Abstract
Background
In modern practice, real-time ultrasound guidance is commonly employed for the placement of internal jugular vein catheters. With a new tool, such as ultrasound, comes the opportunity to refine and further optimize the ultrasound view during jugular vein catheterization. We describe jugular vein access techniques and use the long-axis view as an alternative to the commonly employed short-axis cross-section view for internal jugular vein access and cannulation.
Conclusion
The long-axis ultrasound-guided internal jugular vein approach for internal jugular vein cannulation is a useful alternative technique that can provide better needle tip and guidewire visualization than the more traditional short-axis ultrasound view.
Keywords: cannulation, ultrasound, internal jugular vein, venous catheterization, short axis, long axis
Rezumat
Introducere
În practica modernă, ghidajul ultrasonografic în timp real este frecvent utilizat pentru cateterismul venei jugulare interne. Concomitent cu introducerea acestei noi abordări apare şi necesitatea de a optimiza imaginea ultrasonografică în cursul cateterismului venei jugulare interne. Am descris tehnica de acces a venei jugulare interne cu vizualizarea în ax longitudinal ca pe o alternativă la abordarea în ax transversal, utilizată de regulă pentru canularea venei jugulare interne.
Concluzii
Abordul ultrasonoghidat în ax longitudinal pentru cateterismul venei jugulare interne reprezintă o tehnică alternativă ce permite atât vizualizarea acului, cât şi a ghidului metalic, spre deosebire de tehnica clasică de vizualizare ultrasonografică în ax transversal.
Introduction
Central venous catheter (CVC) placement is performed more than 5 million times each year in the United States [1]. While there are multiple routes for CVC insertion, the most common route used by anesthesia providers is the internal jugular vein (IJV) because it can be conveniently accessed and is associated with less severe mechanical complications than other approaches [2]. Techniques for CVC placement are either anatomical landmark-based or ultrasound-guided. For IJV access, there is compelling evidence that the ultrasound-guided approach is preferred, as it is associated with higher success and lower complication rates [3–6]. Overall, more than 15% of patients who undergo central venous catheterization experience a complication [1, 7–12]. In light of this statistic, there is ongoing debate concerning the best method of needle confirmation and wire placement within the vessel [13]. This brief report reviews the various techniques for CVC placement via the IJV. We describe a practical modification to the traditional short-axis, ultrasound-guided technique to improve patient safety when using the IJV route for CVC placement.
Anatomical landmarks vs. manometry and ultrasound-guided techniques
The traditional technique for CVC placement via the IJV consists of selecting the skin entry site by palpation of the carotid artery and external anatomical landmarks. However, variation in the relationships of these landmarks to the underlying structures exists in up to 20% of patients [14–16]. The anatomic relationship between the IJV and the carotid artery is also substantially influenced by the patient’s head position [17]. It has been noted that variation in location and size of the IJV and its relation to the carotid artery can complicate cannulation when using the anatomic landmark approach. In fact, several reports have described an approximate 5% rate of unintended cervical artery puncture with the landmark-based technique [13, 18].
Given this risk, the use of manometry (i.e., tubing connected to the needle to demonstrate low pressure in the resulting blood column and easy flow of blood back into the vessel) and ultrasound have been reported to decrease the percentage of IJV cannulation complications [13, 19, 20]. Manometry, however, does not decrease overall arterial puncture, as approximately 5% of the cases reported by Ezaru et al. involved puncture of the artery with the finder needle [13]. An argument can be made that a 5% incidence of arterial puncture is not benign, and, therefore, real-time ultrasound guidance is superior in confirming proper needle and wire placement [21].
Several studies have compared the landmark-based technique versus the real-time short-axis view, ultrasound-guided technique for IJV placement of CVCs. Ultrasound-guided IJV access, in comparison to the landmark technique, is associated with significantly lower failure and complication rates [3–6, 22–26]. When compared to using the landmark-based approach, a 2007 meta-analysis reported ultrasound guidance for placement of CVCs to have a relative risk reduction (RRR) of 86% for failed catheter placements, a 57% RRR for complications with catheter placement, and a 41% RRR for failure on the first attempt (p < 0.05) [3].
A less often used ultrasound technique is one that uses a long-axis transducer orientation, in which the vessel image appears as a thick line rather than as a circular structure (short-axis view). Using the long-axis view results in greater accuracy in localizing the needle tip compared to the short-axis orientation on standardized manikins [27–28]. A study performed by Blaivas et al. on life-like, vascular access manikins found that 64% of the participants accidentally penetrated the posterior wall of the IJV during cannulation when using the short-axis view for ultrasound guidance, 20% of which unknowingly penetrated the carotid artery [29]. The conclusion of this study was that even in the setting of direct ultrasound guidance, one can have a false sense of security when the image captured is in the short-axis view. It was suggested that reconfirmation of the guidewire in the long-axis view before line placement could reduce the incidence of accidental arterial dilation/cannulation [29]. Another report using direct ultrasound guidance for CVC placement found that the short-axis, ultrasound-guided approach (without manometry) can also provide a false sense of security to the practitioner, thus placing the patient at risk for accidental arterial cannulation [23] This study concluded that it may be prudent to not only visualize the entire path of the needle using the long-axis approach, but also that correct cannulation should be confirmed by imaging the guidewire lying in the vessel in the long-axis view before line placement. Accordingly, in our report, we describe our approach using the long-axis, ultrasound-guided approach to IJV cannulation.
Ultrasound-guided technique for placement of IJV CVCs using the long-axis view
First, position, prep, and drape the patient as per standard procedure, with the patient’s head rotated less than 30° toward the contralateral side of the planned IJV cannulation. Next, obtain an image of the IJV and carotid artery in the short-axis view. This approach will display an image of the IJV and carotid artery as round structures (Fig. 1). In the majority of patients, the carotid artery is located just medial and deep to the IJV; however, the relative position of the vessels can vary significantly. Of note, the carotid artery usually has a thicker wall, and is noncompressible and pulsatile in comparison to the larger, thin-walled, compressible IJV. Next, scan cephalad and caudad along the path to find the level at which the two vessels are positioned the farthest apart, with the vein most lateral to the artery and where the vein has the largest caliber. Color Doppler, if available, can be applied to the image to confirm blood flow in the vessels to rule out thrombus, determine patency, and to further differentiate between arterial and venous blood flow.
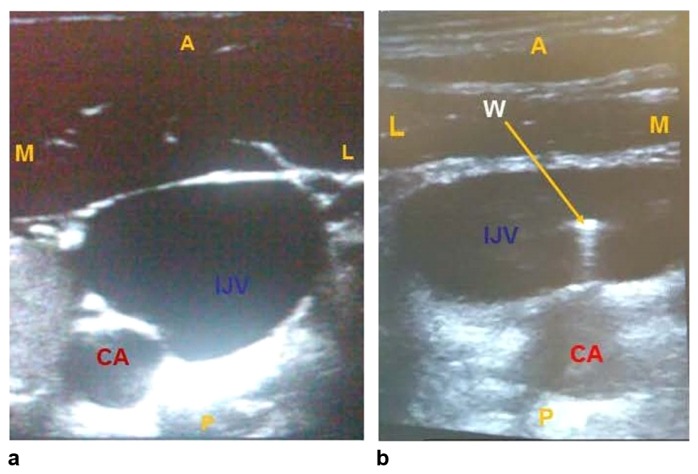
Fig. 1.
These are ultrasound images in the short-axis view showing the relationship of the CA and IJV in the same field appearing as round structures. Classically, the CA is positioned just medial to the IJV (a), but variance in this relationship exists in up to 20% of the population. The CA can often be positioned posterior to the IJV (b). IJV – internal jugular vein, CA – carotid artery. M – medial, L – lateral, A – anterior, P – posterior, W – wire
Following these initial steps, with the IJV centered in the image, the ultrasound probe is rotated 90° into the long-axis view while keeping the IJV visible throughout this maneuver. The ultrasound probe should now be parallel to the vessel. To verify that the imaged vessel is the IJV, move the ultrasound probe medially and visualize the deeper lying artery, or one can also confirm the IJV position by the aforementioned differentiating characteristics between the IJV and artery, including compressibility. It is important to note the orientation of the probe relative to the screen image, as this will affect visualization of the needle entering the field of view. The probe should be positioned such that the cephalad end of the probe in the long-axis orientation is represented on the left side of the screen. Next, the access needle is placed through the skin approximately one centimeter cephalad to the ultrasound probe, and inserted in the imaging plane of the probe at a 45° angle or shallower to the skin while gently aspirating (Fig. 2). The needle should be appreciated in the ultrasound image, and will appear as a hypoechoic (gray) or hyperechoic (white) line (Fig. 3). Typically, when the needle first penetrates the anterior wall of the IJV, this wall of the vessel will be compressed toward, or even against, the posterior wall. Once the needle enters the IJV, it will return to its normal shape. With practice, penetration of the posterior wall of the IJV is much more easily avoided with this technique compared to using the short-axis approach. After the vessel is entered and aspiration of venous blood is confirmed, place the guidewire using the Seldinger technique. An assistant is required to hold the ultrasound probe in position while the operator advances the wire through the introducer needle/angiocatheter. As the wire is advanced through the needle tip, one will be able to visualize the wire tip curve coming out of the needle tip into the vessel (Fig. 4). In doing so, not only can the tip of the needle be visualized, but the wire that remains in the lumen of the IJV can be verified.
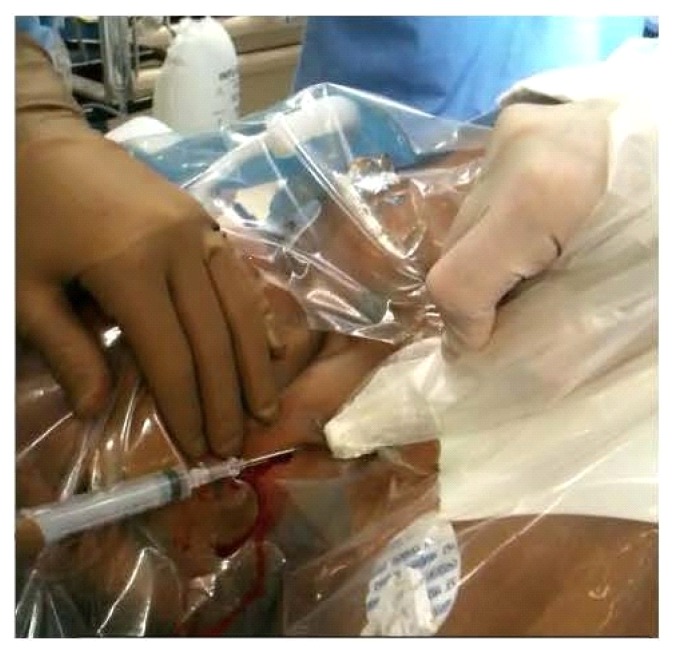
Fig. 2.
This image depicts how the ultrasound probe is positioned to give a long-axis view using a “three-handed technique,” with the physician placing the line being able to use one hand to retract the skin while an assistant holds the probe steady. The ultrasound probe is parallel with the IJV. The introducer needle is placed through the skin approximately 1 cm cephalad to the ultrasound probe and inserted in the imaging plane of the probe at a 45-degree angle to the skin while aspirating. IJV – internal jugular vein
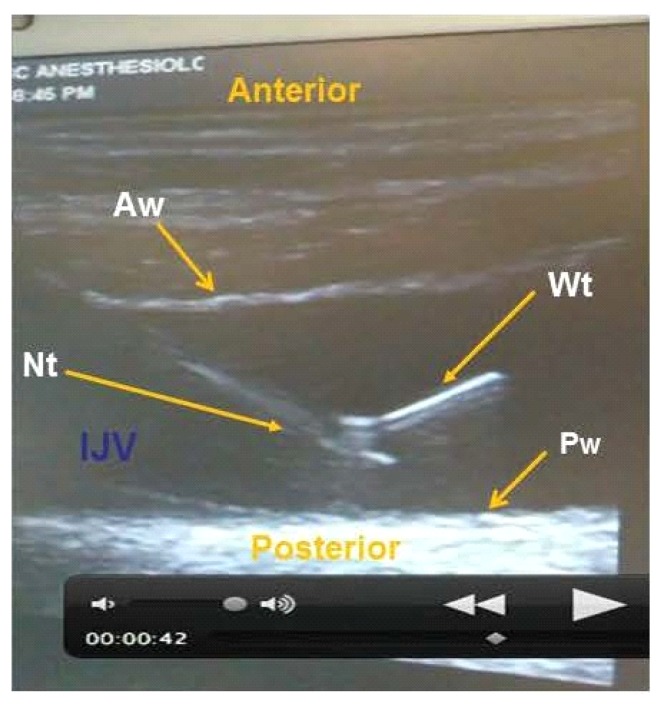
Fig. 3.
This is an ultrasound image in the long-axis view showing the wire tip curving out of the needle tip into the lumen of the IJV. Notice that the needle and wire appear as hyperechoic (white) lines. The needle tip and wire tip can be visualized in this view to verify that they are in the IJV lumen prior to dilation and placement of the CVC. IJV – internal jugular vein lumen, CVC – central venous catheter, Aw – anterior wall of the IJV, Pw – posterior wall of the IJV, Nt – needle tip, Wt – wire tip
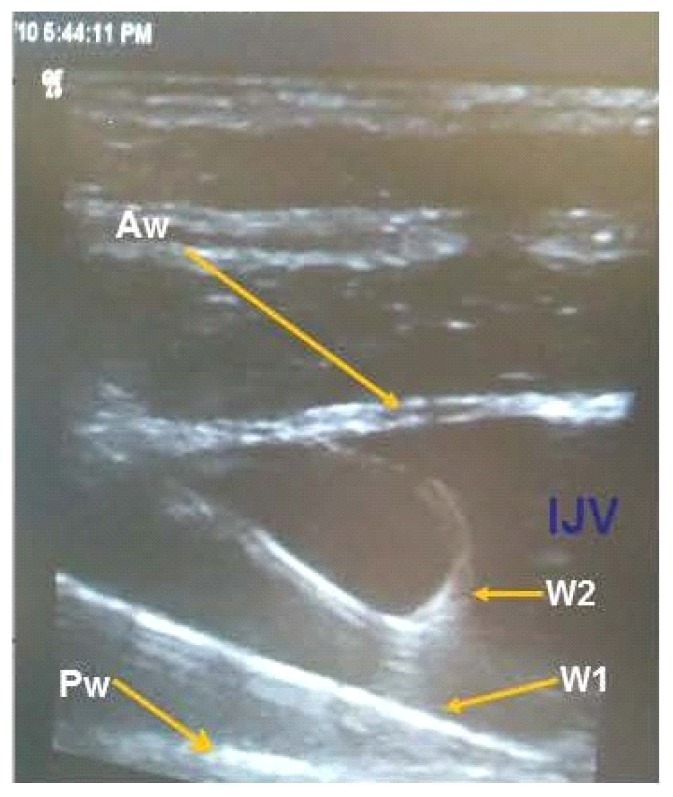
Fig. 4.
These ultrasound images are showing the IJV in the long-axis view with the curved tip of the wire (W2) visualized in the lumen of the IJV. In this instance the IJV was stuck twice for preparation in a liver transplant. W1 shows the first wire fully advanced into the SVC. The tip is not in view and could possibly have penetrated the posterior wall of the IJV. W2 shows the curved tip of the wire in lumen of the IJV. If wire placement is confirmed in this manner prior to advancing the wire and cannulating the IJV, then the likelihood of improper placement of CVCs should be lessened. IJV – internal jugular vein lumen, Aw – anterior wall of the IJV, Pw – posterior wall of the IJV, W1 – wire 1 that is fully advanced into the superior vena cava (SVC), W2 – curved tip of Wire 2
If wire placement is not accomplished using real-time ultrasound guidance, there are alternative methods to verify venous placement: 1) pull the wire back slowly until the J tip is visualized in the IJV in the long-axis view; or, 2) in the short-axis view, use the ultrasound transducer to scan under the clavicle and into the proximal superior vena cava. At this point, the catheterization procedure can be completed as per standard procedure.
Discussion
IJV access, success and avoiding complications remain important clinical goals. We have described a technique for ultrasound-guided CVC placement via the IJV route, and confirmation using real-time, direct ultrasound guidance with the long-axis (longitudinal) view as an alternative to the short-axis (cross-section) approach. Limited in vitro studies have compared the short-axis to the long-axis view for ultrasound-guided CVC placement. Those that have been performed (in vitro) showed better needle tip localization when using the long-axis approach in comparison to the short-axis view. The novel aspect of this approach involves the continuous real-time confirmation of needle and wire position. Confirmation of the curved end of the guidewire in the vessel, prior to wire advancement and vessel cannulation, should serve to further lessen the likelihood of improper central venous catheterization of the IJV. The approach described may replace the need for manometry, as it allows for direct confirmation of not just the needle, but the guidewire as well.
Footnotes
Conflict of interest
Nothing to declare
Funding
Support for this work was solely through institutional and departmental sources
References
- 1.McGee DC, Gould MK. Preventing complications of central venous catheterization. N Engl J Med. 2003;348:1123–1133. doi: 10.1056/NEJMra011883. [DOI] [PubMed] [Google Scholar]
- 2.Timsit JF. What is the best site for central venous catheter insertion in critically ill patients? Crit Care. 2003;7:397–399. doi: 10.1186/cc2179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hind D, Calvert N, McWilliams R, Davidson A, Paisley S, Beverley C, et al. Ultrasonic locating devices for central venous cannulation: meta-analysis. BMJ. 2003;327:361. doi: 10.1136/bmj.327.7411.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hatfield A, Bodenham A. Portable ultrasound for difficult central venous access. Br J Anaesth. 1999;82:822–826. doi: 10.1093/bja/82.6.822. [DOI] [PubMed] [Google Scholar]
- 5.Randolph AG, Cook DJ, Gonzales CA, Pribble CG. Ultrasound guidance for placement of central venous catheters: a meta-anaylsis of the literature. Crit Care Med. 1996;24:2053–2058. doi: 10.1097/00003246-199612000-00020. [DOI] [PubMed] [Google Scholar]
- 6.Armstrong PJ, Cullen M, Scott DHT. The ‘SiteRite’ ultrasound machine – an aid to internal jugular vein cannulation. Anaesthesia. 1993;48:319–323. doi: 10.1111/j.1365-2044.1993.tb06953.x. [DOI] [PubMed] [Google Scholar]
- 7.Merrer J, De Jonghe B, Golliot F, Lefrant JY, Raffy B, Barre E, et al. Complications of femoral and subclavian venous catheterization in critically ill patients: a randomized controlled trial. JAMA. 2001;286:700–707. doi: 10.1001/jama.286.6.700. [DOI] [PubMed] [Google Scholar]
- 8.Sznajder JI, Zveibil FR, Bitterman H, Weiner P, Bursztein S. Central vein catheterization. Failure and complication rates by three percutaneous approaches. Arch Intern Med. 1986;146:259–261. doi: 10.1001/archinte.146.2.259. [DOI] [PubMed] [Google Scholar]
- 9.Veenstra DL, Saint S, Saha S, Lumley T, Sullivan SD. Efficacy of antiseptic-impregnated central venous catheters in preventing catheter-related bloodstream infection: a meta-analysis. JAMA. 1999;281:261–267. doi: 10.1001/jama.281.3.261. [DOI] [PubMed] [Google Scholar]
- 10.Mansfield PF, Hohn DC, Fornage BD, Gregurich MA, Ota DM. Complications and failures of subclavian-vein catheterization. N Engl J Med. 1994;331:1735–1738. doi: 10.1056/NEJM199412293312602. [DOI] [PubMed] [Google Scholar]
- 11.Raad I, Darouiche R, Dupuis J, Abi-Said D, Gabrielli A, Hachem R, et al. Central venous catheters coated with minocycline and rifampin for the prevention of catheter-related colonization and bloodstream infections: a randomized, double-blind trial. Ann Intern Med. 1997;127:267–274. doi: 10.7326/0003-4819-127-4-199708150-00002. [DOI] [PubMed] [Google Scholar]
- 12.Bernard RW, Stahl WM. Subclavian vein catheterizations: a prospective study. I. Non-infectious complications. Ann Surg. 1971;173:184–190. doi: 10.1097/00000658-197102000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ezaru CS, Mangione MP, Oravitz TM, Ibinson JW, Bjerke RJ. Eliminating arterial injury during central venous catheterization using manometry. Anesth Analg. 2009;109:130–134. doi: 10.1213/ane.0b013e31818f87e9. [DOI] [PubMed] [Google Scholar]
- 14.Lim CL, Keshava SN, Lea M. Anatomical variations of the internal jugular veins and their relationship to the carotid arteries: a CT evaluation. Australas Radiol. 2006;50:314–318. doi: 10.1111/j.1440-1673.2006.01589.x. [DOI] [PubMed] [Google Scholar]
- 15.Troianos CA, Kuwik RJ, Pasqual JR, Lim AJ, Odasso DP. Internal jugular vein and carotid artery anatomic relation as determined by ultrasonography. Anesthesiology. 1996;85:43–48. doi: 10.1097/00000542-199607000-00007. [DOI] [PubMed] [Google Scholar]
- 16.Denys BG, Uretsky BF. Anatomical variations of internal jugular vein location: impact on central venous access. Crit Care Med. 1991;19:1516–1519. doi: 10.1097/00003246-199112000-00013. [DOI] [PubMed] [Google Scholar]
- 17.Sulek CA, Gravenstein N, Blackshear RH, Weiss L. Head rotation during internal jugular vein cannulation and the risk of carotid artery puncture. Anesth Analg. 1996;82:125–128. doi: 10.1097/00000539-199601000-00022. [DOI] [PubMed] [Google Scholar]
- 18.Shah PM, Babu SC, Goyal A, Mateo RB, Madden RE. Arterial misplacement of large-caliber cannulas during jugular vein catheterization: case for surgical management. J Am Coll Surg. 2004;198:939–944. doi: 10.1016/j.jamcollsurg.2004.02.015. [DOI] [PubMed] [Google Scholar]
- 19.Leibowitz AB, Rozner MA. Pro: manometry should routinely be used during central venous catheterization. Anesth Analg. 2009;109:3–5. doi: 10.1213/ane.0b013e31818e4347. [DOI] [PubMed] [Google Scholar]
- 20.Ezaru CS, Mangione MP, Oravitz TM, Ibinson JW, Bjerke RJ. Eliminating arterial injury during central venous catheterization using manometry. Anesth Analg. 2009;109:130–134. doi: 10.1213/ane.0b013e31818f87e9. [DOI] [PubMed] [Google Scholar]
- 21.Leone BJ. Con: manometry during internal jugular cannulation: case not proven. Anesth Analg. 2009;109:6–7. doi: 10.1213/ane.0b013e31818e462c. [DOI] [PubMed] [Google Scholar]
- 22.Evans LV, Dodge KL, Shah TD, Kaplan LJ, Siegel MD, Moore CL, et al. Simulation training in central venous catheter insertion: improved performance in clinical practice. Acad Med. 2010;85:1462–1469. doi: 10.1097/ACM.0b013e3181eac9a3. [DOI] [PubMed] [Google Scholar]
- 23.Blaivas M. Video analysis of accidental arterial cannulation with dynamic ultrasound guidance for central venous access. J Ultrasound Med. 2009;28:1239–1244. doi: 10.7863/jum.2009.28.9.1239. [DOI] [PubMed] [Google Scholar]
- 24.Denys BG, Uretsky BF, Reddy PS. Ultrasound-assisted cannulation of the internal jugular vein. A prospective comparison to the external landmark-guided technique. Circulation. 1993;87:1557–1562. doi: 10.1161/01.cir.87.5.1557. [DOI] [PubMed] [Google Scholar]
- 25.Troianos CA, Jobes DR, Ellsion N. Ultrasound-guided cannulation of the internal jugular vein. A prospective, randomized study. Anesth Analg. 1991;72:823–826. doi: 10.1213/00000539-199106000-00020. [DOI] [PubMed] [Google Scholar]
- 26.Mey U, Glasmacher A, Hahn C, Gorschlüter M, Ziske C, Mergelsberg M, et al. Evaluation of an ultrasound-guided technique for central venous access via the internal jugular vein in 493 patients. Support Care Cancer. 2003;11:148–155. doi: 10.1007/s00520-002-0399-3. [DOI] [PubMed] [Google Scholar]
- 27.Stone MB, Moon C, Sutijono D, Blaivas M. Needle tip visualization during ultrasound-guided vascular access: short-axis vs long-axis approach. Am J Emerg Med. 2010;28:343–347. doi: 10.1016/j.ajem.2008.11.022. [DOI] [PubMed] [Google Scholar]
- 28.Sierzenski PR, Baty G, Polan D, Nichols WL, Kochert E, Bollinger M, et al. Long-axis orientation of the ultrasound transducer is more accurate for the identification and determination of vascular access needle-tip location. Ann Emerg Med. 2008;52:S170–S171. [Google Scholar]
- 29.Blaivas M, Adhikari S. An unseen danger: frequency of posterior vessel wall penetration by needles during attempts to place internal jugular vein central catheters using ultrasound guidance. Crit Care Med. 2009;37:2345–2349. doi: 10.1097/CCM.0b013e3181a067d4. [DOI] [PubMed] [Google Scholar]