Abstract
Background
The goal of this study was to identify the in vivo effects in patients with hyposalivation of a novel slowly dissolving adhering test disc upon on enamel remineralization, oral biofilm, salivary production, pH and buffering, gingival health, and on self-evaluation of oral well-being.
Methods
Five subjects with xerostomia wore custom made retainers carrying 5 demineralized enamel chips for periods of 1 week each. In 1 study arm, subjects used the test agent plus oral hygiene self-care; in the other they used oral hygiene self-care only, with a 1 week washout in between arms. The treatment sequence was randomized. Before and after each study arm Plaque Index (PI), Gingival Index (GI) and Sulcus Bleeding Index (mSBI) were recorded. Clinical plaque staining was quantified using digital image analysis. Saliva production, pH and buffering capacity were recorded. Subjects completed a self-evaluation questionnaire for oral comfort. Enamel samples underwent standardized Knoop microhardness testing to quantify mineralization status.
Results
Plaque presence and clinical Plaque Indices decreased significantly with test agent use (p<0.05). Five-minute saliva production almost doubled 10 and 40 minutes after oral test disc insertion (significant, p<0.05). Salivary pH buffering improved in 4/5 subjects with disc use. All demineralized tooth samples re-hardened intraorally (p>0.05). The discs favorably impacted eating problems and dental sensitivity. Subjects were positive about disc flavor and mouth feel.
Conclusion
Using established in vivo techniques, the effects of a novel product in xerostomic patients were evaluated and quantified. The adhering disc facilitated eating, reduced dental sensitivity, improved saliva production and buffering capacity, reduced plaque, and alleviated xerostomia symptoms.
Clinical Relevance
Xerostomia management is challenging. A novel dry mouth disc was effective in alleviating dry mouth symptoms.
Keywords: Xerostomia, Dry mouth, Hyposalivation, Saliva, Remineralization, Enamel microhardness
Introduction
The causes of xerostomia, or dry mouth symptoms, are multiple, and include medications, systemic disorders, and radiation treatments to the head and neck [1]. Chronic dry mouth affects up to 50% of seniors [2] and approximately 10% of younger persons [3]. The symptoms include a sticky, dry feeling in the mouth; trouble chewing, swallowing, tasting, or speaking; sensations of burning and dryness in the mouth or throat; cracked lips; a dry, rough, swollen tongue; oral ulcerations; greater risk of oral fungal and microbial infections; sleep disturbances and increased prevalence of dental sensitivity and dental caries [1].
Hundreds of medications, including many over-the-counter drugs such as antidepressants, decongestants, antihistamines, muscle relaxants, appetite suppressants and diuretics, produce dry mouth as a side effect [4]. Smoking or chewing tobacco may also increase dry mouth symptoms [4]. Hyposalivation is reported to be a consequence of health conditions such as the autoimmune disease [Sjogren syndrome] or HIV/AIDS [5,6]. Stroke and Alzheimer’s disease may cause a perception of dry mouth, even though the salivary glands may function normally [6,7]. Snoring and mouth breathing contribute to dry mouth during sleep [8]. In approximately 80% of patients receiving head and neck chemo-radiotherapy, reduced saliva flow is a consequence of therapy-related injury to the major and minor salivary glands and is a major cause of oral symptoms during and following therapy. This results in significant risk to oral and dental health [9]. Often forgotten is the sugar content of products used for oral care and sore throat, which may increase caries rate, particularly in patients with hyposalivation [10–12].
Reduced saliva flow has considerable clinical and psychological consequences. It is often implicated in a generalized sensation or manifestation of oral irritation and soreness, which can be exacerbated in dental prosthesis-wearers, also affecting prosthesis retention and tolerance [10]. Saliva plays a crucial role in maintaining oral health, promoting important physiological functions such as antimicrobial effects, and oral pH control. Moreover, the oral microbiota is reliant upon the saliva as a source of proteins essential for bacterial aggregation and metabolism [13]. Typically, persons with dry mouth experience an increased risk of developing dental decay and periodontal disease [14]. The caries protective effects of saliva include dilution and breakdown of ingested sugars, pH buffering capacity, promotion of dental remineralization, and antimicrobial properties [15–18]. Supersaturation of the saliva with calcium, fluoride, and phosphate provides a reservoir of ions that support dental remineralization [19].
Xerostomia can considerably impact a person’s quality of life. Patients complain of oral discomfort, and difficulties with speaking and swallowing [6,20,21]. Indeed, one of the primary causes of poor diet that may result in malnutrition in the elderly is difficulty with chewing, eating and swallowing due to dry mouth [10]. Other symptoms include taste alterations, stickiness in the mouth, difficulty in speaking, and poor sleep [10]. These effects often cause embarrassment, and are implicated in social challenges and reduced participation in communal activities that can exacerbate isolation and withdrawal.
Therapeutic approaches to dry mouth include sialagogues and symptomatic approaches [21]. The former may cause unwanted side effects such as sweating, flushing, nausea, and increased urinary frequency [22]. Moreover, they require adequate residual salivary gland function to be effective, limiting their usefulness in some patients [23]. Specially formulated chewing gum can transiently increase salivary output [24]; however, a three-month study into the effectiveness of regular chewing gum did not determine any improvement in saliva presence [25]. Other symptomatic remedies include topical toothpaste, mouthwash or dissolving lozenges [26]. Some of these commercially accessible products contain lubricating properties that have the goal of increasing mouth wetting and some include antimicrobial enzymes with the goal of decreasing oral infections [25], although the potential effect of these enzymes in vivo has not been clearly shown [25].
The study of in vivo dental remineralization requires long-term follow-up in studies, and is fraught with challenges in determining the quality of dental surfaces at risk for demineralization and caries. Longitudinal studies with controls are costly and may be complicated with ethical issues of disease progression. In this study, a previously validated in vivo model of dental remineralization was employed that permits quantification of enamel mineralization, facilitating the evaluation of products for saliva management, symptom evaluation and dental hard tissue resilience [27–30].
The goal of this clinical study was to evaluate in patients with xerostomia the effects of a novel slowly dissolving adhering disc (OraCoat XyliMeltsR, OraHealth Corp., Bellevue, WA 98005) on oral health, enamel remineralization, saliva presence, pH and buffering, as well as patient comfort.
Materials and Methods
Clinical protocol
This study was performed in 5 subjects with xerostomia who demonstrated an unstimulated whole saliva flow rate below 0.2 ml per minute and a stimulated saliva flow rate of less than 0.5 ml in 5 minutes (mean 0.1 ml/min). A minimum of 5 natural teeth were present in each quadrant (excluding third molars), and subjects were not permitted to add or stop any medications throughout the study duration. This research was executed in full compliance with UCI IRB protocol 2013–9778. All subjects signed an informed consent form at study initiation, as well as a statement of patient rights and a photographic release form.
Subjects wore custom fabricated removable retainers (Figure 1) for 2 periods of 1 week each, with 5 sterilized demineralized enamel chips (Figure 1) attached in the palatal surface of the appliance (Figure 1) [27,28]. The study consisted of 2 arms. In 1 segment a novel slowly dissolving adhering disc was added to the subjects’ usual oral hygiene self-care. The disc releases 550 mg xylitol, and cellulose gum which forms a gel with saliva. It has a mild mint flavor. In the other segment, subjects conducted their usual oral hygiene self-care. They were instructed to use the disc as often as needed during the day to relieve symptoms of dry mouth, and to use two discs while sleeping. A one week washout period was inserted between the 2 study arms. During this period subjects did not wear the retainer and they continued their usual oral hygiene self-care. Subjects were randomized with regard to the sequence of the 2 arms of the study.
Figure 1.

Stages of tooth sample use (i) sterilized enamel chip ready for mounting on retainer, (ii) enamel chips mounted on retainer; (iii) enamel chip embedded for microhardness testing.
Plaque Index (PI), Gingival Index (GI) and Sulcus Bleeding Index (mSBI) were recorded 3 times: at baseline and at the end of each study arm to provide a quantitative measure of gingival health [31–33]. Salivary production, pH and buffering capacity were also determined at these 3 time points using standard 5-minute collection procedure and the Saliva Check Buffer test (GC Co., Tokyo, Japan). Saliva collection was performed 10 and 40 minutes after a subject was seated in a dental chair, as physical movement can affect saliva flow. In the test agent arm, the test disc was inserted into the mouth when the subject sat down in the chair and saliva was collected 10 and 40 minutes later. Subjects also underwent plaque staining (2 Tone™ Disclosing Agent, Young Dental Manufacturing, Earth City, MO 63045) and standardized 4 photography at baseline and at the end of each study arm. Plaque age (color-based) and surface coverage were quantified using Image J software, and calculated as percentage of surface coverage for old (>24 h) and new (<24 h) plaque. Finally, subjects completed a standardized self-evaluation questionnaire for dry mouth and dentinal sensitivity at each visit.
Subjects were provided with the regular usage instructions included in each package of the test discs. Briefly, they were instructed to place a disc in the oral buccal sulcus with the adhesive side against the gingiva whenever their mouth felt dry, then to use their tongue to push the disc to a comfortable spot, and leave it there undisturbed, allowing it to adhere to the gingiva and/or adjoining molar. Subjects were instructed to place 2 discs in the buccal sulcus, one on each side, before going to sleep at night.
Enamel Chips and Microhardness Measurements
Using sterilized extracted teeth classified as healthy by an experienced dentist using a loupe and headlamp, a total of 100 samples were prepared: fifty for use as baseline samples, and fifty for intra-oral mounting on a retainer (5 samples × 5 subjects × 2 study arms). The baseline samples were each cut in half; one half underwent microhardness testing at study initiation to establish original sample microhardness; the other half underwent similar microhardness measurements directly after demineralization. All fifty samples for intra-oral wear also underwent demineralization, which involved 6 hours of demineralization using an acetate/calcium/phosphate buffer at pH 4.4. The buffer contained calcium and phosphate at 2.0 mmol/l, 0.075 mmol/l acetate with 40 ml per sample used individually [34]. The mounted samples were worn in the mouth for 1 week, then removed for microhardness measurements, consisting of 3 individual microhardness indentation measurements in Knoop units on each sample [35].
New chips were placed on each retainer for each study arm. Surface remineralization was determined for 2 time points: (1) after 7-day use of the test discs and (2) after 7 days of abstaining from use of the test product.
For each enamel chip sample set, the following ratios were calculated:
Final microhardness after intra-oral wear vs. Original microhardness and
Final microhardness after intra-oral wear vs. post-demineralization.
Results
All 5 subjects completed the study in full compliance with the study protocol. The subjects used a mean of 4+1 discs each day, and 2 discs each night.
Enamel chips
All tooth samples underwent statistically similar levels of de- and remineralization, softening by 25–30% due to demineralization, and then hardening again in the oral cavity to approximately the pre-demineralization level (Table 1). There were no significant differences between any groupings and comparisons (p>0.05).
Table 1.
Mean microhardness values of tooth chips expressed as ratios of (a) final vs. original microhardness and (b) final vs. post-demineralization microhardness.
| Control (no disc) | Control (no disc) | Test (disc use) | Test (disc use) |
|---|---|---|---|
| Mean Microhardness (MH) ratio (n=50): Mean Final/Original MH | Mean Microhardness (MH) ratio (n=50): Mean Final/Demin MH | Mean Microhardness (MH) ratio (n=50): Mean Final/Original MH | Mean Microhardness (MH) ratio (n=50): Mean Final/Demin MH |
| 1.04 (S.D.=0.16) | 1.32 (S.D.=0.24) | 1.08 (S.D.=0.13) | 1.28 (S.D.=0.23) |
Biofilm
A significant reduction was observed in old and new plaque presence after use of the test discs for 1 week (p<0.05). Old plaque presence fell to approximately 42% of the baseline value, while new plaque presence was reduced to approximately 70% of the baseline level. Plaque levels did not change significantly for any of the other treatment groups during the course of this study (Figure 2).
Figure 2.
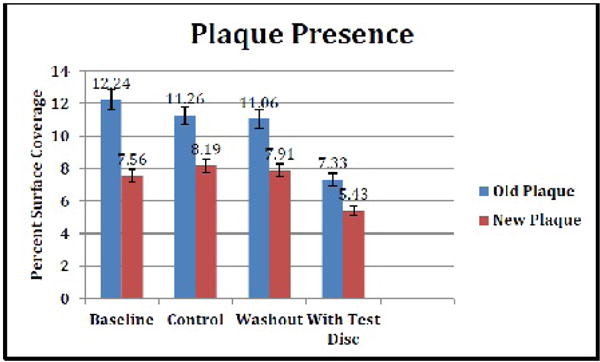
Mean plaque presence on each tooth sample expressed as % of image surface area covered by old (>24 h) and new (<24 h) plaque respectively.
Clinical plaque indices and gingival health
The clinical Plaque Index decreased by approximately 50% after use of the test discs for 1 week (p<0.05). The corresponding reduction in Gingival Index approached a significant level (p=0.0623). All other values did not change significantly during the course of this study (Figure 3).
Figure 3.
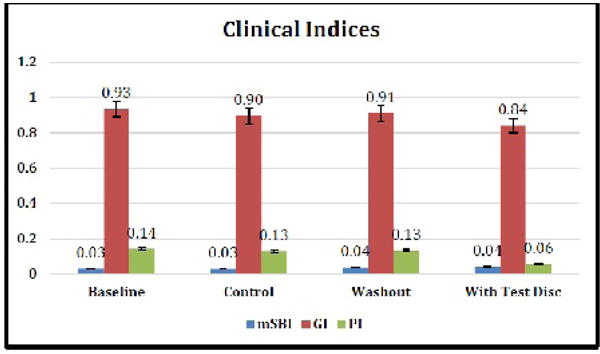
Mean clinical indices at baseline and after 7 days each of Control (no test disc), washout, and test disc use.
Saliva volume, pH and buffering
The volume of saliva collected over 5 minutes after 7 days of XyliMelts use and with a XyliMelts disc adhered in the mouth increased from a mean of 0.23 ml/min at baseline to a mean of 0.56 ml/min, 10 minutes after placement of one disc in the mouth. Forty minutes after disc placement, saliva production was measured at 0.56 ml/min. Thus at both time points more than a doubling of saliva production was measured, representing a statistically significant increase in each case (p<0.05). Salivary pH was not significantly affected by disc use (p>0.05), although salivary pH buffering improved in 4/5 subjects after 7 days of disc use with a disc present in the mouth. No change was observed in the other groups (Figures 4 and 5 and Table 2).
Figure 4.
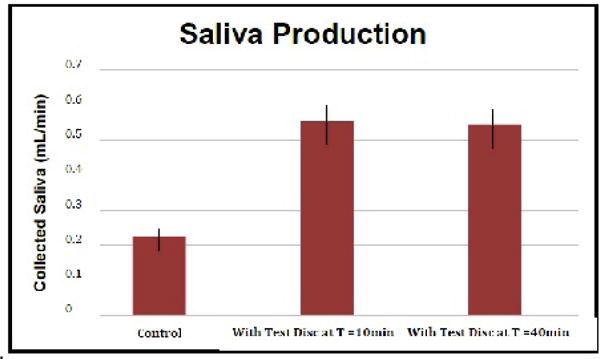
Mean saliva volume collected in xerostomia subjects after 7 days of (i) Control and, (ii) Test disc use, measured at (a) 10 and (b) 40 mins after disc placement in the mouth.
Figure 5.
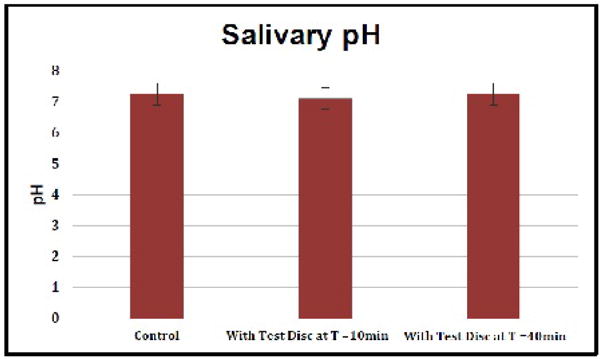
Mean salivary pH in xerostomia subjects after 7 days of (i) Control and (b) Test disc use, measured at (a) 10 and (b) 40 mins after disc placement in the mouth.
Table 2.
PH buffering capacity at (i) baseline, (ii) after 7 days Control and (iii) during use of one test disc.
| Baseline | 7 Days w/o test disc | Washout | 7 Days test disc use with one disc in situ | |
|---|---|---|---|---|
| pH Buffering | Low (5/5) | Low (5/5) | Low (5/5) | Low 1/5; Normal 4/5 |
Self-evaluation questionnaire
Oral health questionnaire: All clinical criteria showed significant (p<0.01) improvement during the test disc use arm of the study except for the categories “oral comfort at waking in the morning” and “do you sip liquids to aid swallowing”, which showed no change from baseline.
Although the subjects reported an improvement in mouth wetness upon awakening, they also reported that the effects and flavor of the discs last approximately 6 hours while sleeping.
The self-evaluation questions showing significant improvement involved oral function, swallowing, and dry mouth symptoms:
I have trouble eating certain solid foods (hard to chew, crumbly, sticky). Food gets stuck in my mouth.
Food gets stuck in my throat.
Problems with dry mouth make chewing and swallowing difficult. I have problems with dry mouth.
Are any of your teeth sensitive to hot, cold, or spicy food or drinks?
Disc Questionnaire
Overall, subject response to the discs was positive, with subjects stating that they would like to continue using the discs, and would recommend them to others. Ease of use, flavor, and mouth feel of the discs as well as overall impression of the product all scored at >80/100. Convenience rated somewhat lower at 60/100; subjects stated that they would prefer a longer-lasting product (Table 3).
Table 3.
Responses to subject questionnaire on a Visual Analogue Scale (VAS) 0–100.
| Mean score on 100 mm VAS (0-worst; 100-best) | ||||
|---|---|---|---|---|
| Oral Health | Baseline | After 7 days test | After 7 days washout | After 7 days control |
| a) Dryness/wetness upon waking in the morning (0-wettest; 100-driest) | 85 | 45 | 80 | 75 |
| b) Mouth comfortable (0)/uncomfortable (100) upon waking in the morning | 90 | 85 | 85 | 90 |
| 2. I have trouble maintaining my weight because of swallowing problems (0-no; 100-a lot) | 0 | 0 | 0 | 0 |
| 3. I have trouble eating certain solid foods (hard to chew, crumbly, sticky)(0-no; 100-a lot) | 75 | 35 | 80 | 70 |
| 4. I have trouble drinking thin liquids (like water, tea, and Ensure®)(0-no; 100-a lot) | 0 | 0 | 0 | 0 |
| 5. Food gets stuck in my mouth (0-no; 100-a lot) | 65 | 10 | 55 | 55 |
| 6. Food gets stuck in my throat (0-no; 100-a lot) | 40 | 5 | 20 | 30 |
| 7. I choke or strangle on liquids (0-no; 100-a lot) | 0 | 0 | 0 | 0 |
| 8. I choke or strangle on solid foods (0-no; 100-a lot) | 0 | 0 | 0 | 0 |
| 9. I have problems with dry mouth (0-no; 100-a lot) | 100 | 60 | 100 | 100 |
| 10. The amount of saliva in my mouth seems to be too little (0-no; 100-a lot) | 100 | 50 | 100 | 100 |
| 11. Problems with dry mouth make chewing and swallowing difficult (0-no; 100-a lot) | 70 | 40 | 60 | 65 |
| 12. Problems with dry mouth affect my ability to sleep (0-no; 100-a lot) | 0 | 0 | 0 | 0 |
| 13. Do you sip liquids to aid in swallowing dry foods? (0-no; 100-a lot) | 50 | 50 | 50 | 50 |
| 14. Problems with dry mouth affect my ability to talk (0-no; 100-a lot) | 0 | 0 | 0 | 0 |
| 15. Are any of your teeth sensitive to hot, cold, or spicy food or drinks (0-no; 100-a lot) | 70 | 40 | 60 | 60 |
| Disc | ||||
| 16. How long do the discs last while sleeping (in hours)? | N/a | 3 | N/a | N/a |
| 17. How long does the effect of the discs last while sleeping (in hours)? | N/a | 6 | N/a | N/a |
| 18. How long does the flavor of the discs last while sleeping (in hours)? | N/a | 6 | N/a | N/a |
| 19. How long do the discs last during the day (in minutes)? | N/a | 120 | N/a | N/a |
| 20. How long does the effect of the discs last during the day (in minutes)? | N/a | 150 | N/a | N/a |
| 21. Please rate the ease of use of the discs (0-100) | N/a | 80 | N/a | N/a |
| 22. Please rate the flavor of the discs (0-100) | N/a | 90 | N/a | N/a |
| 23. Please rate the mouth feel of the discs (0-100) | N/a | 80 | N/a | N/a |
| 24. Please rate the convenience of the discs (0-100) | N/a | 60 | N/a | N/a |
| 25. What is your overall impression of the product? (0-100) | N/a | 80 | N/a | N/a |
| 26. Will you continue to use this product/recommend it to others? Y/N | N/a | Y | N/a | N/a |
Discussion
This 21-day double-blinded, crossover, sequence-randomized study demonstrated the potential usefulness of a novel dissolving disc formulation for symptomatic alleviation of xerostomia. Compliance with use of the study device was excellent. Critical oral functions of eating and swallowing were improved with use of the test product. Also the effect of dry mouth upon sleep disruption was reduced. These are common, severe symptoms that are often difficult to manage. In addition, greater mouth wetness and oral comfort were reported. Importantly, increased salivation was clearly demonstrated in patients using the test product plus standard oral care versus standard oral care alone. This showed that, rather than palliation of dry mouth only, the product also stimulated residual saliva gland function. Key variables for salivary gland stimulation and symptomatic management of xerostomia have been recently described [36].
The previously demineralized enamel slabs that were worn intraorally showed evidence of full remineralization in both the test and control arms of the study. This indicates effective intra-oral remineralization resulting from natural intra-oral processes within the one week trial periods.
Because microhardness was not assessed at earlier endpoints, it was not possible to compare speed and time-based progression of remineralization between test and control legs of the study. In future studies it would be interesting to evaluate time-based remineralization progression in test vs control environments. However, this would require a considerably larger research framework, as microhardness testing cannot be repeated multiple times at different time-points in the same samples. Moreover, an investigation into changes in the oral microbiota related to hyposalivation, and to its mitigation using products such as the one tested in this study would be important, as such shifts can also affect de- and remineralization processes in the dental hard tissues.
Conclusion
This 21-day double-blinded, crossover, sequence-randomized study demonstrated the potential usefulness of a novel slowly dissolving adhering disc formulation for symptomatic alleviation of xerostomia. This research showed desirable effects of the test product on symptomatic management of xerostomia, demonstrating that the test product provided effective local palliation and salivary stimulation without the need for use of systemic sialagogue medications. Advantages of the study design include the feature that each subject acts as his/her own control, cross-over design, and multiple oral health endpoints as well as direct assessment of intra-oral sample remineralization effects. Limitations of this pilot study include the relatively small number of subjects, and the inability to non-invasively and progressively assess sample mineralization status.
Acknowledgments
This research was supported by: LAMMP NIH/NIBIB P41EB05890; NIH/NIBIB R03EB014852; the Arnold and Mabel Beckman Foundation; University of California SOM Seed Grant; UC CRCC 53082, OraHealth Corp.
References
- 1.Ouanounou A. Xerostomia in the Geriatric Patient: Causes, Oral Manifestations, and Treatment. Compend Contin Educ Dent. 2016;145:306–311. [PubMed] [Google Scholar]
- 2.Thomson WM. Issues in the epidemiological investigation of dry mouth. Gerodontology. 2005;22:65–76. doi: 10.1111/j.1741-2358.2005.00058.x. [DOI] [PubMed] [Google Scholar]
- 3.Thomson WM, Poulton R, Broadbent JM, Al-Kubaisy S. Xerostomia and medications among 32-year-olds. Acta Odontologica Scandinavia. 2006;64:249–254. doi: 10.1080/00016350600633243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sreebny LM, Schwartz SS. A reference guide to drugs and dry mouth. (2nd edn) Gerodontology. 1997;14:33–47. doi: 10.1111/j.1741-2358.1997.00033.x. [DOI] [PubMed] [Google Scholar]
- 5.Mignogna MD, Fedele S, Russo L, Muzio L, Wolff A. Sjogren’s syndrome: the diagnostic potential of early oral manifestations preceding hyposalivation/xerostomia. J Oral Pathol Med. 2005;1:1–6. doi: 10.1111/j.1600-0714.2004.00264.x. [DOI] [PubMed] [Google Scholar]
- 6.Ettinger RL. Review: Xerostomia: A Symptom that acts like a Disease. Age and Ageing. 1996;26:409–412. doi: 10.1093/ageing/25.5.409. [DOI] [PubMed] [Google Scholar]
- 7.Donaldson M, Epstein J, Villines D. Managing the care of patients with Sjogren syndrome and dry mouth: comorbidities, medication use and dental care considerations. J Am Dent Assoc. 2014;145:1240–1247. doi: 10.14219/jada.2014.83. [DOI] [PubMed] [Google Scholar]
- 8.Oksenber A, Froom P, Melamed S. Dry mouth upon awakening in obstructive sleep apnea. Journal of Sleep Research. 2006;14:317–320. doi: 10.1111/j.1365-2869.2006.00527.x. [DOI] [PubMed] [Google Scholar]
- 9.Vissink A, Burlage FR, Spijkervet FK, Jansma J, Coppes RP. Prevention and treatment of the consequences of head and neck radiotherapy. Crit Rev Oral Biol Med. 2003;14:213–225. doi: 10.1177/154411130301400306. [DOI] [PubMed] [Google Scholar]
- 10.Cassolato SF, Turnbull RS. Xerostomia: clinical aspects and treatment. Gerodontology. 2003;20:64–77. doi: 10.1111/j.1741-2358.2003.00064.x. [DOI] [PubMed] [Google Scholar]
- 11.Deng J, Jackson L, Epstein JB, Migliorati CA, Murphy BA. Dental demineralization and caries in patients with head and neck cancer. Oral Oncol. 2015;51:824–831. doi: 10.1016/j.oraloncology.2015.06.009. [DOI] [PubMed] [Google Scholar]
- 12.Donaldson M, Goodchild JH, Epstein JB. Sugar content, cariogenicity, and dental concerns with commonly used medications. J Am Dent Assoc. 2015;146:129–133. doi: 10.1016/j.adaj.2014.10.009. 2015. [DOI] [PubMed] [Google Scholar]
- 13.Dowd FJ. Saliva and dental caries. Dent Clin North Am. 1999;43:579–597. [PubMed] [Google Scholar]
- 14.Tjaderhane L. The activation and function of host matrix metalloproteinases in dentin matrix breakdown in caries lesions. Journal of Dental Research. 1998;77:1622–1629. doi: 10.1177/00220345980770081001. [DOI] [PubMed] [Google Scholar]
- 15.Tenovuo JO. Salivary parameters of relevance for assessing caries activity in individuals and populations. Comm Dent Oral Epidemiol. 1997;25:82–86. doi: 10.1111/j.1600-0528.1997.tb00903.x. [DOI] [PubMed] [Google Scholar]
- 16.Dawes C. Salivary Flow Patterns and the Health of Hard and Soft Oral Tissues. The Journal of the American Dental Association. 2008;139:18S–24S. doi: 10.14219/jada.archive.2008.0351. [DOI] [PubMed] [Google Scholar]
- 17.Wolff M, Kleinberg I. Oral mucosal wetness in hypo- and normosalivators. Arch Oral Biol. 1998;43:455–462. doi: 10.1016/s0003-9969(98)00022-3. [DOI] [PubMed] [Google Scholar]
- 18.Koulourides T, Feagin F, Pigman W. Remineralization of dental enamel by saliva in vitro. Annals of the New York Academy of Sciences. 1965;131:751–757. doi: 10.1111/j.1749-6632.1965.tb34839.x. [DOI] [PubMed] [Google Scholar]
- 19.Hicks J, Garcia-Godoy F, Flaitz C. Biological factors in dental caries: role of saliva and dental plaque in the dynamic process of demineralization and remineralization (part 1) Journal of Clinical Pediatric Dentistry. 2004;28:47–52. doi: 10.17796/jcpd.28.1.yg6m443046k50u20. [DOI] [PubMed] [Google Scholar]
- 20.Chambers M, Garden AS, Kies MS, Martin JW. Radiation-induced Xerostomia in Patients with Head and Neck Cancer: Pathogenesis, Impact on Quality of Life, and Management. Head & Neck. 2004;26:796–807. doi: 10.1002/hed.20045. [DOI] [PubMed] [Google Scholar]
- 21.Siegler EL, Capezuti E, Mezey M. The Encyclopedia of Elder Care 2001 [Google Scholar]
- 22.Thelin WR, Brennan MT, Lockhart PB, Singh ML, Fox PC, et al. The oral mucosa as a therapeutic target for xerostomia. Oral Dis. 2008;14:683–689. doi: 10.1111/j.1601-0825.2008.01486.x. [DOI] [PubMed] [Google Scholar]
- 23.Bots CP, Brand HS, Veerman EC. Chewing gum and a saliva substitute alleviate thirst and xerostomia in patients on hemodialysis. Nephrol Dial Transplant. 2005;20:578–584. doi: 10.1093/ndt/gfh675. [DOI] [PubMed] [Google Scholar]
- 24.Jagodzińska M, Zimmer-Nowicka M, Nowicki M. Three Months of Regular Gum Chewing Neither Alleviates Xerostomia nor Reduces Overhydration in Chronic Hemodialysis Patients. J Ren Nutr. 2011;21:410–417. doi: 10.1053/j.jrn.2010.08.002. [DOI] [PubMed] [Google Scholar]
- 25.Epstein JB, Emerton S, Le ND. A double-blind crossover trial of Oral Balance gel and Biotene® toothpaste versus placebo in patients with xerostomia following radiation therapy. Oral Oncology. 1999;25:132–137. doi: 10.1016/s1368-8375(98)00109-2. [DOI] [PubMed] [Google Scholar]
- 26.Nieuw Amerongen AV, Veerman EC. Current therapies for xerostomia and salivary gland hypofunction associated with cancer therapies. Support Care Cancer. 2003;11:226–231. doi: 10.1007/s00520-002-0409-5. [DOI] [PubMed] [Google Scholar]
- 27.Ajdaharian J, Dadkhah M, Sabokpey S, Biren-Fetz J, Chung NE, et al. Multimodality imaging of the effects of a novel dentifrice on oral biofilm. Lasers Surg Med. 2016;46:546–552. doi: 10.1002/lsm.22265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lam T, Ho J, Anbarani AG, Liaw LH, Takesh T, et al. Effects of a Novel Dental Gel on Enamel Surface Recovery from Acid Challenge. Dentistry. 2016;6:397. doi: 10.4172/2161-1122.1000397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nayudu A, Lam T, Ho J, Forghany A. Plaque Removal and Gingival Health after Use of a Novel Dental Gel: A Clinical Study. Dentistry. 2016;6:396. doi: 10.4172/2161-1122.1000396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sahni K, Khashai F, Forghany A, Krasieva T, Wilder-Smith P. Exploring Mechanisms of Biofilm Removal. Dentistry. 2016;6:4. doi: 10.4172/2161-1122.1000371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Löe H. The Gingival Index, the Plaque Index and the Retention Index Systems. J Periodontol. 1967;386:610–616. doi: 10.1902/jop.1967.38.6.610. [DOI] [PubMed] [Google Scholar]
- 32.Turesky S, Gilmore ND, Glickman I. Reduced plaque formation by the chloromethyl analogue of vitamine C. J Periodontol. 1970;41:41–43. doi: 10.1902/jop.1970.41.41.41. [DOI] [PubMed] [Google Scholar]
- 33.Newbrun E. Indices to measure gingival bleeding. J Periodontol. 1996;67:555–561. doi: 10.1902/jop.1996.67.6.555. [DOI] [PubMed] [Google Scholar]
- 34.Stookey GK, Featherstone JD, Rapozo-Hilo M, Schemehorn BR, Williams RA, et al. The Featherstone laboratory pH cycling model: a prospective, multi-site validation exercise. Am J Dent. 2011;24:322–328. [PubMed] [Google Scholar]
- 35.Attin T, Meyer K, Hellwig E, Buchalla W, Lennon AM. Effect of mineral supplements to citric acid on enamel erosion. Arch Oral Biol. 2003;48:753–9. doi: 10.1016/s0003-9969(03)00156-0. [DOI] [PubMed] [Google Scholar]
- 36.Epstein JB, Beier Jensen S. Management of hyposalivation and xerostomia: Criteria for treatment strategies. Compend Contin Educ Dent. 2015;36:600–603. [PubMed] [Google Scholar]


