Abstract
Stress has been extensively studied as a psychosomatic factor associated with breast cancer. This study aims to review the prevalence of post-traumatic stress disorder (PTSD), its associated risk factors, the role of predicting factors for its early diagnosis/prevention, the implications for co-treatment, and the potential links by which stress could impact cancer risk, by closely examining the literature on breast cancer survivors. The authors systematically reviewed studies published from 2002 to 2016 pertaining to PTSD, breast cancer and PTSD, and breast cancer and stress. The prevalence of PTSD varies between 0% and 32.3% mainly as regards the disease phase, the stage of disease, and the instruments adopted to detect prevalence. Higher percentages were observed when the Clinician Administered PTSD Scale was administered. In regard to PTSD-associated risk factors, no consensus has been reached to date; younger age, geographic provenance with higher prevalence in the Middle East, and the presence of previous cancer diagnosis in the family or relational background emerged as the only variables that were unanimously found to be associated with higher PTSD prevalence. Type C personality can be considered a risk factor, together with low social support. In light of the impact of PTSD on cognitive, social, work-related, and physical functioning, co-treatment of cancer and PTSD is warranted and a multidisciplinary perspective including specific training for health care professionals in communication and relational issues with PTSD patients is mandatory. However, even though a significant correlation was found between stressful life events and breast cancer incidence, an unequivocal implication of distress in breast cancer is hard to demonstrate. For the future, overcoming the methodological heterogeneity represents one main focus. Efficacy studies could help when evaluating the effect of co-treating breast cancer and post-traumatic stress symptoms, even if all the criteria for a Diagnostic and Statistical Manual of Mental Disorders diagnosis are not fulfilled.
Keywords: PTSD, post-traumatic stress disorder, breast cancer, disease management
Background
When women affected by breast cancer are asked to recall the very moment of their diagnosis and cancer experience, a series of symptoms may appear including hyper-arousal, emotional numbness, the sensation of the situation happening to a person other than self, and intrusive thinking together with nightmares and flashbacks that guide the clinician to understand how traumatic the cancer diagnosis was across the life span.
The Diagnostic and Statistical Manual of Mental Disorders (DSM) version IV recognized that it is possible for a person to receive a diagnosis of post-traumatic stress disorder (PTSD) as a consequence of life-threatening disease.1 In the newer DSM-V, a medical disease such as cancer is considered a traumatic event only when it is sudden and “catastrophic”.2
The prevalence of PTSD diagnosis in breast cancer is higher than that in colorectal, head and neck, and prostate cancers but lower than that in brain, gynecological, and hematological cancers.3
It is important that such a psychological disorder is detected in order to implement appropriate short- and long-term health care policies and to sustain adherence and compliance in patients whose psychological symptoms cause defects in information processing, problem-solving abilities, decision-making processes, and in communication, relational, and social issues.3,4
The prevalence of PTSD symptoms varies hugely on the basis of diagnostic criteria considered, psychological instruments applied in research studies, disease phase, and stage in which the prevalence study is conducted.4,5
This paper aims to investigate the literature regarding the prevalence of PTSD in breast cancer patients considering the associated sociodemographic and comorbidity risk factors. In addition, it summarizes the potential links and proposed mechanisms by which stress impacts cancer risk, the implication for co-treatment of cancer and related PTS symptomatology, and the role played by predictive factors for early diagnosis and prevention.
Methods
Search strategy to identify review articles for this analysis
To identify the relevant review literature, we chose a 14-year period (December 2002–December 2016). The main reason for this period is that one of the most frequently cited review papers on PTSD in breast cancer patients6 first appeared at the beginning of the 21st century.
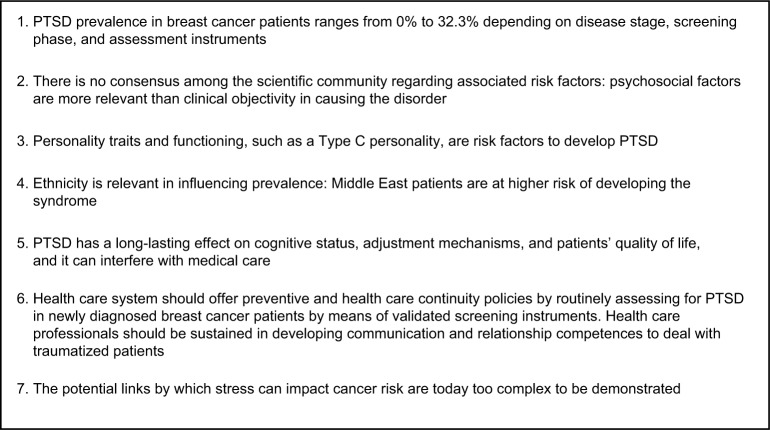
We used the OVID bibliographic software to search three computerized databases: OVID MEDLINE(R), PsycINFO, and SCOPUS. OVID allows multiple searches and deletion of duplicates. Various combinations of database-specific controlled vocabulary (subject headings) were used, supplemented by keywords, title, and abstract terms for the concepts and synonyms relating to PTSD and breast cancer. Keywords used were cancer AND PTSD, cancer AND post-traumatic stress disorder, breast cancer AND stress, breast cancer AND PTSD. The search was limited to the English language and resulted in 520 papers (Figure 1). From these, we extracted 23 relevant papers as described in Table 1.
Figure 1.
Flowchart of literature search.
Table 1.
List of the papers included in the review by themes discussed
| Title | Reference | Year of publication | Prevalence of PTSD in breast cancer | Associated sociodemographic and comorbidity risk factors | Potential links and proposed mechanisms by which stress impacts cancer risk | Role of predicting factors for early diagnosis/prevention of PTSD | Implications for co-treatment | Overall rating of the quality of papers** |
|---|---|---|---|---|---|---|---|---|
| Post-traumatic stress disorder after cancer diagnosis in adults: a meta-analysis | Swartzman et al3 | 2017 | X | X | – | |||
| PTSD symptoms as a consequence of breast cancer diagnosis: clinical implications | Arnaboldi et al4 | 2014 | X | Moderate | ||||
| Post-traumatic stress symptoms in breast cancer patients: temporal evolution, predictors, and mediation | Perez et al5 | 2014 | X | X | Moderate | |||
| Post-traumatic stress disorder following cancer. A conceptual and empirical review |
Kangas et al6 | 2002 | – | |||||
| Distress, psychiatric syndromes, and impairment of function in women with newly diagnosed breast cancer | Hegel et al8 | 2006 | X | X | High | |||
| Prevalence of acute and post-traumatic stress disorder and comorbid mental disorders in breast cancer patients during primary cancer care: a prospective study | Mehnert and Koch9 | 2007 | X | X | High | |||
| PTSD diagnosis, subsyndromal symptoms, and comorbidities contribute to impairment for breast cancer survivors | Shelby et al10 | 2008 | X | X | X | Moderate | ||
| Racial disparities in post-traumatic stress after diagnosis of localized breast cancer: the BQUAL study | Vin-Raviv et al11 | 2013 | X | X | High | |||
| Psychological adjustment 1 year after the diagnosis of breast cancer: a prototype study of delayed post-traumatic stress disorder | Elklit and Blum13 | 2011 | X | X | High | |||
| How traumatic is breast cancer? Post-traumatic stress symptoms (PTSS) and risk factors for severe PTSS at 3 and 15 months after surgery in a nationwide cohort of Danish women treated for primary breast cancer | O’Connor et al12 | 2011 | X | High | ||||
| Post-traumatic stress in women with breast cancer | Alkhyatt et al14 | 2012 | X | X | Moderate | |||
| Prevalence of post-traumatic stress disorder among breast cancer patients: a meta-analysis | Wu et al15 | 2016 | X | X | – | |||
| Post-traumatic stress disorder associated with cancer diagnosis and treatment | Andrykowski et al17 | 2010 | X | X | X | – | ||
| Post-traumatic stress disorder and cancer risk: a nationwide cohort study | Gradus et al18 | 2015 | X | X | High | |||
| Stressful life events and risk of breast cancer in 10,808 women: a cohort study | Lillberg et al19 | 2003 | X | X | High | |||
| Stress and breast cancer: from epidemiology to molecular biology | Antinova et al20 | 2011 | X | – | ||||
| Do stress-related psychosocial factors contribute to cancer incidence and survival? | Chida et al21 | 2008 | X | X | High | |||
| Status of oral ulcerative mucositis and biomarkers to monitor post-traumatic stress disorder effects in breast cancer patients | Loo et al22 | 2013 | X | Moderate | ||||
| Cancer and post-traumatic stress disorder: diagnosis, pathogenesis, and treatment considerations | Rustad et al23 | 2012 | X | – | ||||
| Correlates of post-traumatic stress symptoms and growth in cancer patients: a systematic review and meta-analysis | Shand et al24 | 2015 | X | X | – | |||
| Post-traumatic stress symptoms in cancer survivors: relationship to the impact of cancer scale and other associated risk factors | Hahn et al16 | 2015 | X | Moderate | ||||
| Elucidating pretreatment cognitive impairment in breast cancer patients: the impact of cancer-related post-traumatic stress | Hermelink et al25 | 2015 | X | High | ||||
| Perceived cognitive impairment in Chinese patients with breast cancer and its relationship with post-traumatic stress disorder symptoms and fatigue | Li et al26 | 2015 | X | Moderate |
Notes:
Only for randomized controlled trial and cohort studies. The “–” symbols indicate that the paper was not evaluated for quality.
Abbreviation: PTSD, post-traumatic stress disorder.
SR, PA, and a trained graduate student (CC) reviewed the titles and abstracts from the OVID search to extract relevant papers. When we failed to reach consensus, GP was consulted to review the titles and abstracts of papers. We extracted only those papers with a major focus on factors implicated in PTSD in breast cancer patients, the associated sociodemographic and comorbidity risk factors, and potential links and proposed mechanisms by which stress impacts cancer risk in adult breast cancer patient populations.
We excluded papers in which 1) the focus was not stress related, 2) the primary outcomes were not addressed in the breast population, and 3) only pediatric populations were included. We also excluded papers focused on small qualitative studies, theoretical contributions, and other professional practice guidelines. However, we included other high-quality systematic reviews published after 2002.
Quality of psycho-oncology papers
One goal of our review was to characterize the overall quality of the papers dealing with PTSD in breast cancer patients. We did this by describing the quality of papers by 1) using a systematic and comprehensive search strategy and by 2) controlling for the effects of lesser quality studies on results. We referred to the Cochrane Handbook for Systematic Reviews of Interventions.7
A subjective assessment of methodological quality for randomized controlled trials (RCTs) and observational studies included was conducted by three authors (PA, SR, and CC) on the following items, in which each component was categorized as low, moderate, or high: likelihood of selection bias, study design, control of important confounders, blinding, data collection methods, withdrawals and dropouts, and overall rating. The overall rating is described in Table 1. We excluded studies evaluated as “low.”
Search strategy
Our first analysis examines whether the search strategy used to identify relevant studies could be considered systematic and comprehensive. A systematic search strategy is one that includes a methodology that allows readers to gain a comprehensive understanding of the study. A systematic review should, at the very least, specify the study design, setting, enrollment criteria, and primary and secondary objectives and related end points.
Based on these considerations, we decide to select randomized studies, as well as cohort studies with a good study design quality and review/meta-synthesis that included relevant controlled studies.
Quality controls
Our second analysis examines how studies were selected for inclusion in the review. We selected only those papers checked that met certain methodological quality criteria.
We sorted papers into three categories: 1) those that included both RCTs and nonrandomized intervention studies, 2) those that included only RCTs, and 3) those that included systematic reviews.
For that which regards the risk factors associated with PTSD that emerged from the literature systematic review, we grouped them into three broad categories: clinical oncology variables such as tumor characteristics, disease stage, and type of surgery; psychological variables such as previous lifetime traumas or concomitant psychological/psychiatric symptoms; and sociodemographic variables such as age at evaluation, level of education, socioeconomic status, and race/ethnicity.
Results
PTSD and post-traumatic stress symptoms in breast cancer patients: whether cancer can function as a traumatic stressor
In a meta-analysis by Swartzman et al,3 the summary proportion (%) of patients showing PTSD after breast cancer diagnosis considering 38 studies was around 10% (8%–12.5%). The prevalence of PTSD appeared high if compared to other mental disorders in cancer setting.
Studies included in our review varied greatly mainly as regard to the disease phase in which prevalence was studied, to the stage of disease and to instruments adopted to detect prevalence as described in Table 2: for instance, Hegel et al8 studied the prevalence of PTSD in 236 newly diagnosed breast stage I–II or III cancer patients at the time of their presurgical consultation and found a prevalence of 10% of PTSD. In the study by Mehnert and Koch,9 studying 127 breast cancer patients postsurgery, it was found that only 2.4% patients met the criteria for a mild-to-moderate cancer-related PTSD.
Table 2.
PTSD and symptoms prevalence, region in which the study took place, patients’ ethnicity, number of patients, illness phase, illness stage, and screening instruments
| Reference | Region of the study | Patients’ ethnicity | Number of patients | Illness phase | Illness stage | PTSD prevalence | PTSD symptoms prevalence | Instruments |
|---|---|---|---|---|---|---|---|---|
| Hegel et al (2006)8 | USA | White, Asian | 236 | Presurgical consultation | Stages I, II, III | 10% | The four-item primary care PTSD screen (PC-PTSD) | |
| Mehnert and Koch (2007)9 | Germany | Not specified | 127 | Postsurgery and post-treatment | 2.4% | Structured Clinical Interview for DSM-IV*, IES-R, PCL-C | ||
| Shelby et al (2008)10 | USA | Not specified | 74 | Diagnosis and 18 months later | Stages II and III (node positive) | 3%–14% | Upward of 50% | PTSD Checklist-Civilian Version |
| Elklit and Blum (2011)13 | Denmark | White | 64 | 12 months after diagnosis | 13% | Upward to 75% | Harvard Trauma Questionnaire (HTQ) | |
| O’Connor et al (2011)12 | Denmark | Not immigrant, immigrant | 3343 | 3 and 15 months after surgery | Primary breast cancer | 20.1% 3 months postsurgery, 14.3% 15 months postsurgery | IES | |
| Alkhyatt et al (2012)14 | Iraq | Not specified | 100 | 4–12 months post–cancer treatment | Early stage | 3% | 5% | IES |
| Vin Raviv et al (2013)11 | USA | Asian, Afro-American, White | 1139 | Diagnosis, post-treatment | Nonmetastatic breast cancer | 23% at diagnosis; 16.5% at 4-month follow-up | IES | |
| Arnaboldi et al (2014)4 | Italy | White | 150 | Within 30 days after diagnosis and at 2 years follow-up | Women candidated to a mastectomy procedure | 20% prevalence for intrusion symptoms, 19.1% for avoidance symptoms | IES | |
| Swartzman et al (2017)3 | UK | Caucasian, Middle East, North America | 16,755 | Breast cancer patients in 38 PTSD prevalence studies | 10% | DSM-IV Criteria* | ||
| Wu et al (2016)15 | USA | Caucasian, non-Caucasian | 14,603 | Meta-analysis: prevalence of PTSD among breast cancer patients | 34 observational studies | 0%–32.3% (overall 9.6%) | Various instruments studied on the basis of their PTSD detection rate |
Notes:
DSM-IV criteria for PTSD: the person must have been exposed to, or witnessed a traumatic event that involved actual or threatened death or a threat to the physical integrity of oneself or others and which invoked intense fear, helplessness, or horror in the recipient (Criterion A). Criterion B requires that the individual experiences either intrusive memories, nightmares, a sense of reliving the traumatic event, or psychological and physiological distress when reminded the event. Criterion C requires at least three of avoidance of thoughts, feelings, or reminders of the trauma, inability to recall aspects of the trauma, withdrawal from others, emotional numbing or a sense of foreshortened future. Criterion D stipulates the presence of at least two of the following symptoms: insomnia, irritability, concentration difficulties, hypervigilance, or exaggerated startle response. These symptoms must persist for at least 1 month following exposure to the traumatic event (Criterion E), and they must cause significant impairment to the individual’s functioning (Criterion F).
Abbreviations: DSM-IV, Diagnostic and Statistical Manual of Mental Disorders version IV; IES, Impact of Event Scale; IES-R, IES-Revised; PCL-C, PTSD Checklist-Civilian Version; PTSD, post-traumatic stress disorder.
Similarly, Shelby et al10 studied a sample of 74 breast cancer patients with node-positive disease (stages II and III), treated with breast-conserving surgery at diagnosis/treatment and 18 months later. Diagnostic PTSD rates were demonstrated to be low (3%–14%) but PTSD subsyndromal symptomatology, falling short of the diagnostic criteria of the DSM-IV, may occur in upward of 50% of patients. A higher percentage was found in the study by Vin-Raviv et al,11 where the 23% of 1139 women with newly diagnosed localized breast cancer experienced PTSD symptoms. These symptoms decreased over time, 16.5% had PTSD symptoms at 4-month follow-up; 12.6% at the second follow-up. Also, other studies confirmed these results.4,5,10,12
In a follow-up study by Elklit and Blum,13 the prevalence of PTSD symptoms 1 year after early breast cancer diagnosis was ~13% of the patients, while the large Danish study by O’Connor et al12 showed that in a sample of 3343 Danish women after surgery, the prevalence of PTSD symptoms was 20.1% at 3 months and 14.3% at 15 months.
Alkhyatt et al14 at the Nuclear Medicine Hospital in Iraq found relatively low rates of cancer-related PTSD: 5% at any time post–cancer diagnosis (up to 20 months) with liberal criteria and only 3% with more stringent criteria in a sample of 100 women aged 25–75 years with early-stage breast cancer and being 4–12 months post–cancer treatment.
Arnaboldi et al4 studied the prevalence of PTSD intrusion and avoidance symptomatology in the first 30 days after breast cancer diagnosis, with 20% prevalence for intrusion symptoms and 19.1% for avoidance symptoms.
For that which regards PTSD assessment strategies and PTSD prevalence, Wu et al15 focused on studying the overall prevalence estimate of PTSD among breast cancer patients and the prevalence estimates related to specific PTSD diagnosis tools by means of a meta-analysis. They found that the pooled prevalence of PTSD was 9.6% (95% CI=7.9%–11.5%). Studies that used the Clinician Administered PTSD Scale method alone yielded much higher prevalence (19%, 95% CI=13.1%–25.5%) than third or fourth edition Structured Clinical Interview for Diagnostic and Statistical Manual method alone (3.0%, 95% CI=2.2%–3.9%). Prevalence estimates for studies that used the methods PTSD Checklist-Civilian Version cutoff and Impact of Event Scale cutoff were 7.0% (95% CI=3.9%–10.8%) and 15.1% (95% CI=12.3%–18.2%), respectively.
Outline of associated sociodemographic and comorbidity risk factors
The literature cites different kinds of PTSD-associated sociodemographic and comorbidity risk factors but until now no consensus is reached about the role they play in association to PTSD development as it emerges in Table 3.
Table 3.
Variables associated to PTSD prevalence in breast cancer patients cited by study
| Variables | Association to PTSD prevalence | No association to PTSD prevalence |
|---|---|---|
| Clinical oncology variables | ||
| Time since diagnosis | Swartzman et al (2017)3, Kangas et al (2002)6 | Vin-Raviv et al (2013)11, Hahn et al (2015)16 |
| Type of treatment | Swartzman et al (2017)3, Kangas et al (2002)6 | Vin-Raviv et al (2013)11, Hahn et al (2015)16 |
| Extent of disease | O’Connor et al (2011)12, Shelby et al (2008)10, Kangas et al (2002)6 | Vin-Raviv et al (2013)11, Hahn et al (2015)16 |
| Type of surgery | Shelby et al (2008)10, Kangas et al (2002)6 | Vin-Raviv et al (2013)11 |
| Recurrence | Kangas et al (2002)6 | |
| Positive cancer family history | Arnaboldi et al (2014)4 | |
| Psychological variables | ||
| Comorbid psychological disorders | O’Connor et al (2011)12, Mehnert and Koch (2007)9, Higgins and Green (2011)7 | |
| Prior life stressors | Kangas et al (2002)6, Hegel et al (2006)8 | Perez et al (2014)5 |
| Elevated psychological distress at diagnosis | Hegel et al (2006)8 | |
| Emotionally reactive treatment | Kangas et al (2002)6, Elklit and Blum et al (2011)13 | |
| Avoidant coping style | Kangas et al (2002)6, Elklit and Blumet al (2011)13, Perez et al (2014)5 | |
| Hopelessness/helplessness | Perez et al (2014)5 | |
| Type C personality | Perez et al (2014)5 | |
| Immature defense style | Elklit and Blum et al (2011)13 | |
| Negative affectivity | Elklit and Blum et al (2011)13 | |
| Poor social functioning | Kangas et al (2002)6 | |
| Reduced physical functioning | O’Connor et al (2011)12 | |
| Sociodemographic variables | ||
| Race/ethnicity | Wu et al15, Swartzman et al (2017)3, Vin-Raviv et al (2013)11 | Hahn et al (2015)16 |
| Age | Swartzman et al (2017)3, Vin-Raviv et al (2013)11, Perez et al (2014)5, Hahn et al (2015)16 | |
| Gender | Kangas et al (2002)6 | Hahn et al (2015)16 |
| Education | Kangas et al (2002)6 | |
| Income | O’Connor et al (2011)12, Hahn et al (2015)16 | |
| Employment status | Hahn et al (2015)16 |
Abbreviation: PTSD, post-traumatic stress disorder.
Mehnert and Koch9 reported that women diagnosed with cancer-related PTSD or acute stress disorder were more likely (OR [odds ratio]=22.2) to have a comorbid psychological disorder. In particular, a history of anxiety disorders seems to be significant in causing PTSD symptoms such as mood and substance use/dependence diagnoses. Furthermore, breast cancer patients with PTSD are significantly more likely to have a current mood (OR=8.44, 95% CI=2.08–34.35) or anxiety disorder other than PTSD (OR=7.33, 95% CI=1.37–39.18).10
This evidence is supported by Hegel et al,8 in whose sample, prior psychiatric illness and/or treatment was relatively common in PTSD breast cancer patients. PTSD breast cancer patients seem to differ from others in criterion A life events, F (2, 71)=3.85, p<03, rather than in total number of stressful life events.10
The fact of having been physically attacked/abused influences PTSD prevalence rates10,16 with higher prevalence in patients who were abused or physically attacked.
Perez et al5 did not find such a correlation between prior trauma and PTSD prevalence although prior traumatic events were related to having less social support. Positive cancer family and positive cancer relational history are associated with higher levels of PTSD symptoms.4 With the expression “positive family history” authors referred to the presence of other cancer diagnosis in the family history or in significant others.
As regards medical variables, extent of disease and type of surgery were demonstrated to be the risk factors in developing both PTSD and subsyndromal PTSD,10 but there is mixed evidence pertaining to the predictive value of medical variables: in some studies, more advanced disease stages, recency of treatment at assessment, and experiencing at least one recurrence are associated with more severe PTSD symptoms, while in other studies this influence did not emerge.11 O’Connor et al12 in their nationwide inception cohort of Danish women treated for primary breast cancer found that the main predictors of severe post-traumatic stress symptoms at 15 months postsurgery were low social status, previous physical and mental illness, axillary lymph node involvement (>3), and reduced physical functioning at 3 months postsurgery.
From the review by Swartzman et al,3 it emerges that type of treatment influences the prevalence of PTSD diagnosis with higher prevalence during chemotherapy. Time since diagnosis also influences PTSD prevalence (the more the time the lower the prevalence).
It emerges also that geographic provenance of patients seems to influence PTSD prevalence with the highest prevalence in the Middle East rather than Europe, North America, and Asia3. Non-Caucasian breast cancer patients were more likely to be diagnosed with PTSD than Caucasians.17
Younger age is also associated with higher prevalence: for each additional year increase, PTSD estimates would be predicted to decrease by 0.3%.6 The same result concerning age was supported by Perez et al5 and Wu et al.15
In the hierarchical multiple regression analysis by Elklit and Blum,13 immature defense style, emotional coping, avoidant behavior, and negative affectivity were all implicated as predicting variables in PTSD severity 1 year after diagnosis.
Summary of potential links and proposed mechanisms by which stress impacts cancer risk
Besides the risk of developing PTSD symptoms after the diagnosis of cancer, several researchers suggested the possibility of an inverse correlation, but the reported studies conflict in their findings.
PTSD does not turn out as a risk factor for cancer development in the cohort study by Gradus et al.18 A total of 4,131 adults with PTSD and no history of cancer were included, and after a 7-year follow-up the evidence showed no significant higher incidence of cancer in general, and breast cancer in particular. These results seem to exclude a correlation between PTSD and breast cancer development, although the study did not focus only on breast cancer but included all types of cancer. It should be stressed, however, that the results from other studies seem more significant, as the researchers tried to identify one or more variables as responsible of the interaction between psychosocial distress and cancer development.19–21
Stressful life events
The results by Lillberg et al19 put in evidence the role of stressful events in the incidence of breast cancer. Among 10,808 women included in the study, 180 had a breast cancer diagnosis within the 15 years of the follow-up. A significant correlation was found between stressful life events, such as a divorce/separation, the loss of a husband or a close friend, and breast cancer incidence.19
But what are the mechanisms by which psychosocial distress affects breast cancer development?
Cortisol
Etiologic research has underlined the implications of certain hormones in tumorigenesis. The central nervous system responses may be affected by psychosocial stress, as well as the functions of hypothalamus, pituitary, and adrenal glands. Cortisol seems to play an important role especially in breast cancer development. During periods of higher stress, the cortisol levels are likely to be dysregulated and its presence in the organism is prolonged. Laboratory evidence has shown how cortisol alters the generation or the activity of estrogen; as estrogen appears to be implicated in breast tumorigenesis, it is conceivable to identify cortisol as a risk factor.20
Catecholamines, glucorticoids, and other stress hormones could vary the tumor microenvironment and they could activate oncogenic viruses.21
The results of the etiology studies are not easy to interpret, because of the type of study design and the method by which the exposure to stress has been measured.
Several observational studies support the hypothesis that exposure to psychological stress increases the chance of developing breast cancer.20
In conclusion, stress-related psychosocial factors seem to exert effects especially on the survival rates rather than on the incidence of the disease,21 even though an unequivocal implication of distress in breast cancer is hard to demonstrate. On this basis, it seems plausible that prolonged or cumulative exposure to some psychosocial-stress factors increases the risk of breast cancer and lowers the survival rate. In addition, psychosocial factors may affect cancer development in different ways, depending on the type of cancer.
Role of predicting factors for early diagnosis/prevention of PTSD in breast cancer
A number of factors may be potentially identified as predictors for an early diagnosis of PTSD including individual influences on psychological distress including biological parameters, personality traits, coping strategies, and social support.
At an individual level, it appears that level of distress positively correlates with personal history of previous high level of hormone serum of T3 and T4.22
As Loo et al22 reported “The majority of people with PTSD show a low level of cortisol and high levels of catecholamines in urine through the activation of the hypothalamic–pituitary–adrenal (HPA) axis, which has been a major focus of scrutiny in patients with PTSD.”
At clinical level, another important biological pattern was the elevated blood pressure and pulse ratio.22 Interesting correlations with neurobiological patterns were also found. The review by Rustad et al23 pointed out the association between the augmented sympathetic nervous system output with the PTSD. Chronic high stress is regulated by precise neurobiological substrates, including the HPA axis and monoamine neurotransmitters implicated in the anxiety circuit. Cytokines influence the HPA axis and they can induce chronic activation of the immune system causing high level of stress through PTSD. Apart from physiological values, sociodemographic factors resulted not particularly relevant. In our review, age group, gender, and history of substance abuse seemed not to have any effect on psychological PTSD.18
The importance of age is controversial in the genesis of the disorder. While the great majority of the studies considered did not report differences in age and stress, the research of Perez et al5 stated that younger women experience more increased distress. However, as the research by Andrykowski and Kangas15 mentions, it is always very important to highlight the great interindividual variability. In particular, the exposure to PTSD has been correlated with the phases following diagnosis. As Kangas et al6 stated “it is important to recognize the grief reactions that people can experience after receiving a cancer diagnosis. Adjusting to a poor prognosis requires an adjustment period in which one needs to integrate much novel information, including reevaluating one’s life goal”.
Regarding personality, the relationship between traits and psychological distress was examined in two studies. The active individual’s reaction to life events is thought to alleviate psychological PTSD directly by contributing to expectations of a positive outcome.19
Similarly, the study by Chida et al21 showed that stress-prone personality or unfavorable coping styles and negative emotional responses are correlated with higher stress and high mortality. Type C personality seemed also to have a mediator effect between breast cancer diagnosis and PTSD.5
Accordingly, Type C personality persons, who are significantly not assertive, and not oriented to satisfy their wants, needs, or desires, are more exposed to PTSD than others. Type C personality can be intended as a psychological disposition whereby an individual seems quiet and thoughtful, but is in fact frustrated and angry. Difficulties in processing negative emotions such as anger are specific of this kind of personality functioning: a person with a typical type C personality appears to lack emotions, does not usually assert themselves and strives to pacify others.
Regarding coping strategies, the use of active coping skills has consistently been related to lower levels of distress. Particularly, the epidemiological study by Lilliberg et al19 with 10,808 cases of patients showed that the inability to cope with stressful events happened in the personal history of the patients during the previous 5 years was highly correlated with the development of PTSD and breast cancer. Example of such traumatic events included divorce or separation, death of a husband, and death of a close relative or friend.19
Similarly, Perez et al5 have shown that negative coping strategies such as anxious preoccupation (β=1.20) and cognitive avoidance (β=0.91) are important predictors of PTSD. The review by Shand et al24 concluded by stating that some particular constructs such as optimism, spirituality, and positive attitude are strongly correlated with the capacity to cope and to face adverse events in breast cancer.
Finally, a relationship between social support and psychological PTSD was found in one study. In this research, it was found that patients perceiving less social support were more at risk of developing stress and PTSD.5
Implications for co-treatment
Being diagnosed with breast cancer and concomitant PTSD symptoms or syndrome has influences on different areas of patients’ quality of life (QoL), on the patient’s clinical pathway, and on the way patients cope with their breast cancer experience and show adjustment processes. Patients with PTSD had significant lower functional performance status, physical health-related QoL, and mental health-related QoL scores (p<0.05).10 Again, levels of occupational impairment were higher in PTSD patients, and by 18 months postdiagnosis they were more likely to having sought psychological treatment.10 Hegel et al8 confirmed these evidences: patients who screened positive for PTSD were significantly lower on the Physical Component Score than patients who screened negative (mean score 47.1 vs 54.1, p<0.01) although not in the range of clinical significance. The PTSD patients were significantly statistically and clinically lower on the SF-8 Mental for mental health-related QoL than screen-negative patients (mean score, 36.9 vs 48.8, p<0.0).
Moreover, it seems that the effects of PTSD are long-term effects: patients with high levels of PTSD symptoms before surgery maintain these levels, showing difficulties in adjusting to illness, even 2 years later4 demonstrating an impact of PTSD symptomatology on long-term adjustment to breast cancer.
A specific clarification is required regarding the effect of PTSD on cognitive functioning: Hermelink et al25 demonstrated in a large prospective study that limited cognitive impairment that may occur in breast cancer patients already before treatment initiation is most probably largely caused by traumatic stress symptoms as a consequence of breast cancer diagnosis. Thus, PTSD symptoms were demonstrated to contribute much more to perceived cognitive impairment than did chemotherapy26 with huge impact on QoL, relationship, and communication issues with the multidisciplinary team.
In front of these evidences, the co-treatment of this psychological disturbance is warranted to guarantee patients with a proper medical pathway. The implementation of co-treatment can be intended either in the effort of routinely assessing patients for the presence of the syndrome6 but also developing multidisciplinary policies that focus on health care professional education and training as the main goal because it is necessary with this kind of frail patients to use specific way of delivering information regarding diagnosis, treatment, and illness with attention to their traumatized state of mind.4
Discussion
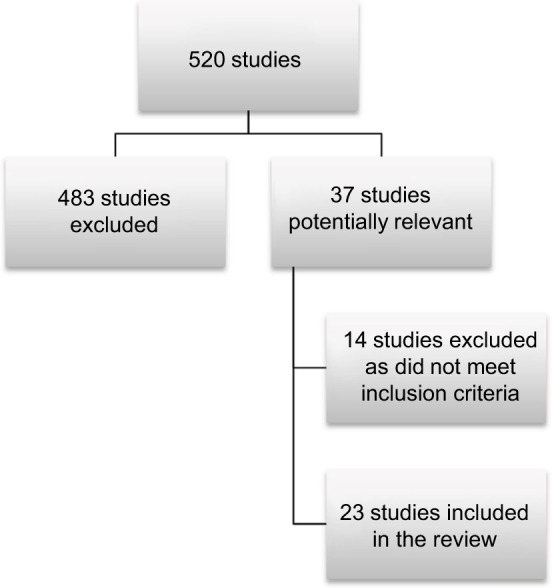
PTSD is undoubtedly a complex psychiatric syndrome, and the aim of our review was to present a comprehensive paper summarizing its prevalence in the breast cancer setting, the associated sociodemographic and comorbidity risk factors together with the other “edge of the sword,” namely, those potential links whereby stress could impact both the cancer risk and coping with the cancer experience. Implications for co-treatment were also addressed (Figure 2).
Figure 2.
Synthesis of the main results of the systematic review.
Abbreviation: PTSD, post-traumatic stress disorder.
We found that PTSD was studied from different perspectives in the literature, in different disease phases and by means of different self-reported or qualitative measures.6–17
This methodological heterogeneity leads to a great variability in study results and, therefore, to difficulties and cautiousness in the generalizability of data. Sample sizes in the revised studies were also small and the lack of RCTs represents an important methodological limitation in the published literature.
The prevalence of PTSD in breast cancer patients resulted possibly high and was seen to range from 0% to 32.3%3,8–15 with different evidence regarding its prevalence over time: some studies attest a higher prevalence of PTSD soon after diagnosis than at the end of the active treatment phases11 while others outline an increase of the prevalence at the end of treatment.10,13
On the other hand, the prevalence of PTSD symptoms themselves, without all criteria for a DSM diagnosis being fulfilled, is upward of 75% in breast cancer patients,4,10,12,13 and it emerges that patients scoring high in avoidant symptoms soon after diagnosis will have difficulties in adjustment even 2 years later. This raises the issue of integrated psychological care delivery: usually in Europe, the psychological welfare of breast cancer patients in the first year of post-treatment is generally not considered a hospital responsibility. Private organizations and private mental health care professionals, under a National Health Care scheme, deliver psychological interventions to patients who survived.13 The fact that PTSD symptoms are prevalent also years after the first diagnosis alerts health care systems in the direction of offering patients health care continuity.
Furthermore, considering the impact of PTSD symptoms on patients’ cognitive functioning4,13 and on QoL (mental, physical, and emotional),8,10 future research should aim at the detection of policies that include PTSD symptoms in breast cancer patients’ health care screening, reaching a consensus about heterogeneity of measures.17
Are there any variables to be included in screening in order to have an idea of how high the risk is that a breast cancer patient will develop PTSD? In the literature, no agreement has been reached either for clinical variables, or for sociodemographic variables. Time since diagnosis, type of treatment, and extent of disease are not unanimously associated with the development of PTSD demonstrating that psychological factors are more relevant than clinical objectivity in causing the disease. Age3,5,11,16 and positive family cancer history4 seem to be the only sociodemographic factors unanimously associated with a higher risk of developing PTSD symptomatology. Among psychological variables, the presence of comorbid psychological disorders is responsible for a higher risk of developing PTSD8,9,12 so that particular attention should be devoted to this category of frail patients whose psychiatric history is not routinely recollected.4
At an individual level, a number of immature coping mechanisms such as hopelessness/helplessness,5 avoidant coping style,5,13 emotionally reactive temperament,13 negative affectivity,13 and Type C personality5 are related to the presence of PTSD symptoms. Biological and chemical aspects, related to the HPA axis, are also relevant.22
PTSD is a multifactorial syndrome, and by means of a simple blood test its risk could be estimated differently from that which occurs in the case of other mental disturbances such as depressive symptoms or adjustment disorders whose biological correlates are nowadays not so clearly defined. Cost-effectiveness evaluation of this preventive screening approach is warranted as is typical in chronic conditions.27,28
In a double-edged sword perspective, if we consider the role of comorbid factors, previous mental history, and stressful life events in developing PTSD, we also argued at evaluating the potential links by which stress can impact cancer risk but the most relevant evidence from the literature is that this link is today too arduous to be demonstrated.18,20 However, it has been demonstrated in other conditions such as pain or chronic blood conditions,28,29 so it may be possible that these relations can be shown in future studies.
A novel and not so examined aspect is the transcultural approach: ethnicity emerged to be a factor associated with PSTD prevalence3,11,17 with the highest prevalence in the Middle East rather than Europe, North America, and Asia probably due to a socially oriented perception of life stressors and to the subjective illness experience, and a qualitative research methodology could help in thoroughly comprehending this aspect.
In conclusion, there is a need for longitudinal, prospective studies to identify patients at risk, determine causal or aggravating factors, and develop a preventive intervention policy.
Moreover, future studies should address the issue of stress and PTSD in education and training among health operators in order to include proper communication and better relationships,30 which may contain the development of that disorder and which may lead to better understanding the course of this type of problem, as PSTD may occur not immediately after diagnosis but also years after first diagnosis.
It should be underlined that the eligible studies of the present review accorded with the DSM-IV criteria for PTSD diagnosis but not with the newer DSM-V that considers a life-threatening disease to be responsible of causing PTSD only under some circumstances, that is, when the diagnosis is sudden and catastrophic. Given this reason, future researchers should be cautious in diagnosing cancer-related PTSD.
Conclusion
Stress is a psychological construct much studied in medicine. This is particularly so in the case of chronic disease such as cancer. Cancer of the breast is one of the most studied from a psychosomatic perspective because it is one of the most prevalent in female population. Despite a number of research studies focused on the relationship between stress and breast cancer, no unique evidence is available. Undoubtedly, the literature demonstrates that a breast cancer diagnosis can be responsible for causing stress, particularly in the form of the renowned PTSD. Little is known as yet regarding the role that previous life stressors and general stress play in determining cancer or in influencing the course of the disease.
Acknowledgments
We thank very much William Russell Edu for his kind and precise assistance in revising the English text.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Diagnostic and Statistical Manual of Mental Disorders, Fourth edition (DSM-4) Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 2.Diagnostic and Statistical Manual of Mental Disorders, Fifth edition (DSM-5) Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- 3.Swartzman S, Booth JN, Munro A, Sani F. Posttraumatic stress disorder after cancer diagnosis in adults: a meta-analysis. Depress Anxiety. 2017;34(4):327–339. doi: 10.1002/da.22542. [DOI] [PubMed] [Google Scholar]
- 4.Arnaboldi P, Lucchiari C, Santoro L, Sangalli C, Luini A, Pravettoni G. PTSD symptoms as a consequence of breast cancer diagnosis: clinical implications. Springerplus. 2014;3:392. doi: 10.1186/2193-1801-3-392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Perez S, Galdon MJ, Andreu Y, et al. Posttraumatic stress symptoms in breast cancer patients: temporal evolution, predictors and mediation. J Trauma Stress. 2014;27(2):224–231. doi: 10.1002/jts.21901. [DOI] [PubMed] [Google Scholar]
- 6.Kangas M, Henry JL, Bryant RA. Posttraumatic stress disorder following cancer A conceptual and empirical review. Clin Psychol Rev. 2002;22(4):499–524. doi: 10.1016/s0272-7358(01)00118-0. [DOI] [PubMed] [Google Scholar]
- 7.Higgins JP, Green S. Cochrane Handbook for Systematic Reviews of Interventions. Vol. 4. The Cochrane Collaboration; 2011. [Google Scholar]
- 8.Hegel MT, Moore CP, Dale Collins E, et al. Distress, psychiatric syndromes and impairment of function in women with newly diagnosed breast cancer. Cancer. 2006;107(12):2924–2931. doi: 10.1002/cncr.22335. [DOI] [PubMed] [Google Scholar]
- 9.Mehnert A, Koch U. Prevalence of acute and post-traumatic stress disorder and comorbid mental disorders in breast cancer patients during primary cancer care: a prospective study. Psychooncology. 2007;16(3):181–188. doi: 10.1002/pon.1057. [DOI] [PubMed] [Google Scholar]
- 10.Shelby RA, Golden-Kreutz DM, Andersen BL. PTSD diagnosis, sub-syndromal symptoms, and comorbidities contribute to impairment for breast cancer survivors. J Trauma Stress. 2008;21(2):165–172. doi: 10.1002/jts.20316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vin-Raviv N, Hillyer GC, Hershman DL, et al. Racial disparities in post-traumatic stress after diagnosis of localized breast cancer: the BQUAL study. J Natl Cancer Inst. 2013;105(8):563–572. doi: 10.1093/jnci/djt024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.O’Connor M, Christensen S, Jensen AB, Møller S, Zachariae1 R. How traumatic is breast cancer? Post-traumatic stress symptoms (PTSS) and risk factors for severe PTSS at 3 and 15 months after surgery in a nationwide cohort of Danish women treated for primary breast cancer. Br J Cancer. 2011;104(3):419–426. doi: 10.1038/sj.bjc.6606073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Elklit A, Blum A. Psychological adjustment one year after the diagnosis of breast cancer: a prototype study of delayed post-traumatic stress disorder. Br J Clin Psychol. 2011;50(4):350–363. doi: 10.1348/014466510X527676. [DOI] [PubMed] [Google Scholar]
- 14.Alkhyatt MK, Elham Kh, Abdullah EK, Ibraim RH, Anee BA, Raho JA. Post-traumatic stress in women with breast cancer. J Med J. 2012;46(4):315–319. [Google Scholar]
- 15.Wu X, Wang J, Cofie R, Kaminga AC, Liu A. Prevalence of post traumatic stress disorder among breast cancer patients: a meta-analysis. Iran J Public Health. 2016;45(12):1533–1544. [PMC free article] [PubMed] [Google Scholar]
- 16.Hahn EE, Hays RD, Kahn KL, Litwin MS, Ganz PA. Post-traumatic stress symptoms in cancer survivors: relationship to the impact of cancer scale and other associated risk factors. Psychooncology. 2015;24(6):643–652. doi: 10.1002/pon.3623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Andrykowski MA, Kangas M. Posttraumatic stress disorder associated with cancer diagnosis and treatment. In: Holland Jimmie C, Breitbart WS, Butow PN, Jacobsen PB, Loscalzo MJ, McCorkle R., editors. Psycho-Oncology. New York: Oxford University Press, Inc.; 2010. pp. 348–357. [Google Scholar]
- 18.Gradus JL, Kormendinè Farkas D, Svensson E, et al. Posttraumatic stress disorder and cancer risk: a nationwide cohort study. Eur J Epidemiol. 2015;30(7):563–568. doi: 10.1007/s10654-015-0032-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lillberg K, Verkasalo PK, Kaprio J, Teppo L, Helenius H, Koskenvuo M. Stressful life events and risk of breast cancer in 10,808 women: a cohort study. Am J Epidemiol. 2003;157(5):415–423. doi: 10.1093/aje/kwg002. [DOI] [PubMed] [Google Scholar]
- 20.Antinova L, Aronson K, Mueller CR. Stress and breast cancer: from epidemiology to molecular biology. Breast Cancer Res. 2011;13(2):208. doi: 10.1186/bcr2836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chida Y, Hamer M, Wardle J, Steptoe A. Do stress-related psychosocial factors contribute to cancer incidence and survival? Nat Clin Pract Oncol. 2008;5(8):466–475. doi: 10.1038/ncponc1134. [DOI] [PubMed] [Google Scholar]
- 22.Loo WT, Liu Q, Yip MC, et al. Status of oral ulcerative mucositis and biomarkers to monitor posttraumatic stress disorder effects in breast cancer patients. Int J Biol Markers. 2013;28(2):168–173. doi: 10.5301/jbm.5000025. [DOI] [PubMed] [Google Scholar]
- 23.Rustad JK, David D, Currier MB. Cancer and posttraumatic stress disorder: diagnosis, pathogenesis and treatment considerations. Palliat Support Care. 2012;10(3):213–223. doi: 10.1017/S1478951511000897. [DOI] [PubMed] [Google Scholar]
- 24.Shand LK, Cowlishaw S, Brooker JE, Burney S, Ricciardelli LA. Correlates of post-traumatic stress symptoms and growth in cancer patients: a systematic review and meta-analysis. Psychooncology. 2015;24(6):624–634. doi: 10.1002/pon.3719. [DOI] [PubMed] [Google Scholar]
- 25.Hermelink K, Voigt V, Kaste J, et al. Elucidating pretreatment cognitive impairment in breast cancer patients: the impact of cancer-related post-traumatic stress. J Natl Cancer Inst. 2015;107(7):djv099. doi: 10.1093/jnci/djv099. [DOI] [PubMed] [Google Scholar]
- 26.Li J, Yu L, Long Z, Li Y, Cao F. Perceived cognitive impairment in Chinese patients with breast cancer and its relationship with post-traumatic stress disorder symptoms and fatigue. Psychooncology. 2015;24(6):676–682. doi: 10.1002/pon.3710. [DOI] [PubMed] [Google Scholar]
- 27.Riva S, Cutica I, Krampe C, et al. A cohort pilot study on HIV-associated neuropsychological impairments in hemophilia patients. Front Hum Neurosci. 2015;9:313. doi: 10.3389/fnhum.2015.00313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mangiafico L, Perja M, Fusco F, Riva S, Mago D, Gringeri A. Safety and effectiveness of raltegravir in patients with haemophilia and anti-HIV multidrug resistance. Haemophilia. 2012;18(1):108–111. doi: 10.1111/j.1365-2516.2011.02610.x. [DOI] [PubMed] [Google Scholar]
- 29.Riva S, Cutica I, Pravettoni G. Is there evidence for neurocognitive dysfunctions in patients with postnatal HIV infection? A review on the cohort of hemophilia patients. Front Hum Neurosci. 2014;8:470. doi: 10.3389/fnhum.2014.00470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Arnaboldi P, Pravettoni G. How and to what extent can the humanities support oncology personnel? Could we devise a formula to guide policy-makers? J Cancer Policy. 2016;8:7–8. [Google Scholar]