Abstract
A 95-year-old Japanese woman presented to our hospital with intermittent vomiting and several episodes of melena. Abdominal computed tomography revealed intussusception of the gastric tumor into the duodenum. After endoscopic reduction, endoscopic ultrasonography identified a hypoechogenic lesion limited to the submucosal layer. Endoscopic resection was performed as a localized treatment for the prevention of recurrent gastroduodenal intussusception. To our knowledge, there have been no other reports describing a gastric gastrointestinal stromal tumor presenting with gastroduodenal intussusception and treated using an endoscopic submucosal dissection technique.
Keywords: gastrointestinal stromal tumor, gastroduodenal intussusception, ball valve syndrome, endoscopic submucosal dissection
Introduction
Gastroduodenal intussusception is a rare occurrence that accounts for less than 10% of all intussusception cases in adults. As the majority of such cases are secondarily caused by a tumorous lesion that serves as a lead point, intussusception in adults often recurs even after successful non-operative reduction and thus requires surgical resection. We herein describe a case of a gastric gastrointestinal stromal tumor (GIST) presenting with gastroduodenal intussusception repositioned via endoscopy and resected using an endoscopic submucosal dissection (ESD) technique.
Case Report
A 95-year-old woman with dementia and a gastric submucosal tumor presented to the emergency room with intermittent vomiting and several episodes of melena. Although the tumor had been identified 10 years prior, considering the patient’s underlying diseases, no further examination was performed at the time.
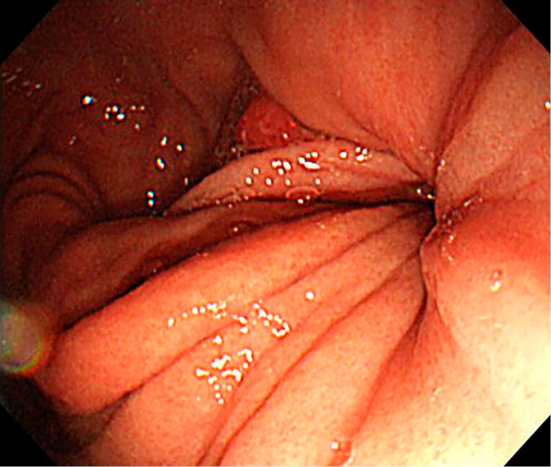
Anemia of the conjunctiva and epigastric tenderness were observed on a physical examination. Laboratory findings revealed microcytic hypochromic anemia [hemoglobin, 8.1 g/dL (normal range: 11.3-15.2 g/dL); hematocrit, 23.8% (normal range: 33.4-44.9%)]; and decreased levels of albumin [2.8 g/dL (normal range: 3.8-5.2 g/dL)]. Abdominal computed tomography (CT) revealed intussusception of the gastric submucosal tumor into the duodenum with no distant metastasis (Fig. 1). An emergency endoscopic examination revealed invagination of the gastric body into the duodenum (Fig. 2). After disinvagination by endoscopic manipulation, a submucosal tumor was identified in the lower gastric body, approximately 40 mm in diameter. Bleeding from the ulceration of the tumor was also observed (Fig. 3). All visible blood vessels were coagulated via argon plasma coagulation. Endoscopic ultrasonography (EUS) revealed a hypoechoic lesion with hyperechoic foci limited to the third (submucosal) layer (Fig. 4). The tumor size had increased slightly over the 10-year period, and the esophageal hiatal hernia had worsened. In addition to the EUS findings, narrowing of the shape in the base and easy mobility of the tumor suggested that the tumor was derived from the submucosal layer as opposed to the muscularis propria.
Figure 1.

Computed tomography scan at the level of the intussusception. The gastric tumor invaginated into the duodenum with extravasation of contrast medium.
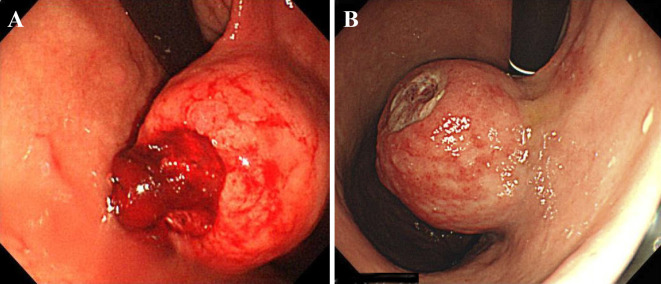
Figure 2.
Endoscopic image showing invagination of the gastric body into the duodenum. The distal stomach appeared folded.
Figure 3.
A: Endoscopic image showing a submucosal tumor with an ulcerated surface and active bleeding on the posterior wall of the gastric body. B: Retrograde distant view after endoscopic hemostasis.
Figure 4.

Endoscopic ultrasound scan showing a hypoechoic lesion with hyperechoic foci limited to the third (submucosal) layer.
Several days after exvagination, the tumor again invaginated into the duodenum, resulting in bleeding. Open laparotomy and resection of the tumor were proposed; however, the patient and her family rejected surgery under general anesthesia. Endoscopic resection was therefore performed for local treatment. ESD was performed using a dual knife (Olympus, Tokyo, Japan). The tumor was completely removed en bloc within 160 minutes. The tumor was cut into segments after ESD in order to pass it through the esophagogastric junction and retrieve it endoscopically. Although no major perforations were observed during ESD, chest radiography performed the following day showed free air in the abdomen. A minor perforation was suspected and conservatively treated with antibiotics and fasting.
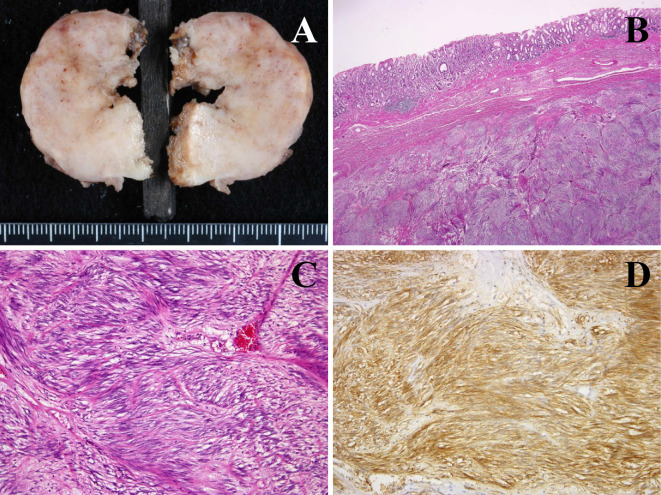
Microscopically, the tumor consisted of sheets of spindle cells with long, oval nuclei. Immunohistochemically, the tumor cells were stained positive for both c-kit protein (CD117) and CD34 and negative for α-smooth muscle actin and S-100. The staining for Ki-67, a proliferation marker, was only positive in a few cells (MIB-1 labeling index, 0.06%). The tumor was histologically diagnosed as a low-grade GIST (Fig. 5). No tumor recurrence was detected, and the patient died of old age 55 months after endoscopic treatment.
Figure 5.
Pathological analysis of the gastric mass confirmed a gastric gastrointestinal stromal tumor via positive immunohistochemical staining for c-kit and CD34. A: Macroscopic findings of the segmented tumor. B: Sheet formatted spindle cell spread in submucosal layer. C: The tumor showed the typical features of a spindle cell tumor with long, oval nuclei. D: C-kit protein immunostaining demonstrated strong cytoplasmic immunoreactivity.
Discussion
Gastroduodenal intussusception, also known as gastroduodenal invagination or ball valve syndrome, is an extremely rare event (1). It typically occurs when a gastric tumor herniates into the duodenum, causing gastric obstruction. Although gastroduodenal intussusception accounts for less than 10% of all intussusception cases in adults (2), the exact prevalence remains uncertain. Zenda et al. previously speculated that greater mobility of the tumor, a higher tumor weight resulting in drooping of the tumor, increased gastric peristalsis, and loosening of the pyloric orifice are all predisposing factors for gastroduodenal intussusception (3). In the present case, the gastric tumor size increased only slightly over a 10-year observation period, although the esophageal hiatal hernia was exacerbated. Therefore, although the exact mechanism is unknown, loosening of the surrounding tissue of the stomach may have been a major contributor towards gastroduodenal intussusception.
Gastroduodenal intussusception caused by gastric GIST is an exceedingly rare cause of gastric obstruction. To our knowledge, there have been 12 previously reported cases of gastroduodenal intussusception caused by gastric GIST (4-15). The characteristics of these 12 cases in addition to the case described here are presented in Table. These cases involved 9 women and 4 men, ranging from 29 to 95 years of age. The tumor sizes ranged from approximately 4 to 7 cm in diameter and were found to have originated in various locations, from the antrum to the fundus. Symptoms appeared from several weeks to several months before presentation at a hospital and were non-specific, including abdominal discomfort, nausea, vomiting, abdominal pain, and loss of appetite. The initial clinical presentations varied and depended on the degree of obstruction. Partial obstruction may cause chronic intermittent symptoms, while complete obstruction may cause abrupt symptoms. Indeed, Shum et al. reported a case of gastroduodenal intussusception that, incidentally, was found on routine follow-up CT scan for GIST with no symptoms of gastric outlet obstruction.
Table.
Review of Case Reports on Gastroduodenal Intussusception with GIST.
| No. | Reference | Age | Sex | Location | Size (cm) | Presentation | Treatment |
|---|---|---|---|---|---|---|---|
| 1 | 15 | 59 | F | Anterior wall of antrum |
6 | Intermittent epigastric pain and vomiting for 3 weeks |
Partial gastrectomy |
| 2 | 14 | 84 | M | Antrum | 4×3×3 | Intermittent abdominal pain, nausea, weight loss, and vomiting for 6 weeks; with dark stools |
Bilroth’s II partial gastrectomy |
| 3 | 13 | 34 | F | Fundus | 5×5, 3×2, 2×1 | Intermittent epigastric pain | Partial gastrectomy |
| 4 | 12 | 29 | M | Antrum | 6×6 | Intermittent epigastric pain, nausea, and vomiting for 5 months; with dark stools |
Bilroth’s I partial gastrectomy |
| 5 | 11 | 34 | F | Posterior wall of fundus |
6.5×4.4×3.8 | Epigastric pain | Laparoscopic wedge resection |
| 6 | 10 | 59 | F | Anterior wall | 7×6×5 | Intermittent vomiting for 5 months | Partial gastrectomy |
| 7 | 9 | 62 | F | Posterior wall of distal body |
5.2×3.5×3.2 | Worsening epigastric pain and dark stools for 3 days |
Bilroth’s II partial gastrectomy |
| 8 | 8 | 78 | F | Antrum | 4.5×3.3×3.4 | Persistent epigastric discomfort and vomiting for 1 week |
Laparoscopic wedge resection |
| 9 | 7 | 52 | F | Fundus | 5×5 | Worsening epigastric pain and vomiting for 1 day |
Laparoscopic wedge resection |
| 10 | 6 | No data | M | Fundus | No data | Intermittent pain and vomiting for 1 year |
No data |
| 11 | 5 | 74 | M | Posterior wall | No data | Intermittent vomiting for 3 weeks | Partial gastrectomy |
| 12 | 4 | 85 | F | Fundus | 6×5 | Abdominal discomfort, nausea, and weight loss for 6 months; acute, severe abdominal pain and vomiting |
Subtotal gastrectomy |
| 13 | Present case | 95 | F | Posterior wall of distal body |
4.2×3.9 | Vomiting and loss of appetite for 1 week and dark stools |
Endoscopic submucosal dissection |
Gastroduodenal intussusception caused by gastric GIST is essentially treated via surgical resection of the tumor. In the case presented here, although reduction of intussusception was endoscopically performed, the tumor invaginated again within several days. We performed endoscopic resection as opposed to surgical resection to remove the tumor, due to the patient’s age (95 years). Several authors have described the usefulness of ESD for small and asymptomatic gastric submucosal tumors (16,17). It was recently reported that endoscopic resection of subepithelial tumors of the stomach has a high success rate with few adverse events (18). In the present case, EUS suggested that the tumor was located within the submucosal layer without involvement of the muscular layer. Therefore, ESD was performed as an alternative to surgery. The tumor was resected en bloc despite its relatively large size. However, because the tumor was divided into segments in the stomach in order to retrieve it perorally, it was difficult to pathologically identify the origin of the GIST and whether it was derived from the muscularis mucosae or proper muscular layer. Furthermore, a minor perforation was suspected in the present case. Several studies have reported that perforation during ESD for gastric GIST occurs in 5% to 15% of cases (19), and no cases of seeding or plantation have been reported. Moreover, recent investigations have demonstrated that perforation during ESD for early gastric carcinoma does not lead to dissemination (20). Similarly, it is assumed that GISTs are at low risk for plantation.
The standard treatment for gastric GISTs is complete surgical resection (21) through conventional open surgery. Less invasive approaches, such as laparoscopic-endoscopic cooperative surgery (LECS) (22), non-exposed endoscopic wall-inversion surgery (NEWS) (23), and a combination of laparoscopic and endoscopic approaches to neoplasia with non-exposure technique (CLEAN-NET) (24), have been developed in recent years. However, these techniques and devices are only available at select institutions. In addition, these treatments are invasive for elderly patients, as general anesthesia and artificial ventilation are required. In contrast to treatments involving laparotomy or laparoscopy, endoscopic resection using the ESD technique is minimally invasive. Therefore, endoscopic resection is considered an option for the treatment of gastroduodenal intussusception caused by gastric GIST originating in the muscularis mucosae, particularly in patients of advanced age and/or with severe underlying disorders in whom general anesthesia and artificial ventilation are risky procedures. If surgical treatment is inadequate, conservative management should be considered before endoscopic treatment. The operative stress, risks of anesthesia, and patient's performance status should be included as evaluation criteria, as well as the age and underlying disease. The method of management must be discussed from a comprehensive perspective.
In summary, we present a case of a gastric GIST with gastrointestinal hemorrhaging and gastroduodenal intussusception that was treated with ESD. We believe that endoscopic resection is an acceptable alternate treatment for elderly patients who are not candidates for surgery.
The authors state that they have no Conflict of Interest (COI).
References
- 1.Hobbs WH, Cohen SE. Gastroduodenal invagination due to a submucous lipoma of the stomach. Am J Surg 71: 505-518, 1946. [DOI] [PubMed] [Google Scholar]
- 2.Stubenbord WT, Thorbjarnarson B. Intussusception in adults. Ann Surg 172: 306-310, 1970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zenda T, Masunaga T, Taguchi T, et al. A case report of gastroduodenal intussusception caused by a leiomyoma arising from upper gastric body (so-called ball valve syndrome). Nihon Shokakibyo Gakkai Zasshi 91: 1228-1233, 1994. (in Japanese). [PubMed] [Google Scholar]
- 4.Yildiz MS, Dogan A, Koparan IH, Adin ME. Acute pancreatitis and gastroduodenal intussusception induced by an underlying gastric gastrointestinal stromal tumor: a case report. J Gastric Cancer 16: 54-57, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.M S PB, Reddy CK, Augustine AJ, Sagari SG. Gastroduodenal intussusception due to pedunculated polypoid gastrointestinal stromal tumour (gist): a rare case. J Clin Diagn Res 9: PD05-PD06, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Indiran V, Vinoth Kumar R, Maduraimuthu P. Gastrointestinal stromal tumor presenting as gastroduodenal intussusception. Indian J Gastroenterol 34: 347-348, 2015. [DOI] [PubMed] [Google Scholar]
- 7.Rittenhouse DW, Lim PW, Shirley LA, Chojnacki KA. Gastroduodenal intussusception of a gastrointestinal stromal tumor (GIST): case report and review of the literature. Surg Laparosc Endosc Percutan Tech 23: e70-e73, 2013. [DOI] [PubMed] [Google Scholar]
- 8.Wilson MH, Ayoub F, McGreal P, Collins C. Gastrointestinal stromal tumour presenting as gastroduodenal intussusception. BMJ Case Rep 2012: bcr2012006787, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Basir N, Yaakub AB, Kafeel G, et al. Gastroduodenal intussusception as a first manifestation of gastric gastrointestinal stromal tumor. Turk J Gastroenterol 23: 185-186, 2012. [DOI] [PubMed] [Google Scholar]
- 10.Gyedu A, Reich SB, Hoyte-Williams PE. Gastrointestinal stromal tumour presenting acutely as gastroduodenal intussusception. Acta Chir Belg 111: 327-328, 2011. [PubMed] [Google Scholar]
- 11.Chan CT, Wong SK, Ping Tai Y, Li MK. Endo-laparoscopic reduction and resection of gastroduodenal intussuception of gastrointestinal stromal tumor (GIST): a synchronous endoscopic and laparoscopic treatment. Surg Laparosc Endosc Percutan Tech 19: e100-e103, 2009. [DOI] [PubMed] [Google Scholar]
- 12.Siam FA, Siow SL. Stomach gastrointestinal stromal tumours (GIST) intussuscepted into duodenum: a case report. Malays J Med Sci 15: 68-70, 2008. [PMC free article] [PubMed] [Google Scholar]
- 13.Shum JS, Lo SS, Ka SY, Yeung CW, Ho JT. Gastroduodenal intussusception. Abdom Imaging 32: 698-700, 2007. [DOI] [PubMed] [Google Scholar]
- 14.Adjepong SE, Parameswaran R, Perry A, et al. Gastroduodenal intussusception due to gastrointestinal stromal tumor (GIST) treated by laparoscopic billroth II distal gastrectomy. Surg Laparosc Endosc Percutan Tech 16: 245-247, 2006. [DOI] [PubMed] [Google Scholar]
- 15.Crowther KS, Wyld L, Yamani Q, Jacob G. Case report: gastroduodenal intussusception of a gastrointestinal stromal tumour. Br J Radiol 75: 987-989, 2002. [DOI] [PubMed] [Google Scholar]
- 16.Huang ZG, Zhang XS, Huang SL, Yuan XG. Endoscopy dissection of small stromal tumors emerged from the muscularis propria in the upper gastrointestinal tract: preliminary study. World J Gastrointest Endosc 4: 565-570, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Catalano F, Rodella L, Lombardo F, et al. Endoscopic submucosal dissection in the treatment of gastric submucosal tumors: results from a retrospective cohort study. Gastric Cancer 16: 563-570, 2013. [DOI] [PubMed] [Google Scholar]
- 18.Godat S, Robert M, Caillol F, et al. Efficiency and safety of endoscopic resection in the management of subepithelial lesions of the stomach. United European Gastroenterol J 4: 250-256, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Park JJ. Long-term outcomes after endoscopic treatment of gastric gastrointestinal stromal tumor. Clin Endosc 49: 232-234, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ikehara H, Gotoda T, Ono H, Oda I, Saito D. Gastric perforation during endoscopic resection for gastric carcinoma and the risk of peritoneal dissemination. Br J Surg 94: 992-995, 2007. [DOI] [PubMed] [Google Scholar]
- 21.Poveda A, del Muro XG, Lopez-Guerrero JA, et al. GEIS 2013 guidelines for gastrointestinal sarcomas (GIST). Cancer Chemother Pharmacol 74: 883-898, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hiki N, Nunobe S, Matsuda T, Hirasawa T, Yamamoto Y, Yamaguchi T. Laparoscopic endoscopic cooperative surgery. Dig Endosc 27: 197-204, 2015. [DOI] [PubMed] [Google Scholar]
- 23.Mitsui T, Niimi K, Yamashita H, et al. Non-exposed endoscopic wall-inversion surgery as a novel partial gastrectomy technique. Gastric Cancer 17: 594-599, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Inoue H, Ikeda H, Hosoya T, et al. Endoscopic mucosal resection, endoscopic submucosal dissection, and beyond: full-layer resection for gastric cancer with nonexposure technique (CLEAN-NET). Surg Oncol Clin N Am 21: 129-140, 2012. [DOI] [PubMed] [Google Scholar]