Abstract
Background
Weaning from mechanical ventilation requires increased respiratory effort, which can heighten anxiety and later prolong the need for mechanical ventilation.
Objectives
To examine the predictive associations of music intervention, anxiety, sedative exposure, and patients’ characteristics on time to initiation and duration of weaning trials of patients receiving mechanical ventilation.
Methods
A descriptive, correlational design was used for a secondary analysis of data from a randomized trial. Music listening was defined as self-initiated, patient-directed music via headphones. Anxiety was measured daily with a visual analog scale. Sedative exposure was operationalized as a daily sedation intensity score and a sedative dose frequency. Analyses consisted of descriptive statistics, graphing, survival analysis, Cox proportional hazards regression, and linear regression.
Results
Of 307 patients, 52% were women and 86% were white. Mean age was 59.3 (SD, 14.4) years, mean Acute Physiology and Chronic Health Evaluation III score was 62.9 (SD, 21.6), mean duration of ventilatory support was 8 (range, 1–52) days, and mean stay in the intensive care unit was 18 (range, 2–71) days. Music listening, anxiety levels, and sedative exposure did not influence time to initial weaning trial or duration of trials. Clinical factors of illness severity, days of weaning trials, and tracheostomy placement influenced weaning patterns in this sample.
Conclusions
Prospective studies of music intervention and other psychophysiological factors during weaning from mechanical ventilation are needed to better understand factors that promote successful weaning.
More than 800 000 patients require mechanical ventilation each year in the United States,1 and that number is expected to increase significantly as the population ages.2 Mechanical ventilation can cause distressing physical and psychological symptoms.3,4 Weaning can further exacerbate these symptoms by requiring increased respiratory effort.5–9 Up to 40% of the time that patients are receiving ventilatory support is spent being weaned off the ventilator.10 Patients who are not weaned successfully report more fatigue, dyspnea, and less weaning self-efficacy.7,9 Additionally, patients requiring mechanical ventilatory support for more than 3 weeks account for greater than 50% of total intensive care unit (ICU) costs.1 Thus, timely weaning is essential to decrease the personal and economic costs of mechanical ventilation.9
Distressing symptoms associated with mechanical ventilation are commonly managed by sedative and analgesic medications. Although these are necessary to promote comfort, decrease oxygen consumption, facilitate nursing care, and ensure patient safety,4,11 overuse of these medications can cause negative adverse effects, such as increased rates of organ failure; short-term and long-term issues with memory, cognition, and emotional stability; inaccurate neurological assessments; reintubation; and medication withdrawal.12 Moreover, oversedation can have grave consequences for weaning success.11,13,14
Current practice guidelines recommend maintaining light levels of sedation to enable responsiveness and awareness sufficient for the patient to follow simple commands while receiving mechanical ventilation.15 Lighter levels of sedation improve clinical outcomes by decreasing total ventilator time and overall ICU lengths of stay; however, lightening sedation may heighten the physiological stress response15 and intensify psychological stressors.8 Thus, it is important to consider alternative symptom-management strategies that maintain alertness and promote physical and psychological well-being during ventilator weaning. Music intervention is 1 viable nonpharmacological option that can be used adjunctively to effectively manage distress in patients receiving mechanical ventilation.16–21 However, the use of music intervention specifically during ventilator weaning has not been sufficiently studied.22
There is a critical need to consider physiological and psychological factors that prolong weaning and delay extubation, to develop innovative interventions that address modifiable factors and promote successful weaning.22 The purpose of this study was to examine predictive associations of music intervention, anxiety, sedative exposure (eg, intensity and dose frequency), and patients’ characteristics on time to initial weaning trial and duration of weaning trials in critically ill patients receiving mechanical ventilation. Primary aims were to determine if music (aim 1) and anxiety (aim 2) influenced time to initial weaning trial after study enrollment and to determine if music (aim 3) and anxiety (aim 4) influenced the duration of weaning trials during the study period in patients receiving mechanical ventilation.
Methods
Overview of the Parent Study
This secondary data analysis was based on a subset of patients who participated in a randomized controlled clinical trial (NCT00440700) between September 2006 and March 2011 that tested whether listening to self-initiated, patient-directed music (PDM) reduced anxiety and sedative exposure during ventilator support of critically ill patients.17 Patients were recruited from 12 adult ICUs in 5 hospitals in Minneapolis, Minnesota. Patients were randomly assigned to (1) self-initiated PDM, (2) self-initiated application of noise-canceling headphones, or (3) usual care. A board-certified music therapist used a music assessment tool to evaluate the musical preferences of patients randomly assigned to the PDM group. Then, the therapist compiled compact discs of a variety of relaxing instrumental music that met established tempo, instrumental, and rhythm requirements and were tailored to the patients’ preferences. PDM patients received usual ICU nursing care and were prompted to listen to preferred music via noise-canceling headphones twice daily whenever they were feeling anxious or needing quiet time, but at their own discretion regarding duration and frequency. Baseline demographic data were collected at enrollment and data collection was continued for the duration of the patient’s time in the study (up to 30 days) and mechanical ventilatory support, or until the patient withdrew, was extubated, transferred, or died. Additional details related to the parent study are reported elsewhere.17
Secondary Data Analysis Project
Design
A descriptive, correlational study design was used to address the study aims for this secondary data analysis from the referenced parent study.17
Sample
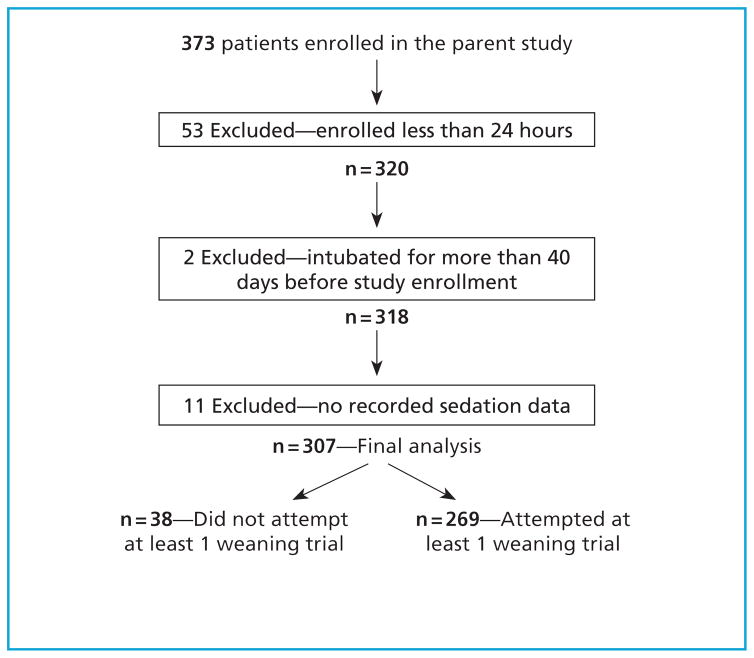
Patients were included in the analysis if they were enrolled in the parent study for at least 24 hours, intubated fewer than 40 days before study enrollment, and if they had recorded sedative-exposure data (Figure 1).
Figure 1.
Flow diagram of study patients.
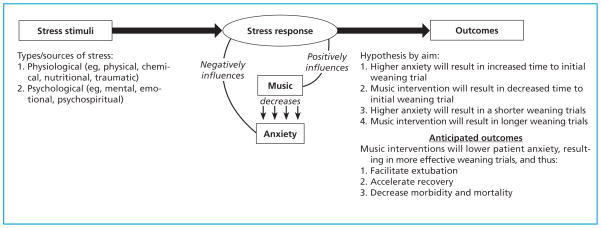
Conceptual Framework
This analysis was guided by a transactional stress-response model (Figure 2). It was hypothesized that patients who listened to music during mechanical ventilation would report lower anxiety levels and have shorter times to initial weaning trial and longer weaning trials.
Figure 2.
Transactional stress-response model.
Demographic and Clinical Variables
Baseline demographic data included age, sex, race, history of mechanical ventilation, and type of artificial airway. Severity of illness was measured by the Acute Physiology, Age, Chronic Health Evaluation (APACHE) III23 score, using medical record data from the first 24 hours of ICU admission. Length of ICU stay was recorded beginning with day of admission and ending with day of discharge from the unit or of death. The number of days in the ICU before study enrollment was recorded beginning with days of admission and ending with the day the patient was enrolled in the study. Length of mechanical ventilatory support was recorded beginning with the day the patient was intubated and ending with the day of extubation, use of tracheostomy dome longer than 24 hours, or death. Ventilator settings, including respiratory rate, mode, tidal volume, pressure support, positive end-expiratory pressure, and fraction of inspired oxygen, were recorded daily.
Anxiety
Anxiety was measured daily using a visual analog scale for anxiety. Patients were asked to rate their current anxiety on a 100-mm vertical line, anchored at the bottom by the statement “not anxious at all” and at the top by the statement “the most anxious I have ever been.”
Sedative Exposure
Sedative exposure was operationalized as a daily sedation intensity score and sedative dose frequency.17,24
Weaning Trials
Weaning trials were recorded for each study day whenever the respiratory therapist or nurse indicated in the electronic medical record that the ventilator was switched to a pressure-support mode or that it was disconnected and a tracheostomy dome was applied instead. In the subset of patients used for this analysis, the most recorded weaning trials for any study day was 5. Although the data set contained the number of weaning trials per day, the exact start and stop times (ie, duration of each weaning trial) were available only for the first weaning trial during the first day of the study period.
Time to Initial Weaning Trial
Time to initial weaning trial was defined as the time, in hours, from study enrollment until the first weaning trial was attempted after study enrollment.
Duration of Weaning Trials
Duration of weaning trials was defined as the length of time, in minutes, from the start of each trial (or trials) to the end of each trial (or trials) for every day of study participation. Not all patients experienced a weaning trial each study day. Patients who experienced a weaning trial at least once daily had weaning trial data recorded, including method of weaning, fraction of inspired oxygen, positive end-expiratory pressure, pressure support, and duration of each weaning trial, and number of weaning trials for that day. Tables 1 and 2 list summaries of the variables and measurements.
Table 1.
Study variables, instruments, and measurement frequencies
| Variable | Instrument or source | Frequency of measurement | |||
|---|---|---|---|---|---|
| ICU admission | Study entry | Daily during study | During each weaning trial | ||
| Demographic data | Electronic medical record | X | |||
| Severity of illness | APACHE III | X | |||
| Group assignment | Computer-generated random numbers list | X | X | ||
| Anxiety | Visual analog scale for anxiety | X | Xa | ||
| Sedative exposure | Sedation intensity score Sedative dose frequency |
Xa | |||
| Length of ICU stay | Electronic medical record | Calculated from admission to transfer, discharge, or death | |||
| Days in ICU before enrollment | Calculated from admission to study enrollment | ||||
| Length of mechanical ventilator support | Electronic medical record | Calculated from intubation to extubation or death | |||
| Ventilator settings | Electronic medical record | X | |||
| Weaning variables | Electronic medical record | X | |||
Abbreviations: APACHE, Acute Physiology and Chronic Health Evaluation; ICU, intensive care unit.
Extracted from the medical record in 4-hour blocks during mechanical ventilation.
Table 2.
Characteristics of study sample
| Variable | Total (N = 307) | Weaned (n = 269) | Not weaned (n = 38) | P |
|---|---|---|---|---|
| Age, mean (SD), y | 59.3 (14.4) | 59.6 (14.4) | 57.3 (14.4) | .36a |
|
| ||||
| Female sex, No. (%) | 161 (52.4) | 140 (52.0) | 21 (55.3) | .71b |
|
| ||||
| Race, No. (%) | .92b | |||
| White | 264 (86.0) | 232 (86.2) | 32 (84.2) | |
| Asian | 2 (0.7) | 2 (0.7) | 0 (0.0) | |
| American Indian | 6 (2.0) | 5 (1.9) | 1 (2.6) | |
| Black | 35 (11.4) | 30 (11.2) | 5 (13.2) | |
|
| ||||
| Group, No. (%) | .91b | |||
| Patient-directed music listening | 104 (33.9) | 92 (34.2) | 12 (31.6) | |
| Headphones | 99 (32.2) | 87 (32.3) | 12 (31.6) | |
| Usual care | 104 (33.9) | 90 (33.5) | 14 (36.8) | |
|
| ||||
| APACHE III score, mean (SD) | 62.9 (21.6) | 63.3 (21.4) | 59.6 (23.0) | .32a |
|
| ||||
| Required mechanical ventilation in past hospitalization, No. (%) | 143 (46.6) | 130 (48.3) | 13 (34.2) | .04b,c |
|
| ||||
| ICU days before study entry, median (range) | 7 (0–40) | 5 (0–40) | 2 (0–32) | .42a |
|
| ||||
| ICU days total, median (range) | 18 (2–71) | 14 (3–71) | 7.5 (2–40) | .05a |
|
| ||||
| Ventilator days before study entry, median (range) | 6 (0–38) | 4 (0–38) | 2 (0–32) | .35a |
|
| ||||
| Ventilator days total, median (range) | 8 (1–52) | 8 (1–53) | 5 (1–40) | .07a |
|
| ||||
| Airway type at enrollment, No. (%) | .12b | |||
| Endotracheal tube/oral | 249 (81.1) | 216 (80.3) | 33 (86.8) | |
| Nasal | 2 (0.7) | 1 (0.4) | 1 (2.6) | |
| Tracheostomy | 56 (18.2) | 52 (19.3) | 4 (10.5) | |
|
| ||||
| Ventilator status, No. (%) | .33b | |||
| Still receiving mechanical ventilation at study end | 123 (40.1) | 107 (39.8) | 16 (42.1) | |
| Discontinued after extubation | 145 (47.2) | 125 (46.5) | 20 (52.6) | |
| Discontinued after tracheostomy dome ≥24 h | 39 (12.7) | 37 (13.8) | 2 (5.3) | |
|
| ||||
| Primary indication for mechanical ventilation, No. (%) | .86b | |||
| Respiratory failure | 169 (55) | 145 (53.9) | 24 (63.2) | |
| Respiratory distress | 79 (25.7) | 71 (26.4) | 8 (21.1) | |
| Chronic obstructive pulmonary disease | 8 (2.6) | 7 (2.6) | 1 (1.0) | |
| Airway protection | 8 (2.6) | 7 (2.6) | 1 (1.0) | |
| Surgery | 7 (2.3) | 7 (2.6) | 0 (0.0) | |
| Other | 36 (11.7) | 32 (11.9) | 4 (10.5) | |
|
| ||||
| Primary medical diagnosis, No. (%) | .57b | |||
| Pulmonary | 182 (59.3) | 162 (60.2) | 20 (52.6) | |
| Cardiovascular | 37 (12.1) | 33 (12.3) | 4 (10.5) | |
| Gastrointestinal | 19 (6.2) | 19 (7.1) | 1 (2.6) | |
| Renal | 3 (1.0) | 3 (1.1) | 0 (0.0) | |
| Oncological | 10 (3.3) | 7 (2.6) | 3 (7.9) | |
| Neurological/neuromuscular | 16 (5.2) | 13 (4.8) | 3 (7.9) | |
| Trauma | 8 (2.6) | 6 (2.2) | 2 (5.3) | |
| Surgery | 3 (1.0) | 3 (1.1) | 0 (0.0) | |
| Sepsis/hypotension | 22 (7.2) | 18 (6.7) | 4 (10.5) | |
| Other | 6 (2.0) | 5 (1.9) | 1 (2.6) | |
|
| ||||
| Types of comorbid conditions | ||||
| Cardiovascular | 223 (72.6) | 199 (74.0) | 24 (63.2) | .23b |
| Pulmonary | 210 (68.4) | 186 (69.1) | 24 (63.2) | .58b |
| Cancer | 47 (15.3) | 40 (14.9) | 7 (18.4) | .53b |
| Renal | 76 (24.8) | 68 (25.3) | 8 (21.1) | .62b |
| Obesity | 46 (15.0) | 41 (15.2) | 5 (13.2) | .82b |
| Diabetes | 91 (29.6) | 83 (30.9) | 8 (21.1) | .24b |
| Sepsis | 36 (11.7) | 31 (11.5) | 5 (13.2) | .73b |
| Neurological | 89 (29.0) | 81 (30.1) | 8 (21.1) | .28b |
| Psychological | 69 (2.5) | 60 (22.3) | 9 (23.7) | .79b |
|
| ||||
| VAS-A score at study entry,d mean (SD) | 50.2 (31.1) | 50.6 (30.5) | 47.7 (35.2) | .60a |
|
| ||||
| Sedation intensity score at study entry, mean (SD) | 4.2 (2.6) | 4.1 (2.6) | 4.7 (2.5) | .73a |
|
| ||||
| Sedative dose frequency at study entry, mean (SD) | 6.4 (4.0) | 6.4 (4.0) | 6.2 (4.1) | .17a |
|
| ||||
| Patient alive at discharge, No. (%) | 279 (90.9) | 249 (92.6) | 30 (78.9) | .01b,c |
Abbreviations: APACHE, Acute Physiology and Chronic Health Evaluation; ICU, intensive care unit; VAS-A, visual analog scale for anxiety.
Independent samples t test.
χ2 test.
Statistically significant at P < .05.
VAS-A score at study entry was available for only 264 of 307 patients (86.0%).
Ethical Considerations
The parent study protocol was approved by the institutional review boards at the University of Minnesota and all participating sites. Additionally, institutional review board approval was obtained from the University of Minnesota for this secondary data analysis.
Statistical Analyses
Data analyses were accomplished using SPSS version 22 (IBM SPSS) and SAS version 9.3 (SAS Institute). All data were analyzed descriptively via univariate statistics using independent-samples t tests and χ2 tests. Results were considered significant a priori at P < .05.
Analysis by Aims
To address the aims of this project, the patients in the PDM and noise-canceling headphones groups were analyzed as separate, independent groups. For the analyses, the usual-care group was considered the reference group. The influence of music (assignment to PDM) and the influence of anxiety on time to initial weaning trial after study enrollment (aims 1 and 2) were analyzed together via a Cox proportional hazards regression using group assignment as a fixed covariate. First, an exploratory survival analysis was graphed to compare the 3 groups and the general trends for time to the initial weaning trial after study enrollment. Daily anxiety ratings were treated as a time-dependent covariate. Other covariates, static and time dependent, were screened individually in the proportional hazards regression and introduced into the model if they were significant at P < .10. Because of the almost collinear relationship between sedative dose frequency and sedation intensity score, 2 models were created.
The influence of music (assignment to the PDM) on duration of weaning trials during the study period and the influence of anxiety on duration of weaning trials during the study period (aims 3 and 4) were analyzed together using linear regression with duration of weaning trial as the dependent variable in the context of mixed models. Mixed models were chosen because there could be multiple trials for 1 patient and the related data had to be accounted for in the model. Covariates were screened individually in the linear regression and introduced into the model if they were significant at P < .10. Because of the almost collinear relationship between sedative dose frequency and sedation intensity score, 2 models were created.
Results
Demographic and Clinical Characteristics
Table 2 summarizes characteristics of the study sample (N = 307), and the PDM (n = 104), noise-canceling headphones (n = 99), and usual-care (n = 104) groups. The mean illness severity score (measured by APACHE III) was 62.9 (SD, 21.6), reflecting a broad range of illness severity upon ICU admission. The majority of patients were orally intubated (n = 249; 81.1%) for respiratory failure (n = 169; 55.0%) or respiratory distress (n = 79; 25.7%). Anxiety, sedation intensity score, and sedative dose frequency did not differ significantly at study entry among groups. Of the 269 patients who had at least 1 recorded weaning trial, 130 (48.3%) had required mechanical ventilation in a previous hospitalization, whereas only 13 of the 38 patients (34.2%) who did not have at least 1 recorded weaning trial during the study period required mechanical ventilation in a previous hospitalization (P = .04). Patient status at discharge (dead vs alive) was significantly different between groups: 93% of patients who had at least 1 recorded weaning trial during the study period were alive at discharge compared with 79% of patients who were not subject to a weaning trial (P = .01).
Influence of Music and Anxiety on Time to Initial Weaning Trial
Models 1 and 2 estimated the time to initial weaning trial after study enrollment by group assignment and anxiety, controlling for measures of sedative exposure in addition to other covariates that may affect time to initial weaning, such as total days in ICU, APACHE III score, and prior history of mechanical ventilation. Both models indicated that group assignment and anxiety were not significant predictors of time to initial weaning trial (Table 3). When sedative dose frequency and sedation intensity score were controlled for separately, patients with higher initial illness severity scores had a shorter time to initial weaning trial after study enrollment.
Table 3.
Influence of group assignment and anxiety on time to initial weaning trial after study enrollment, controlling for sedative dose frequency, sedation intensity score, and other covariates
| Variable | Model 1 controlling for sedative dose frequency | Model 2 controlling for sedation intensity score | ||
|---|---|---|---|---|
|
|
|
|||
| Hazard ratio (95% CI) | P | Hazard ratio (95% CI) | P | |
| Patient-directed musica | 1.1 (0.73–1.6) | .72 | 1.06 (0.73–1.6) | .76 |
|
| ||||
| Noise-canceling headphonesa | 0.98 (0.66–1.5) | .93 | 0.98 (0.66–1.5) | .92 |
|
| ||||
| Score on visual analog scale | 1.004 (0.999–1.007) | .16 | 1.004 (0.998–1.009) | .18 |
|
| ||||
| Total days in ICU before enrollment | 0.995 (0.981–1.018) | .46 | 0.996 (0.983–1.018) | .59 |
|
| ||||
| APACHE III score | 1.01 (1.003–1.018) | .004b | 1.01 (1.003–1.018) | .005b |
|
| ||||
| History of ventilation during prior hospitalization | 1.3 (0.95–1.8) | .10 | 1.3 (0.94–1.8) | .11 |
|
| ||||
| Sedative dose frequency | 0.97 (0.93–1.007) | .11 | ||
|
| ||||
| Sedation intensity score | 0.98 (0.92–1.03) | .42 | ||
Abbreviations: APACHE, Acute Physiology and Chronic Health Evaluation; ICU, intensive care unit.
Reference is usual care.
Statistically significant at P < .05.
Influence of Music and Anxiety on Duration of Weaning Trials
Models 3 and 4 estimated the influence of group assignment and anxiety on duration of weaning trials during the study period, controlling for measures of sedative exposure in addition to other covariates, including day, weaning trial number, age, days receiving mechanical ventilation, days in ICU, fraction of inspired oxygen, and presence of a tracheostomy. Both models indicated that group assignment and anxiety were not significant predictors of duration of weaning trials during the study period (Table 4). Model 3 showed that for each day after study enrollment, duration of weaning trials increased by 8.4 minutes (P < .001), and if a patient was breathing through a tracheostomy tube (compared with an endotracheal tube) on the day of the weaning trial, duration of weaning trials for that day increased by 53.6 minutes (P = .04). Model 4 showed that for each day since study enrollment, duration of weaning trials increased by 8.6 minutes (P < .001). If a patient had a tracheostomy on the day of the weaning trial, duration of weaning trials for that day increased by 54.6 minutes (P = .03).
Table 4.
Influence of group assignment and anxiety on duration of weaning trials during the study period, controlling for sedative dose frequency, sedation intensity score, and other covariates
| Variable | Model 3 controlling for sedative dose frequency | Model 4 controlling for sedation intensity score | ||
|---|---|---|---|---|
|
|
|
|||
| β (SE) | P | β (SE) | P | |
| Patient-directed musica | −44.6 (30.9) | .15 | −46.4 (30.9) | .14 |
|
| ||||
| Noise-canceling headphonesa | −48.7 (32.9) | .14 | −48.9 (32.9) | .14 |
|
| ||||
| Study day | 8.4 (2.3) | <.001b | 8.6 (2.2) | <.001b |
|
| ||||
| Weaning trial number | −10.7 (10.8) | .32 | −10.9 (10.8) | .31 |
|
| ||||
| VAS-A score | −0.09 (0.30) | .77 | −0.09 (0.30) | .77 |
|
| ||||
| Age | −0.21 (0.94) | .82 | −0.17 (0.94) | .85 |
|
| ||||
| Days of mechanical ventilation before enrollment | 4.1 (3.0) | .17 | 4.2 (3.0) | .16 |
|
| ||||
| Days in ICU before enrollment | −1.4 (3.1) | .65 | −1.4 (3.0) | .65 |
|
| ||||
| Fraction of inspired oxygen | 1.8 (1.0) | .08 | 1.7 (1.0) | .08 |
|
| ||||
| Tracheostomy | 53.6 (25.7) | .04b | 54.6 (25.7) | .03b |
|
| ||||
| Sedative dose frequency | −1.8 (2.8) | .52 | ||
|
| ||||
| Sedation intensity score | −1.7 (3.9) | .66 | ||
Abbreviations: ICU, intensive care unit; VAS-A, visual analog scale for anxiety.
Reference is usual care.
Statistically significant at P < .05.
Covariates in all models showed various levels of significant correlations, from weak to moderately strong (Tables 5 and 6).
Table 5.
Correlations among covariates of interest (models 1 and 2)
| Variable | VAS-A score | Sedative dose frequency | Sedation intensity score | Days in ICU before enrollment | APACHE III score | History of ventilation during prior hospitalization |
|---|---|---|---|---|---|---|
| VAS-A score | — | 0.09a | 0.09a | 0.01 | 0.10a | 0.05 |
| Sedative dose frequency | 0.09a | — | 0.83b | −0.22b | −0.04 | −0.08a |
| Sedation intensity score | 0.09a | 0.83b | — | −0.19b | −0.06 | −0.14b |
| Days in ICU before enrollment | 0.01 | −0.22b | −0.19b | — | 0.05 | −0.03 |
| APACHE III score | 0.10a | −0.04 | −0.06 | 0.05 | — | 0.06 |
| History of ventilation during prior hospitalization | 0.05 | −0.08a | −0.14b | −0.03 | 0.06 | — |
Abbreviations: APACHE, Acute Physiology and Chronic Health Evaluation; ICU, intensive care unit; VAS-A, visual analog scale for anxiety.
P < .05.
P < .01.
Table 6.
Correlations among covariates of interest (models 3 and 4)
| Variable | Study day | Weaning trial | VAS-A score | Age | Ventilator days before enrollment | ICU days before enrollment | Sedative dose frequency | Sedation intensity score | Fraction of inspired oxygen | Tracheostomy |
|---|---|---|---|---|---|---|---|---|---|---|
| Study day | — | 0.02 | −0.03 | −0.04 | −0.06a | −0.07a | −0.18a | −0.17a | −0.11a | 0.45a |
|
| ||||||||||
| Weaning trial | 0.02 | — | −0.02 | 0.04 | 0.06b | 0.09a | −0.06b | −0.10a | −0.12a | −0.10a |
|
| ||||||||||
| VAS-A score | −0.03 | −0.02 | — | 0.13a | −0.04 | −0.05 | 0.08b | 0.08b | −0.01 | −0.04 |
|
| ||||||||||
| Age | −0.04 | 0.04 | −0.13a | — | −0.19a | −0.13a | −0.10a | −0.11a | −0.06a | −0.16a |
|
| ||||||||||
| Ventilator days before enrollment | −0.06a | 0.06b | −0.04 | −0.19a | — | 0.88a | −0.15a | −0.09a | −0.10a | 0.38a |
| ICU days before enrollment | −0.07a | 0.09a | −0.046 | −0.13a | 0.88a | — | −0.128a | −0.04 | −0.15a | 0.41a |
| Sedative dose frequency | −0.18a | −0.06b | 0.08b | 0.10a | −0.15a | −0.13a | — | 0.82a | 0.07b | −0.30a |
| Sedation intensity score | −0.17a | −0.10a | 0.08b | −0.11a | −0.09a | −0.04 | 0.82a | — | 0.01 | −0.25a |
| Fraction of inspired oxygen | −0.11a | −0.12a | −0.01 | −0.06a | −0.10a | −0.15a | 0.07b | 0.01 | — | −0.12a |
| Tracheostomy | 0.45a | 0.10a | −0.04 | −0.16a | 0.38a | −0.41a | −0.30a | −0.25a | −0.12a | — |
Abbreviations: ICU, intensive care unit; VAS-A, visual analog scale for anxiety.
P < .01.
P < .05.
Discussion
The purpose of this secondary data analysis was to examine predictive associations of music listening, anxiety, sedative exposure (eg, intensity and dose frequency), and patients’ characteristics with time to initial weaning trial and duration of weaning trials in a sample of patients receiving mechanical ventilation. Results indicate that music and anxiety were not significant predictors of time to initial weaning trial after enrollment, nor were they significant predictors of duration of weaning trials during the study period. However, important information regarding various factors that may affect weaning success were gained from this analysis.
To our knowledge, this is the first investigation of data from a large randomized clinical trial of acutely ill patients in the ICU to examine music-listening interventions and anxiety on weaning from mechanical ventilation. Previous literature has reported the positive impact of music intervention during mechanical ventilation,22,25 but only 1 study26 was identified that examined music intervention as an adjunctive treatment specifically during weaning from mechanical ventilation in the acute care setting. Hunter and colleagues26 relied on heart rate and blood pressure measurements, as well as staff assessment, to evaluate patients’ anxiety after the music intervention. Although the study results were positive, these physiological measurement techniques and proxy assessments for anxiety are dated; future research should consider more precise biological measures in conjunction with direct reports from patients to evaluate anxiety to enhance our understanding of the exact mechanisms in which music affects the stress response.
Our findings document that patients with higher illness severity scores were more likely to experience a shorter time to first weaning trial after study enrollment, which is the opposite of what would be clinically expected. This result is most likely due to the way illness severity was calculated in the parent study.17 APACHE III scores were measured only once, using data from the day of ICU admission. Thus, we could not account for physiological changes over time.27 Also, because of the self-directed nature of the music intervention, eligibility for the parent study required more medically stable critically ill patients who were awake and alert enough to participate in the protocol.
Previous research has indicated that if a patient is expected to require prolonged mechanical ventilation, a tracheostomy should be considered early.14 However, the definition of prolonged mechanical ventilation continues to evolve, and the most ideal timing for tracheostomy placement remains unclear.28 Tracheostomy placement may reduce the work of breathing, facilitate weaning, and lessen the need for sedation and analgesia.28 Our results demonstrated that patients who had a tracheostomy tolerated significantly longer weaning trials, which may suggest that early tracheostomy placement may benefit individuals who are likely to require prolonged ventilator support.
Given clinical similarities of illness severity at study enrollment, it is noteworthy that half of the patients who had at least 1 weaning trial during the protocol had experienced mechanical ventilation during a previous hospitalization, compared with less than a third of patients who never attempted a weaning trial. Furthermore, patients who had previously received mechanical ventilation during a prior hospitalization underwent their first weaning trial sooner after enrollment than did patients who had never received mechanical ventilation. These findings suggest that experience or familiarity with the ventilator may positively influence weaning patterns. The weaning process elicits intense emotions of fear and anxiety because of a perceived lack of familiarity with and understanding of the weaning process.4,29,30 These emotions may be lessened by frequent education about the weaning process.
Limitations
Several inherent limitations are well known to be associated with secondary data analyses.31,32 In addition to these limitations, the primary aims of this secondary analysis were not directly aligned with the specific aims of the parent study, and the data collection measures used could not be amended. Weaning trials were recorded for the parent study beginning on the first day patients were enrolled in the study. It is unknown how many patients in the analysis were already undergoing weaning trials, and to what degree, before study enrollment. Duration of weaning trials was provided, but the exact start and stop times of each weaning trial after the initial weaning trial on the first day of the study were not available in the electronic data set, making it difficult to fully evaluate weaning patterns. The variability in PDM use, timing, and frequency could have affected the ability to capture the group effect on variables of interest specified in the study aims. Only 1 anxiety assessment was obtained daily and, owing to a variety of circumstances, some daily assessments were not completed for reasons such as the patient being “too sleepy” or “too sedated.” In addition, patients were recruited from 12 ICUs, all of which used a variety of weaning practices and protocols as well as sedative administration techniques. It is unknown to what degree this variability in ventilator management and clinical practice influenced our results.
Implications for Practice
Unfortunately, distressing symptoms will continue to be an inherent part of mechanical ventilation and ICU care; therefore, it is critical that innovative nonpharmacological adjunctive treatments for symptom management are investigated and subsequently integrated into ICU nursing practice to provide high-quality care for patients receiving mechanical ventilation. Music intervention is a practical, cost-effective option that can be easily implemented and promoted at the bedside by nursing staff during ventilator weaning.22,25
Directions for Future Research
Future prospective primary studies are warranted and should consider pairing the music intervention specifically with each weaning trial, which may more accurately capture the effect of music intervention on weaning trials, as well as including physiological measures of anxiety such as heart rate, blood pressure, and respiratory rate before, during, and after weaning trials. It would also be worthwhile to analyze pertinent laboratory values or stress biomarkers to evaluate more accurately the influence of stress and anxiety on ventilator weaning.
Conclusions
Neither music listening nor anxiety levels shortened the time to initial weaning trial or influenced the duration of weaning trials in this subset of patients. However, previous publications have indicated that music may be a valuable nonpharmacological adjunctive intervention to reduce burdensome symptoms that may prolong ventilator support and delay weaning. Prospective investigations of the influence of patients’ clinical characteristics and music interventions on psychological distress are warranted to advance symptom-management science and improve outcomes for patients receiving mechanical ventilation.
Acknowledgments
FINANCIAL DISCLOSURES This research was supported by the National Institute of Nursing Research of the National Institutes of Health (Award no. F31-NR014591).
This work was performed at the University of Minnesota. Research sites were the University of Minnesota Medical Center, Abbott-Northwestern Hospital, North Memorial Medical Center, United Hospital, Regions Hospital, and Hennepin County Medical Center.
Footnotes
eLetters
Now that you’ve read the article, create or contribute to an online discussion on this topic. Visit www.ajcconline.org and click “Submit a response” in either the full-text or PDF view of the article.
SEE ALSO
For more about innovative patient care, visit the Critical Care Nurse website, www.ccnonline.org, and read the article by Supnet et al, “Music as Medicine: The Therapeutic Potential of Music for Acute Stroke Patients” (April 2016).
To purchase electronic or print reprints, contact American Association of Critical-Care Nurses, 101 Columbia, Aliso Viejo, CA 92656. Phone, (800) 899-1712 or (949) 362-2050 (ext 532); fax, (949) 362-2049; reprints@aacn.org.
Contributor Information
Breanna Hetland, Postdoctoral fellow, Frances Payne Bolton School of Nursing, Case Western Reserve University, Cleveland, Ohio.
Ruth Lindquist, Professor, School of Nursing, University of Minnesota, Minneapolis, Minnesota.
Craig R. Weinert, Associate professor, School of Medicine, University of Minnesota.
Cynthia Peden-McAlpine, Associate professor, School of Nursing, University of Minnesota, Minneapolis, Minnesota.
Kay Savik, Senior statistician, School of Nursing, University of Minnesota, Minneapolis, Minnesota.
Linda Chlan, Associate dean for nursing research, Mayo Clinic, Rochester, Minnesota.
References
- 1.Wunsch H, Linde-Zwirble WT, Angus DC, Harman ME, Milbrandt EB, Kahn JM. The epidemiology of mechanical ventilation use in the United States. Crit Care Med. 2010;38(10):1947–1953. doi: 10.1097/CCM.0b013e3181ef4460. [DOI] [PubMed] [Google Scholar]
- 2.Zilberberg MD, Shorr AF. Prolonged acute mechanical ventilation and hospital bed utilization in 2020 in the United States: implications for budgets, plant and personnel planning. BMC Health Serv Res. 2008;8(242):1–10. doi: 10.1186/1472-6963-8-242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Puntillo KA, Arai S, Cohen NH, et al. Symptoms experienced by intensive care unit patients at a high risk of dying. Crit Care Med. 2010;38(11):2155–2160. doi: 10.1097/CCM.0b013e3181f267ee. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rotondi AJ, Chelluri L, Sirio C, et al. Patients’ recollections of stressful experiences while receiving prolonged mechanical ventilation in an intensive care unit. Crit Care Med. 2002;30(4):746–752. doi: 10.1097/00003246-200204000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Neligan P. [Accessed May 30, 2015];Critical care medicine tutorials. 2006 www.ccmtutorials.com.
- 6.Nickson C. [Accessed February 5, 2017];Weaning from mechanical ventilation. 2015 http://lifeinthefastlane.com/ccc/weaning-from-mechanicalventilation/
- 7.Blackwood B. The art and science of predicting patient readiness for weaning from mechanical ventilation. Int J Nurs Stud. 2000;37(2):145–151. doi: 10.1016/s0020-7489(99)00062-0. [DOI] [PubMed] [Google Scholar]
- 8.Schou L, Egerod I. A qualitative study into the lived experience of post-CABG patients during mechanical ventilator weaning. Intensive Crit Care Nurs. 2008;24(3):171–179. doi: 10.1016/j.iccn.2007.12.004. [DOI] [PubMed] [Google Scholar]
- 9.Twibell R, Siela D, Mahmoodi M. Subjective perceptions and physiological variables during weaning from mechanical ventilation. Am J Crit Care. 2003;12(2):101–112. [PubMed] [Google Scholar]
- 10.Eskandar N, Apostolakos MJ. Weaning from mechanical ventilation. Crit Care Clin. 2007;23(2):263–274. doi: 10.1016/j.ccc.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 11.Girard TD, Kress JP, Fuchs BD, et al. Efficacy and safety of a paired sedation and ventilator weaning protocol for mechanically ventilated patients in intensive care (Awakening and Breathing Controlled Trial): a randomized controlled trial. Lancet. 2008;371(9607):126–134. doi: 10.1016/S0140-6736(08)60105-1. [DOI] [PubMed] [Google Scholar]
- 12.Brush DR, Kress JP. Sedation and analgesia for the mechanically ventilated patient. Clin Chest Med. 2009;30(1):131–141. doi: 10.1016/j.ccm.2008.09.001. [DOI] [PubMed] [Google Scholar]
- 13.Conti G, Mantz J, Longrois D, Tonner P. Sedation and weaning from mechanical ventilation: time for ‘best practice’ to catch up with new realities. Multidiscip Respir Med. 2014;9(45):1–5. doi: 10.1186/2049-6958-9-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Luetz A, Goldmann A, Weber-Carstens S, Spies C. Weaning from mechanical ventilation and sedation. Curr Opin Anaesthesiol. 2012;25(2):164–169. doi: 10.1097/ACO.0b013e32834f8ce7. [DOI] [PubMed] [Google Scholar]
- 15.Barr J, Fraser GL, Puntillo K, et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med. 2013;41(1):263–306. doi: 10.1097/CCM.0b013e3182783b72. [DOI] [PubMed] [Google Scholar]
- 16.Chlan L. Effectiveness of a music therapy intervention on relaxation and anxiety for patients receiving ventilatory assistance. Heart Lung. 1998;27(3):169–176. doi: 10.1016/s0147-9563(98)90004-8. [DOI] [PubMed] [Google Scholar]
- 17.Chlan LL, Weinert CR, Heiderscheit A, Tracy MF, Skaar DJ, Guttormson JL. Effects of patient-directed music intervention on anxiety and sedative exposure in critically ill patients receiving mechanical ventilator support: a randomized clinical trial. JAMA. 2013;309(22):2335–2344. doi: 10.1001/jama.2013.5670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dijkstra BM, Gamel C, van der Bijl JJ, Bots ML, Kesecioglu J. The effects of music on physiological responses and sedation scores in sedated, mechanically ventilated patients. J Clin Nurs. 2010;19(7–8):1030–1039. doi: 10.1111/j.1365-2702.2009.02968.x. [DOI] [PubMed] [Google Scholar]
- 19.Korhan EA, Khorshid L, Uyar M. The effect of music therapy on physiological signs of anxiety in patients receiving mechanical ventilator support. J Clin Nurs. 2011;20(7–8):1026–1034. doi: 10.1111/j.1365-2702.2010.03434.x. [DOI] [PubMed] [Google Scholar]
- 20.Lee OKA, Chung YFL, Chan MF, Chan WM. Music and its effect on the physiological responses and anxiety levels of patients receiving mechanical ventilation: a pilot study. J Clin Res. 2005;14(5):609–620. doi: 10.1111/j.1365-2702.2004.01103.x. [DOI] [PubMed] [Google Scholar]
- 21.Wong HLC, Lopez-Nahas V, Molassiotis A. Effects of music therapy on anxiety in ventilator-dependent patients. Heart Lung. 2001;30(5):376–386. doi: 10.1067/mhl.2001.118302. [DOI] [PubMed] [Google Scholar]
- 22.Hetland B, Lindquist R, Chlan L. The influence of music during mechanical ventilation and weaning from mechanical ventilation: a review. Heart Lung. 2015;44(5):416–425. doi: 10.1016/j.hrtlng.2015.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Knaus WW, Wagner DP, Draper EA, et al. The APACHE III prognostic system. Risk prediction of hospital mortality for critically ill hospitalized adults. Chest. 1991;100(6):1619–1636. doi: 10.1378/chest.100.6.1619. [DOI] [PubMed] [Google Scholar]
- 24.Weinert CR, Calvin AD. Epidemiology of sedation and sedation adequacy for mechanically ventilated patients in a medical and surgical intensive care unit. Crit Care Med. 2007;35(2):393–401. doi: 10.1097/01.CCM.0000254339.18639.1D. [DOI] [PubMed] [Google Scholar]
- 25.Bradt J, Dileao C, Grocke D. Music interventions for mechanically ventilated patients. Cochrane Database Syst Rev. 2010;12:CD006902. doi: 10.1002/14651858.CD006902.pub2. [DOI] [PubMed] [Google Scholar]
- 26.Hunter BC, Olivia R, Sahler OJZ, Gaisser D, Salipante DM, Arezina CH. Music therapy as an adjunctive treatment in the management of stress for patients being weaned from mechanical ventilation. J Music Ther. 2010;47(3):191–219. doi: 10.1093/jmt/47.3.198. [DOI] [PubMed] [Google Scholar]
- 27.Knaus WW, Wagner DP, Draper EA, et al. The APACHE III Prognostic system. Risk prediction of hospital mortality for critically ill hospitalized adults. Chest. 1991;100(6):1619–1636. doi: 10.1378/chest.100.6.1619. [DOI] [PubMed] [Google Scholar]
- 28.Durbin CG. Tracheostomy: why, when, and how? Resp Care. 2010;55(8):1056–1068. [PubMed] [Google Scholar]
- 29.Moody LE, Lowry L, Yarandi H, Voss A. Psychophysiologic predictors of weaning from mechanical ventilation in chronic bronchitis and emphysema. Clin Nurs Res. 1997;6(4):311–330. doi: 10.1177/105477389700600402. discussion 330–313. [DOI] [PubMed] [Google Scholar]
- 30.Wunderlich RJ, Perry A, Lavin MA, Katz B. Patients’ perceptions of uncertainty and stress during weaning from mechanical ventilation. Dimens Crit Care Nurs. 1999;18(1):8–12. [PubMed] [Google Scholar]
- 31.Boslaugh S. [Accessed February 5, 2017];An introduction to secondary data analysis. http://assets.cambridge.org/97805218/70016/excerpt/9780521870016_excerpt.pdf.
- 32.Smith AK, Ayanian JZ, Covinsky KE, et al. Conducting high-value secondary data analysis: an introductory guide and resources. J Gen Intern Med. 2011;26(8):920–929. doi: 10.1007/s11606-010-1621-5. [DOI] [PMC free article] [PubMed] [Google Scholar]