment alone. However, moving away from inexpensive, easily replicable observational studies produces new challenges.
In this paper, an interdisciplinary group of authors first discuss key threats relevant to both conventional observational analyses and randomized controlled trials (RCTs) when investigating how contexts influence mental health. We point to challenges that vary by national setting, particularly contrasting the US and China. However, we also find great opportunities across national and local contexts, where policymakers and researchers can collaborate to better understand what works where to improve mental health. We suggest that small-scale alterations can serve as relatively inexpensive and flexible natural experiments that help sort out cause and effect. We turn to the broader built environment literature to show how structural time-series modeling can be applied to social and psychiatric epidemiology.
Challenges encountered when quantifying the effects of context
It can be difficult to estimate the effects of context on mental health due to two key methodological challenges: (1) isolating the effects of place on people’s mental health from the effects of mental health or its correlates on place and (2) deciding how to measure place. Randomized trials can partially mitigate these concerns, but trials can also make it difficult to generalize knowledge to new settings.
Distinguishing effects of context on mental health from patterned self-selection into contexts
Operationalizing the effect of context on mental health is challenging. One’s mental health strongly influences his or her ability to afford to live in an environment that is serene, green, clean, crime free, and aligns with his or her preferences [11]. This contributes to higher prevalence of mental illness in some communities [12]. A high prevalence of mental illness in a community, in turn, influences the community’s social capital, human capital, and political capital [13]. And, where a person lives is also “patterned” according to personal or cultural characteristics (e.g. religion) that are in turn associated with mental health [14].
Identifying the scale and characteristics of context most relevant to mental health
It is difficult to define spatial boundaries (e.g., finding a dataset that has high enough resolution to find associations between airplane noise and depression is enough of a challenge that there are only a few such studies) [15]. But, geographic and spatial modeling tools can assist us in understanding how sensitive observational findings are to scale of measurement.
Novel additions to observational studies can help solve spatial and contextual problems. Global positioning system (GPS) monitoring has recently been used to identify personalized activity spaces that may better capture the context in which individual study subjects live [16,17]. Such studies also offer insight into how place preferences affect where people spend time [18]. However, a particular complexity in using GPS devices to define neighborhoods is that geographic units will systematically differ in scale based on individual mobility patterns, with smaller areas traversed by those with limited [16] or relatively linear [17] travel. These travel spaces may be influenced by mental illness. Therefore, again, mental illness produces “selection” that is difficult to sort out in observational studies.
Identifying the “active ingredient” responsible for a contextual effect on health is crucial if we are to move forward to policy and design recommendations. For example, mental health service facilities focusing on homeless populations are nearly always located in neighborhoods with less social capital [13]. Without attention in our observational research to disentangling these, we may underestimate the benefits of new facilities.
Research on physical activity has featured prominently in methods and policy guideline development to this point [19,20], with lessons that can likely be transferred to emerging place and mental health research. In particular, prior research suggests a range of potentially appropriate scales of measurement, and can point to salient characteristics of place shaping perceptions and behavior. Participants to be can be tracked via GPS or other forms of real-time spatial data collection, including recording participants’ own preferences [21]. And, they also allow for very clear boundaries to be placed on context. Yet, while measurement options have expanded, several less tractable challenges have persisted.
The potential for randomized controlled trials to resolve these problems
While measurement options have expanded (at least outside of the mental health literature [20,22]), several less tractable challenges have persisted.
Randomized trials circumvent problems with confounding and reverse causation. However, these benefits are matched by even larger problems. Such studies are limited in their flexibility to address multiple inter-related questions, potentially fraught with regards to ethical issues (especially when populations are vulnerable to mental illness), are not as amenable to sensitivity analyses, and are expensive (Table 1).
Table 1.
Summary of the benefits and drawbacks of the three approaches to assessing the effects of context on health outcomes discussed in this paper.
| Relocation RCTs | Small place-based RCTs | Place-based Natural Experiments | |
|---|---|---|---|
| Estimated effect | Effect of moving persons | Effect of changing a place | Effect of changing a place |
| Pros | Analytic rigor | Analytic rigor | Low cost |
| Cons | Very high cost | May require large number of locations for intervention | Implementation aligned with policy goals Potential for bias due to targeted location selection |
| Disruption of existing social networks | Inherent conflict between goal of consistent implementation and community involvement | Potential for bias due to inconsistent implementation | |
| Does not reflect the full range of realistic policy interventions |
Relocation experiments have used randomization to investigate questions such as how vouchers to move out of public housing affect residents’ health (Moving to Opportunity, or MTO), including their mental health [23,10]. Because the act of moving participants from one neighborhood to another is in of itself a stressor and social disruption that can influence outcomes, such an experiment can only answer the very narrow question of what happens when people are given housing vouchers. Since moving induces short-term psychological stress, it may mediate an association with intermediate-term mental health outcomes. If scientists may get different results depending on when mental health measures are collected, it raises serious questions about whether the research should be done at all.
When mental health is a relevant outcome (as it was in MTO) questions of social justice move to the forefront [24,25]. Specifically, there are concerns about community participation in decision making and about participants’ ability to freely provide informed consent for such investigations. The societal circumstances that go along with top-down interventions affecting entire communities raise concerns about both the process of change (which can itself either amplify or undermine behaviorally-mediated health benefits [24]) and generalizability of findings to places with a more participatory change process.
Alternatively, serious ethical concerns also arise when programs are not evidence-based. This results in a “catch 22” situation in which either randomization is used early (thus, some are exposed to benefit or unforeseen harm through randomization in order to inform decisions on whether and how to scale up), or implementation decisions goes forward without such randomization (thus, larger numbers are exposed to, or miss out on, the health effects of an intervention deployed at full scale before convincing evidence is available).
To illustrate, consider the Chinese housing lottery. When $1 trillion dollars of affordable housing units within healthy communities were built for low-income workers [26], only 1 unit of housing was available for every 2 applicants in most localities. Yet if risks or benefits arose from residence in a subsidized low-income housing unit built around greenspace and public transit, an RCT would make it possible to examine such risks and benefits before the program is made universal.
A much larger (and more practical) concern is the expense and logistics of conducting large place-based RCTs. The inferential advantages of randomization depend on having enough units to randomize, such that the probability that a difference between exposure groups arose by chance is small. In traditional RCTs, this means a large sample size of individuals. In cluster-randomized trials where neighborhoods are the randomized units, this means having many neighborhoods under observation. However, each additional neighborhood unit typically brings with it substantial costs. Because the effects of place on health are expected to be subtle, cluster-randomized trials with sufficient power will need to be particularly large. These concerns are amplified when one considers that the information that can be gathered from such experiments is quite limited. For instance, in the example of the Chinese Housing Lottery, how might one separate out the mental health benefits of greenspace (aesthetic well-being) from public transit (well-being supported through active living and reduced auto-dependence) or rent subsidies (well-being induced from having more disposable income and therefore less financial stress)?
Efficiencies may be gained if researchers can join partnerships to evaluate planned developments, for which infrastructure and building resources have already been allocated. For instance, the Chinese government has been eager to work with researchers in studying the impact of planned “healthy, ecological communities” on indicators of well-being including psychological symptoms [27,28], and there have been examples evaluating new developments in the US [29] and Australia [30]. Such natural experiments are also beneficial because the process of change may be less artificial, and because of efficiencies that can be gained through the use of existing data systems. However, natural experiments may suffer from timing and fidelity complications that undermine plans to use their evaluation to test a particular causal question [31]. Moreover, few existing data systems (e.g., community surveys or surveillance systems) contain relevant mental health outcomes. For mental health data, one often needs to turn to billing data, which is subject to random error and differential misclassification (e.g., access to medical care, selective diagnoses to enhance billing). The routine collection of brief measures (such as the PHQ-2 or PHQ-9) in community surveys could overcome this limitation.
Causal effects of a particular place-based change may be isolated using study designs including relocation RCTs, cluster-randomized trials, and natural experiments. Unfortunately, even having completed such an investigation, questions may remain due to limited external validity.
Capturing variation in implementation to understand external validity
Even those large trials for which funding is allocated have limited relevance beyond the study region. Indeed the most relevant characteristics of place for supporting healthy behaviors appears to vary by national setting [32] or subpopulation [33]. Moreover, any effect of place on mental health outcomes invariably plays out within the context of time, both across the life course of an individual and across generations, raising analytic and conceptual issues (explored in more detail in Appendix 1).
In this light, mixed methods may improve placed-based research as they may help to explore hidden components of an intervention that pose a threat to external validity or help identify opportunities to adapt the implementation strategies to a new setting [34,35]. It may also be useful for maximizing place-based benefits that also depend on social cohesion and perceptions among residents.
Emerging strategies for studying place and mental health
Because of the methodological challenges highlighted above, studies correlating place and mental health are often met with skepticism [21]. Small-scale place-based RCTs and their observational analogues have potential to address this skepticism. Research linking place to mental health is well-poised to leapfrog key challenges faced by current place and health research.
Randomizing deployment of small-scale changes to place over time
Places are frequently redesigned or changed, and such “treatments” can be evaluated at a small geographic scale. Small-scale place-based RCTs have the potential to estimate the effect of changing place on the behaviors and health outcomes of people who use those places [36]. Importantly, the feasibility of rolling out a place-based enhancement strategy often takes years or decades. Randomizing the timing of deployment can minimize biases from self-selection without incurring excessive costs. Because randomized trials each address specific changes to a specific context, an accumulating number of such trials can collectively provide useful information on what does and doesn’t work. For example, as the mental health effects of greenspace, transit access, and subsidized rent are considered, some trials will consider these separately while others do so in combination, moving us toward an understanding of their distinct contributions to mental health, and potential synergies when deployed together.
Another topic that may be amenable to examination through using randomized trials is the link between mental health and exposure to physical disorder. Litter, graffiti, and other indicators of urban deterioration are associated with depressive symptoms [37]. Municipal departments of sanitation, particularly in cities with substantial building abandonment, often include graffiti cleanup squads charged with removing disorder. By randomizing districts to early versus late timing of graffiti cleanup, and monitoring changes in depression diagnoses, prescriptions, or other surveillance-based indicators of worsening mental health between districts, public health authorities might better understand the effectiveness of this change. Here, again, the problem of missing mental health information in existing data systems arises. When secondary data are inadequate, however, mobile phones show promise in monitoring short term changes in mood, behavior, or other experiences [38], and these approaches can explicitly incorporate geographic information [39]. In fact, apps can collect real-time data that links place to mood quite cheaply, and, to the extent that it is predictive of mental health, mood data may be more useful in short-term evaluations than clinical diagnostic thresholds (which can take months or years to show detectable change).
There are several advantages to focusing on ongoing or planned changes to place. The spatial unit will generally be selected for feasibility of intervention deployment, which can then guide measurement of the context for each participant. Second, because modification of place does not require moving people (which can confound measures of mental health), our quest to isolate causal effects does not risk disrupting social networks [40,41]. Third, in many instances practical health-promoting policies involve assessing and addressing the distinct characteristics of each place, which may help during adaptation of the approach to new settings. The reduced costs of working with smaller-scale changes to place may allow for more geographic units to be included and characterized, and thus for sufficient statistical power and potential to explore heterogeneous effects on health.
Optimizing deployment to allow for rigorous investigation of place and mental health
In general, deploying place-based changes in randomized (rather than targeted) order allows for the most rigorous analysis. However, public servants are charged with maximizing public benefits from public funds, and this may result in a strategy that prioritizes early investment in the most “at risk” locations. This creates a tension between a deployment strategy supporting rigorous study, and the deployment strategy that would be optimal if the intervention were already known to be effective.
As an example of this tension, consider an effort in New York City (NYC) to improve the walking environment near schools. Sites for improvements were chosen based on perceived need [42]. This deployment strategy introduced bias into investigators’ ability to develop knowledge about which interventions are the most beneficial. We emphasize that policy strategies posited to have health benefits are often based on only tenuous evidence, and those who advocate for them based on existing evidence are likely to be in tension with those seeking to add new (potentially disconfirming) evidence.
Moving forward, one underutilized aspect of deploying place-based policies or strategies is that such interventions are often rolled out over time. For their potential to be fully realized, these opportunities should be matched with an analysis strategy that takes full advantage of available longitudinal data. In doing so, it is important to consider the relationship between the outcome, the nature of the exposure, the duration of exposure, and the mobility of the population under study. In mental health research, the nature of the exposure under study (e.g., walking) or outcome (e.g., perceived psychological stress) it is difficult to separate the treated participants from untreated participants because the population tends to be much more mobile than those without mental illness. Thus, if walking actually reduces psychological stress in NYC, we may see an exaggerated effect size because those who didn’t experience stress reduction moved to the nearby state of New Jersey, so their stress scores were never captured.
Emerging analytic approaches to place-based studies exploit changes over time and draw on an analogy to randomized trials
Traditional approaches to incorporate time-varying information on an exposure of interest include mixed effects models, generalized estimating equations, and survival analysis. Others have scanned the geographic landscape to detect where the impact from an event had the greatest impact on mental health [43].
For a single intervention, a recently developed approach in the Bayesian tradition is a diffusion-regression state space model. Broadly, this approach treats each observation in a time-series as a parametric function of the previous observation in the series and of other covariates, potentially including time. Observed variance is then partitioned into overall time-trends, periodic time-trends, and estimated effects of covariates [44].
A diffusion-regression state space model can be used to estimate a causal effect from longitudinal data. To do so, the model is first used to estimate a synthetic control condition – that is, the overall time-trend, the periodic time-trend, and all covariates that are not a consequence of the intervention are used to estimate of what would have happened had an intervention not occurred. Contrasting this synthetic control with what was actually observed quantitatively explores the crucial “what if” question central to formal causal thinking: what health outcomes would we have seen if this intervention had not occurred? We illustrate this approach using data about a much acclaimed change to the pedestrian environment in New York City [45].
Case study: Did the opening of High Line Park increase nearby pedestrian activity?
Inspired by the promenade Plantee in Paris, the High Line Park is a 1.45-mile-long linear park in NYC along a previously disused section of railroad [45]. We can examine the casual effect of the High Line opening in 2009 on nearby pedestrian walking activity, and thus its potential proxy effect on attendant social, physical and mental health benefits. Physical activity, particularly if occurring in natural environments, has been tied to mental health benefits [46].
Longitudinal data on pedestrian activity both before and after the change are crucial to establishing the observed time trend and the “what if” time trend, or our projection of what would have happened without intervention. The NYC Department of Transportation has routinely collected pedestrian counts on 114 street segments in the city four days a year, one weekday and one weekend, each spring and fall, from 2007 to 2015. One of these segments is 14th street between Hudson Street and Eighth Avenue, which runs between a popular subway stop and High Line Park. Another busy street segment is on 42nd Street near Grand Central Station, a segment which started the study period with pedestrian counts similar to the 14th street segment. Using the city’s pedestrian count data in conjunction with a Bayesian structural time series model [44,47], we can estimate the causal effect of opening the High Line on pedestrian counts on 14th street.
We first fit a structural time series model predicting counts of pedestrians on 14th Street using pedestrian counts at our comparison location (42nd Street near Grand Central Station). This model predicted pedestrian counts on 14th Street for the period 2007–2008, prior to the opening of High Line Park. With features selected to maximize out-of-sample prediction, this model indeed predicted pre-opening trends in pedestrian counts at 14th Street very accurately (r2 of 0.97). Next, we used the model in combination with observed pedestrian counts on 42nd Street to predict what would have been observed at 14th Street had High Line Park not opened. Finally, we compared observed counts for 2009–2015 to the predicted time series. This approach was implemented using the CausalImpact package in R version 3.2.3 (Vienna, Austria) [48].
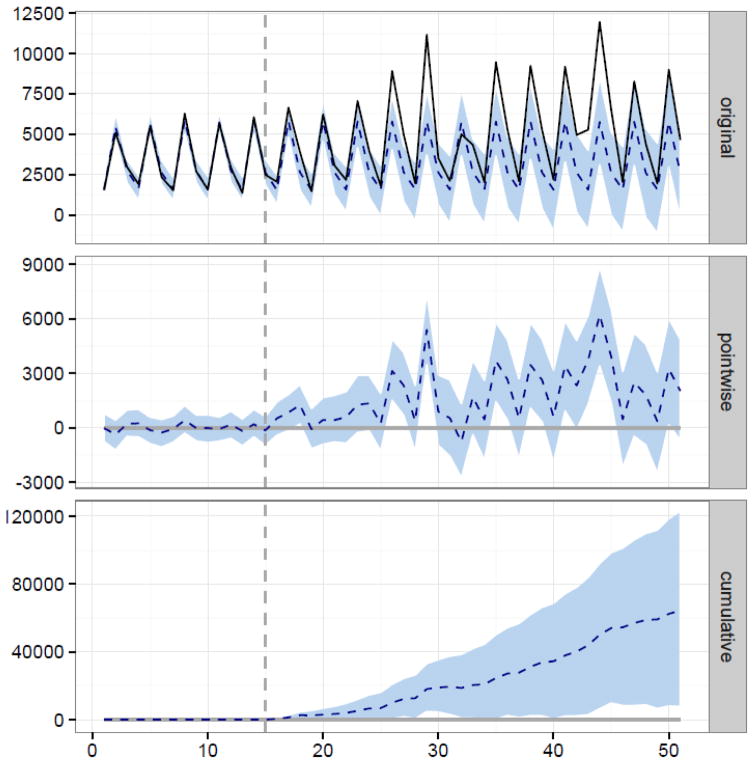
We estimate approximately a 54% increase in pedestrian traffic attributable to the opening of High Line Park (Table 2, Figure 1).
Table 2.
Estimated casual effect of opening the High Line on pedestrian counts on 14th Street between Eighth Avenue and Hudson Street, New York
| Estimate | 95% Posterior Interval | |
|---|---|---|
| Average pedestrian count predicted by the structural time series model in the period after the High Line opened | 3319 | 1690, 4892 |
| Observed average pedestrian count in the period after the High Line opened | 5109 | -- |
| Absolute Effect of opening the High Line on pedestrian counts | 1789 | 216, 3419 |
| Relative Effect of opening the High Line on pedestrian counts | 54% | 7%, 103% |
Figure 1.
Causal Effect of Opening the High Line on Pedestrian Counts on 14th Street between 8th Avenue and Hudson Street, New York City. Panel a) shows the time series of available counts, including the structural time series model predictions in the absence of opening the high line. Panel b) shows the difference between estimated and observed pedestrian counts on 14th street. Panel c) shows the estimated cumulative impact of opening the High Line. On all panels, the vertical line indicates the time at which the High Line was opened.
In the years since 2009, High Line Park has been extended north. Future evaluation efforts might consider emerging approaches particularly suited to evaluating the roll-out of an intervention over time such as the stepped wedge design [49].
This case study is limited by the data available for analysis. Enhanced park access appears to have increased the number of pedestrians walking in this particular location, but it does not necessarily follow that residents of the immediate area have become more active [50]. Rather, increased park access may have attracted more pedestrians from elsewhere (including tourists and those from distant neighborhoods). Yet even this enhanced pedestrian activity could be relevant to social contact within the neighborhood, which in turn has been linked to fewer depressive symptoms [51].
The diffusion-regression state space model builds on conventional difference-in-difference approaches in two ways. First, this approach incorporates the state-space model to decompose time series data into a trend and a periodic component, allowing for more accurate estimation of the counterfactual. Second, the approach allows for Bayesian model averaging in selecting the most appropriate time series with which to predict the counterfactual.
Lingering limitations of place-based approaches
Although we are encouraged by the promise of research using place-based approaches, there are important drawbacks to such approaches as well. While strategies to improve causal inference will continue to be developed and debated, we expect that disentangling the effects of particular context characteristics from selection of and movement within places will remain challenging.
For example, some of the challenges in the High Line Park example could have been solved using data from telecommunications companies or cellphone software on nearby walkers. Again, though, we must be mindful that mental illness interacts with our study outcomes. Even if we were collecting GPS, participants with severe mental illness not mitigated by the park would have been lost.
Another drawback is that place-based approaches are not sufficient if the evidence needed to guide action is focused on individual choices. For example, if exposure to physical disorder negatively affects mood, one response would be to advise individuals to avoid locations with more physical disorder. An individual-level study of how people respond to such advice may then be more appropriate than a place-based study. An alternate solution would be to remove physical disorder in public spaces; evidence for such an intervention would benefit from place-based research. More broadly, it would be problematic to infer that estimated causal effects of context on mental health are the same as causal effects related individual-level changes [52].
Conclusions
In his novel “Justine”, Lawrence Durrell wrote: "We are the children of our landscape; it dictates behavior and even thought in the measure to which we are responsive to it." His observation, frequently repeated in both fictional [53,54] and non-fictional [55] settings, sums up the peril and promise of place for our social and psychological well-being. In this paper, we have attempted to outline the difficulties of causal inference on such questions, and particularly of person-based randomized approaches to characterizing the causal effect of place on physical and mental health. We posited that small place-based RCTs and their observational analogues may partially address these difficulties, and describe a promising statistical approach to evaluating the causal effects of place-base changes that occur over time (Table 1).
Place-based evidence and how best to gather it is relevant in a number of socio-political contexts. In China, for example, officials at most levels of the government deliberately roll out policies in a quasi-experimental fashion so that their effects can be studied [27,36]. Despite this, urban development is often overlooked as a laboratory for rational policymaking. As a result, officials are scrambling to figure out how to reverse the adverse effects of the “car culture” that they have created [56].
Physical location and in particular its interaction with time, may be a missing component in many psychiatric epidemiologic inquiries despite the interest it used to garner [57]. While, we routinely assess individual characteristics of persons (risk factors), and often consider time (follow-up periods; life-course analyses), place is given only inconsistent attention. When we do consider potential effects of place, we seldom consider how such effects play out across time or interact with time. As inquiry proceeds to better locate individuals within multiple spaces across the days and decades of their lives, and as methods advance to allow us to better characterize the complex causes of disease, understanding the role of place and time in becomes central to informed action. Psychiatric epidemiology’s field of inquiry is already broadening to include place-based studies over time, and recent developments from the broader place and health literature can help the field to surmount key challenges and accelerate research progress.
Acknowledgments
The authors would like to acknowledge financial support from the National Institute of Child Health and Human Development (R01HD087460; K01HD067390). The contents of the manuscript are the sole responsibility of the authors and do not necessarily reflect the official views of the funding agency.
Appendix 1: Analytic issues regarding analyses of time and space
Broadly, spatiotemporal data can be thought of as correlated observations of counts of events within fixed spatial and temporal units that evolve over time. The foundational Poisson model for spatial analyses assumes independent events over both place and time. Additional methodological considerations must be used to take possible correlations between place and time into account. There might, for example, be a clustering of events over both place and time. As an example, so-called Hawke's processes can be used to predict events as disparate as the clustering of aftershocks following earthquakes [58] and terrorist attacks [59]. In the psychiatric literature, a similar approach was used to study possible clustering of psychiatric admissions to urban hospitals [60].
As epidemiologists, we are most often interested in disease counts in small areas over some period of time marked by repeated observations. Methodological approaches to spatiotemporal data vary. Bayesian methods are frequently seen in this context and can be traced to work by Besag [61] which was extended by Bernardinelli [62] to include a linear term for space-time interaction, and by Knorr-Held [63] to include a non-parametric spatio-temporal time trend. These type of data have been used to used to characterize suicide risk by location and seasonal temperature [64] and the role of built environment on depressive symptoms. [65] Among the more intriguing applications of spatiotemporal modeling to psychiatric disorders is in the characterization of resting-state neural activity in the brains of persons with schizophrenia [66]. An approach involving structural equation models was been used to demonstrate a link between neighborhood and cognitive ability across generations [67].
Footnotes
Conflicts of interest: The authors declare that they have no conflict of interest
References
- 1.Silver M. Planners and Public Health Professionals Need to Partner... Again. North Carolina medical journal. 2012;73(4):290. [PubMed] [Google Scholar]
- 2.Mooney SJ, Knox J, Morabia A. The Thompson-McFadden Commission and Joseph Goldberger: contrasting 2 historical investigations of pellagra in cotton mill villages in South Carolina. Am J Epidemiol. 2014;180(3):235–244. doi: 10.1093/aje/kwu134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pickett KE, Pearl M. Multilevel analyses of neighbourhood socioeconomic context and health outcomes: a critical review. J Epidemiol Community Health. 2001;55(2):111–122. doi: 10.1136/jech.55.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Galea S, Ahern J, Nandi A, Tracy M, Beard J, Vlahov D. Urban neighborhood poverty and the incidence of depression in a population-based cohort study. Ann Epidemiol. 2007;17(3):171–179. doi: 10.1016/j.annepidem.2006.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.DiMaggio C, Galea S, Emch M. Spatial proximity and the risk of psychopathology after a terrorist attack. Psychiatry research. 2010;176(1):55–61. doi: 10.1016/j.psychres.2008.10.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Halpern D. Mental health and the built environment: more than bricks and mortar? Routledge; 2014. [Google Scholar]
- 7.Evans GW. The built environment and mental health. Journal of Urban Health. 2003;80(4):536–555. doi: 10.1093/jurban/jtg063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Xue Y, Leventhal T, Brooks-Gunn J, Earls FJ. Neighborhood residence and mental health problems of 5-to 11-year-olds. Archives of General Psychiatry. 2005;62(5):554–563. doi: 10.1001/archpsyc.62.5.554. [DOI] [PubMed] [Google Scholar]
- 9.Burls A. People and green spaces: promoting public health and mental well-being through ecotherapy. Journal of Public Mental Health. 2007;6(3):24–39. [Google Scholar]
- 10.Leventhal T, Brooks-Gunn J. Moving to opportunity: an experimental study of neighborhood effects on mental health. Am J Public Health. 2003;93(9):1576–1582. doi: 10.2105/ajph.93.9.1576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dohrenwend BP, Levav I, Shrout PE, Schwartz S, Naveh G, Link BG. Disorders: The Causation-Selection Issue. 1992. [DOI] [PubMed] [Google Scholar]
- 12.Frank LD, Saelens BE, Powell KE, Chapman JE. Stepping towards causation: do built environments or neighborhood and travel preferences explain physical activity, driving, and obesity? Soc Sci Med. 2007;65(9):1898–1914. doi: 10.1016/j.socscimed.2007.05.053. S0277-9536(07)00313-9 [pii] [DOI] [PubMed] [Google Scholar]
- 13.Takahashi LM. The socio-spatial stigmatization of homelessness and HIV/AIDS: toward an explanation of the NIMBY syndrome. Social Science & Medicine. 1997;45(6):903–914. doi: 10.1016/s0277-9536(96)00432-7. [DOI] [PubMed] [Google Scholar]
- 14.Hansen HB, Donaldson Z, Link BG, Bearman PS, Hopper K, Bates LM, Cheslack-Postava K, Harper K, Holmes SM, Lovasi G, Springer KW, Teitler JO. Independent Review Of Social And Population Variation In Mental Health Could Improve Diagnosis In DSM Revisions. Health affairs. 2013;32(5):984–993. doi: 10.1377/hlthaff.2011.0596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Beutel ME, Jünger C, Klein EM, Wild P, Lackner K, Blettner M, Binder H, Michal M, Wiltink J, Brähler E. Noise annoyance is associated with depression and anxiety in the general population-the contribution of aircraft noise. PLoS one. 2016;11(5):e0155357. doi: 10.1371/journal.pone.0155357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rundle AG, Sheehan DM, Quinn JW, Bartley K, Eisenhower D, Bader MM, Lovasi GS, Neckerman KM. Using GPS data to study neighborhood walkability and physical activity. American journal of preventive medicine. 2016;50(3):e65–e72. doi: 10.1016/j.amepre.2015.07.033. [DOI] [PubMed] [Google Scholar]
- 17.Hirsch JA, Winters M, Clarke P, McKay H. Generating GPS activity spaces that shed light upon the mobility habits of older adults: a descriptive analysis. Int J Health Geogr. 2014;13:51. doi: 10.1186/1476-072X-13-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lovasi GS, Grady S, Rundle A. Steps Forward: Review and Recommendations for Research on Walkability, Physical Activity and Cardiovascular Health. Public Health Reviews. 2012;33(2):484–506. doi: 10.1007/BF03391647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.York CoN. Active Living Guidelines: Promoting Physical Activity and Health in Design. New York City: 2010. [Google Scholar]
- 20.Buchner DM, Schmid T. Active living research and public health: natural partners in a new field. Am J Prev Med. 2009;36(2 Suppl):S44–46. doi: 10.1016/j.amepre.2008.11.003. S0749-3797(08)00914-8 [pii] [DOI] [PubMed] [Google Scholar]
- 21.Oakes JM. The (mis)estimation of neighborhood effects: causal inference for a practicable social epidemiology. Soc Sci Med. 2004;58(10):1929–1952. doi: 10.1016/j.socscimed.2003.08.004. [DOI] [PubMed] [Google Scholar]
- 22.Hygiene NYCDoHaM. Epiquery: NYC Interactive Health Data System. 2010 https://a816-healthpsi.nyc.gov/epiquery/EpiQuery/
- 23.Liebman JB, Katz LF, Kling J. KSG Working Papers. SSRN; Cambridge, MA: 2004. Beyond treatment effects: estimating the relationship between neighborhood poverty and individual outcomes in the MTO experiment. [Google Scholar]
- 24.Blacksher E, Lovasi GS. Place-focused physical activity research, human agency, and social justice in public health: taking agency seriously in studies of the built environment. Health Place. 2012;18(2):172–179. doi: 10.1016/j.healthplace.2011.08.019. S1353-8292(11)00159-6 [pii] [DOI] [PubMed] [Google Scholar]
- 25.Venkatapuram S, Marmot M. Epidemiology and social justice in light of social determinants of health research. Bioethics. 2009;23(2):79–89. doi: 10.1111/j.1467-8519.2008.00714.x. BIOT714 [pii] [DOI] [PubMed] [Google Scholar]
- 26.Wang Y. Disparities in Pediatric Obesity in the United States. Advances in Nutrition: An International Review Journal. 2011;2(1):23. doi: 10.3945/an.110.000083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ma J, Lin M. Policymaking in China: A review of Chinese scholarship. China Review. 2012:95–121. [Google Scholar]
- 28.Zheng W, Chow W-H, Yang G, Jin F, Rothman N, Blair A, Li H-L, Wen W, Ji BT, Li Q. The Shanghai Women's Health Study: rationale, study design, and baseline characteristics. American journal of epidemiology. 2005;162(11):1123–1131. doi: 10.1093/aje/kwi322. [DOI] [PubMed] [Google Scholar]
- 29.Dunton GF, Intille SS, Wolch J, Pentz MA. Investigating the impact of a smart growth community on the contexts of children's physical activity using Ecological Momentary Assessment. Health Place. 2012;18(1):76–84. doi: 10.1016/j.healthplace.2011.07.007. S1353-8292(11)00123-7 [pii] [DOI] [PubMed] [Google Scholar]
- 30.Knuiman MW, Christian HE, Divitini ML, Foster SA, Bull FC, Badland HM, Giles-Corti B. A longitudinal analysis of the influence of the neighborhood built environment on walking for transportation: the RESIDE study. Am J Epidemiol. 2014;180(5):453–461. doi: 10.1093/aje/kwu171. [DOI] [PubMed] [Google Scholar]
- 31.Lovasi GS, Goldsmith J. Invited Commentary: Taking Advantage of Time-Varying Neighborhood Environments. Am J Epidemiol. 2014 doi: 10.1093/aje/kwu170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ding D, Adams MA, Sallis JF, Norman GJ, Hovell MF, Chambers CD, Hofstetter CR, Bowles HR, Hagstromer M, Craig CL, Gomez LF, De Bourdeaudhuij I, Macfarlane DJ, Ainsworth BE, Bergman P, Bull FC, Carr H, Klasson-Heggebo L, Inoue S, Murase N, Matsudo S, Matsudo V, McLean G, Sjostrom M, Tomten H, Lefevre J, Volbekiene V, Bauman AE. Perceived neighborhood environment and physical activity in 11 countries: do associations differ by country? Int J Behav Nutr Phys Act. 2013;10:57. doi: 10.1186/1479-5868-10-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lovasi GS, Hutson MA, Guerra M, Neckerman KM. Built environments and obesity in disadvantaged populations. Epidemiol Rev. 2009;31:7–20. doi: 10.1093/epirev/mxp005. mxp005 [pii] [DOI] [PubMed] [Google Scholar]
- 34.Friche A, Dias M, Reis P, Dias C, Caiaffa W, BH-Viva P. Urban upgrading and its impact on health: a" quasi-experimental" mixed-methods study protocol for the BH-Viva Project. Cadernos de saúde pública. 2015;31:51. doi: 10.1590/0102-311X00079715. [DOI] [PubMed] [Google Scholar]
- 35.Garvin E, Branas C, Keddem S, Sellman J, Cannuscio C. More than just an eyesore: local insights and solutions on vacant land and urban health. Journal of Urban Health. 2013;90(3):412–426. doi: 10.1007/s11524-012-9782-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Muennig P. What China's experiment in community building can tell us about tackling health disparities: Community Building and Mental Health in Mid-Life and Older Life: Evidence from China. Social Science & Medicine. 2014;107:217–220. doi: 10.1016/j.socscimed.2014.01.026. [DOI] [PubMed] [Google Scholar]
- 37.Joshi S, Mooney SJ, Rundle AG, Quinn J, Beard J, Cerda M. Pathways from neighborhood poverty to depression among older adults. doi: 10.1016/j.healthplace.2016.12.003. (Under Review) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sandstrom GM, Lathia N, Mascolo C, Rentfrow PJ. Opportunities for Smartphones in Clinical Care: The Future of Mobile Mood Monitoring. The Journal of clinical psychiatry. 2016;77(2):135–137. doi: 10.4088/JCP.15com10054. [DOI] [PubMed] [Google Scholar]
- 39.Kirchner TR, Shiffman S. Spatio-temporal determinants of mental health and well-being: advances in geographically-explicit ecological momentary assessment (GEMA) Social Psychiatry and Psychiatric Epidemiology. 2016;51(9):1211–1223. doi: 10.1007/s00127-016-1277-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Scott SB, Jackson BR, Bergeman CS. What contributes to perceived stress in later life? A recursive partitioning approach. Psychology and aging. 2011;26(4):830–843. doi: 10.1037/a0023180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hawkley LC, Cacioppo JT. Loneliness and pathways to disease. Brain Behav Immun. 2003;17(Suppl 1):S98–105. doi: 10.1016/s0889-1591(02)00073-9. S0889159102000739 [pii] [DOI] [PubMed] [Google Scholar]
- 42.Dimaggio C, Li G. Effectiveness of a safe routes to school program in preventing school-aged pedestrian injury. Pediatrics. 2013;131(2):290–296. doi: 10.1542/peds.2012-2182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gruebner O, Lowe SR, Tracy M, Cerdá M, Joshi S, Norris FH, Galea S. The geography of mental health and general wellness in Galveston Bay after Hurricane Ike: a spatial epidemiologic study with longitudinal data. Disaster medicine and public health preparedness. 2016;10(02):261–273. doi: 10.1017/dmp.2015.172. [DOI] [PubMed] [Google Scholar]
- 44.Scott SL, Varian HR. Predicting the present with bayesian structural time series. International Journal of Mathematical Modelling and Numerical Optimisation. 2014;5(1–2):4–23. [Google Scholar]
- 45.Millington N. From urban scar to ‘park in the sky’: terrain vague, urban design, and the remaking of New York City’s High Line Park. Environment and Planning A. 2015 0308518X15599294. [Google Scholar]
- 46.Mitchell R. Is physical activity in natural environments better for mental health than physical activity in other environments? Social Science & Medicine. 2013;91:130–134. doi: 10.1016/j.socscimed.2012.04.012. [DOI] [PubMed] [Google Scholar]
- 47.Brodersen KH, Gallusser F, Koehler J, Remy N, Scott SL. Inferring causal impact using Bayesian structural time-series models. The Annals of Applied Statistics. 2015;9(1):247–274. [Google Scholar]
- 48.Team RCD. R: A language and environment for statistical computing. R Foundation for Statistical Computing; Vienna, Austria: 2016. [Google Scholar]
- 49.Spiegelman D. Evaluating Public Health Interventions: 2. Stepping Up to Routine Public Health Evaluation With the Stepped Wedge Design. Am J Public Health. 2016;106(3):453–457. doi: 10.2105/AJPH.2016.303068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bancroft C, Joshi S, Rundle A, Hutson M, Chong C, Weiss CC, Genkinger J, Neckerman K, Lovasi G. Association of proximity and density of parks and objectively measured physical activity in the United States: A systematic review. Soc Sci Med. 2015;138:22–30. doi: 10.1016/j.socscimed.2015.05.034. [DOI] [PubMed] [Google Scholar]
- 51.Kruger DJ, Reischl TM, Gee GC. Neighborhood social conditions mediate the association between physical deterioration and mental health. American journal of community psychology. 2007;40(3–4):261–271. doi: 10.1007/s10464-007-9139-7. [DOI] [PubMed] [Google Scholar]
- 52.Diez Roux AV. A glossary for multilevel analysis. J Epidemiol Community Health. 2002;56(8):588–594. doi: 10.1136/jech.56.8.588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Pynchon T. Gravity's rainbow. Penguin; 2012. [Google Scholar]
- 54.Salinger JD. The Catcher in the Rye. 1951. New York: Little; 1991. [Google Scholar]
- 55.Klinenberg E. Heat wave: A social autopsy of disaster in Chicago. University of Chicago Press; 2015. [DOI] [PubMed] [Google Scholar]
- 56.Chen E, Schreier HMC, Strunk R, Brauer M. Chronic traffic-related air pollution and stress interact to predict biological and clinical outcomes in asthma. Env Health Perspec. 2008 doi: 10.1289/ehp.11076. doi:10.10.1289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Brody H, Rip MR, Vinten-Johansen P, Paneth N, Rachman S. Map-making and myth-making in Broad Street: the London cholera epidemic, 1854. The Lancet. 2000;356(9223):64–68. doi: 10.1016/S0140-6736(00)02442-9. [DOI] [PubMed] [Google Scholar]
- 58.Hawkes AG. Spectra of some self-exciting and mutually exciting point processes. Biometrika. 1971;58(1):83–90. [Google Scholar]
- 59.Tench S, Fry H, Gill P. Spatio-temporal patterns of IED usage by the Provisional Irish Republican Army. European Journal of Applied Mathematics. 2016;27(03):377–402. [Google Scholar]
- 60.Meyer S, Warnke I, Rössler W, Held L. Model-based testing for space–time interaction using point processes: An application to psychiatric hospital admissions in an urban area. Spatial and spatio-temporal epidemiology. 2016;17:15–25. doi: 10.1016/j.sste.2016.03.002. [DOI] [PubMed] [Google Scholar]
- 61.Besag J, York J, Mollié A. Bayesian image restoration, with two applications in spatial statistics. Annals of the institute of statistical mathematics. 1991;43(1):1–20. [Google Scholar]
- 62.Bernardinelli L, Clayton D, Pascutto C, Montomoli C, Ghislandi M, Songini M. Bayesian analysis of space—time variation in disease risk. Statistics in medicine. 1995;14(21–22):2433–2443. doi: 10.1002/sim.4780142112. [DOI] [PubMed] [Google Scholar]
- 63.Knorr-Held L. Bayesian modelling of inseparable space-time variation in disease risk. 1999 doi: 10.1002/1097-0258(20000915/30)19:17/18<2555::aid-sim587>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 64.Qi X, Tong S, Hu W. Preliminary spatiotemporal analysis of the association between socio-environmental factors and suicide. Environmental Health. 2009;8(1):1. doi: 10.1186/1476-069X-8-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Duncan DT, Piras G, Dunn EC, Johnson RM, Melly SJ, Molnar BE. The built environment and depressive symptoms among urban youth: a spatial regression study. Spatial and spatio-temporal epidemiology. 2013;5:11–25. doi: 10.1016/j.sste.2013.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Northoff G. Is schizophrenia a spatiotemporal disorder of the brain's resting state? World Psychiatry. 2015;14(1):34–35. doi: 10.1002/wps.20177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Sharkey P, Elwert F. The legacy of disadvantage: Multigenerational neighborhood effects on cognitive ability. AJS; American journal of sociology. 2011;116(6):1934. doi: 10.1086/660009. [DOI] [PMC free article] [PubMed] [Google Scholar]