Abstract
MUC1 is a type I transmembrane glycoprotein and is overexpressed in various epithelial tumor tissues. Some researchers have demonstrated that the glycosylation status of MUC1 can affect MUC1-mediated tumor growth and cell differentiation. In our previous study, we proved that the abilities of cell proliferation, adhesion, invasion and metastasis, and drug resistance were enhanced in ovarian cancer cells stably expressing Lewis(y). Therefore, we hypothesized that Lewis(y) antigen may play a central role in regulating MUC1 expression, and MUC1-mediated cell growth and differentiation may be closely associated with Lewis(y) antigen. This study aimed to examine the correlation between MUC1 expression and Lewis(y) antigen levels in ovarian cancer cell lines and tissue samples. A series of techniques, including RT-qPCR, western blot anlaysis, immunoprecipitation, immunohistochemistry and double-labeling immunofluorescence were applied to detect the expression of Lewis(y) and MUC1. In malignant epithelial ovarian tumors, the positive expression rates of Lewis(y) antigen and MUC1 were 88.33 and 86.67%, respectively, which were markedly higher than those in borderline (60.00 and 53.33%, P<0.05), benign (33.33 and 30%, P<0.01) and normal (0 and 25%, P<0.01) ovarian samples. There was no correlation between the positive expression rates of Lewis(y) or MUC1 and clinicopathological parameters in ovarian cancers (P>0.05). The expression levels of Lewis(y) and MUC1 correlated with the clinical FIGO stage (P<0.05). Both MUC1 and Lewis(y) were highly expressed in ovarian cancer tissues, and their expression levels were positively correlated (P<0.01). In α1,2-fucosyltransferase (α1,2-FT)-transfected cells, the gene and protein expression levels of MUC1 were significantly upregulated compared with the cells that did not overexpress α1,2-FT (P<0.05). The ratio of Lewis(y) immunoprecipitated with MUC1 to total MUC1 increased 1.55-fold in α1,2-FT-overexpressing cells (P<0.05). The overexpression of Lewis(y) resulted in the upregulation of MUC1. On the whole, our data indicate that both MUC1 and Lewis(y) are associated with the occurrence and development of ovarian cancers.
Keywords: epithelial ovarian tumor, MUC1, Lewis(y) antigen, glycoprotein
Introduction
Glycosyl antigen, an important component of glycoproteins and glycolipids, is widely expressed in the cell membrane. Lewis(y) antigen is a difucosylated oligosaccharide with two fucoses carried by glycoconjugates (glycoproteins and glycolipids) on the cell surface. It belongs to the A, B and H Lewis blood group of antigens family with specific fucosylation of the terminal end of carbohydrate structure catalyzed by the α1,2-fucosyltransferase (α1,2-FT) (1). The overexpression of Lewis(y) has been found in 70–90% of human carcinomas of epithelial cell origin, including breast, ovary, prostate and colon cancer, and its high expression has been shown to be associated with a poor prognosis (2,3). The alterations of type II carbohydrate chains, such as Lewis(x) and Lewis(y), are common in ovarian cancer (4). The overexpression of Lewis(y) antigen, which is closely associated with prognosis, exists in 75% of epithelial ovarian cancers. CA125, a tumor marker in epithelial ovarian cancer, also contains Lewis(y) structure (5).
In our previous studies, human α1,2-FT, a key enzyme in the synthesis of Lewis(y), was transfected into the ovarian cancer cell line, RMG-I, which has endogenously a low expression of Lewis(y), by gene transfection technology and the ovarian cancer cell line, RMG-I-H, with a stable and high expression of Lewis(y) was established. Compared with the RMG-I cells, the RMG-I-H cells exhibited enhanced abilities of cell proliferation, invasion, metastasis and drug resistance, indicating that Lewis(y) plays a critical role in the progression of ovarian cancer (6,7).
MUC1 is a type I transmembrane glycoprotein and is overexpressed in various epithelial tumor tissues. Through the activation of other receptor molecules and signaling pathways, MUC1 can directly or indirectly affect the biological behaviors of tumor cells (8). Some researchers have demonstrated that the glycosylation status of MUC1 can affect MUC1-mediated tumor growth and cell differentiation (9,10). We thus hypothesized that Lewis(y) antigen may play a central role in MUC1 expression, and that MUC1-mediated cell growth and differentiation may be closely associated with Lewis(y) antigen.
In this study, we first investigated the expression pattern and the correlation of Lewis(y) and MUC1 in ovarian serous and mucinous carcinoma tissue specimens by immunohistochemistry. At the same time, double-labeling immunofluorescence, co-immunoprecipitation, western blot analysis and reverse transcription-quantitative PCR (RT-qPCR) were carried out to further elucidate the correlation of Lewis(y) antigen and MUC1 in many aspects. Our study provides a theoretical mechanism of ovarian carcinogenesis and tumor progression, and a possible target for the development of biological treatments.
Materials and methods
Materials
The following reagents were purchased from commercial sources: Dulbecco's modified Eagle's medium (DMEM) and fetal bovine serum (FBS) from HyClone (Logan, UT, USA); trypsin and ethylenediamine tetraacetic acid (EDTA) from Amresco (Solon, OH, USA). Mouse anti-human Lewis(y) monoclonal antibody (clone A70-C/C8; ab217909) was purchased from Abcam (Cambridge, UK). Rabbit anti-human MUC1 polyclonal antibody (sc-15333), HRP-labeled second antibodies (sc-51948) and protein G plus-agarose (sc-500778) were obtained from Santa Cruz Biotechnology, Inc. (Santa Cruz, CA, USA). Goat monoclonal anti-mouse immunoglobulin E tetramethylrhodamine isothiocyanate (TRITC; ZF-0313) and goat monoclonal anti-rabbit immunoglobulin G fluorescein isothiocyanate (FITC; ZF-0311) were purchased from Zhongshan Biotechnology (Beijing, China). The immunohistochemical SP kit was purchased from Mai Xin Co. (Fujian, China). TRIzol reagent, the PrimeScript™ RT reagent kit and SYBR® Premix Ex Taq™ were purchased from Takara Biotechnology Co. (Dalian, China). The sequences of the primers were synthesized by Invitrogen Co. (Shanghai, China).
Patients and tissue samples
A total of 140 selected paraffin-embedded samples are obtained from surgeries performed between 2000 to 2009 at the Obstetrics and Gynecology, Shengjing Hospital Affiliated to China Medical University, Shenyang, China. This study was approved by the Ethics Committee of Shengjing Hospital Affiliated to China Medical University (approval no. 2012PS96K) and written informed consent was obtained from all participants prior to obtaining the samples. All the tissue sections were diagnosed by specialists. There were 60 cases of primary malignant ovarian tumors (including 30 mucous and 30 serous cystadenocarcinomas), 30 borderline ovarian tumors, 30 benign ovarian tumors and 20 normal ovarian tissues (from the normal ovarian tissue excised in the cervical cancer surgeries). The mean age of these patients was 47.89 years (15–73 years). The age range of the ovarian cancer group was 36–73 years and the median age was 53 years. The age range of the borderline ovarian tumor group was 22–55 years and median age was 35 years. The age ranges of the benign ovarian tumor and normal tissue groups were 15–72 and 37–52 years, respectively and hte median ages were 44 and 42 years, respectively. Comparing these groups, there was no statistically significant difference (P>0.05). According to the pathological grading, the ovarian cancer group contained 21 cases of high differentiation; 21 middle differentiation and 18 cases of low differentiation. The group included 39 cases of stages I–II and 21 cases of stages III–VI according to the International Federation of Gynecology and Obstetrics (FIGO) standard; there were also 12 cases of metastases to the pelvic lymph nodes. All the cases were primary, and the information was complete; chemical treatment was not used in any of the patients prior to surgery.
Cell culture and treatment
The RMG-I cell line, which originated from human ovarian clear cell carcinoma, was donated by Professor Iwamori Masao of Tokyo University in Japan. A RMG-I cell line, stabling expressing the α1,2-FT gene was established as previously described (11), and was termed RMG-I-H. We transfected α1, 2-FT plasmids and empty plasmids into the RMG-I cells using a Cellphect Transfection kit (Pharmacia, Piscataway, NJ, USA). Transfection was performed according to the manufacturer's instructions. The cells were cultured in DMEM supplemented with 10% FBS at 37°C, 5% CO2 in humidified air. For treatment with anti-Lewis(y) antibody, the final concentration was 10 µg/ml. The duration of treatment was 24 h.
Immunohistochemistry and immunocytochemistry
Histological sections from each group of ovarian tissue were 5-µm-thick. The expression levels of Lewis(y) and MUC1 in the ovarian carcinoma tissues were analyzed by immunohistochemical streptavidin-peroxidase staining. A colon cancer sample served as the positive control for Lewis(y) antigen, and a breast cancer sample (obtained from the Pathology archive of Shengjing Hospital Affiliated to China Medical University) was used as a positive control for MUC1. The group treated with phosphate-buffered saline (PBS) instead of the primary antibody was used as a negative control. The working concentrations of the primary antibodies against Lewis(y) and MUC1 were all 1:150. The empirical procedure was performed according to instructions provided with the kit (immunohistochemical SP kit).
The RMG-I-H and RMG-I cells at the exponential phase of growth were digested by 0.25% trypsin and cultured in DMEM containing 10% FBS to prepare single-cell suspension. The cells were washed twice with cold PBS when growing in a single layer, and fixed with 4% paraformaldehyde for 30 min. The expression of MUC1 in the cells was detected according to the instructions provided with the SP kit. The concentration of MUC1 monoclonal antibody was 1:200. The primary antibody was replaced by PBS for the negative control. Normal mouse IgG (10 µg/ml; sc-2025; Santa Cruz Biotechnology, Inc.) acted as an irrelevant isotype-matched control.
Two independent investigators examined all tumor slides randomly. Five views were examined per slide, and 100 cells were observed per view at ×400 magnification. The immunostaining of Lewis(y) and MUC1 was scored following a semi-quantitative scale by evaluating in representative tumor areas the intensity and percentage of tumor cells. Nuclear and cytoplasmic immunostaining in tumor cells was considered as positive staining. The intensity of Lewis(y) and MUC1 staining was scored as 0 (negative), 1 (weak), 2 (moderate) and 3 (strong). Percentage scores were assigned as 1, 1–25%; 2, 26–50%; 3, 51–75%; and 4, 76–100%. The scores of each tumor sample were multiplied to yield a final score of 0–12, and the tumors were finally determined as negative (−) expression with a score of <4, and a tumor sample with a score of ≥4 was considered as positive. Tumors with a score of ≥4 and <7 were classified as '+'; tumors with a score of ≥7 and <10 were classified as '++'; and tumors with a score of ≥10 were classified as '+++'.
The average optical densities (MOD) were measured under a microscope (BX53; Olympus, Tokyo, Japan) with image processing, being presented as the means ± standard deviation for 3 separate experiments.
Western blot analysis
The cells were washed twice with ice-cold PBS, scraped in lysis buffer [50 mM Tris-HCl (pH 7.4), 150 mM NaCl, 0.5% NP-40, 100 mM NaF, 200 µM Na3VO4, and 10 µg/ml each aprotinin, leupeptin, PMSF and pepstatin], and incubated for 30 min at 4°C while rocking. Lysates were cleared by centrifugation (10 min at 12,000 rpm, 4°C). For immunoblot analysis, the protein content was measured using the protein assay BCA kit (Beyotime Biotechnology, Shanghai, China) and 50 µg of total protein were resolved by sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) and transferred onto poly(vinylidene difluoride) membranes. The membranes were blocked with TTBS [25 mM Tris-HCl, 150 mM NaCl (pH 7.5) and 0.1% Tween-20] containing 5% nonfat milk for 2 h and incubated overnight at 4°C with the appropriate primary antibodies at the dilutions recommended by the suppliers in TBST/1% non-fat milk. The blots were washed in TTBS and incubated with the appropriate HRP-labeled anti-rabbit secondary antibody, and immunoreactive proteins were visualized with ECL detection system. The western blots shown are representative of at least 3 independent experiments. Densitometry of each band for the target proteins was quantified by densitometric analysis with LabWorks 4.6 software. The protein band intensity was quantified by the mean ± SEM of 3 experiments for each group as determined from densitometry relative to β-actin (4967; Cell Signaling Technology, Danvers, MA, USA).
Immunoprecipitation
Washed monolayer cells were lysed with 200 µl lysis buffer as described above. Following protein determination, cell lysate containing 500 µg proteins was incubated with 5 µg of MUC1 antibody, and incubated at 4°C for overnight. Protein G plus-agarose was added and the samples were incubated at 4°C for 3 h for immunoprecipitation.
In brief, the cells immunoprecipitated with MUC1 were subjected to SDS/PAGE, and then transferred onto a poly(vinylidene difluoride) membrane and treated with 1:1,000 diluted anti-Lewis(y) and 1:500 diluted anti-MUC1 sera in Tris-buffered saline with 5% non-fat milk, followed by 1:1,000 HRP-labeled secondary antibody. Finally, the color was developed with enhanced chemiluminescence reagents (Pierce; Thermo Fisher Scientific, Waltham, MA, USA), and followed by densitometric scanning.
Double-labeling immunofluorescence
RMG-I-H cells were used to create a cell climbing slice. Cells were fixed with 4% paraformaldehyde. The tissue sections were selected tissues that exhibited a strong positive result in immunohistochemistry using the double-labeling immunofluorescence method. After blocking with normal goat serum, the cells and sections were incubated primarily with antibodies against Lewis(y) (1:150) and MUC1 (1:150) at the same time. Negative control sections were incubated with PBS instead of the primary antibody. The working concentrations of FITC and TRITC were all 1:100. Nuclei were counterstained with DAPI. The empirical procedure was performed according to the instructions provided with the kit. The stained slides were observed under a laser confocal microscope (C1-SI; Nikon, Tokyo, Japan). Data were collected using a computer and digital images were generated.
RT-qPCR
Total RNA was extracted from the RMG-I and RMG-I-H cells at the exponential phase of growth using TRIzol reagent (1 ml/1×107 cells). The concentration and purity of the RNA were examined using an ultraviolet spectrometer. cDNA was synthesized according to the instructions provided with the RNA reverse transcription kit (Takara Biotechnology Co.). The reaction system contained 4 µl of 5X PrimeScript™ buffer, 1 µl of PrimeScript™ RT Enzyme Mix I, 1 µl of 50 µmol/l oligo(dT) primer, 1 µl of 100 µmol/l Random 6 mers, 2 µl of total RNA, and 11 µl of RNase-free dH2O. The reaction conditions were 37°C for 15 min, 85°C for 5 sec, and 4°C for 5 min. The primer sequences of the MUC1 gene primers were forward, 5′-CGTCGTGGACATTGATGGTA-3′ and reverse, 5′-GGTACCTCCTCTCACCTCCT-3′. The primer sequences of the β-actin gene were forward, 5′-GGACTTCGAGCAAGAGATGG-3′and reverse, 5′-ACATCTGCTGGAAGGTGGAC-3′. The reaction system for real-time fluorescent PCR contained 10 µl of 2X SYBR® Premix Ex Taq™, 1 µl of 5 µmol/l PCR forward primer, 1 µl of 5 µmol/l PCR reverse primer, 2 µl of cDNA and 6 µl of dH2O. The reaction conditions included denaturation at 94°C for 20 sec, 45 cycles of 94°C for 20 sec and 62°C for 20 sec. The Light Cycler PCR system (Roche Diagnostics, Mannheim, Germany) was used for real-time PCR amplification and Ct value detection. The melting curves were analyzed after amplification. PCR reactions of each sample were carried out in triplicate. The change in the target gene expression level was calculated using the 2−ΔΔCq method (12).
Assessment standard and statistical analysis
The presence of brown-colored granules on the cell membrane or in the cytoplasm was considered a positive signal, and was divided by color intensity into not colored, light yellow, brown and tan, and was recorded as 0, 1, 2 and 3, respectively. We selected 5 high-power fields in series from each slice, and these were scored, and the average percentage of stained cells was calculated. A positive cell rate of <5% was given a score of 0, a positive cell rate of 5–25% was given a score of 1, a positive cell rate of 26–50% was given a score of 2, a positive cell rate of 51–75% was given a score of 3, and a positive cell rate of >75% was given a score of 4. The final score was determined by multiplying the positive cell rate and score values: 0–2 was equal to negative expression (−), 3–4 was equal to weakly positive (+), 5–8 was equal to moderately positive (++) and 9–12 was equal to strongly positive (+++). The results were read by 2 independent observers to control for variability. Microscopic red fluorescence indicated Lewis(y) antigen labeled by TRITC, green fluorescence indicated MUC1 labeled by FITC. Images of the 2 individual fluorescence channels were superimposed using image analysis software, with yellow fluorescence indicating the co-localization of Lewis(y) antigen and MUC1. The software SPSS version 16.0 (SPSS, Inc., Chicago, IL, USA) was used for statistical analysis. Data are expressed as the means ± SD. The Student's t test was applied to compare data between the 2 groups, and analysis of variance was applied to compare data among multiple groups. The Chi-square (χ2) test was applied to analyze the expression of Lewis(y) antigen, MUC1 and clinicopathological parameters. The correlation between Lewis(y) antigen and MUC1 expression was examined using Linear correlation and Spearman's rank correlation analysis in ovarian tumors. A value of P<0.05 was considered to indicate a statistically significant difference.
Results
Expression of Lewis(y) antigen and MUC1 in ovarian tissue groups
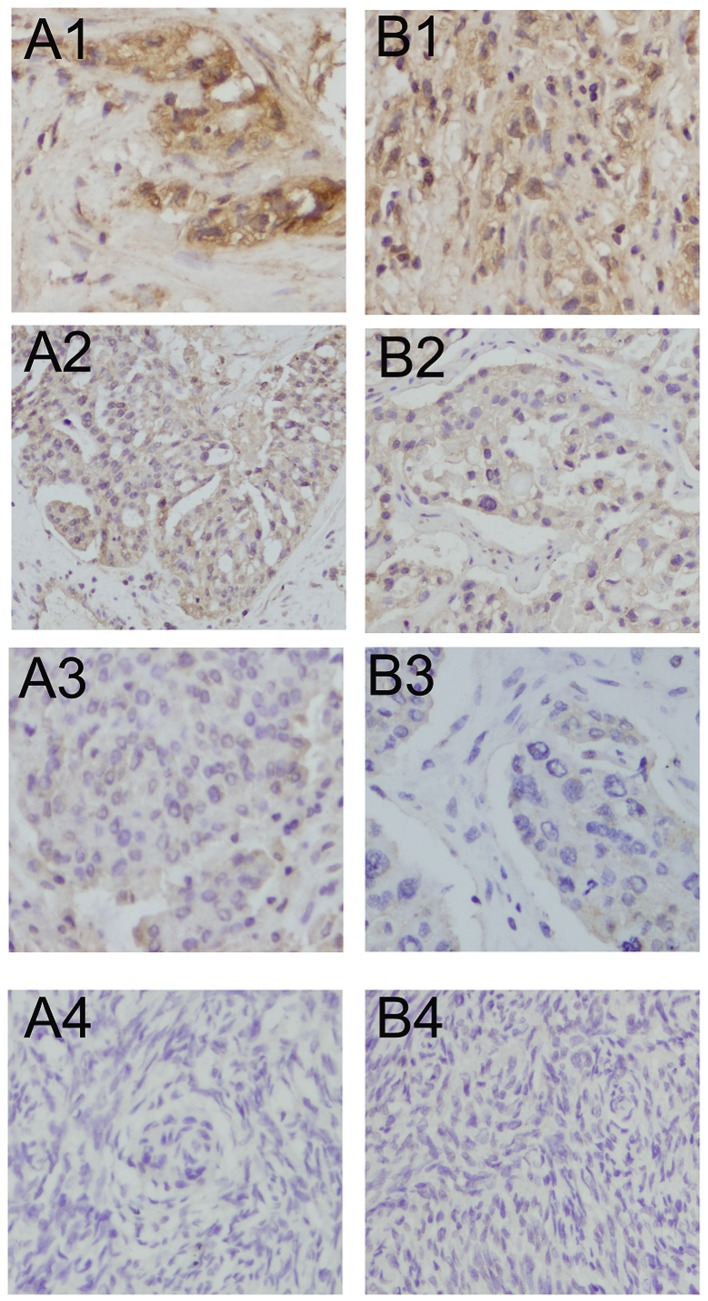
Lewis(y) was mainly localized in the cell membrane, and detected to a limited extent in the cytoplasm. The positive expression rates in the malignant, borderline, benign and normal ovarian tissues for Lewis(y) antigen were 88.33, 60.00, 33.33 and 0%, respectively. The malignant groups displayed the highest positive expression and was significantly higher than the rate of the borderline (P<0.05) and benign and normal groups (P<0.01). The expression rates in borderline groups were markedly higher than those in the normal group (P<0.01). No Lewis(y) expression was detected in the normal groups. However, the difference in positive expression rates for Lewis(y) between ovarian borderline tumors and benign tumors was not statistically significant (P>0.05) (Table I and Fig. 1).
Table I.
Expression of Lewis(y) antigen and MUC1 in various ovarian tissues.
| Group | Cases | Lewis(y)
|
Positive cases | Rate (%) | MUC1
|
Positive cases | Rate (%) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| − | + | ++ | +++ | − | + | ++ | +++ | ||||||
| Malignant group | 60 | 7 | 15 | 20 | 18 | 53 | 88.33a | 8 | 14 | 24 | 14 | 52 | 86.67a |
| Borderline group | 30 | 12 | 6 | 11 | 1 | 18 | 60b | 14 | 9 | 5 | 2 | 16 | 53.33 |
| Benign group | 30 | 20 | 6 | 4 | 0 | 10 | 33.33 | 21 | 6 | 3 | 0 | 9 | 30 |
| Normal group | 20 | 20 | 0 | 0 | 0 | 0 | 0 | 15 | 5 | 0 | 0 | 5 | 25 |
P<0.05 compared with borderline; P<0.01 compared with benign and normal group;
P<0.01 compared with normal group.
Figure 1.
Immunohistochemical staining of Lewis(y) antigen and MUC1 in various ovarian tissues (×400 magnification). (A1–A4) Lewis(y) antigen expression in ovarian malignant tumor, borderline tumor, benign tumor and normal ovarian tissues, respectively; (B1–B4) MUC1 expression in ovarian malignant tumor, borderline tumor, benign tumor and normal ovarian tissues respectively.
MUC1 was mainly detected in the cell membrane with sparse localization in the cytoplasm and nucleus. In malignant epithelial ovarian tumors, the positive expression rate of MUC1 (86.67%) was significantly higher than that in the borderline (53.33%) (P<0.05), benign (30.00%) (P<0.01) and normal ovarian samples (25.00%) (P<0.01). Paired comparisons between the borderline, benign and normal ovarian samples identified no significant difference in positive expression rates (P>0.05) (Table I and Fig. 1).
Correlation of MUC1 and Lewis(y) antigen positive expression rates and clinical features of ovarian cancer
In ovarian serous and mucinous carcinomas, the positive expression rates of Lewis(y) were 90.00 and 86.67%, respectively, which were similar (Chi-square test, P>0.05) (data not shown). Lewis(y) was detected in 95.2% of the cases with stages III–IV ovarian cancer. The rate of expression was higher than that in the cases with stages I–II of the disease (82.05%), although this difference did not reach statistical significance (P>0.05). The expression rates of Lewis(y) in the high, moderate and poor differentiation groups were 80.95, 85.71 and 100%, respectively; however, this increase in the Lewis(y) positive rate with a decrease in the cell differentiation level was not statistically significant (P>0.05). The positive rate of Lewis(y) in the lymphatic metastasis group (100%) was higher than that of the non-lymphatic metastasis group (85.42%), although this difference was not significant in statistical analysis (P>0.05) (Table II).
Table II.
Association between Lewis(y) antigen and MUC1 expression, expression intensity and pathological features in ovarian cancer.
| Features | Case | Lewis(y)
|
MUC1
|
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Positive cases | Rate (%) | P-value | MOD | P-value | Positive cases | Rate (%) | P-value | MOD | P-value | ||
| FIGO stage | |||||||||||
| I–II | 39 | 33 | 84.62 | >0.05 | 0.438±0.089 | <0.05 | 31 | 79.49 | >0.05 | 0.421±0.097 | <0.05 |
| III–IV | 21 | 20 | 95.24 | 0.501±0.098 | 21 | 100 | 0.510±0.083 | ||||
| Differentiation level | |||||||||||
| High | 21 | 17 | 80.95 | >0.05 | 0.431±0.089 | <0.05a | 18 | 85.71 | >0.05 | 0.440±0.095 | <0.05a |
| Moderate | 21 | 18 | 85.71 | 0.465±0.092 | >0.05b | 17 | 80.95 | 0.456±0.081 | >0.05b | ||
| Poor | 18 | 18 | 100 | 0.493±0.104 | <0.05c | 17 | 94.44 | 0.476±0.092 | <0.05c | ||
| Lymphatic metastasis | |||||||||||
| No | 48 | 41 | 85.42 | >0.05 | 0.457±0.094 | >0.05 | 42 | 87.5 | >0.05 | 0.451±0.098 | >0.05 |
| Yes | 12 | 12 | 100 | 0.489±0.077 | 10 | 83.33 | 0.485±0.069 | ||||
Compared with the low differentiation group;
compared with the low and high differentiation groups;
compared with the high differentiation group.
The positive expression rates of MUC1 in the serous and mucinous carcinomas were 90.00 and 83.33% respectively, which did not exhibit a significant difference (Chi-square test, P>0.05) (data not shown). The MUC1 positive rate was detected in 100% of the cases with stages III–IV ovarian cancer. The rate of expression was higher than that in stages I–II (79.49%), although this difference did not reach statistical significance (P>0.05). In the ovarian cancer tissues with high, moderate and poor differentiation, the positive rates of MUC1 were 85.71, 80.95 and 94.44%, respectively, with no statistical significance being detected among the 3 group (P>0.05). The positive rate of MUC1 in the lymphatic metastasis group (83.33%) was not significantly higher than that in the lymphatic metastasis-free group (87.50%) (P>0.05) (Table II).
Correlation of MUC1 and Lewis(y) antigen staining intensity and clinical features of ovarian cancer
We detected and analyzed the staining intensity of ovarian cancer sections that were positive for Lewis(y) and MUC1 by immunohistochemistry. In the tissues with stages III–IV ovarian cancer, the mean optical density (MOD) of Lewis(y) was 0.501±0.098, which was significantly higher than that in stages I–II (0.438±0.089) (P<0.05). In the ovarian cancer tissue with poor differentiation, the MOD of Lewis(y) was 0.493±0.104, which was significantly higher than the value (0.431±0.089) obtained from the well differentiation group (P<0.05). However, there was no significant difference when Lewis(y) staining intensities in the moderate differentiation group were compared with those in the high or poor differentiation group (P>0.05). We also found that the staining intensity of Lewis(y) did not correlate with the histological type of ovarian cancer or with lymph node metastasis (P>0.05) (Table II).
The MOD of MUC1 in the cases with stages III–IV ovarian cancer was 0.510±0.083, which was significantly higher than that in stages I–II (0.421±0.097) (P<0.05). In the ovarian cancer tissues with poor differentiation, the MOD of MUC1 was 0.476±0.092, which was significantly higher than the value (0.440±0.095) obtained from the well differentiation group (P<0.05). However, there was no significant difference when Lewis(y) staining intensities in the moderate differentiation group were compared with those in the well or poor differentiation group (P>0.05). In accordance with Lewis(y), the MOD of MUC1 did not correlate with the histological type of ovarian cancer or with lymph node metastasis (P>0.05) (Table II).
Relevance of MUC1 and Lewis (y) antigen expression in ovarian cancer
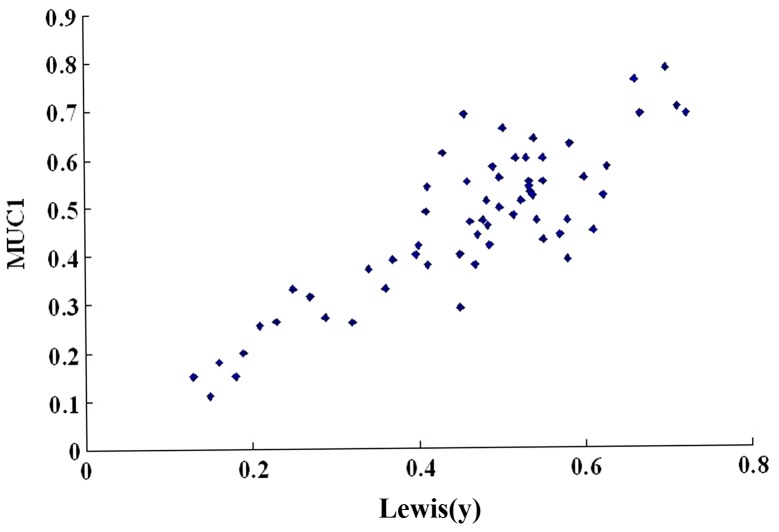
We then used a scatter plot of the MOD value to analyze the relevance of MUC1 and Lewis(y) antigen expression in ovarian cancer. In the majority of cases, the ovarian cancer tissues that highly expressed Lewis(y) antigen concomitantly expressed high levels of MUC1; the expression patterns of MUC1 and Lewis(y) antigen linearly correlated (r=0.657, P<0.01) (Table III and Fig. 2). In addition, Spearman's rank correlation was performed. There was a significant association between MUC1 and Lewis(y) antigen based on the IHC scoring system (P<0.05).
Table III.
Expression and correlation of Lewis(y) antigen and MUC1 in ovarian cancer.
| N | Expression of MUC1
|
||||
|---|---|---|---|---|---|
| (−) | (+) | (++) | (+++) | ||
| Expression of Lewis(y) antigen | |||||
| (−) | 7 | 4 | 2 | 1 | 0 |
| (+) | 15 | 2 | 7 | 4 | 2 |
| (++) | 20 | 2 | 4 | 12 | 2 |
| (+++) | 18 | 0 | 1 | 7 | 10 |
| case | 60 | 8 | 14 | 24 | 14 |
Figure 2.
Scatter plot of mean optical density (MOD) value of Lewis(y) antigen and MUC1 in ovarian cancer. The expression intensities of Lewis(y) antigen and MUC1 were linearly correlated (r=0.657, P<0.01).
MUC1 expression in RMG-I-H cells is higher than that in RMG-I cells
In our previous study, human α1,2-FT, a key enzyme in the synthesis of Lewis(y), was transfected into the ovarian cancer cell line, RMG-I, which has an endogenously low expression of Lewis(y), by gene transfection technology, and the ovarian cancer cell line, RMG-I-H, with a stable and high expression of Lewis(y) was established.
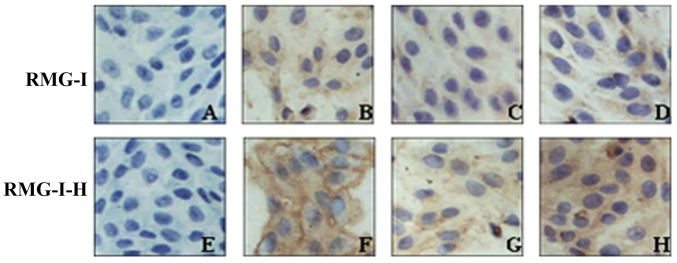
The results of immunocytochemistry revealed that MUC1 was localized in the cytoplasm and membrane. In the RMG-I cells, MUC1 staining presented as light yellow particles and its MOD value was 0.187±0.011. In the RMG-I-H cells, MUC1 staining presented as brown yellow particles and its MOD value was 0.498±0.023, which was significantly higher than that in the RMG-I cells P<0.01) (Fig. 3 and Table IV). In order to demonstrate whether Lewis(y) is the central factor of regulating MUC1 expression, we pre-treated the RMG-I cells and RMG-I-H cells with Lewis(y) monoclonal antibody. Following treatment with Lewis(y) antibody, the expression of MUC1 was decreased in both the RMG-I-H cells and RMG-I cells (P<0.01), although no significant difference was observed between these 2 cell lines (P>0.05). However, following treatment with an irrelevant isotype IgG, MUC1 expression was not altered in the RMG-I-H cells and RMG-I cells (Fig. 3 and Table IV).
Figure 3.
Immunocytochemical staining of MUC1 in cells before and after α1,2-fucosyltransferase (α1,2-FT) gene transfection (×400 magnification). (A and E) Negative control; (B and F) no treatment; (C and G) pre-treatment with Lewis(y) mAb; (D and H) pre-treatment with irrelevant isotype IgG as control.
Table IV.
Average optical indensity of MUC1 in RMG-I and RMG-I-H cells.
| RMG-I | RMG-I-H | |
|---|---|---|
| Negative control | 0.024±0.019 | 0.025±0.018 |
| No treatment | 0.187±0.011 | 0.498±0.023a |
| Pre-treatment with Lewis(y)mAb | 0.125±0.009b | 0.138±0.013b |
| Pre-treatment with irrelevant isotype IgG | 0.194±0.008 | 0.469±0.019 |
P<0.01 vs. RMG-I cell;
P<0.01 vs. irrelevant isotype-matched control.
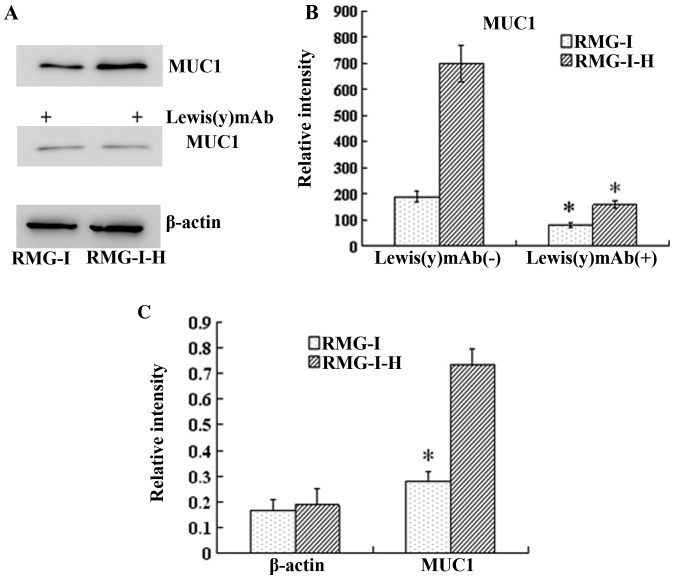
We used RT-qPCR to examine the changes in the mRNA expression levels of MUC1 following transfection with human α1,2-FT. Our results revealed that the mRNA level of MUC1 in the RMG-I-H cells was 1.35-fold higher than that in the RMG-I cells (P<0.01), indicating that MUC1 was regulated at the transcriptional level (Fig. 4).
Figure 4.
Expression of MUC1 proteins in RMG-I and RMG-I-H cells before and after anti-Lewis(y) monoclonal antibody treatment, and the Lewis(y) content of the glycans of MUC1 before and after α1,2-fucosyltransferase (α1,2-FT) gene transfection. (A) Western blots of MUC1 protein in ovarian carcinoma-derived RMG-I and RMG-I-H cells using MUC1 antibody and HRP-labeled secondary antibodies. (B) Densitometric quantification of MUC1 in (A). *P<0.01 compared with RMG-I-H cells without Lewis(y) mAb treatment. Data are presented as the means ± SD (n=3). *P<0.05. (C) RT-qPCR results of mRNA expression of MUC1 of in RMG-I and RMG-I-H cells. *P<0.01 compared with RMG-I-H cells.
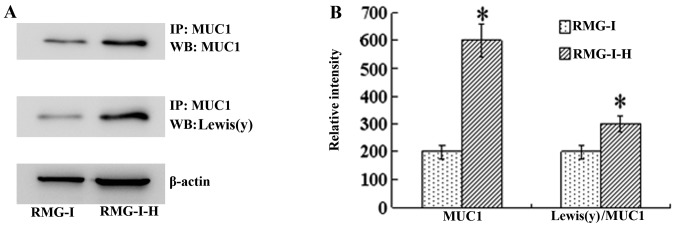
Similarly, the results of western blot analysis demonstrated that the total amount of MUC1 protein was increased in the RMG-I-H cells 3.68-fold compared with the RMG-I cells (P<0.01). When Lewis(y) was blocked with monoclonal antibody, the protein expression of MUC1 was decreased significantly (P<0.01) (Fig. 4). Moreover, the level of Lewis(y) interacting with MUC1 was observed by immunoprecipitation. The ratio of total Lewis(y) immunoprecipitated with MUC1 to total MUC1 protein was increased in the RMG-I-H cells 1.55-fold compared with the RMG-I cells (P<0.01) (Fig. 5).
Figure 5.
Expression of MUC1 and Lewis(y) antigen of the glycans of MUC1 before and after α1,2-fucosyltransferase (α1,2-FT) gene transfection. (A) Western blots of immunoprecipitated MUC1 protein using corresponding antibodies and Lewis(y) antibody and HRP-labeled secondary antibodies. (B) Densitometric quantification of Lewis(y) in (A) and calculation of Lewis(y) expression/MUC1 (set the RMG-I cells as 100%) (n=3). *P<0.01 compared with RMG-I. IP, immunoprecipitation by the antibody of MUC1; WB, western blot with antibodies to MUC1 or Lewis(y). Data are presented as the means ± SD (n=3). *P<0.05.
Co-localization of Lewis(y) and MUC1 protein in epithelial ovarian cancer tissues and cells
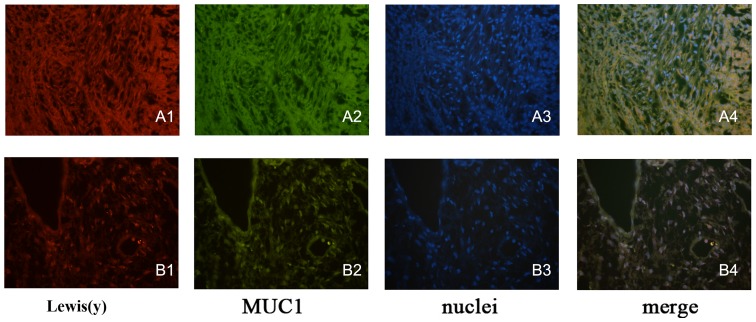
Double-labeling immunofluorescence experiments revealed that red fluorescence-labeled Lewis(y) was localized in the cell membrane, while green fluorescence-labeled MUC1 also appeared in the cell membrane, but was observed to a limited extent in the cytoplasm, and the blue fluorescence staining indicated the nucleus after staining with DAPI. Images were obtained, and image analysis software used to build up 3 fluorescence passages: yellow fluorescence appeared in the positions where red and green fluorescence overlapped simultaneously. Our findings clearly illustrated that MUC1 and Lewis(y) antigen co-localized at the same positions in ovarian cancer tissues and the RMG-I-H cell line (Fig. 6).
Figure 6.
Lewis(y) and MUC1 co-localize in ovarian cancer tissues (A) and ovarian carcinoma cell RMG-I-H (B) (×400 magnification). Using double-labeling immunofluorescence method, Lewis(y) (A1 and B1), MUC1 (A2 and B2), nuclei stained with DAPI (A3 and B3), merged image [(A4 and B4) co-localization (yellow) of Lewis(y) and MUC1].
Discussion
Cell surface receptors predominantly are populated by glycoproteins, and the changes in the carbohydrate chainsstructure can affect its expression and function (13). Some hallmarks of malignant tumor cells, such as adhesion, migration and proliferation, are related to changes in specific carbohydrate chains or residues (14). Fucose residue is a terminal structure of glycan which is involved in the formation of carbohydrate moieties of certain key growth factors, it also plays an important role in mechanisms of tumor growth (15).
Lewis(y) antigen is a difucosylated oligosaccharide antigen, and Lewis(y) expression has been shown to be significantly increased during carcinogenisis, including ovarian cancer, pancreatic cancer, prostate cancer, colon cancer and non-small cell lung cancer (16–22). Lewis(y) can promote tumor angiogenesis (23), inhibit cell apoptosis, and can lead to enhanced cell proliferation and invasion (24). In this study, we confirmed that the Lewis(y) positive expression rate in ovarian cancer tissues was significantly higher than that in borderline, benign and normal groups. In addition, the expression intensity of Lewis(y) increased as the malignancy grade increased. These results indicate a positive correlation between the expression of Lewis(y) antigen and the occurrence and development of ovarian cancer.
MUC1 is a type I transmembrane glycoprotein of high molecular weight (>200 kDa). The carbohydrate chains account for >50% of the molecular weight of MUC1, and play an important role in determining the biochemical features and functionality of MUC1 (25). The abnormal expression of MUC1 exists in a series of malignant tumors. First, the expression levels of MUC1 in malignant tumors is markedly increased compared with normal tissues. Second, MUC1 localization loses its polar distribution, and is instead expressed on the entire cell surface. Third, the structure of MUC1 is altered due to elevated glycosyltransferase activity and abnormal glycosylation. More importantly, MUC1 can protect the structure of the cell surface, release active molecules and is involved in signal transduction, immunomodulation, tumor invasion and metastasis (26,27). MUC1 expression has been found to be higher in tumors with a poor prognosis, demonstrating that the expression of MUC1 is closely associated with tumor development and the prognosis of patients (28,29). Feng et al (30) reported that the expression of MUC1 was associated with the FIGO clinical stage and prognosis, and MUC1 expression and FIGO stage could be recognized as independent prognostic indicators through multivariate analysis. In accordance with previous reports, we found a weak positive expression of MUC1 in normal ovarian tissue. We also noted that the MUC1 expression rate in malignant epithelial ovarian tumors was significantly higher than that in borderline, benign and normal ovarian samples. The expression intensity of MUC1 increased with the malignancy level (P<0.05) and correlated with the FIGO stage (P<0.05). Moreover, the analysis of staining intensity in ovarian cancer tissues indicated that Lewis(y) linearly correlated with MUC1 (r=0.657, P<0.01). Furthermore, using the double-labeling immunofluorescence method, we found that Lewis(y) and MUC1 were located in the same position in ovarian cancer tissues.
Despite that Lewis(y) or MUC1 have been separately reported to be overexpressed and promote cell invasion in various types of human cancer, a direct correlation between Lewis(y) and MUC1 has never been described. Most epithelial tumor cells overexpress Lewis(y) antigen (2), and this may result in the Lewis(y)-induced modification of glycoprotein structures and functions on the cell surface (31). Some researchers have proven that the oligosaccharide chains of MUC1 protein contain the structure of Lewis(y) antigen. We thus speculated that the expression levels of MUC1 and its ability to mediate cell growth and differentiation may be related to Lewis(y) antigen on the cell surface. In this study, we used a scatter plot of the MOD value to analyze the relevance of MUC1 and Lewis(y) antigen expression in ovarian cancer and found a linear correlation between the expression patterns of MUC1 and Lewis(y) antigen. In our previous study, human α1,2-FT, a key enzyme in the synthesis of Lewis(y), was transfected into the ovarian cancer cell line, RMG-I, and the RMG-I-H cell line with a stable and high expression of Lewis(y) was established. In this study, using RT-qPCR, western blot analysis and immunocytochemistry, we discovered that the gene and protein expression levels of MUC1 in the α1,2-FT-transfected cells were significantly upregulated compared with the cells that did not overexpress α1,2-FT. Immunoprecipitation experiments revealed that the ratio of Lewis(y) immunoprecipitated with MUC1 to total MUC1 increased 1.55-fold in the α1,2-FT-overexpressing cells. Exposure to anti-Lewis(y) antibodies can block MUC1 upregulation. The above-mentioned results indicated that the overexpression of Lewis(y) resulted in the upregulation of MUC1. Some studies have found that the abnormal glycosylation of MUC1 can weaken the antitumor effect of DNA vaccine against MUC1 (32), and enhance the adhesion and metastasis of tumor cells (33,34). In double-labeling immunofluorescence experiments, our findings clearly illustrated that MUC1 and Lewis(y) antigen co-localized at the same positions in ovarian cancer tissues and the RMG-I-H cells. We thus speculated the existence of an association between the upregulation of MUC1 expression and the changes in the carbohydrate chain structure of cell surface receptors in the α1,2-FT-transfected cells. As a part of exposed carbohydrate chains of MUC1, the increased content of Lewis(y) can affect the three-dimensional structure of MUC1 protein, exposing more protein binding sites and tyrosine/serine phosphorylation sites, leading to the elevated phosphorylation of MUC1. As a result, downstream signal transduction pathways are activated and growth signals accelerating gene transcription are delivered to the nucleus, finally promoting the expression of MUC1.
In conclusion, in this study, correlation and co-expression were found between Lewis(y) antigen and MUC1 in ovarian cancer tissues. Lewis(y) antigen and MUC1 are relevant to the staging of ovarian cancer. Lewis(y) antigen was not only a subdivision of MUC1, but also accelerated the gene transcription of MUC1 in the endonucleus and then upregulated the expression level of MUC1 proteins. Lewis(y) and MUC1 may be recognized as important indicators of biological behaviors in ovarian cancer. Although the specific mechanisms in this process still need to be elucidated, our results provide new insight into the pathogenesis and development, as well as the treatment of ovarian cancer.
Acknowledgments
This study was supported by the National Natural Science Foundation of China (nos. 30872757, 81072118, 81172491 and 81101527); Ph.D. Programs Foundation of Ministry of Education of China (nos. 20112104110016 and 20112104120019); Science Committee Foundation of Shenyang City, China (no. F10-14-9-9-52); Shengjing Free Researcher Project (no. 200807).
References
- 1.Goupille C, Hallouin F, Meflah K, Le Pendu J. Increase of rat colon carcinoma cells tumorigenicity by alpha(1-2)fucosyltransferase gene transfection. Glycobiology. 1997;7:221–229. doi: 10.1093/glycob/7.2.221. [DOI] [PubMed] [Google Scholar]
- 2.Hellström I, Garrigues HJ, Garrigues U, Hellström KE. Highly tumor-reactive, internalizing, mouse monoclonal antibodies to Le(y)-related cell surface antigens. Cancer Res. 1990;50:2183–2190. [PubMed] [Google Scholar]
- 3.Madjd Z, Parsons T, Watson NF, Spendlove I, Ellis I, Durrant LG. High expression of Lewis y/b antigens is associated with decreased survival in lymph node negative breast carcinomas. Breast Cancer Res. 2005;7:R780–R787. doi: 10.1186/bcr1305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yang Z, Wu JH, Kuo HW, Kannagi R, Wu AM. Expression of sialyl Lex, sialyl Lea, Lex and Ley glycotopes in secreted human ovarian cyst glycoproteins. Biochimie. 2009;91:423–433. doi: 10.1016/j.biochi.2008.11.002. [DOI] [PubMed] [Google Scholar]
- 5.Rodríguez-Burford C, Barnes MN, Berry W, Partridge EE, Grizzle WE. Immunohistochemical expression of molecular markers in an avian model: A potential model for preclinical evaluation of agents for ovarian cancer chemoprevention. Gynecol Oncol. 2001;81:373–379. doi: 10.1006/gyno.2001.6191. [DOI] [PubMed] [Google Scholar]
- 6.Lin B, Hao YY, Wang DD, Zhu LC, Zhang SL, Saito M, Iwamori M. Transfection of alpha1, 2-fucosyltransferase gene increases the antigenic expression of Lewis y in ovarian cancer cell line RMG-I. Zhongguo Yi Xue Ke Xue Yuan Xue Bao. 2008;30:284–289. In Chinese. [PubMed] [Google Scholar]
- 7.Hao YY, Lin B, Zhao Y, Zhang YH, Li FF, Diao B, Ou YL, Zhang SL. Alpha1,2-fucosyltransferase gene transfection influences on biological behavior of ovarian carcinoma-derived RMG-I cells. Fen Zi Xi Bao Sheng Wu Xue Bao. 2008;41:435–442. In Chinese. [PubMed] [Google Scholar]
- 8.Yin L, Kharbanda S, Kufe D. Mucin 1 oncoprotein blocks hypoxia-inducible factor 1alpha activation in a survival response to hypoxia. J Biol Chem. 2007;282:257–266. doi: 10.1074/jbc.M610156200. [DOI] [PubMed] [Google Scholar]
- 9.Creaney J, Segal A, Sterrett G, Platten MA, Baker E, Murch AR, Nowak AK, Robinson BW, Millward MJ. Overexpression and altered glycosylation of MUC1 in malignant mesothelioma. Br J Cancer. 2008;98:1562–1569. doi: 10.1038/sj.bjc.6604340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Premaratne P, Welén K, Damber JE, Hansson GC, Bäckström M. O-glycosylation of MUC1 mucin in prostate cancer and the effects of its expression on tumor growth in a prostate cancer xenograft model. Tumour Biol. 2011;32:203–213. doi: 10.1007/s13277-010-0114-9. [DOI] [PubMed] [Google Scholar]
- 11.Iwamori M, Tanaka K, Kubushiro K, Lin B, Kiguchi K, Ishiwata I, Tsukazaki K, Nozawa S. Alterations in the glycolipid composition and cellular properties of ovarian carcinoma-derived RMG-1 cells on transfection of the alpha1,2-fucosyltransferase gene. Cancer Sci. 2005;96:26–30. doi: 10.1111/j.1349-7006.2005.00005.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 13.Engelstaedter V, Fluegel B, Kunze S, Mayr D, Friese K, Jeschke U, Bergauer F. Expression of the carbohydrate tumour marker Sialyl Lewis A, Sialyl Lewis X, Lewis Y and Thomsen-Friedenreich antigen in normal squamous epithelium of the uterine cervix, cervical dysplasia and cervical cancer. Histol Histopathol. 2012;27:507–514. doi: 10.14670/HH-27.507. [DOI] [PubMed] [Google Scholar]
- 14.Kim YS, Hwang SY, Kang HY, Sohn H, Oh S, Kim JY, Yoo JS, Kim YH, Kim CH, Jeon JH, et al. Functional proteomics study reveals that N-Acetylglucosaminyltransferase V reinforces the invasive/metastatic potential of colon cancer through aberrant glycosylation on tissue inhibitor of metalloproteinase-1. Mol Cell Proteomics. 2008;7:1–14. doi: 10.1074/mcp.M700084-MCP200. [DOI] [PubMed] [Google Scholar]
- 15.Mejías-Luque R, López-Ferrer A, Garrido M, Fabra A, de Bolós C. Changes in the invasive and metastatic capacities of HT-29/M3 cells induced by the expression of fucosyltransferase 1. Cancer Sci. 2007;98:1000–1005. doi: 10.1111/j.1349-7006.2007.00484.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chhieng DC, Rodriguez-Burford C, Talley LI, Sviglin H, Stockard CR, Kleinberg MJ, Barnes MN, Partridge EE, Khazaeli MB, Grizzle WE. Expression of CEA, Tag-72, and Lewis-Y antigen in primary and metastatic lesions of ovarian carcinoma. Hum Pathol. 2003;34:1016–1021. doi: 10.1053/S0046-8177(03)00355-1. [DOI] [PubMed] [Google Scholar]
- 17.Kuemmel A, Single K, Bittinger F, Faldum A, Schmidt LH, Sebastian M, Taube C, Buhl R, Wiewrodt R. The prognostic impact of blood group-related antigen Lewis Y and the ABH blood groups in resected non-small cell lung cancer. Tumour Biol. 2007;28:340–349. doi: 10.1159/000124298. [DOI] [PubMed] [Google Scholar]
- 18.Kobayashi H, Boelte KC, Lin PC. Endothelial cell adhesion molecules and cancer progression. Curr Med Chem. 2007;14:377–386. doi: 10.2174/092986707779941032. [DOI] [PubMed] [Google Scholar]
- 19.Li Q, Liu S, Lin B, Yan L, Wang Y, Wang C, Zhang S. Expression and correlation of Lewis y antigen and integrins α5 and β1 in ovarian serous and mucinous carcinoma. Int J Gynecol Cancer. 2010;20:1482–1489. doi: 10.1111/IGC.0b013e3181ea7ecb. [DOI] [PubMed] [Google Scholar]
- 20.Baldus SE, Hanisch FG, Pütz C, Flucke U, Mönig SP, Schneider PM, Thiele J, Hölscher AH, Dienes HP. Immunoreactivity of Lewis blood group and mucin peptide core antigens: Correlations with grade of dysplasia and malignant transformation in the colorectal adenoma-carcinoma sequence. Histol Histopathol. 2002;17:191–198. doi: 10.14670/HH-17.191. [DOI] [PubMed] [Google Scholar]
- 21.López-Ferrer A, de Bolós C, Barranco C, Garrido M, Isern J, Carlstedt I, Reis CA, Torrado J, Real FX. Role of fucosyltransferases in the association between apomucin and Lewis antigen expression in normal and malignant gastric epithelium. Gut. 2000;47:349–356. doi: 10.1136/gut.47.3.349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kim YS, Yuan M, Itzkowitz SH, Sun QB, Kaizu T, Palekar A, Trump BF, Hakomori S. Expression of LeY and extended LeY blood group-related antigens in human malignant, premalignant, and nonmalignant colonic tissues. Cancer Res. 1986;46:5985–5992. [PubMed] [Google Scholar]
- 23.Kuo CH, Chen PK, Chang BI, Sung MC, Shi CS, Lee JS, Chang CF, Shi GY, Wu HL. The recombinant lectin-like domain of thrombomodulin inhibits angiogenesis through inter-action with Lewis Y antigen. Blood. 2012;119:1302–1313. doi: 10.1182/blood-2011-08-376038. [DOI] [PubMed] [Google Scholar]
- 24.Wang C, Yan L, Wang Y, Lin B, Liu S, Li Q, Gao L, Zhang S, Iwamori M. Overexpression of Lewis(y) antigen protects ovarian cancer RMG-1 cells from carboplatin-induced apoptosis by the upregulation of Topo-I and Topo-II β. Anat Rec (Hoboken) 2011;294:961–969. doi: 10.1002/ar.21398. [DOI] [PubMed] [Google Scholar]
- 25.Kawano T, Ahmad R, Nogi H, Agata N, Anderson K, Kufe D. MUC1 oncoprotein promotes growth and survival of human multiple myeloma cells. Int J Oncol. 2008;33:153–159. [PMC free article] [PubMed] [Google Scholar]
- 26.Kufe DW. Functional targeting of the MUC1 oncogene in human cancers. Cancer Biol Ther. 2009;8:1197–1203. doi: 10.4161/cbt.8.13.8844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pająk J, Liszka L, Mrowiec S, Gołka D, Lampe P. MUC1 immunoexpression is a virtually constant feature of clear cell renal cell carcinoma metastatic to the pancreas. Adv Anat Pathol. 2012;19:125–127. doi: 10.1097/PAP.0b013e318248bd97. [DOI] [PubMed] [Google Scholar]
- 28.Khodarev NN, Pitroda SP, Beckett MA, MacDermed DM, Huang L, Kufe DW, Weichselbaum RR. MUC1-induced transcriptional programs associated with tumorigenesis predict outcome in breast and lung cancer. Cancer Res. 2009;69:2833–2837. doi: 10.1158/0008-5472.CAN-08-4513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Blixt O, Bueti D, Burford B, Allen D, Julien S, Hollingsworth M, Gammerman A, Fentiman I, Taylor-Papadimitriou J, Burchell JM. Autoantibodies to aberrantly glycosylated MUC1 in early stage breast cancer are associated with a better prognosis. Breast Cancer Res. 2011;13:R25. doi: 10.1186/bcr2841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Feng H, Ghazizadeh M, Konishi H, Araki T. Expression of MUC1 and MUC2 mucin gene products in human ovarian carcinomas. Jpn J Clin Oncol. 2002;32:525–529. doi: 10.1093/jjco/hyf111. [DOI] [PubMed] [Google Scholar]
- 31.Li FF, Liu JJ, Liu DW, Lin B, Hao YY, Cong JP, Zhu LC, Gao S, Zhang SL, Iwamori M. Lewis Y regulates signaling molecules of the transforming growth factor β pathway in ovarian carcinoma-derived RMG-I cells. Int J Oncol. 2012;40:1196–1202. doi: 10.3892/ijo.2011.1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rong Y, Jin D, Wu W, Lou W, Wang D, Kuang T, Ni X, Qin X. Induction of protective and therapeutic anti-pancreatic cancer immunity using a reconstructed MUC1 DNA vaccine. BMC Cancer. 2009;9:191. doi: 10.1186/1471-2407-9-191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhao Q, Guo X, Nash GB, Stone PC, Hilkens J, Rhodes JM, Yu LG. Circulating galectin-3 promotes metastasis by modifying MUC1 localization on cancer cell surface. Cancer Res. 2009;69:6799–6806. doi: 10.1158/0008-5472.CAN-09-1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hattrup CL, Gendler SJ. Structure and function of the cell surface (tethered) mucins. Annu Rev Physiol. 2008;70:431–457. doi: 10.1146/annurev.physiol.70.113006.100659. [DOI] [PubMed] [Google Scholar]