Abstract
Background:
Studies have confirmed that breast reconstruction is beneficial to improve health-related quality of life (HR-QoL) in breast cancer patients. Our aim was to compare 4 different methods of breast reconstruction on patient satisfaction and HR-QoL using both general and specific patient-reported outcome instruments.
Methods:
Retrospectively, 459 patients who underwent breast reconstruction with a deep inferior epigastric artery perforator (DIEP) flap, latissimus dorsi flap, lateral thoracodorsal flap, or expander with secondary implant and who had responded to the questionnaires were enrolled. Questionnaire answers, together with demographic and follow-up data, were statistically analyzed and compared between groups. Short-Form 36 Health Survey (SF-36) results were also compared with those from a sample of 930 age-matched women from the Swedish population.
Results:
There were slight differences in the SF-36 results but no significant differences in Psychological General Well-Being Index and EuroQoL-5 Dimension Questionnaire results between groups. Analysis of Breast-Q showed that the DIEP group had significantly higher score on the scale satisfaction with breast, significantly higher score in satisfaction with outcome than the lateral thoracodorsal flap (P = 0.014) and EXP groups (P = 0.024). There were no significant differences in most of the domains of the HR-QoL instruments. The higher satisfaction with breasts and outcome in the DIEP group is interesting, considering the higher complication rates associated with this reconstruction method.
Conclusions:
Patients who underwent breast reconstruction with a DIEP flap were more satisfied with their reconstructed breast and outcome than the other 3 groups. Breast reconstruction centers should make DIEP reconstruction widely available to patients after mastectomy.
BACKGROUND
It is widely accepted that breast reconstruction after breast cancer provides benefits to the patient including increased self-esteem and health-related quality of life (HR-QoL) compared with no reconstruction at all.1–4 However, there are insufficient studies on how the choice of method influences the outcomes of HR-QoL and patient satisfaction. As the principal aim of breast reconstruction is to correct the mastectomy deformity and restore body image and HR-QoL, traditional clinical outcome measures, such as medical or surgical complications, are insufficient in assessing the value of different reconstruction methods for the patient. Currently, there are no guidelines on choosing the best reconstruction method for each individual patient. However, patient satisfaction is important when choosing a reconstruction method, and HR-QoL needs to be investigated in a systematic way when comparing different reconstruction methods.
It is well established that postoperative complications can affect patient satisfaction negatively,5–9 even if this is not seen unanimously.10 Complications are shown to cause anxiety and depressive symptoms and lead to worse health outcomes.7
There are several instruments for measuring HR-QoL, including generic and specific instruments.11 The generic instruments, such as the Short-Form 36 Health Survey (SF-36) and EuroQoL-5 Dimension Questionnaire (EQ-5D), are aimed at a wide range of patients, intended to be relevant to the general population, and have been used for numerous years.12,13 The specific instruments are oriented toward a specific disease or treatment.14–16 The Psychological General Well-Being Index (PGWB) is a validated HR-QoL instrument addressing psychological symptoms.17 A Swedish version of this instrument has been developed.18 It has the following 6 subscales: anxiety, depressed mood, positive well-being, self-control, general health, and vitality. The Breast-Q is also a well-validated, specific patient-reported outcome measure, developed to evaluate HR-QoL and patient satisfaction in women treated with various kinds of breast surgery.19 It has been translated and adapted to Swedish cultural conditions according to MAPI guidelines.20 In a short period of time after development, the Breast-Q has become an accepted instrument to evaluate patient-reported outcomes after breast reconstruction. It is constructed based on the 2 underlying themes: HR-QoL and patient satisfaction. These themes are further broken down into the subthemes of physical, psychosocial, and sexual well-being, satisfaction with care, satisfaction with breasts, and satisfaction with overall outcome.21 The Breast-Q questionnaire scales are developed from these subthemes and address the most important issues to the patients in question.19
The aim of this study was to compare patient satisfaction and quality of life between the following 4 different surgical methods: the deep inferior epigastric artery perforator (DIEP) flap,22 the latissimus dorsi (LD) flap, all with silicone implant,23 the lateral thoracodorsal flap (LTDF), all with silicone implant,24 and expander with secondary implant (EXP) in 2 stages,25 using the SF-36, EQ-5D, PGWB, and the postoperative reconstruction module of Breast-Q.
MATERIALS AND METHODS
Patients
The present study is a retrospective study of 459 consecutive patients previously treated with unilateral mastectomy for breast cancer and that had undergone delayed unilateral breast reconstruction between 2003 and 2009 at the Department of Plastic Surgery, Sahlgrenska University Hospital, Gothenburg, Sweden. Patients were enrolled from the operation database of the clinic, Operätt (C&S Healthcare Software AB, Mölndal, Sweden).
The inclusion criteria were delayed breast reconstruction with DIEP, LD, LTDF, or EXP, a minimum 30-day follow-up, and providing responses to the HR-QoL questionnaires. The exclusion criteria were ongoing treatment, data from follow-up time spanning less than 30 days, nonresponse to the HR-QoL questionnaires, inability to answer questionnaires due to language barriers, or if the patient was deceased or had emigrated and could not be reached. Data were kept in a secure FileMaker database (Filemaker Inc., Santa Clara, Calif.). This work conforms to the Declaration of Helsinki.
Data Collection
Demographic parameters extracted from the database for response analysis were as follows: method of reconstruction, body mass index (BMI), age at the time of surgery, follow-up time in months from first referral to last follow-up visit, scores of the American Society of Anesthesiologists (ASA) physical status classification system,26 history of smoking, chemotherapy, radiotherapy, early and late complications, and early and late resurgery rate.
Questionnaires
In 2012, the questionnaires were distributed with an envelope for return, explanatory letter, and instructions to all patients who had undergone breast reconstruction during the study period. To increase response rates, a reminder letter with the same questionnaires and response envelope was sent to the nonresponders about 6 weeks after the first distribution.
Scores from the SF-36, EQ-5D, and PGWB questionnaires were calculated according to their respective manuals.17,27,28 The responses from SF-36 were compared with a group of 930 age-matched controls from a normal Swedish population of women. Raw data from the Breast-Q questionnaire was converted using the Q-score software into a summary score for each scale, ranging from 0 to 100, which corresponded to “very dissatisfied” (0) and “very satisfied” (100)21; the software constructs scores using the individual answers from each patient.19,29–31
Statistical Analysis
The questionnaire answers were compared between the 4 surgical methods as independent variables. The demographic variables for the 4 groups of surgical methods were also compared between responders and nonresponders as independent variables to evaluate representativity of the responders.
Statistical analyses were performed using SPSS (IBM, Armonk, N.Y.). The normality of the distribution was tested with Kolmogorov–Smirnov’s test. None of the demographic variables and questionnaire answers were normally distributed; therefore, the Kruskal–Wallis test with post hoc pairwise comparisons and adjustment of significance levels was used for these factors. For response analysis, the Mann-Whitney U test was applied for continuous variables, and chi-square test was used for dichotomous variables (history of smoking, chemotherapy, radiotherapy, early and late complications, and need for resurgery).
The results of the comparison between groups on response analysis are presented with median, minimum, and maximum values. P values less than 0.05 were considered statistically significant.
Approval from the Gothenburg Ethical Committee was obtained before the study was initiated (No. 043-08).
RESULTS
Patient Selection
Figure 1 shows the patient selection for the study. Six hundred eighty-five patients were identified as having reconstruction with DIEP, LD, LTDF, or EXP and existing follow-up data for at least 30 days. Three hundred forty-one patients were excluded according to the exclusion criteria. A total of 459 patients responded to the questionnaires (67.0%) with no significant differences between the surgical methods (P = 0.338).
Fig. 1.
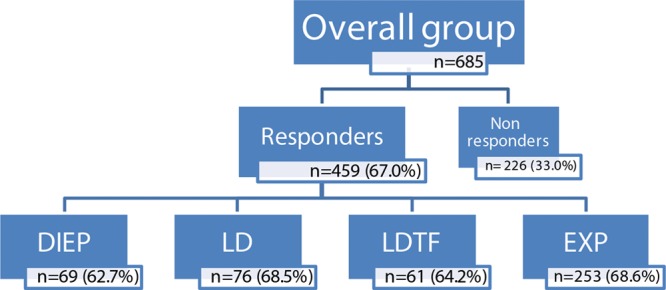
Patient selection and rates of response to HR-QoL questionnaires by surgical method. A flowchart of patient selection and response rate to HR-QoL questionnaires by surgical method.
Demographic parameters for the study groups are displayed in Table 1.
Table 1.
Demography of Study Groups
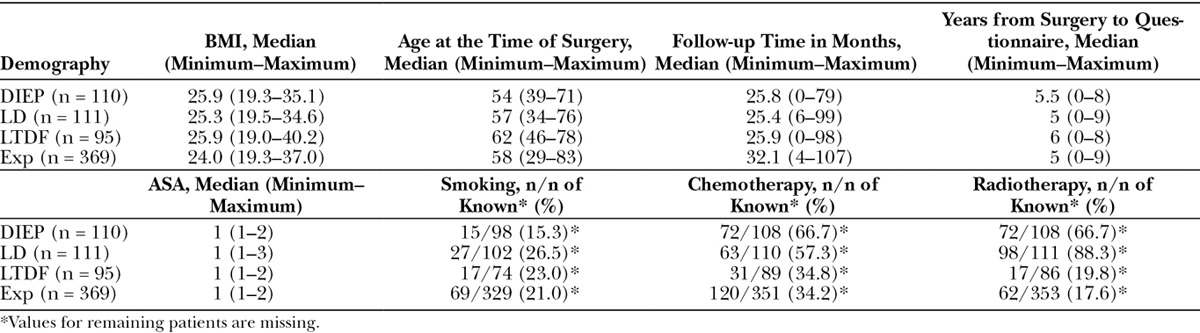
SF-36 Results between Groups
The SF-36 questionnaire results were compared by reconstruction method (Fig. 2). There were significant differences between groups in the vitality domain, where patients in the DIEP group had a lower score than those who received LTDF (P = 0.019) and EXP (P = 0.022).
Fig. 2.
Results of the SF-36 questionnaire by surgical method. Brackets indicate statistically significant differences, and the color of the brackets indicates which group has the higher score.
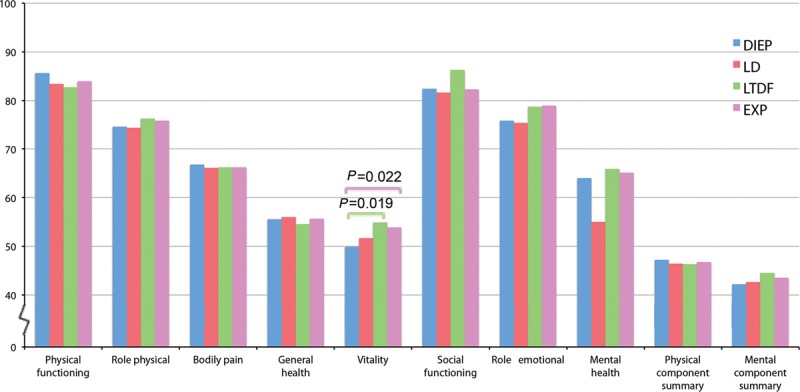
SF-36 Comparison of Overall Group with Normal Population
Figure 3 displays the results from the comparison between the overall study group (all methods) and 930 age-matched women from the normal Swedish population. Patients in the study group had a significantly higher score in the domain of physical functioning (P < 0.001). The age-matched normal population had higher scores in the domains of general health (P < 0.001), vitality (P < 0.001), social functioning (P = 0.013), mental health (P < 0.001), and the mental component summary (P < 0.001).
Fig. 3.
Comparison of study group compared with age-matched normal population of 930 Swedish women.
SF-36—Comparison with Normal Population—Each Reconstruction Method
When each subgroup of the 4 reconstruction methods was compared with the normal population, all methods had significantly lower scores in the domains of general health, vitality, mental health, and the mental component summary (all P values < 0.001).
The DIEP group had a significantly higher score in the domain of physical functioning (P < 0.041) than the normal population. The difference was not statistically significant among the other 3 groups.
EQ-5D—Comparison between Groups
There were no significant differences between the subgroups of the 4 reconstruction methods, neither in among the descriptive items nor the visual analog scale.
PGWB—Comparison between Groups
There were no significant differences in the Global score between the subgroups of the 4 reconstruction methods. There also were no significant differences between the subgroups in each of the domains of anxiety, depressed mood, positive well-being, self-control, general health, and vitality.
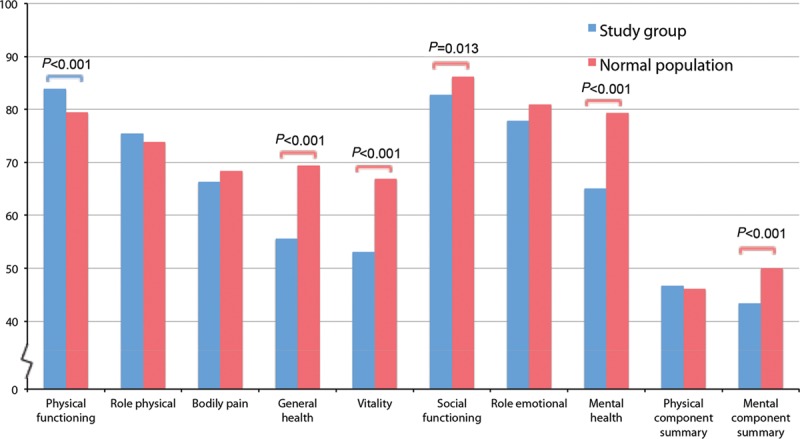
Breast-Q—Comparison between Groups
There were significant differences between the groups regarding the Breast-Q scale of satisfaction with breasts (P < 0.001). The DIEP group had a higher score compared with that of the other groups (compared with LD, P = 0.017; LTDF, P < 0.001; and EXP, P < 0.001). Regarding the scale of satisfaction with outcome, the DIEP group also had a higher score compared with that of the LTDF (P = 0.014) and EXP (P = 0.024) groups. There were no significant differences between the groups regarding the Breast-Q scales on psychosocial well-being, sexual well-being, physical well-being chest, satisfaction with nipples, satisfaction with information, satisfaction with surgeon, satisfaction with medical staff, or satisfaction with office staff (Fig. 4).
Fig. 4.
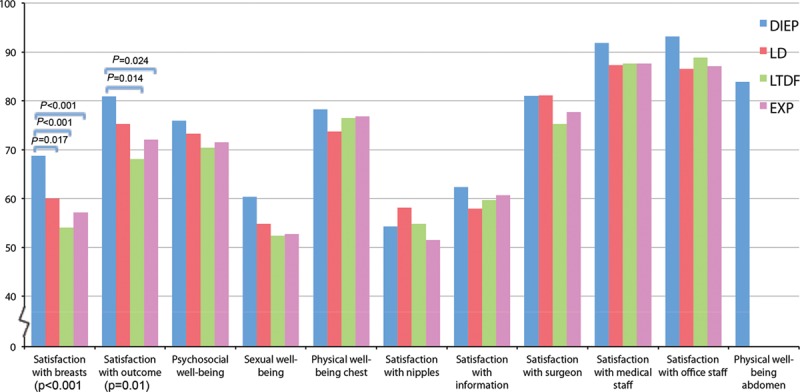
Results of the Breast-Q questionnaire, divided into method groups. P value under the bars for the domains of satisfaction with breasts, and satisfaction with outcome are for the overall group. Brackets indicate statistically significant differences between the groups, the color of the brackets indicates which group has the higher score.
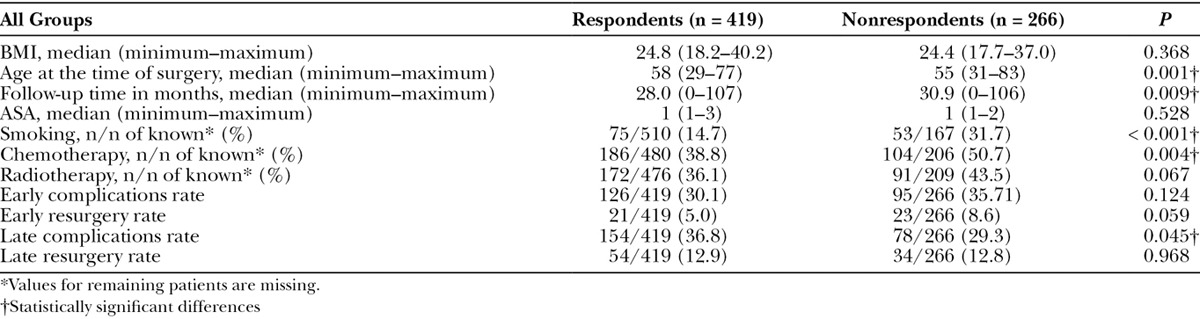
Response Analysis
Table 2 shows the demographic parameters for all groups and separated into responders and nonresponders. There were no significant differences in the overall group between responders and nonresponders regarding BMI, ASA classification, history of radiotherapy, early complication rate, and early and late resurgery. There were significant differences in age at the time of surgery showing the respondents were older than the nonrespondents (P = 0.001). The follow-up time was shorter in the respondents group than the nonrespondents group (P = 0.009). The nonresponder group had higher frequencies of smoking (P < 0.001) and history of chemotherapy (P = 0.004). The respondents had a higher late complication rate (P = 0.045).
Table 2.
Response Analysis
DISCUSSION
There are two main findings of the present study. First, there were no significant differences in most of the domains of the HR-QoL instruments, suggesting that none of the reconstruction methods were unquestionably superior to the others. Second, the only differences between the groups were found in the most specific of the instruments, the Breast-Q, with the exception of the vitality domain of SF-36. The patients in the DIEP group were more satisfied than the other groups in the Breast-Q domains satisfaction with breasts and satisfaction with outcome. The domain satisfaction with breasts measures the perception of the breast appearance and comprises the patient’s opinion on size, symmetry, and softness of the breast. The domain satisfaction with outcome measures the overall sense of satisfaction with the outcome after undergoing breast reconstruction.32 The patients who underwent DIEP were more satisfied with their reconstruction; this is especially interesting, given that the patients in this group had a higher frequency of complications than the patients in the other groups (previously published data),33 and it is known that postoperative complications tend to decrease satisfaction with the outcome of breast reconstruction. The results of the present study therefore do not agree with those of previous studies.5–9 Furthermore, the results show a trend toward a higher HR-QoL in the DIEP group, and it is possible that an even a larger sample of patients would show additional significant differences.
The high satisfaction with breasts in the DIEP group is, however, in line with previous studies reporting similarly high rates of satisfaction in this group of patients.34–40 A study comparing autologous microsurgical reconstruction with expander/implant reconstruction, showed similar results as in the present study using Breast-Q, but only 2 methods were compared.40 Another study, which also shows autologous reconstruction to be superior to implant-based reconstruction, compared as many methods as in the present study but used other outcome measures.37 Most studies evaluate DIEP as a single method without comparing it with any other method,9,38,41–45 or compare it only with the pedicled transverse rectus abdominis myocutaneous flap.46–49
All groups scored similarly on the SF-36, EQ-5D, and PGWB. Both the LTDF and EXP groups had a higher score than the DIEP group in the vitality domain of the SF-36; this is puzzling and might be interpreted as type 1 error, especially as there are no significant differences in the vitality domain of the PGWB. The reason for the inability of the instruments to detect significant differences is that they are likely too generic and not specific enough for this group of patients.
Another interesting finding of the present study is that there are clear differences between several domains of the SF-36, when the study group is compared with normal population values. The study group scores higher in the domain of physical function but scores lower in the domains of general health, vitality, social functioning, mental health, and the mental component summary.
On analysis of the representativity of the responders group compared with the nonresponders group, slight differences were found in age, follow-up time, smoking, history of chemotherapy, and late complication rate. Smoking and history of chemotherapy are factors that can negatively affect the surgical results. It is possible that they cause a nonresponse bias, whereby a group of patients exposed to complications do not wish to answer the questionnaires because of dissatisfaction with the results. However, it is important to consider that some data regarding smoking and chemotherapy were missing, and this might also affect the significance of these results. The shorter follow-up time of the responders and higher rate of late complications suggest that patients who are still actively thinking about their breast reconstruction are more likely to respond to the questionnaires.
The advantages of the present study are its relatively good response rate and well-validated generic and specific patient-reported outcome measures. The study also includes a greater number of patients compared with that of other studies evaluating patient satisfaction after breast reconstruction3,36,38 and is based on the registration of consecutive patients during a relatively long period of time.
This study has some limitations. A noticeable limitation to the present study is the fact that it does not contain baseline data on HR-QoL from before breast reconstruction. The Breast-Q has modules for both preoperative and postoperative evaluation31 but no values for a normal population. However, since only nonvalidated specific questionnaires were in use at the time, and the Breast-Q had not been developed, baseline data on this group of patients were not available. However, postoperative patient-reported outcome measurements alone do provide valuable insights into HR-QoL and patient satisfaction after breast reconstruction and can be efficiently utilized to compare reconstruction methods. To get a more comprehensive picture, a prospective study with randomized selection of reconstruction methods using both the pre- and postoperative questionnaires would be appropriate and is recommended.
A source of potential error in the present is that no multivariate analysis was carried out between all demographic factors and the results of the questionnaires. However, all demographic factors for the study group have been previously been analyzed.33
Another source of potential error is that the number of patients who received an autologous reconstruction (the DIEP group) are modest in comparison with the implant reconstructions (LD, LTDF, and EXP groups).
The emphasis an individual patient places on satisfaction with breasts versus the other factors such as length of recovery time, aesthetic results, or complication rates needs to be analyzed and is an important factor to consider when deciding on a suitable method of breast reconstruction.
CONCLUSIONS
In terms of HR-QoL, patients who underwent reconstruction with the DIEP flap were more satisfied with their reconstruction and overall outcome than patients who underwent reconstruction with other methods. This should be taken into consideration when deciding on a suitable method of reconstruction. The results suggest that major breast reconstruction centers should make DIEP reconstruction more widely available to patients after mastectomy.
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Al-Ghazal SK, Sully L, Fallowfield L, et al. The psychological impact of immediate rather than delayed breast reconstruction. Eur J Surg Oncol. 2000;26:17–19. [DOI] [PubMed] [Google Scholar]
- 2.Dean C, Chetty U, Forrest AP.Effects of immediate breast reconstruction on psychosocial morbidity after mastectomy. Lancet. 1983;1:459–462. [DOI] [PubMed] [Google Scholar]
- 3.Elder EE, Brandberg Y, Björklund T, et al. Quality of life and patient satisfaction in breast cancer patients after immediate breast reconstruction: a prospective study. Breast. 2005;14:201–208. [DOI] [PubMed] [Google Scholar]
- 4.Wilkins EG, Cederna PS, Lowery JC, et al. Prospective analysis of psychosocial outcomes in breast reconstruction: one-year postoperative results from the Michigan Breast Reconstruction Outcome Study. Plast Reconstr Surg. 2000;106:1014–1025; discussion 1026. [DOI] [PubMed] [Google Scholar]
- 5.Andrade WN, Baxter N, Semple JL.Clinical determinants of patient satisfaction with breast reconstruction. Plast Reconstr Surg. 2001;107:46–54. [DOI] [PubMed] [Google Scholar]
- 6.Colakoglu S, Khansa I, Curtis MS, et al. Impact of complications on patient satisfaction in breast reconstruction. Plast Reconstr Surg. 2011;127:1428–1436. [DOI] [PubMed] [Google Scholar]
- 7.Gopie JP, Timman R, Hilhorst MT, et al. The short-term psychological impact of complications after breast reconstruction. Psychooncology. 2013;22:290–298. [DOI] [PubMed] [Google Scholar]
- 8.Krueger EA, Wilkins EG, Strawderman M, et al. Complications and patient satisfaction following expander/implant breast reconstruction with and without radiotherapy. Int J Radiat Oncol Biol Phys. 2001;49:713–721. [DOI] [PubMed] [Google Scholar]
- 9.Zhong T, McCarthy C, Min S, et al. Patient satisfaction and health-related quality of life after autologous tissue breast reconstruction: a prospective analysis of early postoperative outcomes. Cancer. 2012;118:1701–1709. [DOI] [PubMed] [Google Scholar]
- 10.van Vuuren TMAJ, van Haaren ERM, vd Kar TJ, et al. Patient satisfaction and complication rate after mastectomy with immediate two-stage breast reconstruction as compared to mastectomy without immediate breast reconstruction. Surg Pract 2015;19:120–127. [Google Scholar]
- 11.Sajid MS, Tonsi A, Baig MK.Health-related quality of life measurement. Int J Health Care Qual Assur. 2008;21:365–373. [DOI] [PubMed] [Google Scholar]
- 12.Ware JE., Jr.SF-36 health survey update. Spine (Phila Pa 1976). 2000;25:3130–3139. [DOI] [PubMed] [Google Scholar]
- 13.Nordlund A, Ekberg K, Kristenson M.EQ-5D in a general population survey—a description of the most commonly reported EQ-5D health states using the SF-36. Qual Life Res. 2005;14:1099–1109. [DOI] [PubMed] [Google Scholar]
- 14.Davies N.Measuring health-related quality of life in cancer patients. Nurs Stand. 2009;23:42–49. [DOI] [PubMed] [Google Scholar]
- 15.Testa MA, Simonson DC.Assessment of quality-of-life outcomes. N Engl J Med. 1996;334:835–840. [DOI] [PubMed] [Google Scholar]
- 16.Hamming JF, De Vries J.Measuring quality of life. Br J Surg. 2007;94:923–924. [DOI] [PubMed] [Google Scholar]
- 17.Chassany O, Dimenäs E, Dubois D, Wu A.The Psychological General Well-Being Index (PGWBI) User Manual. Available at http://178.23.156.107:8085/Instruments_files/USERS/pgwbi.pdf.
- 18.Wiklund I, Karlberg J.Evaluation of quality of life in clinical trials. Selecting quality-of-life measures. Control Clin Trials. 1991;12:204S–216S. [DOI] [PubMed] [Google Scholar]
- 19.Pusic AL, Klassen AF, Scott AM, et al. Development of a new patient-reported outcome measure for breast surgery: the BREAST-Q. Plast Reconstr Surg. 2009;124:345–353. [DOI] [PubMed] [Google Scholar]
- 20.Linguistic Validation Manual for Health Outcome Assessments. 20122nd ed Lyon, France: MAPI Research Trust; [Google Scholar]
- 21.Breast-Q Users’ Manual Version 1.0. Available at https://webcore.mskcc.org/breastq/qscore/qscore-manual.pdf.
- 22.Allen RJ, Treece P.Deep inferior epigastric perforator flap for breast reconstruction. Ann Plast Surg. 1994;32:32–38. [DOI] [PubMed] [Google Scholar]
- 23.Bostwick J, 3rd, Scheflan M.The latissimus dorsi musculocutaneous flap: a one-stage breast reconstruction. Clin Plast Surg. 1980;7:71–78. [PubMed] [Google Scholar]
- 24.Holmström H, Lossing C.The lateral thoracodorsal flap in breast reconstruction. Plast Reconstr Surg. 1986;77:933–943. [DOI] [PubMed] [Google Scholar]
- 25.Strock LL.Two-stage expander implant reconstruction: recent experience. Plast Reconstr Surg. 2009;124:1429–1436. [DOI] [PubMed] [Google Scholar]
- 26.Daabiss M.American Society of Anaesthesiologists physical status classification. Indian J Anaesth. 2011;55:111–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sullivan M, Karlsson J, Taft C.SF-36 Health Survey: Swedish Manual and Interpretation Guide. 2002Gothenburg, Sweeden: Sahlgrenska University Hospital; [Google Scholar]
- 28.Reene M, Janssen B.EQ-5D-5L User Guide, Vol. 2016, Version 2.1 ed. 2015EuroQoL; [Google Scholar]
- 29.Rasch Unidimensional Measurement Models Laboratory. Available at http://www.rummlab.com.au/.
- 30.Pusic AL, Klassen A, Cano SJ, et al. Validation of the breast evaluation questionnaire. Plast Reconstr Surg. 2007;120:352–353. [DOI] [PubMed] [Google Scholar]
- 31.Breast-Q.org. Users Manual. Available at https://webcore.mskcc.org/breastq/scoring.html.
- 32.Breast-Q. Breast-Q.org. Available at: https://webcore.mskcc.org/breastq/domains.html2015.
- 33.Thorarinsson A, Fröjd V, Kölby L, et al. A retrospective review of the incidence of various complications in different delayed breast reconstruction methods. J Plast Surg Hand Surg. 2016;50:25–34. [DOI] [PubMed] [Google Scholar]
- 34.Damen TH, Mureau MA, Timman R, et al. The pleasing end result after DIEP flap breast reconstruction: a review of additional operations. J Plast Reconstr Aesthet Surg. 2009;62:71–76. [DOI] [PubMed] [Google Scholar]
- 35.Tønseth KA, Hokland BM, Tindholdt TT, et al. Patient-reported outcomes after breast reconstruction with deep inferior epigastric perforator flaps. Scand J Plast Reconstr Surg Hand Surg. 2007;41:173–177. [DOI] [PubMed] [Google Scholar]
- 36.Tønseth KA, Hokland BM, Tindholdt TT, et al. Quality of life, patient satisfaction and cosmetic outcome after breast reconstruction using DIEP flap or expandable breast implant. J Plast Reconstr Aesthet Surg. 2008;61:1188–1194. [DOI] [PubMed] [Google Scholar]
- 37.Yueh JH, Slavin SA, Adesiyun T, et al. Patient satisfaction in postmastectomy breast reconstruction: a comparative evaluation of DIEP, TRAM, latissimus flap, and implant techniques. Plast Reconstr Surg. 2010;125:1585–1595. [DOI] [PubMed] [Google Scholar]
- 38.Damen TH, Timman R, Kunst EH, et al. High satisfaction rates in women after DIEP flap breast reconstruction. J Plast Reconstr Aesthet Surg. 2010;63:93–100. [DOI] [PubMed] [Google Scholar]
- 39.Damen TH, Wei W, Mureau MA, et al. Medium-term cost analysis of breast reconstructions in a single Dutch centre: a comparison of implants, implants preceded by tissue expansion, LD transpositions and DIEP flaps. J Plast Reconstr Aesthet Surg. 2011;64:1043–1053. [DOI] [PubMed] [Google Scholar]
- 40.Liu C, Zhuang Y, Momeni A, et al. Quality of life and patient satisfaction after microsurgical abdominal flap versus staged expander/implant breast reconstruction: a critical study of unilateral immediate breast reconstruction using patient-reported outcomes instrument BREAST-Q. Breast Cancer Res Treat. 2014;146:117–126. [DOI] [PubMed] [Google Scholar]
- 41.Munhoz AM, Arruda E, Montag E, et al. Immediate skin-sparing mastectomy reconstruction with deep inferior epigastric perforator (DIEP) flap. Technical aspects and outcome. Breast J. 2007;13:470–478. [DOI] [PubMed] [Google Scholar]
- 42.Venkat R, Lee JC, Rad AN, et al. Bilateral autologous breast reconstruction with deep inferior epigastric artery perforator flaps: review of a single surgeon’s early experience. Microsurgery. 2012;32:275–280. [DOI] [PubMed] [Google Scholar]
- 43.Hamdi M, Weiler-Mithoff EM, Webster MH.Deep inferior epigastric perforator flap in breast reconstruction: experience with the first 50 flaps. Plast Reconstr Surg. 1999;103:86–95. [DOI] [PubMed] [Google Scholar]
- 44.Gill PS, Hunt JP, Guerra AB, et al. A 10-year retrospective review of 758 DIEP flaps for breast reconstruction. Plast Reconstr Surg. 2004;113:1153–1160. [DOI] [PubMed] [Google Scholar]
- 45.Guerra AB, Metzinger SE, Bidros RS, et al. Bilateral breast reconstruction with the deep inferior epigastric perforator (DIEP) flap: an experience with 280 flaps. Ann Plast Surg. 2004;52:246–252. [DOI] [PubMed] [Google Scholar]
- 46.Chun YS, Sinha I, Turko A, et al. Comparison of morbidity, functional outcome, and satisfaction following bilateral TRAM versus bilateral DIEP flap breast reconstruction. Plast Reconstr Surg. 2010;126:1133–1141. [DOI] [PubMed] [Google Scholar]
- 47.Andree C, Munder BI, Seidenstuecker K, et al. Skin-sparing mastectomy and immediate reconstruction with DIEP flap after breast-conserving therapy. Med Sci Monit. 2012;18:CR716–CR720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Selber JC, Nelson J, Fosnot J, et al. A prospective study comparing the functional impact of SIEA, DIEP, and muscle-sparing free TRAM flaps on the abdominal wall: part I. Unilateral reconstruction. Plast Reconstr Surg. 2010;126:1142–1153. [DOI] [PubMed] [Google Scholar]
- 49.Garvey PB, Buchel EW, Pockaj BA, et al. DIEP and pedicled TRAM flaps: a comparison of outcomes. Plast Reconstr Surg. 2006;117:1711–1719; discussion 1720. [DOI] [PubMed] [Google Scholar]


