Abstract
Background:
There is growing evidence for the feasibility of text-based interventions for pediatric patients with type 1 diabetes (T1D). However, less is known regarding whether the use of personalized text messages with high-risk youth and their caregivers is associated with improvements in youth health. This study examines the use of diabetes-specific texts and associated health outcomes for participants of the Novel Interventions in Children’s Healthcare (NICH) program.
Methods:
Text messages sent to youth with T1D and their caregivers during NICH intervention were coded regarding diabetes relevance and adherence-related content. Health outcome data (eg, HbA1c values, hospital admissions) prior to and following NICH program enrollment were collected.
Results:
Fewer than half (43%) of texts sent to patients and their caregivers were identified as being related to diabetes, and over 95% of diabetes-related texts were identified as adherence-related. Participants in the NICH program demonstrated a significant decrease in HbA1c values, t(23) = 2.78, p ≤ .05, and DKA-related hospital visits, t(24) = 2.78, p ≤ .01, during program involvement. Although no relationships were identified between patient-recipient text characteristics and health outcomes, the frequency and type of text messaging with caregivers was significantly associated with changes in health outcomes.
Conclusions:
This study represents the most extensive evaluation of diabetes-related SMS use and health outcomes for NICH participants to date. Findings demonstrate improvements in patient health during NICH program involvement. Implications include that sending frequent, personalized, and adherence-reinforcing texts to patients’ caregivers may result in improved patient health, decreased utilization, and, potentially, associated reductions in health care costs.
Keywords: adolescence, mHealth, NICH, SMS, text message, type 1 diabetes
Type 1 diabetes (T1D) is a challenging chronic illness characterized by a complex treatment regimen. Therefore, for even the most motivated adolescents, adherence to the diabetes regimen (eg, glucose monitoring, insulin dose adjustment and delivery) can be problematic in the context of various developmental demands.1,2 Risk factors for suboptimal adherence and associated diabetes-related complications are vast and include peer influences, psychological factors (eg, depressed mood), demographic factors (eg, lower socioeconomic status), and family factors (eg, high family conflict).1,3 Given that suboptimal adherence to medical regimens can result in negative short- and long-term outcomes, it is paramount that efficacious interventions are adapted to improve adherence in adolescents with T1D.
Since the beginning of the 21st century, there has been growing emphasis on the use of technology to address adherence difficulties in a variety of chronic health conditions. For example, automated alerts and telemonitoring programs have been increasingly utilized by health care professionals to improve adherence.4 More specifically, treatment developers and researchers have expanded examination of text-messaging interventions for diabetes care in youth with T1D.5-7 Below, we review existing interventions with text message components and describe an innovative intervention specifically aimed to improve adherence in difficult-to-treat youth with T1D through the use of text-messaging and other behavioral supports.
Existing Interventions
Several studies have evaluated the use of text messaging or Short Message Service (SMS) as a part of diabetes management interventions for pediatric patients with T1D,8 targeting blood glucose monitoring,9-12 use of insulin,9,13 diabetes education,9,11,13 physical activity,9,11,14 and barriers to adherence.15 Text messaging programs present with varying structures, which include text messages created by the research team sent at predetermined times,9,12-14 text messages based on personal T1D-related goals sent at predetermined times,11,15 and text messages containing feedback from the medical team in response to participant-generated texts.10,13 One recent study16 combined daily predetermined informational messages with weekly interactive messages related to managing the diabetes regimen. In addition, a number of text messaging programs have been combined with other interventions, including changes to insulin regimen,11 photo diaries,13 web-based interventions,12,15 and pedometers;14 however, no such programs have been combined with in-person behavioral health support.
Existing programs which utilize texting as an intervention component and their associated evaluations demonstrate several notable limitations. For example, programs which utilize “personalized” messages (ie, not automated) do not typically include text content, intervention purpose, and message timing in their descriptions and program evaluations, while relying on a seemingly predetermined list of text selections. Although predetermined lists may result in increased efficiency and consistency amongst providers, this component also limits provider flexibility to adapt texts to best fit the individual and context. In addition, despite the importance of caregiver behaviors in T1D management, our literature review identified only one previous text program that delivered messages designed specifically for caregivers.9 While text messaging interventions appear to be both feasible and preferable for youth,8 few studies have demonstrated that these interventions are associated with improvements in glycemic control from baseline to follow-up.10,11,16 Furthermore, the average baseline HbA1c levels reported for these programs (ie, range of 8.3% to 10.0%) suggest sample populations which, although not well-controlled, do not represent those patients at greatest risk. Taken together, it remains unclear whether interventions with text messaging components are associated with improved glycemic control, especially in youth with poorly controlled diabetes.
Novel Interventions in Children’s Healthcare (NICH)
Novel Interventions in Children’s Healthcare (NICH) was developed for youth repeatedly hospitalized for diabetic ketoacidosis (DKA). NICH services involve intensive home- and community-based treatment for patients and their families intended to reduce barriers to disease management. Because NICH is grounded in the ecological systems theory of human development, interventions are delivered across the multiple systems in which youth are embedded and in the settings in which health behaviors are developed and maintained (see Harris et al17 for a more thorough description of the NICH intervention and theoretical bases). Thus, text messaging is used in combination with in-person interventions whenever possible to increase contact with patients and families, provide immediate reinforcement for diabetes management, assist with on-the-fly problem solving, build rapport, provide skills coaching, and ultimately improve adherence to the diabetes regimen. Text messages are all personalized (ie, no text messages are automated or written in advance), patients have access to providers 24 hours per day, seven days per week, and all outgoing texts are sent at times tailored to the patient’s needs (ie, 58.7% of text messages were sent outside of business hours). Previous research18 has suggested that NICH providers, hereafter referred to as “interventionists,” text NICH patients and their caregivers more than once per day, that patients and their caregivers have a high rate of response, and that text content is consistent with program efforts to use texting to provide more opportunities for encouragement and support (68.4% of outgoing texts) and behavioral intervention (76.4% of outgoing texts). Although relatively small pilot evaluations of the NICH program have demonstrated associated improvements in diabetes management (eg, decreased HbA1c, reduced frequency of DKA), the association between text messaging interventions and treatment outcomes within this model have yet to be explored.
The Current Study
The purpose of the current study is to expand on previous evaluations of the NICH program by coding diabetes-related relevance of SMS, increasing the sample size of health-related outcome evaluation, and examining the association between text messaging interventions and treatment outcomes in youth with T1D and their caregivers. Specifically, we investigated (1) how NICH interventionists utilize personalized texts related to diabetes, (2) whether NICH program involvement was associated with changes in health (ie, glycemic control) and health care utilization (eg, ED visits, hospital admissions), and (3) whether changes in health-related outcomes were associated with text type and recipient. This study represents the most expansive evaluation to date of NICH program outcomes and is unique in its examination of the relationship between program outcomes and use of personalized text messaging characteristics. To our knowledge, this study also represents the first examination of the association between the SMS component of an intervention and intervention outcomes for high-risk youth with poorly controlled diabetes.
Method
Procedure and Eligibility
The current study utilizes a retrospective evaluation of text messages sent by NICH interventionists to youth with diabetes and their caregivers. Youth were referred to NICH by providers at a children’s hospital at a major academic medical center on the West Coast of the United States. Eligible youth were identified by medical staff as having experienced poor glycemic control, more than one potentially avoidable hospitalization (ie, hospital admission, emergency department visit), presence of psychosocial vulnerability (eg, youth mental health diagnosis, family financial insecurity, involvement of child protective services), and poor response to standard medical interventions. Youth and families included in this particular study had already received NICH services, and retrospective chart reviews of interventionist text records and patient medical records were conducted to collect text data.
Only patients and caregivers who had received at least six months of NICH services and two months of associated text records were included. In families with more than one identified caregiver, only texts sent to the interventionist’s primary contact person were included. If the patient or caregiver did not have access to a phone, the NICH program provided one. At the time of this study, 67 patients with diabetes had been approved for NICH services. Sixty-four families consented to treatment (95.5% engagement rate), and 26 of these families had at least two months of text records. Of these 26 patient-caregiver dyads, one patient was excluded due to caregiver discomfort with child phone access, one family was excluded due to withdrawal from program, and four caregivers were excluded due to lack of involvement in treatment. Overall, data for 25 youth (11 males and 14 females) and 22 primary caregivers (15 mothers, four fathers, one sister, one grandmother, and one girlfriend) were collected. Patient mean age at onset of treatment was 15.8 years (SD = 1.7). Twenty-three of the participating patients had been diagnosed with type 1 diabetes, and two patients had been diagnosed with type 2 diabetes and insulin dependence. All research procedures were approved by the university Institutional Review Board.
NICH Program Description
The interventions used in NICH, in addition to a case example, have been described in detail previously.17,19 At the time of this study, NICH services were being provided by eight interventionists with caseloads of approximately 8 to 10 patients and families each. Supervision was provided by doctoral-level providers, and NICH interventionists received 2 hours of weekly interdisciplinary group supervision (eg, psychologists, pediatricians, nurses, public health professionals, social workers) as well as weekly individual supervision and phone support as needed.
Data Collection
Text data were collected retrospectively by research volunteers who logged the date, time, and content of two continuous months of interventionists’ text records. Although only outgoing text messages were coded and included in analyses, incoming texts were considered to determine context of outgoing texts. Research volunteers were trained to code the content (eg, adherence, appointment) and intended intervention (ie, reminding, reinforcing, coaching) of each text. Patient age and sex as well as caregiver sex and caregiving status were recorded.
Four trained research volunteers uninvolved in data analysis and treatment conducted retrospective chart reviews of patients’ electronic health records (EHR). Volunteers collected HbA1c values, hospital admissions, emergency department (ED) visits, number of days spent in the hospital, and number of DKA episodes for the 12-month period prior to NICH enrollment and the 12-month period following enrollment. Unlike previous characterizations of this sample,18 admissions and ED visits were treated as distinct outcomes, and ED visits which resulted in an immediate admission were collapsed into a single admission. Interrater reliability estimates between the staff conducting reviews were excellent (k = 1.0).20
Text Coding
During phase one of text coding, a list of potential diabetes-related categories was created by a focus group of interventionists, researchers, and supervisors. Categories that appeared overly similar were combined, and those judged likely to be poorly represented were removed. Coders were trained to categorize whether each text was related to diabetes, appointment attendance, adherence to the medical regimen, or none of these categories. Adherence-related texts were then coded as intended to remind, reinforce, and/or coach the recipient (see Figure 1).
Figure 1.
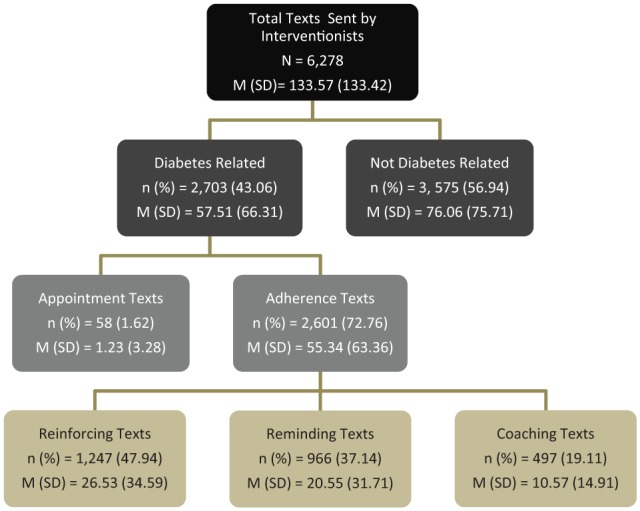
Outgoing Text Coding.
Note: M, mean; SD, standard deviation; n, number of texts sent by interventionists; %, percentage of category in row above. Means reflect the average number of texts received by each participant.
Then, in phase two, to ensure coder reliability, approximately 2800 outgoing texts from interventionists to a combination of 30 youth and caregivers were coded. This resulted in high interrater reliability (k = 0.94).
Reminding
Texts that suggested that the interventionist was reminding, requesting, or prompting the patient or parent to adhere or provide evidence of adherence in the immediate future were coded as “reminding” texts. Examples include the following statements: “Send your numbers!,” “BGL time,” an emoji of a camera, video camera, or a check mark, “Have you taken your insulin?,” and a picture or suggestion of a reward (eg, skateboard, boots, videogame, manicure) with suspected intention of prompting a patient to adhere.
Reinforcing
If a text suggested that the interventionist was providing encouragement or reinforcement related to adherence, coders were asked to code these texts as “reinforcing” texts. Examples include texts which state “Great job,” “you go girl!!!,” or “Nice!” or include a picture or suggestion of a reward (eg, skateboard, new boots, videogame, manicure) in response to a picture or text demonstrating proof of adherence.
Coaching
Coders were directed to categorize texts as “coaching” in situations in which the interventionist was problem-solving with and/or coaching a patient through how to adhere to their medical regimen. Coaching texts were in response to an issue raised in an incoming text (eg, “I don’t feel good,” “Passing ketones!,” “my BGL is 550”). Instances in which an interventionist was identified as preparing the patient in advance for how to manage diabetes were also coded as “coaching.”
Results
Descriptive Outcome Information
HbA1c
The last available HbA1c prior to NICH onset ranged from 8.30 to 14.00 (mean = 12.28, SD = 1.80) and the last HbA1c 1 year subsequent to NICH onset ranged from 8.50 to 13.60 (mean = 11.10, SD = 1.54). A paired samples t-test revealed a significant difference between HbA1c prior to NICH initiation and 1 year post-NICH initiation, t(23) = 2.78, p ≤ .05 (see Figure 2 and Table 1).
Figure 2.
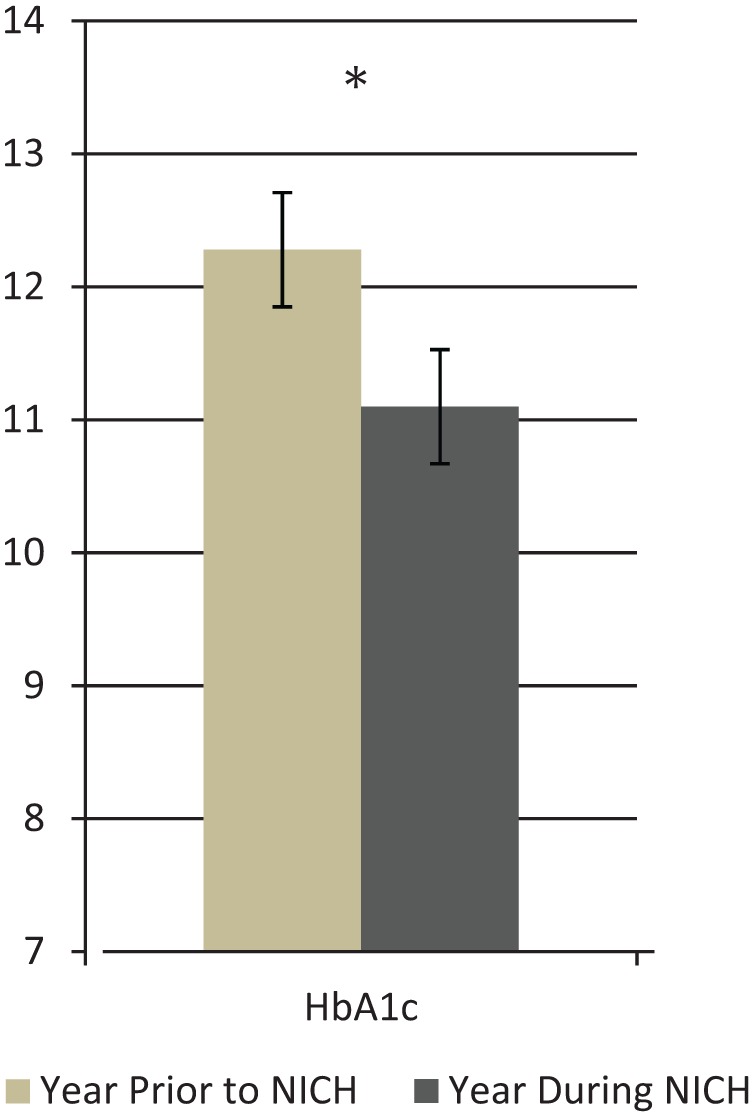
NICH Participant Lab Values.
Note: *p ≤ .05. NICH, Novel Interventions in Children’s Healthcare. Data include last value during the specified time period (ie, last available lab value carried forward).
Table 1.
NICH Participant Health Outcomes.
| Outcome measures | Year prior to NICH |
Year during NICH |
t-test | p value | ES |
|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | ||||
| HbA1ca | 12.28 (1.80) | 11.10 (1.54) | 2.78* | .011 | 0.568 |
| Number of admissionsb | 1.20 (1.16) | 0.76 (1.48) | 1.55 | .134 | 0.311 |
| Number of days admittedb | 1.92 (2.02) | 1.36 (2.90) | 1.33 | .196 | 0.266 |
| Number of ED visitsb | 1.88 (2.05) | 1.56 (2.16) | 0.58 | .566 | 0.116 |
| Number of visits in DKAb | 1.16 (1.11) | 0.56 (1.00) | 2.78** | .010 | 0.555 |
p ≤ .05. **p ≤ .01. NICH, Novel Interventions in Children’s Healthcare; SD, standard deviation; ED, emergency department; DKA, diabetic ketoacidosis.
Last available HbA1c value during specified time frame.
Total number recorded during the specified time frame.
Hospital Visits
Patients had a total of 47 ED visits during the year prior to NICH onset, ranging from 0 to 8 (mean = 1.88, SD = 2.05) and a total of 39 ED visits during the year subsequent to NICH onset, ranging from 0 to 10 (mean = 1.56, SD = 2.16). Of ED visits prior to NICH onset, 29 (61.7%) were due to a DKA episode (range = 0 to 4; mean = 1.88, SD = 2.05) and, of ED visits during the year subsequent to NICH onset, 14 (35.9%) were due to a DKA episode (range = 0 to 3; mean = 0.56, SD = 1.00). Paired samples t-tests revealed no significant difference between the number of ED visits during the year prior to NICH onset and the year subsequent to NICH onset, t(24) = 0.58, p = .566, but revealed a significant decrease from the number of DKA episodes during the year prior to NICH onset to the year subsequent to NICH onset, t(24) = 2.78, p ≤ .01 (see Figure 3 and Table 1).
Figure 3.
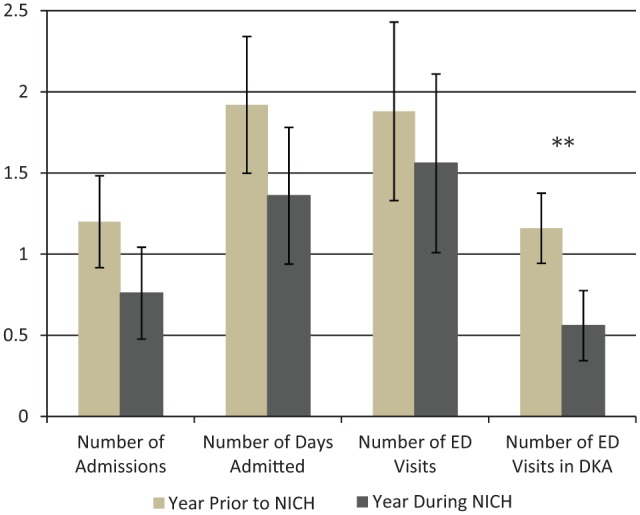
NICH Participant Hospital Utilization.
Note: **p ≤ .01. NICH, Novel Interventions in Children’s Healthcare; ED, emergency department; DKA, diabetic ketoacidosis. Error bars reflect standard error means.
In addition, patients had a total of 30 hospital admissions during the year prior to NICH onset, ranging from 0 to 4 (mean = 1.20, SD = 1.16) and a total of 19 hospital admissions during the year subsequent to NICH onset, ranging from 0 to 6 (mean = 0.76, SD = 1.48). Of recorded hospital admissions, patients spent a total of 48 days in the hospital during the year prior to NICH onset, ranging from 0 to 6 (mean = 1.92, SD = 2.02) and a total of 34 days in the hospital during the year subsequent to NICH onset, ranging from 0 to 12 (mean = 1.36, SD = 2.90). Paired samples t-tests revealed no significant differences between the number of admissions during the year prior to NICH onset and the year subsequent to NICH onset, t(24) = 1.55, p = .134, or between the number of days admitted during the year prior to NICH onset and the year subsequent to NICH onset, t(24) = 1.33, p = .196 (see Figure 3 and Table 1). However, descriptive data reveals that 9 of 25 patients (36%) did not experience a hospital admission (ie, 0 days admitted) during the year prior to NICH, whereas 18 of 25 patients (72%) did not experience a hospital admission during the year subsequent to NICH onset.
Descriptive Text Information
Interventionists sent a total of 6278 text messages to patients and caregivers (referred to hereafter as “participants” when data are combined), ranging from 6 to 571 texts per participant (mean = 133.57, SD = 133.42; Figure 1) and received a total of 6633 text messages from patients and caregivers, ranging from 8 to 672 texts per participant (mean = 141.13, SD = 155.26). Bivariate correlations examined relations among frequencies of text messages sent to and from participants and revealed significant associations between the number of incoming and the number of outgoing text messages for patients (r = .97, p < .001) and caregivers (r = .84, p < .001), suggesting that incoming and outgoing text messages are significantly positively associated within each group. The frequency of texts sent by each participant was divided by the frequency of total texts both sent and received by each participant to calculate a proxy for participant responding (ie, the percentage of total texts that were sent by participants). Thus, 50% reflects balanced texting between the participant and the interventionist (ie, the participant sent and received the same number of texts), percentages greater than 50 reflect higher rates of participant texting as compared to interventionist texting, and percentages lower than 50 reflect lower rates of participant texting as compared to interventionist texting. On average, participants sent 49.60% (SD = 8.41%) of total text messages sent and received. One-way ANOVAs examined the effect of participant type (ie, patient vs caregiver) on rate of incoming texts, rate of outgoing texts, and percentage of total texts sent by participants and did not yield significant main effects.
Text message frequencies by text type revealed that, of the 6278 text messages sent by interventionists, 43.0% were diabetes-related texts (n = 2703) and, of those diabetes-related texts, 96.2% were adherence-related texts (n = 2601) and 2.14% were appointment-related texts (n = 58). Furthermore, of adherence-related text messages sent by interventionists, 47.9% were reinforcing texts (n = 1247), 37.1% were reminding texts (n = 966), and 19.1% were coaching texts (n = 497). As such, reinforcement texts were the most commonly represented text content. Participants received an average of 25.38 (SD = 34.59) reinforcing texts, 20.55 (SD = 31.71) reminding texts, and 10.57 (SD = 14.91) coaching texts. One-way ANOVAs examining the effect of participant type (ie, patient vs mother vs father vs other caregiver) on type of texts received by the participant did not reveal significant main effects.
Relations Among Type of Outgoing Texts and Participant Response Rates
Regression analysis examining main effects of text categories (ie, reinforcing, reminding, and coaching texts) was significant among caregivers, accounting for 60.3% of the variability in proportion of caregiver texts. The main effect of reinforcing texts was significant (β = 0.77, t = 4.00, p < .01), whereas the main effects of reminding and coaching texts were null.
Regression analysis examining main effects of text categories was not significant among patients in accounting for the proportion of patient texts. Furthermore, main effects examined within this model were not significant.
Relationships Between Text and Outcome Variables
Bivariate correlations revealed that, among caregivers, the number of text messages received by the caregiver from the interventionist was significantly correlated with changes in number of hospital admissions for the patient from the year prior to NICH onset to the year subsequent to NICH onset (r = –.49, p < .05), such that sending more text messages to the caregiver was associated with a greater decrease in number of admissions during the first year of NICH for the respective patient. The bivariate correlation between frequency of text messages sent by the caregiver and change in hospital admissions was null. In addition, bivariate correlations examining associations between incoming and outgoing caregiver text frequencies and other outcome variables (ie, number of days admitted, ED visits, DKA episodes) were null. Among caregivers, further bivariate correlations revealed that changes in number of hospital admissions for the patient was significantly and negatively associated with frequency of received diabetes-related texts (r = –.50, p < .05), reinforcement texts (r = -.45, p < .05), and coaching texts (r = –.55, p < .05), such that more texts in these categories were associated with a greater decrease in the number of hospital admissions during NICH. The frequencies of adherence-related, appointment-related, and reminder texts were not significantly correlated with change in number of hospital admissions. In addition, bivariate correlations examining associations between text categories and other outcome variables (ie, number of days admitted, ED visits, DKA episodes) were null.
Among patients, bivariate correlations revealed that the frequency of text messages sent by the patient, frequency of text messages received by the patient, and changes in outcome data (ie, number of admissions, days admitted, ED visits, DKA episodes, HbA1c) were null. In addition, among patients there were no significant correlations between type of text and changes in outcome data.
Discussion
These findings represent the most extensive evaluation to date of NICH program outcomes and contribute to the broader understanding of how text message components may relate to changes in health outcomes. Results indicate that patients in the NICH program evidenced improved health during program involvement, as demonstrated by significant improvements in metabolic control. In addition, patients experienced fewer DKA episodes, on average, while involved in NICH. Furthermore, NICH participation was associated with a significant decrease in likelihood of patient hospitalization. Taken together, these findings are consistent with previous evaluations of the NICH program and suggest that NICH involvement is associated with improvements in patient health and reductions in acute medical complications (eg, DKA), both of which likely result in reduced health care costs for patients, hospitals, payors, and the general public.
Text coding results suggest that interventionists often sent texts that were designed to engage patients and reinforce their efforts to adhere to their medical regimen. These findings also demonstrate that the majority of texts sent to patients and caregivers were unrelated to diabetes. This particular finding appears unique compared to other text-based interventions described in the literature but is consistent with NICH program emphases on building rapport and the importance of the human element in behavior change. In stark contrast with continued attempts to automate interventions,21 the NICH program’s text-messaging component remains truly personalized. This unique component, although more time consuming than automated delivery systems, may allow interventionists the needed flexibility to tailor text content to individual patient and family characteristics. As such, this central component of the NICH program may allow interventionists to more effectively engage and intervene with high-risk youth and their difficult-to-engage caregivers.
Interestingly, although there was no association between outgoing texts sent to patients and health outcomes, the frequency of diabetes-related, reinforcing, and coaching texts sent to caregivers was significantly associated with decreases in hospital admissions. There are several potential explanations for this finding. The frequency with which an interventionist texts a caregiver may be a proxy for caregiver engagement, and anecdotal reports by interventionists indicate that the more involved in treatment the caregiver is, the more likely program involvement will improve health. Indeed, caregiver involvement is often integral to positive youth outcomes, and numerous studies have documented both the mediating role of caregivers as well as the barriers to treatment progress ascribed to disengaged caregivers.22,23 Alternatively, it is possible that interventionists are more likely to send texts frequently to those caregivers whose children are displaying improvements in health. Related to this, it’s possible that an unmeasured third variable (eg, caregiver stress) may drive both findings, such that high caregiver stress may result in poor child health outcomes and insufficient time for caregiver texting. Another possible explanation is that more frequent texting of caregivers results in increased caregiver engagement in their children’s medical regimen, leading to decreased likelihood of an acute medical complication. Regardless of the explanation, in combination with the wealth of evidence demonstrating the importance of family and caregiver functioning in pediatric T1D outcomes,24-29 this finding suggests that texting caregivers frequently and in a reinforcing manner should be a component considered for other text-based programs.
Regarding limitations, there was no control group with which to compare the health outcome and text data, limiting conclusions drawn regarding causality. In addition, the data presented here are retrospective, specific to the NICH program, and were collected only for those NICH patients with available text data. As such, these findings may not generalize well to other clinical programs or patient populations. Furthermore, texting is one of many potentially impactful interventions delivered during the provision of NICH. Thus, we are unable to ascertain the unique role text message interventions may play in NICH outcomes. Also, the sample size was relatively small, so analyses were underpowered and less likely to detect some relationships. Indeed, the changes in health outcomes unanimously suggested meaningful improvements during NICH, but not all were significant based on p-values. Due to the underpowered analyses and the paucity of research in this area, we did not provide a correction for multiple comparisons. Future evaluations of NICH program technology use and health outcomes would benefit from inclusion of a control group as well as a larger sample size, data regarding health care costs and interventionist time spent texting, and a more detailed examination of the temporal relationship between incoming texts, outgoing texts, and patient health behaviors.
Conclusion
Despite these limitations, this study evidences several strengths and contributes to an increasingly growing body of the literature. These findings represent the largest evaluation of the NICH program to date and demonstrate associations between program involvement and improved health in patients with T1D, which are consistent with smaller-scale examinations of the NICH model for other populations.30 In addition, this is the first examination, to our knowledge, of how diabetes-specific text content sent to both patients and caregivers is related to patient health outcomes. Study results indicate that text interventions for pediatric patients with T1D may benefit from inclusion of caregivers, high frequency of communication, flexibility in how texts are tailored, and a greater emphasis on adherence reinforcement than reminders. Ultimately, these findings suggest that NICH and similar interventions can feasibly include a personalized text component that may benefit patient health and, as a result, also reduce health care costs.
Acknowledgments
We sincerely thank the participating families who made this study possible. We greatly appreciate the help of numerous research volunteers who assisted with this project, especially Alexandra Hartman, Kirsten Hagen, Sarah Park, and Mary Kate Koch. We are also grateful to Kim Spiro, Annan Sheffield, Liz Karkula, and Rachel Raphael for their contributions to the provision of NICH services for this study. MAH developed the NICH model, participated in reviewing the literature, and edited the manuscript. DVW led the study design and data collection. SAB conducted the analyses, and LT contributed to data collection procedures, treatment provision, and manuscript edits. DVW, SAB, and MS reviewed the literature and wrote the manuscript. MAH takes responsibility for the contents of this article.
Footnotes
Abbreviations: DKA, diabetic ketoacidosis; ED, emergency department; EHR, electronic health record; M, mean; NICH, Novel Interventions in Children’s Healthcare; SD, standard deviation; SMS, Short Message Service.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Borus JS, Laffel L. Adherence challenges in the management of type 1 diabetes in adolescents: prevention and intervention. Curr Opin Pediatr. 2010;22(4):405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Harris M, Hood K, Weissberg-Benchell J. Teens with Diabetes: A Clinician’s Guide. Alexandria, VA: American Diabetes Association; 2014. [Google Scholar]
- 3. Wagner DV, Stoeckel M, Tudor ME, Harris MA. Treating the most vulnerable and costly in diabetes. Curr Diabetes Rep. 2015;15(6):1-7. [DOI] [PubMed] [Google Scholar]
- 4. Granger BB, Bosworth H. Medication adherence: emerging use of technology. Curr Opin Cardiol. 2011;26(4):279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Deacon AJ, Edirippulige S. Using mobile technology to motivate adolescents with type 1 diabetes mellitus: a systematic review of recent literature. J Telemed Telecare. 2015;0(0):1-8. [DOI] [PubMed] [Google Scholar]
- 6. Guljas R, Ahmed A, Chang K, Whitlock A. Impact of telemedicine in managing type 1 diabetes among school-age children and adolescents: an integrative review. J Pediatr Nurs. 2014;29(3):198-204. [DOI] [PubMed] [Google Scholar]
- 7. Harris MA, Hood KK, Mulvaney SA. Pumpers, Skypers, surfers and texters: technology to improve the management of diabetes in teenagers. Diabetes Obes Metab. 2012;14(11):967-72. [DOI] [PubMed] [Google Scholar]
- 8. Herbert L, Owen V, Pascarella L, Streisand R. Text message interventions for children and adolescents with type 1 diabetes: a systematic review. Diabetes Technol Ther. 2013;15(5):362-370. [DOI] [PubMed] [Google Scholar]
- 9. Wangberg SC, Årsand E, Andersson N. Diabetes education via mobile text messaging. J Telemed Telecare. 2006;12(suppl 1):55-56. [DOI] [PubMed] [Google Scholar]
- 10. Rami B, Popow C, Horn W, Waldhoer T, Schober E. Telemedical support to improve glycemic control in adolescents with type 1 diabetes mellitus. Eur J Pediatr. 2006;165(10):701-705. [DOI] [PubMed] [Google Scholar]
- 11. Franklin VL, Waller A, Pagliari C, Greene SA. A randomized controlled trial of Sweet Talk, a text-messaging system to support young people with diabetes. Diabet Med. 2006;23(12):1332-1338. [DOI] [PubMed] [Google Scholar]
- 12. Hanauer DA, Wentzell K, Laffel N, Laffel LM. Computerized Automated Reminder Diabetes System (CARDS): e-mail and SMS cell phone text messaging reminders to support diabetes management. Diabetes Technol Ther. 2009;11(2):99-106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Frøisland DH, Årsand E, Skårderud F. Improving diabetes care for young people with type 1 diabetes through visual learning on mobile phones: mixed-methods study. J Med Internet Res. 2012;14(4):111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Newton KH, Wiltshire EJ, Elley CR. Pedometers and text messaging to increase physical activity randomized controlled trial of adolescents with type 1 diabetes. Diabetes Care. 2009;32(5):813-815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Mulvaney SA, Anders S, Smith AK, Pittel EJ, Johnson KB. A pilot test of a tailored mobile and web-based diabetes messaging system for adolescents. J Telemed Telecare. 2012;18(2):115-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Bin-Abbas B, Jabbari M, Al-Fares A, El-Dali A, Al-Orifi F. Effect of mobile phone short text messages on glycaemic control in children with type 1 diabetes. J Telemed Telecare. 2014;20(3):153-156. [DOI] [PubMed] [Google Scholar]
- 17. Harris MA, Spiro K, Heywood M, et al. Novel interventions in children’s health care (NICH): innovative treatment for youth with complex medical conditions. Clin Pract Pediatr Psychol. 2013;1(2):137-145. [Google Scholar]
- 18. Wagner DV, Barry S, Teplitsky L, et al. Texting adolescents in repeat DKA and their caregivers. J Diabetes Sci Technol. 2016;10(4):831-839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Harris MA, Wagner D, Heywood M, et al. Online observation: youth repeatedly hospitalized for DKA: proof of concept for Novel Interventions in Children’s Healthcare (NICH). Diabetes Care. 2014;37:e125-e126. [DOI] [PubMed] [Google Scholar]
- 20. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159-174. [PubMed] [Google Scholar]
- 21. Shah H, Warwick K, Vallverdu J, Wu D. Can machines talk? Comparison of Eliza with modern dialogue systems. Comput Human Behav. 2016;58:278-295. [Google Scholar]
- 22. Armbruster P, Kazdin AE. Attrition in child psychotherapy. Adv Clin Child Psychol. 1994;16:81-109. [Google Scholar]
- 23. Sandler I, Ingram A, Wolchik S, Tein J, Winslow E. Interventions to promote resilience of children and adolescents. Child Dev Perspect. 2015;9(3):164-171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Cameron FJ, Skinner TC, De beaufort CE, et al. Are family factors universally related to metabolic outcomes in adolescents with type 1 diabetes? Diabet Med. 2008;25(4):463-468. [DOI] [PubMed] [Google Scholar]
- 25. Cohen DM, Lumley MA, Naar-King S, et al. Child behavior problems and family functioning as predictors of adherence and glycemic control in economically disadvantaged children with type 1 diabetes: a prospective study. J Pediatr Psychol. 2004;29(3):171-184. [DOI] [PubMed] [Google Scholar]
- 26. Hilliard ME, Wu YP, Rausch J, Dolan LM, Hood KK. Predictors of deteriorations in diabetes management and control in adolescents with type 1 diabetes. J Adolesc Health. 2013;52(1):28-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Jacobson AM, Hauser ST, Lavori P, et al. Family environment and glycemic control: a four-year prospective study of children and adolescents with insulin-dependent diabetes mellitus. Psychosom Med. 1994;56(5):401-409. [DOI] [PubMed] [Google Scholar]
- 28. Anderson BJ, Vangsness L, Connell A, et al. Family conflict, adherence, and glycaemic control in youth with short duration type 1 diabetes. Diabet Med. 2002;19(8):635-642. [DOI] [PubMed] [Google Scholar]
- 29. Lancaster BM, Gadaire DM, Holman K, Leblanc LA. Association between diabetes treatment adherence and parent child agreement regarding treatment responsibilities. Fam Syst Health. 2015;33(2):120-125. [DOI] [PubMed] [Google Scholar]
- 30. Harris MA, Wagner D, Wilson A, Heywood M, Hoehn D, Spiro K. Case study: an evaluation of Novel Interventions in Children’s Healthcare (NICH) for youth repeatedly hospitalized for chronic pain. Clin Pract Pediatr Psychol. 2015;3:48-58. [DOI] [PMC free article] [PubMed] [Google Scholar]


