Abstract
The aim of the study was to systematically review the patient reported and functional outcomes of treatment for extra-articular proximal or middle phalangeal fractures of the hand in order to determine the best treatment options. The review methodology was registered with PROSPERO. A systematic literature search was conducted in electronic bibliographic databases. Two independent reviewers performed screening and data extraction. The evaluation of quality of the included studies was performed using the Structured Effectiveness Quality Evaluation scale. The initial search yielded 2354 studies. The full text manuscripts of 79 studies were evaluated of which 16 studies met the inclusion criteria. In total, 513 extra-articular proximal and middle phalangeal fractures of the hand were included of which 118 (23%) were treated non-operatively, 188 (37%) were treated by closed reduction internal fixation (CRIF) and 207 (40%) by open reduction internal fixation. It can be recommended that closed displaced extra-articular phalangeal fractures can be treated non-operatively, even fractures with an oblique or complex pattern, provided that closed reduction is possible and maintained. Conservative treatment is preferably performed with a cast/brace allowing free mobilization of the wrist. No definite conclusion could be drawn upon whether closed reduction with extra-articular K-wire pinning or transarticular pinning is superior; however, it might be suggested that extra-articular K-wire pinning is favoured. When open reduction is necessary for oblique or spiral extra-articular fractures, lag screw fixation is preferable to plate and screw fixation. But, similar recovery and functional results are achieved with transversally inserted K-wires compared to lag screw fixation.
Type of study/level of evidence: therapeutic III.
Keywords: Extra-articular phalangeal fractures, Fracture treatment, ORIF, Systematic review
Introduction
Phalangeal fractures account for approximately 18% of all upper-extremity fractures and are the most common fractures of the hand [1, 2]. The proximal phalanx of the long finger is fractured most frequently compared with the middle or distal phalanges [2, 3]. However, phalangeal fractures regularly result in unsatisfactory outcomes possibly because too often these phalangeal fractures are regarded as trivial injuries [4, 5].
Treatment of extra-articular middle and proximal phalangeal fractures of the hand is aimed at achieving solid bone union and restoring hand function. Various treatment methods including buddy strapping, splinting, closed reduction internal fixation (CRIF) with Kirschner-wires and open reduction internal fixation (ORIF) with plates and/or screws have been described. When selecting a treatment method, factors such as fracture classification, displacement, stability and whether it is an open or closed fracture have to be taken into account [6, 7].
However, there is no evidence-based consensus concerning the best treatment for extra-articular middle and proximal phalangeal fractures of the hand. This paper systematically reviewed the literature and assessed the patient reported and functional outcomes to determine the most favourable treatment options.
Methods
This review was conducted and reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses protocols (PRISMA-P) [8]. A review protocol was drafted and registered on PROSPERO with number CRD42015026979. All of the following steps were performed by two independent reviewers (LT and DV). Disagreement was resolved by discussion.
Eligibility criteria
Inclusion criteria were randomized controlled trials, case–control studies, cohort studies and case series (n ≥ 10) including adult and adolescent (≥14 years) patients treated for extra-articular proximal or middle phalangeal fractures of the hand and reporting patient reported and/or functional outcomes. English or German manuscripts were included exclusively. Studies describing distal phalangeal fractures, intra-articular fractures and/or pathological fractures were excluded in addition to reviews, animal studies, cadaver studies, case reports, surveys, editorials, commentaries, conference abstracts and letters.
Open fractures can be classified according to concurrent soft tissue injury [9]. Type I open fractures consist of a simple skin laceration, superficial skin injury and/or digital nerve injury, whereas type II open fractures consist of complete extensor tendon injury or extensive skin loss requiring reconstruction and type III consists of flexor tendon injury or combined extensor tendon injury and extensive skin loss requiring reconstruction. Studies including patients with closed or type I open fractures were included exclusively.
Outcome measures
The primary outcome was validated patient reported outcome measures (PROMs) such as the Disabilities of the Arm, Shoulder and Hand (DASH) Score. Secondary outcomes included other patient reported outcomes such as satisfaction, pain and time to return to work and functional outcomes including total active range of motion (TAM), range of motion (ROM), grip strength, union, malunion, loss of reduction, secondary procedures, infection. A TAM of a typical finger is 260°, which is the sum of active flexion at the metacarpophalangeal (MCP) (normal range: 0°–85°), proximal interphalangeal (PIP) (normal range: 0°–110°) and distal interphalangeal (DIP) (normal range: 0°–65°) joints [10].
Literature search and study selection
A search strategy was constructed with help of a clinical librarian by using descriptors that included synonyms for ‘phalanx fracture’, ‘proximal and/or middle phalanx’ and ‘fracture treatment’ in various combinations. Articles were sourced from Embase, Medline, Web-of-Science, Cinahl, Pubmed (the subset as applied by publisher, containing references not yet indexed by Medline), Cochrane, Lilacs, Scielo, Proquest and Google Scholar. The search was performed in August 2015. If the eligibility criteria were met, full manuscripts were procured and reviewed. Additionally, reference lists from included articles were examined for suitable studies.
Data extraction
Data were extracted using a standardized data collection form that was developed according to the Cochrane guidelines [11]. Data collected included publication details (authors, year, journal), type of study (e.g. retrospective case series), demographic data (number of subjects, age, sex), follow-up period, the type of treatment applied and the described patient reported and functional outcomes. If necessary, the primary authors were contacted to retrieve further information. The level of evidence was determined using the Oxford Centre for Evidence-based Medicine Levels of Evidence (2011).
The evaluation of quality of the included studies was performed using the Structured Effectiveness Quality Evaluation scale (SEQES) [12]. The SEQES appraises the overall quality of a study based on study design, subjects, intervention, outcomes, analysis and recommendations. Each category has individual criteria that can be scored from 0 to 2. A score between 1–16 is regarded as low quality, 17–32 as moderate quality and 33–48 as high quality.
Statistical analysis
A meta-analysis was planned but not performed due to heterogeneity between studies, varying methodology and lack of direct comparative results.
Results
Study selection
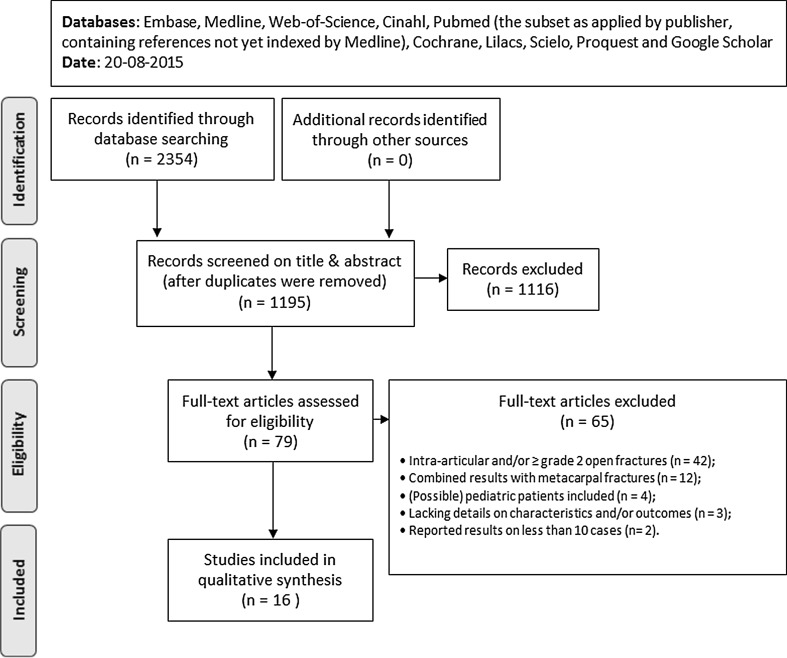
Figure 1 shows a flow chart depicting the study identification process. The initial search yielded a total of 2354 studies, of which 1195 remained after excluding the duplicates. The full text manuscripts of 79 studies were evaluated, and 16 studies were included in the systematic review. Examination of reference lists from included articles did not yield any additional suitable articles.
Fig. 1.
Flow chart
Quality assessment
The SEQES scores varied from 15 to 31 with a mean of 21.7. Most studies (87.5%) were of intermediate quality. Table 1 illustrates a summary of SEQES scores of the included studies.
Table 1.
Structured Effectiveness Quality Evaluation scale (SEQES)
| References | Descriptors | Study design | Subjects | Intervention | Outcome | Analysis | Recommendations | Totala | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | 23 | 24 | ||
| Al-Qattan [23] | 1 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 2 | 1 | 1 | 0 | 2 | 1 | 0 | 0 | 0 | 0 | 2 | 1 | 2 | 17 |
| Al-Qattan [20] | 1 | 2 | 0 | 0 | 0 | 1 | 1 | 0 | 2 | 2 | 0 | 2 | 1 | 1 | 2 | 2 | 1 | 0 | 2 | 1 | 1 | 2 | 1 | 1 | 26 |
| Al-Qattan [24] | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 2 | 0 | 2 | 1 | 1 | 2 | 2 | 1 | 0 | 2 | 1 | 1 | 2 | 1 | 2 | 23 |
| Al-Qattan [21] | 1 | 2 | 0 | 1 | 0 | 1 | 1 | 0 | 0 | 2 | 0 | 2 | 1 | 1 | 2 | 2 | 1 | 1 | 2 | 0 | 1 | 2 | 1 | 1 | 25 |
| Başar [13] | 2 | 2 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 0 | 2 | 1 | 1 | 2 | 2 | 1 | 1 | 2 | 0 | 2 | 2 | 1 | 1 | 27 |
| Brei-Thoma [25] | 2 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 2 | 0 | 1 | 1 | 1 | 0 | 2 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 16 |
| Faruqui [22] | 1 | 2 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 2 | 0 | 2 | 1 | 0 | 2 | 2 | 1 | 1 | 2 | 1 | 0 | 2 | 1 | 2 | 25 |
| Franz [17] | 2 | 0 | 1 | 2 | 0 | 0 | 0 | 0 | 1 | 2 | 0 | 2 | 1 | 1 | 0 | 2 | 1 | 0 | 0 | 0 | 0 | 2 | 1 | 2 | 20 |
| Franz [16] | 2 | 2 | 1 | 2 | 1 | 1 | 1 | 0 | 1 | 2 | 0 | 2 | 1 | 1 | 2 | 2 | 1 | 0 | 2 | 1 | 1 | 2 | 1 | 2 | 31 |
| Held [18] | 2 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 2 | 0 | 2 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 2 | 1 | 1 | 17 |
| Hornbach [14] | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 2 | 1 | 1 | 0 | 2 | 1 | 1 | 2 | 0 | 1 | 2 | 1 | 1 | 19 |
| Horton [19] | 1 | 2 | 1 | 2 | 2 | 1 | 1 | 1 | 2 | 2 | 0 | 1 | 1 | 1 | 2 | 2 | 1 | 1 | 2 | 0 | 1 | 1 | 1 | 2 | 31 |
| Nalbantoǧlu [15] | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 2 | 1 | 1 | 0 | 2 | 1 | 1 | 0 | 0 | 0 | 2 | 1 | 2 | 17 |
| Patankar [26] | 1 | 0 | 1 | 2 | 0 | 0 | 0 | 0 | 1 | 2 | 0 | 2 | 1 | 1 | 0 | 2 | 1 | 1 | 0 | 0 | 0 | 2 | 1 | 2 | 20 |
| Pehlivan [27] | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 2 | 1 | 1 | 0 | 2 | 1 | 1 | 0 | 0 | 0 | 2 | 1 | 1 | 15 |
| Thomas [28] | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 2 | 0 | 2 | 1 | 1 | 0 | 2 | 1 | 1 | 0 | 0 | 0 | 2 | 1 | 2 | 18 |
a Total points: 1–16 low quality, 17–32 moderate quality, 33–48 high quality
Study and patient characteristics
Among the 16 included studies, there were two randomized controlled trials, four cohort studies and ten case series. In total, 513 extra-articular proximal and middle phalangeal fractures of the hand in 484 patients were included. The mean age of the included patients ranged from 22 to 49 years. Most patients were male (79%). A total of 118 fractures (23%) were treated non-operatively, 188 fractures (37%) were treated by CRIF and 207 fractures (40%) by ORIF. The mean follow-up time ranged from 7 weeks to 40 months. Details on the included fractures, the various applied treatment methods and the post-operative protocols are depicted in Table 2.
Table 2.
Identified studies
| References | Design | Na (fract.) | Pb | Oc | Trauma | Fracture pattern | Type of treatment | Treatment details | LOE |
|---|---|---|---|---|---|---|---|---|---|
| Al-Qattan [23] | Pros. series | 15 (15) | P1 | 0% | Industrial | Long oblique Spiral |
Cerclage wires | Dorsal approach, longitudinally splitting extensor tendon, 2 or 3 pieces; light bandage overnight | IV |
| Al-Qattan [20] | Retro. cohort | 78 (78) | P1 | 26% | Industrial | Transverse (100%) | K-wires (transarticular) | Antegrade or retrograde insertion (fixed MCPJ, free PIPJ), 2 pieces; palmar splint 10 days, K-wire removal 4–5 weeks | IV |
| Interosseous loop wires | Dorsal approach/adjusting existing laceration, longitudinally splitting extensor tendon; light bandage overnight | ||||||||
| Al-Qattan [24] | Retro. series | 35 (35) | P1 | 100% | Industrial | Transverse (100%) | K-wires (extra-articular) | Antegrade insertion (N = 20), mid-lateral approach with retrograde insertion (N = 15), 1 or 2 pieces; no splint, K-wire removal 5–6 weeks | IV |
| Al-Qattan [21] | Pros. cohort | 20 (29) | P2 | 100% | Industrial | N.D. | K-wire | Insertion from tip of digit (fixed DIPJ, free PIPJ); K-wire removal 5 weeks | III |
| Başar [13] | Retro. cohort | 22 (22) | P1 | 0% | N.D. | Oblique (64%) Spiral (36%) |
Mini plate and screws | Dorsal approach, longitudinally splitting extensor tendon; splint 2 weeks | IV |
| Screws only | Dorsal approach, longitudinally splitting extensor tendon, ≥2 pieces; splint 3 weeks | ||||||||
| Brei-Thoma [25] | Retro. series | 25 (29) | P1 | 19% | N.D. | Basal transverse (50%) Transverse (28%) Oblique (17%) Spiral (6%) |
Plate and screws, plate | Dorsal approach/adjusting existing laceration, longitudinally splitting extensor tendon; removable splint 4 weeks | IV |
| Faruqui [22] | Retro. cohort | P1 | 0% | N.D. | Transverse Short oblique |
K-wires (transarticular) | Antegrade insertion (fixed MCPJ, free PIPJ), 2 pieces; splint 3–7 days, dorsal extension block splint 4 weeks, K-wire removal 3–4 weeks | IV | |
| K-wires (extra-articular) | Cross-pinning from radial and ulnar base, 2 pieces; splint 3–7 days, dorsal extension block splint 4 weeks, K-wire removal 3–4 weeks | ||||||||
| Franz [17] | Pros. series | 15 (20) | P1 | 0% | N.D. | Transverse (45%) Oblique (30%) Spiral (25%) |
LuCa | Metacarpal brace, dorsal extension PIPJs, free wrist, buddy tape | IV |
| Franz [16] | RCT | 65 (74) | P1 | 0% | N.D. | Basal transverse (53%) Transverse (13%) Oblique (17%) Spiral (12%) Longitudinal (4%) |
LuCa | Metacarpal brace, dorsal extension PIPJs, free wrist, buddy tape | II |
| Forearm cast | Dorsopalmar plaster splint, dorsal extension PIPJs, fixed wrist, buddy tape | ||||||||
| Held [18] | Pros. series | 23 (23) | P1 | 0% | Low velocityd | Transverse (39%) Oblique (39%) Complex (22%) |
Dorsal splint | Dorsal plaster slab, buddy tape | IV |
| Hornbach [14] | Retro. series | 11 (12) | P1 | 0% | N.D. | N.D. | K-wires (transarticular) | Antegrade insertion (fixed MCPJ, free PIPJ), 2 pieces; removable splint 3–4 weeks, K-wire removal 3–4 weeks | IV |
| Horton [19] | RCT | 28 (28) | P1 | N.D. | Sports, low velocityd | Long oblique Spiral |
K-wires (transversal) | Transversal insertion, 2 or 3 pieces; palmar slab 3–4 weeks, K-wire removal 4 weeks | II |
| Lag screws | Mid-lateral approach, excision lateral band extensor tendon, 2 pieces; splint 2 days, removable splint 3–4 weeks | ||||||||
| Nalbantoǧlu [15] | Retro. series | 17 (18) | P1, P2 | 0% | Low- velocityd | Transverse (6%) Oblique (39%) Spiral (22%) Comminuted (33%) |
Plate and screws and mini screws only | Dorsoulnar or radial approach w/o separating extensor tendon, ≥2 pieces; splint <3 weeks | IV |
| Patankar [26] | Pros. series | 35 (35) | P1 | 0% | Industrial, sports, low velocityd | Transverse (40%) Short oblique (34%) Long oblique (20%) Segmental (6%) |
Intra-medullary nailing | Dorsal approach, longitudinally splitting extensor tendon (N = 15), closed reduction (N = 20), 2 or 3 pieces; plaster slab 3 weeks | IV |
| Pehlivan [27] | Retro. series | 23 (23) | P1, P2 | 0% | N.D. | Transverse (100%) | Tension band wiring | Dorsal approach, longitudinally splitting extensor tendon | IV |
| Thomas [28] | Retro. series | 10 (10) | P1 | 100% | Road traffic accidents | Transverse (100%) | Theta fixation | Dorsal approach/adjusting existing laceration, longitudinally splitting extensor tendon; removable volar plaster 3 weeks | IV |
DIPJ distal interphalangeal joint, MCPJ metacarpophalangeal joint, N.D. not described, PIPJ proximal interphalangeal joint
aRemaining patients and fractures in analysis after excluding patients lost to follow-up or with incomplete data
bPhalanx: proximal (P1) or middle (P2)
cType I open fractures: without complete tendon injury or extensive soft tissue loss requiring reconstruction
dLow velocity: falling, straining, contusion
Only three studies of which one cohort study [13] and two case series [14, 15] evaluated validated PROMs. Başar [13] and Nalbantoǧlu [15] assessed disability of the hand/finger using the QuickDASH score, and Hornbach [14] evaluated general health using the Short-Form-36 (SF-36).
Treatment
One RCT [16] and two case series [17, 18] comprised a total of 117 fractures in 103 patients treated non-operatively. One RCT [19], three cohort studies [20–22] and three case series comprised a total of 186 fractures in 176 patients treated with CRIF. One RCT [19], two cohorts [13, 20] and seven case series [15, 23–28] comprised a total of 198 fractures in 193 patients treated with ORIF. One RCT [19], one cohort study [20] and two case series [24, 26] reported on CRIF and ORIF. The outcomes per study are depicted in Table 3, and the pooled results of all studies are depicted in Table 4.
Table 3.
Outcomes
| References | Mean FU | Treatment | N | Outcomes | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean TAM (range/SD) | TAM categories | NU | TAM <180° | TAM >240° | Inf. | Failurea | SSPs | Other/statistical outcomes | ||||
| 3A Non-operative treatment | ||||||||||||
| Franz [17] | 12 weeks | LuCa | 20 | 240° (155°–290°) | N.D. | 0 | 0 | 12 | N.A. | 0 | 0 | N.D. |
| Franz [16] | 12 weeks | A: LuCa | 44 | 246.6° (150°–300°) | N.D. | 0 | 1 | 23 | N.A. | 2: loss of reduction | 2: revision surgery (RS) | Mean TAM: NSD, P value N.D. Satisfaction (VAS): A 9.4 vs. B 8.4, P = 0.022* Mean wrist motion: A 128° vs. B 137°, P = 0.074 |
| B: Forearm cast | 30 | 231.6° (145°–300°) | N.D. | 0 | 1 | 14 | N.A. | 0 | 0 | |||
| Held [18] | 7 weeks | Dorsal splint | 23 | N.D. | N.D. | 0 | N.D. | N.D. | N.A. | 2: MU requiring RS | 2: revision surgery (RS) | N.D. |
| 3B Closed Reduction Internal Fixation (CRIF) | ||||||||||||
| Al-Qattan [21] | 30 weeks | A: K-wire, w/o SSTC | 16 | 241.3° (SD 8.5°) | Excellent (≥240°): 10 (63%) Good (210°–240°): 6 (38%) Fair (180°–209°): 0 Poor (<180°): 0 |
0 | 0 | N.D. | 0 | 0 | 0 | Mean TAM: A vs. B, P < 0.001* Mean TTRBTW: A 15.1 weeks (SD ± 1.6) vs. B 26.8 weeks (SD ± 2.0), P < 0.001* |
| B: K-wire with SSTC |
13 | 186.9° (SD 20.7°) |
Excellent (≥240°):0 Good (210°–240°): 3 (23%) Fair (180°–209°): 2 (23%) Poor (<180°): 7 (54%) |
0 | 7 | N.D. | 0 | 0 | 0 | |||
| Faruqui [22] | 8 months | A: K-wires (transarticular) | 25 | 201° | N.D. | 1 | N.D. | N.D. | 1 | 2: loss of reduction | 5: tenolysis 1: capsulotomy |
Mean TAM: NSD, P value N.D. Overall % complications (as defined by authors): A 56% vs. B 48%, NSD, P value N.D. |
| B: K-wires (extra-articular) | 25 | 198° | N.D. | 0 | N.D. | N.D. | 0 | 0 | 1: tenolysis 1: capsulotomy |
|||
| Hornbach [14] | 20 months | K-wires (transarticular) | 12 | 265° (SD 25°) | N.D. | 0 | 0 | 10 | 0 | 1: rotational MU requiring RS | 1: tenolysis | SF-36: NSD compared to standardized values for general population Mean grip strength: compared to contralateral hand, P > 0.05 |
| 3C Open Reduction Internal Fixation (ORIF) | ||||||||||||
| Al-Qattan [23] | 12 weeks | Cerclage wires | 15 | 258° (245°–260°) | Excellent (> 75%): 17 (74%) Good (50–75%): 6 (26%) Fair (25–50%): 0 Poor (<25%): 0 |
0 | 0 | N.D. | 0 | 0 | 2: implant removal | N.D. |
| Başar [13] | 19.2 months | A: Mini plate and screws | N.D. | 212.3° (SD 30.3°) | N.D. | 0 | N.D. | N.D. | 2 | 0 | 0 | Mean TAM, A vs. B, P = 0.022* QuickDASH score: A 6.45 vs. B 2.58, P = 0.022* Loss of grip strength: A 6.1% (SD ± 8.6) vs. B 2.5% (SD ± 4.6), P = 0.1447 Mean TTRBTW: A 33.2 days vs. B 46.0 days, P < 0.05* |
| B: Screws only | N.D. | 235.0° (SD 25.6°) | N.D. | 0 | N.D. | N.D. | 0 | 0 | 0 | |||
| Brei-Thoma [25] | 10 months | Plate and screws, plate | 29 | 213° (100°–285°) | Excellent (>250°): 7 (24%) Good (210°–250°): 11 (38%) Fair (180°–209°): 3 (10%) Poor (<180°): 8 (28%) |
0 | 8 | 8 | 0 | 1: implant failure 2: rotational MU requiring RS |
2: revision surgery (RS) 12: implant removal + tenolysis |
N.D. |
| Nalbantoǧlu [15] | 35 months | Plate and screws, mini screw only | 18 | 200° (160°–260°, SD 39.5°) | Excellent (≥220°): 6 (33%) Good (180°219°): 5 (28%) Fair (130°179°): 7 (39%) Poor (<130°): 0 |
0 | 7 | 4 | 0 | 0 | 4: implant removal + tenolysis | Mean QuickDASH score: 3.4 |
| Pehlivan [27] | 13 months | Tension band wiring | 23 | N.D. | Excellent (> 75%): 17 (74%) Good (50–75%): 6 (26%) Fair (25–50%): 0 Poor (<25%): 0 |
0 | 0 | N.D. | 0 | 0 | 2: implant removal | N.D. |
| Thomas [28] | 28.8 months | Theta fixation | 10 | N.D. | Excellent (> 250°): 9 (90%) Good (> 180°): 1 (10%) Fair (<180°): 0 Poor (no change): 0 |
0 | N.D. | 9b | 0 | 0 | 3: implant removal | N.D. |
| 3D CRIF and/versus ORIF | ||||||||||||
| Al-Qattan [20] | 14 weeks | A: K-wires (transarticular) | 40 | N.D. | Excellent (> 240°): 5 (13%) Good (220–240°): 20 (50%) Fair (180–219°): 10 (25%) Poor (<180°): 5 (13%) |
0 | 5 | 5 | 2 | 2: re-displacement | 1: implant removal | TAM scores: A vs. B, P = 0.03* Mean TTRBTW: A 15 weeks vs. B 14 weeks, NSD, P value N.D. |
| B: Interosseous loop wires | 38 | N.D. | Excellent (> 240°): 15 (39%) Good (220–240°): 16 (42%) Fair (180–219°): 3 (8%) Poor (<180°): 4 (11%) |
0 | 4 | 15 | 0 | 3: re-displacement | 0 | |||
| Al-Qattan [24] | 16 weeks | C: K-wires (extra-articular) | 35c | N.D. | Excellent (> 240°): 15 (43%) Good (220–240°): 10 (29%) Fair (180–219°): 5 (14%) Poor (<180°): 5 (14%) |
0 | 5 | 15 | 4 | 0 | 0 | Comparison with Al-Qattan 2008: TAM scores: A vs. C, P = 0.021* TAM scores: B vs. C, P = 0.599 |
| Horton [19] | 40 months | A: K-wires (transversal) | 15 | N.D. | N.D. | 0 | N.D. | N.D. | 3 | 1: fixation failure | 3: tenolysis 1: release of palmar plate |
Mean (range) flexion PIPJ: A 81° (40–105) vs. B 80° (25–105), NSD, P value N.D. Mean (range) flexion DIPJ: A 55° (25–90) vs. B 49° (0–95), NSD, P value N.D. Median TTRBTW: A 3 weeks vs. B 1 week, NSD, P value N.D. Functional recovery: P = 0.3 Median VAS scores on pain and cold intolerance: NSD, P value N.D. |
| B: Lag screws | 13 | N.D. | N.D. | 0 | N.D. | N.D. | 3 | 1: fixation failure | 0 | |||
| Patankar [26] | ≥6 months | Intra-medullary nailingc | 35d | N.D. | Excellent (≥85%): 35 (100%) Good (70–84%): 6 Fair (50–69%): 0 Poor (<50%): 0 |
0 | 0 | N.D. | 1 | 0 | 0 | N.D. |
FU follow-up, Inf infection, MU malunion, N.A. not applicable, N.D. not described, NSD not significantly different, NU non-union, SSPs secondary surgical procedures, SSTC significant soft tissue crush, TTRBTW time to return back to work
aAs defined by authors
bTAM score of the remaining patient cannot be retrieved
cOf the 35 included patients, 15 were treated with open reduction and 20 patients with closed reduction, no differentiation made
Table 4.
Pooled results
| Treatment | N | Non-union | Poor TAM (<180°) | Good TAM (>240°) | Infection | Failurea | SSPs |
|---|---|---|---|---|---|---|---|
| Non-operative | 117 | 0 | 2.1% (2/94) | 52.1% (49/94) | N.A. | 3.4% (4/117) | 3.4% (4/117) |
| CRIF | 186 | 0.5% (1/86) | 14.8% (12/81) | 28.8% (15/52) | 4.1% (6/146) | 3.2% (6/186) | 7.5% (14/186) |
| ORIF | 198 | 0 | 13.1% (19/145) | 44.0% (51/116) | 2.9% (5/175) | 3.5% (7/198) | 12.1% (24/198) |
| Total | 501 | 0.2% (1/508) | 10.3% (33/320) | 43.7% (115/263) | 3.4% (11/321) | 3.4% (17/501) | 8.4% (42/501) |
N.A. not applicable, SSPs secondary surgical procedures
aIncludes loss of reduction, fixation failures, unacceptable malunion (as defined by authors)
Discussion
This systematic review provides an overview of the literature on treatment regimens used for closed or type I open extra-articular fractures of the proximal or middle phalanx of the hand in adolescent and adult patients, and outlines associated patient reported and functional outcomes. After a thorough search, available evidence was limited. Only two randomized controlled trials, four cohort studies and ten case series were included. The most important conclusions are depicted in Table 5.
Table 5.
Most important conclusions
| Conclusions | LOE |
|---|---|
| Non-operative treatment | |
| A cast/brace (with fixed MCP joints in 70°–90° flexion) allowing free mobilization of the wrist is preferred | II |
| Conservative treatment can also be used for closed displaced oblique or complex extra-articular fractures of the proximal phalanx, provided that closed reduction is possible and maintained, to achieve good functional results | IV |
| CRIF | |
| Patients with extra-articular fractures of the proximal phalanx in which initial non-operative treatment has failed can be successfully treated with CRIF | IV |
| ORIF | |
| Fixation with screw only, compared to plate and screws, is preferred in extra-articular spiral and oblique fractures of the proximal phalanx. | IV |
| CRIF vs. ORIF | |
| Similar recovery and functional results are achieved with transversally inserted K-wires compared to lag screw fixation in extra-articular fractures of the proximal phalanx | II |
LOE level of evidence
Outcomes non-operative treatment
There is no significant difference in radiological and functional outcome when a cast/brace (with fixed MCP joints in 70°–90° flexion) immobilizing the wrist is compared to a cast/brace without immobilization of the wrist (Level II, [16]). However, patients prefer a functional cast which enables free mobilization of the wrist as is shown by a significant higher score on a visual analogue scale (VAS) (Level II, [16]). Conventionally, almost all oblique, spiral or complex fractures were considered to be inherently unstable requiring internal fixation. However, it has been shown that closed displaced oblique and complex extra-articular fractures of the proximal phalanx from low-velocity injuries (including falling, straining, contusion) do not necessarily need to be treated with internal fixation, provided that closed reduction is possible and maintained, to achieve good functional results (Level IV, [18]).
Outcomes CRIF
The degree of soft tissue crush is an important factor that influences both functional and patient reported outcomes as is shown by Al-Qattan [21]. He reported that industrial workers with extra-articular fractures of the middle phalanx with significant soft tissue crush have a lower active range of motion and take longer to return back to work (Level III). Faruqui [22] did not find a significant difference in active range of motion or complication rate (as defined by authors) between CRIF with transarticular (across the MCP joint) or extra-articular pinning used in closed extra-articular fractures of the proximal phalanx (Level IV). Patients with extra-articular fractures of the proximal phalanx in which initial conservative treatment has failed can be successfully treated with CRIF with transarticular inserted K-wires as is shown by Hornbach [14] (Level IV). This is noteworthy because the included articles on non-operative treatments all used (or anticipated to use) open surgery for correction in case of treatment failure.
Outcomes ORIF
Başar [13] compared plate and screw versus screws only. They found a statistically significant difference in mean QuickDASH scores in favour of screw only fixation (2.58 versus 6.45); however, this difference (3.87) was lower than the established Minimal Important Difference (a score change that is related to a meaningful change in health status perceived by the patient) of 11 points [29]. Therefore, this difference may not be clinically relevant. Furthermore, finger range of motion was significantly more restricted in plate plus screw fixation in comparison with screw only fixation. On the other hand, patients with screw only fixation took significantly longer to return to work, but this was related to a longer period of immobilization that was necessary to prevent breaking of screws or loss of reduction. Nevertheless, it can be suggested that fixation with screw only is preferred in extra-articular spiral and oblique fractures of the proximal phalanx (Level IV).
Outcomes CRIF versus ORIF
Open reduction with lag screws did not yield better functional results than closed reduction with transversally inserted K-wires in extra-articular fractures of the proximal phalanx. Also patients experience a similar functional recovery and time to return to work was comparable (Level II, [19]). Open reduction with interosseous loop wire fixation yields better TAM scores than closed reduction with transarticular K-wire fixation (across the MCP joint) in closed or type I open fractures of the proximal phalanx in industrial workers; however, time to return to work was similar (Level IV, [20]). Al-Qattan [24] found a better active range of motion in industrial workers treated with extra-articular K-wire pinning (with open or closed reduction) when compared to CRIF with transarticular K-wire pinning for type I open extra-articular fractures of the proximal phalanx (Level IV).
CRIF with transarticular or extra-articular inserted K-wires
This systematic review showed contradictory results regarding CRIF using transarticular or extra-articular inserted K-wires. As stated earlier, Faruqui [22] did not find a significant difference in active range of motion or complication rate (as defined by authors) between CRIF with transarticular or extra-articular pinning used in closed extra-articular fractures of the proximal phalanx, whereas, on the other hand, Al-Qattan [24] did find a better active range of motion in industrial workers treated with extra-articular K-wire pinning (with open or closed reduction) when compared to CRIF with transarticular K-wire pinning. This might be explained by the fact that Al-Qattan [24] included patients with type I open fractures caused by industrial injuries. Those injuries are known to be associated with more crush and oedema. Hence, extra-articular K-wire insertion, which allows early mobilization of all joints, is expected to have better results in industrial injuries while the difference in closed extra-articular fractures caused by low-velocity injuries may not reach statistical significance. Both studies reporting on transarticular pinning have not assessed complications that might be induced by the potential cartilage damage that could be caused by transarticular pinning (across the MCP joint) such as secondary osteoarthritis or arthrosis. Thus, no definitive conclusions can be drawn upon whether transarticular pinning truly has similar complication rates as extra-articular pinning. Careful pinning is therefore always required when choosing transarticular K-wire fixation to minimize potential cartilage damage.
Limitations
The first limitation of this review was the availability of only a few prospective comparable studies. The majority of the included studies were retrospective cohort studies and case series. The conclusions that can be drawn from these studies are limited by the lack of adequate control groups, and post-treatment complications are likely to be underestimated due to the retrospective design. In addition, the methodological quality of all the included studies was generally of moderate quality.
Second, many studies failed to provide specific information on the included patients and fractures (see Table 2 for detailed information regarding fracture patterns and involved phalanx). For example, most studies did not report on the type of injury that had caused the fractures and only one study specified the degree of soft tissue crush that was present. This lack of specifications may bias the results.
Thirdly, a large variation in reported outcomes was observed across the included studies. Some studies only reported on union, whereas others evaluated a mean TAM, extension lag in the PIP joint, grip strength, angulation in any plane, infection, satisfaction, time to return back to work, etc. This implies there is no general consensus which outcome measures (both patient reported and functional) we must focus on in order to conclude whether a certain treatment is effective and whether it is more preferable than another.
Also, the mean follow-up time between the studies included in this review varied considerable, namely from 7 weeks to 40 months. This adds difficulty in comparing treatments, especially when comparing outcomes such as treatment failure and secondary procedures because length of follow-up influences these results.
Another limitation that adds difficulty in comparing treatments is the lacking consensus on several definitions between studies. Eight studies reported on TAM scores that were categorized in groups ranging from excellent to poor. However, the definition per subgroup varied substantially. An excellent TAM score varied from >220° to >250° and a poor outcome varied from no change to <180°. Also, the definition of malunion and the degree of malunion that can be accepted before considering a corrective re-intervention varied across the included studies or was not defined at all. Some studies reported that any rotational malalignment was unacceptable, whereas others still accepted a rotational malalignment of 10°. Different degrees of angulation in any plane that were still accepted varied from 10° to 25°.
Last but not least, this review included both middle and proximal phalangeal fractures. However, most of the included studies were on extra-articular proximal phalangeal fractures. This must be taken into account when interpreting the results.
Recommendations
The heterogeneity between the included studies made it impossible to adequately compare treatments and to demonstrate that one of the methods is superior. In future studies, there is need for consistency of definitions, treatment methods and structured follow-up for patients with extra-articular fractures of the proximal or middle phalanx of the hand. Despite the limitations of this systematic review, it can be recommended that closed displaced extra-articular proximal phalangeal fractures can be treated non-operatively, even fractures with an oblique or complex pattern, provided that closed reduction is possible and maintained. Conservative treatment is preferably performed with a cast/brace allowing free mobilization of the wrist. Although no definite conclusion could be drawn upon whether closed reduction with extra-articular K-wire pinning or transarticular K-wire pinning is superior, it might be suggested that extra-articular K-wire pinning is favoured. When open reduction is necessary, lag screw fixation is preferable to plate and screw fixation. But, similar recovery and functional results are achieved with transversally inserted K-wires compared to lag screw fixation.
Acknowledgements
We would like to thank Wichor. M. Bramer for his expert assistance with the systematic literature search.
Compliance with ethical standards
Conflict of interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval
This article does not contain any studies with animals performed by any of the authors.
Informed consent
For this type of study formal consent is not required.
References
- 1.Karl JW, Olson PR, Rosenwasser MP. The epidemiology of upper extremity fractures in the United States 2009. J Orthop Trauma. 2015;29(8):e242–e244. doi: 10.1097/BOT.0000000000000312. [DOI] [PubMed] [Google Scholar]
- 2.Onselen EBHV, Karim RB, Hage JJ. Prevalence and distribution of hand fractures. J Hand Surg Eur. 2003;28:491–495. doi: 10.1016/S0266-7681(03)00103-7. [DOI] [PubMed] [Google Scholar]
- 3.Laugharne E, Bhavsar D, Rajaratnam V. The distribution of hand fractures: a British perspective. Eur J Plast Surg. 2013;36(6):367–370. doi: 10.1007/s00238-012-0775-2. [DOI] [Google Scholar]
- 4.Kamath JB, Harshvardhan Naik DM, Bansal A. Current concepts in managing fractures of metacarpal and phalangess. Indian J Plast Surg. 2011;44(2):203–211. doi: 10.4103/0970-0358.85341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Oetgen ME, Dodds SD. Non-operative treatment of common finger injuries. Curr Rev Musculoskelet Med. 2008;1(2):97–102. doi: 10.1007/s12178-007-9014-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Meals C, Meals R. Hand fractures: a review of current treatment strategies. J Hand Surg Am. 2013;38A(5):1021–1031. doi: 10.1016/j.jhsa.2013.02.017. [DOI] [PubMed] [Google Scholar]
- 7.Freeland AE, Orbay JL. Extraarticular hand fractures in adults: a review of new developments. Clin Orthop Relat Res. 2006;445:133–145. doi: 10.1097/01.blo.0000205888.04200.c5. [DOI] [PubMed] [Google Scholar]
- 8.Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chow SP, Pun WK, So YC, Luk KD, Chiu KY, Ng KH, Ng C, Crosby C. A prospective study of 245 open digital fractures of the hand. J Hand Surg Br. 1991;16(2):137–140. doi: 10.1016/0266-7681(91)90162-H. [DOI] [PubMed] [Google Scholar]
- 10.American Society for Surgery of the Hand A . The hand, examination and diagnosis. 3. New York: Churchill Livingstone; 1990. [Google Scholar]
- 11.Higgins JPT, Green S (2011) Cochrane handbook for systematic reviews of interventions. Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. http://www.handbook.cochrane.org
- 12.Law M, MacDermid J. Evidence-based rehabilitation: a guide to practice. 2. Philadelphia: Slack Publishing; 2008. [Google Scholar]
- 13.Başar H, Başar B, Başçı O, Topkar OM, Erol B, Tetik C. Comparison of treatment of oblique and spiral metacarpal and phalangeal fractures with mini plate plus screw or screw only. Arch Orthop Trauma Surg. 2015;135(4):499–504. doi: 10.1007/s00402-015-2164-3. [DOI] [PubMed] [Google Scholar]
- 14.Hornbach EE, Cohen MS (2001) Closed reduction and percutaneous pinning of fractures of the proximal phalanx. J Hand Surg Br 26 B(1):45–49. doi:10.1054/jhsb.2000.0524 [DOI] [PubMed]
- 15.Nalbantoǧlu U, Gereli A, Cilli F, Uçar BY, Türkmen M. Open reduction and low-profile plate and/or screw fixation in the treatment of phalangeal fractures. Acta Orthop Traumatol Turc. 2009;43(4):317–323. doi: 10.3944/AOTT.2009.317. [DOI] [PubMed] [Google Scholar]
- 16.Franz T, Von Wartburg U, Schibli-Beer S, Jung FJ, Jandali AR, Calcagni M, Hug U. Extra-articular fractures of the proximal phalanges of the fingers: a comparison of 2 methods of functional, conservative treatment. J Hand Surg Am. 2012;37(5):889–898. doi: 10.1016/j.jhsa.2012.02.017. [DOI] [PubMed] [Google Scholar]
- 17.Franz T, Von Wartburg U, Hug U. Extraarticular proximal phalangeal fractures of the hand: functional conservative management using the lucerne cast (LuCa) a preliminary prospective study. Handchir Mikrochir Plast Chir. 2010;42(5):293–298. doi: 10.1055/s-0030-1249015. [DOI] [PubMed] [Google Scholar]
- 18.Held M, Jordaan P, Laubscher M, Singer M, Solomons M. Conservative treatment of fractures of the proximal phalanx: an option even for unstable fracture patterns. Hand Surg. 2013;18(2):229–234. doi: 10.1142/S0218810413500287. [DOI] [PubMed] [Google Scholar]
- 19.Horton TC, Hatton M, Davis TRC (2003) A prospective randomized controlled study of fixation of long oblique and spiral shaft fractures of the proximal phalanx: Closed reduction and percutaneous Kirschner wiring versus open reduction and lag screw fixation. J Hand Surg Br 28 B (1):5–9. doi:10.1054/jhsb.2002.0807 [DOI] [PubMed]
- 20.Al-Qattan MM. Closed reduction and percutaneous K-Wires versus open reduction and interosseous loop wires for displaced unstable transverse fractures of the shaft of the proximal phalanx of the fingers in industrial workers. J Hand Surg Eur. 2008;33(5):552–556. doi: 10.1177/1753193408090130. [DOI] [PubMed] [Google Scholar]
- 21.Al-Qattan MM. Extraarticular fractures of the middle phalanx with no associated tendon injury or extensive skin loss: the “soft-tissue crush” as a prognostic factor. Ann Plast Surg. 2013;70(3):280–283. doi: 10.1097/SAP.0b013e318234e934. [DOI] [PubMed] [Google Scholar]
- 22.Faruqui S, Stern PJ, Kiefhaber TR. Percutaneous pinning of fractures in the proximal third of the proximal phalanx: complications and outcomes. J Hand Surg Am. 2012;37(7):1342–1348. doi: 10.1016/j.jhsa.2012.04.019. [DOI] [PubMed] [Google Scholar]
- 23.Al-Qattan MM, Al-Zahrani K. Open reduction and cerclage wire fixation for long oblique/spiral fractures of the proximal phalanx of the fingers. J Hand Surg Eur. 2008;33(2):170–173. doi: 10.1177/1753193408087027. [DOI] [PubMed] [Google Scholar]
- 24.Al-Qattan MM. Displaced unstable transverse fractures of the shaft of the proximal phalanx of the fingers in industrial workers: reduction and K-wire fixation leaving the metacarpophalangeal and proximal interphalangeal joints free. J Hand Surg Eur. 2011;36(7):577–583. doi: 10.1177/1753193411405943. [DOI] [PubMed] [Google Scholar]
- 25.Brei-Thoma P, Vögelin E, Franz T. Plate fixation of extra-articular fractures of the proximal phalanx: do new implants cause less problems? Arch Orthop Trauma Surg. 2015;135(3):439–445. doi: 10.1007/s00402-015-2155-4. [DOI] [PubMed] [Google Scholar]
- 26.Patankar H, Meman FW. Multiple intramedullary nailing of proximal phalangeal fractures of hand. Indian j orthop. 2008;42(3):342–346. doi: 10.4103/0019-5413.39573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pehlivan O, Kiral A, Solakoglu C, Akmaz I, Kaplan H, Pehlivan O (2004) Tension band wiring of unstable transverse fractures of the proximal and middle phalanges of the hand. J Hand Surg Br 29 B (2):130–134. doi:10.1016/j.jhsb.2003.10.013 [DOI] [PubMed]
- 28.Thomas BP, Sreekanth R, Pallapati SC. Open proximal phalangeal shaft fractures of the hand treated by theta fixation. Indian j orthop. 2015;49(3):312–316. doi: 10.4103/0019-5413.156204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Polson K, Reid D, McNair PJ, Larmer P. Responsiveness, minimal importance difference and minimal detectable change scores of the shortened disability arm shoulder hand (QuickDASH) questionnaire. Man Ther. 2010;15(4):404–407. doi: 10.1016/j.math.2010.03.008. [DOI] [PubMed] [Google Scholar]