Abstract
Mothers raising a child with ADHD can experience high parenting stress. Mothers’ personality traits and own ADHD symptoms could also affect parenting stress. 430 biological mothers from the Multimodal Treatment Study of Children with ADHD (MTA mothers) and 237 of a local normative comparison group (LNCG mothers) were evaluated at baseline. Interactions were tested between mothers’ group and maternal personality/ADHD symptoms related to parenting stress. Compared to LNCG, MTA mothers had higher parenting stress, self-reported ADHD, neuroticism, and lower conscientiousness and agreeableness. When personality and ADHD were evaluated together, ADHD symptoms interacted with mothers’ group: high maternal ADHD was positively associated with parenting stress for LNCG but not MTA mothers. Personality traits or ADHD characteristics do not appear operative for the high parenting stress of mothers of a child with ADHD. However, high maternal ADHD or low conscientiousness are associated with stress levels similar to raising a child with ADHD.
Keywords: Personality, ADHD, Parenting, Stress
Raising a child with ADHD is challenging because ADHD symptoms are linked to dysfunctional behaviors (e.g., non-compliance to a parent’s instructions, distractibility that prevents task completion) yielding high levels of friction for family life (Gupta, 2007; Johnston & Mash, 2001). Some aspects of this tension can be conceptualized as parenting stress, which has been defined as the demands, consequences, responsibilities, and difficulties related to caring for a child with special needs (Brannan, Heflinger, & Bickman, 1997). In general, stress has been defined as “an external load or demand on a biological, social, or psychological system” (Lazarus, 1993). In order to achieve homeostasis, people utilize coping mechanisms to either change the stressor or the interpretation of the stressful situation. Parenting stress can motivate parents to use various resources to support their parenting (Mash & Johnston, 1990). Without proper coping resources, the stress of raising a child with ADHD can cause strain on the parent’s mental health. Identifying candidate moderators that exacerbate or diminish parenting stress and strain, in order to improve psychoeducational and other treatment interventions to favor family well-being and reduce parental distress, is potentially beneficial for both parents and their offspring.
Parenting stress has been shown to be higher in parents raising a child with ADHD compared to parents raising a child with another disorder/illness or a healthy child (Fischer, 1990). Compared to the normative data, parents with children with ADHD demonstrated elevated levels of parenting stress (Anastopoulos et al., 1992; Pimentel et al., 2011). Low-income and ethnically diverse parents raising a child with ADHD or with a developmental disability also had greater overall stress than parents raising a child with HIV or asthma (Gupta, 2007). Furthermore, middle-class mothers raising a child with ADHD reported significantly greater parenting stress related to child characteristics than mothers raising a child with a learning disability or a child without any handicapping condition (Baker & McCal, 1995). When compared to mothers of healthy children, mothers of “hyperactive” children reported more stress on the Parenting Stress Index, the variable of interest in this study (Mash & Johnston, 1983; for meta-analysis, see Theule et al., 2013).
Several studies have reported information about parents with ADHD, parent personality characteristics and/or parenting stress.
For example, Epstein et al. (2000), found that ADHD symptoms were higher in parents of children from the Multimodal Treatment Study of Children with ADHD (MTA) than in a local normative comparison group (LNCG). More recently, Langberg et al. (2010), also using MTA data, evaluated the moderating effect of parenting stress on the level of mother-father agreement about child ADHD symptom ratings. Also Wells et al., (2000), discussed the association of parenting stress and parental psychopathology in the context of treatment outcome in the MTA.
Other studies have focused on personality characteristics in parents of children with ADHD (e.g., Nigg et al., 2002; Steinhausen et al., 2013), and on personality characteristics of adults with ADHD (e.g., McKinney et al., 2013; Parker et al., 2004). These studies converge on an association of parent’s ADHD with high levels of neuroticism and low levels of conscientiousness and agreeableness.
To our knowledge, few studies have been conducted to evaluate the moderating effect of parental characteristics on the experience of parenting stress/strain in families of children with ADHD (Mash & Johnston, 1990; Theule et al., 2011 ). Based on the previous literature, two candidate variables are (a) maternal ADHD symptom level and (b) maternal personality traits. A parent’s ADHD diagnosis or ADHD symptoms are associated with deficits in parenting control behaviors, with disorganization and chaos, low monitoring of child behavior, ineffective child-rearing problem-solving, and inconsistent and over-reactive discipline (Johnston et al., 2012; Theule et al., 2011). To our knowledge, no studies have empirically evaluated mother’s ADHD symptom domain levels (inattention/ cognitive problems, hyperactivity/restlessness, and impulsivity/emotional lability) as a candidate moderator of parenting stress/strain for mothers with children with versus without ADHD.
Over and above potential genetic mediation (i.e., genetically driven similarity in parental and child ADHD symptomatology), it has been proposed that parent’s ADHD contributes significantly to child development trajectories: “…ADHD-linked parenting difficulties are reciprocally related to child vulnerabilities and each drives dynamic changes in the other over time” (Johnston et al., 2012, p. 216). We would expect up to a fourth of mothers of children with ADHD to have ADHD (Faraone et al, 2000). Johnston and colleagues (2012) leave open the possibility of pathways through which parental ADHD symptoms serve to attenuate or buffer the development of child problems (e.g., parents with ADHD could be in synchrony with a child’s preference for fast-paced activities, or may be more empathic with the children’s attention problems). From a developmental perspective, knowledge of the mechanisms and variations that underlie how a mother’s ADHD interacts with child vulnerabilities across development is critical to informing early interventions for children with ADHD (Johnston & Mash, 2001).
Moreover, mothers with ADHD who have children with ADHD may also be more likely to have personality characteristics that are maladaptive. In a pilot study using the NEO five factor inventory, mothers with ADHD who also had children with ADHD had higher neuroticism and lower conscientiousness than mothers without ADHD who had children with ADHD or children without ADHD (Weinstein, Apfel, & Weinstein, 1998). As such, they may have especially heightened stress due to the combination of their personal characteristics and parenting a child who displays the symptoms and impairments associated with ADHD. Personality traits have been proposed as important resources in coping, decision-making, and other aspects of parenting practices (Abidin, 1992). For example, coping has been described as “personality in action under stress” (Bolger, 1990). That is, a person’s personality traits influence what coping mechanisms a person utilizes. From an extensive meta-analysis (Connor-Smith & Flachsbart, 2007), the NEO-Five personality traits of extraversion and conscientiousness predicted problem-solving and cognitive restructuring. On the other hand, neuroticism predicted problematic strategies like wishful thinking, withdrawal, and emotion-focused coping but (like extraversion) predicted support seeking as well (Connor-Smith & Flachsbart, 2007).
Our main goal is to evaluate whether there are significant differences between biological mothers who have a child with ADHD-Combined type (MTA mothers) and those with a child without ADHD (comparison group mothers) with respect to how maternal “Big Five” personality traits, maternal ADHD symptomatology, or their interaction contribute to the mothers’ experience of parenting stress. We hypothesize that 1) mothers of children with ADHD will report more parenting stress than mothers of comparison children (consistent with previous reports); 2) mothers of children with ADHD will have less adaptive personality traits and higher levels of ADHD symptoms themselves (consistent with previous reports); and 3) the combination of these factors will be associated with the highest levels of parenting stress. Specifically, positive personality traits (high levels of conscientiousness, extraversion, agreeableness and openness) will buffer the stress of rearing a child with ADHD, whereas negative personality traits (high neuroticism) and/or maternal ADHD symptomatology will aggravate parenting stress. In short, maternal personality traits and maternal ADHD will be significant moderators of the parenting stress associated with raising a child with ADHD.
Method
Participants
We utilized data from the Multimodal Treatment Study of Children with ADHD (MTA) (Arnold et al., 1997; MTA Cooperative Group, 2004, 1999), including the auxiliary local normative comparison group (LNCG). MTA children were 7.0 – 9.9 years old at baseline, with carefully diagnosed ADHD-Combined type (for details of diagnostic procedures, see Hinshaw et al., 1997). The LNCG was recruited at the 24-month MTA assessment from the same schools as the MTA, matched for sex and grade; thus the LNCG baseline occurred 2 yr. later than the MTA baseline at each site. At respective baselines, 430 biological mothers of children with carefully diagnosed combined-type ADHD (MTA mothers) and 237 biological mothers of children without ADHD (LNCG mothers) filled out the NEO Five Factor Inventory, the Conners Adult ADHD rating Scale (CAARS), and the Parenting Stress Index (PSI)-short form. The 237 LNCG cases used here excluded 31 LNCG children with ADHD.
Measures
NEO Five Factor Inventory (Costa and McCrae, 1992)
The NEO Five Factor Inventory assesses the Big Five personality traits: neuroticism, extraversion, openness to experience, agreeableness, and conscientiousness. The self-report inventory is 60 questions long, with 12 questions for each construct, rated from 0 to 4. Example items for each construct are: neuroticism: “I often feel tense or jittery,” extraversion: “I like to have a lot of people around me,” openness: “I often try new and foreign foods,” agreeableness, “I generally try to be thoughtful and considerate,” conscientiousness: “When I make a commitment, I can always be counted on to follow through.” For psychometric details, see McCrae et al. 2011.
Conners Adult ADHD Rating Scale (CAARS; Conners, Erhardt, & Sparrow, 1999)
The CAARS has 93 items rated from 0 for “not at all true” to 3 for “very much true. Each of the 4 scale points also includes temporal descriptions (e.g., very often) in order to simplify both responding and interpretation. The items include symptom criteria from the DSM-IV, the Conners’ rating scales for children and adolescents (Conners, 1989), clinical impressions, and conceptualizations of adult ADHD (Wender, 1995). From a previous report (Conners, Erhardt, Epstein, et al., 1999), four factors emerged, using 42 of the 93 items: Inattention/Cognitive Problems, Hyperactivity/Restlessness, Impulsivity/Emotional lability, and problems with self-concept. Erhardt et al. (1999) evaluated a sample of 1006 adults to verify the factor structure and to create norms using confirmatory factor analysis. Internal reliability of the factor scales ranged between .86 and .92; test-retest reliabilities ranged between .88 and .91. Sensitivity (the true positive rate) was 82% and specificity (the true negative rate) was 87%. In order to build a crosswalk with previous MTA studies using the CAARS (Epstein et al., 2000), and considering our interest in maternal ADHD-related symptom dimensions, only the first three factors of the CAARS were used in this study, excluding problems with self-concept.
Parenting Stress Index-short form (PSI; Abidin, 1986, 1990)
The PSI-short form contains 36 parent-completed items using a 5-point scale (strongly agree to strongly disagree). Each item asks about a characteristic of the parent, the child, or their situation. There are 3 factors, resulting in subscales for distress, dysfunctional interaction, and the child’s problematic behaviors. The test-retest (range = .68–.85) and internal reliability (range = .80–.87) are acceptable (Abidin, 1990). For analyses presented here, we used a composite of the Distress and Dysfunctional Interaction scales because we were focusing on the parent’s actual experienced stress, not the child’s behavior. The correlation between Distress and Dysfunctional Interaction in the full sample was r=.62, p<.001.
Procedure
The MTA was a multisite 4-group randomized clinical trial with multi-year follow-up as explained in detail in previous articles (Arnold et al., 1997; Hinshaw et al., 1997,MTA Cooperative Group, 1999). For this study, we used data from participant’s baseline assessments. We were not concerned with the ADHD treatment groups, but rather the differences, if any, between parents of children with ADHD and parents of children without ADHD, prior to randomly assigned intervention. Thus the analyses are on baseline measures.
Statistical Analyses
Statistical analyses were conducted with SPSS version 21 (IBM Corp., 2012). Little’s test indicated that the missing-completely-at-random (MCAR) assumption was tenable for the LNCG (χ2=49.10, df=41, p=.18), but not for the MTA group of mothers (χ2=62.28, df=42, p=.02). Because the MCAR was tenable and the amount of missing data was small in the LNCG, we used listwise deletion for this group of mothers. For the MTA group, where n=57 mothers had incomplete CAARS data, the multiple imputation procedure was employed, imputing five sets of values for all measures (Rubin, 1996).
After examining the data using descriptive statistics, we used, to contrast MTA and LNCG mothers, chi squared tests (for categorical variables) or independent t-tests (for dimensional variables). For the latter, the measure of effect size was Cohen’s d, which was computed using the pooled within-group SD.
To answer our main question --whether mother’s NEO “Big Five” personality traits and/or mother’s ADHD symptomatology interact with the relation between mothers’ group (MTA or LNCG) and parenting stress-- we utilized hierarchical regression analyses. After a preliminary examination of candidate sociodemographic moderators (e.g., mother’s age, employment status), those that showed to be significant were considered as potential confounders and were entered into a final model. These (e.g., marital status) were entered in the first block before testing the interaction term of each main candidate moderator (e.g., ADHD index or NEO trait) x mother’s group (Aiken & West, 1991; Cohen, et al., 2003). Continuous variables were centered to zero, and 95% confidence intervals around the regression coefficients are reported. When a significant two-way interaction was observed, signifying significant differences in slopes between groups, graphs were constructed to depict the different associations, using Bauer et al. approach (Bauer & Curran, 2005; Preacher, Currant & Bauer, 2006).
Finally, sensitivity analyses were conducted in order to compare the stress levels of MTA mothers whose child had comorbid ODD/CD to those whose children did not.
Results
MTA mothers were younger when their child was born and reported lower incomes and more lifetime mental/nervous problems than LNCG mothers (Table 1). The observed difference in child’s age and most of the difference in mother’s age at the time of filling out the NEO are artifacts of the baseline evaluation of the MTA sample occurring two years earlier than the matched LNCG mothers.
Table 1.
Sociodemographic and clinical characteristics of LNCG and MTA biological mothers.
| Variables | LNCG Mothers (n=237) | MTA Mothers (n=430) | t-test or χ2 | p |
|---|---|---|---|---|
| Child Age at baseline, M (SD) | 9.87 (1.10) | 7.80 (.81) | 27.54 | <.001 |
| Mother Age when child was born, M (SD) | 29.17 (5.82) | 28.10 (5.77) | 2.28 | .02 |
| Mother Age at completing NEO, M (SD) | 39.03 (6.00) | 36.28 (5.76) | 5.82 | <.001 |
| Married, n (%) | 186 (79) | 314 (73) | 2.73 | .11 |
| High school or more education., n (%) | 223 (95) | 410 (95) | 0.24 | .71 |
| Full time job, n (%) | 116 (49) | 234 (54) | 1.84 | .19 |
| Income, $<40.000, n (%) | 83 (36) | 201 (47) | 6.72 | .01 |
| Public assistance, welfare, n (%) | 27 (11) | 60 (14) | .85 | .40 |
| Mental/nervous problems, n (%) | 30 (13) | 88 (21) | 5.19 | .02 |
| NEO Five Factor Inventory, M (SD) | ||||
| Neuroticism | 1.37 (.53) | 1.72 (.68) | −6.76 | <.001 |
| Extraversion | 2.43 (.45) | 2.37 (.50) | 1.61 | .11 |
| Openness | 2.24 (.45) | 2.26 (.47) | −.34 | .74 |
| Agreeableness | 2.92 (.41) | 2.79 (.41) | 3.81 | <.001 |
| Conscientiousness | 2.98 (.46) | 2.75 (.55) | 5.35 | <.001 |
| Conners Adult ADHD rating Scales, M (SD) | ||||
| Inattention/Cognitive Problems | .52 (.37) | .72 (.55) | −4.72 | <.001 |
| Hyperactivity/Restlessness | .59 (.37) | .79 (.52) | −4.88 | <.001 |
| Impulsivity/Emotional Lability | .49 (.34) | .68 (.42) | −5.83 | <.001 |
| CAARS ADHD Index | .53 (.30) | .73 (.43) | −7.03 | <.001 |
| Parent Stress Index Composite, M (SD) | 23.33 (16.35) | 44.26 (19.06) | −13.88 | <.001 |
Note. The 2-year difference in children’s age at baseline, and part of the 3-yr. difference in mother’s age when the NEO was completed are reflecting artifacts of the design: the baseline evaluation of the MTA children and mothers occurred 2 years earlier than the matched LNCG children and mothers.
LNCG=Local Normative Comparison Group; MTA=Multimodal Treatment Study of ADHD.
ADHD Index = average of the 3 relevant CAARS factors. The Parent Stress Index Composite, was transformed into percentage of maximum possible (POMP) scoring in order to facilitate interpretation (range score 0 to 100).
On the PSI, MTA mothers reported far higher parenting stress than LNCG mothers (d=1.15).
In terms of personality, MTA mothers, compared to LNCG mothers, scored higher on the neuroticism (d=.56) scale and lower on conscientiousness (d=−.44) and agreeableness (d=−.32) scales. Differences between groups for extraversion and openness were not significant. MTA mothers rated themselves significantly higher on all three CAARS factors than LNCG mothers (d=.39 to d=.48). The item mean for composited symptoms of inattention, hyperactivity and impulsivity were .73 for the MTA mothers, .53 for the LNCG.
The correlation between children’s age and parenting stress was not significant in either the LNCG (r=−.04, p>.05) or the MTA group (r=.04, p>.05). Thus children’s age did not account for the differences in parenting stress.
Mothers’ group differences in predictors of parenting stress
When each personality trait was independently evaluated from the other four personality traits, no statistically significant interactions were observed (Supplemental Table 1). However, in a model in which the five personality traits were entered simultaneously (Table 2), a statistically significant interaction revealed a residual group difference in slopes (b=8.28, 95% CI = [2.74, 13.82]) for the association of conscientiousness with parenting stress after controlling for the remaining four personality traits.
Table 2.
All NEO personality trait factors were entered in a single model to evaluate group differences on intercepts and slopes between LNCG and MTA mothers, adjusting for the potential confounding effect of the remaining four personality traits.
| R2 | ΔR2 | B | SE | β | 95% CI | ||
|---|---|---|---|---|---|---|---|
| LB | UB | ||||||
| Step 1 | .35 | .35*** | |||||
| Constant | 36.91 | .64 | [35.65, | 38.18] | |||
| Neuroticism | 12.97 | 1.20 | .41 | [10.61, | 15.33] | ||
| Extraversion | −4.43 | 1.52 | −.10 | [−7.42, | −1.44] | ||
| Openness | −.95 | 1.41 | −.02 | [−3.71, | 1.81] | ||
| Agreeableness | −7.01 | 1.71 | −.14 | [−10.37, | −3.65] | ||
| Conscientiousness | −3.67 | 1.42 | −.10 | [−6.46, | −.87] | ||
| Step 2 | .48 | .13*** | |||||
| Constant | 27.29 | 1.08 | [25.16, | 29.41] | |||
| Neuroticism | 10.02 | 2.17 | .32 | [5.77, | 14.27] | ||
| Extraversion | −4.02 | 2.42 | −.10 | [−8.77, | .73] | ||
| Openness | −2.36 | 2.14 | −.05 | [−6.57, | 1.84] | ||
| Agreeableness | −2.95 | 2.66 | −.06 | [−8.16, | 2.27] | ||
| Conscientiousness | −8.04 | 2.37 | −.21 | [−12.68, | −3.39] | ||
| Mother’s group | 15.16 | 1.31 | .35 | [12.59, | 17.72] | ||
| Mother’s group* Neuroticism | .99 | 2.51 | .03 | [−3.95, | 5.92] | ||
| Mother’s group* Extraversion | −2.01 | 2.94 | −.04 | [−7.78, | 3.77] | ||
| Mother’s group* Openness | 2.03 | 2.66 | .04 | [−3.20, | 7.25] | ||
| Mother’s group* Agreeableness | −4.03 | 3.27 | −.07 | [−10.44, | 2.39] | ||
| Mother’s group* Conscientiousness | 8.28 | 2.82 | .18 | [2.74, | 13.82] | ||
Note: F(2,653)=26.58, p= <.001
p<.05,
p<.01,
p<.001
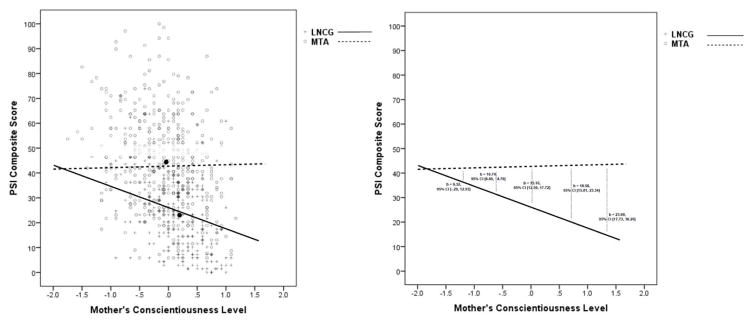
As depicted in Figure 1, the estimated parenting stress level by mothers’ group at the pooled sample mean for conscientiousness was 27.29 for LNCG and 42.45 for MTA. Reflecting the statistically significant interaction, conscientiousness was negatively associated with parenting stress for LNCG (b=−8.04, 95% CI [−12.68, −3.39]) but not MTA mothers (b=0.24, 95% CI [−2.78, 3.27]). Relatedly, the estimated mean difference in parenting stress between mother groups was significant at a moderate to high level of conscientiousness (>1 SD above the pooled sample mean) but not at a very low level (<2 SD below the pooled sample mean) of conscientiousness.
Figure 1.
The relationship between maternal level of conscientiousness and parenting stress in the MTA and LNCG samples. Conscientiousness (x axis) was centered on the pooled sample mean. Conscientiousness protects against parenting stress for LNCG mothers, who do not have a child with ADHD, but not for MTA mothers, who have a childwith ADHD. The diverging lines suggest that having a child with ADHD neutralizes the protective effect of conscientiousness against parenting stress. Estimate intercept differences between groups at different levels of conscientiousness (pooled −2SD, −1SD, Mean, +1SD and +2SD) are offered with their respective 95% CI in the right panel. The dark dots represent sample means for the MTA group (upper left) and the LNCG (lower right).
For CAARS factors (Supplemental Table 2), significant interactions were observed on inattention/cognitive problems (b=−.73, 95% CI= [−1.29, −.16]); and hyperactivity/restlessness (b=−.70, 95% CI= [−1.28, −.11]). With both predictors, the level of parenting stress was higher for MTA mothers than for LNCG mothers, but the effect of inattention/cognitive problems and hyperactive/restlessness on parenting stress (slope) was greater for LNCG than MTA mothers.
The high correlation between CAARS factors (rs=.50 to .70), prevented us from generating a similar model to that used with the NEO personality traits (adjusting for the others and evaluating the marginal effect). Therefore, to prevent collinearity problems, we generated a single composite index of mothers’ ADHD symptom level from the three CAARS factors to be entered together with sociodemographic and NEO variables in a single model.
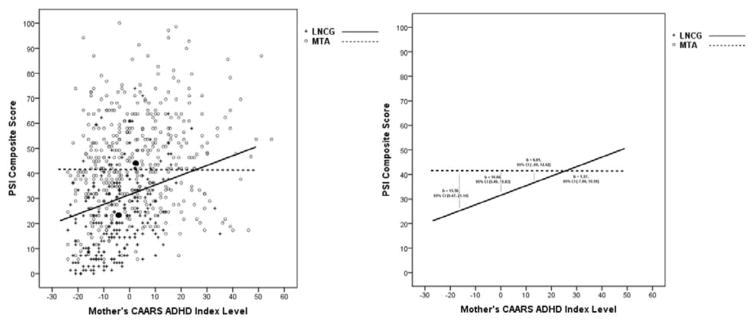
Being married was associated with less parenting stress for the LNCG (b = −.6.85) but not for the MTA (b =.064) (see Supplemental Table 3). When marital status, NEO personality traits, and the composite ADHD index were entered together in a single model (Table 3), the only significant two-way interaction observed was on the CAARS ADHD index (b=−.32, 95% CI = [−.56, −.08]). As represented in Figure 2, the two-way interaction was identical to the effect observed for inattention/cognitive problems and hyperactivity/restlessness described before. Maternal ADHD symptom level had a significantly stronger association with parenting stress for the LNCG than for the ADHD mothers, to the point that parenting stress turned out to be non-significantly different between mothers’ groups when the CAARS ADHD index score was 1 SD above the pooled sample mean.
Table 3.
Marital status, NEO personality traits and CAARS ADHD Index together in a single model to evaluate intercept and slope differences between LNCG and MTA mother, adjusting for the potential confounding effect of the remainder predictors in the model.
| R2 | ΔR2 | B | SE | β | 95% CI | ||
|---|---|---|---|---|---|---|---|
| LB | UB | ||||||
| Step1 | .36 | .36*** | |||||
| Constant | 38.30 | 1.31 | [35.73, | 40.87] | |||
| Married | −1.66 | 1.52 | −.04 | [−4.65, | 1.32] | ||
| Neuroticism | 12.19 | 1.27 | .39 | [9.70, | 14.69] | ||
| Extraversion | −5.12 | 1.58 | −.12 | [−8.22, | −2.03] | ||
| Openness | −1.41 | 1.46 | −.03 | [−4.27, | 1.46] | ||
| Agreeableness | −6.67 | 1.75 | −.14 | [10.11, | −3.23] | ||
| Conscientiousness | −2.18 | 1.54 | −.06 | [−5.21, | .84] | ||
| ADHD Index | .12 | .06 | .09 | [.01, | .23] | ||
| Step 2 | 49 | .13*** | |||||
| Constant | 31.05 | 2.23 | [26.67, | 35.43] | |||
| Married | −4.57 | 2.51 | −.10 | [−9.49, | .35] | ||
| Neuroticism | 8.38 | 2.30 | .27 | [3.86, | 12.91] | ||
| Extraversion | −5.72 | 2.59 | −.13 | [−10.81, | −.63] | ||
| Openness | −2.69 | 2.27 | −.06 | [−7.15, | 1.77] | ||
| Agreeableness | −1.26 | 2.83 | −.03 | [−6.81, | 4.30] | ||
| Conscientiousness | −4.83 | 2.61 | −.13 | [−9.96, | .30] | ||
| ADHD Index | .32 | .11 | .22 | [.10, | .53] | ||
| Mother’s group | 10.66 | 2.63 | .25 | [5.49, | 15.83] | ||
| Mother’s group* Married | 5.58 | 2.99 | .14 | [−.30, | 11.46] | ||
| Mother’s group* Neuroticism | 2.63 | 2.67 | .07 | [−2.60, | 7.87] | ||
| Mother’s group* Extraversion | −.33 | 3.10 | −.01 | [−6.42, | 5.76] | ||
| Mother’s group* Openness | 2.37 | 2.78 | .05 | [−3.09, | 7.84] | ||
| Mother’s group* Agreeableness | −5.77 | 3.41 | −.10 | [−12.47, | .93] | ||
| Mother’s group* Conscientiousness | 5.09 | 3.08 | .11 | [−.97, | 11.14] | ||
| Mother’s group* ADHD Index | −.32 | .12 | −.20 | [−.56, | −.08] | ||
Note: F(2,632)=20.22, p= <.001
p<.05,
p<.01,
p<.001
Figure 2.
The relationship between maternal ADHD index level and parenting stress in the MTA and LNCG samples. CAARS ADHD index level was centered on the pooled sample mean (x axis = 0). The convergence of lines suggests that having a child with ADHD or the mother having ADHD herself has similar effects on the level of parenting stress. Estimate intercept differences between groups at different levels of CAARS ADHD Index (pooled −1SD, Mean, +1SD and +2SD) are offered with their respective 95% CI in the right panel. Black dots represent PSI composite and CAARS ADHD index sample means for LNCG lower (left) and MTA (upper right). X axis values are raw CAARS ADHD index scores.
Neither marital status nor conscientiousness remained significant after adjusting for the effect of the other competing predictors.
Sensitiviy Analyses
An additional secondary analysis explored the finding that conscientious did not protect MTA mothers from parenting stress as it did for the LNCG mothers. The secondary hypothesis is that the strong admixture of oppositional-defiant comorbidity with combined type ADHD (54% of the MTA sample had oppositional-defiant disorder or conduct disorder) may, besides adding to the mother-child friction (Johnston, 1996; Podolski & Nigg, 2001; Edwards et al. 2001), also neutralize any benefit of the mother’s conscientiousness. When comparing the stress of MTA mothers whose child had comorbid ODD/CD to those whose children did not, significantly different intercepts emerged at the level of the pooled mean conscientiousness: mothers with a child with ADHD+ODD/CD showed more parenting stress than mothers with a child with ADHD alone (b=4.45, 95% CI [.86, 8.05]), but no significant interaction between comorbidity group and conscientiousness was observed. This indicates that stress is higher when a child’s behavior is more troublesome, but mother’s adaptive personality (conscientiousness) still does not buffer (not moderate) the stress associated with raising a child with or without ODD/CD.
Discussion
Consistent with previous reports, having a child with ADHD is associated with high levels of parenting stress. MTA mothers’ mean level of parenting stress was greater than the level of parenting stress observed in 68% of the comparison LNCG mothers. Anastopoulos et al. (1992) also found higher stress in mothers of children with ADHD, but they used all three PSI factors as an indicator of stress, which confounds parental perceptions of the child’s problematic behavior with perceptions of stress.
Crucially, maternal characteristics do not appear to either exacerbate or buffer the perceived stress of parenting a child with ADHD, whereas conscientiousness buffers and maternal ADHD symptoms exacerbate parenting stress of comparison mothers. Possibly LNCG mothers’ stress might have resulted from other factors more sensitive to maternal characteristics. Or perhaps the LNCG had a low enough range of stress to allow the influence of maternal characteristics to emerge. At 2 SD below the mean of conscientiousness, there was no significant difference in stress level between MTA and LNCG mothers, suggesting that low maternal conscientiousness and having a child with ADHD have similar (not additive) linkages to maternal stress.
One explanation could be that, whereas a typical child may respond positively to his/her mothers’ careful parenting efforts –with such efforts possibly influenced by their conscientiousness level– a child with ADHD may react negatively to a mother’s directive efforts. As reflected in some NEO conscientiousness items, organization, good use of time, setting clear goals and work to accomplish these aims are some behavioral examples that characterize highly conscientious mothers. The inability of a child with ADHD to carry out maternal conscientious ideals may be frustrating to the mother and, by adding to stress, neutralize any benefit of mother’s conscientiousness.
Mother’s conscientiousness has been found to be significantly related to the parenting behavior of ease of setting limits which is associated with fewer externalizing problems in late adolescence (Oliver, Guerin, and Coffman, 2009, Prinzie et al. 2003; McCabe, 2013).
Although there is individual variability, mothers of children with ADHD have on average lower conscientiousness and agreeableness and higher neuroticism than mothers of children without ADHD. These differences may reflect either genetically linked maternal ADHD or mothers’ “giving up” their conscientious ideals under stress, becoming less agreeable because of stress, and developing anxiety, moodiness and other negative valence feelings. Because personality traits are relatively stable in adulthood (Roberts & DelVecchio, 2000), a genetic link seems more probable. However, research has suggested that some traits such as conscientiousness change in middle and old age (Roberts, et al. 2006), so some interaction of genetics and effects of child’s behavior remains a possibility
When maternal ADHD symptomatology and personality traits were evaluated simultaneously, maternal ADHD level was the only variable that contributed to an interaction with mothers’ group in relation to stress. Intriguingly, the ADHD symptom level reported by the LNCG mothers contributed to their perceived parenting stress. The convergence of lines in Figure 2 suggests that having a child with ADHD and the mother having a high level of ADHD symptomatology herself are associated with similar high levels of parenting stress.
Disorganization within the family appears stressful whether the source of disorganization is the parent or the child. The child’s ADHD symptoms may exert a ceiling effect on parental stress for which parental ADHD is not additive (see below for further comment). Alternatively, parental ADHD symptoms may either prevent the parent from noticing and being bothered by the child’s problems, or may help the parent to be empathic, identifying with the child and being hopeful that the child will eventually improve as the parent presumably has.
These results suggest screening for psychopathology in parents seeking mental health services because of high levels of parenting stress, even when the child does not meet criteria for a diagnosis of ADHD or other mental disorder. As observed, a mother’s high ADHD symptomatology is associated with a high level of parenting stress similar to that experienced by a mother raising a child with ADHD. The mother’s symptoms need to be carefully evaluated.
The line of virtually zero slope for MTA mothers in Figure 2 shows that maternal stress is already so high by having a child with ADHD combined-type that it is not increased further by maternal ADHD symptomatology (contrary to our prediction). Our finding of high maternal stress regardless of her ADHD symptom level was striking given the high heritability of ADHD (Larsson et al. 2013) and recent findings that maternal ADHD impacts treatment (Chronis-Tuscano et al. 2011). Careful inspection of Figure 2 suggests that the flat slope observed in MTA mothers is not attributable to a ceiling effect.
As is well documented in previous studies (Pimentel et al., 2011; Weinstein, Apfel, & Weinstein, 1998), MTA mothers manifested a higher level of parenting stress, higher levels of neuroticism, and lower levels of agreeableness and conscientiousness than LNCG mothers. But from our results, neither maternal ADHD symptomatology nor personality traits measured by the NEO moderated the level of parenting stress associated with raising a child with ADHD. Apparently, having a child with ADHD, especially one with comorbid ODD/CD, is a severe enough stressor to trump maternal personality and ADHD symptoms in determining parenting stress level.
Limitations of the findings include that both predictors and criterion variables were derived from cross-sectional mother’s self-report. The self-report nature of the data explain in part the non-independence observed between mother personality and ADHD (informant bias). Further, some correlation is to be expected, given the ubiquitous overlaps in psychopathology. Also, baseline measures for the two groups occurred two years apart. Another limitation is that by restricting to biological mothers, we were not able to use the whole MTA sample, leaving out adoptive parents and cases where the father was primary caregiver. The focus on mothers prevents generalization to all parents; fathers may show different findings. Also, it is possible that the sample was not representative of mothers of children with ADHD, because enrolling their child in a study that required much effort could be a form of coping that distinguished this sample from most mothers of children with ADHD.
The findings confirm that biological mothers of children with ADHD are more stressed than biological mothers of children without ADHD. This high level of stress could lead to an increase in family conflict, undermine positive parenting resources, negatively influence the family process, and exacerbate child dysfunctional behaviors. More research is needed to identify other potential moderators of parenting stress for mothers raising a child with ADHD in order to tailor (and improve) child and family treatments. Based on the association observed between depressive symptoms and parenting behaviors in the MTA sample (Gerdes et al., 2007), and with parenting stress in general (Theule, 2012), maternal depressive symptoms would be a good potential moderator. However, we decided not to enter maternal depression into the current models because although the neuroticism scale of the NEO is not, strictly speaking, a measure of depression, neuroticism has been associated with depressive symptoms on both theoretical and empirical grounds (Trull & Sher, 1994; Watson & Clark, 1984). Many of the items of the neuroticism scale demonstrate good face validity with respect to depressive symptoms (e.g., I am seldom sad or depressed, Sometimes I feel completely worthless).
Regarding future research, presence of support in the family environment, such as partner level of involvement in parenting, warrants further study. Before concluding that mother’s personality assessment is not relevant to tailoring a child’s ADHD treatment, we might evaluate other related constructs (e.g. maternal temperament, or parenting strategies) or assess whether a multifactor view of the NEO personality traits (trait combinations instead of using a single factor approach) reveal other results than those observed here. Also, it may be fruitful to test alternative models that consider the impact of maternal characteristics on parenting behaviors, child behaviors, response to treatment, and parenting stress.
Acknowledgments
This work was supported cooperative agreement grants and contracts from the National Institute of Mental Health to the following: University of California, Berkeley: U01 MH50461, N01MH12009, and HHSN271200800005-C; Duke University: U01 MH50477, N01MH12012, and HHSN271200800009-C; University of California, Irvine: U01 MH50440, N01MH 12011, and HHSN271200800006-C; Research Foundation for Mental Hygiene (New York State Psychiatric Institute/Columbia University): U01 MH50467, N01 MH12007, and HHSN271200800007-C; Long Island-Jewish Medical Center U01 MH50453; New York University: N01MH12004 and HHSN271200800004-C; University of Pittsburgh:
U01 MH50467, N01MH12010, and HHSN271200800008-C; and McGill University N01MH12008 and HHSN271200800003-C. The Office of Special Education Programs of the U.S. Department of Education, the Office of Juvenile Justice and Delinquency Prevention of the Justice Department, and the National Institute on Drug Abuse also participated in funding.
Dr. Arnold has received research funding from CureMark, Forest, Lilly, and Shire, advisory board honoraria from Biomarin, Novartis, Noven, Roche, Seaside Therapeutics, and Shire, consulting fees from Tris Pharma, and travel support from Noven. Dr. Swanson reports receiving consulting fees to his institution from Noven Pharmaceuticals, lecture fees from Johnson & Johnson and Janssen, travel support from Shire, and payment for providing testimony as an expert witness for Janssen–Ortho on the pharmacokinetic and pharmacodynamic properties of methylphenidate, and filing a lawsuit to be named as an inventor on filed patents. He also received a research contract from the National Institute of Child Health and Development (NICHD) and a research grant form the National Institute of Mental Health (NIMH) and was employed by the University of California, Irvine (UCI) and Florida International University (FIU). Dr. Hechtman is a presenter, on advisory board, and received research funding from Lilly, Purdue, Janssen and Shire. Dr. Jensen has received consulting fees and a charitable contribution from Shire, Inc. Dr. Copley participated in pharmaceutical research summer internships with Pfizer and Parke Davis during her undergraduate education. She also received fellowship support for travel from the American Psychiatric Association/Shire Child and Adolescent Psychiatry Fellowship.
References
- Abidin RR. Parenting Stress Index: Test manual. Charlottesville, VA: Pediatric Psychology Press; 1986. [Google Scholar]
- Abidin RR. Parenting Stress Index – short form: Test manual. Charlottesville, VA: Pediatric Psychology Press; 1990. [Google Scholar]
- Abidin RR. The determinants of parenting behavior. Journal of Clinical Child Psychology. 1992;21(4):407–412. doi: 10.1207/s15374424jccp2104_12. [DOI] [Google Scholar]
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Newbury Park, CA: Sage; 1991. [Google Scholar]
- Anastopoulos AD, Guevremont DC, Shelton TL, DuPaul GJ. Parenting stress among families of children with attention deficit hyperactivity disorder. Journal of Abnormal Child Psychology. 1992;20(5):503–520. doi: 10.1007/BF00916812. [DOI] [PubMed] [Google Scholar]
- Arnold LE, Abikoff HB, Cantwell DP, Conners CK, Elliott G, Greenhill LL, … Jensen PS. National Institute of Mental Health Collaborative Multimodal Treatment Study of children with ADHD (the MTA) design challenges and choices. Archives of General Psychiatry. 1997;54(9):865. doi: 10.1001/archpsyc.1997.01830210113015. [DOI] [PubMed] [Google Scholar]
- Baker DB, McCal K. Parenting stress in parents of children with attention-deficit hyperactivity disorder and parents of children with learning disabilities. Journal of Child and Family Studies. 1995;4(1):57–68. doi: 10.1007/BF02233954. [DOI] [Google Scholar]
- Bauer DJ, Curran PJ. Probing interactions in fixed and multilevel regression: Inferential and graphical techniques. Multivariate Behavioral Research. 2005;40(3):373–400. doi: 10.1207/s15327906mbr4003_5. [DOI] [PubMed] [Google Scholar]
- Bolger N. Coping as a personality process: a prospective study. Journal of Personality and Socical Psychology. 1990;59(3):525–537. doi: 10.1037//0022-3514.59.3.525. [DOI] [PubMed] [Google Scholar]
- Brannan AM, Heflinger CA, Bickman L. The caregiver strain questionnaire measuring the impact on the family of living with a child with serious emotional disturbance. Journal of Emotional and Behavioral Disorders. 1997;5(4):212–222. doi: 10.1177/106342669700500404. [DOI] [Google Scholar]
- Chronis-Tuscano A, O’Brien K, Johnston C, Jones H, Clarke T, Raggi V, … Seymour K. The relation between maternal ADHD symptoms and improvement in child behavior following brief behavioral parent training is mediated by change in negative parenting. Journal of Abnormal Child Psychology. 2011;39(7):1047–1057. doi: 10.1007/s10802-011-9518-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences. 3. Hillsdale, NJ: Lawrence Erlbaum; 2003. [Google Scholar]
- Conners C, Erhardt D, Epstein J, Parker J, Sitarenios G, Sparrow E. Self-ratings of ADHD symptoms in adults I: Factor structure and normative data. Journal of Attention Disorders. 1999;3(3):141–151. doi: 10.1177/108705479900300303. [DOI] [Google Scholar]
- Conners C, Erhardt D, Sparrow E. Conners’ Adult ADHD Rating Scales (CAARS) Technical Manual. North Tonawanda, NY: Multi-Health Systems: Inc; 1999. [Google Scholar]
- Conners CK. Manual for Conners’ rating scales. Toronto: Multi-Health Systems, Inc; 1989. [Google Scholar]
- Connor-Smith JK, Flachsbart C. Relations between personality and coping: a meta-analysis. Journal of Personality and Socical Psychology. 2007;93(6):1080–1107. doi: 10.1037/0022-3514.93.6.1080. [DOI] [PubMed] [Google Scholar]
- Costa PT, McCrae RR. NEO PI-R Professional manual. Odessa, FL: Psychological Assessment Resources; 1992. [Google Scholar]
- Edwards G, Barkley RA, Laneri M, Fletcher K, Metevia L. Parent–adolescent conflict in teenagers with ADHD and ODD. Journal of Abnormal Child Psychology. 2001;29(6):557–572. doi: 10.1023/A:1012285326937. [DOI] [PubMed] [Google Scholar]
- Epstein JN, Conners CK, Erhardt D, Arnold LE, Hechtman L, Hinshaw SP, … Vitiello B. Familial aggregation of ADHD characteristics. Journal of Abnormal Child Psychology. 2000;28(6):585–594. doi: 10.1023/A:1005187216138. [DOI] [PubMed] [Google Scholar]
- Erhardt D, Epstein J, Conners C, Parker J, Sitarenios G. Self-ratings of ADHD symptomas in auts II: Reliability, validity, and diagnostic sensitivity. Journal of Attentional Disorders. 1999;3(3):153–158. doi: 10.1177/108705479900300304. [DOI] [Google Scholar]
- Faraone SV. Genetics of childhood disorders: XX. ADHD, Part 4: is ADHD genetically heterogeneous? J Am Acad Child Adolesc Psychiatry. 2000;39(11):1455–1457. doi: 10.1097/00004583-200011000-00022. [DOI] [PubMed] [Google Scholar]
- Fischer M. Parenting stress and the child with attention deficit hyperactivity disorder. Journal of Clinical Child Psychology. 1990;19(4):337–346. doi: 10.1207/s15374424jccp1904_5. [DOI] [Google Scholar]
- Gupta VB. Comparison of parenting stress in different developmental disabilities. Journal of Developmental and Physical Disabilities. 2007;19(4):417–425. doi: 10.1007/s10882-007-9060-x. [DOI] [Google Scholar]
- Hinshaw SP, March JS, Abikoff H, Arnold LE, Cantwell DP, Conners CK, … Wigal T. Comprehensive assessment of childhood attention-deficit hyperactivity disorder in the context of a multisite, multimodal clinical trial. Journal of Attention Disorders. 1997;1(4):217–234. doi: 10.1177/108705479700100403. [DOI] [Google Scholar]
- IBM Corp. IBM SPSS Statistics for Windows, Version 21.0. Armonk, NY: IBM Corp; 2012. [Google Scholar]
- Johnston C. Parent characteristics and parent-child interactions in families of nonproblem children and ADHD children with higher and lower levels of oppositional-defiant behavior. Journal of Abnormal Child Psychology. 1996;24(1):85–104. doi: 10.1007/BF01448375. [DOI] [PubMed] [Google Scholar]
- Johnston C, Mash EJ. Families of children with attention-deficit/hyperactivity disorder: review and recommendations for future research. Clinical Child and Family Psychology Review. 2001;4(3):183–207. doi: 10.1023/A:1017592030434. [DOI] [PubMed] [Google Scholar]
- Johnston C, Mash EJ, Miller N, Ninowski JE. Parenting in adults with attention-deficit/hyperactivity disorder (ADHD) Clinical Psychology Review. 2012;32(4):215–228. doi: 10.1016/j.cpr.2012.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langberg JM, Epstein JN, Simon JO, Loren RE, Arnold LE, Hechtman L, … Wigal T. Parental Agreement on ADHD Symptom-Specific and Broadband Externalizing Ratings of Child Behavior. Journal of Emotional and Behavioral Disorders. 2010;18(1):41–50. doi: 10.1177/1063426608330792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larsson H, Chang Z, D’Onofrio BM, Lichtenstein P. The heritability of clinically diagnosed attention deficit hyperactivity disorder across the lifespan. Psychological Medicine Journal. 2013:1–7. doi: 10.1017/S0033291713002493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus RS. From psychological stress to the emotions: a history of changing outlooks. Annual Review of Psychology. 1993;44:1–21. doi: 10.1146/annurev.psych.44.1.1. [DOI] [PubMed] [Google Scholar]
- Mash EJ, Johnston C. Parental perceptions of child behavior problems, parenting self-esteem, and mothers’ reported stress in younger and older hyperactive and normal children. Journal of Consulting and Clinical Psychology. 1983;51(1):86–99. doi: 10.1037//0022-006X.51.1.86. [DOI] [PubMed] [Google Scholar]
- Mash EJ, Johnston C. Determinants of parenting stress: Illustrations from families of hyperactive children and families of physically abused children. Journal of Clinical Child Psychology. 1990;19(4):313–328. doi: 10.1207/s15374424jccp1904_3. [DOI] [Google Scholar]
- McCabe JE. Maternal personality and psychopathology as determinants of parenting behavior: A quantitative integration of two parenting literatures. Psychological Bulletin. 2014;140(3):722–750. doi: 10.1037/a0034835. [DOI] [PubMed] [Google Scholar]
- McCrae RR, Kurtz JE, Yamagata S, Terracciano A. Internal consistency, retest reliability, and their implication for personality scale validity. Personality and Social Psychology Review. 2011;15(1):28–50. doi: 10.1177/1088868310366253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKinney AA, Canu WH, Schneider HG. Distinct ADHD symptom clusters differentially associated with personality traits. Journal of Attentional Disorders. 2013;17(4):358–366. doi: 10.1177/1087054711430842. [DOI] [PubMed] [Google Scholar]
- MTA Cooperative Group. A 14-month randomized clinical trial of treatment strategies for Attention-Deficit/Hyperactivity Disorder. Archives of General Psychiatry. 1999;56:1073–86. doi: 10.1001/archpsyc.56.12.1073. [DOI] [PubMed] [Google Scholar]
- MTA Cooperative Group. The NIMH MTA follow-up: 24-month outcomes of treatment strategies for attention-deficit/hyperactivity disorder (ADHD) Pediatrics. 2004;113:754–761. doi: 10.1542/peds.113.4.754. [DOI] [PubMed] [Google Scholar]
- Nigg JT, John OP, Blaskey LG, Huang-Pollock CL, Willicut EG, Hinshaw SP, Pennington B. Big Five dimensions and ADHD symptoms: Links between personality traits and clinical symptoms. Journal of Personality and Social Psychology. 2002;83(2):451. doi: 10.1037//0022-3514.83.2.451. [DOI] [PubMed] [Google Scholar]
- Oliver PH, Guerin D, Coffman JK. Big five parental personality traits, parenting behaviors, and adolescent behavior problems: a mediation model. Personality And Individual Differences. 2009;47(6):631–636. doi: 10.1016/j.paid.2009.05.026. [DOI] [Google Scholar]
- Parker JD, Majeski SA, Collin VT. ADHD symptoms and personality: Relationships with the five-factor model. Personality and Individual Differences. 2004;36(4):977–987. doi: 10.1016/S0191-8869(03)00166-1. [DOI] [Google Scholar]
- Pimentel MJ, Vieira-Santos S, Santos V, Vale MC. Mothers of children with attention deficit/hyperactivity disorder: relationship among parenting stress, parental practices and child behaviour. ADHD Attention Deficit and Hyperactivity Disorders. 2011;3(1):61–68. doi: 10.1007/s12402-011-0053-3. [DOI] [PubMed] [Google Scholar]
- Podolski CL, Nigg JT. Parent stress and coping in relation to child ADHD severity and associated child disruptive behavior problems. Journal of Clinical Child Psychology. 2001;30(4):503–513. doi: 10.1207/S15374424JCCP3004_07. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Curran PJ, Bauer DJ. Computational tools for probing interactions in multiple linear regression, multilevel modeling, and latent curve analysis. Journal of Educational and Behavioral Statistics. 2000;31(4):437–448. doi: 10.3102/10769986031004437. [DOI] [Google Scholar]
- Prinzie P, Onghena P, Hellinckx W, Grietens H, Ghesquière P, Colpin H. Parent and child personality characteristics as predictors of negative discipline and externalizing problem behaviour in children. European Journal of Personality. 2004;18(2):73–102. doi: 10.1002/per.501. [DOI] [Google Scholar]
- Roberts BW, DelVecchio WF. The rank-order consistency of personality traits from childhood to old age: a quantitative review of longitudinal studies. Psychological Bulletin. 2000;126(1):3–25. doi: 10.1037//0033-2909.126.1.3. [DOI] [PubMed] [Google Scholar]
- Roberts BW, Walton KE, Viechtbauer W. Patterns of mean-level change in personality traits across the life course: a meta-analysis of longitudinal studies. Psychological Bulletin. 2006;132(1):1–25. doi: 10.1037/0033-2909.132.1.1. [DOI] [PubMed] [Google Scholar]
- Rubin DB. Multiple imputation after 18+ years. Journal of the American Statistical Association. 1996;91(434):473–489. doi: 10.2307/2291635. [DOI] [Google Scholar]
- Steinhausen HC, Gollner J, Brandeis D, Muller UC, Valko L, Drechsler R. Psychopathology and personality in parents of children with ADHD. Journal of Attentional Disorders. 2013;17(1):38–46. doi: 10.1177/1087054711427562. [DOI] [PubMed] [Google Scholar]
- Theule J, Wiener J, Rogers MA, Marton I. Predicting parenting stress in families of children with ADHD: parent and contextual factors. Journal of Child and Family Studies. 2011;20(5):640–647. doi: 10.1007/s10826-010-9439-7. [DOI] [Google Scholar]
- Theule J, Wiener J, Tannock R, Jenkins JM. Parenting stress in families of children with ADHD: a meta-analysis. Journal of Emotional and Behavioral Disorders. 2013;21(1):3–17. doi: 10.1177/1063426610387433. [DOI] [Google Scholar]
- Trull TJ, Sher KJ. Relationship between the five-factor model of personality and Axis I disorders in a nonclinical sample. Journal of Abnormal Psychology. 1994;103(2):350–360. doi: 10.1037//0021-843X.103.2.350. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA. Negative affectivity: The disposition to experience aversive emotional states. Psychological Bulletin. 1984;96(3):465–490. doi: 10.1037//0033-2909.96.3.465. [DOI] [PubMed] [Google Scholar]
- Weinstein CS, Apfel RJ, Weinstein SR. Description of mothers with ADHD with children with ADHD. Psychiatry. 1998;61(1):12–19. doi: 10.1080/00332747.1998.11024815. [DOI] [PubMed] [Google Scholar]
- Wells KC, Epstein JN, Hinshaw SP, Conners CK, Klaric J, Abikoff HB, … Wigal T. Parenting and family stress treatment outcomes in attention deficit hyperactivity disorder (ADHD): an empirical analysis in the MTA study. Journal of Abnormal Child Psychology. 2000;28(6):543–553. doi: 10.1023/A:1005131131159. [DOI] [PubMed] [Google Scholar]
- Wender PH. O. Press, editor. Attention-deficit hyperactivity disorder in adults. New York: 1995. [DOI] [PubMed] [Google Scholar]