Abstract
Objective
This study evaluated the psychometric properties of the Youth Eating Disorder Examination Questionnaire (YEDE-Q) and its utility for detecting loss of control (LOC) eating (i.e., eating episodes, regardless of size, involving a perceived inability to control what or how much one is eating) among school-age children with overweight or obesity. Identifying eating pathology, particularly LOC eating, in this population may facilitate treatment that improves weight outcomes and reduces eating disorder risk.
Methods
Children with overweight or obesity (N = 241; 7–11y) completed the YEDE-Q and abbreviated Child EDE (ChEDE) to assess LOC eating, prior to entering a weight management treatment trial. Confirmatory factor analyses (CFA) were conducted on children’s YEDE-Q responses and compared to the standard adult EDE-Q factor structure and newer, alternate factor structures.
Results
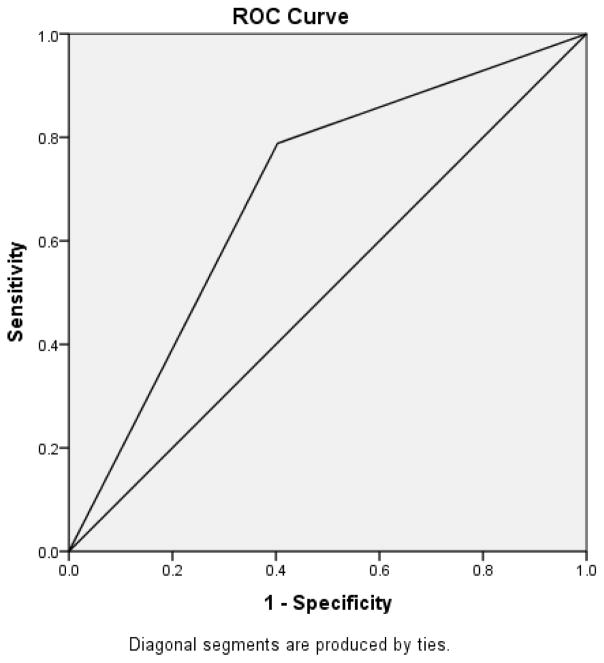
CFA supported a three-factor structure, which distinguished youth with versus without LOC. The YEDE-Q showed low accuracy for detecting LOC eating as measured by the ChEDE, which served as the gold-standard benchmark (AUC = 0.69). Among children who endorsed LOC eating, more episodes per month were reported on the YEDE-Q than ChEDE (p < 0.001).
Conclusions
The YEDE-Q may not have utility as a screener for identifying true cases of LOC eating among school-age children with overweight or obesity. Further evaluation of the YEDE-Q and the alternate three-factor structure is warranted.
Keywords: assessment, eating disorder pathology, loss of control eating, children, overweight
Some children with overweight or obesity experience loss of control (LOC) eating (i.e., eating episodes, regardless of size, involving a perceived inability to control what or how much one is eating).1 LOC eating is associated with elevated disordered eating attitudes and psychosocial impairment,2 predicts excess weight and fat gain over time,3, 4 and predicts development of an eating disorder (ED).5 Detecting LOC eating during childhood may facilitate tailored intervention to improve weight outcomes and reduce ED risk.
The Child Eating Disorder Examination (ChEDE) is a semi-structured interview adapted from the adult EDE6 to assess ED psychopathology, including LOC eating.7 The ChEDE relies on clinician administration, which can be burdensome to clinicians and patients, time-consuming, and requires training to administer with fidelity. An efficient self-report screener to detect LOC eating may enhance the feasibility of identifying youth with ED pathology, which can lead to more precise intervention.
The EDE Questionnaire (EDE-Q)8, 9—developed from the adult EDE to be a self-report measure for adults—has been adapted for youth as the Youth EDE-Q (YEDE-Qa).10, 11 Adaptations comprised modified language for children’s comprehension and added vignettes and pictures describing LOC eating. The interview and questionnaire are matched in terms of item content and scoring (i.e., both measures yield information on behavioral features using frequency data and on severity of psychopathology using four subscales and a global score12), and thus share a common language for assessing ED psychopathology.13, 14 However, meta-analytic results of the adult measures suggest these assessment tools should not be used interchangeably, particularly for assessing binge eating frequency.13
Other measures assess eating-related pathology in youth. The Questionnaire on Eating and Weight Patterns–Adolescent version (QEWP-A) was developed to assess for binge eating disorder (BED).15 However, the QEWP-A has not demonstrated concordance with either the ChEDE among children16 or the YEDE-Q among adolescents10 for assessing binge eating. The YEDE-Q also enables assessment of ED psychopathology beyond the criteria to diagnose BED.
YEDE-Q norms are available for adolescent girls,17 and data from youth ≥10 years old with overweight or obesity suggest the YEDE-Q may be a useful screener for ED pathology.10, 18 However, no study has evaluated the YEDE-Q’s utility for detecting LOC eating among school-aged children as young as 7 years old, despite evidence showing that children experience their first LOC episode, on average, by 8 years old (range=5–13 years).19 Further, no study has evaluated whether EDE-Q factor structures observed in adults and adolescents are similar to the YEDE-Q factor structure among school-age children, an examination of which is warranted given that past evaluations have failed to replicate the EDE-Q’s standard four-factor structure in adults14, 20–25 and adolescents.26 Thus, we examined the YEDE-Q’s psychometric properties and use as a screening tool for LOC eating in treatment-seeking children ages 7–11 years old with overweight or obesity. We hypothesized the YEDE-Q would fail to confirm the standard EDE-Q factor structure but support newer, alternative structures, and would have utility for detecting LOC eating in children.
Methods
Participants
Participants were 241 children (63% female; 65% non-Hispanic White/Caucasian; mean age = 9.9±1.3 years) enrolled in a family-based treatment trial for weight management. At entry, children had a body mass index (BMI; kg/m2) ≥85th percentile for age and sex (M = 97.9±2.5) and at least one parent with overweight or obesity (BMI ≥25). Child BMI percentile and parent BMI were calculated using objectively-measured height and weight.
Children were excluded from the trial if (by self- or parent-report) they had: a) suicidal ideation or a thought disorder, bipolar disorder, substance dependence, or current/past ED; b) an inability to comprehend English ≥1st-grade level; c) a physical disability or illness that precluded moderate physical activity; or d) been taking weight-affecting medications.
Procedure
Participants were recruited from the St. Louis and Seattle areas via advertisements, physician referrals, and word of mouth. Parents completed a telephone screen to assess family eligibility. Potentially eligible families then attended in-person orientation and baseline assessment visits, during which children completed the YEDE-Q and ChEDE. For additional details, see Best et al.27
The study was approved by each site’s Institutional Review Board. Parents and children provided informed consent and assent, respectively.
Measures
The ChEDE7 overeating section was administered to identify objective binge episodes (OBEs; involving an objectively large amount of food and LOC) and subjective binge episodes (SBEs, involving an amount of food not objectively large based on clinical rating but perceived as overeating, accompanied by LOC).
On the same day, children completed the 39-item YEDE-Q.10, 11 Response options for most items are on a Likert-type 0–6 scale; higher scores indicate greater pathology. Nine items had response options on a 1–7 scale, which were recoded 0–6 for consistency with the other items. The measure’s standard factor structure has four subscales—Restraint (5 items), Eating Concern (5 items), Weight Concern (5 items), and Shape Concern (8 items). Separately, the presence and frequency of OBEs and SBEs were assessed.
Analytic Plan
For both measures, LOC eating was calculated as OBEs plus SBEs over the past 28 days, given that the small number of youth endorsing OBEs and SBEs on the ChEDE precluded separate analyses of these behaviors. This sum was then log transformed to reduce skew. Outliers (>3 standard deviations above the mean) were observed for LOC episodes on the ChEDE (n = 4) and YEDEQ (n = 1); however, the presented results include all participants, as the pattern of results was consistent with versus without the outliers.
YEDE-Q internal consistency was calculated using Cronbach’s alpha coefficients and average inter-item correlations (AICs). Internal consistency standard is α ≥0.7028, and AIC values between 0.15–0.50 are considered ideal.29 Confirmatory factor analyses (CFA) were used to test the fit of the standard YEDE-Q four-factor structure, an alternate three-factor structure of the adult EDE-Q identified by Grilo and colleagues among adults with BED or obesity,23, 24 and an alternate four-factor structure of the adult EDE-Q identified by White and colleagues among community-based adolescents.26 Goodness of fit was determined by inspecting the overall model chi-square, comparative fit index (CFI) and Tucker-Lewis Fit Index (TLI) ≥0.95, and root mean square error of approximation (RMSEA) ≤0.60.30
Agreement between the YEDE-Q and the ChEDE for the presence of LOC eating was examined using Pearson chi-square tests, following Goldschmidt and colleagues’ approach.10 Spearman rho correlations and Wilcoxon signed-rank tests were used to examine differences in frequency of LOC episodes assessed by the two measures. Receiver operating characteristic (ROC) analysis was used to test the YEDE-Q compared to ChEDE for detecting cases screening positive for any LOC eating.31 Using YEDE-Q subscales from the model with the best fit, convergent validity for differentiating youth with versus without LOC was evaluated using t-tests.
Analyses were conducted using SPSS v.22, except for the CFA, which were conducted using MPlus version 7. Statistical significance was set at p < .05; all tests were two-tailed.
Results
There was moderate to good internal consistency of the YEDE-Q subscales based on the standard four factors: Restraint (α = 0.68; AIC = 0.29), Eating Concern (α = 0.74; AIC = 0.36), Weight Concern (α = 0.78; AIC = 0.42), and Shape Concern (α = 0.90; AIC = 0.52). However, CFA did not show good fit between the YEDE-Q and the standard four-factor structure (χ2 = 624.43; p < .001; CFI = 0.84; TLI = 0.82; RMSEA = 0.09) or the alternate four-factor structure identified by White and colleagues26 among adolescents (χ2 = 690.66; p < .001; CFI = 0.82; TLI = 0.80; RMSEA = 0.10). The YEDE-Q did show good fit with the alternate three-factor structure identified by Grilo and colleagues23, 24 (χ2 = 14.98; p = .18; CFI = 0.99; TLI = 0.99; RMSEA = 0.04).
A higher proportion of children endorsed the presence of LOC eating on the YEDE-Q (48.7%) than on the ChEDE (21.8%), (χ2 = 24.1; p < 0.001). Forty-one children (17.2%) endorsed LOC eating on both assessments. Using the ChEDE as the referent, the YEDE-Q yielded 75 (31.5%) false positives (i.e., children who reported LOC via questionnaire but not interview) and 11 (4.6%) false negatives (i.e., children who denied LOC via questionnaire but reported LOC on the interview). Children who were false negatives did not differ from the other children in terms of age, sex, BMI z-score, or global YEDE-Q score (p’s > .61). Figure 1 shows results testing the ROC curve; these results suggest the YEDE-Q identifies LOC cases, though with low accuracy.32 Using YEDE-Q subscales from the three-factor structure that had the best fit, youth who endorsed LOC eating on the YEDE-Q had higher subscale scores than did youth who denied LOC eating (Table 1).
FIGURE 1.
Receiver operating characteristic analysis for cases screening positive for loss of control eating on the Youth Eating Disorder Examination Questionnaire compared to the Child Eating Disorder Examination.
Area under the curve = 0.69 (SE = 0.04; Asymptotic 95% CI = 0.62 – 0.77); Asymptotic p < .001
TABLE 1.
Differences in eating disorder pathology between youth who did versus did not endorse LOC eating on the YEDE-Q.
| Factor* | Cronbach’s α | Average Inter-item Correlation | Full Sample, Mean (SD) | Endorsed LOC, Mean (SD) | Did not Endorse LOC, Mean (SD) | Test Statistic and p-value comparing those who did versus did not endorse LOC |
|---|---|---|---|---|---|---|
| Dietary Restraint (3 items) | 0.72 | 0.46 | 2.06 (1.54) | 2.32 (1.46) | 1.80 (1.58) | t(1, 236) = −2.68; p = .008 |
| Shape/Weight Overvaluation (2 items) | 0.84 | 0.72 | 1.92 (1.64) | 2.45 (1.56) | 1.39 (1.56) | t(1, 234) = −5.21; p < .001 |
| Body Dissatisfaction (2 items) | 0.87 | 0.77 | 2.36 (1.95) | 3.09 (1.85) | 1.65 (1.78) | t(1, 236) = −6.12; p < .001 |
Among children who endorsed LOC eating on at least one measure, the mean number of LOC eating episodes was significantly higher on the YEDE-Q versus ChEDE (z = −8.19; p < .001). Among these children, the number of LOC episodes was not significantly correlated between the YEDE-Q and ChEDE (ρ = 0.09; p = .33).
Discussion
This study evaluated the psychometric properties of the YEDE-Q and its utility as a screening tool for LOC eating among children ages 7–11y with overweight or obesity. Consistent with hypotheses, results failed to confirm the standard four-factor EDE-Q structure observed in adults and four-factor structure observed in adolescents;26 rather, results supported the alternate three-factor structure observed by Grilo and colleagues,23, 24 which has shown good fit among adult samples presenting for bariatric surgery24 or presenting with BED (the latter sample had a mean BMI of 37.9).23 The alternate factor structure had good convergent validity for differentiating youth with LOC from those without LOC eating, although reliability values for two of the subscales fell outside of the ideal range. Taken together, this alternate structure may be appropriate for children and adults with a higher weight status and be more efficient to deliver, as it is comprised of 7 items instead of 22; however, further evaluation of this three-factor structure is warranted.
In contrast to hypotheses, the YEDE-Q showed low utility for identifying true cases of LOC eating compared to the ChEDE, and participants reported significantly more LOC eating episodes on the YEDE-Q than on the ChEDE, consistent with research among adolescents and adults.9, 10, 13, 18, 33, 34 The correlation between these measures for LOC eating frequency was low even when limited to children who indicated any LOC on either measure. This low correlation may have resulted from differences in the format and administration procedure. The interview allows assessors to clarify difficult-to-understand items, such as LOC, and uses a calendar guide, which could affect how accurately youth report frequencies. Alternatively, youth may be more willing to endorse LOC eating via self-report, which is private, than to an assessor. By comparison, in studies of older youth, Goldschmidt and colleagues10 found a significant correlation between the YEDE-Q and ChEDE for OBEs but not SBEs (and the YEDE-Q yielded significantly greater frequency ratings than the ChEDE for both OBEs and SBEs), Goossens and Braet18 found no differences between measures in percent endorsing OBEs and SBEs, and Delacuwe and Braet33 did not find a correlation between measures in OBE frequency. Comparison between the ChEDE and QEWP-A has also shown the QEWP-A is not concordant with the ChEDE for assessing binge eating either: only 4.5% of children reported LOC episodes on both the ChEDE and QEWP-A,16 whereas agreement was higher in our sample using the YEDE-Q.
The YEDE-Q yielded more false positives than false negatives for detecting LOC eating; however, false positives are preferable to false negatives on a self-report screener to avoid missing cases. Accordingly, if used as a screener, it may be useful to administer the YEDE-Q followed by a diagnostic assessment (e.g., ChEDE) among those who screen positive. Enhancements to the YEDE-Q, such as embedding vignettes regarding LOC within the overeating section rather than in the initial instructions, may also help the YEDE-Q more precisely identify youth with LOC eating. Additionally, it may be helpful to determine factors that predict concordance and discordance, to enhance our understanding of subpopulations for whom the YEDE-Q might be an effective and accurate screener.
To our knowledge, this is the first evaluation of the YEDE-Q in youth as young as 7 years old. However, a study limitation is that the results may not generalize to non-treatment seeking youth or children with full-syndrome EDs. Additionally, although assessments were ordered with the intent of the YEDE-Q being administered prior to the ChEDE, our data are limited as they do not allow us to confirm whether this administration order was consistently accomplished in practice, thus creating a potential limitation of this study.
Taken together, our findings support a three-factor structure and show that the YEDE-Q detects LOC eating but is not concordant with the ChEDE for identifying true cases of LOC eating in school-age children with overweight or obesity. These results suggest the YEDE-Q may have greater utility as a screener, to indicate whether to administer the ChEDE overeating section to evaluate LOC eating. Further evaluation of the YEDE-Q is warranted to validate the alternate structure in a different sample of youth, including among children with known clinical ED pathology.
Acknowledgments
This work was supported by grants R01 HD036904, T32 HL007456, K24 MH070446, F32 HD089586, T32 HS000078, and KL2 RR024994.
Footnotes
Measure available from corresponding author upon request.
Disclosure of Conflicts
The authors report no conflicts of interest.
References
- 1.Shomaker LB, Tanofsky-Kraff M, Elliott C, et al. Salience of loss of control for pediatric binge episodes: does size really matter? Int J Eat Disord. 2010;43:707–716. doi: 10.1002/eat.20767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tanofsky-Kraff M, Yanovski SZ, Wilfley DE, Marmarosh C, Morgan CM, Yanovski JA. Eating-disordered behaviors, body fat, and psychopathology in overweight and normal-weight children. J Consult Clin Psychol. 2004;72:53–61. doi: 10.1037/0022-006X.72.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tanofsky-Kraff M, Yanovski SZ, Schvey NA, Olsen CH, Gustafson J, Yanovski JA. A prospective study of loss of control eating for body weight gain in children at high risk for adult obesity. Int J Eat Disord. 2009;42:26–30. doi: 10.1002/eat.20580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tanofsky-Kraff M, Cohen ML, Yanovski SZ, et al. A prospective study of psychological predictors of body fat gain among children at high risk for adult obesity. Pediatrics. 2006;117:1203–1209. doi: 10.1542/peds.2005-1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tanofsky-Kraff M, Shomaker LB, Olsen C, et al. A prospective study of pediatric loss of control eating and psychological outcomes. J Abnorm Psychol. 2011;120:108–118. doi: 10.1037/a0021406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fairburn CG, Cooper Z. The Eating Disorder Examination. In: Fairburn CG, Wilson GT, editors. Binge Eating: Nature, Assessment and Treatment. 12. New York: Guilford; 1993. pp. 317–60. [Google Scholar]
- 7.Bryant-Waugh RJ, Cooper PJ, Taylor CL, Lask BD. The use of the eating disorder examination with children: a pilot study. Int J Eat Disord. 1996;19:391–397. doi: 10.1002/(SICI)1098-108X(199605)19:4<391::AID-EAT6>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- 8.Fairburn CG, Beglin SJ. Eating Disorder Examination Questionnaire (EDE-Q 6.0) In: Fairburn CG, editor. Cognitive behavior therapy and eating disorders. New York: Guilford Press; 2008. pp. 309–314. [Google Scholar]
- 9.Fairburn CG, Beglin SJ. Assessment of eating disorders: interview or self-report questionnaire? Int J Eat Disord. 1994;16:363–370. [PubMed] [Google Scholar]
- 10.Goldschmidt AB, Doyle AC, Wilfley DE. Assessment of binge eating in overweight youth using a questionnaire version of the Child Eating Disorder Examination with Instructions. Int J Eat Disord. 2007;40:460–467. doi: 10.1002/eat.20387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goldfein JA, Devlin MJ, Kamenetz C. Eating Disorder Examination-Questionnaire with and without instruction to assess binge eating in patients with binge eating disorder. The Int J Eat Disord. 2005;37:107–111. doi: 10.1002/eat.20075. [DOI] [PubMed] [Google Scholar]
- 12.Fairburn CG, Cooper Z, O’Connor ME. Eating Disorder Examination (Edition 16.0D) In: Fairburn CG, editor. Cognitive Behavior Therapy and Eating Disorders. New York: Guilford Press; 2008. pp. 265–308. [Google Scholar]
- 13.Berg KC, Peterson CB, Frazier P, Crow SJ. Convergence of scores on the interview and questionnaire versions of the Eating Disorder Examination: a meta-analytic review. Psychol Assess. 2011;23:714–724. doi: 10.1037/a0023246. doi:710.1037/a0023246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Berg KC, Peterson CB, Frazier P, Crow SJ. Psychometric evaluation of the eating disorder examination and eating disorder examination-questionnaire: a systematic review of the literature. Int J Eat Disord. 2012;45:428–438. doi: 10.1002/eat.20931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Johnson WG, Grieve FG, Adams CD, Sandy J. Measuring binge eating in adolescents: adolescent and parent versions of the questionnaire of eating and weight patterns. Int J Eat Disord. 1999;26:301–314. doi: 10.1002/(sici)1098-108x(199911)26:3<301::aid-eat8>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 16.Tanofsky-Kraff M, Morgan CM, Yanovski SZ, Marmarosh C, Wilfley DE, Yanovski JA. Comparison of assessments of children’s eating-disordered behaviors by interview and questionnaire. Int J Eat Disord. 2003;33:213–224. doi: 10.1002/eat.10128. [DOI] [PubMed] [Google Scholar]
- 17.Carter JC, Stewart DA, Fairburn CG. Eating disorder examination questionnaire: norms for young adolescent girls. Behav Res Ther. 2001;39:625–632. doi: 10.1016/s0005-7967(00)00033-4. [DOI] [PubMed] [Google Scholar]
- 18.Goossens L, Braet C. Screening for eating pathology in the pediatric field. Int J Pediatr Obes. 2010;5:483–490. doi: 10.3109/17477160903571995. [DOI] [PubMed] [Google Scholar]
- 19.Tanofsky-Kraff M, Faden D, Yanovski SZ, Wilfley DE, Yanovski JA. The perceived onset of dieting and loss of control eating behaviors in overweight children. Int J Eat Disord. 2005;38:112–122. doi: 10.1002/eat.20158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Peterson CB, Crosby RD, Wonderlich SA, et al. Psychometric properties of the eating disorder examination-questionnaire: factor structure and internal consistency. Int J Eat Disord. 2007;40:386–389. doi: 10.1002/eat.20373. [DOI] [PubMed] [Google Scholar]
- 21.Hrabosky JI, White MA, Masheb RM, Rothschild BS, Burke-Martindale CH, Grilo CM. Psychometric evaluation of the eating disorder examination-questionnaire for bariatric surgery candidates. Obesity. 2008;16:763–769. doi: 10.1038/oby.2008.3. doi:710.1038/oby.2008.1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Allen KL, Byrne SM, Lampard A, Watson H, Fursland A. Confirmatory factor analysis of the Eating Disorder Examination-Questionnaire (EDE-Q) Eat Behav. 2011;12:143–151. doi: 10.1016/j.eatbeh.2011.01.005. [DOI] [PubMed] [Google Scholar]
- 23.Grilo CM, Crosby RD, Peterson CB, et al. Factor structure of the eating disorder examination interview in patients with binge-eating disorder. Obesity. 2010;18:977–981. doi: 10.1038/oby.2009.321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Grilo CM, Henderson KE, Bell RL, Crosby RD. Eating disorder examination-questionnaire factor structure and construct validity in bariatric surgery candidates. Obes Surg. 2013;23:657–662. doi: 10.1007/s11695-012-0840-8. doi:610.1007/s11695-11012-10840-11698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Grilo CM, Reas DL, Hopwood CJ, Crosby RD. Factor structure and construct validity of the Eating Disorder Examination-Questionnaire in college students: further support for a modified brief version. Int J Eat Disord. 2015;48:284–289. doi: 10.1002/eat.22358. doi:210.1002/eat.22358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.White HJ, Haycraft E, Goodwin H, Meyer C. Eating disorder examination questionnaire: factor structure for adolescent girls and boys. Int J Eat Disord. 2014;47:99–104. doi: 10.1002/eat.22199. doi:110.1002/eat.22199. [DOI] [PubMed] [Google Scholar]
- 27.Best JR, Theim KR, Gredysa DM, et al. Behavioral economic predictors of overweight children’s weight loss. J Consult Clin Psychol. 2012;80:1086–1096. doi: 10.1037/a0029827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nunnally JC. Psychometric Theory. New York: McGraw-Hill; 1978. [Google Scholar]
- 29.Clark LA, Watson D. Constructing validity: Basic issues in objective scale development. Psychol Assess. 1995;7:309–319. [Google Scholar]
- 30.Hu L-t, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal. 1999;6:1–55. [Google Scholar]
- 31.McFall RM, Treat TA. Quantifying the information value of clinical assessments with signal detection theory. Annu Rev Psychol. 1999;50:215–241. doi: 10.1146/annurev.psych.50.1.215. [DOI] [PubMed] [Google Scholar]
- 32.Streiner DL, Cairney J. What’s under the ROC? An introduction to receiver operating characteristics curves. Can J Psychiatry. 2007;52:121–128. doi: 10.1177/070674370705200210. [DOI] [PubMed] [Google Scholar]
- 33.Decaluwe V, Braet C. Assessment of eating disorder psychopathology in obese children and adolescents: interview versus self-report questionnaire. Behav Res Ther. 2004;42:799–811. doi: 10.1016/j.brat.2003.07.008. [DOI] [PubMed] [Google Scholar]
- 34.Wilfley DE, Schwartz MB, Spurrell EB, Fairburn CG. Assessing the specific psychopathology of binge eating disorder patients: interview or self-report? Behav Res Ther. 1997;35:1151–1159. [PubMed] [Google Scholar]