Abstract
Policy-makers are interested in early-years interventions to ameliorate childhood risks. They hope for improved adult outcomes in the long run, bringing return on investment. How much return can be expected depends, partly, on how strongly childhood risks forecast adult outcomes. But there is disagreement about whether childhood determines adulthood. We integrated multiple nationwide administrative databases and electronic medical records with the four-decade Dunedin birth-cohort study to test child-to-adult prediction in a different way, by using a population-segmentation approach. A segment comprising one-fifth of the cohort accounted for 36% of the cohort’s injury insurance-claims; 40% of excess obese-kilograms; 54% of cigarettes smoked; 57% of hospital nights; 66% of welfare benefits; 77% of fatherless childrearing; 78% of prescription fills; and 81% of criminal convictions. Childhood risks, including poor age-three brain health, predicted this segment with large effect sizes. Early-years interventions effective with this population segment could yield very large returns on investment.
Around the world, the population is aging and total fertility rates are declining. As a result, nations increasingly view children and young people as valuable resources for the economic and social wellbeing of whole societies. This view is accompanied by public-policy interest in early interventions to help as many children as possible achieve their full potential. A key question concerns how much potential impact might be brought about by interventions in the early years of children’s lives 1,2. Research teams that have followed up small samples of children who were enrolled in intervention experiments carried out decades ago point to reductions in school leaving, unemployment, crime, overweight, and even blood pressure 3–6. Some argue that today’s better-designed interventions might achieve greater reductions in adult problems than yesteryear’s efforts 7–11. Others assert that interventions for the youngest children will bring even greater return on investment, compared to interventions that begin when children are older 12. However, a skeptic could point out that return on investment for society will depend not only on an intervention’s capacity to ameliorate childhood risks, but also on how relevant those risks are for downstream adult functioning in the general population. Thus, to a large extent, the question of how much early-years intervention can lift health and social wellbeing and reduce costs depends on how strongly early-years risk factors are tied to adult outcomes in the population. Our own research and that of others suggests that while childhood risk factors do predict adult outcomes with statistical significance, the effect sizes are typically modest 13–15. The interpretation of these modest child-to-adult effect sizes is polarizing, and has sown confusion among scientists, policy makers, and the public 16–18. On the one hand, claims are made that the ‘child is father of the man,’ because continuity from childhood risks to adult outcomes is stronger than expected, given the long duration of follow-up. On the other hand, on the basis of the same data, warnings are issued about the myth of early-childhood determinism and about unwarranted over-emphasis on childhood.
Here we tackled the prediction question anew in the context of the Dunedin Longitudinal Study, a population-representative 1972-73 birth cohort of 1,037 New Zealanders assessed at ages 3, 5, 7, 9, 11, 13, 15, 18, 21, 26, 32, and 38 years and followed from birth to midlife with 95% retention (Supplemental Material). We first integrated our longitudinal survey data and clinical data with multiple nationwide government administrative databases and electronic medical records. Then, using a novel segmentation approach, we tested the hypothesis that a small segment of the adult population accounts for large cumulative economic burden and that this segment can be predicted with good accuracy from early childhood.
Results
Throughout the cohort’s childhood, during the first decade of life, we measured risk factors that are thought to augur poor adult outcomes: growing up in a socioeconomically deprived family, exposure to maltreatment, low IQ, and poor self-control. We report these four risk factors here because they are proven predictors of adult health and social outcomes and are high-priority targets in many early-years intervention programs 19–21. A strength of this analysis is that all childhood risk predictors were measured prospectively, unbiased by participants’ knowledge of their adult outcomes.
At the most recent follow-up assessment when the cohort reached age 38, roughly the midpoint in the human lifespan, we drew on personal interviews and on New Zealand’s multiple nationwide administrative databases and electronic medical records to ascertain the cumulative distributions of economically burdensome outcomes in eight social and health sectors. This article refers to these outcomes as ‘economically burdensome’ because, in each instance, these are events, behaviours, and conditions that saddle society and government with both direct and indirect costs. These are also the same outcomes that early-years interventions hope to reduce 22. We predicted: social welfare dependency, fatherless child-rearing (defined by the absence of the biological father from the households in which a cohort member’s offspring live), tobacco smoking, excess body weight, admissions to taxpayer-funded national-health-service hospitals, taxpayer-funded prescription drug fills, taxpayer-funded insurance claims paid out for accidents and injuries, and convictions for crime (Figure 1). Analyses tested how strongly childhood risks predicted these economically burdensome outcomes in this cohort.
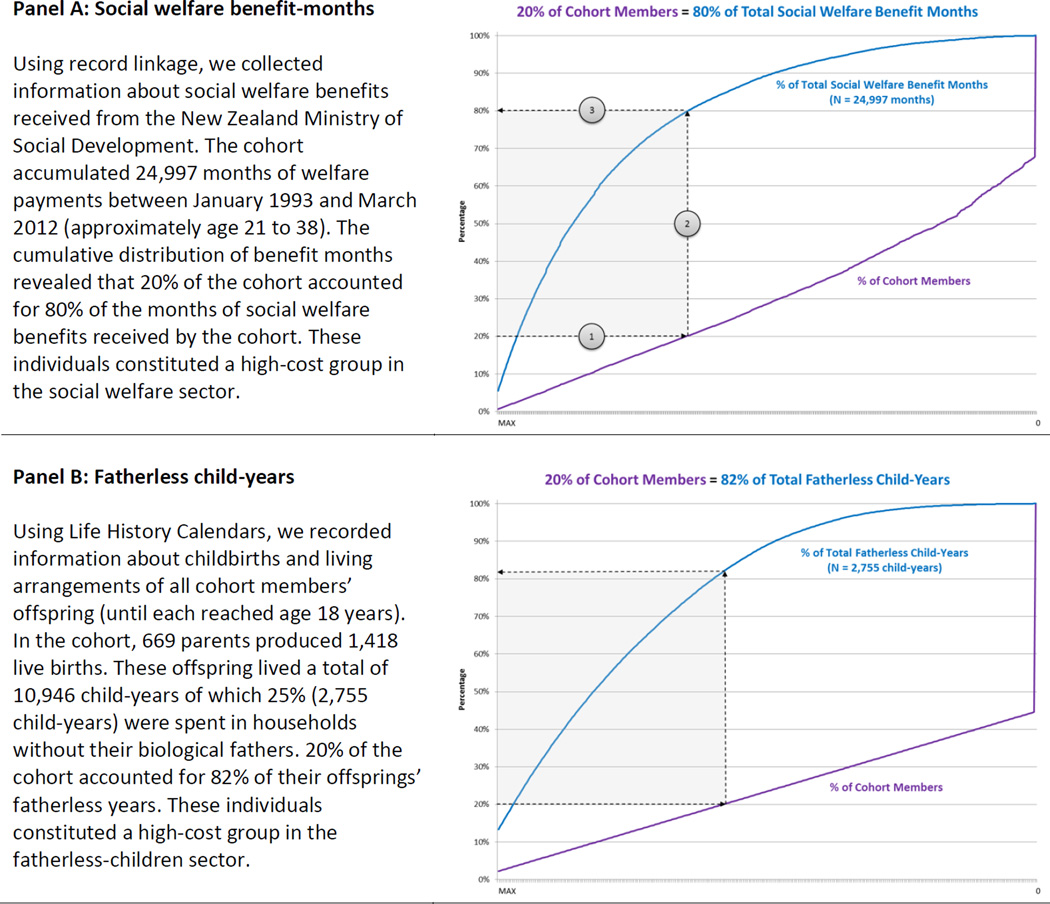
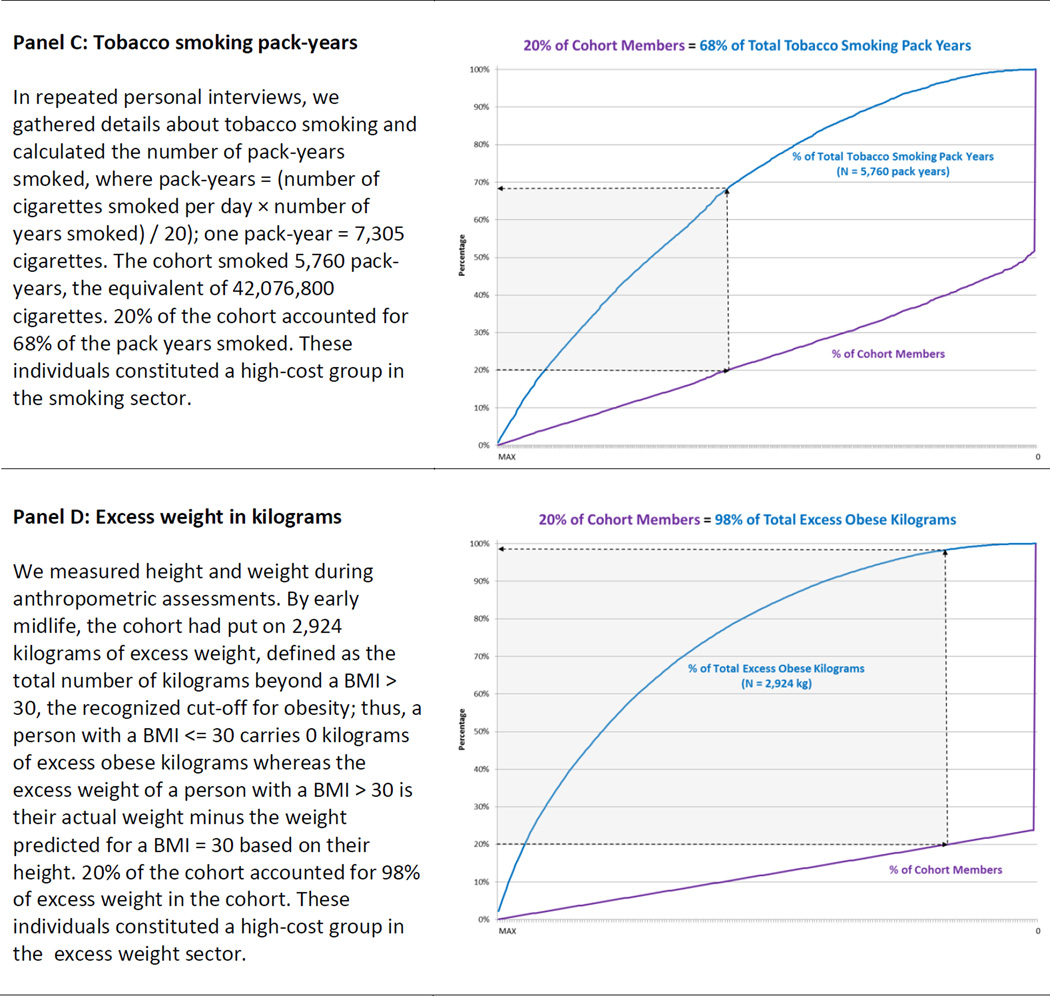
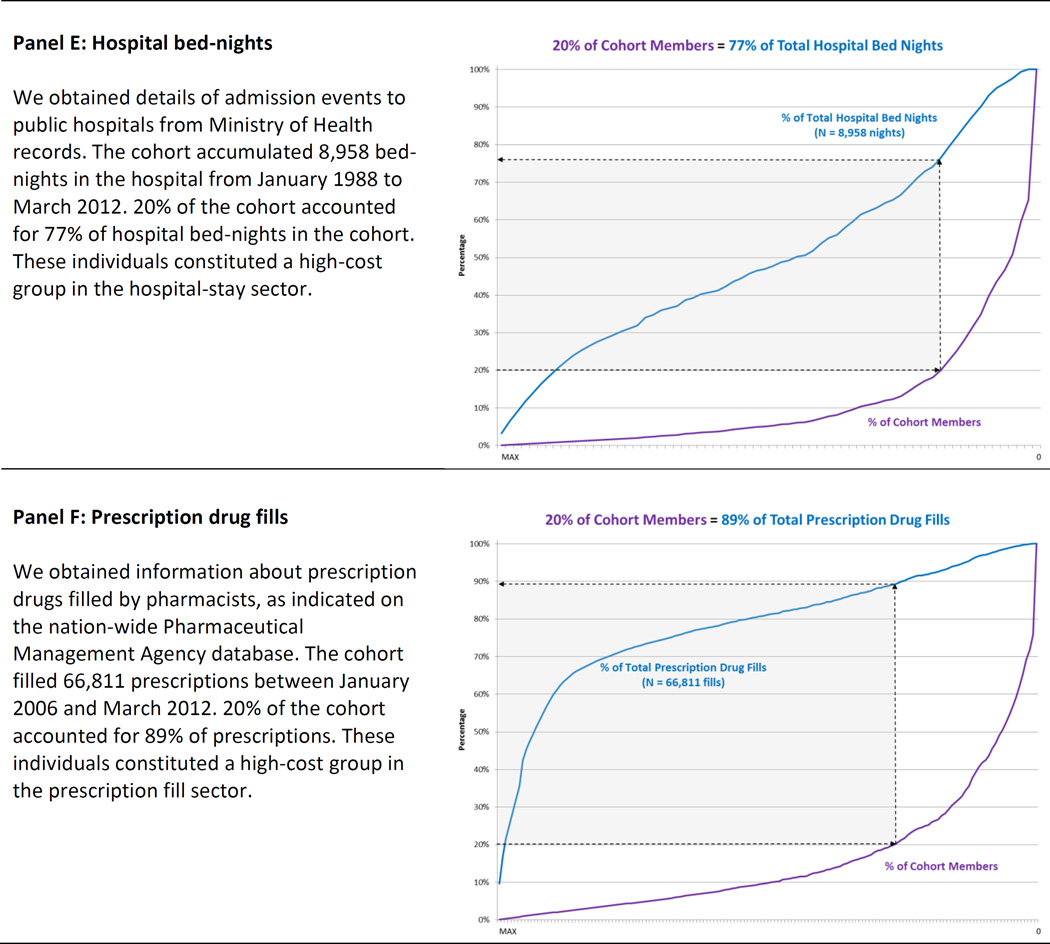
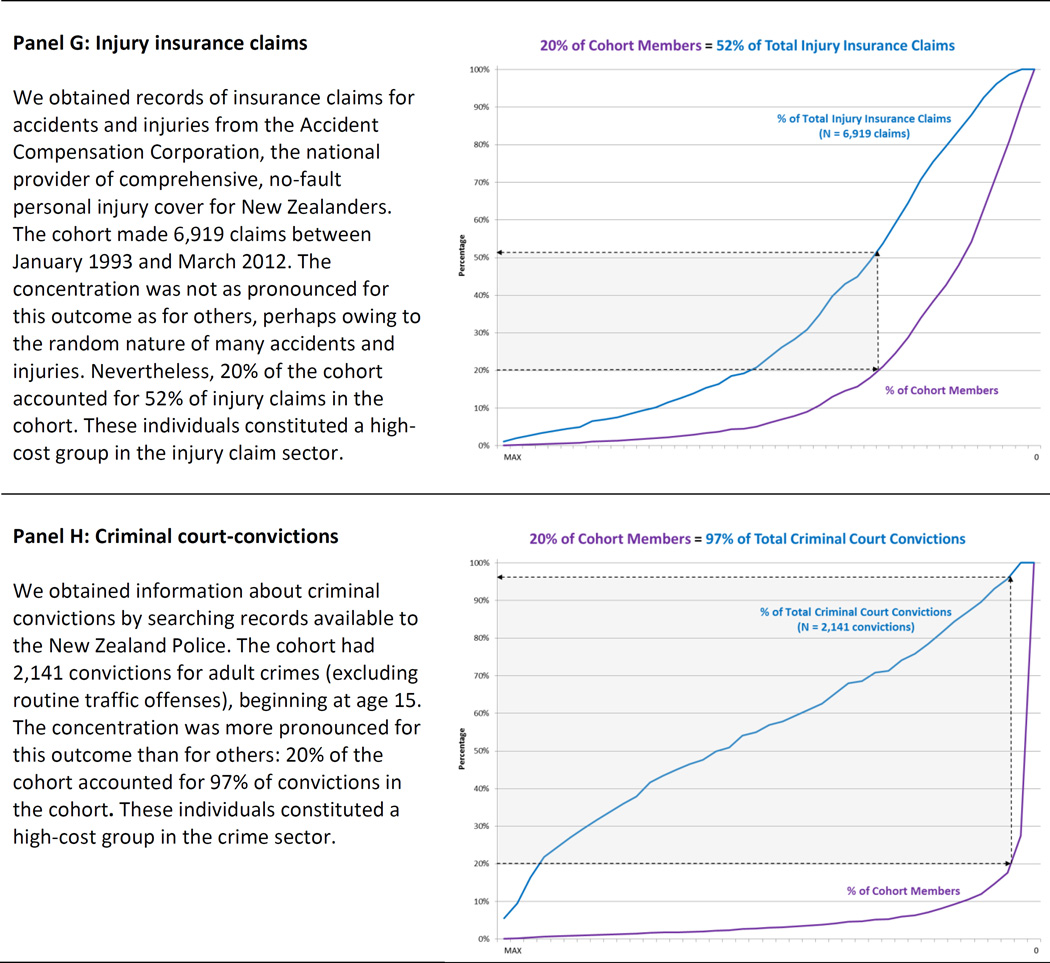
Figure 1.
Measuring the concentration of economic-burden outcomes in a birth cohort. The data represent information about 940 people who were born in one hospital in 1972-73 and are life-long participants in the Dunedin Longitudinal Study. The panels show that a minority of individuals accounts for a majority of outcomes in a birth cohort, in each of 8 different social and health sectors: social welfare (Panel A), fatherless children (Panel B), smoking (Panel C), excess obese kilograms (Panel D), hospital stays (Panel E), prescription fills (Panel F), injury claims (Panel G), and crime (Panel H). Each Panel displays the cumulative distribution of an outcome in the cohort. To find the proportion of each outcome that 20% of the population accounts for, start at 20% on the vertical axis and follow arrow 1 to the right, to the purple line; then, follow arrow 2 up to the blue line; and then follow arrow 3 to the left, back to the vertical axis to find the corresponding proportion of the total.
Prospective-longitudinal cohort studies have tackled the prediction question before 23. Here we draw attention to two infrequently tried approaches to prediction. Our first fresh approach was to predict the concentration of each economically burdensome behaviour by focusing on its cumulative distribution across the cohort. Typically, prediction has focused on dimensional outcomes, such as the number of crime convictions accrued by a person, or nominal outcomes, such as whether the person is a convicted offender or not. Instead, we noted that most economically burdensome outcomes have a markedly skewed distribution, and accordingly defined our prediction target as the small group of cohort members who could be considered high-cost because they accounted for an excessive amount of an outcome (e.g., a few individuals account for the majority of criminal convictions and are thus high-cost users of the criminal justice sector). To define this concentration, we followed the lead of Vilfredo Pareto who, over 100 years ago, observed that 80% of ‘effects’ emanate from 20% of ‘sources’ 24. In Pareto’s day, the problem definition was that 20% of families owned 80% of land in Italy. The so-called Pareto principle is alive and useful today: For example, in software engineering, 20% of the code is said to contain 80% of the errors 25. Here, we studied each outcome variable measured in units that could be meaningfully counted (e.g., tobacco pack-years, hospital bednights, prescription fills, criminal convictions, etc.). Such measures allowed us to identify the minority of individuals who accounted for the majority of each economically burdensome outcome.
Our second fresh approach was to predict the aggregation of different types of economically burdensome behavioural outcomes. Economic analyses of early-years interventions illustrate the advantages of estimating costs associated with multiple outcomes 26. However, typical approaches to prediction in population studies continue to predict only one outcome at a time. We noted that some cohort members appeared to be engaged in economically burdensome behaviour across multiple health and social sectors. This observation suggests a relatively small population segment may generate a large share of societal costs. If this is true, this group would be a high value target for prevention. We hypothesized that predicting such “aggregated concentration” would yield stronger estimates of prediction from childhood to adulthood than reported in previous research. We analyzed aggregation as the second step, after analyzing concentration.
Adult outcomes were concentrated as anticipated from the Pareto principle (or ‘80–20 rule’). Cumulative distribution functions showed that, in each of the eight social and health sectors where we collected data, 20% of individuals consistently accounted for a disproportionate share (close to 80%) of the outcome (Figure 1, Panels A–H). These distributions led us to operationally define a high-cost group in each sector as 20% of the cohort members who accounted for a disproportionate share in that sector.
We observed that members of the high-cost group in every sector could be differentiated from their peers by the same four childhood disadvantages: they tended to have grown up in more socioeconomically deprived environments; experienced child maltreatment; scored poorly on childhood IQ tests; and exhibited low childhood self-control (Table 1). The predictions were fairly uniform across each of the eight different social and health sectors, with the exception of injury claims. In addition to being less concentrated within a high-cost group, injury claims were less strongly associated with childhood risk factors.
Table 1.
Childhood predictors of economic-burden outcomes in a birth cohort. The Table shows that children who grew up in socioeconomically deprived environments, who experienced child maltreatment, who scored more poorly on childhood IQ tests, and who exhibited less self-control were more likely to belong to a high-cost economic burden group as adults, in each of 8 different sectors.
| Predicting High-Cost in Each of 8 Different Sectors |
Univariate Models | Multivariate Models | ||||||
|---|---|---|---|---|---|---|---|---|
| RR | RR 95% CI | AUC | AUC 95% CI | RR | RR 95% CI | AUC | AUC 95% CI | |
| Social Welfare * | 0.78 | (0.74, 0.82) | ||||||
| Childhood Low SES | 1.47 | (1.28, 1.69) | 0.73 | (0.69, 0.77) | 1.18 | (1.02, 1.36) | ||
| Child Maltreatment | 1.47 | (1.33, 1.62) | 0.74 | (0.70, 0.78) | 1.31 | (1.18, 1.46) | ||
| Childhood Low IQ | 1.50 | (1.37, 1.65) | 0.73 | (0.69, 0.77) | 1.19 | (1.05, 1.34) | ||
| Childhood Low Self-Control | 1.51 | (1.37, 1.65) | 0.75 | (0.71, 0.79) | 1.24 | (1.10, 1.39) | ||
| Fatherless Children | 0.67 | (0.62, 0.72) | ||||||
| Childhood Low SES | 1.39 | (1.17, 1.65) | 0.63 | (0.58, 0.68) | 1.24 | (1.03, 1.49) | ||
| Child Maltreatment | 1.36 | (1.19, 1.56) | 0.63 | (0.58, 0.68) | 1.26 | (1.09, 1.46) | ||
| Childhood Low IQ | 1.26 | (1.09, 1.47) | 0.62 | (0.56, 0.67) | 1.04 | (0.86, 1.26) | ||
| Childhood Low Self-Control | 1.33 | (1.18, 1.50) | 0.64 | (0.59, 0.69) | 1.15 | (0.99, 1.34) | ||
| Smoking | 0.69 | (0.65, 0.74) | ||||||
| Childhood Low SES | 1.50 | (1.30, 1.73) | 0.64 | (0.60, 0.69) | 1.29 | (1.11, 1.50) | ||
| Child Maltreatment | 1.34 | (1.21, 1.49) | 0.61 | (0.56, 0.66) | 1.20 | (1.06, 1.35) | ||
| Childhood Low IQ | 1.36 | (1.21, 1.53) | 0.64 | (0.59, 0.68) | 1.08 | (0.93, 1.25) | ||
| Childhood Low Self-Control | 1.43 | (1.30, 1.57) | 0.65 | (0.60, 0.70) | 1.21 | (1.07, 1.37) | ||
| Excess obese kilograms | 0.61 | (0.56, 0.65) | ||||||
| Childhood Low SES | 1.26 | (1.11, 1.43) | 0.59 | (0.55, 0.64) | 1.16 | (1.00, 1.35) | ||
| Child Maltreatment | 1.13 | (1.01, 1.28) | 0.56 | (0.52, 0.61) | 1.09 | (0.96, 1.24) | ||
| Childhood Low IQ | 1.24 | (1.10, 1.40) | 0.58 | (0.53, 0.63) | 1.14 | (0.97, 1.34) | ||
| Childhood Low Self-Control | 1.18 | (1.06, 1.32) | 0.57 | (0.52, 0.62) | 1.04 | (0.89, 1.20) | ||
| Hospital Stays * | 0.75 | (0.71, 0.79) | ||||||
| Childhood Low SES | 1.35 | (1.18, 1.54) | 0.74 | (0.70, 0.78) | 1.23 | (1.07, 1.43) | ||
| Child Maltreatment | 1.14 | (1.02, 1.29) | 0.72 | (0.68, 0.76) | 1.06 | (0.93, 1.20) | ||
| Childhood Low IQ | 1.26 | (1.12, 1.43) | 0.73 | (0.69, 0.77) | 1.09 | (0.95, 1.26) | ||
| Childhood Low Self-Control | 1.27 | (1.14, 1.42) | 0.74 | (0.70, 0.77) | 1.15 | (1.01, 1.32) | ||
| Prescription Fills * | 0.75 | (0.71, 0.78) | ||||||
| Childhood Low SES | 1.27 | (1.11, 1.44) | 0.73 | (0.70, 0.77) | 1.18 | (1.03, 1.37) | ||
| Child Maltreatment | 1.10 | (0.98, 1.25) | 0.71 | (0.67, 0.74) | 1.02 | (0.89, 1.17) | ||
| Childhood Low IQ | 1.30 | (1.16, 1.45) | 0.73 | (0.70, 0.77) | 1.14 | (0.99, 1.32) | ||
| Childhood Low Self-Control | 1.25 | (1.12, 1.39) | 0.73 | (0.70, 0.77) | 1.11 | (0.98, 1.27) | ||
| Injury Claims * | 0.74 | (0.71, 0.78) | ||||||
| Childhood Low SES | 1.18 | (1.03, 1.34) | 0.74 | (0.70, 0.78) | 1.19 | (1.02, 1.38) | ||
| Child Maltreatment | 1.03 | (0.92, 1.16) | 0.73 | (0.69, 0.77) | 0.98 | (0.86, 1.12) | ||
| Childhood Low IQ | 1.07 | (0.95, 1.20) | 0.73 | (0.69, 0.77) | 0.95 | (0.82, 1.10) | ||
| Childhood Low Self-Control | 1.12 | (1.01, 1.24) | 0.74 | (0.70, 0.78) | 1.09 | (0.95, 1.24) | ||
| Crime * | 0.77 | (0.74, 0.80) | ||||||
| Childhood Low SES | 1.36 | (1.22, 1.52) | 0.74 | (0.70, 0.77) | 1.24 | (1.11, 1.39) | ||
| Child Maltreatment | 1.31 | (1.20, 1.43) | 0.73 | (0.70, 0.77) | 1.18 | (1.07, 1.30) | ||
| Childhood Low IQ | 1.19 | (1.08, 1.31) | 0.72 | (0.68, 0.76) | 0.93 | (0.83, 1.04) | ||
| Childhood Low Self-Control | 1.35 | (1.25, 1.46) | 0.75 | (0.71, 0.79) | 1.26 | (1.15, 1.38) | ||
Childhood socioeconomic status (SES), IQ, and self-control are standardized z-scores (M = 0, SD = 1); childhood maltreatment is coded as 0 = none, 1 = probable, 2 = definite maltreatment. All models control for sex. Prediction was the same when men and women were analyzed separately (see Supplemental materials for details).
Time spent outside New Zealand is added as a covariate in analyses that use New Zealand administrative data.
RR = Risk Ratio; AUC = Area Under the Curve; CI = Confidence Interval
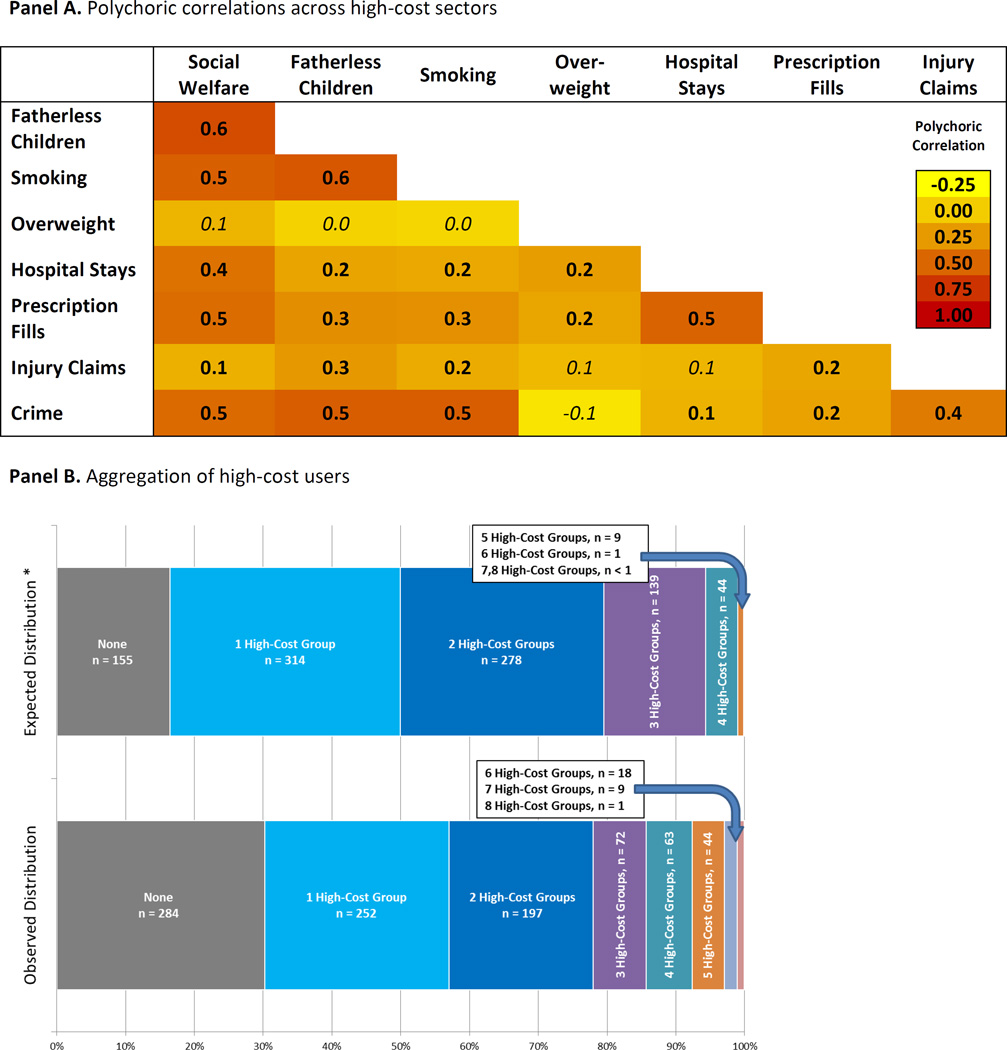
Figure 1 and Table 1 both focus on one sector at a time. However, a heat-map (Figure 2, Panels A and B) showed that high-cost group members in one sector were often significantly more likely to reappear as high-cost in other sectors too, and that the observed distribution of high-cost individuals across multiple sectors deviated from the distribution that would be expected if the high-cost groups were independent, χ2 (7, N=940)= 2103.44, p<0.001. The fact that membership in one high-cost group is associated with greater likelihood of membership in other high-cost groups re-framed the prediction question: How well could childhood risks predict the number of high-cost groups to which an individual belonged?
Figure 2.
The aggregation of adult economic-burden outcomes. The polychoric correlations in Panel A show that high-cost group members in one sector were significantly more likely to re-appear as high-cost in other sectors. Panel B shows that the distribution of high-cost individuals across multiple sectors deviated from the expectation of a random distribution, χ2 (7, N = 940) = 2103.44, p < 0.001, with excesses at the two tails (i.e., there are more people than expected who do not belong to any high-cost group and there are more people than expected who belong to multiple high-cost groups). The expected distribution is based on the assumption that the high-cost groups were independent and did not overlap beyond chance. The observed:expected ratios in each cell are: 1.83, .80, .71, .52, 1.45, 5.09, 16.89, 120.53, 439.47.
At a population level, each of the childhood factors was a statistically significant predictor of risk for belonging to more high-cost groups (Table 2, Panels A & B). Prediction was the same when men and women were analyzed separately (Supplemental Material). However, this population-level analysis did not answer the question of whether childhood factors were useful in predicting the outcome of an individual child 27. We evaluated the accuracy of individual predictions by applying receiver operating characteristic (ROC) curve analysis. A ROC curve plots the sensitivity and specificity of prediction at various thresholds and yields a metric indexing predictive accuracy: the Area Under the Curve 28. The Area Under the Curve reflects the probability of correctly classifying any randomly selected pair of cohort members in which one person belongs to a high-cost group and the other does not. It can take on any value between 0.50 (indicating chance prediction) and 1.00 (indicating perfect prediction). Some pundits grade the values as: worthless (0.5–0.6), poor (0.6–0.7), fair (0.7–0.8), good (0.8–0.9), and excellent (0.9–1.0). Behavioural scientists note that AUC values of 0.54, 0.64, and 0.71 correspond to Cohen’s d values of 0.20, 0.50, and 0.80, which are regarded as small, medium, and large effects, respectively 29. Using the standards of medical research, values approaching 0.8 suggest adequate discrimination for consideration in decision-making aboutintervention 30.
Table 2.
Childhood predictors of economic-burden outcomes in a birth cohort. Panel A shows that children who grew up in socioeconomically deprived environments, who experienced child maltreatment, who scored more poorly on childhood IQ tests, and who exhibited less self-control were more likely to belong to more high-cost economic-burden groups in adulthood (ranging from 0–8). PanelB shows that these childhood factors differentiated a group of cohort members who became, as adults, members of the multiple-high-cost segment of their society.
| Panel A: Predicting Number of High-Cost Sectors (range 0–8) |
Univariate Models | Multivariate Models | ||||||
|---|---|---|---|---|---|---|---|---|
| IRR | IRR 95% CI | IRR | IRR 95% CI | |||||
| Number of High-Cost Sectors * | ||||||||
| Childhood Low SES | 1.33 | (1.25, 1.42) | 1.21 | (1.13, 1.29) | ||||
| Child Maltreatment | 1.23 | (1.17, 1.30) | 1.13 | (1.07, 1.20) | ||||
| Childhood Low IQ | 1.26 | (1.18, 1.34) | 1.05 | (0.98, 1.13) | ||||
| Childhood Low Self-Control | 1.32 | (1.25, 1.40) | 1.18 | (1.11, 1.26) | ||||
|
Panel B: Predicting the Multiple-High-Cost Sector |
RR | RR 95% CI | AUC | AUC 95% CI | RR | RR 95% CI | AUC | AUC 95% CI |
| 0 vs 1 High-Cost Sectors * | 0.67 | (0.62, 0.72) | ||||||
| Childhood Low SES | 1.20 | (1.08, 1.32) | 0.66 | (0.61, 0.71) | 1.17 | (1.06, 1.30) | ||
| Child Maltreatment | 1.12 | (1.02, 1.22) | 0.64 | (0.59, 0.69) | 1.08 | (0.98, 1.18) | ||
| Childhood Low IQ | 1.07 | (0.97, 1.18) | 0.62 | (0.57, 0.67) | 0.97 | (0.88, 1.08) | ||
| Childhood Low Self-Control | 1.16 | (1.06, 1.27) | 0.65 | (0.60, 0.70) | 1.10 | (0.99, 1.21) | ||
| 0 vs 2 High-Cost Sectors * | 0.73 | (0.69, 0.78) | ||||||
| Childhood Low SES | 1.23 | (1.10, 1.37) | 0.69 | (0.64, 0.74) | 1.12 | (1.00, 1.26) | ||
| Child Maltreatment | 1.07 | (0.96, 1.19) | 0.66 | (0.61, 0.71) | 1.00 | (0.89, 1.12) | ||
| Childhood Low IQ | 1.33 | (1.20, 1.48) | 0.71 | (0.67, 0.76) | 1.16 | (1.01, 1.32) | ||
| Childhood Low Self-Control | 1.29 | (1.19, 1.39) | 0.72 | (0.68, 0.77) | 1.19 | (1.07, 1.31) | ||
| 0 vs 3+ High-Cost Sectors = Multiple-High-Cost * | 0.87 | (0.84, 0.90) | ||||||
| Childhood Low SES | 1.49 | (1.35, 1.64) | 0.83 | (0.79, 0.86) | 1.31 | (1.18, 1.45) | ||
| Child Maltreatment | 1.28 | (1.19, 1.37) | 0.8 | (0.76, 0.84) | 1.14 | (1.05, 1.23) | ||
| Childhood Low IQ | 1.35 | (1.24, 1.47) | 0.81 | (0.77, 0.85) | 1.08 | (0.98, 1.20) | ||
| Childhood Low Self-Control | 1.38 | (1.27, 1.49) | 0.84 | (0.80, 0.87) | 1.17 | (1.07, 1.29) | ||
Childhood socioeconomic status (SES), IQ, and self-control are standardized z-scores (M = 0, SD = 1); childhood maltreatment is coded as 0 = none, 1 = probable, 2 = definite maltreatment. All models control for sex. Prediction was the same when men and women were analyzed separately (see Supplemental materials for details).
Time spent outside New Zealand is added as a covariate in analyses that use New Zealand administrative data.
RR = Risk Ratio; IRR = Incidence Rate Ratio; AUC = Area Under the Curve; CI = Confidence Interval
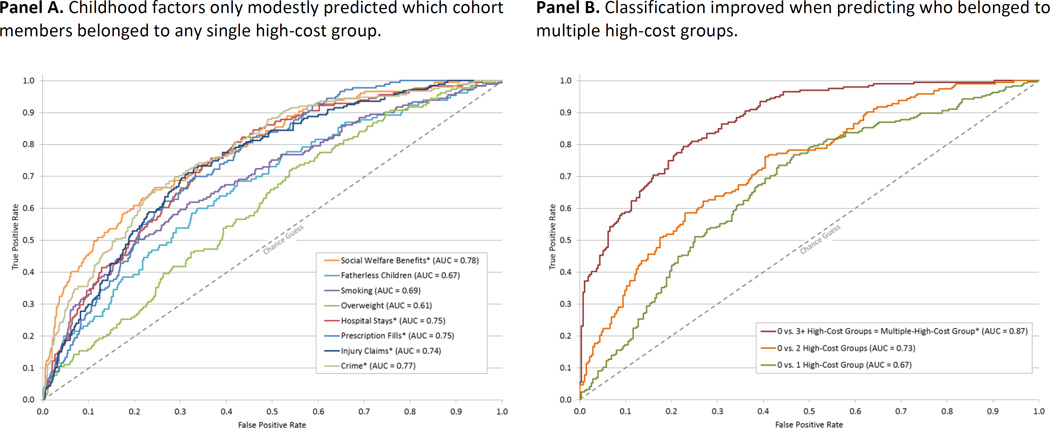
The four childhood risks predicted which cohort members belonged to any particular single high-cost group with poor-to-fair accuracy (Figure 3, Panel A). However, as hypothesized, prediction improved when we turned to predict who belonged to multiple high-cost groups (Figure 3, Panel B). Hereafter this article refers to individuals who belonged to three or more high-cost outcome groups as the “multiple-high-cost population segment.” The multiple-high-cost segment comprised 22% of the Dunedin cohort (N = 207 of 940 cohort members). Childhood socio-economic deprivation, maltreatment, low IQ, and poor self-control predicted these multiple-high-cost adults with considerable accuracy, as indicated by an Area Under the Curve of 0.87 (approaching excellent). To answer the question of whether accurate prediction of the multiple-high-cost segment capitalized on the fact that high-cost membership in one particular sector (e.g., crime sector, welfare sector, etc.) could be predicted well, sensitivity analyses were undertaken, in which each high-cost group was left out one sector at a time, in turn. Results showed that accurate prediction was not simply an artifact of predicting well in any one sector (Figure 3, Panel C).
Figure 3.
Predicting the probability of economic-burden outcomes. In Panels A-C we tested the predictive performance of a model that included information about four childhood risk factors. We assessed discrimination (that is, the model’s ability to classify correctly) using the area under the receiver-operating-characteristic curve (AUC). The diagonal line in each panel indicates random classification. Points above the diagonal represent good (better than random) classification results. Panel A shows that childhood factors only modestly predicted which cohort members belonged to any particular single high-cost group. Panel B shows that classification improved when predicting who belonged to multiple high-cost groups. Panel C shows the results of a leave-one-out analysis and documents that accurate prediction was not simply an artifact of predicting one high-cost group well. Panel D shows that, reaching back to early childhood, age-3 brain health predicted which cohort members belonged to multiple high-cost groups. All models included sex. Models in Panels A-C included childhood socioeconomic status (SES), childhood maltreatment, IQ,and self-control. * Time spent outside New Zealand is added as a covariate in analyses that use New Zealand administrative data. AUC = Area Under the Curve.
Our prediction was based on risk measures (familial socioeconomic characteristics, maltreatment, IQ, and self-control) that we constructed using repeated measurements collected across the first decade of children’s lives. However, multi-wave risk measurement is not a realistic standard that can be achieved by many other studies, nor implemented by policy analysts. Moreover, multi-wave measures from birth to age-11 years did not address the possible importance of early-childhood interventions targeting preschoolers. As such, we asked: how well could outcomes be predicted from a single brief evaluation of each child, using a standard pediatric assessment during the preschool years?
At age three years, each child in the cohort participated in a 45-minute examination that included assessments of neurological soft signs, intelligence, receptive language, and motor skills, and afterwards the examiners (having no prior knowledge of the child) rated each child’s frustration tolerance, resistance, restlessness, impulsivity, and lack of persistence in reaching goals. This examination yielded a summary index we have termed brain health, a global index of the three-year-old’s neurocognitive status 31 (Supplemental Material). Variation in age-three brain health significantly predicted economically burdensome outcomes in each sector, except injury claims (Table 3). Moreover, variation in cohort members’ age-three brain health predicted with considerable accuracy which individuals would 35 years later be members of the multiple-high cost segment, with an Area Under the Curve of 0.79 (Figure 3, Panel D).
Table 3.
Variation in children’s age-3 brain health predicted which children belonged to high-cost economic-burden groups, 35 years later. Panel A shows that variation in age-3 brain health predicted who was more likely to belong to a high-cost group in adulthood, in each of 8 different sectors. Panel B shows that age-3 brain health predicted the number of high-cost groups (ranging from 0–8) to which each cohort member belonged. Panel C shows that age-3 brain health differentiated cohort members who became, as adults, members of the multiple-high-cost segment of their society.
| Panel A: Predicting High-Cost in Each of 8 Different Sectors |
RR | RR 95% CI | AUC | AUC 95% CI |
|---|---|---|---|---|
| Social Welfare * | 1.38 | (1.25, 1.53) | 0.73 | (0.69, 0.77) |
| Fatherless Children | 1.22 | (1.07, 1.38) | 0.61 | (0.56, 0.66) |
| Smoking | 1.25 | (1.12, 1.40) | 0.60 | (0.55, 0.64) |
| Excess obese kilograms | 1.15 | (1.02, 1.29) | 0.56 | (0.52, 0.61) |
| Hospital Stays * | 1.18 | (1.05, 1.34) | 0.72 | (0.68, 0.76) |
| Prescription Fills * | 1.23 | (1.10, 1.38) | 0.73 | (0.69, 0.76) |
| Injury Claims * | 1.10 | (0.99, 1.23) | 0.74 | (0.70, 0.77) |
| Crime* | 1.19 | (1.09, 1.29) | 0.72 | (0.68, 0.75) |
|
Panel B: Predicting Number of High-Cost Sectors (range 0–8) |
IRR | IRR 95% CI | ||
| Number of High-Cost Sectors * | 1.20 | (1.13, 1.27) | ||
| Panel C: Predicting the Multiple-High-Cost Sector | RR | RR 95% CI | AUC | AUC 95% CI |
| 0 vs. 1 High-Cost Sectors * | 1.03 | (0.94, 1.14) | 0.62 | (0.57, 0.67) |
| 0 vs. 2 High-Cost Sectors * | 1.17 | (1.07, 1.28) | 0.68 | (0.63, 0.73) |
| 0 vs. 3+ High-Cost Sectors * | 1.26 | (1.17, 1.36) | 0.79 | (0.75, 0.83) |
All models control for sex. Prediction was the same when men and women were analyzed separately (see Supplemental materials for details).
Time spent outside New Zealand is added as a covariate in analyses that use New Zealand administrative data.
RR = Risk Ratio; IRR = Incidence Rate Ratio; AUC = Area Under the Curve; CI = Confidence Interval
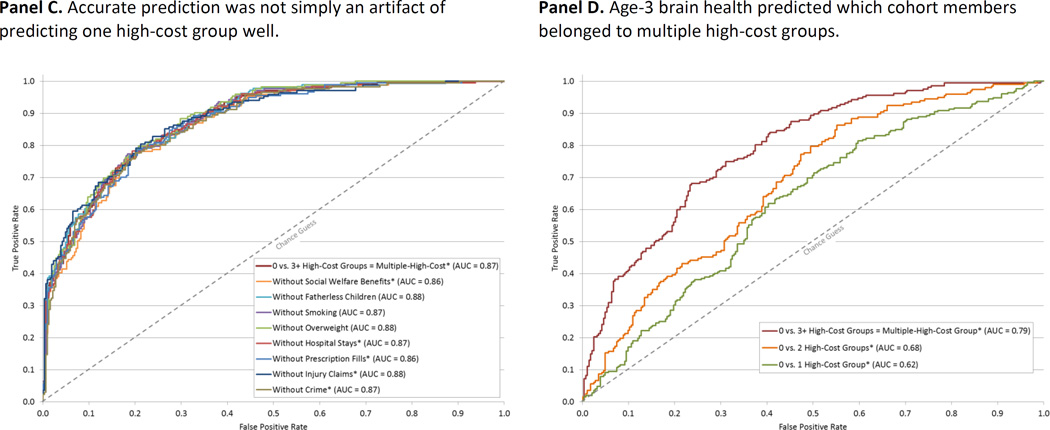
Is this multiple-high-cost population segment a priority prevention target? This group was operationally defined as individuals belonging to three or more high-cost groups. They made up only 22% of their age cohort born in one year in one city. However, they left a big footprint on costs of service delivery (Figure 4, Panel A). By age 38 years they used 66% of the birth cohort’s welfare benefits; accounted for 77% of the next generation’s years growing up fatherless; smoked 54% of the cohort’s tobacco cigarettes; carried 40% of the cohort’s kilograms of overweight; occupied 57% of their cohort’s hospital bed-nights; filled 78% of all prescriptions; were convicted for 81% of the crimes charged to the cohort; and even made a disproportionate number (36%) of injury claims. In contrast, the data also reveal a substantial segment of the cohort (30%) who did not belong to the high-cost group in any sector. Figure 4, Panel B shows that this group has left an unusually small footprint on their society so far.
Figure 4.
The big footprint of multiple-high-cost users. Panel A shows that although the multiple-high-cost group made up only 22% of the cohort (N = 207), it accounted for a disproportionate share of economic-burden outcomes across all 8 health and social sectors that we examined. In contrast, Panel B shows that a substantial segment of the cohort did not belong to any high-cost group (30%; N = 289) and left an unusually light footprint on society.
Discussion
This research yielded two results. First, the study uncovered a population segment that featured as high-cost across multiple health and social sectors. This illustrates the potential discovery value offered by data integration of multiple longitudinal administrative databases and electronic health records. Without such data, this population segment would have remained hidden. Second, by linking administrative data with individual-level longitudinal data, the study provides the strongest effect sizes yet measuring the connection between an at-risk childhood and costly adult outcomes in the population. The prediction was excellent when it relied on multiple risk factors measured during the first decade of children’s lives, and was still good when it relied on information derived from a relatively brief assessment of brain health when the children were three years old. Given two three-year-old children (one who grew up to belong to multiple high-cost groups and one who grew up to belong to none), the model was able to classify them accurately 80% of the time. If this pattern of findings is replicated elsewhere, it will imply that early-years interventions, if efficiently effective with this population segment, have the opportunity to make very large reductions in economic burden. How much economic burden can be reduced remains an empirical question at present. However, historical interventions that have targeted children on the basis of low IQ have proven effective with good a rate of return, giving reason for optimism 32.
This research has limitations. First, results reflect the New Zealand context and a specific historical period. New Zealand is a useful laboratory because it suffers income inequalities similar to the USA and the UK (after-tax Gini coefficient: NZ=0.33, UK=0.34, US=0.37) 33, spends a comparable amount on health care (NZ=10%, UK=9%, US=17% of GDP) 34, has a national health-care system, and, has a generous social safety net. Nevertheless, geographical and generational variations require investigation. Second, using 20% to identify a vital proportion of the population may seem arbitrary, but rather than choosing a sample-specific operant, we chose the Pareto principle a priori as a useful rule-of-thumb because it is familiar to researchers, policy makers, and the public. Third, the data were right-hand censored at age 38 years, and we could not test how well early childhood risks predict economically burdensome outcomes across the full life course. This is an important question because the health-care burden of developed societies concentrates in older age groups. To the extent that factors such as smoking, excess weight, and health problems during midlife foretell health-care burden and social dependency, findings here should extend to later life (keeping in mind that midlife smoking, overweight, and health problems also forecast premature mortality). Fourth, this article addresses the strength of prediction only; we did not address causal mechanisms behind the predictive associations reported here. Whether the risk factors studied here are causal, or whether they mediate other prior causal influences, the finding that economically burdensome adult outcomes are predictable from these early-life factors with moderate to strong effects suggests that these risk factors are not unreasonable targets for randomized experimental intervention trials. Moreover, many interventions have treated risk factors that are not root causes, and improved outcome nevertheless. Fifth, we are unable to directly compare costs across sectors because we did not monetize outcomes within each sector. Although the multiple high-cost group is clearly ‘expensive’, we did not convert each of our outcomes (e.g., pack years of smoking, criminal convictions, injury insurance claims) to (New Zealand) dollars, for the following three reasons: Monetizing outcomes is informative when evaluating return on investment of an intervention of known cost, but we did not study an intervention26. Monetizing costs is not without assumptions, and estimates are time- and place-specific. Compared to New-Zealand-specific monetized estimates the concentration metric reported here will be a more feasible target for replication and extension studies. The concentration metric can be used, for example, to ask whether high-cost groups aggregate to the same extent in different times and places, whether the same risk factors predict a multiple-high-cost group across time and place, and how historical events such as economic recessions or immigration affect high-cost distributions.
As a final limitation, we are aware that from a different perspective, the economically burdensome behaviours we have studied can be considered economically generative, or at least neutral. Smokers fuel the tobacco industry; crime provides jobs in policing, courts, and corrections; hospital admissions, prescription fills, and injury insurance claims animate health-care and pharmaceutical industries. Such cost-benefit analyses were beyond our scope. Moreover, it is not we who designated these outcomes as burdensome; rather, we selected them because they are oft-cited long-term targets of early-years intervention policy 22,35
This research revealed a predictable aggregation of different economically-burdensome adult outcomes in the same multiple-high-cost segment of the population. This aggregation has implications for methodology, prevention science, and human rights. Methodologically, the finding illustrates that social-science research on risk prediction can benefit from considering the accumulation of outcomes within a life. Social scientists have observed that failure to aggregate information about risk predictors results in small or null effects in prediction 36,37, but the recommendation to aggregate has typically been applied only to predictor variables, such as when studying cumulative disadvantage or adverse childhood experiences 38 39. We turned this recommendation on its head, by showing how aggregating outcome variables, not just predictors, can improve effect sizes in longitudinal prediction research. Such aggregation has been used in medical epidemiology, for example to index the cumulative deficits associated with aging 40, but it is rarely used in the social and behavioural sciences. Treatment studies, as well as observational studies, can make use of this principle to more comprehensively evaluate impact. Moreover, health, social, and justice sectors might benefit from understanding that the bulk of their services are going to the same clients.
The finding also has implications for early-years prevention science 2,41–43. We sought to inform a question which nags the behavioural and social sciences, and which has strategic consequences for national policy on children: How strong is the connection between childhood risk and future costly life-course outcomes? Results reported here suggest that the importance of childhood risks for poor adult outcomes has generally been underestimated. It is not news to service-delivery professionals that some individuals use more than their share of services. What is news is that individuals feature in multiple service sectors and they can be identified as children, with reasonable accuracy. The question for intervention science becomes not just “what works?” but “what works for this multiple-high-cost population segment of children?”
Finally, the finding has implications for human rights. We aimed to test if population segmentation could give a more accurate evidence base to clarify the need for early-years intervention. We are aware of potential for misuse; population segments are often stigmatized and stereotyped. However, the predictions reported here make clear that the most costly adults in our cohort started the race of life from a starting block somewhere behind the rest, and while carrying a heavy handicap in brain health. Such a disadvantaged citizen is unlikely to be able to cover his or her share of health and social costs, but there is no merit in blaming the victim for economic burden following from childhood disadvantage. Instead, ameliorating the effects of childhood disadvantage is an important aim 44,45 and achieving this through early-years support for families and children could benefit all members of a society.
Method
A more detailed report of the study design, measurement, and statistical analysis is provided in the Supplemental Material.
Dunedin Study Sample
Participants are members of the Dunedin Multidisciplinary Health and Development Study, which tracks the development of 1,037 individuals born in 1972–1973 in Dunedin, New Zealand 46.
Measuring economic-burden outcomes
We drew on personal interviews and on New Zealand’s multiple nationwide administrative databases and electronic medical records to ascertain the cumulative distributions of eight economically burdensome outcomes (Figure 1, Panels A–H):
(Panel A) Social welfare benefit-months
Using record linkage, we collected information about social welfare benefits received from the New Zealand Ministry of Social Development. The cohort accumulated 24,997 months of welfare payments between January 1993 and March 2012 (approximately age 21 to 38). The cumulative distribution of benefit months revealed that 20% of the cohort accounted for 80% of the months of social welfare benefits received by the cohort. These individuals constituted a high-cost group in the social welfare sector.
(Panel B) Fatherless child-years (defined by the absence of the biological father from the households in which a cohort member’s offspring live). Using Life History Calendars, we recorded information about childbirths and living arrangements of all cohort members’ offspring (until each reached age 18 years). In the cohort, 669 parents produced 1,418 live births. These offspring lived a total of 10,946 child-years of which 25% (2,755 child-years) were spent in households without their biological fathers. 20% of the cohort accounted for 82% of their offsprings’ fatherless years. These individuals constituted a high-cost group in the fatherless-children sector.
(Panel C) Tobacco smoking pack-years
In repeated personal interviews, we gathered details about tobacco smoking and calculated the number of pack-years smoked, where pack-years = (number of cigarettes smoked per day × number of years smoked) / 20); one pack-year = 7,305 cigarettes. The cohort smoked 5,760 pack-years, the equivalent of 42,076,800 cigarettes. 20% of the cohort accounted for 68% of the pack years smoked. These individuals constituted a high-cost group in the smoking sector.
(Panel D) Excess obese kilograms
We measured height and weight during anthropometric assessments. By early midlife, the cohort had put on 2,924 kilograms of excess weight, defined as the total number of kilograms beyond a BMI > 30, the recognized cut-off for obesity; thus, a person with a BMI <= 30 carries 0 kilograms of excess obese kilograms whereas the excess weight of a person with a BMI > 30 is their actual weight minus the weight predicted for a BMI = 30 based on their height. 20% of the cohort accounted for 98% of excess weight in the cohort. These individuals constituted a high-cost group in the excess weight sector.
(Panel E) Hospital bed-nights
We obtained details of admission events to public hospitals from Ministry of Health records. The cohort accumulated 8,958 bed-nights in the hospital from January 1988 to March 2012. 20% of the cohort accounted for 77% of hospital bed-nights in the cohort. These individuals constituted a high-cost group in the hospital-stay sector.
(Panel F) Prescription drug-fills
We obtained information about prescription drugs filled by pharmacists, as indicated on the nation-wide Pharmaceutical Management Agency database. The cohort filled 66,811 prescriptions between January 2006 and March 2012. 20% of the cohort accounted for 89% of prescriptions. These individuals constituted a high-cost group in the prescription fill sector.
(Panel G) Injury insurance-claims
We obtained records of insurance claims for accidents and injuries from the Accident Compensation Corporation, the national provider of comprehensive, no-fault personal injury cover for New Zealanders. The cohort made 6,919 claims between January 1993 and March 2012. The concentration was not as pronounced for this outcome as for others, perhaps owing to the random nature of many accidents and injuries. Nevertheless, 20% of the cohort accounted for 52% of injury claims in the cohort. These individuals constituted a high-cost group in the injury claim sector.
(Panel H) Convictions for crime
We obtained information about criminal convictions by searching records available to the New Zealand Police. The cohort had 2,141 convictions for adult crimes (excluding routine traffic offenses), beginning at age 15. The concentration was more pronounced for this outcome than for others: 20% of the cohort accounted for 97% of convictions in the cohort. These individuals constituted a high-cost group in the crime sector.
Measuring childhood risk factors
We measured risk factors that are thought to augur poor adult outcomes. All risk factor measures have been described in previous reports about this cohort.
Childhood socioeconomic status 47
Childhood socioeconomic status was defined as the average of the highest occupational status level of either parent across study assessments from the Study member’s birth through 11 years (1=unskilled laborer; 6=professional), on New Zealand’s occupational rating of the 1970s.
Childhood maltreatment 48
Childhood maltreatment 48 includes evidence of (1) maternal rejection assessed at age 3 years by observational ratings of mothers’ interaction with the study children, (2) harsh discipline assessed at ages 7 and 9 years by parental report of disciplinary behaviours, (3) 2 or more changes in the child’s primary caregiver, and (4) physical abuse and (5) sexual abuse reported by study members once they reached adulthood. For each child, our cumulative index counts the number of maltreatment indicators during the first decade of life; 63.7% of children experienced no maltreatment, 26.7% experienced 1 indicator of maltreatment (hereinafter “probable” maltreatment), and 9.6% experienced 2 or more indicators of maltreatment (“definite” maltreatment).
Childhood intelligence (IQ) 13
Childhood intelligence (IQ) 13 was measured with the Wechsler Intelligence Scale for Children – Revised (WISC-R) administered at ages 7, 9, and 11 years. IQ scores for the three ages were averaged and standardized.
Childhood self-control 13
Childhood self-control 13 during the first decade of life was measured using nine measures of self-control: observational ratings of children’s lack of control (ages 3 and 5 years) and parent, teacher, and self-reports of hyperactivity, lack of persistence, inattention, impulsive aggression and impulsivity (ages 5, 7, 9, and 11 years). The nine measures were positively and significantly correlated. Based on principal components analysis, the standardized measures were averaged into a single composite comprising multiple ages and informants, with strong internal reliability α = 0.86.
Age-3 brain health
At age 3 years, each child in the cohort participated in a 45-minute examination that included assessments of neurological soft signs, intelligence, receptive language, and motor skills, and afterwards the examiners (having no prior knowledge of the child) rated each child’s behaviour. Using this information, we created a summary factor score via confirmatory factor analysis which we termed brain health, a global index of the child’s early neurocognitive status 31.
Statistical analysis
We began our work by examining the cumulative distributions of each of the eight outcomes (Figure 1). Using these distributions, we operationally defined a high-cost group in each sector as 20% of the cohort members who accounted for a disproportionate share of economically burdensome behaviour in that sector.
We tested associations between childhood risk factors and growing up to be a member of a high-cost group using modified Poisson regression models to estimate risk ratios (RR). We then added up (0–8) the number of high-cost groups to which each individual belonged and used Negative Binomial regressions to model incident rate ratios (IRR). We followed up this analysis to test associations between childhood risk factors and membership in the multiple-high-cost sector. We evaluated predictive accuracy using receiver operating characteristic (ROC) curve analysis to estimate each individual’s probability of belonging to a high-cost group in society based on their childhood risks.
Supplementary Material
Acknowledgments
We thank Dunedin Study members, their families, and Dunedin Study founder Phil Silva. This research received support from US National Institute on Aging (NIA) grants AG032282, AG048895, AG049789 and UK Medical Research Council (MRC) grant MR/K00381X and ESRC grant ES/M010309/1. The Dunedin Study was supported by the New Zealand Health Research Council and New Zealand Ministry of Business, Innovation and Employment (MBIE). Additional support was provided by the Jacobs Foundation and the Avielle Foundation. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. Our thanks to David Reiss, James Heckman and his seminar members, and the New Zealand agencies that offered guidance and assistance to the Dunedin Study. Special thanks to Zeeman van der Merwe (ACC), Chris Lewis (Ministry of Health), Moira Wilson and Rissa Ota (Ministry of Social Development), the Otago Police District Commander, Paul Stevenson, Joanne Curren and the Dunedin Police. The Otago University Ethics Committee, Duke University, and King’s College London provided ethical approval for the Dunedin Study. Participants gave written consent before data were collected. Dunedin Study data are available to researchers on application. A managed-access process ensures that approval is granted to research that comes under the terms of participant consent and privacy (see Supplemental Material for data-sharing details).
Footnotes
The authors declare no competing interests.
Author Contributions: A. Caspi, R. Poulton, and T.E. Moffitt designed the research; A. Caspi, R. Houts, and T.E. Moffitt wrote the manuscript; A. Caspi, S. Hogan, S. Ramrakha, R. Poulton, and T.E. Moffitt collected the data; A. Caspi, R. Houts, and HL. Harrington analyzed the data. All the authors reviewed drafts, provided critical feedback, and approved the final manuscript.
References
- 1.Almond D, Currie J. Human capital development before age five. 2010 < http://www.nber.org/papers/w15827>.
- 2.Duncan GJ, Magnuson K. Investing in preschool programs. Journal of Economic Perspectives. 2013;27:109–131. doi: 10.1257/jep.27.2.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Campbell F, et al. Early childhood investments substantially boost adult health. Science. 2014;343:1478–1485. doi: 10.1126/science.1248429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gertler P, et al. Labor market returns to an early childhood stimulation intervention in Jamaica. Science. 2014;344:998–1001. doi: 10.1126/science.1251178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Heckman J, Pinto R, Savelyev P. Understanding the mechanisms through which an influential early childhood program boosted adult outcomes. American Economic Review. 2013;103:2052–2086. doi: 10.1257/aer.103.6.2052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reynolds AJ, Temple JA, Ou SR, Arteaga IA, White BAB. School-based early childhood education and age-28 well-being: Effects by timing, dosage, and subgroups. Science. 2011;333:360–364. doi: 10.1126/science.1203618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rand Corporation. Proven benefits of early childhood interventions. 2005 < http://www.rand.org/pubs/research_briefs/RB9145.html>.
- 8.Nuffield Foundation. Early years education and childcare. 2015 < www.nuffieldfoundation.org>.
- 9.Blueprints. Blueprints for healthy youth development. 2016 < http://www.blueprintsprograms.com/>.
- 10.Institute of Education Sciences. Institute of Education Sciences. 2016 < http://ies.ed.gov/ncee/wwc/>.
- 11.The Incredible Years. The Incredible Years. 2016 < http://incredibleyears.com/>.
- 12.Heckman JJ. Skill formation and the economics of investing in disadvantaged children. Science. 2006;312:1900–1902. doi: 10.1126/science.1128898. [DOI] [PubMed] [Google Scholar]
- 13.Moffitt TE, et al. A gradient of childhood self-control predicts health, wealth, and public safety. Proceedings of the National Academy of Sciences of the United States of America. 2011;108:2693–2698. doi: 10.1073/pnas.1010076108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Roberts BW, Kuncel NR, Shiner R, Caspi A, Goldberg LR. The power of personality: The comparative validity of personality traits, socioeconomic status, and cognitive ability for predicting important life outcomes. Perspectives on Psychological Science. 2007;2:313–345. doi: 10.1111/j.1745-6916.2007.00047.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Felitti VJ, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults The Adverse Childhood Experiences (ACE) Study. Am.J.Prev.Med. 1998;14:245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 16.Rutter M. Nature, nurture, and development: From evangelism through science toward policy and practice. Child Development. 2002;73:1–21. doi: 10.1111/1467-8624.00388. [DOI] [PubMed] [Google Scholar]
- 17.Sampson R. The characterological imperative. Journal of Economic Literature. 2016 in press. [Google Scholar]
- 18.Steuerle E, Jackson LM. Advancing the Power of Economic Evidence to Inform Investments in Children, Youth, and Families. National Academies Press; 2016. [PubMed] [Google Scholar]
- 19.Shonkoff JP, Boyce WT, McEwen BS. Neuroscience, molecular biology, and the childhood roots of health disparities: Building a new framework for health promotion and disease prevention. Journal of the American Medical Association. 2009;301:2252–2259. doi: 10.1001/jama.2009.754. [DOI] [PubMed] [Google Scholar]
- 20.Diamond A. Activities and programs that improve children’s executive functions. Current Directions in Psychological Science. 2012;21:335–341. doi: 10.1177/0963721412453722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Black MM, Dewey KG. Promoting equity through integrated early child development and nutrition interventions. Ann N Y Acad Sci. 2014;1308:1–10. doi: 10.1111/nyas.12351. [DOI] [PubMed] [Google Scholar]
- 22.U.S. Department of Health & Human Services. Surgeon General.gov. 2011 < http://www.surgeongeneral.gov/priorities/prevention/strategy>.
- 23.Power C, Kuh D, Morton S. From developmental origins of adult disease to life course research on adult disease and aging: insights from birth cohort studies. Annu Rev Public Health. 2013;34:7–28. doi: 10.1146/annurev-publhealth-031912-114423. [DOI] [PubMed] [Google Scholar]
- 24.The New York Times. Jospeh Juran, 103, Pioneer in quality control dies. 2008 < http://www.nytimes.com/2008/03/03/business/03juran.html?_r=0>.
- 25.CRN Magazine. Microsoft’s CEO: 80-20 Rule applies to bugs, not just features. 2002 < http://www.crn.com/news/security/18821726/microsofts-ceo-80-20-rule-applies-to-bugs-not-just-features.htm>.
- 26.Heckman J, Moon SH, Pinto R, Savelyev P, Yavitz A. Analyzing social experiments as implemented: A reexamination of the evidence from the HighScope Perry Preschool Program. Quant Econom. 2010;1:1–46. doi: 10.3982/qe8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pepe MS, Janes H, Longton G, Leisenring W, Newcomb P. Limitations of the odds ratio in gauging the performance of a diagnostic, prognostic, or screening marker. Am J Epidemiol. 2004;159:882–890. doi: 10.1093/aje/kwh101. [DOI] [PubMed] [Google Scholar]
- 28.Kraemer HC, et al. Coming to terms with the terms of risk. Arch Gen Psychiatry. 1997;54:337–343. doi: 10.1001/archpsyc.1997.01830160065009. [DOI] [PubMed] [Google Scholar]
- 29.Rice ME, Harris GT. Comparing effect sizes in follow-up studies: ROC Area, Cohen’s d, and r. Law Hum Behav. 2005;29:615–620. doi: 10.1007/s10979-005-6832-7. [DOI] [PubMed] [Google Scholar]
- 30.Hosmer D, Lemeshow S. Applied logistic regression. Wiley; 2005. [Google Scholar]
- 31.Caspi A et al. The p Factor: One general psychopathology factor in the structure of psychiatric disorders? Clin Psychol Sci. 2014;2:119–137. doi: 10.1177/2167702613497473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Heckman JJ, Moon SH, Pinto R, Savelyev PA, Yavitz A. The rate of return to the High/Scope Perry Preschool Program. J Public Econ. 2010;94:114–128. doi: 10.1016/j.jpubeco.2009.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wikipedia. List of countries by income equality. 2016 < http://en.wikipedia.org/wiki/List_of_countries_by_income_equality>.
- 34.The World Bank. Health expenditure, total (% of GDP) 2016 < http://data.worldbank.org/indicator/SH.XPD.TOTL.ZS/>.
- 35.Education.Gov.UK. Every Child Matterso. 2003 < https://www.education.gov.uk/consultations/downloadableDocs/EveryChildMatters.pdf>.
- 36.Thomas DC. Invited commentary: Is it time to retire the “pack-years” variable? Maybe not! Am J Epidemiol. 2014;179:299–302. doi: 10.1093/aje/kwt274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rushton JP, Brainerd CJ, Pressley M. Behavioral development and construct validity: The principle of aggregation. Psychological Bulletin. 1983;94:18–38. [Google Scholar]
- 38.Evans GW, Li D, Whipple SS. Cumulative risk and child development. Psychol Bull. 2013;139:1342–1396. doi: 10.1037/a0031808. [DOI] [PubMed] [Google Scholar]
- 39.Centers for Disease Control and Prevention. Injury prevention & control: Division of violence prevention. 2016 < http://www.cdc.gov/violenceprevention/acestudy>.
- 40.Kulminski AM, et al. Do gender, disability, and morbidity affect aging rate in the LLFS? Application of indices of cumulative deficits. Mech Ageing Dev. 2011;132:195–201. doi: 10.1016/j.mad.2011.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gormley WT., Jr From science to policy in early childhood education. Science. 2011;333:978–981. doi: 10.1126/science.1206150. [DOI] [PubMed] [Google Scholar]
- 42.Heckman JJ. The economics, technology, and neuroscience of human capability formation. Proc Natl Acad Sci U S A. 2007;104:13250–13255. doi: 10.1073/pnas.0701362104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gabrieli C, Ansel D, Krachman SB. Ready to be counted: The research case for education policy action on non-cognitive skills. 2015 < http://www.transformingeducation.org/resources/>.
- 44.Hoedemaekers R, Dekkers W. Justice and solidarity in priority setting in health care. Health Care Anal. 2003;11:325–343. doi: 10.1023/B:HCAN.0000010061.71961.87. [DOI] [PubMed] [Google Scholar]
- 45.Copenhagen Consensus Center. Population Assessment. 2015 < http://www.copenhagenconsensus.com/sites/default/files/population_assessment_-_kohler_behrman_0.pdf>.
- 46.Poulton R, Moffitt TE, Silva PA. The Dunedin Multidisciplinary Health and Development Study: Overview of the first 40 years, with an eye to the future. Soc Psychiatry Psychiatr Epidemiol. 2015;50:679–693. doi: 10.1007/s00127-015-1048-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Poulton R, et al. Association between children’s experience of socioeconomic disadvantage and adult health: A life-course study. Lancet. 2002;360:1640–1645. doi: 10.1016/S0140-6736(02)11602-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Caspi A, et al. Role of genotype in the cycle of violence in maltreated children. Science. 2002;297:851–854. doi: 10.1126/science.1072290. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.