Abstract
Objective
Adolescents with ADHD are at increased risk for alcohol and marijuana use. This study’s objective is to describe adolescents’ ADHD-specific reasons for marijuana use, knowledge of ADHD-specific alcohol risks, and reported subspecialty provider messaging/education regarding alcohol use among adolescents with ADHD.
Methods
Youths with ADHD ages 12–18 years completed a survey about alcohol and marijuana use, ADHD-specific reasons for marijuana use, knowledge of ADHD-specific alcohol risks, and reported provider messaging/education regarding alcohol use. We assessed knowledge towards substance use using descriptive statistics. We used chi-square and t-tests to determine if knowledge or provider messaging/education differed by sociodemographic characteristics.
Results
Of the 96 participants, 61.5% were male, average age was 15.7 years; 31.3% reported past year alcohol use and 20.8% reported past year marijuana use. The majority (65.2%) said “no/don’t know” to both “Can alcohol make ADHD symptoms worse?” and “Can alcohol interfere or get in the way of the medications you take?”. Older participants were more likely to correctly answer the medication question “yes”. Despite most (74%) participants reporting that their provider asked about alcohol use, few youth reported that their providers gave specific messages/education that alcohol could make ADHD symptoms worse (9.4%) or interfere with ADHD medications (14.6%); older participants and past-year alcohol users were more likely to have received these alcohol specific messages.
Conclusion
Many youth with ADHD are unaware of the risks of alcohol use in relation to ADHD and providers are not consistently discussing these risks in the context of clinical ADHD care.
Introduction
Attention-Deficit/Hyperactivity Disorder (ADHD) impacts 8% (approximately 4 million) of school aged children1 in the United States and often persists into adulthood.2 Youth with ADHD initiate alcohol and other substance use earlier,3 and are more vulnerable to developing substance use disorders (SUDs) once exposed.4, 5 Early onset SUD increases the likelihood of academic failure, suicidal behavior, and incarceration.6, 7 The use of alcohol, marijuana, and other illicit substances by youth with ADHD may contribute to and accelerate negative psychiatric and psychosocial consequences. Alcohol use is also associated with treatment nonadherence in youth with chronic medical conditions.8 Considering these numerous risks, substance use screening is particularly important for youth with ADHD. Screening and subsequent counseling about ADHD-specific substance use risks could help ameliorate the risk of negative outcomes in ADHD.
Stimulant medications are the first-line medication treatment recommended for ADHD, and alpha2 agonist medications and atomoxetine also have U.S. Food and Drug Administration approval as treatment.9 All of these medications have risks when used in combination with marijuana or alcohol. Marijuana use is associated with loss of concentration and challenges with short term memory,10 thus it may counter the positive benefits of a medication used to treat ADHD symptoms. The combination of marijuana and stimulant medication is associated with increases in peak heart rate and subjective effects, and slower reaction times, compared to use of either substance alone.11 Alcohol may enhance the adverse/toxic effects of stimulants,12 increase risk of central nervous system depression in combination with alpha2 agonists, and could result in temporary liver impairment which would contraindicate the use of atomoxetine.13 Given these risks, adolescents with ADHD should be informed about the possible dangerous outcomes of using ADHD medications in combination with alcohol, marijuana, and/or illicit drugs.
However, to our knowledge, there are no published studies describing either ADHD youths’ knowledge about dangers of substance use or substance use messages/education used by their physicians. As such, we sought to describe adolescents’ ADHD-specific reasons for marijuana use and knowledge of ADHD-specific alcohol risks, as well as youth-reported screening and messaging/education regarding alcohol use by their subspecialty providers.
Methods
Study Design and Sample
This was a cross-sectional study in which we recruited from an outpatient developmental medicine subspecialty clinic affiliated with a large pediatric teaching hospital in the Northeast United States a convenience sample of 96 English-speaking youth, ages 12–18 years who had been diagnosed with ADHD for at least one year. Patients who were medically or emotionally unstable on the day of the clinic visit were excluded. We obtained a certificate of confidentiality for this study and assented youth with a waiver of parental consent under the approval of our hospital’s Institutional Review Board.
In total, 99 youth enrolled in this study of 137 invited (response rate 72.3%). Of these 99, 2 were excluded because of active mental health issues on the day of the visit and one subject was excluded due to missing responses for the outcome variables; thus the final analytic sample consisted of 96 participants.
Assessment
In the waiting room, assented youth completed a self-administered survey about: 1) alcohol and marijuana use behaviors (up to 11 items, sample, “In the past year, on how many days have you used marijuana?”), 2) ADHD-specific reasons for marijuana use (2 items asked to participants who had reported marijuana use, “When you used marijuana in the past year, how often did you use it because you thought it would make your ADHD symptoms better or help with medication side effects?” and “When you used marijuana in the past year, how often did you choose it instead of alcohol because you thought alcohol was worse for your ADHD?”), 3) knowledge of ADHD-specific alcohol risks (2 items, “Can alcohol make ADHD symptoms worse?” and “Can alcohol interfere with or get in the way of the medications you take?”; both with answer choices of “yes”, “no”, or “don’t know” which, given cell size numbers, were dichotomized to yes versus no/don’t know for this study), 4) reported provider screening and messaging/education regarding alcohol use (5 items, “In the past year, did your doctor or a member of your health care team ask you if you drink alcohol?”), and 5) sociodemographic and health information (including: gender, age, grade, race/ethnicity, and mental health). Surveys were completed on a tablet computer with a polarizing screen for privacy and an optional audio recording of the assessment. The assessment was 57 to 281 questions in length, contingent on responses to programmed skip logic.
Past year alcohol and marijuana use were dichotomized (any versus none). Responses to questions about knowledge of risks associated with alcohol use were dichotomized as “yes” versus “no” and “don’t know.” To assess mental health status, we used the validated 5-question scale from the Mental Health Inventory (MHI-5) of the Short Form-36 (SF-36);14 responses were transformed to a 100-point scale for analysis consistent with published reports.15 High scores indicated better mental health, with values < 40 considered clinically relevant.
Analytic Approach
All analyses were performed using SAS 9.3. We calculated prevalence of alcohol and marijuana use behaviors and attitudes towards marijuana use among the whole sample and assessed differences in sociodemographics by substance use and knowledge using t-tests and X2 analyses. We calculated the percentage of participants who reported that their healthcare provider had asked if they drink alcohol and the percentage of participants who reported that their healthcare provider discussed specific messages about alcohol use. T-tests and X2 analyses were used to assess differences in receipt of specific messages from providers by age, gender, race/ethnicity, past year drinking status, and medication status.
Results
Demographics and Reported Substance Use Patterns
The mean age was 15.7 years (SD=1.7), 61.5% were male, and race/ethnicity was predominantly white (78.1%). The majority of participants (N=90) achieved a mental health score above the clinically significant range, indicating overall good mental health functioning (range 24.0–100.0; score < 40 indicates concern). A total of 81 participants (84.4%) were taking medication for their ADHD with 73 taking stimulant medication (76.0%), 15 taking alpha2 agonist medications (15.6%) and four taking atomoxetine (4.2%).
Past-year alcohol use was reported by 31.3% of the sample, and past-year binge drinking was reported by 16.7% of past-year alcohol users. Average age at first alcohol use was 14.9 years (SD=2.1). Past-year marijuana use was reported by 20.8% of the sample. Average age at first marijuana use was 14.7 years (SD=1.2). Of the 20 participants who reported past-year marijuana use, the majority (85%) also reported past-year alcohol use. Respondents who reported past year alcohol and marijuana use were older on average than non-users (16.7 years vs. 15.3 years, p<0.0001; 16.7 years vs. 15.5 years, p=0.0002; respectively). Gender, race, and mental health score were not associated with substance use patterns (Table 1).
Table 1.
Sample Sociodemographic Characteristics by Substance Use Status
| Sociodemographic characteristic | Total Sample (N=96) |
Past Year Alcohol Use
|
Past Year Marijuana Use
|
||||
|---|---|---|---|---|---|---|---|
| Any (N=30) |
None (N=66) |
p-valueb | Any (N=20) |
None (N=76) |
p-valueb | ||
|
| |||||||
|
Age in years, Mean (SD) |
15.7 (1.7) | 16.7 (1.2) | 15.3 (1.7) | <0.001c | 16.7 (1.0) | 15.5 (1.8) | <0.001c |
|
| |||||||
| Gendera: | |||||||
| Male | 59 (61.5) | 19 (63.3) | 40 (60.6) | 0.799 | 13 (65.0) | 46 (60.5) | 0.715 |
| Female | 37 (38.5) | 11 (36.7) | 26 (39.4) | 7 (35.0) | 30 (39.5) | ||
|
| |||||||
| Race/ethnicitya: | |||||||
| White, non-Hispanic | 75 (78.1) | 25 (83.3) | 50 (75.8) | 0.405 | 19 (95.0) | 56 (73.7) | 0.064 |
| Other | 21 (21.9) | 5 (16.7) | 16 (24.2) | 1 (5.0) | 20 (26.3) | ||
|
| |||||||
| Mental health scorea, Mean (SD) | 67.4 (18.6) | 64 (16.1) | 69 (19.6) | 0.229c | 62.6 (17.9) | 68.7 (18.7) | 0.196c |
|
| |||||||
| Past-year binge drinking, N (%) | 5 (5.2) | 5 (16.7) | 0 | – | – | – | – |
|
| |||||||
| Age in years at use onset, Mean (SD) | – | 14.9 (2.1) (N=35)* |
– | 14.7 (1.2) (N=21)* |
– | ||
Data are presented as number n (column percent)
P-value for chi-square test, unless otherwise indicated
Two-sample t test
Shaded cells indicate that the p-value is statistically significant (<0.05)
Some subjects who did not report past year alcohol/marijuana use did report an age at use onset given that they had a history of prior substance use.
ADHD-Specific Reasons for Marijuana Use
The majority (61%) of participants reporting past year marijuana use endorsed that they “thought it would make [their] ADHD symptoms better or help with medication side effects.” Over half (56%) of participants endorsed choosing marijuana “instead of alcohol because [they] thought alcohol was worse for [their] ADHD” (Figure 1).
Figure 1. ADHD-Specific Reasons for Marijuana Use among Past-year Marijuana Users.
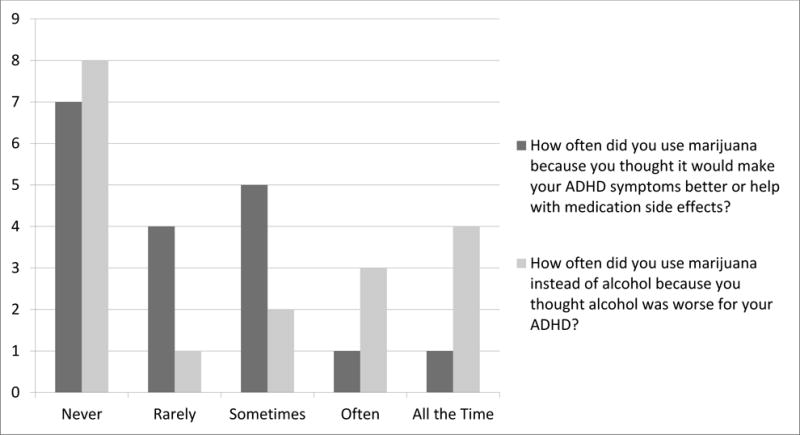
Figure shows the frequency distribution for participants’ response about reasons for choosing marijuana, among past-year marijuana users who responded to these questions (N=18). Of these past-year marijuana users, 61% (N=11) reported ever using marijuana because they thought it would make their ADHD symptoms better or help with medication side effects, and 56% (N=10) reported ever using marijuana instead of alcohol because they thought alcohol was worse for their ADHD.
Knowledge of ADHD-Specific Alcohol Risks
The majority (62.5%) of participants answered incorrectly (no/don’t know) when asked if alcohol could make ADHD symptoms worse. Bivariate analyses found that age, gender, race/ethnicity, past year alcohol use, and medication use were not significantly different between those who correctly identified that alcohol could make ADHD symptoms worse and those who answered incorrectly. The majority (62.5%) also incorrectly answered when asked if alcohol could interfere with their medications. Older participants were more likely to correctly identify that alcohol interferes with their medications (16.3 years vs. 15.4 years, p=0.015). Gender, race/ethnicity, past year drinking status, and medication status were not significantly different across reported knowledge for this question (Table 2).
Table 2.
Knowledge of ADHD-Specific Alcohol Use Risks by Sociodemographic Characteristics
| Covariates | Can alcohol make ADHD symptoms worse?
|
Can alcohol interfere with medications you take?
|
||||
|---|---|---|---|---|---|---|
| Yes (n=36) | No/Don’t know (n=60) | p-valueb | Yes (n=36) | No/Don’t know (n=60) | p-valueb | |
|
| ||||||
| Age in year, Mean (SD) | 16.0 (1.3) | 15.6 (1.9) | 0.206c | 16.3 (1.4) | 15.4 (1.81) | 0.015c |
|
| ||||||
| Gender:a | ||||||
| Male | 25 (69.4) | 34 (56.7) | 0.213 | 24 (66.7) | 35 (58.3) | 0.417 |
| Female | 11 (30.6) | 26 (43.3) | 12 (33.3) | 25 (41.7) | ||
|
| ||||||
| Race/ethnicity:a | ||||||
| White, non-Hispanic | 30 (83.3) | 45 (75.0) | 0.339 | 27 (75.0) | 48 (80.0) | 0.566 |
| Other | 6 (16.7) | 15 (25.0) | 9 (25.0) | 12 (20.0) | ||
|
| ||||||
| Past year alcohol use:a | ||||||
| Any | 11 (30.6) | 19 (31.7) | 0.909 | 11 (30.6) | 19 (31.7) | 0.909 |
| None | 25 (69.4) | 41 (68.3) | 25 (69.4) | 41 (68.3) | ||
|
| ||||||
| ADHD medication use a: | ||||||
| Any | 33 (91.7) | 48 (80.0) | 0.156 | 31 (86.1) | 50 (83.3) | 0.717 |
| None | 3 (8.3) | 12 (20.0) | 5 (13.9) | 10 (16.7) | ||
Data are presented as number n (column percent)
P-value for chi-square test, unless otherwise indicated
Two-sample t test
Shaded cells indicate that the p-value is statistically significant (<0.05)
Reported Provider Screening and Messaging/Education Regarding Alcohol Use
Seventy-one participants (74%) reported that in the past year their doctor or healthcare provider asked if they drank alcohol. There was no statistically significant difference in likelihood of being asked about past alcohol use for past-year drinkers versus non-drinkers (73.3% versus 74.2%, p-value=0.925). Only a minority of participants reported that their healthcare provider discussed each of the following four specific messages about alcohol use: “alcohol use is not healthy” (27.1%), “alcohol use could make ADHD symptoms worse” (9.4%), “alcohol could interfere or get in the way of my medications” (14.6%), and “I should not drink at all or I should stop or cut down my drinking” (5.2%). Sixty-seven participants (69.8%) reported that they did not receive any of these four specific messages about alcohol use, while 15 (15.6%) participants reporting receiving just one message, 5 participants (5.2%) reported receiving two messages, 7 (7.3%) reported receiving three messages, and 2 (2.1%) reported receiving all four of the messages. Bivariate analyses found that youth who were older and drank alcohol in the past year were more likely to report receiving each specific message about alcohol use (Table 3).
Table 3.
Healthcare Provider Screening and Messaging/Education about Alcohol Use by Sociodemographic Characteristics
| Reported Messages Received | Alcohol use is not healthy | Alcohol use could make ADHD symptoms worse | Alcohol could interfere with or get in the way of my medications | I should not drink at all or I should stop or cut down my drinking | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Covariates | Yes (n=26) |
No (n=70) |
p-valueb | Yes (n=9) | No (n=87) |
p-valueb | Yes (n=14) |
No (n=82) |
p-valueb | Yes (n=5) |
No (N=91) |
p-valueb |
|
| ||||||||||||
| Age in years, Mean (SD) | 16.5 (0.99) | 15.4 (1.82) | <0.001c | 17.0 (0.87) | 15.6 (1.7) | <0.001c | 16.8 (0.80) | 15.6 (1.75) | <0.001c | 16.6 (0.55) | 15.7 (1.73) | 0.015c |
|
| ||||||||||||
| Gendera | ||||||||||||
| Male | 18 (69.2) | 41 (58.6) | 0.340 | 6 (66.7) | 53 (60.9) | 0.736 | 8 (57.1) | 51 (62.2) | 0.720 | 4 (80.0) | 55 (60.4) | 0.382 |
| Female | 8 (30.8) | 29 (41.4) | 3 (33.3) | 34 (39.1) | 6 (42.8) | 31 (37.8) | 1 (20.0) | 36 (39.5) | ||||
|
| ||||||||||||
| Race/ethnicitya: | ||||||||||||
| White, non-Hispanic | 21 (80.8) | 54 (77.1) | 0.703 | 9 (100.0) | 66 (75.9) | 0.095 | 12 (85.7) | 63 (76.8) | 0.457 | 3 (60.0) | 72 (79.1) | 0.314 |
| Other | 5 (19.2) | 16 (22.8) | 0 (0.0) | 21 (24.1) | 2 (14.3) | 19 (23.1) | 2 (40.0) | 19 (20.9) | ||||
|
| ||||||||||||
| Past year alcohol usea: | ||||||||||||
| Any | 16 (61.5) | 14 (20.0) | <0.001 | 7 (77.8) | 23 (26.4) | 0.002 | 10 (71.4) | 20 (24.4) | <0.001 | 5 (100.0) | 25 (27.5) | <0.001 |
| None | 10 (38.5) | 56 (80.0) | 2 (22.2) | 64 (73.5) | 4 (28.6) | 62 (75.6) | 0 (0.0) | 66 (72.5) | ||||
|
| ||||||||||||
| ADHD medication usea: | ||||||||||||
| Any | 23 (88.5) | 58 (82.8) | 0.502 | 7 (77.8) | 74 (85.0) | 0.567 | 12 (85.7) | 69 (84.1) | 0.881 | 4 (80.0) | 77 (84.6) | 0.782 |
| None | 3 (11.5) | 12 (17.1) | 2 (22.2) | 13 (14.9) | 2 (14.3) | 13 (15.8) | 1 (20.0) | 14 (15.4) | ||||
Data are presented as number n (column percent)
P-value for chi-square test, unless otherwise indicated
Two-sample t test
Shaded cells indicate that the p-value is statistically significant (<0.05)
Discussion
This study reported on ADHD-specicific reasons for marijuana use, knowledge of ADHD-specific alcohol risks, and reported provider screening and messaging/education regarding alcohol use among adolescents with ADHD. Past-year marijuana use was reported by 20.8% of the sample and many of these participants reportedly chose marijuana because they thought it would help with their ADHD symptoms or medication side effects, suggesting an under-appreciation of the risks of marijuana use. We found that most (62.5%) of the adolescents with ADHD in this study lacked knowledge about how alcohol can negatively impact ADHD symptoms and medication treatment. Despite most (74%) participants reporting that their provider asked about alcohol use in the past year, few participants received specific messages/education that alcohol could make ADHD symptoms worse (9.4%) or interfere with ADHD medications (14.6%). These findings highlight the need to educate youth with ADHD about their unique substance use risks. Incorporating education about ADHD-specific substance use risks into clinical ADHD care may fill a currently missing gap in care.
Despite current scientific research highlighting the unique risks of substance use among ADHD youth,8 our study is the first to show that most adolescents with ADHD may be unaware of these specific risks, as the majority of participants were unaware of the negative impact alcohol use can have on ADHD symptoms and medications. Moreover, we identified that many participants endorsing marijuana use reported doing so because they thought it would make their ADHD symptoms better or help with medication side effects; this is very concerning given that adolescent marijuana use can result in impairments in executive functioning, a source of the symptomatology in ADHD,16 and cognitive skills later in adulthood.17, 18 Although older participants were more likely to know that alcohol can interfere with medications, they were not more likely to know that alcohol can make ADHD symptoms worse. The finding that gender, race/ethnicity, past year drinking status, and medication status were not significantly different across knowledge of ADHD-specific alcohol risks indicates that while there may not be large disparities in knowledge within this sample, all groups were similarly unaware of important risks.
Our study showed that although both older age and reported past-year drinking for participants were associated with increased likelihood of receiving specific information about alcohol harms/risks, the vast majority of participants did not receive specific messaging/education about the risk of alcohol making ADHD symptoms worse or interfering with medications. These findings highlight a missed educational opportunity. The mean age of participants who reported receiving specific messages/education from providers (16.5 – 17.0 years, depending on the message) was noticeably higher than the mean age of onset of alcohol use in the sample, which was 14.9 years. This discrepancy suggests that providers may be underestimating the prevalence of alcohol use among their younger patients with ADHD and highlights the need to educate youth with ADHD about specific alcohol risks at a younger age, ideally prior to initiation of alcohol use. We also found that nearly 70% of youth did not receive any specific messages about alcohol use and only 15% reported receiving two or more messages from their providers. Although further research is needed to identify which messages are the most salient for youth and most likely to motivate behavior change, it is reasonable to speculate that providing tailored, specific messaging around alcohol use harms (i.e., alcohol use could make ADHD symptoms worse, alcohol could interfere with medications, etc.) may increase youths’ knowledge about the tangible, ADHD-specific risks of substance use, and in turn motivate youth with ADHD to abstain or reduce their consumption. Additionally, future work can identify which, if any, specific provider messages about marijuana use are given to youth with ADHD. Identifying and validating ways to improve knowledge and awareness about substance use risk within clinical ADHD care is an important area for further research to prevent the negative outcomes of substance use and substance use disorders among individuals with ADHD.
The findings of this study must be interpreted in the context of a few limitations. Our sample size was relatively small and homogeneous with all participants recruited from one developmental subspecialty clinic. Our findings may not be generalizable to adolescents that receive care from their primary care physician, or to those from other geographic areas. Further, we may have been underpowered to detect some differences in the outcomes by demographics. It is possible that participants in this study may represent a different type of patient with ADHD, given that they are already receiving subspecialty ADHD care, and knowledge about ADHD-specific substance use risks may differ in other populations. Participants did not provide information about current level of ADHD symptoms, thus we are unable to determine if substance use varied by the level of ADHD symptoms reported. We did not collect information about co-morbid conditions and most participants indicated overall good mental health functioning, according to their scores of the MHI-5. It is possible that either the participants in this study had fewer co-morbid mental health difficulties than expected for youth with ADHD or that self-report of mental health with a short screen did not adequately capture existing mental health problems. Rates of both alcohol and marijuana use were lower than those reported in the Multimodal Treatment of ADHD (MTA) Study in which 47.0% reported past lifetime alcohol and 32.1% reported past lifetime marijuana use at the 8 year follow-up period.19 Differences in age (participants in MTA were slightly older than youth in our sample) or in recall time (past-year for this study versus lifetime for MTA) may partially account for this discrepancy. Another limitation is that we ascertained healthcare provider screening practices and ADHD-specific messaging/education from the adolescent youth, rather than directly from observing clinical encounters or asking healthcare providers themselves and it is possible that more information was delivered by providers than retained by participants. Nonetheless, the messages that the youths recall are likely to have the greatest impact on their behavior.
In conclusion, the results of this study suggest that incorporation of ADHD-specific substance use information in clinical practice could help to address gaps in knowledge about the risks of substance use for youth with ADHD.
Acknowledgments
Acknowledgements: We would like to acknowledge Kara Magane for her help with manuscript preparation as well the funding source of National Institute on Alcohol Abuse and Alcoholism, R01AA021913 (PIs: Sharon Levy; Elissa Weitzman).
Footnotes
We have no conflicts of interest to disclose.
References
- 1.Barbaresi W, Katusic S, Colligan R, et al. How common is attention-deficit/hyperactivity disorder? Towards resolution of the controversy: results from a population-based study. Acta Paediatr Suppl. 2004;93:55–59. doi: 10.1111/j.1651-2227.2004.tb03058.x. [DOI] [PubMed] [Google Scholar]
- 2.Barkley RA, Fischer M, Smallish L, et al. The persistence of attention-deficit/hyperactivity disorder into young adulthood as a function of reporting source and definition of disorder. Journal of abnormal psychology. 2002;111:279–289. [PubMed] [Google Scholar]
- 3.Brinkman WB, Epstein JN, Auinger P, et al. Association of attention-deficit/hyperactivity disorder and conduct disorder with early tobacco and alcohol use. Drug and alcohol dependence. 2014 doi: 10.1016/j.drugalcdep.2014.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Levy S, Katusic SK, Colligan RC, et al. Childhood ADHD and risk for substance dependence in adulthood: a longitudinal, population-based study. PloS one. 2014;9:e105640. doi: 10.1371/journal.pone.0105640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wilens TE, Martelon M, Joshi G, et al. Does ADHD predict substance-use disorders? A 10-year follow-up study of young adults with ADHD. J Am Acad Child Adolesc Psychiatry. 2011;50:543–553. doi: 10.1016/j.jaac.2011.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brook JS, Whiteman M, Cohen P, et al. Longitudinally predicting late adolescent and young adult drug use: childhood and adolescent precursors. J Am Acad Child Adolesc Psychiatry. 1995;34:1230–1238. doi: 10.1097/00004583-199509000-00022. [DOI] [PubMed] [Google Scholar]
- 7.Kandel DB, Johnson JG, Bird HR, et al. Psychiatric comorbidity among adolescents with substance use disorders: findings from the MECA Study. J Am Acad Child Adolesc Psychiatry. 1999;38:693–699. doi: 10.1097/00004583-199906000-00016. [DOI] [PubMed] [Google Scholar]
- 8.Weitzman ER, Ziemnik RE, Huang Q, et al. Alcohol and Marijuana Use and Treatment Nonadherence Among Medically Vulnerable Youth. Pediatrics. 2015;136:450–457. doi: 10.1542/peds.2015-0722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wolraich M, Brown L, Brown RT, et al. ADHD: clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics. 2011;128:1007–1022. doi: 10.1542/peds.2011-2654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grotenhermen F. The toxicology of cannabis and cannabis prohibition. Chemistry & biodiversity. 2007;4:1744–1769. doi: 10.1002/cbdv.200790151. [DOI] [PubMed] [Google Scholar]
- 11.Kollins SH, Schoenfelder EN, English JS, et al. An exploratory study of the combined effects of orally administered methylphenidate and delta-9-tetrahydrocannabinol (THC) on cardiovascular function, subjective effects, and performance in healthy adults. Journal of substance abuse treatment. 2015;48:96–103. doi: 10.1016/j.jsat.2014.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Barkla XM, McArdle PA, Newbury-Birch D. Are there any potentially dangerous pharmacological effects of combining ADHD medication with alcohol and drugs of abuse? A systematic review of the literature. BMC psychiatry. 2015;15:270. doi: 10.1186/s12888-015-0657-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lexi-Comp I. Lexi-Drugs. Lexi-Comp, Inc; [Google Scholar]
- 14.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Medical care. 1992;30:473–483. [PubMed] [Google Scholar]
- 15.Weitzman ER. Poor mental health, depression, and associations with alcohol consumption, harm, and abuse in a national sample of young adults in college. The Journal of nervous and mental disease. 2004;192:269–277. doi: 10.1097/01.nmd.0000120885.17362.94. [DOI] [PubMed] [Google Scholar]
- 16.Weyandt LL, Oster DR, Gudmundsdottir BG, et al. Neuropsychological Functioning in College Students With Without ADHD. Neuropsychology. 2016 doi: 10.1037/neu0000326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Meier MH, Caspi A, Ambler A, et al. Persistent cannabis users show neuropsychological decline from childhood to midlife. Proceedings of the National Academy of Sciences of the United States of America. 2012;109:E2657–2664. doi: 10.1073/pnas.1206820109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lisdahl KM, Gilbart ER, Wright NE, et al. Dare to delay? The impacts of adolescent alcohol and marijuana use onset on cognition, brain structure, and function. Frontiers in psychiatry. 2013;4:53. doi: 10.3389/fpsyt.2013.00053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Molina BS, Hinshaw SP, Eugene Arnold L, et al. Adolescent substance use in the multimodal treatment study of attention-deficit/hyperactivity disorder (ADHD) (MTA) as a function of childhood ADHD, random assignment to childhood treatments, and subsequent medication. J Am Acad Child Adolesc Psychiatry. 2013;52:250–263. doi: 10.1016/j.jaac.2012.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]


