Summary
Background:
Mechanical factors are at the basis of any tendon healing process, being pressure an aspect able to positively influence it. For this reason transosseous rotator cuff repair represents the gold standard procedure for patients affected by a cuff tear, maximizing the tendon footprint contact area and reducing motion at the tendon to bone interface.
Methods:
The Authors present an all arthroscopic suture bridge-like transosseous repair with the preparation of a single transosseous tunnel perfor med thanks to a precise dedicated instrument (Compasso®) and one implant (Elite-SPK®) with the use of only 3 suture wires. In addition this technique permits to accurately prepare the bony side of the lesion without any risk or complication, such as anchor pull-out and greater tuberosity bone osteolysis.
Conclusions:
However, even if this technique seems less demanding, the arthroscopic transosseous repair is still an advanced procedure, and should be performed only by well prepared arthroscopic shoulder surgeons.
Level of evidence:
V.
Keywords: arthroscopy, repair, rotator cuff, shoulder, tear, tendon, trans-osseous technique
Introduction
Arthroscopic rotator cuff (RC) repair techniques have evolved significantly during the last decades1. However the occurrence of re-tear2 or non-healing3 is still high, and numerous variables are to be considered in order to make an adequate surgical choice4. Different kinds of suture configurations were developed in the last years trying to optimize RC tendon healing biology at the repaired site5–7. At first, the double-row techniques added a row of suture anchors fixation lateral to the conventionally placed medial row that had represented the standard fixation strategy for arthroscopic RC repairs8. Later, in an effort to combine the stronger biomechanical repair of the double-row configuration with the increased tendon-bone interface pressure benefits, the transosseous-equivalent (TOE) suture bridge repair was developed9,10.
This technique preserves the suture limbs of the medial row bridging them over the tendon’s native insertion with fixation in the lateral humeral cortex providing also an optimal load sharing. Several studies reported the biomechanical superiority of TOE RC repair over the standard double row and single-row repair techniques due to the ability to provide compression through the footprint by increasing the contact area. This is achieved by connecting the medial and lateral rows, thus exerting compression throughout the repair, instead of only at the anchor insertion points2,9–11.
However, failures at the medial row with a well-attached tendon on the great tuberosity have been reported with the TOE technique12,13.
Moreover other anchor-related complications (pull out in presence of poor bone stock, greater tuberosity bone osteolysis, difficult revision, increased cost) called into question the use of anchor fixation for RC repair14,15.
For these reasons, the best arthroscopic technique has not yet been established and open transosseous (TO) RC repair is to be considered the gold standard procedure15. As recently established, mechanical factors are at the basis of any healing process, being pressure an aspect able to positively influence the healing process16. The TO technique permits to maximize the tendon footprint contact area2 and to reduce motion at the tendon to bone interface17. In addition to this mechanical aspect, TO technique permits to accurately prepare the bony side of the lesion without any risk or complication, such as anchor pull-out and greater tuberosity bone osteolysis15,18.
In an attempt to overcome the limitations of anchor repair, arthroscopic TO anchorless RC repair techniques have recently been developed6,14,15,17–19 (Tab. I).
Table I.
Arthroscopic trans-osseous rotator cuff repair techniques recently published for the treatment of full-thickness tendon tear.
| Authors | Year | N° of tunnel | N° of sutures | Instrumentation |
|---|---|---|---|---|
| H Frick11 | 2010 | 1 or more | 1–3 for each tunnel | Bone needle |
| R Garofalo12 | 2012 | 1 or more | 2–3 for each tunnel | ArthroTunneler |
| S Kuroda17 | 2013 | 3 | 5 | Drill guide + 3 k-wires |
| EM Black3 | 2015 | 2 | 6 | ArthroTunneler |
| M Aramberri-Gutierrez1 | 2015 | 1(medial calcar) | 2(1 soft anchor) | ACL-guide |
| BA Flanagin9 | 2016 | 1 or 2 | 3 or 6 | ArthroTunneler |
In this paper a novel and reproducible all-arthroscopic TO anchorless technique that replicates the TOE suture bridge repair is reported. This novel technique avoids all the disadvantages related to anchor fixation. The principle is to combine the double-row suture bridge fixation with the classic TO approach of suture fixation as performed in the open rotator cuff repair.
Surgical technique
The procedure can be performed depending on anesthesiologist preference under general anesthesia or interscalene brachial plexus block or combined, and in beach-chair position or lateral decubitus according to surgeon request.
The Authors suggest using a 3 portals surgical technique: standard posterior (for the scope), lateral and antero-superior (working) portals. Once the reparability of the RC lesion is assessed we advise firstly to treat possible associated pathology (LHB tenotomy/tenodesis, subscapularis repair).
After tendon and bone preparation for suture (respectively cutting and refreshing the torn tendinous edge and wide surface decortication of the footprint providing maximum spongy bone) is possible to prepare the TO tunnel. A dedicated instrument, named Compasso® (NCS Lab s.r.l. - Medical Devices Factory, Italy) was developed with the aim to simplify and accelerate the operative procedures avoiding pitfalls or damages to soft tissues.
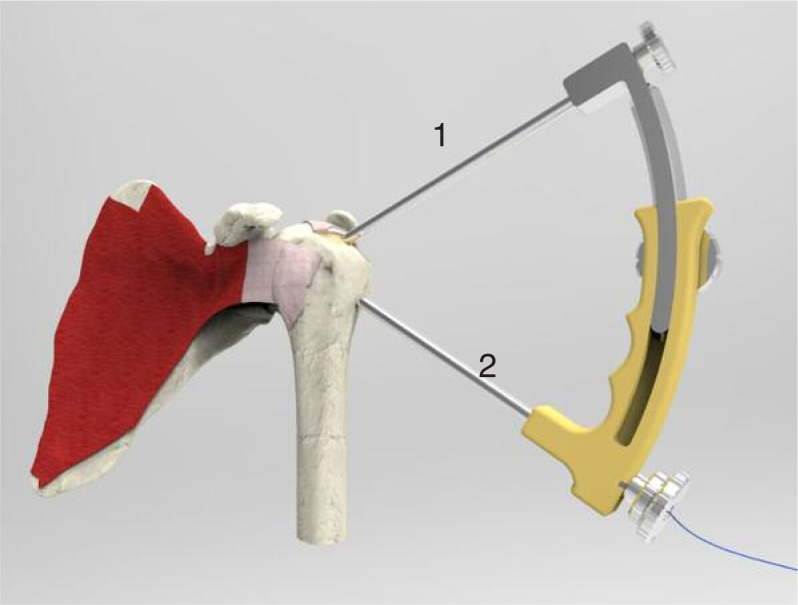
Place the Compasso® (Fig. 1) parallel to the coronal plane with the tip of the proximal punch (part 1 with lanceolate tip) corresponding to the desired exit point of the transosseous tunnel you wish to perform. The angle of insertion of the proximal punch should be between 30° and 45°, depending on the protrusion of the acromion. Use the hammer to sink the proximal punch in the humeral head until it stops and reach the cannula enlargement (mechanical stop). Insert the distal punch (2) inside the distal cannula, then assemble these parts on the main body of Compasso® until the pin of the punch reaches the lateral cortex of humerus. For a correct insertion align the laser marks of cannula and main body. Unscrew the locking ring on the main frame to set the angle between the distal and the proximal cannula so as to place the pin of the distal punch approximately at 12–15 mm from the edge of the greater tuberosity, then tighten the locking ring firmly again, once in the desired optimal position. The cranial-caudal angle can be defined until cannula 2 is inserted into the bone. The anterior-posterior position of the instrument, instead, must be defined before the subcutaneous insertion. Hammer the distal punch (2) to pass the lateral cortex of the humerus for some millimeters, to stabilize the device, then lift the proximal loading punch (1) until the laser mark on it becomes visible. Hammer the distal cannula (2) till it comes in contact with the main body of Compasso®. Remove the distal inner punch from its cannula. Load a monofilament shuttle suture (PDS size USP 1 or 2) through the distal cannula until it stops. Insert the suture locker (part 1 with rounded tip) through the proximal cannula (1), then tighten it to steadily capture the shuttle suture.
Figure 1.
Positioning of the guide (Compasso®) to perform the transosseous tunnel: the tip of the proximal punch (1) corresponds to the desired exit point of the tunnel, while the pin of the distal punch (2) reaches the lateral cortex of humerus. A monofilament shuttle suture is loaded distally and captured by a suture locker proximally.
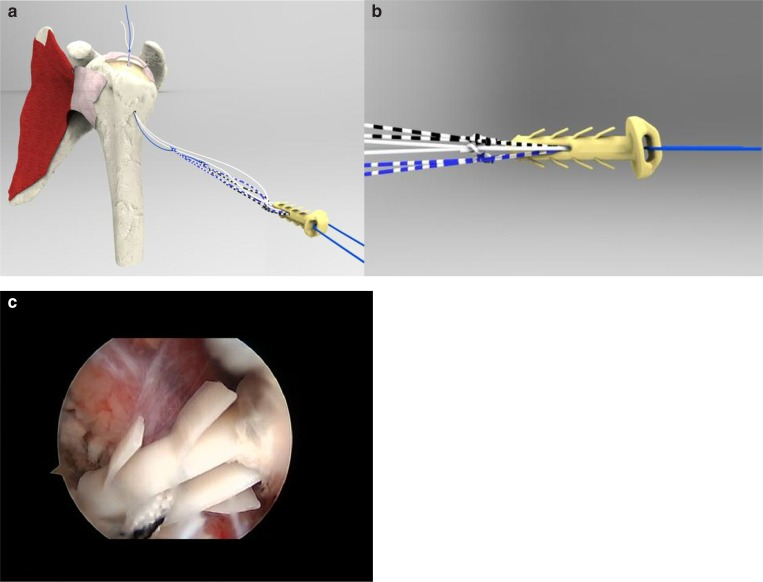
Check the optimal engaging of the shuttle suture by pulling the external limb. Remove the distal cannula from the main body of Compasso®. Pull the Compasso® out from the medial access of the transosseous tunnel by dragging with it the shuttle suture. This shuttle could drag the suture wires connected to the front part of the implant, the Elite-SPK® (NCS Lab s.r.l. - Medical Devices Factory, Italy) (Fig. 2a). It is an implant made of PEEK containing two separated eyelets: a rear one, that remains externally on the lateral cortex of the humerus, and a front, smaller one through which sutures are initially loaded. Along the body of the device several stabilising flaps are attached to the main body which, in combination with the wide contact surface beneath the head of the implant, have the function of providing an optimal primary stability (Fig. 2b).
Figure 2 a–c.
a) The shuttle suture drag the suture wires connected to the front part of the implant, the Elite-SPK®.
b) The Elite SPK® is an implant made of peek containing two separated eyelets: a rear one, that remains externally on the lateral cortex of the humerus, and a front, smaller one through which sutures (in number of 3, of different colours) are initially loaded. To avoid any sliding of the wires, it is better to perform 2 simple knots for each suture. Along the body of the device several stabilising flaps are attached to the main body which, in combination with the wide contact surface beneath the head of the implant, have the function of providing an optimal primary stability.
c) Arthroscopic view (with the scope posterior). Insertion of the Elite SPK® into the TO tunnel through the hole yet performed into the lateral cortex of the humerus. Note the stabilising flaps.
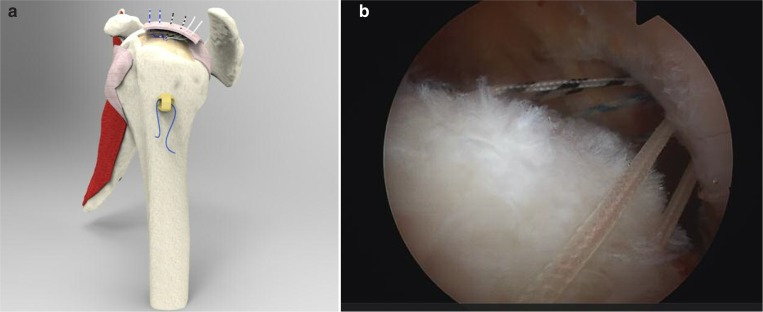
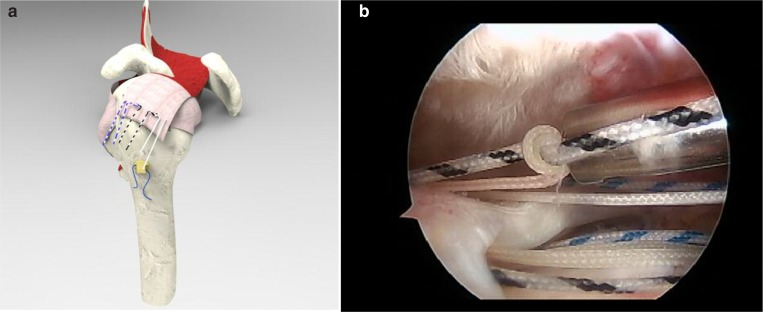
Depending on the tear size a different numbers of sutures can be passed. We recommend to shuttle 3 sutures (of different colours). Before this step to avoid any sliding of the wires, we perform 2 simple knots for each suture, in the front part of the implant (Fig. 2b). All the six stitches are then passed through the cuff (Fig. 3) with different devices according to surgeon preference, from posterior to anterior, and different kinds of suture configurations can be created. The senior surgeon (CC) in collaboration with the engineer (MM) developed the configuration below reported and named 2MC (double MC). Schematically we refer to limb 1 as the most anterior, going to limb 6 for the most posterior. We firstly close the limb 2 with 3 (suture 1), and later the limb 4 with 5 (suture 2) leaving free the limbs 1 and 6 (Fig. 4). After cutting respectively one of the end of suture 1 and 2, we shuttle from anterior to posterior in the external eyelet of the Elite SPK® the limb 1 and the remaining end of suture 1 (Fig. 5). At this point, in order to achieve a repair in closed loop configuration, we tie the knot (laterally) between the limbs 1 and 6, and the remaining limb of suture 1 and 2 (Fig. 6). This represents a very tight and stable repair configuration that permits to completely cover the greater tuberosity. Surgery ends with subacromial decompression if necessary.
Figure 3 a, b.
a) All the six stitches are then passed through the cuff (with different devices according to surgeon preference) from posterior to anterior. b) Arthroscopic view (with the scope posterior). Note the six stitches passed through the cuff, and all retrieved through the lateral portal.
Figure 4 a, b.
2MC suture configuration. a) Schematically we refer to limb 1 as the most anterior, going to limb 6 for the most posterior. Firstly close the limb 2 with 3 (suture 1), and later the limb 4 with 5 (suture 2) leaving free the limbs 1 and 6. b) Arthroscopic view (with the scope posterior). The surgeon firstly ties the knot between the limb 2 with 3.
Figure 5.
2MC suture configuration. After cutting respectively one of the end of suture 1 and 2, shuttle from anterior to posterior in the external eyelet of the Elite SPK® the limb 1 and the remaining end of suture 1.
Figure 6.
2MC suture configuration. At this point, in order to achieve a repair in closed loop configuration, tie the knot (laterally) between the limbs 1 and 6, and the remaining limb of suture 1 and 2.
Discussion
A larger and more stable tendon-to-bone contact interface during the early phase of the healing process is nowadays a worldwide accepted concept16,20,21, so that different techniques have been developed to obtain a more anatomic configuration of the RC repair on the footprint providing a better environment for tendon healing.
During the last years the demonstration that the suture tension for any TO technique provides a more direct tendon-to-bone compression vector and a larger repair site contact area when compared to the suture anchor technique has lead to the introduction of arthroscopic TO RC repair techniques9,10.
Several papers in literature deal with this topic, but the general impression is that the arthroscopic TO technique are still technically demanding and with a lot of uncontrollable variables. Numerous dedicated instruments have been employed to create the TO tunnels into the greater tuberosity from the ACL tibial guide to different kinds of needle or tunneler devices15,22–24. However, all the arthroscopic TO techniques described until now are complex procedures that requires several surgical steps, the creation of 2 or more TO tunnels and the use of many sutures making these procedures very difficult to reproduce and standardize6,14,15,18,19.
In addition some complications such as needle breakage, neurological damage or greater tuberosity fracture can be encountered. Moreover, depending on the tear size, in order to equally distribute the forces on the tendon and to prevent the bone cutting phenomenon, it is mandatory to create more than 1 TO tunnel and use at least 2 or 3 sutures in each tunnel with the risk of suture twist and an increase of the surgical time required.
Using a dedicated and very precise instrument (Compasso®) to create a single TO tunnel and a single implant (Elite-SPK®) with 3 sutures the current technique permits to obtain a wide contact surface between the tendon and the bone with a biomechanical effectiveness comparable with the open TO technique while reducing the complexity and difficulty that is usually encountered with other arthroscopic TO techniques.
The peculiar shape of the implant and its features make it a suture platform that can also be used on very fragile bone tissue without the problem of migration and pull out, providing a reliable fixation. Two of the major problems previously described with arthroscopic TO techniques have been suture abrasion against the bone tunnel which can result in suture rupture, and bone cut in presence of poor bone (cheese cut effect) with damage of the remaining bone integrity and weakening of the tuberosity. With the use of Elite-SPK®, as there is no sliding of the suture wires into the TO tunnel, the risk of suture cut and bone damage is significantly reduced. In addition, while the other arthroscopic TO techniques generate a tendon compression vector directed laterally and tangential to the bone, the tendon compression vector provided by the Elite-SPK® is perpendicular to the footprint resulting in a maximization of the contact area (with an optimal pressure distribution) while reducing sutures-bone tunnel impingement and thus suture abrasion and bone damage. For this reason the Elite-SPK® seems particularly convenient in presence of osteoporotic bone or intraosseous cysts where usually suture anchors fail.
The 2 MC suture configuration allows the surgeon to build a suture-bridge like construct that increases the contact area and optimizes the compression of the tendon on the footprint. In particular, the 2 central double-row sutures provide stability and compression while the most anterior and the most posterior wires once tied together on the lateral aspect of the great tuberosity result in an enveloping effect on the tendon providing a complete coverage of the footprint.
The 2 simple knots for each suture tied in the front part of the implant are essential to avoid any sliding up of the limbs when tying the knot between limb 2 and 3 and limb 4 and 5, permitting a really good contact tendon to bone. Moreover, it is known that the three sutures passed through the TO tunnel share the load on the tendon resulting in a reduction of the local stress spikes at the tendon interface25.
Conclusion
The current technique allows to perform an all arthroscopic suture bridge-like TO repair with the preparation of a single TO tunnel performed thanks to a precise dedicated instrument (Compasso®) and one implant (Elite-SPK®) with the use of only 3 suture wires. However, even if this technique is less demanding, the arthroscopic TO repair is still an advanced procedure, and should be performed only by well prepared arthroscopic shoulder surgeons.
Ethic
The Authors declare that this research was conducted following basic ethical aspects and international standards as required by the journal and recently updated in26.
Acknowledgments
To all the staff of the Operating Theatre of ICOT -Latina and of the Laboratory of NCS - Carpi.
Footnotes
Conflict of interest
Claudio Chillemi declares that he has no conflict of interest. Matteo Mantovani designed and manufactured the Compasso® + Elite-SPK®.
This study was not funded and/or sponsored by Companies.
References
- 1.Kim SH, Kim J, Choi YE, Lee HR. Healing disturbance with suture bridge configuration repair in rabbit rotator cuff tear. J Shoulder Elbow Surg. 2016;25(3):478–486. doi: 10.1016/j.jse.2015.08.035. [DOI] [PubMed] [Google Scholar]
- 2.Imam MA, Abdelkafy A. Outcomes following arthroscopic transosseous equivalent suture bridge double row rotator cuff repair: a prospective study and short-term results. SICOT J. 2016;2:7–14. doi: 10.1051/sicotj/2015041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chillemi C, Petrozza V, Garro L, et al. Rotator cuff re-tear or non-healing: histopathological aspects and predictive factors. Knee Surg Sports Traumatol Arthrosc. 2011;19(9):1588–1596. doi: 10.1007/s00167-011-1521-1. [DOI] [PubMed] [Google Scholar]
- 4.Oliva F, Piccirilli E, Bossa M, et al. I.S.Mu.L.T - Rotator Cuff Tears Guidelines. Muscles Ligaments Tendons J. 2016;5(4):227–263. doi: 10.11138/mltj/2015.5.4.227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dilisio MF, Miller LR, Higgins LD. Transtendon, double-row, transosseous-equivalent arthroscopic repair of partial-thickness, articular-surface rotator cuff tears. Arthrosc Tech. 2014;3(5):559–563. doi: 10.1016/j.eats.2014.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kuroda S, Ishige N, Mikasa M. Advantages of arthroscopic transosseous suture repair of the rotator cuff without the use of anchors. Clin Orthop Relat Res. 2013;471(11):3514–3522. doi: 10.1007/s11999-013-3148-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mihata T, Watanabe C, Fukunishi K, Ohue M, Tsujimura T, Fujiwara K, Kinoshita M. Functional and structural outcomes of single-row versus double-row versus combined double-row and suture-bridge repair for rotator cuff tears. Am J Sports Med. 2011;39(10):2091–2098. doi: 10.1177/0363546511415660. [DOI] [PubMed] [Google Scholar]
- 8.Lo IK, Burkhart SS. Double-row arthroscopic rotator cuff repair: re-establishing the footprint of the rotator cuff. Arthroscopy. 2003;19:1035–1042. doi: 10.1016/j.arthro.2003.09.036. [DOI] [PubMed] [Google Scholar]
- 9.Park MC, ElAttrache NS, Tibone JE, Ahmad CS, Jun BJ, Lee TQ. Part I: footprint contact characteristics for a transosseou-sequivalent rotator cuff repair technique compared with a doublerow repair technique. J Shoulder Elbow Surg. 2007;16(4):461–468. doi: 10.1016/j.jse.2006.09.010. [DOI] [PubMed] [Google Scholar]
- 10.Park MC, Tibone JE, Elattrache NS, et al. Part II: Biomechanical assessment for a footprint-restoring transosseous-equivalent rotator cuff repair technique compared with a double-row repair technique. J Shoulder Elbow Surg. 2007;16:469–476. doi: 10.1016/j.jse.2006.09.011. [DOI] [PubMed] [Google Scholar]
- 11.Burkhart SS, Cole BJ. Bridging self-reinforcing double-row rotator cuff repair: we really are doing better. Arthroscopy. 2010;26(5):677–680. doi: 10.1016/j.arthro.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 12.Cho NS, Lee BG, Rhee YG. Arthroscopic rotator cuff repair using a suture bridge technique: is the repair integrity actually maintained? Am J Sports Med. 2011;39(10):2108–2116. doi: 10.1177/0363546510397171. [DOI] [PubMed] [Google Scholar]
- 13.Voigt C, Bosse C, Vosshenrich R, Schulz AP, Lill H. Arthroscopic supraspinatus tendon repair with suture-bridging technique: functional outcome and magnetic resonance imaging. Am J Sports Med. 2010;38(5):983–991. doi: 10.1177/0363546509359063. [DOI] [PubMed] [Google Scholar]
- 14.Black EM, Lin A, Srikumaran U, Jain N, Freehill MT. Arthroscopic transosseous rotator cuff repair: technical note, outcomes, and complications. Orthopedics. 2015;38(5):352–358. doi: 10.3928/01477447-20150504-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Garofalo R, Castagna A, Borroni M, Krishnan SG. Arthroscopic transosseous (anchorless) rotator cuff repair. Knee Surg Sports Traumatol Arthrosc. 2012;20(6):1031–1035. doi: 10.1007/s00167-011-1725-4. [DOI] [PubMed] [Google Scholar]
- 16.Mantovani M, Pellegrini A, Garofalo P, Baudi P. A 3D finite element model for geometrical and mechanical comparison of different supraspinatus repair techniques. J Shoulder Elbow Surg. 2016;25(4):557–563. doi: 10.1016/j.jse.2015.09.002. [DOI] [PubMed] [Google Scholar]
- 17.Flanagin BA, Garofalo R, Lo EY, Feher L, Castagna A, Qin H, Krishnan SG. Midterm clinical outcomes following arthroscopic transosseous rotator cuff repair. Int J Shoulder Surg. 2016;10(1):3–9. doi: 10.4103/0973-6042.174511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Benson EC, MacDermid JC, Drosdowech DS, Athwal GS. The incidence of early metallic suture anchor pull-out after arthroscopic rotator cuff repair. Arthroscopy. 2010;26(3):310–315. doi: 10.1016/j.arthro.2009.08.015. [DOI] [PubMed] [Google Scholar]
- 19.Aramberri-Gutiérrez M, Martínez-Menduiña A, Valencia-Mora M, Boyle S. All-Suture Transosseous Repair for Rotator Cuff Tear Fixation Using Medial Calcar Fixation. Arthrosc Tech. 2015;4(2):169–173. doi: 10.1016/j.eats.2015.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dines JS, Bedi A, Elattrache NS, Dines DM. Single-row versus double-row rotator cuff repair: techniques and outcomes. J Am Acad Orthop Surg. 2010;18(2):83–93. doi: 10.5435/00124635-201002000-00003. [DOI] [PubMed] [Google Scholar]
- 21.Ozbaydar M, Elhassan B, Esenyel C, et al. A comparison of single-versus double-row suture anchor techniques in a simulated repair of the rotator cuff: an experimental study in rabbits. J Bone Joint Surg Br. 2008;90(10):1386–1391. doi: 10.1302/0301-620X.90B10.20862. [DOI] [PubMed] [Google Scholar]
- 22.Fleega BA. Arthroscopic transhumeral rotator cuff repair: Giant needle technique. Arthroscopy. 2002;18(2):218–223. doi: 10.1053/jars.2002.30661. [DOI] [PubMed] [Google Scholar]
- 23.Frick H, Haag M, Volz M, Stehle J. Arthroscopic bone needle: a new, safe, and cost-effective technique for rotator cuff repair. Tech Should Surg. 2010;11:107–112. [Google Scholar]
- 24.Kim KC, Rhee KJ, Shin HD, Kim YM. Arthroscopic transosseous rotator cuff repair. Orthopedics. 2008;31(4):327–330. doi: 10.3928/01477447-20080401-19. [DOI] [PubMed] [Google Scholar]
- 25.Kummer FJ, Hahn M, Day M, Meislin RJ, Jazrawi LM. A laboratory comparison of a new arthroscopic transosseous rotator cuff repair to a double row transosseous equivalent rotator cuff repair using suture anchors. Bull Hosp Jt Dis. 2013;71(2):128–131. [PubMed] [Google Scholar]
- 26.Padulo J, Oliva F, Frizziero A, Maffulli N. Muscles, Ligaments and Tendons Journal - Basic principles and recommendations in clinical and field science research. 2016 Update. MLTJ. 2016;6(1):1–5. doi: 10.11138/mltj/2016.6.1.001. [DOI] [PMC free article] [PubMed] [Google Scholar]