Abstract
A rare case of a giant thymoma in a patient witness of Jehova treated by single port thoracoscopic resection is reported. A 78-year-old man with chest pain and mild dyspnea had been previously diagnosed with giant thymoma went to our hospital and asked for second opinion of operation. Computed tomography showed a 12.5 cm × 9.5 cm × 10 cm mass in the anterior mediastinum. Under the request of this patient, he is only willing to receive minimal invasive surgery without blood transfusion. Thirty-six hours after surgical resection, the patient safely discharged from our hospital without complication. Pathological diagnosis indicated a thymoma without capsular invasion, and a diagnosis of Masaoka stage I thymoma was made. Giant mediastinal thymoma is not rare, but how to perform minimal invasive surgery without complication and blood transfusion is a great challenge even for an experienced surgeon.
Keywords: Giant thymoma, single port video-assisted thoracic surgery (VATS), mediastinal tumor
Introduction
Thymoma is one of the common types of anterior mediastinal tumor and trans-sterno thymectomy is the standard treatment of early or advanced thymoma patients. With the development of thoracoscopic surgical instruments and techniques in recent year, single port video assisted thoracoscopic thymectomy are increasing practiced for the treatment of thymoma patients (1,2). However, for giant anterior mediastinal tumor, the feasibility and safety of single port video-assisted thoracic surgery (VATS) thymectomy are being questioned. This report describes a case of large thymoma (12.5 cm) that was successfully removed by singe port VATS without sternotomy in a patient witness of Jehova.
Case presentation
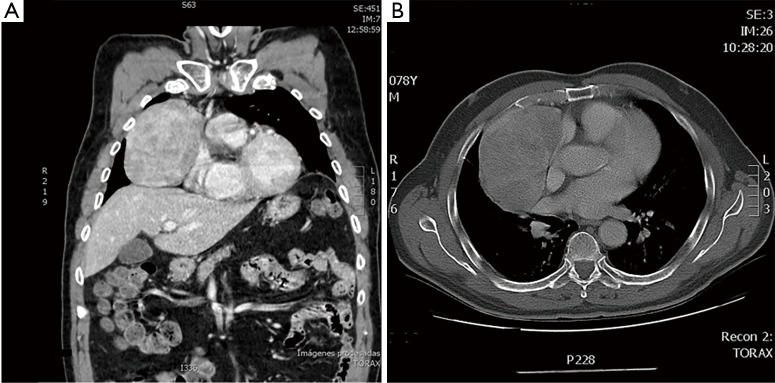
A 78-year-old man without significant medical history suffered from chest pain for 3 months and came to the outpatient clinical for help. The initially plain film revealed a huge chest mass and then chest computed tomography (chest CT) with contrast was arranged for further evaluation. Chest CT showed a large inhomogeneous mass with capsule in the anterior mediastinal space, consistent with anterior mediastinal tumor (Figure1A,B). Fine needle aspiration showed the mass was thymoma AB. The initial consultation doctor told the patient it was necessary to do a sternotomy to retrieve the tumor and then the patient refused this option and came to our hospital for second opinion. When we explained the benefit and risk of operation to the patient, the patient revealed himself a Jehovah's Witnesses and he was eager to receive minimal invasive surgery and any kind of blood transfusion was forbidden. However, we still well informed the possibility of conversion to open surgery to retrieve the specimen.
Figure 1.
Chest CT in frontal (A) and axial (B) views of the heterogeneous right side anterior lateral mass with complete capsule of the tumor.
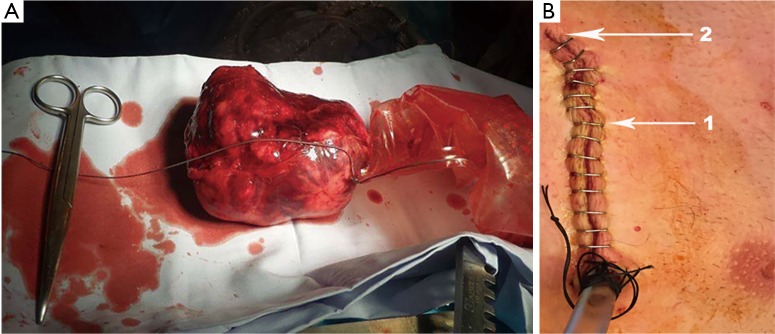
The patient elected to receive right side single port VATS thymectomy. After the patient was intubated with double lumen endotracheal tube, he was positioned in a 30-degree semi-supine position on the operating table with a roll placed beneath the shoulder and the ipsilateral arm held abducted over a padded L-screen in order to expose the axilla area. The 4th intercostal space was chosen for wound creation. When the 30-degree high resolution lens was introduced in the chest cavity, one huge well capsulated thymoma leaped out at operator. We start to dissect the tumor from surrounding tissue with suction tube and harmonic scalpel. Mediastinal pleural was opened first and then dissected the tumor from pericardium and kept the tumor capsule and pericardium intact. It is very difficult to resect the such kind of huge thymoma with whole thymus tissue at once, thus we decided to do en bloc resection of the huge thymoma first and then resect the residual thymus horn and tissue. Finally, the thymoma was carefully dissected, and complete excision was achieved. The tumor was 12.5 cm × 9.5 cm × 10 cm (Figure 2A) through a 6-cm wound (Figure 2B), whole operation blood loss and operation time were 90 mL and 105 min (Figure 3). Due to the well recovery of this patient, we removed the chest tube on the next operation day and the patient discharged from hospital on the postoperative 36 h. Final pathological revealed the giant tumor was a Masaoka stage I tumor a whole tumor capsule was intact under microscopic examination.
Figure 2.
Surgical images. (A) Surgical specimen of the thymoma, (B) original wound was only to arrow 1, due to the huge size, wound was enlarged to arrow 2 (6 cm in size) to retrieve the tumor out of the chest wall cavity.
Figure 3.
Single port VATS huge mediastinal tumor resection (3). Available online: http://www.asvide.com/articles/1568
Discussion
Various surgical methods are available for anterior mediastinal tumor resection, including midline exploratory sternotomy (4), anterior lateral thoracotomy (5), and VATS (4). Advocates of minimally invasive surgery have emphasized its benefits, including shorter recovery, less blood loss during operation and shorter hospitalization. We indeed found the result of minimal invasive surgery was not inferior to traditional open surgery (4,6,7). Thus, the flourishing development and redefinition of minimally invasive surgery to mediastinal tumor over the last two decades has gradually changed the surgical requirements of patients. Not only just want to be remove the whole tumor completely, but also look for shorter recovery and better cosmetics are the desires of each patient. That is why robot-assisted and VATS has become increasingly popular, however, these new techniques seem to be unsuitable for giant tumor, especially for tumor greater than 10 cm. We have advocated single port VATS since 2010 for major pulmonary resections (8). Series of reports have proved its feasibility and safety (6,7). Good surgeons always compete with themselves when they could balance the safety of the patients and surgical techniques. The surgical challenges arise from the size of tumor and no major bleeding during operation. Sternotomy might increase the possibility of blood transfusion and late recovery. A giant tumor may hinder the instruments and operation view and it might cause unexpected intraoperation bleeding or other kind of complications. Due to the religious condition of the patient, a careful dissection by using bimanual instrumentation with harmonic scalpel and long and curved suction device is recommended to avoid oozing or bleeding from vessels such as the innominate or thymic vein. Besides, in order to reduce the chance of bleeding accident, we decided to remove the thymoma first and then retrieved the bilateral horn of thymus. It could help us with a more clearly view when we dissect the thymus tissue above innominate vein.
In conclusion, this report describes a case of successful removal of a giant thymoma by uniportal VATS in a patient who refused open surgery. The optimal approach for removal of such kind of tumor depends on different variables for each patient and the experience of surgeons. However, the less post-operative pain, the reduction of hospital stay and the better cosmetic results are all potential advantages of this approach over traditional technique. We believe that in the hands of appropriately experienced surgeons, single port thoracoscopic excision of mediastinal represents a safe, effective surgical options even for such kind of patient.
Acknowledgements
None.
Informed Consent: Informed consent was obtained from the patient for publication of this case report and of the accompanying images.
Footnotes
Conflicts of Interest: Diego Gonzalez-Rivas serves as a consultant for Scanlan International, Inc.
References
- 1.Suda T, Sugimura H, Tochii D, et al. Single-port thymectomy through an infrasternal approach. Ann Thorac Surg 2012;93:334-6. 10.1016/j.athoracsur.2011.08.047 [DOI] [PubMed] [Google Scholar]
- 2.Wu CF, Gonzalez-Rivas D, Wen CT, et al. Single-port video-assisted thoracoscopic mediastinal tumour resection. Interact Cardiovasc Thorac Surg 2015;21:644-9. 10.1093/icvts/ivv224 [DOI] [PubMed] [Google Scholar]
- 3.Gonzalez-Rivas D, Wu CF, de la Torre M. Single port VATS huge mediastinal tumor resection. Asvide 2017;4:259. Available online: http://www.asvide.com/articles/1568
- 4.Orsini B, Santelmo N, Pages PB, et al. Comparative study for surgical management of thymectomy for non-thymomatous myasthenia gravis from the French national database EPITHOR. Eur J Cardiothorac Surg 2016;50:418-22. 10.1093/ejcts/ezw064 [DOI] [PubMed] [Google Scholar]
- 5.Saito T, Makino T, Hata Y, et al. Giant thymoma successfully resected via anterolateral thoracotomy: a case report. J Cardiothorac Surg 2015;10:110. 10.1186/s13019-015-0321-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shen Y, Wang H, Feng M, et al. Single- versus multiple-port thoracoscopic lobectomy for lung cancer: a propensity-matched study. Eur J Cardiothorac Surg 2016;49 Suppl 1:i48-53. [DOI] [PubMed] [Google Scholar]
- 7.Wu CF, Gonzalez-Rivas D, Wen CT, et al. Comparative Short-Term Clinical Outcomes of Mediastinum Tumor Excision Performed by Conventional VATS and Single-Port VATS: Is It Worthwhile? Medicine (Baltimore) 2015;94:e1975. 10.1097/MD.0000000000001975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gonzalez-Rivas D, Paradela M, Fieira E, et al. Single-incision video-assisted thoracoscopic lobectomy: initial results. J Thorac Cardiovasc Surg 2012;143:745-7. 10.1016/j.jtcvs.2011.07.049 [DOI] [PubMed] [Google Scholar]