Abstract
Purpose
The increase in use of health information technologies (HIT) presents new opportunities for patient engagement and self-management. Patients in rural areas stand to benefit especially from increased access to health care tools and electronic communication with providers. We assessed the adoption of 4 HIT tools over time by rural or urban residency.
Methods
Analyses were conducted using data from 7 iterations of the National Cancer Institute’s Health Information National Trends Survey (HINTS; 2003–2014). Rural/urban residency was based on the USDA’s 2003 Rural-Urban Continuum Codes. Outcomes of interest included managing personal health information online; whether providers maintain electronic health records (EHRs); e-mailing health care providers; and purchasing medicine online. Bivariate analyses and logistic regression were used to assess relationships between geography and outcomes, controlling for sociodemographic characteristics.
Findings
In total, 6,043 (17.6%, weighted) of the 33,749 respondents across the 7 administrations of HINTS lived in rural areas. Rural participants were less likely to report regular access to Internet (OR = 0.70, 95% CI = 0.61–0.80). Rural respondents were neither more nor less likely to report that their health care providers maintained EHRs than were urban respondents; however, they had decreased odds of managing personal health information online (OR = 0.59, 95% CI = 0.40–0.78) and e-mailing health care providers (OR = 0.62, 95% CI = 0.49–0.77).
Conclusions
The digital divide between rural and urban residents extends to HIT. Additional investigation is needed to determine whether the decreased use of HIT may be due to lack of Internet connectivity or awareness of these tools.
Keywords: access to care, health disparities, health services research, technology, utilization of health services
Internet connectivity is a driving force in innovation and provides access to information through search engines, learning platforms and social media. As we move into a more digitally connected world, we are working to harness the power of Internet connectivity into health information technologies (HIT) to improve access to health care. As a result of the Affordable Care Act and its mandates, patients are now offered access to their electronic health records (EHRs) through online patient portals and, with the advent of telemedicine, are able to communicate with their doctors via email or text messages to help form and monitor treatment plans.1,2 These types of exchanges between patients and their health care providers have been effective in reducing travel time to appointments and long waiting periods.3–5 Most importantly, they have provided efficient and direct access to health information and health care providers. However, studies have shown that, despite efforts to ensure access to Internet resources, some populations remain behind in Internet access, connection quality, and technological literacy, thus creating a digital divide in access to both providers and health information.6,7
Statistics from the National Cancer Institute’s Health Information National Trends Survey (HINTS) show that among US adults, 83% had accessed the Internet in 2014, a dramatic increase of 20% from 2003.8–10 Additional investigations have revealed that there remains a divide in Internet access among racial groups, education levels and age, in spite of this overall progress. Indeed, the digital divide between African Americans, Hispanics, Native Americans, and their white counterparts extends beyond Internet usage to health technologies.11 This digital divide also extends beyond typical sociodemographic characteristics to the types of communities in which Americans reside. According to the 2010 United States Census, roughly 59 million Americans (19.3%) live in rural areas where health care workforce shortages are critical, leading to reduced access to general and specialty health care.12–14 For patients in rural areas, the rise of HIT implementation, including EHRs and their associated patient portals, may be part of the solution for reducing barriers in access to care and communication with health care providers. Unfortunately, Americans residing in rural areas are approximately 2 times less likely to report Internet use than those who live in urban areas.15 Furthermore, two-thirds of rural counties have poverty rates at or above the national average of 14.4%; lower education rates; and an influx of black and Hispanic populations, all adding potential risk for increased disparities in HIT access and health literacy.6,12 In short, these populations are less likely to benefit from the recent advances in HIT and telemedicine due to lack of access to the Internet.
As evidenced by recent policy changes, closing the digital divide has become a priority in the past 15 years. Goals aiming to provide equal access to electronic health across the US population were included in the Healthy People 2010 and Healthy People 2020 objectives, a comprehensive set of health priorities for the nation.16,17 The Obama administration has supported the HIT objectives by investing in network infrastructure, sponsoring high-speed Internet access in classrooms, and providing resources to local and state government for increased Internet connectivity.6 Additional efforts to increase broadband access in rural areas have been supported by the United States Department of Agriculture’s Rural Utilities Service (RUS) program.18 HIT has proven to be beneficial in several communities and holds promise for rural populations; however, only a few studies have examined uptake of HIT tools by rural residents.19–21 Furthermore, a 2015 assessment of Healthy People 2020 in a rural context revealed that access to health care and resources remains the number one challenge for rural residents.22 In this report, we assess the overall rates of utilization of HIT tools by those residing in rural parts of the US and compare these rates with that of urban residents using data from the National Cancer Institute's HINTS program.
Methods
Survey Population and Data Collection
For this study, we utilized data from all 7 administrations of the Health Information National Trends Survey (HINTS), a nationally representative probability-based cross-sectional survey of non-institutionalized adults (18+) in the US. HINTS collects information from the general public on topics including demographics, perceptions and use of health-related information, and attitudes towards and use of health information technologies. Survey administrations occurred periodically between 2003 and 2014 via random digit dialing and mailing. The 7 iterations of HINTS have yielded a total sample of 34,080 respondents. For the telephone random digit dialing administration, response rates were 33% in 2003, 21% in 2005, and 21% in 2008; for mail administration, response rates were 31% in 2008 (dual administration), 37% in 2011, 40% in 2012, 35% in 2013, and 34% in 2014. Respondents to the first 6 administrations tended to be non-Hispanic white, female, higher income, more educated, older, and urban residents. The most recent survey in 2014 oversampled for minorities and individuals living in Appalachia. Additional information about data collection, including sampling frames and weighting methodologies, can be found in the corresponding methodology reports.8,23,24
Categorizing Urbanity
The HINTS dataset includes a variable classifying respondent “urbanity” using the United States Department of Agriculture’s 2003 Rural-Urban Continuum (RUC) Code. Briefly, the RUC code divides respondents into categories based on whether they are in a metro or non-metro county and the population of the county. Additional information regarding RUC codes can be found at http://www.ers.usda.gov/data-products/rural-urban-continuum-codes/.aspx.25 Codes 1–3 representing metro counties with populations of 250,000 or greater make up our urban category; codes 4–9 for non-metro counties, both adjacent and nonadjacent to metro counties, with populations ranging from 2,500–20,000 were included in our rural designation.
Bivariate Analyses of Sociodemographic Characteristics and Geography
Analyses were conducted using SAS-callable SUDAAN 11.0.0 (RTI International, Research Triangle Park, North Carolina), which allows for the incorporation of the jackknife replicate weights to estimate accurate variance estimates for statistical modeling; all analyses were weighted to obtain population estimates. Descriptive and bivariate analyses were conducted for each of the survey items of interest to compare urban and rural populations. Sociodemographic variables examined in relation to these items included age, sex, race/ethnicity, education, income level, and health insurance coverage.
Multivariate Logistic Regression of Utilizing Electronic PHI Tools by Geography
As with the bivariate analyses, multivariate logistic regression was conducted using SAS-callable SUDAAN 11.0.0, allowing the use of jackknife replicate weights to obtain population estimates. To investigate differences in associations and trends in the items of interest by urban and rural status, logistic regression analyses were performed for each of the following outcomes of interest (all with response options of Yes or No):
“Do you ever go on-line to access the Internet or World Wide Web, or to send and receive e-mail?”
“As far as you know, do your health care providers maintain your medical information in a portable, electronic format?”
“In the last 12 months, have you used the Internet for any of the following reasons? Kept track of personal health information such as care received, test results, or upcoming medical appointments?”
“In the last 12 months, have you used e-mail or the Internet to communicate with a doctor or doctor’s office?”
“In the last 12 months, have you bought medicine or vitamins on-line?”
All multivariate logistic regression models controlled for age, sex, race/ethnicity, education, income level, and survey year. As health insurance was not significantly different between urban and rural respondents, it was dropped to create more parsimonious models. Additionally, regular Internet use was 100% correlated with managing protected health information (PHI) online in the past 12 months, emailing a doctor in the past 12 months, and purchasing medicine online in the past 12 months; therefore, the sample was restricted to only individuals who reported having regular Internet access (N=23,024). Interaction terms for geography and survey administration were added to each model to assess differential change over time of administration and calculate predicted marginals.
Results
Associations Between Sociodemographic Characteristics and Geography
Of the respondents, 27,706 (82.4%) were urban residents and 6,043 (17.6%) were rural residents. Although there was variation in the sociodemographic characteristics of respondents to HINTS administrations, the samples were generally representative of the US population. Respondents in the weighted samples tended to be female, aged 34 and older, non-Hispanic white, have some college education, have health insurance, and have higher incomes (Table 1). While Chi-squared tests revealed a significant difference in the number of rural and urban respondents across HINTS administrations, the percentages themselves did not vary greatly.
Table 1.
Sociodemographic and Internet Accessibility by Urban-Rural Classificationa
| Geographic Location n (%) |
|||||
|---|---|---|---|---|---|
| Urban | Rural | Chi-square | P value | ||
| Overall | 27706 | 6043 | |||
| Gender | 3.058 | .081 | |||
| Male | 10674 (48.7%) | 2308 (46.7%) | |||
| Female | 17032 (51.3%) | 3735 (53.3%) | |||
| Age | 14.9316 | < .001 | |||
| 18–34 | 4974 (31.4%) | 831 (24.9%) | |||
| 35–49 | 7142 (29.0%) | 1376 (27.6%) | |||
| 50–64 | 8323 (23.6%) | 1939 (26.6%) | |||
| 65–74 | 3944 (8.7%) | 1040 (11.7%) | |||
| ≥75 | 3112 (7.3%) | 810 (9.1%) | |||
| Race/ethnicity | 118.222 | < .001 | |||
| NH white | 17203 (61.6%) | 4639 (78.7%) | |||
| Hispanic | 3632 (15.1%) | 273 (4.6%) | |||
| NH black | 3427 (11.1%) | 441 (6.5%) | |||
| NH other | 1712 (7.0%) | 250 (4.3%) | |||
| Missing | 1346 (5.2%) | 311 (5.9%) | |||
| Education | 80.33 | < .001 | |||
| Less than high school | 2622 (12.6%) | 820 (16.1%) | |||
| High school graduate | 6139 (23.0%) | 1869 (32.7%) | |||
| Some college | 7939 (32.2%) | 1682 (32.6%) | |||
| College graduate | 10315 (32.3%) | 1481 (18.6%) | |||
| Income | 44.5309 | < .001 | |||
| <$20,000 | 4830 (19.4%) | 1345 (25.5%) | |||
| $20,000 to < $35,000 | 4078 (15.6%) | 1133 (20.3%) | |||
| $35,000 to <$50,000 | 3533 (14.2%) | 805 (17.0%) | |||
| $50,000 to < $75,000 | 4257 (18.1%) | 939 (18.2%) | |||
| $75,000+ | 7205 (32.7%) | 937 (19.0%) | |||
| Health Insurance | 1.58 | .210 | |||
| Yes | 24077 (16.2%) | 5207 (17.5%) | |||
| No | 3290 (83.8%) | 754 (82.5%) | |||
| Regular Internet Access | 106.0 | < .001 | |||
| Yes | 19521 (75.4%) | 3503 (65.0%) | |||
| No | 8378 (24.6%) | 2559 (35.0%) | |||
| HINTS Administration | 4.749 | < .001 | |||
| 2003 (HINTS 1) | 5174 (12.9%) | 1195 (14.3%) | |||
| 2005 (HINTS 2) | 4352 (13.2%) | 1234 (15.4%) | |||
| 2008 (HINTS 3) | 6192 (14.1%) | 1482 (14.3%) | |||
| 2011 (HINTS 4 Cycle 1) | 3321 (15.0%) | 638 (13.3%) | |||
| 2012 (HINTS 4 Cycle 2) | 3087 (15.1%) | 543 (13.8%) | |||
| 2013(HINTS 4 Cycle 3) | 2709 (14.7%) | 476 (15.0%) | |||
| 2014 (HINTS 4 Cycle 4) | 3157 (15.1%) | 520 (113.9%) | |||
Based on respondents to the Health Information National Trends Survey (HINTS) across all 7 HINTS administrations (2003–2014). Column percentages are weighted to reflect the US population per the 2010 US Census (see Methods for additional details).
Significant differences were found by age, race/ethnicity, education, and income by geography. There tended to be a higher percentage of older respondents in rural areas compared to urban areas; similarly, there was a higher percentage of non-Hispanic white rural respondents compared to non-Hispanic white urban respondents (Table 1). Of those respondents living in rural areas, there was a significantly lower percentage with at least some college education or higher (51.2%) as compared to respondents in urban areas (64.5%). Of those living in urban areas, 50.8% reported an annual income of $50,000 or greater, compared to 37.2% of rural respondents. Additionally, a significant difference was found in the percentage of respondents reporting regular Internet access between urban and rural areas (75.4% vs 65.0%, respectively). No significant difference was found in the number of respondents reporting having health insurance coverage (Table 1).
Assessing Differences in Probability of Utilizing Electronic PHI Tools by Geography
We then conducted multivariable binomial logistic regression analyses on our outcomes of interest using model selection techniques (including Hosmer-Lemeshow and Akaike’s Information Criterion). All dependent variables were analyzed with urban/rural status, age, sex, race/ethnicity, education, income, Internet use, and health insurance status as independent variables (see Appendix Supplementary Tables 1–5, available online only).
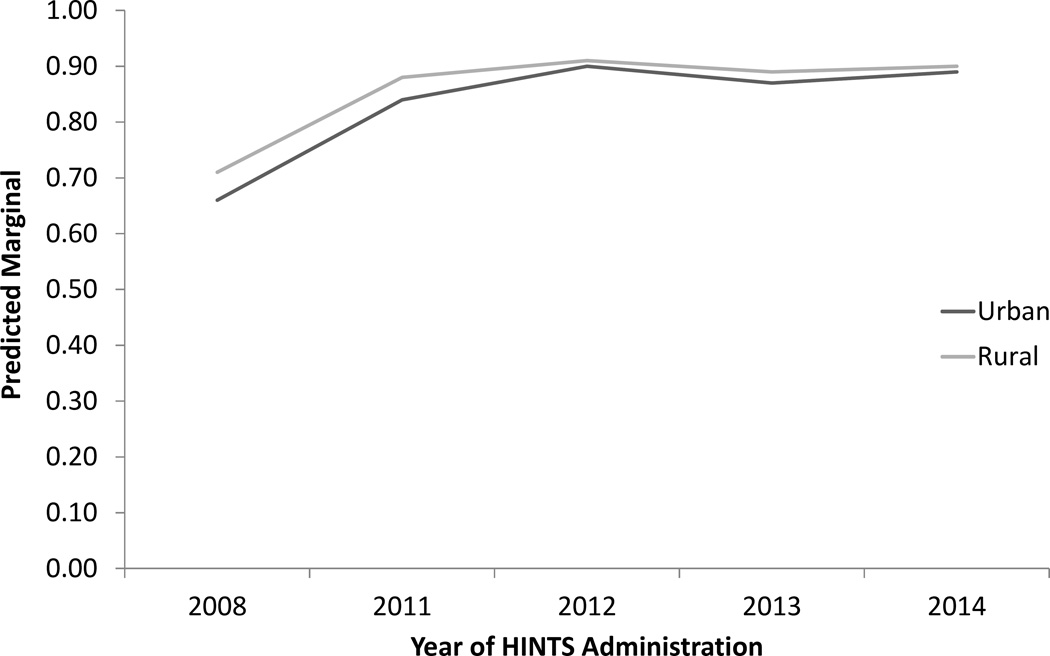
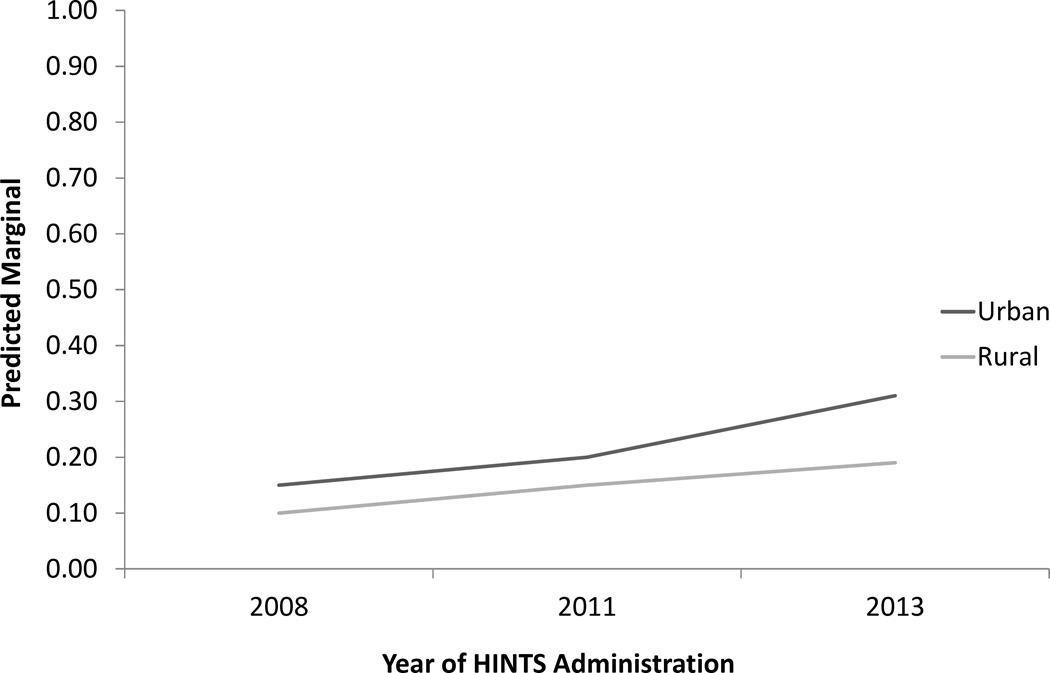
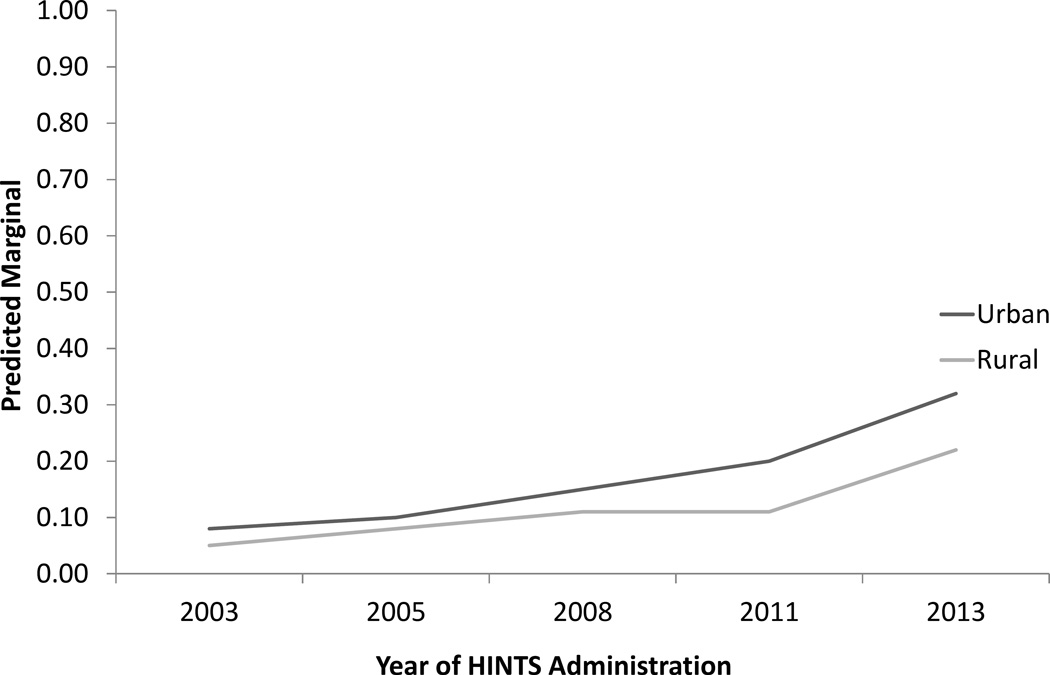
Analyses revealed that individuals who reside in rural areas have significantly lower odds of having regular Internet access or use (OR = 0.70, 95% CI = 0.61–0.80; Table 2; Figure 1). Rural respondents are neither more nor less likely to report that their provider maintained EHRs compared to urban respondents (OR = 1.23, 95% CI = 0.98–1.58; Table 2; Supplemental Table 2; Figure 2). However, rural respondents who reported having regular Internet access had significantly lower odds of having managed either PHI online in the past 12 months (OR = 0.59, 95% CI = 0.45–0.78; Table 2; Figure 3) and of having emailed a doctor in the past 12 months (OR = 0.62, 95% CI = 0.49–0.77; Table 2; Figure 4) compared to their urban counterparts with regular Internet access. No significant difference was found in odds of whether a respondent ordered medicine or vitamins online in the past 12 months (Table 2). Increases in uptake of these tools were seen across all HINTS administration years, with rural participants generally lagging behind urban participants in adoption, but still increasing (Figures 1–4). No significant interactions were observed between rural/urban residency and survey year in any of the models examined, indicating that there was no change in survey response over time by geography.
Table 2.
Results of Logistic Regression Models of Use of Online HIT and Tools by Rural vs Urban Respondents to the Health Information National Trends Surveya
| HINTS Administrations |
Odds Ratio (95% CI) |
Beta coefficient |
SE Beta |
Adj Wald F |
P value | |
|---|---|---|---|---|---|---|
| Regular Internet access |
All (2003, 2005, 2008, 2011–2014) |
0.70 (0.61–0.80) |
−0.36 | 0.07 | 25.70 | < .001 |
| Provider maintains EHRs |
2008, 2011–2014 | 1.25 (0.98–1.58) |
0.22 | 0.12 | 3.25 | .072 |
| Managed PHI online in past 12 months |
2008, 2011, 2013 | 0.59 (0.45–0.78) |
−0.53 | 0.14 | 14.01 | < .001 |
| E-mailed doctor in the past 12 months |
2003, 2005, 2008, 2011, 2013 |
0.62 (0.49–0.77) |
−0.48 | 0.12 | 17.41 | < .001 |
| Bought medicine online in the past 12 months |
2003, 2005, 2008, 2011, 2013 |
0.95 (0.75–1.22) |
−0.05 | 0.12 | 0.14 | .706 |
Weighted using data from the 2010 United States Census and controlling for age category, sex, race/ethnicity, education, income, and survey year. Years each item was included in the survey are included. For full models, see Supplementary Tables 1–5.
Figure 1.
Predicted marginals of having regular Internet access by urban-rural categorization across the 7 administrations of the Health Information National Trends Survey (HINTS) from 2003–2014, weighted to data from the 2010 US Census and controlling for age, sex, race/ethnicity, education, income level, and survey year.
Figure 2.
Predicted marginals of reporting that health care providers maintained electronic health records by urban-rural categorization across 5 administrations of the Health Information National Trends Survey (HINTS) from 2008–2014, weighted to data from the 2010 US Census and controlling for age, sex, race/ethnicity, education, income level, and survey year.
Figure 3.
Predicted marginals of having managed personal health information online in the past 12 months by urban-rural categorization across 3 administrations of the Health Information National Trends Survey (HINTS) from 2008–2014, weighted to data from the 2010 US Census and controlling for age, sex, race/ethnicity, education, income level, and survey year.
Figure 4.
Predicted marginals of having emailed a health care provider in the past 12 months by urban-rural categorization across 5 administrations of the Health Information National Trends Survey (HINTS) from 2003–2013, weighted to data from the 2010 US Census and controlling for age, sex, race/ethnicity, education, income level, and survey year.
Discussion
The digital divide, often characterized by race, education, and income, includes unequal access by geography, notably by rural versus urban residence.6,11,20,26 To determine whether the digital divide extends to and impacts use of HIT tools by rural residents compared to urban residents, we analyzed data from a nationally representative sample of non-institutionalized Americans aged 18 and older. Our results showed a significant difference in emailing doctors and managing PHI online for rural residents versus urban. These results point to a delayed adoption of certain HIT tools, likely due to the lag in Internet access and literacy for rural communities.10,27
Analysis of our sample revealed that individuals residing in rural areas generally had lower levels of education. No difference, however, was seen in the proportion of those reporting having health insurance; this is in contrast with a report from the Kaiser Family Foundation, which found that there are higher rates of uninsured patients in rural areas, as two-thirds of rural individuals live in states which are not expanding Medicaid.28 We hypothesize that this lack of difference in our sample may be a function of self-selection of respondents (ie, those with health insurance may have been more likely to respond to a health-related survey than those without).28–30 Consistent with existing literature, regular access to Internet was lower among rural residents compared to urban residents.7,15 While uptake of Internet use has increased dramatically in both settings, our data support the conclusion that this disparity persists, even after adjusting for relevant sociodemographic characteristics.
Our findings revealed that respondents living in rural areas were neither more nor less likely to report that their providers maintain EHRs compared to urban respondents. Recent reports from the Office of the National Coordinator for Health Information Technology, among others, have stated that there is a similar rate of uptake and implementation of EHRs in rural and urban health care settings.31 Despite the similar levels of implementation and the greater awareness of use of the HIT tools among rural and urban patients, however, those residing in rural areas in our study had significantly lower odds of e-mailing a health care provider or managing their PHI online. Furthermore, only respondents reporting regular Internet access had ever engaged with any of these tools. No difference was seen in the rates of rural and urban residents in ordering medication online.
Collectively these data suggest that, while there is a high level of implementation of these tools by health care providers in rural areas of the US, there is a distinct need for targeted interventions to increase Internet access for rural patients to be able to reap the benefits of their providers’ forward-thinking nature. A few states and regions of Canada with high proportions of rural residents have piloted interventions using telehealth to bridge the access gaps in care for rural areas; however, few interventions have focused on increasing the use of electronic health records and personal health information management online in these populations.3,4,32
When examining trends over time, we observed that the percentages of managing PHI online and emailing a health care provider were very similar between urban and rural populations in 2008. After that time, overall utilization began to increase more rapidly; however, rural populations began to lag in uptake, with the gap increasing through the last administration of HINTS in 2014. These findings are consistent with results in a previous publication, which examined these items using only data from the 2008 administration (HINTS 3) and found low overall utilization and no significant difference in use of these technologies by geography.10 The authors hypothesized that the low use was due to lack of institutional support for these HIT tools. We, in turn, hypothesize that the overall increase in use of these technologies since 2010 may be a result of the implementation of the US government’s Health Information Technology for Economic and Clinical Health (HITECH) Act and the Centers for Medicare and Medicaid Services’ Meaningful Use program, and that the difference in use of these tools between rural and urban populations may be attributable to differences in Internet access.33,34 A recent study conducted by analysts at the Office of the National Coordinator for Health Information Technology supports this hypothesis, as it revealed that adoption of HIT by rural providers is greater than or equal to that of their urban counterparts, but that the rates of meaningful use attestation may be lower among rural providers than among urban ones.35
Additionally, mobile technologies have the potential to serve as an additional avenue for increasing access to HIT tools and online PHI. According to the Pew Research Center, 87% of rural residents own a cell phone; of these, approximately half use their cell phone to access the Internet.36,37 While several interventions have successfully used mobile devices to support rural health care providers, investigators and care providers are only beginning to create technologies that specifically target rural residents who own mobile devices.38,39 Nonetheless, we propose that there is potential for targeted implementation of mHealth technologies among rural communities to help patients in these locations manage their care. One example of such an intervention is body sensors and monitoring using mobile devices to allow for improved self-management of blood pressure, falls, and diabetes.40,41 Another is in teledermatology, in which a patient can photograph a lesion and receive clinical feedback from a primary care provider; this is already being piloted in South Dakota.42 While uptake of these interventions on a broader scale will require additional study, similar methods and HIT tools have been shown to be highly successful in rural areas worldwide, such as Ethiopia, Uganda, and Zambia.43–46
One of the major strengths of this investigation is in the use of a large, multi-year, nationally representative sample of US adults to examine differences in use of HIT tools by whether respondents lived in rural or urban areas. This is the first study we are aware of that examines differences in uptake of these technologies in this manner and across time. Limitations of this investigation are those often associated with cross-sectional surveys, including low response rates and inability to infer causation. Additionally, the outcomes examined do not include follow-up questions regarding what type of PHI or online tools were used, which provider was emailed, and frequency of use. Finally, because we used HINTS data dating back to 2003, we were unable to analyze all cycles using the updated Rural-Urban Continuum codes from 2013, and therefore we had to apply the 2003 definitions to all HINTS administrations for consistency.
Conclusion
In the present investigation, we sought to determine whether there are differences in use of various forms of HIT between rural and urban residents in a national probability sample of adults in the US. Although our results demonstrate that there is a significant difference in utilization of different forms of HIT tools between the 2 populations, there are several other components which play an important role in Internet access and utilization of HIT which we were unable to explore due to limitations of secondary analysis of these data. Interventions targeted towards increasing access to, awareness of, and use of these tools in rural areas has great potential to not only improve the care delivered to these individuals but also to increase patients’ self-efficacy with regard to taking care of their own health. Future investigations should focus on these interventions as well as whether implementation of these tools in rural areas affects clinical and patient-reported outcomes.
Supplementary Material
Acknowledgments
Funding: Dr. Greenberg was funded by the National Cancer Institute (intramural), Contract Number HHSN261201600107M.
Footnotes
Disclosures: The authors report no disclosures.
References
- 1.Hayrinen K, Saranto K, Nykanen P. Definition, structure, content, use and impacts of electronic health records: a review of the research literature. Int J Med Inform. 2008;77(5):291–304. doi: 10.1016/j.ijmedinf.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 2.The Affordable Care Act, Section by Section. [Accessed Aug 25, 2016];2010 Available at: http://www.hhs.gov/healthcare/about-the-law/read-the-law/#.
- 3.O'Gorman LD, Hogenbirk JC. Driving Distance to Telemedicine Units in Northern Ontario as a Measure of Potential Access to Healthcare. Telemed J E Health. 2016;22(4):269–275. doi: 10.1089/tmj.2015.0133. [DOI] [PubMed] [Google Scholar]
- 4.Meyers L, Gibbs D, Thacker M, Lafile L. Building a telehealth network through collaboration: the story of the Nebraska statewide telehealth network. Crit Care Nurs Q. 2012;35(4):346–352. doi: 10.1097/CNQ.0b013e318266bed1. [DOI] [PubMed] [Google Scholar]
- 5.Wade VA, Karnon J, Elshaug AG, Hiller JE. A systematic review of economic analyses of telehealth services using real time video communication. BMC Health Serv Res. 2010;10:233. doi: 10.1186/1472-6963-10-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mapping the Digital Divide [press release] Washington, DC: White House Council of Economic Advisers Issue Brief; 2015. Jul 1, [Accessed August 25, 2015]. Available at: https://www.whitehouse.gov/sites/default/files/wh_digital_divide_issue_brief.pdf. [Google Scholar]
- 7.Horrigan JB, Duggan M. Home Broadband 2015. Washington, DC: Pew Research Center; 2015. Dec 21, [Google Scholar]
- 8.Nelson DE, Kreps GL, Hesse BW, et al. The Health Information National Trends Survey (HINTS): development, design, and dissemination. J Health Commun. 2004;9(5):443–460. doi: 10.1080/10810730490504233. [DOI] [PubMed] [Google Scholar]
- 9.Hesse BW, Greenberg AJ, Rutten LJ. The role of Internet resources in clinical oncology: promises and challenges. Nat Rev Clin Oncol. 2016:767–776. doi: 10.1038/nrclinonc.2016.78. [epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 10.Lustria MLA, Smith SA, Hinnant CC. Exploring digital divides: An examination of eHealth technology use in health information seeking, communication and personal health information management in the USA. Health Informatics Journal. 2011;17(3):224–243. doi: 10.1177/1460458211414843. [DOI] [PubMed] [Google Scholar]
- 11.Chang BL, Bakken S, Brown SS, et al. Bridging the digital divide: reaching vulnerable populations. J Am Med Inform Assoc. 2004;11(6):448–457. doi: 10.1197/jamia.M1535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Census U. 2010 Census Data. [Accessed August 1, 2016]; Available at: http://www.census.gov/2010census/data/
- 13.Marcin JP, Shaikh U, Steinhorn RH. Addressing health disparities in rural communities using telehealth. Pediatr Res. 2016;79(1–2):169–176. doi: 10.1038/pr.2015.192. [DOI] [PubMed] [Google Scholar]
- 14.Douthit N, Kiv S, Dwolatzky T, Biswas S. Exposing some important barriers to health care access in the rural USA. Public Health. 2016;129(6):611–620. doi: 10.1016/j.puhe.2015.04.001. [DOI] [PubMed] [Google Scholar]
- 15.Anderson M, Perrin A. FactTank: News in the Numbers. Vol. 2016. Washington, DC: Pew Research Center; 2015. 15% of Americans don’t use the internet. Who are they? [Google Scholar]
- 16.Hesse BW, Gaysynsky A, Ottenbacher A, et al. Meeting the healthy people 2020 goals: using the Health Information National Trends Survey to monitor progress on health communication objectives. J Health Commun. 2014;19(12):1497–1509. doi: 10.1080/10810730.2014.954084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.U.S. Department of Health and Human Services OoDPaHP. [Accessed August 1, 2016];Healthy People. 2020 Available at: http://www.healthypeople.gov/2020/topics-objectives/topic/health-communication-and-health-information-technology.
- 18.United States Department of Agriculture Rural Development. [Accessed August 1, 2016];Rural Utilities Service. 2016 Available at: https://www.rd.usda.gov/about-rd/agencies/rural-utilities-service.
- 19.Bhuyan SS, Lu N, Chandak A, et al. Use of Mobile Health Applications for Health-Seeking Behavior Among US Adults. J Med Syst. 2016;40(6):153. doi: 10.1007/s10916-016-0492-7. [DOI] [PubMed] [Google Scholar]
- 20.Wang JY, Bennett K, Probst J. Subdividing the digital divide: differences in internet access and use among rural residents with medical limitations. J Med Internet Res. 2011;13(1):e25. doi: 10.2196/jmir.1534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shane-McWhorter L, Lenert L, Petersen M, et al. The Utah Remote Monitoring Project: improving health care one patient at a time. Diabetes Technol Ther. 2014;16(10):653–660. doi: 10.1089/dia.2014.0045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bolin JN, Bellamy GR, Ferdinand AO, et al. Rural Healthy People 2020: New Decade, Same Challenges. J Rural Health. 2015;31(3):326–333. doi: 10.1111/jrh.12116. [DOI] [PubMed] [Google Scholar]
- 23.Westat. Health Information National Trends Survey 4 (HINTS 4): Cycle 4 Methodology Report. [Accessed August 25, 2015];2015 Available at: http://hints.cancer.gov/docs/HINTS_4_Cycle_4_Methodology_Report.pdf.
- 24.Rutten LJF, Davis T, Beckjord EB, Blake K, Moser RP, Hesse BW. Picking up the pace: changes in method and frame for the Health Information National Trends Survey (2011–2014) J Health Commun. 2012;17(8):979–989. doi: 10.1080/10810730.2012.700998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Parker T. Rural-Urban Continuum Codes Documentation. [Accessed August 1, 2016];2013 Available at: http://www.ers.usda.gov/data-products/rural-urban-continuum-codes/documentation.aspx.
- 26.Brodie M, Flournoy RE, Altman DE, Blendon RJ, Benson JM, Rosenbaum MD. Health information, the Internet, and the digital divide. Health Affairs. 2000;19(6):255–265. doi: 10.1377/hlthaff.19.6.255. [DOI] [PubMed] [Google Scholar]
- 27.Zahnd WE, Scaife SL, Francis ML. Health literacy skills in rural and urban populations. Am J Health Behav. 2009;33(5):550–557. doi: 10.5993/ajhb.33.5.8. [DOI] [PubMed] [Google Scholar]
- 28.II VRN, Damico A. The Affordable Care Act and Insurance Coverage in Rural Areas. Menlo Park, CA: Kaiser Family Foundation; 2014. May, [Google Scholar]
- 29.Lu N, Samuels ME, Kletke PR, Whitler ET. Rural-urban differences in health insurance coverage and patterns among working-age adults in Kentucky. J Rural Health. 2010;26(2):129–138. doi: 10.1111/j.1748-0361.2010.00274.x. [DOI] [PubMed] [Google Scholar]
- 30.Services USDoHaH. Washington, DC: U. S. Department of Health and Human Services; 2013. Sep 20, The Affordable Care Act -- What it means for rural america. [Google Scholar]
- 31.Technology OotNCfHI. Health IT Quick-State #5: Hospital Progress to Meaningful Use by Size, Type, and Urban/Rural Location. [Accessed August 1, 2016];2016 Available at: dashboard.healthit.gov/quickstats/pages/FIG-Hospital-Progress-to-Meaningful-Use-by-size-practice-setting-area-type.php.
- 32.O'Gorman LD, Hogenbirk JC, Warry W. Clinical Telemedicine Utilization in Ontario over the Ontario Telemedicine Network. Telemed J E Health. 2015;22(6):473–479. doi: 10.1089/tmj.2015.0166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Select Portions of the HITECH Act and Relationship to ONC Work. [Accessed August 11, 2016];Health IT Legislation. 2015 Available at: https://www.healthit.gov/policy-researchers-implementers/select-portions-hitech-act-and-relationship-onc-work.
- 34.Meaningful Use Definition & Objectives. [Accessed August 11, 2016];EHR Incentives and Certification. 2015 Available at: https://www.healthit.gov/providers-professionals/meaningful-use-definition-objectives.
- 35.Heisey-Grove DM. Variation In Rural Health Information Technology Adoption And Use. Health Aff. 2016;35(2):365–370. doi: 10.1377/hlthaff.2015.0861. [DOI] [PubMed] [Google Scholar]
- 36.Anderson M. The Demographics of Device Ownership. [Accessed August 1, 2016];Technology Device Ownership: 2015. 2015 Available at: http://www.pewinternet.org/2015/10/29/the-demographics-of-device-ownership/. [Google Scholar]
- 37.Duggan M, Smith A. Cell Internet Use 2013: Main Findings. [Accessed August 5, 2016];2013 Available at: http://www.pewinternet.org/2013/09/16/main-findings-2/. [Google Scholar]
- 38.Cook SE, Palmer LC, Shuler FD. Smartphone Mobile Applications to Enhance Diagnosis of Skin Cancer: A Guide for the Rural Practitioner. W V Med J. 2015;111(5):22–28. [PubMed] [Google Scholar]
- 39.Carter-Templeton HD, Wu L. Using Mobile Technologies to Access Evidence-Based Resources: A Rural Health Clinic Experience. Nurs Clin North Am. 2015;50(3):595–603. doi: 10.1016/j.cnur.2015.05.012. [DOI] [PubMed] [Google Scholar]
- 40.Panicker NV, Kumar AS. Tablet PC Enabled Body Sensor System for Rural Telehealth Applications. Int J Telemed Appl. 2016 doi: 10.1155/2016/5747961. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wood FG, Alley E, Baer S, Johnson R. Interactive Multimedia Tailored to Improve Diabetes Self-Management. Nurs Clin North Am. 2015;50(3):565–576. doi: 10.1016/j.cnur.2015.05.009. [DOI] [PubMed] [Google Scholar]
- 42.Gaster EE, Chabra I, Burrish GF. Smartphones Enable Teledermatology in South Dakota: An Overview and Primer for Primary Care Providers. S D Med. 2015;68(10):449–453. 455. [PubMed] [Google Scholar]
- 43.Siedner MJ, Santorino D, Lankowski AJ, et al. A combination SMS and transportation reimbursement intervention to improve HIV care following abnormal CD4 test results in rural Uganda: a prospective observational cohort study. BMC Med. 2015;13:160. doi: 10.1186/s12916-015-0397-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kim J, Zhang W, Nyonyitono M, et al. Feasibility and acceptability of mobile phone short message service as a support for patients receiving antiretroviral therapy in rural Uganda: a cross-sectional study. J Int AIDS Soc. 2015;18(20311) doi: 10.7448/IAS.18.1.20311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Medhanjie AA, Moser A, Spigt M, et al. Mobile health data collection at primary health care in Ethiopia: a feasible challenge. J Clin Epidemiol. 2015;68(1):80–86. doi: 10.1016/j.jclinepi.2014.09.006. [DOI] [PubMed] [Google Scholar]
- 46.Schuttner L, Sindano N, Theis M, et al. A mobile phone-based, community health worker program for referral, follow-up, and service outreach in rural Zambia: outcomes and overview. Telemed J E Health. 2014;20(8):721–728. doi: 10.1089/tmj.2013.0240. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.