Abstract
Background
Early mobilization protocols have been successfully implemented to improve function in critically ill patients; however, no study has focused on the oncology population.
Objectives
To investigate the feasibility of early mobilization and describe the rehabilitation interventions and discharge outcomes in a cohort of critically ill patients with cancer.
Design
Retrospective review.
Methods
A retrospective analysis of patients with cancer who participated in occupational and physical therapy while on mechanical ventilation utilizing an institutional early mobilization protocol from June 2010 – July 2011, was completed. Demographic and clinical variables were abstracted, as well as occupational and physical therapy interventions.
Results
A cohort of 42 cancer patients on mechanical ventilation in the mixed medical/surgical intensive care unit of a comprehensive cancer center received early mobilization during the study period. The majority of participants demonstrated improved cognitive and functional status from the intensive care unit to hospital discharge. There were no reported adverse events during the occupational and physical therapy sessions. Among the 30 hospital survivors, 53% required continued rehabilitation services in their home environment and 40% were transferred to a rehabilitation facility.
Limitations
Due to the small sample size, these findings are not generalizable to all critically ill cancer patients. There was no post-acute care follow-up of cognitive and physical functional performance.
Conclusion
Early mobilization appears feasible in addressing the cognitive and functional needs of oncology patients in the intensive care unit.
Keywords: cancer, early mobility, ICU, mechanical ventilation, cognition
Introduction
Patients who require mechanical ventilation (MV) for acute respiratory failure in the intensive care unit (ICU) are at increased risk for developing neuromuscular, cognitive and psychosocial complications, which can result in decreased quality of life and altered occupational performance.1–3 Acute respiratory distress syndrome (ARDS) is a life-threatening respiratory condition due to severe inflammation of the lungs. ARDS is caused by direct and/or indirect injury to the lung parenchyma from pneumonia, sepsis, trauma, medications, etc. and is associated with hypoxia and opacities on chest radiographs.4 ARDS can lead to acute hypoxic respiratory failure requiring mechanical ventilation in the ICU.5 Patients with a cancer diagnosis who develop (ARDS) have a significantly higher risk of mortality when compared to patients without cancer, perhaps because of additional medical complications such as neutropenia, severe sepsis, pneumonia, and medication or radiation-induced pneumonitis.6–8 Additionally, pre-ICU length of stay (LOS) has been associated with sepsis-related ARDS9, prolonged ICU LOS, and hospital mortality.10,11
Over the past two decades, improvement in the management of ARDS, severe sepsis and cancer has resulted in a higher number of patients surviving to hospital discharge.12–14 Survivors of critical illness report decreased quality of life, impaired ability to function autonomously and difficulty with return to work because of lingering cognitive and physical impairments.15,16 Functional outcomes and quality of life in critically ill patients with cancer are significantly altered following an ICU admission.17 Furthermore, patients with cancer have the potential to develop multiple side effects and treatment complications throughout the cancer care continuum, requiring supportive care to maximize or maintain function.18,19
Early mobilization has been described in the literature as the initiation of cognitive and physical activities performed by occupational therapy (OT) and physical therapy (PT) for patients on MV within 48–72 hours of intubation, and has gained acceptance among healthcare providers because of its feasibility, cost-effectiveness, improved functional outcomes, and reduction in the incidence of delirium.20–22 There are currently no published data on the functional outcomes of patients with cancer who develop critical illness and receive early mobilization in the ICU. However, rehabilitation has been shown to be beneficial for patients with cancer across the continuum of care to provide restorative and supportive interventions.18 The primary aim of this study is to investigate the feasibility of early mobilization and describe the rehabilitation interventions and functional discharge outcomes in critically ill patients with cancer.
Methods
Research Design
The study was performed in a 20-bed medical/surgical ICU at a tertiary care cancer center in the United States. Data were abstracted through a retrospective review of a cohort of 42 patients’ charts who met the study criteria. The institutional review board granted a waiver of authorization for the study.
Early Mobilization Program Design
A multidisciplinary team of occupational therapists, physical therapists, respiratory therapists, nurses, and physicians collaboratively developed the early mobilization program utilized at the institution based on published protocols and clinical experience treating critically ill cancer patients. The institutional early mobilization program occurred for patients within 72 hours of initiation of MV in the ICU with an evaluation performed by occupational and physical therapists with support from respiratory therapy and nursing staff.
Program Participants
Patients who required MV for acute respiratory failure and participated in an early mobilization program during admission to the ICU from June 1, 2010 – July 31, 2011 were identified through hospital database queries. The clinical team of rehabilitation therapists, nurses, respiratory therapists, and physicians met daily and determined the appropriateness for participation based on a specific set of criteria. All patients who participated in early mobilization were considered possible candidates if the Richmond Agitation Sedation Scale (RASS) score was between minus two and plus one.23 Exclusion criteria were based on previous studies to minimize the risk of fatal complications.20 Patients considered for termination of life-sustaining treatment, with a do-not-resuscitate order (DNR), or tracheostomies were excluded. Patients already participating in EM who had a change in code status to DNR were not placed on hold; the same quality of OT and PT interventions continued. Additional exclusion criteria included: mean arterial pressure of < 66 or > 100 mmHg; systolic blood pressure of > 200 mmHg; pulse rate of < 40 or > 130 beats per minute, saturation by pulse oximetry of < 88%, active gastrointestinal hemorrhage, RASS score of minus three to five or plus two to four within 30 minutes before planned early mobilization sessions, difficult endotracheal intubation due to airway restrictions, intracranial hypertension, active myocardial ischemia, open surgical abdominal wound.
Upon determination of patient’s suitability for participation in early mobilization, extensive coordination of care was required between OT, PT, respiratory therapy, and nursing in order to schedule the session and to overcome barriers posed by conflicting tests, procedures, sedation, patient’s change in medical status, and therapists’ schedules. There were no instances when a medical provider declined EM services if a patient met participation criteria. There was no difference in the OT and PT care provided to patients pre- and post-extubation with consistent therapy received throughout the continuum of care.
Early Mobilization Activities
Physical activities
Physical and occupational therapists assessed the patient’s strength, balance, coordination, and sensation for safe progression of mobility. The sequence of mobility began with bed-level activities with active patient participation (ie, rolling, upper and lower extremity exercises, breathing exercises, or self-care activities), followed by seated edge of bed activities, transferring from the bed to a chair, and ambulation as tolerated and appropriate.24
The OT facilitated participation in self care tasks including grooming, bathing and dressing in varied positions (ie, bed-level, seated edge of bed, supported sitting in chair), and intensity based on each patient’s tolerance. Continuous monitoring of vital signs (oxygen saturation, heart rate, blood pressure, and respiratory rate) occurred during each session to assess the patient’s level of tolerance and ability to progress functional participation. OT and PT staff provided recommendations regarding patients’ physical tolerance for nursing staff to implement in bed and out of bed activities as appropriate. The majority of physical activities occurred during OT and PT sessions with the assistance of respiratory therapists.
Cognitive activities
The occupational therapists assessed patient orientation, communication, and ability to follow-directions through participation in functional and therapeutic activities.18 The Hospital Elder Life Program (HELP) strategies and sensory stimulation were incorporated.25–27 Occupational therapists utilized recommended interventions for the prevention and management of delirium according to HELP such as (a) a reality orientation program (orientation board, providing a daily schedule, reorienting communication); (b) a therapeutic activities program (ie, activities focused on cognitive stimulation including the use of word search games and reading/summarizing current events); (c) a routine schedule for completion of self-care tasks such as oral care, grooming, bathing, and dressing; (d) early mobilization; and (e) adaptive equipment/compensatory strategies for individuals with hearing and vision impairments including tablet use, educational material with large print, and simplified communication boards with images instead of written words.27
Data Collection
The investigators collected patient demographics (age and gender), reasons for ICU admission, primary cancer diagnosis, change in code status during ICU stay and ICU and hospital LOS and mortality, as well as mortality probability model (MPM) II score on ICU admission (Table 1). MPM II score is a validated predictive model to determine severity of illness and probability of mortality in ICU patients.28,29 The rehabilitation team could not use the Functional Independence Measure (FIM), a validated 18-item scale for assessing motor and cognitive status and measuring rehabilitation outcomes, because of the retrospective study methodology.30 Hence, through a review of the medical records, the OT and PT team identified the five most commonly used items adapted from the FIM and translated the documented milestones of physical function in critically ill patients on MV e.g. grooming, lower body dressing, supine to sit, sit to stand and level of assistance required for ambulation into an adapted composite score. The scoring system utilized for the study models the FIM seven-point ordinal scale with a score of seven indicating functional independence in a specific task. The highest achievable functional composite score was 35 (Table 2). Three components of cognitive status were collected independently from the FIM including orientation, direction-following, and communication with an ordinal scoring system from zero-three. The highest summative cognitive composite score was nine (Table 2).
Table 1.
Patient demographic and clinical characteristics
| Variables | Median (25th, 75th percentile) |
|---|---|
| Age | 60 (50, 73) |
| MPM II Score | 0.3 (0.1, 0.5) |
| ICU LOS | 20 (13, 28) |
| Hospital LOS | 50 (29, 72) |
| Variables | n (%) |
| Gender [Males = n; (%)] | 22 (52%) |
| Reasons for ICU admission | |
| Abdominal Catastrophe | 2 (5%) |
| Airway Management | 2 (5%) |
| Altered mental status | 2 (5%) |
| Bleeding | 1 (2%) |
| Cardiac | 2 (5%) |
| Hypotension | 1 (2%) |
| Renal failure | 1 (2%) |
| Respiratory failure | 27 (64%) |
| Sepsis | 4 (10%) |
| Medical Oncology Service | 25 (60%) |
| Cancer Diagnosis | |
| Breast | 1 (2%) |
| Gastrointestinal | 5 (12%) |
| Genitourinary | 4 (10%) |
| Head and Neck | 4 (10%) |
| Hematological | 13 (31%) |
| Thoracic | 15 (35%) |
| Change to DNR during ICU Stay | 10 (24%) |
| Vasopressor Use in ICU | 30 (71%) |
| ICU Mortality | 5 (12%) |
| Hospital Mortality | 12 (29%) |
Table 2.
Cognitive and Functional Status Scoring System
| COGNITIVE TASK | SCORE RANGE |
SCORE KEY (A & O x 3 = alert and oriented) |
|---|---|---|
| Orientation | 0–3 | 0= not oriented, 1=A&Ox1, 2=A&Ox2, 3= A&Ox3 |
| Direction Following | 0–3 | 0= not following, 1=inconsistently following, 2=following 1-step commands, 3=following >or= 2-step commands |
| Communication | 0–3 | 0=unable to communicate, 1=nonverbal/gestures, 2= written communication, 3=verbal communication |
| Sum of all 3 tasks | 0–9 | |
| FUNCTIONAL TASK |
SCORE RANGE |
SCORE KEY |
| Grooming | 0–7 | 0 = patient unable to perform, 1 = total assistance, 2 = maximal assistance, 3 = moderate assistance, 4 = minimal contact assistance, 5 = supervision, 6 = modified independent, 7 = independent |
| Lower body dressing | 0–7 | |
| Supine to sit | 0–7 | |
| Sit to stand | 0–7 | |
| Ambulation assistance | 0–7 | |
| Sum of all 5 tasks | 0–35 |
Cognitive and functional data were analyzed at three different time points by the research team: at initial early mobilization OT and PT evaluation in the ICU, at ICU discharge, and at hospital discharge (Tables 3 & 4). The number of OT and PT sessions completed throughout the hospital stay for each patient was collected. All charts were reviewed for any adverse events that occurred during the OT and PT sessions including falls, unplanned extubation, and line removal. Finally, discharge disposition was determined through review of discharge summary documentation and case management notes.
Table 3.
Analysis of Change in Functional Status Composite Score
| Functional Status Composite Score | n (deceased) | Median (25th, 75th percentile) |
Wilcoxon Signed rank test p-value |
|---|---|---|---|
| Baseline ICU | 42 | 4.0 (2.0, 8.0) | |
| ICU discharge/last visit | 42 (51) | 7.0 (4.0, 15.0) | <0.00013 |
| Hospital discharge/last visit | 37 (72) | 22.0 (13.0, 28.0) | <0.00014 |
5 patients deceased during ICU stay, ICU last visit score was used.
7 patients deceased during hospital stay, last hospital visit score was used.
ICU discharge/last visit vs. baseline ICU.
Hospital discharge/last visit vs. ICU discharge/last visit.
Table 4.
Analysis of Change in Cognitive Status Composite Score
| Cognitive Status Composite Score | n (deceased) | Median (25th, 75th percentile) |
Wilcoxon Signed rank test p-value |
|---|---|---|---|
| Baseline ICU | 42 | 6.0 (3.0, 8.0) | |
| ICU discharge/last visit | 42 (51) | 7.0 (6.0, 9.0) | <0.00013 |
| Hospital discharge/last visit | 37 (72) | 9.0 (7.0, 9.0) | 0.0474 |
5 patients deceased during ICU stay, ICU last visit score was used.
7 patients deceased during hospital stay, last hospital visit score was used.
ICU discharge/last visit vs. baseline ICU.
Hospital discharge/last visit vs. ICU discharge/last visit.
Data Analysis
All investigators contributed to the data analysis that was led by the statistician. Data are presented as median (25th, 75th percentile) for continuous variables, and absolute numbers (n=) and percentages (%) for categorical variables. Wilcoxon signed rank sum test was used to assess changes in functional and cognitive composite scores over time. A p-value <0.05 was considered statistically significant. Statistical analysis was conducted with the software SAS version 9.4 (SAS Institute Inc. Cary, NC).
Results
During the study period, 446 patients required MV during admission to the medical/surgical oncology ICU. Of these patients, 42 (9%) met inclusion criteria for the study. While 14 patients were intubated on ICU admission, 28 required intubation after ICU admission. A total of 30 (71%) patients required vasopressors and 10 (24%) patients’ code status was changed to DNR during ICU stay. The majority of the patients were from the thoracic (n= 15, 35%) and hematological services (n = 13, 31%). Other patients were from the gastrointestinal (n= five, 12%), head and neck (n= four, 10%), urology (n= four, 10%), and breast (n=one, 2%) services. Acute respiratory failure was the primary ICU diagnosis in 27 (64%) patients (Table 1).
The median age was 60 years, 52% were male, median MPM II score was 30%, and 60% were medical oncology patients. Overall, median ICU LOS was 20 days (IQR range 13, 28) and hospital median LOS was 50 days [(29, 72); (Table 1)]. The total hospital mortality was 29% (n = 12). Of the 30 survivors, 40% (n = 12) were discharged to a rehabilitation facility and 53% (n = 16) were discharged home with or without OT and PT services, while 7% (n = 2) received home hospice. For more details see (Figure 1).
Figure 1.
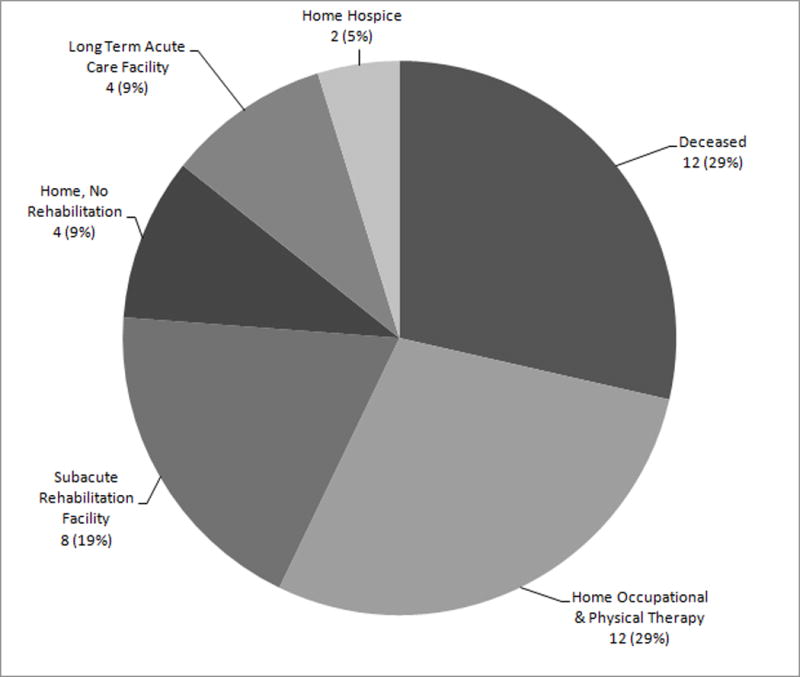
Early mobilization participants discharge placement.
In this cohort, Wilcoxon signed rank test showed that functional status composite score significantly increased over time [(ICU discharge/last visit vs. baseline ICU, T statistic= 278.5 p<0.0001; hospital discharge/last visit vs. ICU discharge/last visit, T statistic= 259, p<0.0001); (Table 3)]. Wilcoxon signed rank test also showed that cognitive status composite score significantly increased over time [(ICU discharge/last visit vs. baseline ICU, T statistic=266.5, p<0.0001; hospital discharge/last visit vs. ICU discharge/last visit, T statistic= 47.5, p= 0.047); (Table 4)].
There were no documented adverse events (falls, unplanned extubation, or line removal) during EM sessions as determined through review of the OT and PT treatment notes and through the hospital event reporting system. The investigators did not collect data on the number of patient refusals or number of times the patient was unavailable due to tests/procedures for OT and PT follow up sessions; however, instances of patient refusal were anecdotally infrequent as a result of pre-scheduling session time.
Patients received an average of one OT and two PT sessions consisting of cognitive and physical activities prior to ICU admission and 15 OT sessions and 17 PT from ICU to hospital discharge, including five OT and five PT sessions in the ICU.
Discussion
The objective of this study was to explore the feasibility of early mobilization and describe the rehabilitation interventions and functional discharge outcomes in cancer patients with a critically illness. Neutropenia, sepsis, pneumonia, and medication- or radiation-induced pneumonitis, and high MPM II score predispose patients with cancer who develop (ARDS) to a higher risk of mortality when compared to patients without cancer.6,7 Although early mobilization has been associated with a multitude of benefits including prevention of debility, pressure ulcers, pneumonia and other medical sequelae, such data are scarce in the critically ill cancer population.20
Early mobilization was determined to be feasible with a cohort of cancer patients. Of the 42 patient charts reviewed, there were no documented adverse events, including falls, unplanned extubation or line removal during the OT and PT sessions throughout the hospital stay. This pilot initiative warrants further exploration, and presents the possibility that an early mobilization program can be implemented with critically ill cancer patients in other institutions, despite severity of illness and multiple co-morbidities.
Irrespective of pre-ICU LOS, rehabilitation interventions appeared to demonstrate improvement in the cognitive and physical status of patients with cancer who required MV. For a majority of participants in the study, an increase in functional and cognitive scores was observed regardless of baseline status at the time of early mobilization initial assessment (Table 3 & 4). Overall, mean cognitive composite score at ICU discharge and hospital discharge was significantly increased compared to the baseline score, highlighting that participation in early mobilization may be applicable for patients with physical and cognitive impairments. Evidence shows there are multiple contributing factors that can improve a patient’s cognitive and physical outcomes, including decreased use of medications/sedatives, more comprehensive nursing care, and increased utilization of OT and PT with patients who have acute lung injury.31
Integrating a multidisciplinary approach to address cognitive and functional status throughout an episode of care is the key for a successful early rehabilitation program.32 An increased number of OT and PT encounters beginning within the ICU has shown to reduce overall hospital length of stay.31 The average number of OT sessions (15) and PT sessions (17) study participants received from ICU admission to hospital discharge may have contributed to length of stay and facilitation of optimal hospital discharge placement.
In this cohort, 12 (29%) patients died prior to hospital discharge and two (5%) patients were discharged to home hospice. These findings suggest that the culture and attitude of multidisciplinary rehabilitation care delivery for critically ill cancer patients is shifting to address functional performance outcomes and quality of life regardless of prognosis. Also, these results seem to indicate a patient centered approach to address the physical, cognitive and emotional consequences throughout the cancer care continuum.18 Early mobilization supportive care services can enable a patient to improve remaining quality of life, preserve human dignity, maintain meaningful roles and routines, decrease pain, decrease immobility associated pressure ulcers, and facilitate meaningful interaction with family and friends.33–35
A growing number of cancer patients survive critical illnesses and are discharged home.17 Yet, published data on the discharge needs and outcomes of patients with cancer surviving critical illness are limited. Approximately 12 (29%) patients were discharged with home-based OT and PT services. The acute care OT and PT services were instrumental in communicating discharge recommendations to the medical team based on patients’ progress and anticipated rehabilitation needs after hospital discharge. Regardless of medical prognosis, the rehabilitation team recommended to the multidisciplinary team ongoing patient/caregiver education, adaptive equipment, cognitive and functional activities, and home-based OT and PT services when appropriate.
Limitations and Future Research
This was a carefully selected convenience sample of patients with specific exclusion criteria. There were multiple factors that influenced the small sample size, including candidate screening process and sedation management in the ICU. The institutional practice has now changed to incorporate daily multidisciplinary rounds to allow thorough screening of patients on mechanical ventilation and to more effectively identify potential candidates for early mobilization who may have been previously excluded.
Due to the small sample size, this analysis is not generalizable to all critically ill cancer patients on MV. Future research is needed to determine the application of early mobilization in a larger population of critically ill patients with cancer. The investigators did not assess pre-hospital cognitive and physical deficits or the impact of cancer or cancer-directed therapies on patients’ functional status prior to ICU admission. Lastly, there was no long-term follow-up of cognitive or functional status after hospital discharge to assess post-discharge outcomes. Further research is needed to determine the effectiveness of specific rehabilitation interventions addressing cognitive and physical performance of patients with cancer who have critical illness, as well as the impact of these interventions on quality of life.
Conclusion
This study indicates that cognitive and physical interventions are potentially feasible with patients with cancer who require mechanical ventilation in the ICU. Critically ill patients with cancer may develop rehabilitation needs at all stages of the treatment continuum, therefore OT and PT can be integrated into the multidisciplinary care team to address both the cognitive and physical impairments limiting functional performance. Follow up post-discharge determination of cognitive and functional needs may trigger additional supportive resources needed in the critically ill cancer population to truly optimize quality of life.
Acknowledgments
Weiji Shi is partly supported by an NIH Core Grant P30 CA008748
Contributor Information
Amanda Weeks, Memorial Sloan Kettering Cancer Center.
Claudine Campbell, Memorial Sloan Kettering Cancer Center.
Prabalini Rajendram, Cleveland Clinic.
Weiji Shi, Memorial Sloan Kettering Cancer Center.
Louis Voigt, Memorial Sloan Kettering Cancer Center.
References
- 1.Girard TD, Jackson JC, Pandharipande PP, et al. Delirium as a predictor of long-term cognitive impairment in survivors of critical illness. Crit Care Med. 2010;38(7):1513–1520. doi: 10.1097/CCM.0b013e3181e47be1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hermans G, Van Mechelen H, Clerckx B, et al. Acute outcomes and 1-year mortality of intensive care unit-acquired weakness: A cohort study and propensity-matched analysis. Am J Respir Crit Care Med. 2014;190(4):410–420. doi: 10.1164/rccm.201312-2257OC. [DOI] [PubMed] [Google Scholar]
- 3.Pandharipande PP, Girard TD, Jackson JC, et al. Long-term cognitive impairment after critical illness. N Engl J Med. 2013;369(14):1306–1316. doi: 10.1056/NEJMoa1301372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Force ADT, Ranieri VM, Rubenfeld GD, et al. Acute respiratory distress syndrome: the Berlin Definition. JAMA. 2012;307(23):2526–2533. doi: 10.1001/jama.2012.5669. [DOI] [PubMed] [Google Scholar]
- 5.Sweeney RM, McAuley DF. Acute respiratory distress syndrome. Lancet. 388(10058):2416–2430. doi: 10.1016/S0140-6736(16)00578-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Soubani A, Shehada E, Chen W, Smith D. The outcome of cancer patients with acute respiratory distress syndrome. J Crit Care. 2014;29(1):183 e187–183 e112. doi: 10.1016/j.jcrc.2013.10.011. [DOI] [PubMed] [Google Scholar]
- 7.Azoulay E, Lemiale V, Mokart D, et al. Acute respiratory distress syndrome in patients with malignancies. Intensive Care Med. 2014;40(8):1106–1114. doi: 10.1007/s00134-014-3354-0. [DOI] [PubMed] [Google Scholar]
- 8.Taccone FS, Artigas AA, Sprung CL, Moreno R, Sakr Y, Vincent JL. Characteristics and outcomes of cancer patients in European ICUs. Crit Care. 2009;13(1):R15. doi: 10.1186/cc7713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sheu CC, Gong MN, Zhai R, et al. Clinical characteristics and outcomes of sepsis-related vs non-sepsis-related ARDS. Chest. 2010;138(3):559–567. doi: 10.1378/chest.09-2933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Higgins TL, McGee WT, Steingrub JS, Rapoport J, Lemeshow S, Teres D. Early indicators of prolonged intensive care unit stay: impact of illness severity, physician staffing, and pre-intensive care unit length of stay. Crit Care Med. 2003;31(1):45–51. doi: 10.1097/00003246-200301000-00007. [DOI] [PubMed] [Google Scholar]
- 11.Goldhill DR, McNarry AF, Hadjianastassiou VG, Tekkis PP. The longer patients are in hospital before intensive care admission the higher their mortality. Intensive Care Med. 2004;30(10):1908–1913. doi: 10.1007/s00134-004-2386-2. [DOI] [PubMed] [Google Scholar]
- 12.Esteban A, Frutos-Vivar F, Muriel A, et al. Evolution of mortality over time in patients receiving mechanical ventilation. Am J Respir Crit Care Med. 2013;188(2):220–230. doi: 10.1164/rccm.201212-2169OC. [DOI] [PubMed] [Google Scholar]
- 13.Kumar G, Kumar N, Taneja A, et al. Nationwide trends of severe sepsis in the 21st century (2000–2007) Chest. 2011;140(5):1223–1231. doi: 10.1378/chest.11-0352. [DOI] [PubMed] [Google Scholar]
- 14.Aygencel G, Turkoglu M, Turkoz Sucak G, Benekli M. Prognostic factors in critically ill cancer patients admitted to the intensive care unit. J Crit Care. 2014;29(4):618–626. doi: 10.1016/j.jcrc.2014.01.014. [DOI] [PubMed] [Google Scholar]
- 15.Herridge MS, Tansey CM, Matte A, et al. Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med. 2011;364(14):1293–1304. doi: 10.1056/NEJMoa1011802. [DOI] [PubMed] [Google Scholar]
- 16.Iwashyna TJ, Ely EW, Smith DM, Langa KM. Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA. 2010;304(16):1787–1794. doi: 10.1001/jama.2010.1553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Soares M, Caruso P, Silva E, et al. Characteristics and outcomes of patients with cancer requiring admission to intensive care units: a prospective multicenter study. Crit Care Med. 2010;38(1):9–15. doi: 10.1097/CCM.0b013e3181c0349e. [DOI] [PubMed] [Google Scholar]
- 18.Sleight AG, Duker LI. Toward a Broader Role for Occupational Therapy in Supportive Oncology Care. Am J Occup Ther. 2016;70(4):7004360030p7004360031–7004360038p7004360031. doi: 10.5014/ajot.2016.018101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Harrison JD, Young JM, Price MA, Butow PN, Solomon MJ. What are the unmet supportive care needs of people with cancer? A systematic review. Support Care Cancer. 2009;17(8):1117–1128. doi: 10.1007/s00520-009-0615-5. [DOI] [PubMed] [Google Scholar]
- 20.Schweickert WD, Pohlman MC, Pohlman AS, et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: A randomised controlled trial. Lancet. 2009;373(9678):1874–1882. doi: 10.1016/S0140-6736(09)60658-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li Z, Peng X, Zhu B, Zhang Y, Xi X. Active mobilization for mechanically ventilated patients: A systematic review. Arch Phys Med Rehabil. 2013;94(3):551–561. doi: 10.1016/j.apmr.2012.10.023. [DOI] [PubMed] [Google Scholar]
- 22.Adler J, Malone D. Early mobilization in the intensive care unit: A systematic review. Cardiopulm Phys Ther J. 2012;23(1):5–13. [PMC free article] [PubMed] [Google Scholar]
- 23.Sessler CN, Gosnell MS, Grap MJ, et al. The Richmond Agitation-Sedation Scale: Validity and reliability in adult intensive care unit patients. Am J Respir Crit Care Med. 2002;166(10):1338–1344. doi: 10.1164/rccm.2107138. [DOI] [PubMed] [Google Scholar]
- 24.Perme C, Chandrashekar R. Early mobility and walking program for patients in intensive care units: creating a standard of care. Am J Crit Care. 2009;18(3):212–221. doi: 10.4037/ajcc2009598. [DOI] [PubMed] [Google Scholar]
- 25.Howell D. Neuro-occupation: Linking sensory deprivation and self-care in the ICU patient. Occupational therapy in health care. 1999;11(4):75–85. doi: 10.1080/J003v11n04_07. [DOI] [PubMed] [Google Scholar]
- 26.Campbell C. The role of occupational therapy in an early mobility program in the intensive care unit. Physical Disabilities Special Interest Section Quarterly. 2014;37(1):4. [Google Scholar]
- 27.Inouye SK. Prevention of delirium in hospitalized older patients: risk factors and targeted intervention strategies. Ann Med. 2000;32(4):257–263. doi: 10.3109/07853890009011770. [DOI] [PubMed] [Google Scholar]
- 28.Lemeshow S, Teres D, Klar J, Avrunin JS, Gehlbach SH, Rapoport J. Mortality Probability Models (MPM II) based on an international cohort of intensive care unit patients. JAMA. 1993;270(20):2478–2486. [PubMed] [Google Scholar]
- 29.Groeger JS, Lemeshow S, Price K, et al. Multicenter outcome study of cancer patients admitted to the intensive care unit: A probability of mortality model. J Clin Oncol. 1998;16(2):761–770. doi: 10.1200/JCO.1998.16.2.761. [DOI] [PubMed] [Google Scholar]
- 30.Granger CV, Hamilton BB, Linacre JM, Heinemann AW, Wright BD. Performance profiles of the functional independence measure. Am J Phys Med Rehabil. 1993;72(2):84–89. doi: 10.1097/00002060-199304000-00005. [DOI] [PubMed] [Google Scholar]
- 31.Needham DM, Korupolu R, Zanni JM, et al. Early physical medicine and rehabilitation for patients with acute respiratory failure: a quality improvement project. Arch Phys Med Rehabil. 2010;91(4):536–542. doi: 10.1016/j.apmr.2010.01.002. [DOI] [PubMed] [Google Scholar]
- 32.Dinglas VD, Colantuoni E, Ciesla N, Mendez-Tellez PA, Shanholtz C, Needham DM. Occupational therapy for patients with acute lung injury: factors associated with time to first intervention in the intensive care unit. Am J Occup Ther. 2013;67(3):355–362. doi: 10.5014/ajot.2013.007807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Badger S, Macleod R, Honey A. "It's not about treatment, it's how to improve your life": The lived experience of occupational therapy in palliative care. Palliat Support Care. 2016;14(3):225–231. doi: 10.1017/S1478951515000826. [DOI] [PubMed] [Google Scholar]
- 34.Kumar SP. Cancer Pain: A Critical Review of Mechanism-based Classification and Physical Therapy Management in Palliative Care. Indian J Palliat Care. 2011;17(2):116–126. doi: 10.4103/0973-1075.84532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kumar SP, Jim A. Physical therapy in palliative care: from symptom control to quality of life: a critical review. Indian J Palliat Care. 2010;16(3):138–146. doi: 10.4103/0973-1075.73670. [DOI] [PMC free article] [PubMed] [Google Scholar]


