Abstract
We describe the current state of mHealth skills acquisition, education, and training available to clinical professionals in educational programs. We discuss how telemedicine experienced exponential growth due in large part to the ubiquity of the mobile phone. An outcome of this unprecedented growth has been the emergence of the need for technology skills training programs for clinicians that address extant curricula gaps. We propose a model to guide the development of future training programs that incorporate effective training strategies across five domains: (I) digital communication skills; (II) technology literacy and usage skills; (III) deploying telehealth products and services; (VI) regulatory and compliance issues; and (V) telehealth business case. These domains are discussed within the context of interprofessional teams and broader organizational factors.
Keywords: mHealth, academic model, technology skills
The impetus for this paper is to bring to the foreground a discussion of the potential for a new model for mHealth skills training for clinicians. The use of mHealth in diagnosing and treating patients is a relatively recent phenomenon, and there is scant evidence of curricula changes to reflect the challenges of integrating mHealth skills into training programs. Too often educational institutions assume that clinicians will either acquire mHealth skills on the job or assume that as digital natives, the students have grown up along with technology and can easily facilitate the transition to professional practice with mobile technologies. However, mHealth is a major technological phenomenon that deserves significant educational reformation and consideration in medical curricula.
The need for a new model
Change is rapid and ubiquitous in healthcare and nowhere is this more evident than in deployment of mHealth products and services. This technology-centric industry movement has been described as “a natural, inevitable and necessary evolution” (1) from the expected “point of care” occurring in the clinician’s physical location. Medical professionals are increasingly connecting with patients via email, telephone, and webcam, and using these same tools to consult with each other electronically. Moreover, mHealth and related technologies extend the boundaries of healthcare beyond the walls of the physical facility allowing medical professionals to provide quality healthcare services in places that previously were unreachable. For example, doctors without borders located in Niger, Sudan and elsewhere report using the Internet to engage a network of almost 300 experts around the world for assistance with the toughest of clinical cases (2).
A key function of healthcare applications of digital technologies is facilitating electronic communication and data exchange between patients and healthcare providers. These systems have demonstrated the capability to facilitate and improve patients’ access to some forms of care, and their perception of quality of care received is good (3). Additionally, studies of mobile systems that allow for the exchange of health information between patients and medical professionals have been shown to substantially reduce the number of hospital admissions in sample populations, thereby reducing costs (3,4). Personal mobile computers, such as smartphones, tablets, and other Internet-linked devices, are ubiquitous. Publicly accessible platforms such as Skype enable audio and video communications between patients and providers without regard for geographical distance, thus enabling a more aggressive deployment of telemedicine services and programs.
While research on increased use of digital technologies in healthcare delivery has been linked to improved healthcare outcomes and suggests strong potential for further optimization, relatively few clinical professionals have been formally trained to deliver their professional services using these devices. In this same vein, few medical professionals have received education or training in communication skills using digital technologies. Many academic institutions do not integrate formal coursework or incorporate clinical practice experiences specific to using digital technologies for patient encounters in their professional curricula. Healthcare technology innovation has created what amounts to a new lens through which educators must reinterpret curriculum needs to address modes of delivering healthcare other than the historic face-to-face model in addition to preparing graduates to employ current diagnostic and treatment modalities and associated technology tools.
Thus, this article proposes a set of core competencies to inform design of clinical skills training to utilize technology-enhanced delivery models for health professionals. Integrating these skill-building activities into academic and professional development programs will be challenging, but necessary in order to improve clinical professional competency in technology-centric care and widespread adoption of mobile health devices and services. This is not a call to abandon any components of conventional medical education and training programs, rather, the integration of digital technology content into clinical training programs should be viewed as a necessary enhancement that ultimately will benefit both providers and patients.
Roots of technology-assisted healthcare delivery
While technology has been a driving force in changing the way routine job activities are performed in most industries, healthcare was a laggard adopter of information technology. Most early computer adoption in healthcare was limited to financial and business processes, often using mainframe computers, and clinical processes were not automated until well past the advent of distributed processing capability.
The earliest forms of telemedicine, hard-wired telephone lines and limited video capability, entered the healthcare environment less than 50 years ago. Early use was essentially a means for providing limited diagnostic services and monitoring of chronic health conditions for persons living in rural areas (4). Technology innovations continue to be primary drivers in the evolution to the current capability for robust remote and mobile health care delivery, especially broadband wireless communication and high-speed data processing. In particular, more than two billion smartphones and other mobile devices provide individuals worldwide with a continuous wireless global connection that can be used to access a wide range of healthcare information and services.
Most telemedicine and digital health initiatives have been under the purview of individual healthcare organizations or health systems, generally as a means to improve access to important services or to reduce costs of providing needed services to a particular category of patients, such as those with chronic conditions that require predictable types of support. A 2016 Department of Health and Human Services report to Congress estimated that “61 percent of healthcare institutions currently use some form of telehealth,” including 40–50% of hospitals (5). The same report estimated the 2013 telehealth market at 9.6 billion dollars of revenue, representing 60% growth in 1 year. The University of Pittsburgh Medical Center’s Chief Information Officer described telemedicine as “fundamental to (our) efforts … (going) right to the heart of the value-based movement” (1).
Currently, medical professionals use telemedicine and other digital technologies to both supplement face-to-face care and to treat several chronic conditions comprehensively. In one umbrella review of 58 systematic reviews, the predominant use of telehealth was for remote patient monitoring, communication with patients, and providing counseling or psychotherapy for patients with conditions related to cardiovascular disease, diabetes, behavioral health complications, rehabilitation, and respiratory disease (3).
While rural areas often demonstrate the greatest need for improved access to healthcare, many barriers hamper increasing that access, even when telemedicine technologies are available. Stating a complex situation simplistically, retaining skilled practitioners in remote areas is often difficult. In addition to the social aspects of rural living (which may contrast strongly with the urban attractions surrounding most academic medical centers), a lack of access to ongoing professional training and clinical supervision, peer consultation networks, and the nature of rural medicine also influence rural practitioner retention (6).
Insufficient support resources, including development and application of skills in clinical technologies, compromise the health professionals’ ability to administer effective care, which subsequently discourages long-term perseverance in rural medical practice. This migration of medical professionals out of rural practice creates a cyclical relationship that in turn results in fewer opportunities for emerging practitioners to receive professional practice education and training in rural settings, which leads to fewer medical professionals being prepared to administer healthcare effectively in remote areas.
Changing the landscape of healthcare with digital technology skills
In Europe, there are single authorities that oversee the training and education of health professionals and telemedicine is included in this training. However, in the United States, there is no single point of contact that mandates the incorporation of specific training. As a result, the amount and type of telemedicine training and education is the purview of each clinical domain, and no mandate or oversight agency guarantees appropriate inclusion or standardized content and skills development.
Prior to the early twentieth century, much of academic medicine was rooted in private practice, following an apprenticeship model that resulted in wide variation in education and training approaches. However, with the assimilation of medical education into universities, where it eventually became standardized in terms of admission requirements, curricula, and training, medicine effectively moved toward a model of physician dominance of medical practice and oversight of other clinical professions, including the education, training, and practice requirements of those professions (7).
The pendulum appears to be swinging away from physician dominance toward a shared or team approach in which interprofessional care teams representing multiple health professions provide patient care in collaboration. This approach is in large part attributable to rising health care costs, the growing complexity of patient care options, and the delivery environment itself. The delivery environment incorporates sophisticated technology applications, including telemedicine alternatives, and regulation and payment models that are increasingly defining the “current” healthcare environment.
The ability to use mobile technologies such as smartphones and tablets to connect patients with a team of healthcare providers enables much-needed access to a variety of healthcare services anywhere, anytime, and at lower costs. While this technological capability provides a new avenue for patient-provider engagement, a particularly salient point that is often unaddressed is the introduction of a third partner into the physician-patient relationship. That is, the organization furnishing the technology and establishing the parameters of the virtual encounter (8). Realistically, the partnership has expanded and now involves a team of professionals, all of whom may engage directly with the patient as well as with each other. The desirable interprofessional healthcare team involves more stakeholders than doctors and patients, and the conversation among these stakeholders becomes more complex, incorporating needs for data sharing and issues of interoperability (9). The ability of all health professionals to work effectively as a collaborative, integrated healthcare team that values diversity and cultural competence is pivotal to success in the current healthcare model. Ideally, this team is skilled in employing multiple delivery models, including telemedicine.
Current medical and health professional students (and recent graduates) are in the cohort of digital natives—the first generation born and educated in a digital environment. They grew up surrounded by digital technology, and are extremely comfortable with personal and work-related computing and communication devices. However, the comfort factor alone does not guarantee that this cohort will be able to perform high quality care via telemedicine approaches. While these students do have an advantage in their familiarity and comfort with technology, their skills in using the technology as an alternative to face-to-face interaction must be developed through structured training (10). Examples of core requirements identified previously include digital literacy, basic health information technology skills, and appropriate security and privacy training (11).
Proposed key technology competencies for clinicians
Some authors have described many of the desirable technology skills for clinicians as “not novel” (12), at least with regard to their profession of focus (i.e., nursing), while others suggest that what telehealth providers need is a “new skill mix” (11). We find merit in both contentions. While the skill set we propose includes nothing “new” per se, the skills have not necessarily developed concurrently with and in the context of the relevant professional body of knowledge, and some may not be introduced at all.
Our proposed educational model for preparing health professionals to deploy mHealth interventions successfully is illustrated in Figure 1. The model presumes the individual mastery of the relevant clinical or professional bodies of knowledge and associated technical skills, and suggests five knowledge and skills areas specific to using biomedical and communication technologies effectively in the delivery of healthcare services using a telehealth delivery modality. These recommended areas are: (I) digital communication skills; (II) technology literacy and usage skills; (III) mHealth products and services; (VI) regulatory and compliance issues; and (V) the technology business case. Additionally, it is important to remember that in actual delivery of telemedicine services, the organizational context becomes important as a driver of process and policy (8), and organizational issues should be addressed concurrently with other areas of study, particularly for those training components in the job setting.
Figure 1.
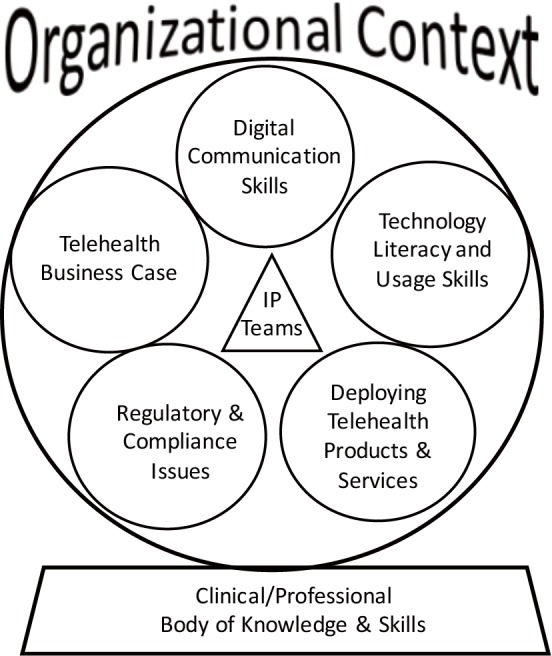
The proposed organizational framework for a model of training and education on core competencies related to mHealth and telemedicine for clinical professionals. IP, interprofessional teams.
Digital communication skills
As noted previously, although recent and emerging clinical professionals are digital natives, some experienced healthcare providers may have insufficient comfort and skill with a range of computing devices and emerging technologies. Nevertheless, even for digital natives, social digital communication differs greatly from the type of information exchange required in a healthcare encounter. Eliciting information in a face-to-face encounter permits auditory and visual cues that are more nuanced or may be absent in a virtual encounter, unless they are specifically probed. Physicians must learn effective means of interviewing and examining patients using two-way auditory, video, and digital data. While basic communication concepts can be outlined in a brief document, digital communication is essentially a behavioral skill learned best through application, feedback, and practice. One recommended approach is for students to complete digital on-call training (10), which enables their mentors to give feedback and guidance about how to improve their skills.
Technology literacy and usage skills
Technology alone will not transform healthcare, and while digital literacy is important, it is not sufficient. In order to optimize the potential of telemedicine tools, providers must know how and when to use them for specific purposes. The provider’s purposes may be clinically driven, but just as often, the organization’s goal may be to achieve better patient compliance or satisfaction, or even for financial benefit. Medical trainees often are well versed in various digital technologies, but the actual practice of telemedicine as an integrated delivery approach is not necessarily intuitive just because the individual technology components can be operated correctly.
Graduates must use their knowledge across a myriad of organizational contexts. Consequently, physicians must learn to offer a level of telemedicine care that is the equivalent of an in-person consultation (10). Clinical rotations through telemedicine services are useful in understanding the “big picture” of the delivery model, but a simulated learning environment could be very effective as well, perhaps using standardized patients (13). Conference presentations, journal articles, and other professional information exchange forums are important means of continued learning as technologies and delivery models evolve.
Deploying telehealth products and services
The clinical benefits of technology-centric healthcare cannot be realized if the business model is unsound, or if the delivery model is unsustainable over time (14). Thus, successful deployment of mHealth, which is effectively creating new ways of delivering care, “requires managing multiple stakeholders, policies, and organizational dynamics, in addition to having a thorough understanding of the technology involved.” (14).
Collaboration among members of an interprofessional team with diverse knowledge, experience, and skills is paramount to design, implementation, and evaluation of telehealth programming just as it is with any facet of healthcare delivery. Team-based training is particularly relevant for this domain of knowledge. Individuals must understand team roles and dynamics, participative decision-making models, and conflict management and consensus building techniques. Scenario case studies, both classroom-based and in professional development sessions, can provide effective means of engaging participants in discussion, offer opportunities for role-playing, and allow reflective self- and peer-assessment of team outcomes.
Regulatory and compliance issues
Regulation is pervasive in the healthcare industry, and information security breaches not only can result in significant financial risks for organizations, they often engender high profile and undesirable media attention that may have negative reputational impacts as well. Therefore, the importance of comprehensive knowledge about regulation of telehealth products and services and associated liability for improper use cannot be overstated. Government agencies such as the Federal Communications Commission, the Federal Trade Commission, the Food and Drug Administration, and the Department of Health and Human Services are key players in regulation of telemedicine. Specific legislation, such as the Health Insurance Portability and Accountability Act (HIPAA) and the Health Information Technology for Economic and Clinical Health Act (HITECH), include stringent requirements related to data privacy and security, and have severe penalties for non-compliance. Foundation knowledge can be incorporated in classroom or online programming, but the dynamic nature of the regulatory environment mandates regular “updates” through workshops, webinars, newsletters, and other efficient, focused information transmissions.
The telehealth business case
The business case and the clinical evidence-based case (i.e., cost, access), are important for both clinicians and managers to consider. Ideally, the clinical and business perspectives of issues should be explored concurrently to achieve the best potential outcomes without detriment to either side. Again, this topic is best explored using team-learning approaches, such as case analyses and simulation or role-playing. For example, clinicians could present a clinical rationale for a telemedicine product and managers could rebut with the business case, or vice versa, and the team collectively could generate a cost-benefit analysis of the proposed program. Individuals will develop relevant foundation skills in their clinical or business education background, but the collaborative evaluation of proposed products and services needs to occur within the organizational context.
Current challenges in the administration and integration of telemedicine education
Unfortunately, current medical professionals (as a collective) have had minimal exposure to telemedicine delivery concepts during their education and training. These individuals also typically receive few opportunities for skill development and acquisition during, or even subsequent to, their academic training. Compounding this issue, no academic discipline lays specific claim to telemedicine-related bodies of knowledge. For example, the fields of biomedical technology and information sciences, cognitive psychology, healthcare quality and safety, and ethics and health law, all have established streams of research and training related to telemedicine and mHealth. This presents the potential for a lack of cross-discipline training for clinical and medical professionals interacting with patients through telemedical means. More cross-communication between these fields is necessary to inform the education and training of current medical students.
Another major challenge, with regard to continuing innovation and deployment of telemedicine, will be forecasting health workforce skills and training needs in the context of integrated delivery models that involve virtual service delivery and implementing responsive programming. These evolving skill needs likely will encompass changes in educational planning across a variety of clinical professions. Instead of each clinical discipline reinventing the wheel in terms of developing telemedicine knowledge and skill sets, a core set of fundamental skills and knowledge could be defined to which medical disciplines might add specific requirements or contextual frameworks for their particular domains of professional practice.
Limitations of current telemedical training and education
Robust academic programming to teach medical professionals how to employ telemedicine technologies effectively has not been well defined, and little has been done to motivate clinicians to explore technology-assisted alternatives to face-to-face care. In fact, some suggest that formal training in telemedicine-based services is deficient relative to the widespread need for such skills (15). Most existing training is designed for individuals who have finished their professional training, and focuses on relatively quick acquisition of selected practical skills and concepts. For example, many programs offer continued learning credits for workshops that last only a few hours (16,17).
Additionally, there is little tailoring to teach these specific skills in the context of the professional discipline, and there is little standardization and uniformity across training programs with regard to the core competencies (15). In short, some training programs emphasize certain skills, while others do not. This approach results in a uniquely trained workforce, but not necessarily a holistically trained workforce.
Despite some localized efforts, the fact remains that many medical professionals have had minimal exposure to telemedicine concepts during or subsequent to their academic training. In one survey of family physicians, 41% (638/1,557) of respondents indicated that one of the biggest barriers to using technology-assisted delivery systems in their practice was a lack of training (18). Others have reported that a lack of training and education has created hesitation in the adoption of telehealth systems (19).
Conclusions
As stated at the outset, the impetus for this paper was to propose a model representing a set of core competencies to inform design of training and education for clinical professionals who will use digital technologies to deliver their professional services. There is a paucity of information available on such training programs, and there is little evidence that much formal training actually occurs in either the public or private sectors. In addition, there is little to no transparency about what is occurring in terms of training at academic intuitions.
While recent and future medical graduates will benefit from current and pending medical curriculum reforms, a very large segment of the medical workforce, as well as other clinical and administrative professionals, will not receive the scope of education needed to be effective providers in the current technology-rich and highly regulated environment. Educational intervention on a large scale, and in a relatively short timeframe, is needed to build system-wide competency in employing telemedicine technologies to achieve reliability of desired patient and organizational outcomes.
It is also naïve to assume that clinicians will be able to deliver telemedicine services safely and of high quality without formal and systematic training. After all, there are intrinsic differences between the practice of traditional medicine and that of telemedicine. Students must have opportunities to directly compare and contrast traditional medicine practices with those of telemedicine. Doing so will permit them to recognize when it is safe and appropriate to use a telemedicine approach and to acquire and ultimately adopt best practices (10).
Given these caveats, it is important to consider what is needed to meet the future. First, one important answer is an aggressive commitment to the education and training of physicians and other clinical professionals so as to promote their use of telemedicine tools that will not only empower their patients but also themselves (20). Medical education will continue to be challenged to leverage health technologies in service of patients. Doing so will require updating curricula to reflect advances in both the scientific domains and in technologies. The ATA may be a source of valuable resources to informing curriculum development (9).
Second, both didactic and applied components for telemedical training are needed to build core skills. Simulation-based training offers risk-free opportunities for hands-on practice and should be pursued. Building the training to be delivered in an interprofessional team context, and incorporating organizational factors will be a key success factor.
Third, as with any significant organizational endeavor associated with large scale change, the role of leadership in creating and maintaining an institutional environment that supports technology-assisted delivery of safe, effective health care cannot be overstated. The responsibility of leadership in achieving quality healthcare outcomes, regardless of the mode of delivery, is regularly emphasized in professional and research literature.
Finally, this proposed model for training and education on core competencies related to telemedicine and telehealth is intended to generate discussion among stakeholders and change agents, a starting point. Much work will be required to establish and validate competencies and to develop the curricula and learning forums to achieve broad scale competence among health professionals who will deliver their services using a broad array of current and emerging technologies.
Acknowledgements
None.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Bowman D. UPMC’s Andrew Watson: Telemedicine a natural evolution of care. Available online: http://www.fiercehealthcare.com/it/upmc-s-andrew-watson-telemedicine-a-natural-evolution-care
- 2.Beck M. How telemedicine is transforming healthcare. Available online: http://www.wsj.com/articles/how-telemedicine-is-transforming-health-care-1466993402
- 3.Totten AM, Womack DM, Eden KB, et al. Telehealth: Mapping the Evidence for Patient Outcomes From Systematic Reviews [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2016. [PubMed] [Google Scholar]
- 4.Malvey D, Slovensky D. mHealth: Transforming Healthcare. New York, NY: Springer; 2014. [Google Scholar]
- 5.Mack H. HHS report outlines problems, potential of telemedicine. Available online: http://mobihealthnews.com/content/hhs-report-outlines-problems-potential-telemedicine
- 6.Wood JA, Miller TW, Hargrove DS. Clinical Supervision in Rural Settings: A Telehealth Model. Prof Psychol Res Pr 2005;36:173-9. 10.1037/0735-7028.36.2.173 [DOI] [Google Scholar]
- 7.Starr P. The social transformation of American medicine. New York, NY: BasicBooks, Inc.; 1982. [Google Scholar]
- 8.Malvey DM, Slovensky DJ, Alderman B, et al. The mHealthcare Team: Beyond Doctors and Patients [workshop]. Fort Worth, TX: Annual Meeting of the Society for Design and Process Science; 2015. [Google Scholar]
- 9.DeJong C, Lucey CR, Dudley RA. Incorporating a new technology while doing no harm virtually. JAMA 2015;314: 2351-2. 10.1001/jama.2015.13572 [DOI] [PubMed] [Google Scholar]
- 10.Pathipati AS, Azad TD, Jethwani K. Tele-medical education: Training digital natives in telemedicine. J Med Internet Res 2016;18:193-6. 10.2196/jmir.5534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fisk MJ. Necessary skills and knowledge for staff providing telehealth service. In: Jordanova M, Lievens F. Global Telemedicine and eHealth Updates: KnowledgeResources. Basel, Switzerland: International Society for Telemedicine and eHealth; 2014. [Google Scholar]
- 12.van Houwelingen CT, Moerman AH, Ettma RG, et al. Competencies required for nursing telehealth activities: A Delphi-study. Nurse Educ Today 2016;39:50-62. 10.1016/j.nedt.2015.12.025 [DOI] [PubMed] [Google Scholar]
- 13.Miller GE. The assessment of clinical skills/competence/performance. Acad Med 1990;65:S63-7. 10.1097/00001888-199009000-00045 [DOI] [PubMed] [Google Scholar]
- 14.Driver M. Is the mHealth industry facing a skills shortage? Available online: http://www.thejournalofmhealth.com/single-post/2016/07/25/Is-the-mHealth-Industry-Facing-a-Skills-Shortage
- 15.Colbow AJ. Looking to the Future: Integrating Telemental Health Therapy intoPsychologist Training. Train Educ Prof Psychol 2013;7:155-65. 10.1037/a0033454 [DOI] [Google Scholar]
- 16.University of California-Davis. Center for Telehealth and Technology: TelehealthEducation Program. Available online: http://www.ucdmc.ucdavis.edu/cht/education/telehealth/courseinfo.html
- 17.American Telemedicine Association.Upcoming Events. Available online: http://www.americantelemed.org/events-and-education/upcoming-events
- 18.Klink K, Coffman M, Moore M, et al. Family Physicians and Telehealth: Findings from a National Survey. Washington, D.C.: Robert Graham Center; 2015. [Google Scholar]
- 19.Perle JG, Burt J, Higgins WJ. Psychologist and Physician Interest in Telehealth Training and Referral for Mental Health Services: An Exploratory Study. J Technol Hum Serv 2014;32:158-85. 10.1080/15228835.2014.894488 [DOI] [Google Scholar]
- 20.Topol E. The patient will see you now. New York, NY: Basic Books, Inc.; 2015. [Google Scholar]


