Abstract
PURPOSE
Despite considerable investment in increasing the number of primary care physicians in rural shortage areas, little is known about their movement rates and factors influencing their mobility. We aimed to characterize geographic mobility among rural primary care physicians, and to identify location and individual factors that influence such mobility.
METHODS
Using data from the American Medical Association Physician Masterfile for each clinically active US physician, we created seven 2-year (biennial) mobility periods during 2000–2014. These periods were merged with county-level “rurality,” physician supply, economic characteristics, key demographic measures, and individual physician characteristics. We computed (1) mobility rates of physicians by rurality; (2) linear regression models of county-level rural nonretention (departure); and (3) logit models of physicians leaving rural practice.
RESULTS
Biennial turnover was about 17% among physicians aged 45 and younger, compared with 9% among physicians aged 46 to 65, with little difference between rural and metropolitan groups. County-level physician mobility was higher for counties that lacked a hospital (absolute increase = 5.7%), had a smaller population size, and had lower primary care physician supply, but area-level economic and demographic factors had little impact. Female physicians (odds ratios = 1.24 and 1.46 for those aged 45 or younger and those aged 46 to 65, respectively) and physicians born in a metropolitan area (odds ratios = 1.75 and 1.56 for those aged 45 or younger and those aged 46 to 65, respectively) were more likely to leave rural practice.
CONCLUSIONS
These flndings provide national-level evidence of rural physician mobility rates and factors associated with both county-level retention and individual-level departures. Outcomes were notably poorer in the most remote locations and those already having poorer physician supply and professional support. Rural health workforce planners and policymakers must be cognizant of these key factors to more effectively target retention policies and to take into account the additional support needed by these more vulnerable communities.
Keywords: retention, primary care physicians, mobility, rural, workforce
INTRODUCTION
Rural populations continue to experience relative shortages of the supply of primary care physicians,1 with associated links to poorer health.2 Difficulties of both recruitment and retention of physicians in rural areas, which greatly contribute to experienced shortages, are well acknowledged.3,4 There are many reasons for this ongoing workforce supply disparity, including professional, economic, infrastructural, political, educational, and sociocultural aspects.5 Although considerable research has identified factors that facilitate or impede supply of physicians in rural areas, macro-level empirical evidence of observed rural mobility of physicians—notably, which are more likely to move and why—is limited.6–9 Additionally, the frequencies with which specific rural physicians move over short periods of time, including moves driven by factors influenced by political cycle (as in the 2-year window that we have studied), are less explored.
The mobility of rural physicians includes both moving within rural areas and the least desirable outcome of leaving the rural workforce entirely by moving to large metropolitan areas. Improved understanding of mobility and nonretention of rural physicians is important because of its impact on training and workforce policy, and resultant physician supply to both the origin area (ie, the location from which the physician moved) and to the destination area (ie, the location to which the physician has moved). The cost of mobility and staff turnover can be large, both in direct costs10 but also in terms of service quality and continuity to the community.11
Primary care physicians initially choose to work in rural areas for a variety of reasons. Factors that increase the attraction and likelihood of undertaking rural practice include having a rural interest from rural origin, rural training pathways, and familiarity with the area by the physician or his/her spouse,12–14 as well as professional expectations of an increased variety of work and autonomy, and desires for nonprofessional lifestyle aspects in rural areas.15,16 In addition, a number of key policy incentives such as J-1 waivers for international medical graduate (IMG) and National Health Service Corps (NHSC) programs bring other physicians into rural locations,17,18 with some positive results.19
Although the social sciences have explored migration patterns and factors influencing both interregional and intraregional migration of the general population,20 it is not clear whether this research transfers to medical workforce mobility. The physician mobility literature has focused on 2 broad categories. First, a large focus is given to the international movement of physicians, notably, to the ethical issues related to recruiting physicians from developing countries into developed countries such as the United States.3,21 The second focus is the interregional or cross-country movement of physicians (eg, between East and West regions of the United States).22–24 Meanwhile, literature specific to the observed mobility of physicians between rural and metropolitan areas is sparse.6,25
Observed rural physician mobility generally results from factors that both push individuals toward and pull individuals away from rural areas. Associations between mobility of physicians and contributing factors have rarely been quantified,1,26,27 with younger age (current and recent medical residents) being the dominant common factor linked with increased mobility.22,28 Poorer availability of physicians, most prominent in rural areas, has been linked to increased mobility of physicians in some areas.24,29 Physicians working in small rural communities additionally report that many community-led factors such as integration, connection, and appreciation contribute to increased retention, but these factors cannot readily be measured.30,31 Place attractiveness has been linked to migration of rural populations32–34; however, its influence on rural physicians’ retention or mobility decisions remains unclear.35
In our study, we aimed to describe the geographic mobility patterns of rural primary care physicians. In particular, the study quantifies, over an extended period, mobility rates of rural physicians and investigates the moderating effect of both area-level and individual-level factors on observed rural nonretention (departure). This evidence will provide stronger understanding of the factors behind the observed mobility and nonretention of rural primary care physicians.
METHODS
Physician location data were obtained from multiple years of the American Medical Association (AMA) Masterfile. Specifically, records were drawn from 2000, 2002, 2004, 2006, 2008, 2010, 2012, and 2014, and merged together. Individual-level records were matched based on unique AMA identifiers. All physician practice locations were geocoded to the county level and then classified according to the 9-level Rural-Urban Continuum Codes (RUCC) for 2003 or 2013.36 The 6 nonmetropolitan (henceforth called rural) RUCC levels were additionally combined into the 3 population groupings (<2,500; 2,500–20,000; >20,000), with adjacency to a metropolitan area used as a separate binary variable.
Individual physicians were observed in up to 7 observation periods as potentially moving between an origin and destination across each successive 2-year interval. We chose this gap to smooth out possible lag times in the accuracy of location in the AMA data sets. Only primary care physicians (family medicine physicians, general pediatricians, geriatricians, and general internal medicine physicians) were included in the analyses; those recorded as being not in direct patient care or as residents were excluded. Further description of data selection using RUCC and the AMA data set is given in the Supplemental Appendix, available at http://www.annfammed.org/content/15/4/322/suppl/DC1/. All calculations were performed using StataMP 13.1 (StataCorp LP) with a 5% significance level.
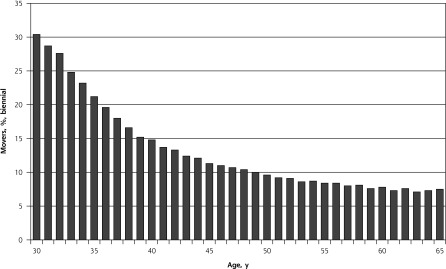
Observed physicians were split into 2 categories—those aged up to 45 years (capturing early-career increased mobility—see Figure 1) and those aged 45 to 65 years (capturing more stable mid- and late-career mobility). We excluded physicians aged older than 65 years from this study, chiefly because of data quality concerns regarding identification of clinically active physicians in this cohort.
Figure 1.
Biennial mobility rate of primary care physicians, by age.
Our first analysis examined the biennial mobility rates of all primary care physicians, both within and between rural and metropolitan counties. All location pairings were categorized as either stayers (retention) or movers (nonretention) in the same county. Our second analysis used multivariate linear regression models, weighted by population size, to examine county-level nonretention (departure) rates. The denominator is equal to the number of location pairings where that county is the origin location (irrespective of destination), while the numerator is equal to the number of location pairings where the destination county differs to the origin location. Where an observed destination location was metropolitan, all subsequent pairings were ignored until that physician moved back to a rural location. Similarly, physicians could be first observed as rural physicians only in later years because of either moving from a metropolitan area or being new to the data set (eg, because they recently completed residency). Potential impact of outlier rates, considerably more likely in small rural counties, was controlled by using a robust regression model.37 Our third analysis, using multivariate logit models with clustering, examined individual physicians observed moving from rural counties to metropolitan counties, also using only rural-origin location pairings.
All multivariate models used data from the Robert Wood Johnson Foundation (2014), American Community Survey (2011), and Health Resources and Services Administration (2014) to examine the effect on mobility of characteristics of place thought to be desirable, such as proximity to a hospital, higher house values, greater accessibility as assessed with the primary care physician–to-population ratio (PPR), more affluent communities, and larger population size, as well as characteristics thought to be less desirable, including higher uninsured rates and more unemployment. Our third analysis, split by age, additionally examined individual characteristics available in the AMA data set, and included sex, age, international medical graduate status, family physician, physician type (osteopathic or medical), Health Professional Shortage Area status, and having a rural origin (for US-born physicians).
RESULTS
Between 2000 and 2014, about 1.4 million biennial location pairings of US primary care physicians were observed. Table 1 summarizes the level of mobility by RUCC category (further detail is given in the Supplemental Appendix). The overall proportion of movers was very similar by RUCC, except for greater mobility in RUCC 8 and 9 counties. The mobility rate of younger physicians was approximately double that of older physicians (17% vs 9%). A majority of moves from rural locations were to metropolitan locations, both for younger physicians (68%) and older physicians (58%), and such moves were more common in the “adjacent to metropolitan” RUCC 4, 6, and 8 areas (younger: 74% vs 60%, older: 65% vs 47%); overall, there were slightly more moves observed from rural to metropolitan than vice versa.
Table 1.
Summary of Biennial Movers by Rurality and Age Cohorts—Primary Care Physicians, 2000–2014
| Original Location: RUCC Categorya | Aged ≤45 y | Aged 46–65 y | ||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Of Those Moving | Of Those Moving | |||||||
|
|
|
|||||||
| Physicians, No. | Movers, % | Moving to Rural, % | Moving to Metropolitan, % | Physicians, No. | Movers, % | Moving to Rural, % | Moving to Metropolitan, % | |
| 1 (M) | 354,823 | 17 | 6 | 94 | 428,357 | 9 | 7 | 93 |
| 2 (M) | 127,524 | 16 | 15 | 85 | 161,661 | 8 | 17 | 83 |
| 3 (M) | 55,284 | 17 | 20 | 80 | 70,986 | 9 | 25 | 75 |
| 4 (R) | 21,937 | 17 | 22 | 78 | 30,442 | 10 | 30 | 70 |
| 5 (R) | 10,329 | 18 | 32 | 68 | 14,528 | 8 | 45 | 55 |
| 6 (R) | 20,053 | 20 | 29 | 71 | 28,736 | 12 | 38 | 62 |
| 7 (R) | 13,512 | 18 | 42 | 58 | 19,682 | 11 | 53 | 47 |
| 8 (R) | 2,262 | 23 | 36 | 64 | 3,045 | 17 | 48 | 52 |
| 9 (R) | 2,917 | 26 | 53 | 47 | 4,441 | 16 | 67 | 33 |
| Total | 608,641 | 16.9 | 12.2b | 87.8b | 761,878 | 8.9 | 16.3c | 83.7c |
RUCC=Rural-Urban Continuum Codes.
Original location postresidency; higher category indicates increasing rurality. M indicates metropolitan; R indicates rural.
Number moving metropolitan to rural: 8,354; number moving rural to metropolitan: 9,137.
Number moving metropolitan to rural: 6,504; number moving; rural to metropolitan: 6,391.
Note: Not shown here, analysis was repeated for family physicians only, but there were no differences of note.
Table 2 shows the associations between observed mobility (nonretention) rates and place characteristics for all rural counties. Nonretention rates were significantly worse (higher) in rural counties having 3 notable and interrelated characteristics: (1) lack of a hospital in that county (5.7%), (2) a smaller population (RUCC 8 or 9), and (3) lower physician supply (6.7%, per each PPR per 1,000 step). No additional tested place characteristics were significantly associated with nonretention levels within rural counties.
Table 2.
Factors Associated With Increased County-Level Mobility (Nonretention) of Rural Primary Care Physicians
| Factor | β Estimate (95% CI)a |
|---|---|
| Primary care physician supply (PPR per 1,000 residents) | −6.70 (−8.66 to −4.75)b |
| RUCC category | |
| 4 or 5 | −4.50 (−6.21 to −2.78)b |
| 6 or 7 | −3.09 (−4.64 to −1.54)b |
| No hospital in county | 5.74 (3.78 to 7.67)b |
| Long work commute (%) | −0.001 (−0.055 to 0.053) |
| Population uninsured (%) | 0.084 (−0.089 to 0.256) |
| Median house price (per $100,000) | −0.163 (−0.953 to 0.627) |
| Unemployment rate (%) | 0.160 (−0.083 to 0.403) |
| Population aged ≥65 years (%) | −0.082 (−0.216 to 0.052) |
| Population race/ethnicity (%) | |
| Non-Hispanic African American | 0.014 (−0.032 to 0.060) |
| Hispanic | 0.029 (−0.022 to 0.081) |
| Adjacent to metropolitan | −0.080 (−0.927 to 0.767) |
PPR = primary care physician–to-population ratio; RUCC = Rural-Urban Continuum Code.
Outcome measure is a score between 0 and 100 (eg, 20 = 20% nonretention).
P <.01.
Notes: The number of observations was 1,797. The R2 value was 0.25.
Table 3 shows the associations between observed moves of rural primary care physicians to metropolitan counties and both county-level place characteristics and individual-level characteristics. There were limited differences of rural-to-metropolitan mobility of younger and older primary care physicians. Working in a rural area adjacent to a metropolitan area was associated with increased risk of moving to a metropolitan location for both physician age-groups (P <.01), but in particular for older physicians (odds ratio = 1.28; 95% CI, 1.21–1.36). Younger family physicians were less likely to leave rural areas compared with other primary care physicians (odds ratio = 0.86; 95% CI, 0.82–0.90), but there was no difference for older physicians. Female physicians, international medical graduates, and those not born in rural areas were all more likely to move back to metropolitan locations irrespective of age, as were as older osteopathic physicians. Physicians located in areas with poorer supply (measured by PPR) were also significantly more likely to leave rural areas (younger: odds ratio = 0.77; 95% CI, 0.71–0.84; older: odds ratio = 0.75; 95% CI, 0.66–0.82).
Table 3.
Factors Associated With Observed Odds of Rural Primary Care Physicians Moving to Metropolitan Counties
| Factor | Odds Ratio (95% CI) | |
|---|---|---|
|
| ||
| Aged ≤45 y (n=70,568) | Aged 46–65 y (n=100,374) | |
| Female | 1.24 (1.18 to 1.30)a | 1.46 (1.37 to 1.54)a |
| Family physician | 0.86 (0.82 to 0.90)a | 0.99 (0.94 to 1.04) |
| Osteopathic | 1.02 (0.94 to 1.10) | 1.25 (1.15 to 1.35)a |
| International medical graduate | 1.65 (1.53 to 1.77)a | 1.41 (1.31 to 1.53)a |
| Health Professional Shortage Area (HPSA) | 1.05 (0.99 to 1.11) | 1.06 (1.00 to 1.13) |
| Born in rural area | 0.57 (0.53 to 0.62)a | 0.64 (0.59 to 0.70)a |
| Primary care physician supply (PPR per 1,000 residents) | 0.77 (0.71 to 0.84)a | 0.74 (0.66 to 0.82)a |
| No hospital in county | 1.09 (0.97 to 1.23) | 1.02 (0.89 to 1.17) |
| RUCC category (reference: 8 or 9) | ||
| 4 or 5 | 0.92 (0.83 to 1.03) | 0.90 (0.80 to 1.01) |
| 6 or 7 | 0.93 (0.84 to 1.03) | 0.98 (0.87 to 1.09) |
| Adjacent to metropolitan | 1.10 (1.05 to 1.16)a | 1.28 (1.21 to 1.36)a |
| Median household income (per $10,000) | 1.08 (1.03 to 1.14)a | 1.07 (1.02 to 1.13)a |
| Median house price (per $100,000) | 0.94 (0.89 to 1.00) | 1.07 (1.01 to 1.13)b |
| Unemployment rate (%) | 1.012 (1.002 to 1.032)b | 1.012 (0.995 to 1.029) |
| Population aged ≥65 years (%) | 0.984 (0.977 to 0.991)a | 1.004 (0.996 to 1.013) |
| Population race/ethnicity (%) | ||
| Non-Hispanic African American | 1.000 (0.997 to 1.002) | 1.005 (1.002 to 1.008)a |
| Hispanic | 1.004 (1.001 to 1.007)b | 1.003 (1.000 to 1.006) |
PPR = primary care physician–to-population ratio; RUCC = Rural-Urban Continuum Code.
P <.01.
P <.05.
County-level demographics were also related to odds of moving into metropolitan areas. Higher house prices and areas with larger numbers of African American residents were significantly associated with greater mobility for older physicians only, whereas higher household income was consistently associated with increased odds of mobility. Younger physicians had a higher risk of mobility only in areas with smaller numbers of older residents, higher unemployment, and greater numbers of Hispanic residents.
DISCUSSION
We found that increased rural primary care physician mobility was strongly linked with interrelated county-level characteristics of poorer physician supply, less population, and lack of a hospital, but not with county-level economic demographic measures. Overall, biennial mobility rates between counties of different rurality varied between 17% (for physicians aged 45 or younger) and 9% (for those aged 45–64). Individual physicians more often left rural areas if they were female, international medical graduates, not of rural origin, or working in counties adjacent to metropolitan areas.
Primary care physician workforce supply disparities between rural and metropolitan areas remain a major problem nationwide. The National Health Service Corps is a key program attempting to address this problem, financing more than 9,000 clinicians to work in underserved areas, with a further 1,100 in the training pipeline. Federal and state officials are perpetually seeking to address the shortage of rural physicians using policy levers such as loan forgiveness, small business incentives, and scholarships. This study’s evidence can help evaluate the effectiveness of these programs and refine future iterations.
Rural populations experience mobility of existing physicians as supply departure (turnover). Irrespective of where the physician is moving to, local rural residents experience a considerable loss of supply to their community. Furthermore, unlike the case in larger metropolitan areas and practices, this loss is not easily absorbed by nearby services in small populations of low density. Of great concern are the higher mobility rates and risk of leaving rural practice altogether, irrespective of age, of physicians who work in counties with poorer supply (lower PPR). These results are consistent with those of other non–rural-specific studies1,29 but highlight the difficult battle to improve physician availability for small rural communities. Rural areas that can least afford to lose physicians are those dealing with difficulties of increased mobility. Improved retention of rural physicians in these communities remains a target of health policies.
The higher nonretention of the existing rural physician workforce in the most remote rural communities (those in RUCC categories 8 and 9: population <2,500) and counties without a hospital is likely more problematic because of a lack of alternative service choices for these populations. Targeted policy support to rural physicians in these small and often isolated communities, who are likely struggling without a critical mass of other health professionals nearby, is needed.
Our results further highlight the difficulty of retaining both female and non–rural-origin physicians when they do initially spend time in a rural area.38 Older osteopathic-trained physicians also had significantly higher odds of leaving rural practice, perhaps because of increased initial uptake of rural practice in their early career stages.39
Much of the medical literature on rural retention relates to professional issues, whereas the social sciences literature on migration patterns and population mobility mostly relates to environmental aspects. In this study, somewhat surprisingly, we did not find higher rates of turnover among physicians working in poorer rural communities, measured by household income and median house prices, although higher unemployment was significantly associated with lower retention. Economic aspects appear to have only a minor role in mobility decisions of primary care physicians compared with geographic aspects of population size and hospital access. Stronger economic aspects, in particular, were expected to be important when choosing between rural locations40—for example, given a choice between a rural town with strong growth vs a rural town with no growth or even slowly dying, the latter would deter most individuals; however, this pattern was not reflected in the results of this study over and above physician shortage levels.
Fringe rural locations, defined as “adjacent to metropolitan,” were similarly likely to have workforce mobility as other, nonadjacent rural counties; however, rural physicians in these locations were more likely to be observed leaving rural practice, particularly if they were older. With the likely increased proximity to metropolitan areas, it is not known whether these moves coincide with the physician’s family also moving to metropolitan areas or whether the physician is perhaps able to commute without the need for his or her family to also move.
The main limitation of this study is its reliance on the accuracy of location information in the AMA data set. Our study used a biennial approach to smooth out some of the issues regarding timeliness of location changes within the AMA data, which could miss short-term mobility of less than 2 years, but it also remains questionable how sensitive this data set is to the longitudinal movement of physicians. In addition, many physicians practice in more than 1 location, which may cut across multiple counties, but this analysis has used only their main work location. Locations were aggregated to the county level, which will undercount the true level of all physician mobility down to the practice level. Lastly, physicians older than 65 years were excluded from this study, which may limit the totality of our results.
This study is strengthened by the removal of resident physicians from all analysis, as well as the separation of key mobility results by age. As confirmed in Figure 1, younger physicians change work locations more frequently compared with older physicians, and the reasons for moving are likely to be different too. Residents (excluded in this study) may be required to undertake short-term placements in rural areas; thus, moves into and out of rural areas can be observed that are totally unrelated to push and pull factors. Shortly after residency, physicians may choose initial employment locations based more on availability than on preference until their preferred option becomes available.
Increasing rural workforce supply and retaining the existing rural physician workforce remain key issues of the United States. Our study provides national-level evidence that enables rural health workforce planners and policymakers to better understand which characteristics are most strongly associated with physician geographic mobility each year, how often moves occur, and where physicians might move to and from. In addition, the strengths of key community-level push and pull factors have been measured against observed mobility behavior. Such evidence may be useful in guiding more effective targeting of rural health policies and workforce planning and incentives, as well as highlighting the specific needs of the most vulnerable communities.
Footnotes
Conflicts of interest: authors report none.
Prior presentations: Wingrove P, McGrail M, Petterson S, Bazemore A, “Mobility and Retention of Rural Primary Care Physicians: Evidence From 2000–2014” was previously presented at the North American Primary Care Research Group (NAPCRG) Annual Meeting; October 24–28, 2015; Cancun, Mexico.
Supplementary materials: Available at http://www.AnnFamMed.org/content/15/4/322/suppl/DC1/.
Funding support: Matthew McGrail, lead author, received a visiting scholar grant to the Robert Graham Center for Policy Studies in Family Medicine and Primary Care, Washington, DC, through the Australian Primary Health Care Research Institute, Canberra Australia.
References
- 1.Ricketts TC. The migration of physicians and the local supply of practitioners: a flve-year comparison. Acad Med. 2013;88(12): 1913–1918. [DOI] [PubMed] [Google Scholar]
- 2.Jones C, Parker T, Ahearn M, Mishra A, Variyam J. Health Status and Health Care Access of Farm and Rural Populations. Washington, DC: United States Department of Agriculture, Economic Research Service; 2009. Economic Information Bulletin Number 57. [Google Scholar]
- 3.Dussault G, Franceschini MC. Not enough there, too many here: understanding geographical imbalances in the distribution of the health workforce. Hum Resour Health. 2006;4:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. Increasing Access to Health Workers in Remote and Rural Locations Through Improved Retention: Global Policy Recommendations. Geneva, Switzerland: WHO Press; 2010. [PubMed] [Google Scholar]
- 5.Weinhold I, Gurtner S. Understanding shortages of sufflcient health care in rural areas. Health Policy. 2014;118(2):201–214. [DOI] [PubMed] [Google Scholar]
- 6.Ricketts TC, Randolph R. Urban-rural flows of physicians. J Rural Health. 2007;23(4):277–285. [DOI] [PubMed] [Google Scholar]
- 7.Rosenblatt RA, Hart LG. Physicians and rural America. West J Med. 2000;173(5):348–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Petterson SM, Phillips RL, Jr, Bazemore AW, Koinis GT. Unequal distribution of the U.S. primary care workforce. Am Fam Physician. 2013;87(11). [PubMed] [Google Scholar]
- 9.Fordyce M, Chen F, Doescher M, Hart L. 2005 Physician Supply and Distribution in Rural Areas of the United States. Seattle, WA: WWAMI Rural Health Reseach Center; 2007. [Google Scholar]
- 10.Buchbinder SB, Wilson M, Melick CF, Powe NR. Estimates of costs of primary care physician turnover. Am J Manag Care. 1999;5(11): 1431–1438. [PubMed] [Google Scholar]
- 11.Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83(3):457–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rabinowitz HK, Diamond JJ, Markham FW, Santana AJ. The relationship between matriculating medical students’ planned specialties and eventual rural practice outcomes. Acad Med. 2012;87(8):1086–1090. [DOI] [PubMed] [Google Scholar]
- 13.Rabinowitz HK, Diamond JJ, Markham FW, Santana AJ. Retention of rural family physicians after 20–25 years: outcomes of a comprehensive medical school rural program. J Am Board Fam Med. 2013; 26(1):24–27. [DOI] [PubMed] [Google Scholar]
- 14.Rabinowitz HK, Petterson S, Boulger JG, et al. Medical school rural programs: a comparison with international medical graduates in addressing state-level rural family physician and primary care supply. Acad Med. 2012;87(4):488–492. [DOI] [PubMed] [Google Scholar]
- 15.Scott A, Witt J, Humphreys J, et al. Getting doctors into the bush: general practitioners’ preferences for rural location. Soc Sci Med. 2013;96(1):33–44. [DOI] [PubMed] [Google Scholar]
- 16.Wilson NW, Couper ID, De Vries E, Reid S, Fish T, Marais BJ. A critical review of interventions to redress the inequitable distribution of healthcare professionals to rural and remote areas. Rural Remote Health. 2009;9(2):1060. [PubMed] [Google Scholar]
- 17.United States Department of Health and Human Services. National Health Service Corps. 2015; http://www.nhsc.hrsa.gov/ Accessed May 18, 2015.
- 18.Foreign Physicians: Data on Use of J-1 Visa Waivers Needed to Better Address Physician Shortages. Washington, DC: United States Government Accountability Office; 2006. Report GAO 07-52. [Google Scholar]
- 19.Opoku ST, Apenteng BA, Lin G, Chen LW, Palm D, Rauner T. A comparison of the J-1 visa waiver and loan repayment programs in the recruitment and retention of physicians in rural Nebraska. J Rural Health. 2015;31(3):300–309. [DOI] [PubMed] [Google Scholar]
- 20.Simini F, González MC, Maritan A, Barabási A-L. A universal model for mobility and migration patterns. Nature. 2012;484(7392):96–100. [DOI] [PubMed] [Google Scholar]
- 21.van Zanten M, Boulet J, Norcini J. Ethical integration of internationally educated health professionals: Ethical and regulatory contexts – report from the United States. Presented at: 13th International Health Workforce Collaborative; October 24–26, 2011; Brisbane, Australia. [Google Scholar]
- 22.McDonald JT, Worswick C. The migration decisions of physicians in Canada: the roles of immigrant status and spousal characteristics. Soc Sci Med. 2012;75(9):1581–1588. [DOI] [PubMed] [Google Scholar]
- 23.Rajbhandary S, Basu K. Interprovincial migration of physicians in Canada: where are they moving and why? Health Policy. 2006;79(2–3):265–273. [DOI] [PubMed] [Google Scholar]
- 24.Vanasse A, Ricketts TC, Courteau J, Orzanco MG, Randolph R, Asghari S. Long term regional migration patterns of physicians over the course of their active practice careers. Rural Remote Health. 2007;7(4):812. [PubMed] [Google Scholar]
- 25.McGrail MR, Humphreys JS. Geographical mobility of general practitioners in rural Australia. Med J Aust. 2015;203(2):92–96. [DOI] [PubMed] [Google Scholar]
- 26.Inoue K, Matsumoto M, Toyokawa S, Kobayashi Y. Transition of physician distribution (1980–2002) in Japan and factors predicting future rural practice. Rural Remote Health. 2009;9(2):1070. [PubMed] [Google Scholar]
- 27.Ricketts TC, Randolph R. The diffusion of physicians. Health Aff (Millwood). 2008;27(5):1409–1415. [DOI] [PubMed] [Google Scholar]
- 28.Kindig DA, Schmelzer JR, Hong W. Age distribution and turnover of physicians in nonmetropolitan counties of the United States. Health Serv Res. 1992;27(4):565–578. [PMC free article] [PubMed] [Google Scholar]
- 29.Matsumoto M, Inoue K, Bowman R, Noguchi S, Kajii E. Physician scarcity is a predictor of further scarcity in US, and a predictor of concentration in Japan. Health Policy. 2010;95(2–3):129–136. [DOI] [PubMed] [Google Scholar]
- 30.Cameron PJ, Este DC, Worthington CA. Physician retention in rural Alberta: key community factors. Can J Public Health. 2010;101(1): 79–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Han GS, Humphreys JS. Overseastrained doctors in Australia: community integration and their intention to stay in a rural community. Aust J Rural Health. 2005;13(4):236–241. [DOI] [PubMed] [Google Scholar]
- 32.McGranahan DA. Landscape influence on recent rural migration in the U.S. Landsc Urban Plan. 2008;85(3–4):228–240. [Google Scholar]
- 33.Rappaport J. Moving to nice weather. Reg Sci Urban Econ. 2007;37(3):375–398. [Google Scholar]
- 34.Gosnell H, Abrams J. Amenity migration: diverse conceptualizations of drivers, socioeconomic dimensions, and emerging challenges. GeoJournal. 2011;76(4):303–322. [Google Scholar]
- 35.McGrail MR, Humphreys JS, Joyce C, Scott A, Kalb G. Rural amenity and medical workforce shortage: Is there a relationship. Geogr Res. 2011;49(2):192–202. [Google Scholar]
- 36.United States Department of Agriculture – Economic Research Service. Rural-Urban Continuum Codes - documentation and map. https://www.ers.usda.gov/data-products/rural-urban-continuum-codes/documentation/ Published 2013. Accessed Jan 18, 2017.
- 37.Verardi V, Croux C. Robust regression in Stata. Stata J. 2009;9(3): 439–453. [Google Scholar]
- 38.McGrail MR, Humphreys JS, Joyce CM. Nature of association between rural background and practice location: a comparison of general practitioners and specialists. BMC Health Serv Res. 2011;11:63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fordyce MA, Doescher MP, Chen FM, Hart LG. Osteopathic physicians and international medical graduates in the rural primary care physician workforce. Fam Med. 2012;44(6):396–403. [PubMed] [Google Scholar]
- 40.Argent N, Tonts M, Jones R, Holmes J. The amenity principle, internal migration, and rural development in Australia. Ann Assoc Am Geogr. 2014;104(2):305–318. [Google Scholar]