Summary
The aim of this paper is to report our experience and to present a review of literature about the use of teriparatide off-label in the therapy of non-unions. Teriparatide is used exclusively in treatment of osteoporosis and to prevent bone fracture because it has a positive effect on bone strength and architecture. The use of teriparatide in non-unions is described as effective in numerous case report.
Keywords: teriparatide, osteoporosis, non-union, bone remodeling
Introduction
Fracture healing usually occurs spontaneously, by a primary way, if fracture fragments are very close and stable, or more often by a secondary healing through the production of abundant repairing tissue, the callus, if a gap or micro-movements between the fracture fragments are present (1).
There are several conditions affecting the rate of fracture healing: they are divided in general and local factors.
In the first group there are the age, the type of bone involved, nutritional status, drug therapy and bone pathology: speed of union of the fracture decreases with skeletal maturity and also if the patient is not in good nutritional status, many drugs and pre-existing bone pathology adversely affect fracture healing such as corticosteroids, NSAIDs or osteogenesis imperfecta and others metabolic disease of bone.
Local factors are the separation of bone ends, the disturbance of blood supply, infections, the property of bone involved and the type of fracture: bone ends must not be separated or with soft tissue interposition, blood supply is fundamental and its interruption may lead to necrosis, pathogens interact with reparative cellular activity resulting in a prolonged inflammatory phase and finally, any type and localization of fracture heal according to their intrinsic characteristics.
Movement of the fracture site interferes with vascularization of haematoma, disrupts bridging callus and endosteal bone growth. On the other side, an optimal balance between stability and micro-motion encourages callus formation and produces electrical local currents which improve bone healing by stimulating an inflammatory-type response and promoting calcification of fibrocartilage. Low-intensity pulsed ultrasound plays a relevant role in biomechanical environment, it accelerates fracture healing perhaps by acting directly to proliferation and differentiation of multipotent human bone marrow-derived mesenchymal stromal cells (2). Actually, the use of Platelet-Rich Plasma (PRP) seems to play an important role in the fracture healing and to favor fusion processes in spinal arthrodesis (3). Due to their osteoconduction activity, bone substitutes too such as hydroxyapatite and tricalcium phosphate represent an important resource to be used in delayed bone healing and in atrophic non-union with large bone gap (4).
The definition of non-union in fracture healing is a disturbance of normal repairing process with the expectation that no consolidation will be achieved without focused and accurate treatment (5).
Non-union are defined according to the American Food and drug Administration (FDA 1988) as “established when a minimum of 9 months has elapsed since injury and the fracture shows no visible progressive signs of healing for 3 months” (6). This definition is not always true because the healing time of a fracture depends from the bone concerned, for example a diaphyseal fracture of the femur needs for at least 4–6 months to heal. In some cases, it needs more time, especially if the fracture is open or comminuted. On the other hand, a femoral neck fracture can be considered as a non-union after only 3 months.
Here we want to focus on some of the aspects shown in non-unions that seem to be potential biomechanical and biochemical environment targets for teriparatide.
Non-union classifications
The non-union of fractures remains a challenging and clinically important problem in orthopaedic surgery.
There are many classifications on non-union, but the one that best classifies them according to different vitality and healing potential is the work of Weber and Ĉech in 1976. He described three type of non-union: hypertrophic, oligotrophic, and atrophic.
Hypertrophic non-union is characterized by hypervascular and/or hypertrophic ends of the fragment, high inflammatory reaction with rich blood supply visible in bone scintigraphy. The amount of the external callus is variable in response to motion at the fracture site. Bone scans in this type of non-union show increased activity at the fracture site, implying vascularity and osteogenesis (7).
In atrophic non-union, fragments have no biological reaction. Contrary to what happens in hypertrophic non-unions, here we do not find an adequate blood supply at the ends of the fragment, the inflammatory reaction is abolished, there is not a callus visible and the facture line persist.
In oligotrophic non-unions, there is minimal callus formation, but some biologic activity is maintained. This happens when the fracture fragments are not correctly apposed.
It is the oligotrophic and atrophic non-unions, which have impaired biologic potential to unite, that require a treatment directed toward improving the osteogenic ability and biology of fracture-healing.
The role of PTH in bone remodeling
PTH has a predominant role in regulating calcium-phosphate metabolism and it is secreted by parathyroid when serum calcium levels decrease.
Parathyroid hormone (PTH) secretion is characterized by an ultradian rhythm with tonic and pulsatile components. In healthy subjects, the majority of PTH is secreted in tonic fashion, whereas approximately 30% is secreted in low-amplitude and high-frequency bursts occurring every 10–20 min, superimposed on tonic secretion (8).
The pulsatile secretion of PTH may have a role in physiological regulation of bone metabolism and structure. Although there are no animal models investigating specifically the skeletal effects of pulsatile PTH secretion, there is experimental evidence that intermittent administration of pharmacological doses of PTH has a bone anabolic effect, while continuous PTH administration is detrimental for the skeleton due to stimulation of bone resorption (9).
In hyperparathyroidism is well-known the catabolic effect on skeleton by continuous exposure to PTH, bone loss can be appreciated in both cortical and trabecular compartments of the skeleton (10).
Conversely, the foreshortened amino terminal peptide of PTH, teriparatide [PTH (1–34)] and the full length molecule [PTH (1–84)] are osteoanabolic when administered once daily in low doses for the treatment of osteoporosis (11–15).
It has been shown that teriparatide also accelerates fracture healing by improving the biomechanical properties of the fracture callus, increasing endochondral ossification and bone remodeling in animal models. This effect has been observed in several case reports (16).
The increase in the PTH-mediated bone resorption is due to an increased activity of the osteoclasts, but in vivo and in vitro studies show that the PTH action on osteoclast is indirect and mediated by osteoblasts and osteocytes (17, 18).
The OPG-RANKL-RANK pathway plays a critical role in bone resorption induced by PTH. In fact, continuous and high PTH levels increase RANKL and decrease OPG expression; the final result is an increased RANKL/OPG ratio that leads osteoclastogenesis and bone resorption (19–21).
The cells involved in bone formation process are many and they have all the PTH receptors. They are preosteoblasts, osteoblasts, lining cells, T-cells and osteocytes (22).
The stimulatory effects of PTH on bone formation have been explained by the so-called ‘anabolic window’, which means that during PTH treatment, bone formation is in excess over bone resorption during the first 6–18 months. This is due to the following: 1) PTH(1–34) seems to induce the proto-oncogene c-fos levels in osteoblastic cells in vitro via the activation of cyclic adenosine mono phosphate (cAMP) (23), 2) PTH induces an increase in IGF-I expression in osteoblasts, 3) bone lining cells are driven to differentiate into osteoblasts and mesenchymal stem cells residing in the bone marrow increase c-fos expression (24), 4) mesenchymal stem cells adhesion to bone surface is enhanced, 5) PTH has a direct antiapoptotic effect on osteoblasts throw a pathway involving cAMP-mediated PKA signaling, and subsequent phosphorylation and inactivation of the apoptotic protein Bad, 6) when PTH interferes with remodeling, the osteoblasts over-compensate (25), and 7) PTH also decreases sclerostin levels, thereby removing inhibition of Wnt signaling which is required for PTH’s anabolic actions (26, 27).
Clinical data on use of teriparatide off-label
So far only a few studies have been conducted on the use of teriparatide in fracture healing.
In 2012 a prospective study was conducted involving 14 consecutive patients presenting during 2 years with atypical femoral fracture. Administration of 20 μg of teriparatide subcutaneously daily for 6 months to 5 of the 14 patients was associated with 2–3 fold increase in bone remodeling markers and fracture healing (28).
In 2011, a prospective randomized controlled study was published where PTH (1–84) administration determined in 21 patients, within a sample of 65 postmenopausal osteoporotic women suffering from pelvis fracture, a faster repair with an improvement in functional outcome (29).
In 2009, a prospectic double blinded randomized controlled study on the effect of teriparatide therapy on the fracture healing, in 102 postmenopausal women with Colles fracture, demonstrated that 20 μg of teriparatide significantly reduce healing time, compared with placebo, but also with the 40 μg higher dose therapy. The study failed to prove the initial hypothesis of a dose related positive effect of teriparatide on bone healing. The effect was also seen through an increase in the resistance to load (30).
In the last years many case reports about the efficacy of use of teriparatide off-labels have been presented to the scientific community.
In 2009, Angel Otero-Alvaro reported of a 32-year-old Caucasian male with right diaphyseal humeral fracture fixed with elastic nail that after 6 months shown an atrophic non-union. The patient was treated with 20 μg/days of teriparatide and after 5 months of treatment healing was complete (31).
In 2015, was performed a retrospective chart review of patients with fracture non-union, aged 10 to 99, treated with teriparatide between 2002 and 2013. Six patients aged 19 to 64 years with tibial or femoral fractures that had not healed for 3 to 36 months were treated with teriparatide 20 μg/day. Accelerated healing of fracture non-union was confirmed in 5 of 6 patients with time to complete union of 3 to 9 months. The shortest time to recovery was observed in younger patients without comorbidities (32).
Holm J. reported a case of a successfully healed atypical femoral fracture (AFF) following treatment with teriparatide in a patient with osteogenesis imperfecta (OI). The patient was treated with hormone replacement therapy for 18 years and bisphosphonates for 9 years before suffering a spontaneous AFF in the form of a dislocated non-comminute transverse fracture of the right femoral shaft, and an open reduction and internal fixation (ORIF) with a T2 femoral nail was done. Due to non-union and another fracture distal to the nail, the patient was re-operated on with exchange ORIF and off-label treatment with teriparatide 20 μg/day was started. An X-ray 1 month later showed early signs of fracture healing. A subsequent X-ray 6 months after the last operation showed a solid healing of both right femoral fractures (33).
Etxebarria-Foronda I. reported of a young male patient diagnosed with osteogenesis imperfecta and who received treatment with bisphosphonates for several years, developing over time an atypical diaphyseal femoral fracture which was treated surgically by means of an intramedullary nailing and with later pharmacological treatment with teriparatide, with a satisfactory outcome at one-year follow-up (34).
Mouyis M. reported a case of a 76-years-old-woman with rheumatoid arthritis, osteoporosis, multiple comorbidities and septic left elbow prosthesis. Treatment included combination antibiotic therapy and removal of the prosthesis. Week later she was started on teriparatide. Her elbow symptoms resolved (35).
Lee YK. reported 3 cases of femur non-union after initial surgical intervention. Teriparatide was administered for 3–9 months after a diagnosis of non-union. A successful union was obtained in all 3 patients without further surgical intervention, and no adverse events related to the use of teri-paratide were observed (36).
Hiroyuki T. presented two cases of incomplete atypical femoral fractures showing a favorable course after being treated by locking plate surgery and prescribed teriparatide (37).
Caffarelli C. described a successful novel therapeutic intervention with teriparatide with one patient with Rett syndrome, after suffering from recurrent low-trauma fractures at intervals of several years. Treatment consists with teriparatide and subsequently with intravenous bisphosphonate. Since the initiation of the treatment, there was an evident improvement at densitometric and QUS parameters. Until the present, no new fractures have appeared (38).
Corrigan R.A. reported a case of a 21-year-old female with extended oligoarticular juvenile idiopathic arthritis diagnosed at the age of 8 years who sustained a low-impact short oblique closed fracture of her right lower tibia. The fracture failed to unite over 2 years. Bone healing following prolonged non-union was induced by combined treatment with teriparatide and a single zoledronic acid infusion; while calcification of the callus could have occurred in the absence of zoledronic acid, the callus should have started to calcify within 12 weeks of teriparatide therapy (39).
Chintamaneni S. reported a case of a 67-year-old white male who was involved in a motor vehicle accident in December 2007. He sustained a fracture of the body of the sternum which subsequently failed to heal, and an atrophic non-union was demonstrated by repeated CT. The patient consented to an empiric trial of teriparatide (20 μg sq injection daily) in an attempt to treat the atrophic non-union. Follow-up imaging studies revealed significant healing of the sternal non-union within 3 months and complete healing after 9 months (40).
Mitani Y. described a case of 88-year-old female with rheumatoid arthritis and a Garden type II displaced femoral neck fracture who underwent surgery with a Hansson hook-pin system. At 11 months, the patient still complained of mild groin pain on ambulation. A diagnosis of non-union was given. The patient accepted treatment with a once-weekly injection of 56.5 μg chemically synthesized teriparatide. At 18 months post-operatively, CT imaging after 20 consecutive weekly administrations of teriparatide revealed signs of healing and the patient reported a gradual decrease in groin pain on ambulation. Complete union of the fracture was obtained at 23 months (41).
Nozaka K.reported a case of a 56-year-old Japanese male with a femoral shaft fracture who underwent intramedullary osteosynthesis nailing initially. He had no radiologic or clinical sign of healing 3 months later and low-intensity pulsed ultrasound was initiated at that time. He was reassessed in another 3 months, with evidence of mild bone consolidation but the fracture gap persisted. Subsequent treatment with human parathyroid hormone was initiated in combination with low-intensity pulsed ultrasound. Full fracture healing was present 6 months after beginning the combination low-intensity pulsed ultrasound and teriparatide (42).
Giannotti S. reported a case of a Caucasian 80-year-old white woman who had an accident in October 2011. She was diagnosed with right distal metaphyseal femoral fracture on total knee arthroplasty. She underwent surgery at our center consisting of ORIF with lateral femoral locking plate. Radiological controls at 5 and 7 months show signs of atrophic non-union. After 2 months of treatment with 20 μg/day of teriparatide, X-ray showed the presence of bone bridges and a decreased gap. After 3 months of treatment healing was complete (43).
Ochi K. described a case of a 74-year-old woman with a 26-year history of rheumatoid arthritis who sustained a peri-prosthetic femoral fracture secondary to a fall from the stairs that occurred 13 years after she underwent TKA. The fracture was internally fixed with a periarticular locking plate and hydroxyapatite graft and additionally treated with daily low-intensity pulsed ultrasound. Non-union became apparent when the locking plate broke 9 months after the internal fixation. Patient underwent to a second intervention. Nine months after, scan revealed signs of non-union. Thus, the patient was additionally treated with once-weekly teriparatide injections for 6 months so as to heal the fracture (44).
Tachiiri H. reported 2 cases of delayed union that were effectively treated with weekly teriparatide administration. The first case is a 72-year-old woman with delayed union after 4 months from treatment of hallux valgus. The second case is a 72-year-old woman with delayed union after 4 months from open reduction and internal fixation of an olecranon fracture (45).
Personal experience
We report of a case of a 38-year-old man who had a car accident in June of 2011 (the patient authorized his clinical data to be published in a scientific journal) with a left diaphyseal comminuted humeral fracture. He underwent surgery consisting of osteosynthesis with a bridge plate and 6 screws. Radiologic controls at 4 months did not show any signs of healing, a 1 cm gap between fracture fragments was present (Figure 1). The patient underwent revision surgery 8 months after the first surgery removing plate and screws and positioning anterograde intramedullary nailing and autologous iliac bone grafts (Figure 2). X-rays achieved 3 months after the revision surgery did not show any signs of healing (Figure 3). This was consistent with the clinical manifestations of pain, movements at the fracture site, and left arm weakness. The physical examination and laboratory tests, including white blood cell counts, C-reactive protein, and erythrocyte sedimentation rate, were normal, which permitted to rule out underlying infection. The patient denied smoking, alcohol abuse, and had no history of metabolic disease or glucocorticoid intake.
Figure 1.
Plain radiographs achieved 4 months post-op show atrophic non-union with a 1 cm gap of the fracture line.
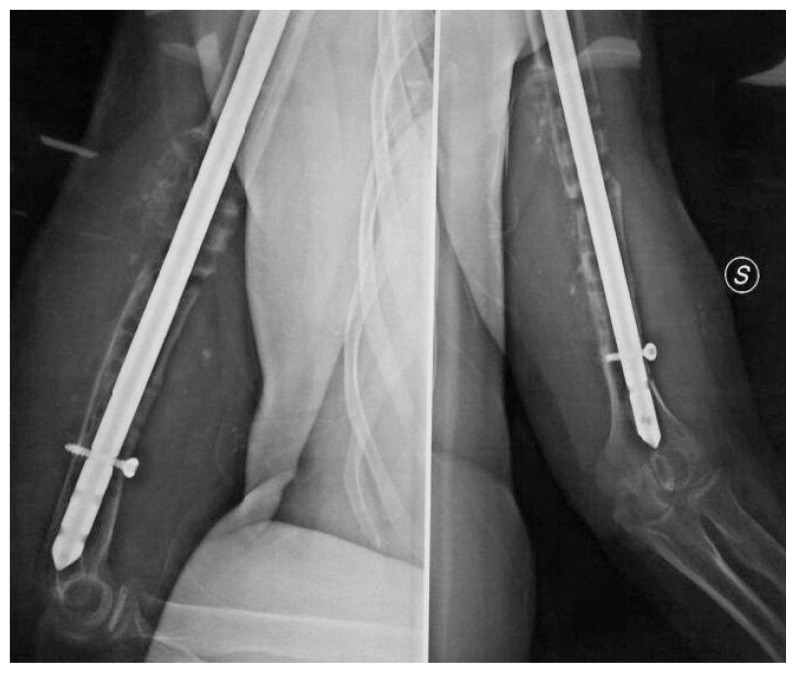
Figure 2.
Plain radiographs achieved after revision surgery using anterograde intramedullary nail.
Figure 3.
Plain radiographs achieved 3 months after the revision surgery did not show any signs of bone healing.
The patient refused to be re-operated to perform a new osteosynthetis, and accepted an empiric, off-label therapy with teriparatide at approved doses for the treatment of osteoporosis (20 μg/day). After 3 months of treatment with teriparatide radiographs showed bone bridges and a reduction of the gap between fragments (Figure 4). After 6 months of treatment bone healing was complete (Figure 5) and clinical manifestations disappeared. No side effect due to the drug was observed during treatment.
Figure 4.
Plain radiographs achieved after 3 months of treatment with teriparatide showed bone bridges and a reduction of the gap of the fracture line.
Figure 5.
Plain radiographs achieved after 6 months of treatment with teriparatide showed fracture healing and bone remodeling.
Discussion
Scientific literature of last year seems to show a great efficacy of teriparatide to treat bone non-unions.
There is increasing evidence that treatment with PTH (1–34) enhances callus formation by stimulating the proliferation and differentiation of osteoprogenitor cells and increasing the production of bone matrix proteins (46, 47).
The basic science studies suggest at least two mechanisms for bone formation: 1) stimulation of endochondral ossification, perhaps by slowing hypertrophic chondrocyte differentiation and thus maintaining a pool of proliferative chondrocytes and 2) stimulation of mesenchymal cell differentiation into osteoblasts (48).
These mechanisms and the anabolic effect of PTH (1–34) on bone density and periosteal bone formation in osteoporotic patients suggest a role for this agent in accelerating fracture healing.
Conclusion
In different case reports teriparatide showed to have positive effect on fracture healing.
The evidence suggests that teriparatide may give a further boost in healing process when fracture environments do not permit its healing.
Especially in hypertrophic non-union where the biologic reaction is increased in response to an altered biomechanical environment we can find several cytokines that play an important regulatory role in the process of osteogenesis. Most importantly, the expression of many of these molecules has been shown to be influenced by mechanical load (49).
Mechanical stress can be considered the cause of hypertrophic non-union but many studies supports the notion that the microenvironment or niche is chiefly modulated by the mechanical forces applied to the area. The osteoblasteosteocyte network is reported to play an essential role by providing natural cues for osteocyte differentiation (50, 51).
It is not yet clear how teriparatide acts on fracture healing, but the presented evidences show a hypothetical common points in non-union biomechanical environment and action of teriparatide.
In conclusion, on the strength of available data, it is possible to affirm that the use of teriparatide off-label has a positive and additive effect when combined with primary treatment.
Ethical considerations
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
References
- 1.Wraighte PJ, Scammell BE. Principles of fracture healing. Surgery (Oxford) 2006;24(6):198–207. doi: 10.1383/surg.2006.24.6.198. (2006) [DOI] [Google Scholar]
- 2.Nam HY, Pingguan-Murphy B, Amir Abbas A, Merican AM, Kamarul T. The proliferation and tenogenic differentiation potential of bone marrow-derived mesenchymal stromal cell are influenced by specific uniaxial cyclic tensile loading conditions. Biomechanics and Modeling in Mechanobiology. 2015;14(3):649–663. doi: 10.1007/s10237-014-0628-y. [DOI] [PubMed] [Google Scholar]
- 3.Caggiari G, Mosele GR, Leonardo Puddu L, Ciurlia E, Doria C. Efficacy of platelet-rich plasma in experimental instrumented interbody spinal fusion. Euromediterranean Biomedical Journal. 2016;11(20):141–147. [Google Scholar]
- 4.Doria C, De Santis V, Falcone G, Proietti L, De Santis E. Osseointegration in hip prostheses: Experimental study in sheep. International Orthopaedics (SICOT) 2003;27:272–277. doi: 10.1007/s00264-003-0474-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Frölke JPM, Patka P. Definition and classification of fracture non-unions. Injury. 2007;38( Suppl 2):S19–S22. doi: 10.1016/s0020-1383(07)80005-2. [DOI] [PubMed] [Google Scholar]
- 6.USFDA. Guidance Document for the Preparation of Investigational Device Exemptions and Pre-Marked Approval Application for Bone Growth Stimulator Devices. Rockville, MD: United States Food and Drug Administration; 1988. [Google Scholar]
- 7.Kivinitty PK, Kaski P. Strontium-85 profile counting in fractures of the tibial shaft. Acta Orthop Scand. 1975;46:569–578. doi: 10.3109/17453677508989239. [DOI] [PubMed] [Google Scholar]
- 8.Chiavistelli S, Giustina A, Mazziotti G. Parathyroid hormone pulsatility: physiological and clinical aspects. Bone Res. 2015;3:14049. doi: 10.1038/boneres.2014.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hock JM, Gera I. Effects of continuous and intermittent administration and inhibition of resorption on the anabolic response of bone to parathyroid hormone. J Bone Miner Res. 1992;7:65–72. doi: 10.1002/jbmr.5650070110. [DOI] [PubMed] [Google Scholar]
- 10.Stein EM, Silva BC, Boutroy S, Zhou B, Wang J, Udesky J, Zhang C, McMahon DJ, Romano M, Dworakowski E, et al. Primary hyper-parathyroidism is associated with abnormal cortical and trabecular microstructure and reduced bone stiffness in postmenopausal women. J Bone Miner Res. 2013;28(5):1029–1040. doi: 10.1002/jbmr.1841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Neer RM, Arnaud CD, Zanchetta JR, Prince R, Gaich GA, Reginster JY, Hodsman AB, Eriksen EF, Ish-Shalom S, Genant HK, et al. Effect of parathyroid hormone (1–34) on fractures and bone mineral density in postmenopausal women with osteoporosis. N Engl J Med. 2001;344:1434–1441. doi: 10.1056/NEJM200105103441904. [DOI] [PubMed] [Google Scholar]
- 12.Greenspan L, Bone HG, Ettinger MP, Hanley DA, Lindsay R, Zanchetta JR, Blosch CM, Mathisen AL, Morris SA, Marriott TB. Effect of recombinant human parathyroid hormone (1–84) on vertebral fracture and bone mineral density in postmenopausal women with osteoporosis: a randomized trial. Ann Intern Med. 2007;146:326–339. doi: 10.7326/0003-4819-146-5-200703060-00005. [DOI] [PubMed] [Google Scholar]
- 13.Caggiari G, Tranquilli Leali P, Mosele GR, Puddu L, Badessi F, Doria C. Safety and effectiveness of teriparatide vs alendronate in post-menopausal osteoporosis: A prospective non randomized clinical study. Clin Cases Miner Bone Metab. 2016;13(3):200–203. doi: 10.11138/ccmbm/2016.13.3.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tranquilli Leali P, Muresu F, Melis A, Ruggiu A, Zachos A, Doria C. Skeletal fragility definition. Clin Cases Miner Bone Metab. 2011;8(2):11–13. [PMC free article] [PubMed] [Google Scholar]
- 15.Tranquilli Leali P, Doria C, Zachos A, Ruggiu A, Milia F, Barca F. Bone fragility: Current reviews and clinical features. Clin Cases Miner Bone Metab. 2009;6(2):109–113. [PMC free article] [PubMed] [Google Scholar]
- 16.Cipriano CA, Issack PS, Shindle L, et al. Recent advances toward the clinical application of PTH (1–34) in fracture healing. HSSJ. 2009;5(2):149–153. doi: 10.1007/s11420-009-9109-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McSheehy PM, Chambers TJ. Osteoblastic cells mediate osteoclastic responsiveness to parathyroid hormone. Endocrinology. 1986;118:824–828. doi: 10.1210/endo-118-2-824. [DOI] [PubMed] [Google Scholar]
- 18.Xiong J, O’Brien CA. Osteocyte RANKL: new insights into the control of bone remodeling. J Bone Miner Res. 2012;27:499–505. doi: 10.1002/jbmr.1547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee K, Deeds JD, Chiba S, Un-No M, Bond AT, Segre GV. Parathyroid hormone induces sequential c-fos expression in bone cells in vivo: in situ localization of its receptor and c-fos messenger ribonucleic acids. Endocrinology. 1994;134:441–450. doi: 10.1210/endo.134.1.8275957. [DOI] [PubMed] [Google Scholar]
- 20.Ma YL, Cain RL, Halladay DL, Yang X, Zeng Q, Miles RR, Chandrasekhar S, Martin TJ, Onyia JE. Catabolic effects of continuous human PTH (1–38) in vivo is associated with sustained stimulation of RANKL and inhibition of osteoprotegerin and gene-associated bone formation. Endocrinology. 2001;142:4047–4054. doi: 10.1210/endo.142.9.8356. [DOI] [PubMed] [Google Scholar]
- 21.Huang JC, Sakata T, Pfleger LL, Bencsik M, Halloran BP, Bikle DD, Nissenson RA. PTH differentially regulates expression of RANKL and OPG. J Bone Miner Res. 2004;19:235–244. doi: 10.1359/JBMR.0301226. [DOI] [PubMed] [Google Scholar]
- 22.Bringhurst FR, Demay MB, Kronenberg HM. Hormones and disorders of mineral metabolism. In: Kronenberg HM, Melmed S, Polonsky KS, Larsen PR, editors. Williams Textbook of Endocrinology. edn 11. Vol. 1. Saunders: Elsevier; 2008. pp. 1203–1268. [Google Scholar]
- 23.Karaplis AC, Goltzman D. PTH and PTHrP effects on the skeleton. Rev Endocr Metab Disord. 2000;1:331–341. doi: 10.1023/a:1026526703898. [DOI] [PubMed] [Google Scholar]
- 24.Lee K, Deeds JD, Chiba S, Un-No M, Bond AT, Segre GV. Parathyroid hormone induces sequential c-fos expression in bone cells in vivo: in situ localization of its receptor and c-fos messenger ribonucleic acids. Endocrinology. 1994;134:441–450. doi: 10.1210/endo.134.1.8275957. [DOI] [PubMed] [Google Scholar]
- 25.Komarova SV. Mathematical model of paracrine interactions between osteoclasts and osteoblasts predicts anabolic action of parathyroid hormone on bone. Endocrinology. 2005;146:3589–3595. doi: 10.1210/en.2004-1642. [DOI] [PubMed] [Google Scholar]
- 26.Aslan D, Andersen MD, Gede LB, de Franca TK, Jørgensen SR, Schwarz P, Jørgensen NR. Mechanisms for the bone anabolic effect of parathyroid hormone treatment in humans. Scand J Clin Lab Invest. 2012;72(1):14–22. doi: 10.3109/00365513.2011.624631. [DOI] [PubMed] [Google Scholar]
- 27.Liu F, Kohlmeier S, Wang CY. Wnt signaling and skeletal development. Cell Signal. 2008;20:999–1009. doi: 10.1016/j.cellsig.2007.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chiang CY, Zebaze RM, Ghasem-Zadeh A, Iuliano-Burns S, Hardidge A, Seeman E. Teriparatide improves bone quality and healing of atypical femoral fractures associated with bisphosphonate therapy. Bone. 2013;52(1):360–365. doi: 10.1016/j.bone.2012.10.006. [DOI] [PubMed] [Google Scholar]
- 29.Peichl P, Holzer LA, Maier R, Holzer G. Parathyroid Hormone 1–84 Accelerates Fracture-Healing in Pubic Bones of Elderly Osteoporotic Women. J Bone Joint Surg Am. 2011;93:1583–1587. doi: 10.2106/JBJS.J.01379. [DOI] [PubMed] [Google Scholar]
- 30.Aspenberg P, Genant HK, Johansson T, Nino AJ, See K, Krohn K, García-Hernández PA, Recknor CP, Einhorn TA, Dalsky GP, Mitlak BH, Fierlinger A, Lakshmanan MC. Teriparatide for acceleration of fracture repair in humans: a prospective, randomized, double-blind study of 102 postmenopausal women with distal radial fractures. J Bone Miner Res. 2010;25:404–414. doi: 10.1359/jbmr.090731. [DOI] [PubMed] [Google Scholar]
- 31.Oteo-Alvaro A, Moreno E. Atrophic humeral shaft nonunion treated with teriparatide (rh PTH 1–34): a case report. J Shoulder Elbow Surg. 2010;19:22–28. doi: 10.1016/j.jse.2010.05.005. [DOI] [PubMed] [Google Scholar]
- 32.Mancilla EE, Brodsky JL, Mehta S, Pignolo RJ, Levine MA. Teriparatide as a systemic treatment for lower extremity nonunion fractures: a case series. Endocr Pract. 2015;21(2):136–142. doi: 10.4158/EP14315.OR. [DOI] [PubMed] [Google Scholar]
- 33.Holm J, Eiken P, Hyldstrup L, Jensen JE. Atypical femoral fracture in an osteogenesis imperfecta patient successfully treated with teriparatide. Endocr Pract. 2014;20(10):187–190. doi: 10.4158/EP14141.CR. [DOI] [PubMed] [Google Scholar]
- 34.Etxebarria-Foronda I, Carpintero P. An atypical fracture in male patient with osteogenesis imperfecta. Clin Cases Miner Bone Metab. 2015;12( 3):278–281. doi: 10.11138/ccmbm/2015.12.3.278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mouyis M, Fitz-Clarence H, Manson J, Ciurtin C. Teriparatide: an unexpected adjunct for the treatment of a long-standing infected elbow prosthesis prevented arm amputation. Clin Rheumatol. 2015;34(4):799–800. doi: 10.1007/s10067-015-2909-y. [DOI] [PubMed] [Google Scholar]
- 36.Lee YK, Ha YC, Koo KH. Teriparatide, a nonsurgical solution for femoral nonunion? A report of three cases. Osteoporos Int. 2012;23(12):2897–2900. doi: 10.1007/s00198-012-2172-x. [DOI] [PubMed] [Google Scholar]
- 37.Tsuchie H, Miyakoshi N, Nishi T, Abe H, Segawa T, Shimada Y. Combined Effect of a Locking Plate and Teriparatide for Incomplete Atypical Femoral Fracture: Two Case Reports of Curved Femurs. Case Reports in Orthopedics. 2015 doi: 10.1155/2015/213614. Article ID 213614. http://dx.doi.org/10.1155/2015/213614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Caffarelli C, Hayek J, Nuti R, Gonnelli S. Teriparatide in the treatment of recurrent fractures in a Rett patient. Clin Cases Miner Bone Metab. 2015;12(3):253–256. doi: 10.11138/ccmbm/2015.12.3.253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Corrigan RA, Miller A, McNally MA, Javaid MK. Treatment of fracture non-union in a young adult with combination anabolic and anti-resorptive bone therapy. Rheumatology. 2013;52(6):1147–1149. doi: 10.1093/rheumatology/kes319. [DOI] [PubMed] [Google Scholar]
- 40.Chintamaneni S, Finzel K, Gruber BL. Successful treatment of sternal fracture nonunion with teriparatide. Osteoporos Int. 2010;21(6):1059–1063. doi: 10.1007/s00198-009-1061-4. [DOI] [PubMed] [Google Scholar]
- 41.Mitani Y. Effective treatment of a steroid-induced femoral neck fracture nonunion with a once-weekly administration of teriparatide in a rheumatoid patient: a case report. Arch Osteoporos. 2013;8:131. doi: 10.1007/s11657-013-0131-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nozaka K, Shimada Y, Miyakoshi N, Yamada S, Hongo M, Kasukawa Y, Saito H, Kijima H. Combined effect of teriparatide and low-intensity pulsed ultrasound for nonunion: a case report. BMC Res Notes. 2014;7:317. doi: 10.1186/1756-0500-7-317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Giannotti S, Bottai V, Dell’Osso G, De Paola G, Pini E, Guido G. Atrophic femoral nonunion successfully treated with teriparatide. European Journal of Orthopaedic Surgery & Traumatology. 2013;23(Suppl 2):291–294. doi: 10.1007/s00590-012-1143-4. [DOI] [PubMed] [Google Scholar]
- 44.Ochi K, Ikari K, Naomi A, Momohara S. Administration of teriparatide treatment for a challenging case of nonunion of periprosthetic fracture after total knee arthroplasty. Arch Osteoporos. 2013;8:159. doi: 10.1007/s11657-013-0159-7. [DOI] [PubMed] [Google Scholar]
- 45.Tachiiri H, Okuda Y, Yamasaki T, Kusakabe T. Weekly teriparatide administration for the treatment of delayed union: a report of two cases. Arch Osteoporos. 2014;9:179. doi: 10.1007/s11657-014-0179-y. [DOI] [PubMed] [Google Scholar]
- 46.Kronenberg HM. PTHrP and skeletal development. Ann NY Acad Sci. 2006;1068:1–13. doi: 10.1196/annals.1346.002. [DOI] [PubMed] [Google Scholar]
- 47.Martin TJ, Quinn JM, Gillespie MT, et al. Mechanisms involved in skeletal anabolic therapies. Ann NY Acad Sci. 2006;1068:458–470. doi: 10.1196/annals.1346.043. [DOI] [PubMed] [Google Scholar]
- 48.Dhaliwal K, Kunchur R, Farhadieh R. Review of the cellular and biological principles of distraction osteogenesis: An in vivo bioreactor tissue engineering model. Journal of Plastic, Reconstructive & Aesthetic Surgery. 2016;69:19–26. doi: 10.1016/j.bjps.2015.11.003. [DOI] [PubMed] [Google Scholar]
- 49.Park JS, Chu JS, Cheng C, et al. Differential effects of equiaxial and uniaxial strain on mesenchymal stem cells. Biotechnol Bioeng. 2004;88(3):359–368. doi: 10.1002/bit.20250. [DOI] [PubMed] [Google Scholar]
- 50.Koike T, Takaoka K, Nihon Rinsho. Stimulation of bone formation. Jpn J Clin Med. 2005;63(Suppl 10):426–430. [PubMed] [Google Scholar]
- 51.Birmingham E, Niebur GL, McHugh PE, et al. Osteogenic differentiation of mesenchymal stem cells is regulated by osteocyte and osteoblast cells in a simplified bone niche. Eur Cell Mater. 2012;12(23):13–27. doi: 10.22203/ecm.v023a02. [DOI] [PubMed] [Google Scholar]