Abstract
Introduction
Hookahs (water pipes) are rapidly increasing in popularity worldwide. Evidence suggests that although perceived as safer than cigarette smoke, hookah smoke may be as, or even more, dangerous as cigarette smoke.
Methods
Air samples from 33 homes—11 where only hookah-smoking occurred, 12 with only cigarettes and 10 with no smoking—were collected to analyse concentrations of particulate matter (PM2.5), black carbon, elemental and organic carbon and carbon monoxide (CO). Air quality was assessed in rooms where smoking occurred and in an adjacent room.
Results
Hookah and cigarette smoking impaired home air quality. The rooms in which hookahs were smoked showed the highest concentrations for all pollutants. CO was significantly greater in the rooms where hookahs were smoked than in the cigarette-smoking rooms and the non-smoking households (p<0.05). In addition, CO levels in the rooms adjacent to where hookah was smoked were 2.5-fold to 4-fold greater than those in the smoking and non-smoking rooms of the cigarette homes (p<0.05). PM2.5 levels were also elevated in hookah homes compared to cigarette and non-smoking homes, although not significantly different.
Conclusions
This study, the first of its kind, demonstrates potentially hazardous levels of home air pollution in rooms where hookahs are being smoked as well as in adjacent rooms. These levels were greater than those in cigarette smoking homes, raising concerns about potential negative health effects on all individuals living in homes where hookahs are smoked.
INTRODUCTION
Although cigarette use has dramatically declined globally, there has been a recent, rapid upturn in the use of other forms of tobacco.1 From 2000 to 2011, cigarette consumption in the USA has declined 33%, but the drop in cigarette use is being offset by the marked increase in the consumption of alternative tobacco products, including cigars, cigarillos, smokeless tobacco and hookah.2,3 A recent review suggests that hookah (also called water pipe, hubble-bubble or narghile) use may be the ‘second global tobacco epidemic since the cigarette’.4 The National Youth Tobacco Survey reported that in 2011, 8% of male and 5% of female middle school and high school students in the USA ever used hookah, but by 2014, these rates had more than doubled to 14% for boys and almost tripled to 15% for girls.5 In 2015, 25% of male and 22% of female college students in the USA reported ever used hookah.6 Among young adults, almost one in four have used hookah.7
Secondhand smoke (SHS) from cigarettes includes more than 7000 toxic chemicals that kill more than 600 000 non-smokers globally each year.8 In addition to the adult mortality and morbidity that is widely recognised, it is well known that SHS is responsible for causing an increased risk of ear infections, respiratory infections, asthma attacks and sudden infant death syndrome, as well as a myriad of other health problems among children, such as increased risks of attention deficit hyperactivity disorder and the metabolic syndrome.9 WHO estimates that 700 million or half of the world’s children may be exposed to SHS, especially in homes.10 The 2011–2012 National Health and Nutrition Examination Survey found that 41% of children aged 3–11 years were exposed to SHS.2 Among non-smoking adults, more than 20% reported SHS exposure in their workplace.11 To date, SHS has largely been investigated and thought to arise mainly from cigarette smoke, and there is very limited research on hookah smoking as a source of SHS, even though hookah smoking has already been associated with an increased risk of lung cancer,12 periodontal disease,13 respiratory disease,14 and low birthweight in infants15 and the sharing of hookahs can spread infectious diseases, such as hepatitis C, tuberculosis and herpes.16,17
Hookah use is widely perceived to be a safer alternative to cigarettes because the smoke is filtered through water,18,19 but growing evidence indicates that actively smoking hookahs may be as or more harmful than smoking cigarettes.20–22 Moreover, a number of studies have found that SHS from hookah use contains high concentrations of particulate matter (PM2.5).23,24 Studies measuring the indoor air quality of hookah bars have shown PM2.5 and carbon monoxide (CO) concentrations ranging from ‘unhealthy’ to ‘hazardous’ according to Environmental Protection Agency (EPA) standards for outdoor air pollution, but these studies have focused on commercial hookah bars, despite widespread home use of these devices.25–30 It is likely that many hookah smokers smoke at home, and that this is the most likely place where children and other non-hookah smokers are exposed to hookah-related SHS. To date, however, there is only one study that we are aware of that has assessed air quality in the homes of hookah smokers,31 demonstrating nicotine in the air and on surfaces, as well as biological evidence of children’s exposure. No other measures of air quality in homes of hookah smokers have been assessed.
We report the results of a study that assessed indoor air quality in homes where hookahs were smoked and compared the air quality in these homes to that in homes where cigarettes but not hookahs were smoked, and in homes where no smoking (hookah or cigarettes) occurred. To assess the air quality in homes where hookah or cigarettes were smoked, multiple measures of air pollution were examined in this study. The primary measurements were airborne particles <2.5 μm in aerodynamic diameter (PM2.5) and CO. Both pollutants are associated with adverse health effects and are of major concern in the SHS produced by hookahs.21,23,30
METHODS
Participants
A convenience sample of 33 homes, in Dubai, the United Arab Emirates (UAE), was recruited to participate in the study of the air quality in their homes; 11 homes where only hookah was smoked, 12 homes where only cigarettes were smoked and 10 homes where neither hookahs nor cigarettes were smoked. Research field staff were trained by two of the investigators (TG and MW) in collection of air samples to assess: PM2.5, black carbon (BC), organic and elemental carbon (OC/EC) and CO. Air quality was measured in the room where smoking occurred and in one adjacent non-smoking room in homes where hookahs or cigarettes were smoked. In non-smoking homes, air sampling was conducted in the bedroom and living room and the values were averaged.
Inclusion criteria was restricted to the customary use of hookahs or cigarettes at home or the use of no tobacco product in the home, and the use of a single smoking product at a time during the sampling period (ie, hookah or cigarettes). The length of smoking time, the number of smokers, the number of children in households, number of hookahs or cigarettes smoked, ventilation during smoking sessions, sampling time, as well as the size of the room where smoking occurred during air quality assessment are shown in table 1. Informed consent was received from one adult in each participating household after the study was approved by the New York University School of Medicine and by the Dubai Health Authority’s Institutional Review Boards.
Table 1.
Characteristics of sampled rooms
| Number of homes | Active smokers during session, mean (range) | Number of products smoked*, mean (range) | Ventilation during session | Sampling time (min), mean (range) | Number of children in household, mean | Area of room (m2), mean (range) |
|---|---|---|---|---|---|---|
| Hookah smoking homes | ||||||
| 11 | 1.7 (1–4) | 1.1 (1–2) | 5 Open windows 3 AC on 3 Incense† |
68.4 (58–89) | 0.6 | 22.7 (7–38) |
| Cigarette smoking homes | ||||||
| 12 | 2.3 (1–5) | 6.3 (1–14) | 6 Open windows 1 AC on 3 Incense† |
74.3 (62–95) | 0.9 | 20.5 (4–60) |
| Non-smoking homes | ||||||
| 10 | NA | NA | 2 Open windows 3 AC on 1 Incense† |
71.0 (60–125) | 1.1 | 40.7 (12–160) |
In hookah smoking homes, this was the number of water pipes smoked and, in cigarette smoking homes, the number of cigarettes smoked.
Incense use reported in the home, but not during the smoking sessions.
AC, air conditioning; NA, not applicable.
Sample collection
In each home, research staff operated pre-calibrated monitoring equipment with personal environmental monitors (PEM) (SKC; Eighty Four, Pennsylvania, USA) to collect total PM2.5 gravimetric samples on polytetrafluoroethylene (PTFE) filters (Pall Corp, Port Washington, New York, USA) at 10 L/min using Legacy pumps (SKC). Airborne OC/EC levels were collected on pre-baked (650°C overnight) quartz (Pall) filters and PEMs that operated at a sample flow rate of 10 L/min. After collection, quartz filters were sealed and transferred to a −20°C freezer. A dry gas meter (BIOS Dry Cal DC-Lite, Brandt Instruments, Prairieville, Louisiana, USA) was used before each run to calibrate sample flow rates. Continuously logging microaethalometers (Model AE51 with a PM2.5 inlet, AethLabs, San Francisco, California, USA), CO data loggers (0–300 ppm, EL-USB-CO, Lascar, Erie, Pennsylvania, USA), and pressure-compensated and humidity-compensated aerosol monitors (pDR-1500 with a PM2.5 inlet, resolution of 1 μg/m3, Thermo Fisher Scientific, Pittsburgh, Pennsylvania, USA) were used to monitor real time BC (1 min intervals), CO, and PM2.5 (1 min intervals), respectively.
During a 60–75 min hookah smoking session within each study home where hookah was smoked, the research team collected air samples in the room where hookah was smoked and simultaneously in an adjacent room within the house. In cigarette-only homes, cigarettes were smoked for 60–85 min with a range of 1–14 cigarettes smoked by 1–4 people in each home. Similar sampling times were conducted in homes where no smoking occurred.
Chemical analysis
Gravimetric analysis of PTFE filters were performed in an environmentally controlled weighing facility (22°±1°C and 40% ±1% relative humidity) using established operating procedures. Filters were equilibrated to ambient conditions in the weighing facility for a minimum of 24 hours before measurement, degaussed and weighed repeatedly until the mass values agreed within 5 μg. The mass concentrations of EC and OC were measured from the quartz filters using the Lab OCEC Aerosol Analyzer following the NIOSH (2003) method 5040 (Sunset Instruments, Hillsborough, North Carolina, USA).
Statistical analysis
The collected data were categorised into five groups: hookah-smoking rooms, rooms adjacent to where hookah was smoked, cigarette smoking rooms, rooms adjacent to where cigarettes were smoked and homes where there was neither hookah nor cigarette smoking. Statistical analyses were performed using Stata 14.0 (StataCorp, College Station, Texas, USA). Data were summarised with descriptive statistics (mean, range and 95% CIs). All outcome variables, that is, PM 2.5, BC and CO, were log-transformed to perform t-tests because they were not normally distributed as assessed by the Shapiro-Wilk test. Spearman’s rank correlation coefficient was used to apprise the correlation between PM2.5 levels and CO levels, the area of the smoking room, the number of active smokers and the number of hookahs or cigarettes smoked. A p value of ≤0.05 was considered statistically significant for all analyses.
RESULTS
As noted, table 1 illustrates the number of smokers, the number of children in households, the number of hookahs or cigarettes smoked, ventilation during smoking sessions, sampling time, as well as the size of the room where smoking occurred during air quality assessment.
PM2.5, BC and CO levels were consistently higher in the hookah/cigarette smoking rooms compared to the adjacent non-smoking rooms (table 2). The levels of these pollutants were also greater than the values in the non-smoking homes.
Table 2.
Comparison of mean level (95% CI) of pollutants by room and home type
| Home type | Room type | PM2.5 gravimetric samples (μg/m3) | BC (μg/m3) | CO (ppm) |
|---|---|---|---|---|
| Hookah | Smoking | 428.6 (50.3 to 806.9)*,†,‡ | 5.4 (1.9 to 8.9)‡ | 11.0 (8.2, 13.7)*,†,‡ |
| Hookah | Non-smoking | 210.8 (78.4 to 343.2)§ | 3.7 (1.7 to 5.8) | 5.8 (2.1 to 13.0)†,§,¶ |
| Cigarette | Smoking | 201.2 (101.3 to 301.1)** | 4.2 (2.2 to 6.2)** | 2.3 (1.6 to 3.0)‡,**,†† |
| Cigarette | Non-smoking | 96.7 (45.5 to 147.9) | 3.0 (1.5 to 4.6) | 1.6 (1.0 to 2.2)§ |
| Non-smoking | – | 93.2 (66.2 to 120.1) | 2.1 (1.4 to 2.9) | 1.5 (0.5 to 1.9) |
| Regulatory standard‡‡ | – | 35 | – | 9 |
t-test was conducted after log-transformation of pollutant levels.
Hookah smoking versus hookah non-smoking (p<0.05).
Hookah/cigarette non-smoking versus cigarette/hookah smoking (p<0.05).
Hookah/cigarette smoking versus non-smoking home (p<0.05).
Hookah/cigarette non-smoking versus non-smoking home (p<0.05).
Hookah non-smoking versus cigarette non-smoking (p<0.05).
Cigarette smoking versus cigarette non-smoking (p<0.05).
Hookah smoking versus cigarette smoking (p<0.05).
The regulatory standard for PM2.5 and CO are the U.S. EPA’s 24hour and 8 hour standards, respectively. There is no regulatory level for BC.
BC, black carbon; CO, carbon monoxide; PM, particulate matter <2.5 μm.
When comparing pollutant levels from smoking rooms in hookah homes with smoking rooms in cigarettes homes, levels of CO were found to be significantly higher in the hookah smoking rooms. In rooms where hookahs were smoked and their adjacent non-smoking rooms, CO levels (table 2) were 4.8 and 3.6 times greater (11.0 vs 2.3 ppm, and 5.8 vs 1.6 ppm), respectively, than in rooms where cigarettes were smoked and their adjacent non-smoking rooms (p<0.05). They were also 7.3 and 3.9 times greater (11.0 vs 1.5 ppm and 5.8 vs 1.5 ppm), respectively, than CO levels in rooms in non-smoking homes (p<0.05). Importantly, the mean level of CO in the non-smoking rooms in the hookah homes, 5.8 ppm, was more than twice as high as in the smoking rooms from cigarette homes, 2.3 ppm (p<0.05).
PM2.5 levels in the hookah smoking rooms varied widely among homes (95% CI 50.3 to 806.9 mg/m3, table 1); the mean value was more than twice the PM2.5 levels in the cigarette smoking rooms although this difference was not statistically significant. PM2.5 levels in the cigarette smoking rooms were elevated above the levels in the adjacent rooms (201.2 vs 96.7, p<0.05) while not being elevated compared to levels in non-smoking homes. In contrast, PM 2.5 levels in hookah smoking rooms were significantly higher than those in non-smoking homes (428.6 vs 91.2, p<0.05).
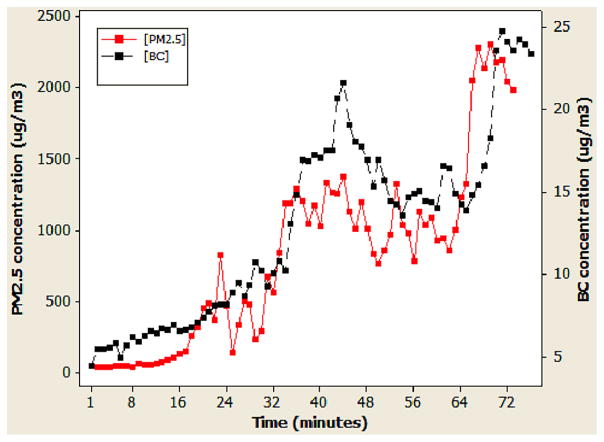
BC levels in hookah smoking rooms were not statistically different than adjacent rooms (5.4 vs 3.7). The levels of BC in the cigarette smoking room were higher than the levels in the adjacent room (4.2 vs 3.0, p<0.05). Compared to the non-smoking homes, (1.5 ppm), BC levels were elevated in the smoking and adjacent rooms of the cigarette homes, but did not reach statistical significance (2.3 ppm for cigarette smoking rooms and 1.6 ppm for cigarette adjacent rooms, p<0.05). Mean BC concentrations were 2.5 times greater in hookah smoking rooms than in rooms in non-smoking homes (p<0.05). As seen in the hookah smoking room with the highest PM2.5 levels (figure 1), the baseline values were low, suggesting that other smoking products were not in use; this finding was consistent with other homes where hookahs were smoked. The observed increase in real-time PM2.5 and BC concentrations varied greatly, but in parallel, over time. Although the composition of the airborne PM2.5 was not extensively assessed in this study, the measurement of OC and EC levels suggest that EC made up a minor fraction of PM2.5, whereas OC accounted for 66% and 88% of the PM2.5 mass in the hookah and cigarette smoking homes, respectively.
Figure 1.
Real-time levels of PM2.5 and black carbon in one hookah smoking room. BC, black carbon; PM2.5, particulate matter <2.5 μm.
Several individual home characteristics were evaluated for their effect on airborne PM2.5 levels in the smoking room of the hookah and cigarette homes. The room area, number of active smokers and number of hookahs simultaneously smoked were not significantly correlated with the PM2.5 levels in the hookah homes and only the number of smoked cigarettes were correlated with PM2.5 in the cigarette homes.
DISCUSSION
The growing epidemic of hookah use is not exclusively nor primarily a US problem. It is a global problem, primarily emanating from the Middle East,4 and as a result, countries like the UAE have enacted a number of laws concerning tobacco use and hookah use in the past decade.32 Virtually all that we know to date about air quality and health effects of hookah use and exposure to hookah-related SHS, however, comes from studies conducted in settings other than homes where hookah is smoked.20,25,29,30 This is the first study that we are aware of that investigates multiple air pollutants in homes where hookahs are smoked, demonstrating potentially hazardously high levels of all pollutants assessed in rooms where hookah was smoked and in the adjacent rooms. Levels of these pollutants were higher in homes where hookah was smoked than in homes where cigarettes were smoked and levels of CO in the room adjacent to the one where hookah was smoked were even higher than in rooms where cigarettes were smoked.
PM2.5 levels in homes where nothing was smoked were markedly higher than the WHO’s 24 hour guideline of 25 μg/m3 for outdoor air pollution, consistent with findings of poor air quality in homes and in the ambient environment in Dubai in general.33 Burning incense is common in the UAE and can be a source of indoor PM;34 however, it should be noted that although ~1/3 to 1/2 of the hookah and cigarette homes in this study reported the occasional, weekly or monthly use of incense, none was burned during this study. Concentrations of PM2.5 and BC in hookah smoking homes were higher than those found in cigarette-smoking and non-smoking homes, suggesting that in-home hookah smoking may pose similar or even worse cardiovascular and pulmonary risks to non-smokers living in such homes than SHS in homes where cigarettes are smoked. Toxicity of ambient particles depends, of course, on the composition of inhaled particles. Our analyses determined that the majority of PM2.5 in the hookah and cigarette homes was comprised of OC, whereas EC or BC made up only a small fraction of the total PM2.5. Thus, additional research is needed to assess the composition of secondhand hookah smoke when comparing its toxicity to that for secondhand cigarette smoke.
The WHO recommends that indoor CO levels not exceed 9 ppm for 8 hours or 26 ppm for 1 hour.35 None of the sampled rooms demonstrated mean CO levels above the 1 hour guidance level. The present study demonstrates that hookah and cigarette smoke elevate indoor CO levels, but significantly more so with hookah smoke, resulting in CO levels several folds greater than the cigarette smoke and control concentrations. CO has been implicated to play a major role in a multitude of cardiovascular and airway diseases, including atherosclerosis,36,37 cardiomyopathy,38 chronic obstructive pulmonary disease,39 respiratory infections,40 asthma41 and cystic fibrosis.42 CO poisoning after hookah smoking has already been found in a number of case reports, with users presenting carboxyhaemoglobin levels 34% higher than normal after hookah use,43,44 syncope45 and confusion.46 It has been suggested that CO intoxication due to hookah smoking is likely to be more common than that was realised due to inefficient charcoal burning.30,47 These findings suggest that the substitution of the burning charcoal with an electronic heating source may be beneficial in reducing CO levels during the use of hookahs.
The well-documented adverse health effects of cigarette SHS have been translated into extensive public health policy to protect non-smokers. As a result, 84% of adults11 and 75% teenagers48 recognise that SHS from cigarettes is harmful and believe that non-smokers should be protected from such exposure. However, comparable awareness and beliefs regarding SHS from hookah are severely lacking.49,50 Owing to the lack of data concerning the dangers of SHS from hookah, the findings reported here, if corroborated and effectively communicated to the public, may significantly decrease hookah smoking in homes.
For the most part, the dangers and prevalence of hookah smoking in homes have been unexplored, and it is likely that homes are the most common place where children are exposed to SHS from hookahs. In one study, children living in homes with hookah use were 12% more likely to report wheezing and nasal congestion.14 Another study found that children living in homes of hookah smokers are at risk of exposure to nicotine and 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone, a tobacco-specific carcinogen.31 Thus, these studies and the current study demonstrate that the air quality is poor inside homes where hookahs have been used and that adverse health effects, similar to those seen in children exposed to cigarette SHS, are likely to occur.
Hookah smokers appear to generally smoke hookah in their homes although there is admittedly only a few studies on this and on the extent and dangers of home hookah use. Among college students at one university, 78% of hookah smokers surveyed reported smoking hookah in their homes, whereas at a different university, 43% reported that the home was their primary location for smoking hookah.19,50 The present study provides data that all children and adults in a hookah-smoking household are exposed to hazardous levels of CO and PM2.5. Prior studies have shown that SHS can transfer between units in a multiunit housing building51,52 via open windows, doors and vents, exposing unaware non-smokers. Thus, it would be prudent that emerging multiunit housing smoke-free policies should also be extended to hookah smoking.
In comparison to cigarette smoking homes and consistent with previous studies,26 the rooms where hookah is smoked and the adjacent rooms exhibited higher concentrations of CO, PM2.5 and BC than cigarette-smoking homes and control homes. Interestingly, air quality levels in the smoking rooms and adjacent rooms in hookah-smoking homes were found to be similar with those of hookah bars with multiple smokers and little to no ventilation.25,30
There are a number of limitations to the present study. The study was limited by a small sample size and the use of a convenience sample, thus limiting generalisability. Air collection was initiated just prior to smoking so the temporal change in PM2.5 and BC was able to be captured (figure 1), although air sampling was not conducted for a long term after termination of smoking, leaving unanswered how long the indoor air quality stayed at dangerous levels and what concentration of pollutants continued to contaminate the adjacent rooms. Given that the baseline values for PM2.5 and BC were very low compared to the rapid rise after smoking was initiated (figure 1) suggests that any potential carryover from prior use of smoking products would have had minimal effect on the results of this study. Future studies should measure, in real time, pollutant and nicotine levels prior to and after smoking as well as integrative sampling to evaluate daily total exposures to secondhand hookah smoke in the home.
Importantly, hookah smokers usually smoke less frequently per day in comparison to cigarette smokers but for a longer time period per smoking session53 and it is unclear how this difference in smoking patterns affects the accumulation and dissipation of pollutants in hookah SHS. Additional factors that may have affected the observed inter-home variability in indoor air quality include ventilation factors, such as windows, doors and air conditioning, the types of cigarette, shisha and charcoal being used, air exchange rate, the size of the rooms and the amount of time smoking occurred, although such factors were not correlated with airborne PM2.5 levels in the hookah smoking homes in the present study. Future efforts are needed with larger sample sizes and controlled hookah and cigarette products. Furthermore, these data are limited to one region of the world and because shisha and hookah smoking protocols are not yet standardised, more research is needed to determine whether the above results are generalisable to hookah used in other areas of the world.
To the best of our knowledge, however, this is the first study to assess the indoor air quality of hookah smoking homes in comparison to cigarette smoking homes and non-smoking homes. The findings provide evidence that hookah smoking generates levels of SHS that are potentially hazardous to the health of others in their homes, and particularly pose potentially serious threats to children’s long-term health. Given the UAE’s current attention to Clean Air Acts and tobacco regulation, a paper such as this, demonstrating the danger of indoor hooking smoking, conducted in the country, is likely to have a marked effect. The US Surgeon General concluded that no safe level of SHS exists and the home is the primary source of SHS exposure for children and non-smokers.9,52 Eliminating smoking in indoor spaces is the only effective way to fully protect non-smokers from the effects of SHS exposure. Given the results presented here coupled with the more extensive literature demonstrating remarkably poor air quality in hookah bars, it seems judicious for public health efforts, regulatory and educational, to include home hookah smoking as a danger not only to the hookah smoker but also to others passively exposed to the combustion products of hookah smoke regardless of whether they actually go into the room where hookah is smoked.
What this paper adds.
This study is the first of its kind to demonstrate potentially hazardous levels of home air pollution in rooms where hookahs are being smoked as well as in adjacent rooms. These levels were greater than those in cigarette smoking homes, raising concerns about potential negative health effects on all individuals living in homes where hookahs are smoked. It seems judicious for public health efforts, regulatory and educational, to include home hookah smoking as a danger not only to the hookah smoker but also to others passively exposed to the combustion products of hookah smoke regardless of whether they actually go into the room where hookah is smoked.
Acknowledgments
The authors are also grateful for the technical support from Dr Eric Saunders, Aisha Siddiqui, Ali Alaauddin Shaikh, Haider Iqbal, Noof Rashid Muhammad Ali Al Shirawi, Nujood Rashid Muhammad Ali Al Shirawi, Madiha Hamdi Saif Abdelmotagali, Magdi Khalaf Said Fergani, Maryam Al Saud, Roaa Al-Shams Adnan Baroud, Sadia Furhad, Saubia Fathima and Sidiqa Rafi.
Funding This research was supported in part by the NYU/Abu Dhabi Public Health Research Center (MW, TG and SS), NIH/NIDA 1K24DA038345 (SS), NIH/NIEHS 5 P30 ES000260–49 (TG), and NIH/NCI 3 P30 CA016087–33S1 (TG and MW).
Footnotes
Contributors MW, SS, TG, AHY, FB, RP are responsible for conception, design, analysis and interpretation of data. LL and SG drafted the article. ZH, SHP, AN and MJRV conducted statistical analysis of data. JS revised the manuscript critically for important intellectual content. All authors read and approved the final draft of the manuscript.
Competing interests None declared.
Patient consent Obtained.
Ethics approval Dubai Health Authority’s Institutional Review Boards.
Provenance and peer review Not commissioned; externally peer reviewed.
References
- 1.Samet JM. Tobacco smoking: the leading cause of preventable disease worldwide. Thorac Surg Clin. 2013;23:103–12. doi: 10.1016/j.thorsurg.2013.01.009. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention (CDC) Disparities in nonsmokers’ exposure to secondhand smoke—United States, 1999–2012. MMWR Morb Mortal Wkly Rep. 2012;64:103–8. [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention (CDC) Drop in cigarette consumption offset by increases in other forms of smoked tobacco. 2012 http://www.cdc.gov/mediareleases/2012/p0802_tobacco_consumption.html.
- 4.Maziak W. The global epidemic of waterpipe smoking. Addict Behav. 2011;36:1–5. doi: 10.1016/j.addbeh.2010.08.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Amrock SM, Gordon T, Zelikoff JT, et al. Hookah use among adolescents in the United States: results of a national survey. Nicotine Tob Res. 2014;16:231–7. doi: 10.1093/ntr/ntt160. [published Online First: Epub Date]|. [DOI] [PubMed] [Google Scholar]
- 6.American College Health Association. American College Health Association-National College Health Assessment II: Reference Group Executive Summary. Hanover, MD: American College Health Association; Spring. 2015. [Google Scholar]
- 7.Villanti AC, Cobb CO, Cohn AM, et al. Correlates of hookah use and predictors of hookah trial in U.S. young adults. Am J Prev Med. 2015;48:742–6. doi: 10.1016/j.amepre.2015.01.010. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention (US); National Center for Chronic Disease Prevention and Health Promotion (US); Office on Smoking and Health (US) How tobacco smoke causes disease: the biology and behavioral basis for smoking-attributable disease: a report of the surgeon general. Atlanta (GA): Centers for Disease Control and Prevention (US); 2010. Publications and Reports of the Surgeon General. [PubMed] [Google Scholar]
- 9.Office on Smoking and Health. The Health Consequences of Involuntary Exposure to Tobacco Smoke: a Report of the Surgeon General. Atlanta (GA): Centers for Disease Control and Prevention (US); 2006. Publications and Reports of the Surgeon General. [PubMed] [Google Scholar]
- 10.World Health Organization (WHO) Tobacco. Fact Sheet No 339. 2013 http://www.who.int/mediacentre/factsheets/fs339/en/
- 11.King BA, Homa DM, Dube SR, et al. Exposure to secondhand smoke and attitudes toward smoke-free workplaces among employed U.S. adults: findings from The National Adult Tobacco Survey. Nicotine Tob Res. 2014;16:1307–18. doi: 10.1093/ntr/ntu069. [published Online First: Epub Date] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kadhum M, Sweidan A, Jaffery AE, et al. A review of the health effects of smoking shisha. Clin Med (Lond) 2015;15:263–6. doi: 10.7861/clinmedicine.15-3-263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.El-Zaatari ZM, Chami HA, Zaatari GS. Health effects associated with waterpipe smoking. Tob Control. 2015;24(Suppl 1):i31–43. doi: 10.1136/tobaccocontrol-2014-051908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tamim H, Musharrafieh U, El Roueiheb Z, et al. Exposure of children to environmental tobacco smoke (ETS) and its association with respiratory ailments. J Asthma. 2003;40:571–6. doi: 10.1081/jas-120019029. [DOI] [PubMed] [Google Scholar]
- 15.Akl EA, Gaddam S, Gunukula SK, et al. The effects of waterpipe tobacco smoking on health outcomes: a systematic review. Int J Epidemiol. 2010;39:834–57. doi: 10.1093/ije/dyq002. [DOI] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention (CDC) Tobacco product use among middle and high school students: United States, 2011 and 2012. MMWR Morb Mortal Wkly Rep. 2013;62:893–7. [PMC free article] [PubMed] [Google Scholar]
- 17.Blachman-Braun R, Del Mazo-Rodriguez RL, Lopez-Samano G, et al. Hookah, is it really harmless? Respir Med. 2014;108:661–7. doi: 10.1016/j.rmed.2014.01.013. [DOI] [PubMed] [Google Scholar]
- 18.Rankin KV. Hookah smoking: a popular alternative to cigarettes. Tex Dent J. 2011;128:441–5. [PubMed] [Google Scholar]
- 19.Heinz AJ, Giedgowd GE, Crane NA, et al. A comprehensive examination of hookah smoking in college students: use patterns and contexts, social norms and attitudes, harm perception, psychological correlates and co-occurring substance use. Addict Behav. 2013;38:2751–60. doi: 10.1016/j.addbeh.2013.07.009. [DOI] [PubMed] [Google Scholar]
- 20.Cobb C, Ward KD, Maziak W, et al. Waterpipe tobacco smoking: an emerging health crisis in the United States. Am J Health Behav. 2010;34:275–85. doi: 10.5993/ajhb.34.3.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Daher N, Saleh R, Jaroudi E, et al. Comparison of carcinogen, carbon monoxide, and ultrafine particle emissions from narghile waterpipe and cigarette smoking: Sidestream smoke measurements and assessment of second-hand smoke emission factors. Atmos Environ (1994) 2010;44:8–14. doi: 10.1016/j.atmosenv.2009.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Noonan D, Kulbok PA. New tobacco trends: waterpipe (hookah) smoking and implications for healthcare providers. J Am Acad Nurse Pract. 2009;21:258–60. doi: 10.1111/j.1745-7599.2009.00402.x. [DOI] [PubMed] [Google Scholar]
- 23.Kumar SR, Davies S, Weitzman M, et al. A review of air quality, biological indicators and health effects of second-hand waterpipe smoke exposure. Tob Control. 2015;24(Suppl 1):i54–9. doi: 10.1136/tobaccocontrol-2014-052038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chaouachi K. Hookah (Shisha, Narghile) Smoking and Environmental Tobacco Smoke (ETS). A critical review of the relevant literature and the public health consequences. Int J Environ Res Public Health. 2009;6:798–843. doi: 10.3390/ijerph6020798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fiala SC, Morris DS, Pawlak RL. Measuring indoor air quality of hookah lounges. Am J Public Health. 2012;102:2043–5. doi: 10.2105/AJPH.2012.300751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cobb CO, Vansickel AR, Blank MD, et al. Indoor air quality in Virginia waterpipe cafes. Tob Control. 2013;22:338–43. doi: 10.1136/tobaccocontrol-2011-050350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hammal F, Chappell A, Wild TC, et al. ‘Herbal’ but potentially hazardous: an analysis of the constituents and smoke emissions of tobacco-free waterpipe products and the air quality in the cafes where they are served. Tob Control. 2015;24:290–7. doi: 10.1136/tobaccocontrol-2013-051169. [DOI] [PubMed] [Google Scholar]
- 28.Zaidi SM, Moin O, Khan JA. Second-hand smoke in indoor hospitality venues in Pakistan. Int J Tuberc Lung Dis. 2011;15:972–7. doi: 10.5588/ijtld.10.0524. [DOI] [PubMed] [Google Scholar]
- 29.Zhang B, Haji F, Kaufman P, et al. ‘Enter at your own risk’: a multimethod study of air quality and biological measures in Canadian waterpipe cafes. Tob Control. 2015;24:175–81. doi: 10.1136/tobaccocontrol-2013-051180. [DOI] [PubMed] [Google Scholar]
- 30.Zhou S, Weitzman M, Vilcassim R, et al. Air quality in New York City hookah bars. Tob Control. 2014;24(e3):e193–8. doi: 10.1136/tobaccocontrol-2014-051763. [published Online First: Epub Date]|. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kassem NO, Daffa RM, Liles S, et al. Children’s exposure to secondhand and thirdhand smoke carcinogens and toxicants in homes of hookah smokers. Nicotine Tob Res. 2014;16:961–75. doi: 10.1093/ntr/ntu016. [published Online First: Epub Date] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jawad M, El Kadi L, Mugharbil S, et al. Waterpipe tobacco smoking legislation and policy enactment: a global analysis. Tob Control. 2015;24(Suppl 1):i60–5. doi: 10.1136/tobaccocontrol-2014-051911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.World Bank. The Little Green Data Book. Washington, DC, USA: International Bank for Reconstruction and Development/The World Bank; 2015. (Creative Commons Attribution CC BY 3.0 IGO Ed.) [Google Scholar]
- 34.Yeatts KB, El-Sadig M, Leith D, et al. Indoor air pollutants and health in the United Arab Emirates. Environ Health Perspect. 2012;120:687–94. doi: 10.1289/ehp.1104090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.World Health Organization (WHO) Environmental Health Criteria 213: Carbon Monoxide. 2. Geneva: World Health Organization; 2013. [Google Scholar]
- 36.Astrup P, Kjeldsen K, Wanstrup J. Effects of carbon monoxide exposure on the arterial walls. Ann N Y Acad Sci. 1970;174:294–300. doi: 10.1111/j.1749-6632.1970.tb49796.x. [DOI] [PubMed] [Google Scholar]
- 37.Thomsen HK. Carbon monoxide-induced atherosclerosis in primates. An electron-microscopic study on the coronary arteries of Macaca trus monkeys. Atherosclerosis. 1974;20:233–40. doi: 10.1016/0021-9150(74)90008-2. [DOI] [PubMed] [Google Scholar]
- 38.Jung YS, Lee JS, Min YG, et al. Carbon monoxide-induced cardiomyopathy. Circ J. 2014;78:1437–44. doi: 10.1253/circj.cj-13-1282. [DOI] [PubMed] [Google Scholar]
- 39.Tian L, Ho KF, Wang T, et al. Ambient carbon monoxide and the risk of hospitalization due to chronic obstructive pulmonary disease. Am J Epidemiol. 2014;180:1159–67. doi: 10.1093/aje/kwu248. [DOI] [PubMed] [Google Scholar]
- 40.Tian L, Qiu H, Pun VC, et al. Ambient carbon monoxide associated with reduced risk of hospital admissions for respiratory tract infections. Am J Respir Crit Care Med. 2013;188:1240–5. doi: 10.1164/rccm.201304-0676OC. [DOI] [PubMed] [Google Scholar]
- 41.Delfino RJ, Chang J, Wu J, et al. Repeated hospital encounters for asthma in children and exposure to traffic-related air pollution near the home. Ann Allergy Asthma Immunol. 2009;102:138–44. doi: 10.1016/S1081-1206(10)60244-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Paredi P, Shah P, Montuschi P, et al. Increased carbon monoxide in exhaled air of patients with cystic fibrosis. Thorax. 1999;54:917–20. doi: 10.1136/thx.54.10.917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Misek R, Patte C. Carbon monoxide toxicity after lighting coals at a hookah bar. J Med Toxicol. 2014;10:295–8. doi: 10.1007/s13181-013-0368-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.von Rappard J, Schonenberger M, Barlocher L. Carbon monoxide poisoning following use of a water pipe/hookah. Dtsch Arztebl Int. 2014;111:674–9. doi: 10.3238/arztebl.2014.0674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ozkan S, Ozturk T, Ozmen Y, et al. Syncope associated with carbon monoxide poisoning due to narghile smoking. Case Rep Emerg Med. 2013;2013:796857. doi: 10.1155/2013/796857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.La Fauci G, Weiser G, Steiner IP, et al. Carbon monoxide poisoning in narghile (water pipe) tobacco smokers. CJEM. 2012;14:57–9. doi: 10.2310/8000.2011.110431. [DOI] [PubMed] [Google Scholar]
- 47.Monzer B, Sepetdjian E, Saliba N, et al. Charcoal emissions as a source of CO and carcinogenic PAH in mainstream narghile waterpipe smoke. Food Chem Toxicol. 2008;46:2991–5. doi: 10.1016/j.fct.2008.05.031. [DOI] [PubMed] [Google Scholar]
- 48.King BA, Dube SR, Babb SD. Perceptions about the harm of secondhand smoke exposure among U.S. middle and high school students: findings from the 2012 National Youth Tobacco Survey. Tob Induc Dis. 2013;11:16–16. doi: 10.1186/1617-9625-11-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Aljarrah K, Ababneh ZQ, Al-Delaimy WK. Perceptions of hookah smoking harmfulness: predictors and characteristics among current hookah users. Tob Induc Dis. 2009;5:16–16. doi: 10.1186/1617-9625-5-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lipkus IM, Eissenberg T, Schwartz-Bloom RD, et al. Affecting perceptions of harm and addiction among college waterpipe tobacco smokers. Nicotine Tob Res N. 2011;13:599–610. doi: 10.1093/ntr/ntr049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.King BA, Dube SR, Homa DM. Smoke-free rules and secondhand smoke exposure in homes and vehicles among US adults, 2009–2010. Prev Chronic Dis. 2013;10:E79. doi: 10.5888/pcd10.120218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.King BA, Travers MJ, Cummings KM, et al. Secondhand smoke transfer in multiunit housing. Nicotine Tob Res. 2010;12:1133–41. doi: 10.1093/ntr/ntq162. [published Online First: Epub Date]|. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Primack BA, Sidani J, Agarwal AA, et al. Prevalence of and associations with waterpipe tobacco smoking among U.S. university students. Ann Behav Med. 2008;36:81–6. doi: 10.1007/s12160-008-9047-6. [DOI] [PMC free article] [PubMed] [Google Scholar]