Abstract
During blood pressure (BP) measurement, the recommended positioning of the cuff bladder center is directly above the brachial artery. We investigated the relevance of incorrect cuff positioning during (1) auscultatory measurement with an appropriate or improperly small cuff and (2) oscillometric measurement with a wide-range cuff designed to guarantee accurate measurements regardless of position. In subjects with wide BP and arm circumference ranges, (1) auscultatory BP was repeatedly measured with a properly positioned cuff (reference) and, simultaneously, with an identical cuff placed on the other arm in either a correct or an incorrect position (test). The measurements were performed with a properly sized (N=57) or an improperly small cuff (N=33). (2) Auscultatory measurements obtained with a properly positioned and sized cuff were compared with oscillometric measurements obtained with a specially designed wide-range cuff (Omron IntelliWrap) placed on the contralateral arm either in a correct or an incorrect position. Auscultatory BP measures were unaffected by incorrect positioning of a properly sized cuff, whereas with undercuffing, BP was overestimated with the cuff displaced by 90° laterally (systolic/diastolic BP differences: 4.9±4.6/4.0±4.6 mm Hg, P<0.01) or by 180° (3.9±5.4/4.2±5.1 mm Hg, P<0.01) in relation to the correct position. Incorrect placement of the oscillometric cuff had no significant effect on the accuracy of the measurements (difference with correct position <1.5 mm Hg). Incorrect cuff positioning introduces a systematic overestimation of auscultatory BP when the cuff is too small in relation to arm circumference but not when it is correctly sized. No systematic error was observed with oscillometric measurements obtained with a specially designed wide-range cuff.
Keywords: blood pressure determination, diagnostic errors, home blood pressure monitoring, obesity, sphygmomanometers
Introduction
Accurate diagnosis of hypertension is of utmost importance considering the clinical consequences of this highly prevalent condition, which remains a severe burden for societies in terms of morbidity, disability and mortality, as well as a high cost for health-care systems.1, 2 Although much progress has been made in out-of-office blood pressure (BP) assessment over the past decades, conventional BP measurement in a physician’s office remains the cornerstone of hypertension diagnosis.2 The standards for accurate BP assessment have been described in detail in several documents published by national and international societies,2, 3, 4, 5, 6 but their application in clinical practice remains unsatisfactory.7, 8 The importance of correctly positioning the cuff in relation to the brachial artery is commonly emphasized among these recommendations and is also included in the instruction manuals by the manufacturers of BP-measuring devices. Specifically, it is recommended that the center of the bladder used for BP measurement should be placed over the course of the brachial artery.3, 6, 9, 10 Interestingly, although the theoretical principle of this recommendation seems reasonable, to our knowledge, there are no published studies available to support such a recommendation. Thus, it is not clear whether a clinically relevant error is indeed made when the cuff of a BP measuring device is placed incorrectly. Moreover, incorrect cuff positioning might interact with the error caused by an insufficient arm coverage by the usage of inappropriately small cuffs (undercuffing). The latter error commonly occurs in real-life settings, where BP is often measured with standard cuffs in obese subjects, therefore causing a clinically relevant BP overestimation.11, 12
The error of cuff positioning may be of particular relevance in case of BP self-measurement at home, where user training is frequently inadequate. The impact of such error in populations may be large, as home BP monitoring is a widely used technique, owing to the availability of accurate, cheap and easy-to-use automated oscillometric devices, good acceptance by patients, confirmed prognostic value and possible positive impact on patients’ adherence to treatment.3, 13 Several current guidelines recommend the implementation of home BP monitoring to support the diagnosis of hypertension and to monitor the efficacy of BP-lowering treatment.2, 3
The potential inaccuracy in BP measurement related to incorrect cuff size and placement might be overcome by using specifically designed cuffs. One such cuff, developed to guarantee adequate accuracy in a wide range of arm circumferences regardless of the positioning of its center in relation to the brachial artery, has recently been introduced to the market (IntelliWrap cuff, Omron, Kyoto, Japan). However, it has not been demonstrated whether its performance is indeed unaffected by incorrect cuff positioning.
The aims of our study were: (1) to verify the actual presence and size of the error introduced in auscultatory BP measurement by incorrect cuff positioning when using either a properly sized or an improperly small cuff, and (2) to verify whether such error is present and relevant when an oscillometric device equipped with a wide-range cuff is used.
Methods
Study design
This was an observational study in which repeated BP measurements were performed simultaneously with two devices whose cuffs were positioned on both arms; one arm was used to obtain the reference BP (the auscultatory device always used with correctly positioned cuff), whereas BP on the other arm was measured using a test device whose cuff was placed in varying positions in relation to the brachial artery. The first phase of the study was aimed at verifying the effect of incorrect cuff positioning on auscultatory measurement and involved a mercury sphygmomanometer as the test device. The measurements in this phase were performed in two groups of subjects; in one group, properly sized cuffs were used with both devices (Main Study), whereas in the other group, both cuffs were inappropriately small in relation to the arm circumference (Undercuffing Study). The second phase of the study tested the performance of a wide-range (IntelliWrap) cuff in different positions. This phase was performed in the participants of the Main Study and used an oscillometric sphygmomanometer coupled with an IntelliWrap cuff as the test device and a mercury sphygmomanometer with a properly positioned cuff as the reference device.
Participants
Our study included healthy volunteers and patients of Istituto Auxologico Italiano in Italy (San Luca Hospital, Milan, and San Giuseppe Hospital, Verbania). Subjects were included if aged 18–80 years, in sinus rhythm, arm circumference was between 23 and 42 cm and clinical conditions were stable. An entry BP limit was not set because the recruitment aimed to include subjects with a wide range of entry BP values. Moreover, subjects were recruited to ensure the representation of the entire range of acceptable cuff circumferences, while favoring the participation of subjects with large arm circumferences (>32 cm), in whom the effect of cuff positioning was expected to be more evident. All participants of the Undercuffing Study had arm circumferences ⩾28 cm. The main exclusion criteria were: vascular disease, BP difference between arms >5 mm Hg (mean of two measurements), relevant medical conditions affecting either arm, relevant arrhythmias or implanted cardiac pacemaker, oral anticoagulants use or other coagulation alterations and pregnancy. All participants gave written informed consent before initiating study procedures. The study was performed according to the principles of the Declaration of Helsinki and the study protocol was approved by the Ethics Committee of the Istituto Auxologico Italiano.
BP measurement
Two types of devices were used: (1) a standard mercury sphygmomanometer (reference device; Ecometer New, ERKA, Bad Tölz, Germany), also referred to as an ‘auscultatory device’ (2) commercially available, validated Omron M6 Comfort oscillometric device (HEM-7321-E), used in combination with the semi-rigid IntelliWrap Cuff (HEM-FL31-E, arm circumference range 22–42 cm), both manufactured by Omron Healthcare (Kyoto, Japan) and also referred to as an ‘oscillometric device’.14 In the Main Study, the auscultatory device was equipped with cuffs adequately sized for each participant (arm circumference ranges: small, 20.5–28 cm; adult, 27–35 cm; large, 34–43 cm; and the corresponding bladder sizes were: 24 × 11 cm, 28 × 14 cm and 35 × 17 cm, respectively). The Undercuffing Study measurements were performed with a mercury sphygmomanometer equipped with a standard cuff with a bladder size of 22.5 × 11.5 cm that did not sufficiently cover the entire arm circumference of the included subjects. The IntelliWrap is a bladderless cuff with a troncoconical shape, with the following dimensions: length 39 (lower edge) to 42 (upper edge) cm × 12 cm.
For each device, the measurement technique followed the standard recommendations for BP measurement3, 4 and the manufacturer’s instructions, with exception to the positioning of the cuff on the arm in relation to the brachial artery. The cuffs were placed in a correct position (the center of the bladder directly above the brachial artery), rotated by 90° either medially (90°M) or laterally (90°L), or rotated by 180° during study measurements. Three trained investigators were involved in each measurement: one supervisor (responsible for ensuring the correct measurements sequence, registering the measured BP values and performing oscillometric measurements) and two observers (responsible for auscultatory measurements). The observers were blinded both to each other’s measurements and to the oscillometric measurement results.
For the duration of the study procedures, each participant remained in a comfortable, seated position, with their back leaning against the chair’s back and both arms supported to maintain the upper arm at the level of the heart. After a brief rest, a preliminary measurement was performed by the observers with two mercury devices (both in a correct position) in order to familiarize the subject with the measurements and identify possible problems. After an additional 10 min of rest, two entry measurements were performed to determine basal BP level and to exclude between-arm differences (the observers switched sides between measurements). After that, a sequence of actual study measurements followed. First (sequence A, performed in both Main and Undercuffing studies), two mercury devices were used on two arms, each operated by a single observer. The device on one of the arms (randomly selected) remained in a correct position during all measurements, whereas on the other arm measurements were performed with the cuff sequentially placed in the four previously described positions. To reduce possible biases, in each position, the measurement was repeated twice, with the observers switching sides after the first measurement. In the Main Study, a second sequence was also performed (sequence B). In this sequence, one mercury device was used on one of the arms, remaining in a correct position. Measurements with this device were performed simultaneously by two operators with a binaural stethoscope. In case of a BP difference between the observers exceeding 4 mm Hg, the measurement was repeated. The oscillometric device was placed on the opposite arm and two measurements were performed in the correct, 90°L and 180° positions (90°M position was omitted to reduce the total number of measurements, being, among the incorrect positions, the least likely to induce errors). Then, the auscultatory and oscillometric device placement were changed to the opposite arms, and the measurements were repeated. The detailed sequence of measurements is reported in Supplementary Table S1 (see Supplementary digital content).
Sample size
The sample size of the Main Study was calculated assuming s.d. of mean BP difference between correct and incorrect cuff positioning to be 5 mm Hg, 90% power and α error level of 0.05 in the two-tailed t-test. With these assumptions, a sample size of 22 participants was required to detect a BP difference of 5.0 mm Hg and 50 participants were needed to demonstrate with 90% power and at an α error level of 0.05 the equivalence between BP measured with correct and incorrect cuff position, tested with an equivalence margin of 3 mm Hg and a coefficient of correlation between BP measured with correct and incorrect cuff position equal to 0.8.
Statistical analysis
The analyses were performed with R software version 2.15.3 (R Foundation for Statistical Computing, Vienna, Austria). Continuous data are expressed as mean±s.d. and ranges, or otherwise, as absolute numbers and percentages. The normality distribution and the homogeneity of variances were tested with the Shapiro test and Bartlett test, respectively. Linear mixed-effect models, fitting the models by maximizing the restricted log-likelihood, were used to compare BP values in different cuff positions, taking into account the reference BP measured in the correct position. The post hoc analysis was performed with a posteriori contrasts adjusted for multiple comparisons using the algorithm that controls the expected rate of false-positive results for all positive results. Bland–Altman analysis with a correction of agreement limits for repeated measures was performed to assess the distribution of differences between the two measurements over the range of average BPs.15 Repeatability was assessed by calculating repeatability coefficients as 1.96·√2 within-subject s.d. (sw) and by two-way, random-average measure intraclass correlation coefficients.16 An α level of 0.05 was used for all hypothesis tests.
Results
A total of 10 participants were excluded after initial measurements: 4 in the Main Study (because of between-arm BP differences >5 mm Hg) and 6 in the Undercuffing Study (between-arm BP differences >5 mm Hg in 5 participants and consent withdrawal in 1 participant). The characteristics of the participants who completed the study are reported in Table 1. For the IntelliWrap cuff (taking 39 cm as air chamber length), 51 (89%) patients in the Main Study and 29 (88%) in the Undercuffing Study had arm coverage >100% and all the participants had at least 90% arm coverage.
Table 1. Characteristics of study participants.
| Variable | Main study (n=57) | Undercuffing study (n=33) |
|---|---|---|
| Age (years) | 44.4±14.0 (24–78) | 50.8±16.9 (21–79) |
| Males/females | 25 (44%)/32 (56%) | 22 (67%)/11 (33%) |
| BMI (kg m−2) | 29.8±8.8 | 30.2±6.2 |
| Arm circumference (cm) | 31.9±5.8 (23–42) | 31.9±3.7 (28–41) |
| Arm circumference category | ||
| <28 cm | 19 (33.3%) | 0 (0.0%) |
| 28–31 cm | 6 (10.5%) | 20 (60.6%) |
| 32–36 cm | 14 (24.6%) | 8 (24.2%) |
| >36 cm | 18 (31.6%) | 5 (15.2%) |
| Entry systolic BP (mm Hg) | 117.6±17.7 (95–197) | 126.8±16.1 (99–157) |
| Entry diastolic BP (mm Hg) | 76.2±10.8 (56–109) | 85.2±10.1 (57–101) |
| Entry systolic BP category | ||
| ⩽100 mm Hg | 7 (12.3%) | 1 (3.0%) |
| 101–139 mm Hg | 45 (78.9%) | 24 (72.7%) |
| 140–159 mm Hg | 3 (5.3%) | 8 (24.2%) |
| ⩾160 mm Hg | 2 (3.5%) | 0 (0.0%) |
| Entry diastolic BP category | ||
| ⩽60 mm Hg | 2 (3.5%) | 1 (3.0%) |
| 61–84 mm Hg | 44 (77.2%) | 14 (42.4%) |
| 85–99 mm Hg | 9 (15.8%) | 16 (48.5%) |
| ⩾100 mm Hg | 2 (3.5%) | 2 (6.1%) |
Abbreviations: BMI, body mass index; BP, blood pressure.
Data are shown as means±s.d. (range) or counts (proportions) as appropriate.
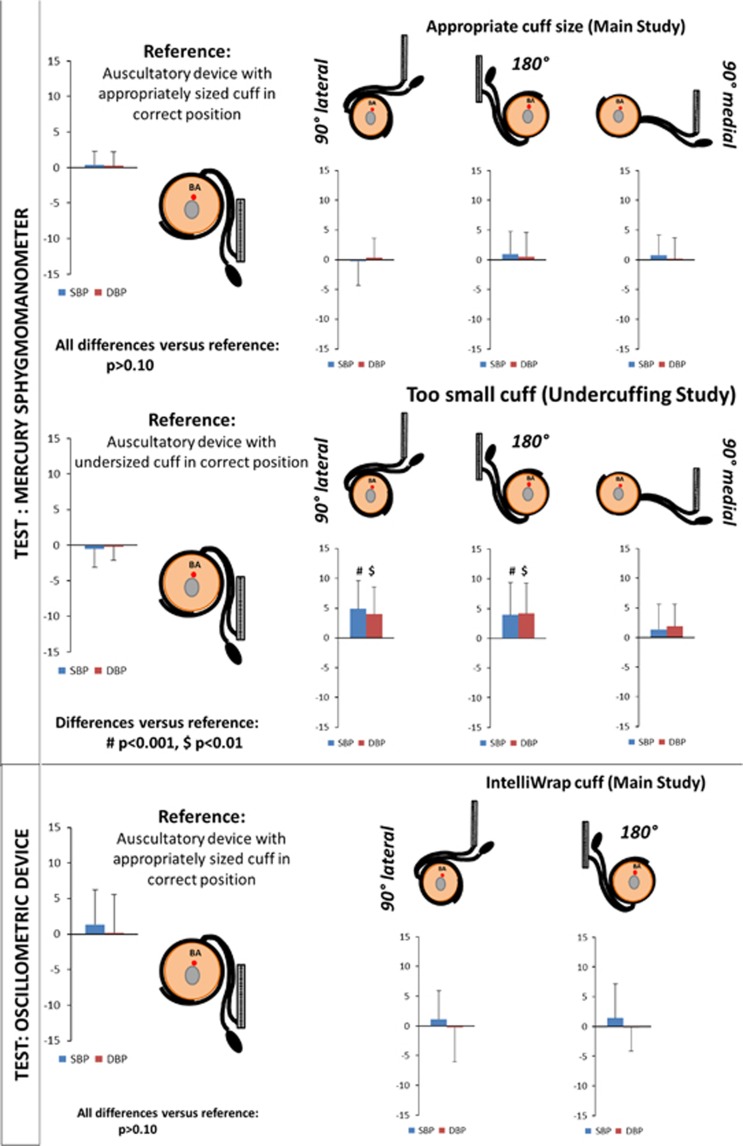
The results of sequence A in the Main Study (N=57) did not reveal significant between-arm differences in BP (mean difference was always <1 mm Hg) measured with the two auscultatory devices in any position, either correct or incorrect. This was also true in the subset of subjects in whom the arm coverage was between 80 and 90%. Conversely, in the Undercuffing Study (N=33), an incorrect placement of one of the cuffs led to systematically higher systolic and diastolic BP values, with the differences reaching ∼4–5 mm Hg and achieving statistical significance, when the cuff was rotated by 90°L or by 180°. In addition, in this study, there were no significant between-arm differences in BP when the cuffs of both devices were correctly placed (Table 2 and Figure 1).
Table 2. Mean blood pressure (BP) values obtained with two devices: reference auscultatory device always in correct position and test device (either auscultatory or oscillometric) in varying positions.
|
Systolic BP |
Diastolic BP |
|||
|---|---|---|---|---|
| Position of test device cuff | Reference | Test | Reference | Test |
| Test device: auscultatory, appropriately sized cuff (Main Study; n=57) | ||||
| Correct | 115.9±18.3 | 116.3±18.5 | 75.8±11.3 | 76.1±11.6 |
| 90° Medially | 114.1±18.4 | 114.9±18.8 | 75.6±11.1 | 75.8±11.6 |
| 90° Laterally | 114.9±17.9 | 114.6±17.1 | 75.5±11.3 | 75.8±10.9 |
| 180° | 115.1±18.9 | 116.0±19.9 | 75.9±11.2 | 76.4±11.3 |
| Test device: auscultatory, undersized cuff (Undercuffing Study; n=33) | ||||
| Correct | 124.6±15.0 | 124.1±15.1 | 85.2±10.4 | 85.0±9.7 |
| 90° Medially | 123.9±15.0 | 125.2±15.7 | 84.4±10.5 | 86.3±11.5 |
| 90° Laterally | 124.5±15.6 | 129.5±15.4a | 85.1±10.4 | 89.1±11.6a |
| 180° | 124.4±15.2 | 128.3±15.9a | 84.9±10.6 | 89.1±11.6a |
| Test device: oscillometric, IntelliWrap cuff (Main Study; n=57) | ||||
| Correct | 113.8±17.9 | 115.2±18.0 | 76.3±11.2 | 76.5±10.8 |
| 90° Laterally | 113.8±18.2 | 114.9±17.1 | 76.3±11.7 | 76.1±11.8 |
| 180° | 113.7±17.7 | 115.1±17.6 | 76.3±11.4 | 76.2±11.9 |
P<0.001 for difference between the reference and test device.
Figure 1.
Blood pressure (BP) effects of incorrect positioning of appropriately sized or undersized auscultatory device cuff and of ‘IntelliWrap’ cuff. The systolic BP (SBP, blue bars) and diastolic BP (DBP, red bars) values are shown as the mean difference±s.d. BA, brachial artery.
In the Main Study, both systolic and diastolic BP values measured with the oscillometric device were similar to those obtained with the auscultatory device on the contralateral arm, regardless of oscillometric device cuff position (the mean difference in systolic BP was always <1.5 mm Hg and diastolic BP was always <0.5 mm Hg; Table 2 and Figure 1). In this part of the study, the average difference in systolic/diastolic BP reported by the two observers amounted to 0.16±2.15/0.05±2.2 mm Hg.
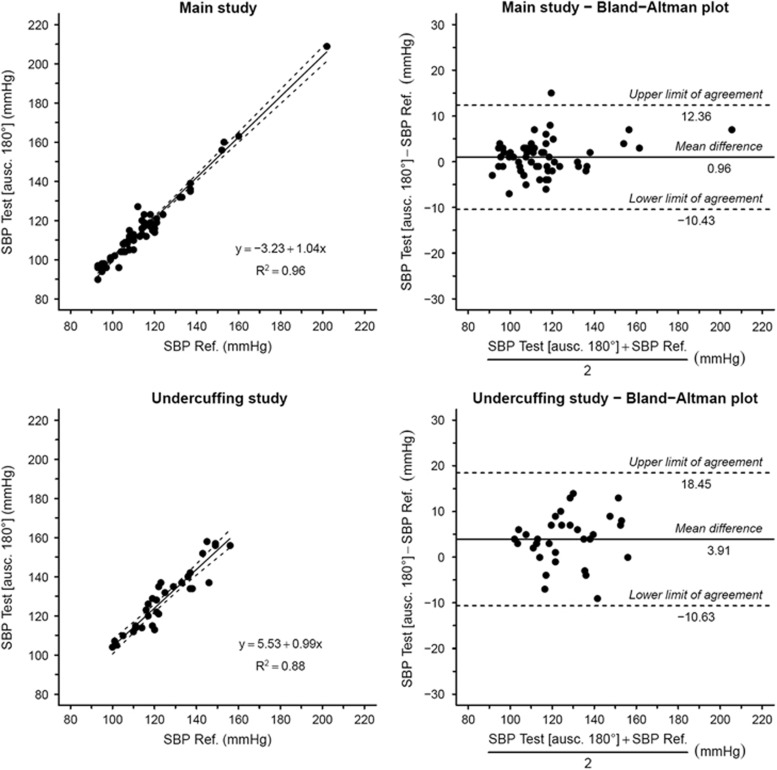
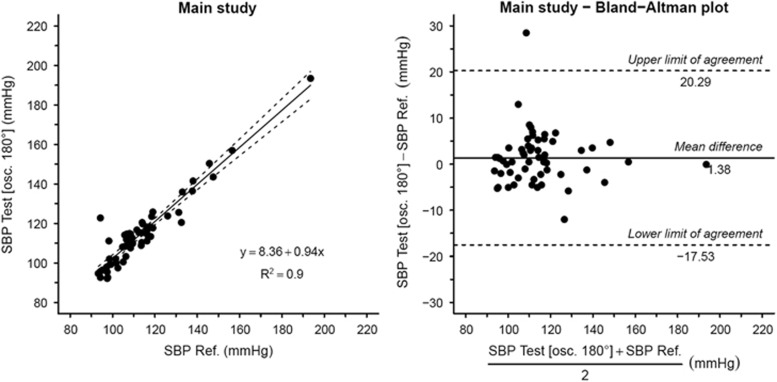
Bland–Altman analysis indicates that the differences between the reference and test devices in any position were similarly distributed across the investigated BP range in the Main Study (Figure 2). In the Undercuffing Study the extent of BP overestimation in incorrect positions remained constant across the mean BP range (Figure 3). We found no significant correlation between the reference-test difference in different positions and arm circumference for either the auscultatory (sequence A) or oscillometric measurements (sequence B) in the Main Study. In the Undercuffing Study, there was a weak positive correlation (r=0.42) between arm circumference and the overestimation of systolic BP in the rotated 180° position. In fact, all three subjects who exhibited systolic BP overestimation in this position exceeding 10mm Hg had arm circumferences ⩾34 cm.
Figure 2.
Bland–Altman plots (right panels) of differences in systolic blood pressure (SBP) between the auscultatory reference device with the cuff in correct position (Ref.) and the auscultatory test device when the cuff of the latter was rotated by 180°. The data are shown separately for appropriately sized (top) or undersized cuffs (bottom). The corresponding correlations are also shown (left panels).
Figure 3.
Bland–Altman plot (right panel) of differences in systolic blood pressure (SBP) between the auscultatory reference device with the cuff in the correct position (Ref.) and the oscillometric test device with the IntelliWrap cuff rotated by 180°. The corresponding correlation is also shown (left panel).
To assess whether the incorrect cuff position may affect the reproducibility of measurements, we calculated the repeatability coefficients and intraclass correlation coefficients for the repeated measurements in sequence A (two measurements per condition) and in sequence B (four measurements per condition). Repeatability coefficients for the reference measurements (auscultatory device in correct position) of systolic/diastolic BP were: in sequence A, 10.4/6.9 mm Hg in the Main Study and 10.7/9.4 mm Hg in the Undercuffing Study; in sequence B, 11.2/8.2 mm Hg. The coefficients for test measurements with the auscultatory device were similar, except for the Undercuffing Study where they were higher in 90°L position (13.3/10.4 mm Hg) and in 180° position (15.8/14.0 mm Hg). Higher repeatability coefficients were also observed for oscillometric measurements with no systematic differences between different cuff positions (correct: 23.1/11.4 mm Hg, 90°L: 14.4/11.7 mm Hg, 180°: 22.0/12.7 mm Hg). Intraclass correlation coefficients were high in the Undercuffing Study for all cuff positions, with both the auscultatory and oscillometric measurements (always ⩾0.90).
Discussion
Our study provides, for the first time, a formal demonstration of the effects of incorrectly positioned measuring cuff on BP measurement when the center of the bladder is not positioned directly over the brachial artery course as recommended in many guidelines and in device manufacturers’ instructions.3, 6, 9, 10 We found that (1) when the size of a standard auscultatory BP measuring device cuff was appropriate, its incorrect placement in relation to the brachial artery did not significantly affect measurement accuracy; (2) conversely, when the cuff was too small in relation to the arm circumference (undercuffing), cuff displacement resulted in a significant overestimation of BP, mainly when the cuff was displaced by 90°L or by 180° in relation to the correct position; and (3) when a wide-range cuff of an oscillometric device specifically designed to ensure adequate arm coverage and homogeneous pressure transmission independently of cuff positioning (the ‘IntelliWrap’ cuff, Omron) was used, its incorrect placement in relation to the brachial artery did not affect measurement accuracy even in subjects with very large arm circumferences.
A number of studies have assessed the impact of different BP measurement errors on the obtained BP values. The impact of hydrostatic height difference between heart and cuff, lack of arm support, leg crossing and reporting errors on BP measurement accuracy is well known,17, 18, 19, 20, 21 although the relevance of other factors, for example, mercury column oscillations, is less well defined.22 Among the different sources of error, the issue of cuff size has been extensively investigated, demonstrating that when an under-sized cuff is used (undercuffing, that is, when the bladder covers <80% of the arm circumference), BP values are overestimated because of the higher pressures needed to occlude the brachial artery when the cuff pressure is not transmitted to the full arm circumference.11, 12 Our data indicate that whenever the center of the (inadequately sized) bladder of the auscultatory device is not positioned above the brachial artery, BP is systematically overestimated. In the sample of subjects with undercuffing, this additional error amounted to, on average, 4–5 mm Hg when the cuff was placed in the 90°L or 180° position. It should be clear that our study was not designed to assess the impact of undercuffing with a correctly positioned cuff (because the cuffs we used on both arms of the Undercuffing Study participants were too small), but previous studies have shown that, in such a situation, BP is significantly overestimated.11, 12 When both errors, that is, undercuffing and incorrect cuff positioning are committed simultaneously, the overestimation of BP values may, on average, exceed 10 mm Hg, and even more in individual cases; an error that is clearly clinically relevant. The theoretical basis of these findings appears plausible, considering that the center of the bladder represents the point of maximum pressure transmission between the cuff and the arm tissues. When an interposition of a thick layer of tissues (including the humerus) between this point and the artery occurs, the pressure transmission is worse, and thus the pressure applied to the arm surface in order to occlude the artery must be higher. These theoretical considerations also explain an asymmetry found between 90°M and 90°L cuff displacement. In the former position, the intervening tissue layer is thinner and includes mainly soft tissues without large muscles. Consequently, the error size in this position was smaller.
When the auscultatory cuff size was correct, there was no significant difference observed in the BP measurements, even in the extreme position (180° rotation). This finding, likely deriving from a more homogeneous distribution of force applied to the arm surface when the cuff coverage is complete, clearly reinforces the need to use appropriately sized cuffs. Interestingly, the results of our study support the recommendation of an early paper by O’Brien and O’Malley23 on BP measurement that stated that ‘the center of bladders less than 35 cm long must be positioned over the line of the artery’. This recommendation was maintained in the European Society of Hypertension 2003 BP measurement guidelines4 and was extended in later guideline documents to all measurements, regardless of cuff size.3, 6
Measurement errors deriving from incorrect BP measurement technique may be of particular relevance in the setting of home BP measurement, where the inadequate degree of user training and expert supervision may have a negative impact on the reported BP values.24 In particular, the problem of miscuffing is not uncommon, and previous reports indicated that in over 80% of cases, it is because of under-sized cuffs (undercuffing).25 This is not surprising considering the epidemic of obesity in populations worldwide26 as well as the fact that many devices for home measurements are sold with standard-sized cuffs and that many individuals with large arms are not aware of the need to use a larger cuff.27, 28, 29 Although published data on the patterns of cuff positioning among users of home BP monitors are missing, marketing research performed among 150 users of home BP monitors revealed that only one out of three accurately placed the BP cuff over the artery (±15°), whereas 1 out of 10 committed placement errors exceeding 90° (unpublished data). Considering that subjects with large arms may have major difficulty in properly fitting a BP cuff, it is reasonable to suspect that the number of subjects in whom the combination of undercuffing and inappropriate cuff positioning occurs is not negligible.
A practical solution to this problem may be the use of wide-range cuffs that are able to provide adequate coverage in both normal and large arms. The IntelliWrap cuff tested in our study provides an adequate coverage of arms in the circumference range of 22 to 42 cm and was specifically designed to provide homogeneous pressure distribution around the arm in order to minimize the effects of incorrect positioning. Our data confirm the manufacturer’s statement that BP measurement with an oscillometric device coupled with this cuff provides accurate results independent of the cuff placement in relation to the brachial artery. Although ours was not a formal validation study, the test device and the auscultatory measurement on the contralateral arm were in very good agreement, with the mean difference never exceeding 1.5 mm Hg in any position and the s.d. of the difference remaining within the 8 mm Hg limit recommended in the ANSI/AAMI/ISO 81060-2:2013 standard.30 This was true across the investigated range of BP values and arm circumferences.
The data from the Undercuffing Study, where systematic error occurred in 90°L and 180° positions, indicate that incorrect positioning of a cuff too small in relation to the arm size may indeed affect the accuracy of BP measurement. To verify whether cuff placement errors may also affect the precision of BP measurement, we performed a repeatability analysis that suggests that, indeed, when the cuff size is too small, auscultatory cuff positioning in a 90°L or 180° position may decrease measurement repeatability. The repeatability was also lower for oscillometric measurement, but consistent effects of cuff position were not observed in this case. In either case, elevated intraclass correlation coefficient values suggest that the effect of introduced random error is minor.
Our study has a few limitations that, in our view, do not affect its main conclusions. First, our sample included few subjects with elevated BP values, in whom the observed errors could be larger. However, our data do not suggest systematic changes in the pattern of observed errors in the range between 140 and 160 mm Hg for systolic and 90 and 100 mm Hg for diastolic BP and, therefore, our results seem to apply to the majority of home BP users. Second, the study design did not include the evaluation of 90°M positioning of the IntelliWrap cuff. This was done in order to limit the already high number of consecutive measurements (24 plus repetitions, if needed) aimed at avoiding the possibility that the patients’ uneasiness might affect BP values, as well as increasing patients’ compliance with study measurements. However, the results of the test performed with the auscultatory device support our initial hypothesis that the 90°M position has no relevant effect on BP measurement accuracy, even in case of undercuffing, a finding that could safely be extrapolated to the oscillometric measurements. Third, we did not compare the performance of the oscillometric device with the ‘IntelliWrap’ cuff against the performance of the same device with a standard cuff. This was because another cuff type was not available for use with the device model used in our study. Finally, our study did not specifically assess the possible impact of conical shape arms on the accuracy of BP measurement, where the use of rectangular cuffs may cause BP overestimation, even if the cuff range appears adequate for the arm circumference.31
Conclusions
Our study shows that inappropriate positioning of an auscultatory device cuff appears relevant only when the cuff size is inadequate and that an appropriately designed wide-range cuff for home BP monitoring may minimize the impact of user error in cuff placement on the arm. When combined with the common undercuffing error, incorrect cuff placement may therefore lead to a systematic overestimation of BP (and, possibly, to excessive dosing of antihypertensive treatment) in obese subjects. These findings may provide a basis for revising current recommendations on BP measurement technique and instructions for BP measuring devices. They may also support a widespread use of appropriately designed wide-range cuffs that appear accurate regardless of cuff positioning, even in subjects with large arms. Considering the elevated predictive value of home BP monitoring, such technological development, which simplifies the BP measurement procedure without affecting its accuracy, may be an important step forward in optimizing the approach to accurate BP phenotype definition.
Acknowledgments
We thank Dr Luca Gondoni, Professor Massimo Scacchi, Dr Matteo Raimondi and the staff of San Giuseppe Hospital in Piancavallo for their support in organizing data collection. We thank Doctors Cristina Zorzi, Andrea Grillo and Cinzia Vergani for their support in data collection. We also thank all the volunteers for the dedicated time.
Footnotes
Supplementary Information accompanies the paper on Hypertension Research website (http://www.nature.com/hr)
The corresponding author’s institution has received financial support for the present study from Omron Healthcare Europe. GP has received honoraria for lectures from Omron. The remaining authors declare no conflict of interest.
Supplementary Material
References
- GBD 2013 Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015; 386: 2287–2323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mancia G, Fagard R, Narkiewicz K, Redón J, Zanchetti A, Böhm M, Christiaens T, Cifkova R, De Backer G, Dominiczak A, Galderisi M, Grobbee DE, Jaarsma T, Kirchhof P, Kjeldsen SE, Laurent S, Manolis AJ, Nilsson PM, Ruilope LM, Schmieder RE, Sirnes PA, Sleight P, Viigimaa M, Waeber B, Zannad F. Task Force Members. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 2013; 31: 1281–1357.23817082 [Google Scholar]
- Parati G, Stergiou GS, Asmar R, Bilo G, de Leeuw P, Imai Y, Kario K, Lurbe E, Manolis A, Mengden T, O'Brien E, Ohkubo T, Padfield P, Palatini P, Pickering T, Redon J, Revera M, Ruilope LM, Shennan A, Staessen JA, Tisler A, Waeber B, Zanchetti A, Mancia G, . ESH Working Group on Blood Pressure Monitoring. European Society of Hypertension guidelines for blood pressure monitoring at home: a summary report of the Second International Consensus Conference on Home Blood Pressure Monitoring. J Hypertens 2008; 26: 1505–1530. [DOI] [PubMed] [Google Scholar]
- O'Brien E, Asmar R, Beilin L, Imai Y, Mallion JM, Mancia G, Mengden T, Myers M, Padfield P, Palatini P, Parati G, Pickering T, Redon J, Staessen J, Stergiou G, Verdecchia P, . European Society of Hypertension Working Group on Blood Pressure Monitoring. European Society of Hypertension recommendations for conventional, ambulatory and home blood pressure measurement. J Hypertens 2003; 21: 821–848. [DOI] [PubMed] [Google Scholar]
- O'Brien E, Parati G, Stergiou G, Asmar R, Beilin L, Bilo G, Clement D, de la Sierra A, de Leeuw P, Dolan E, Fagard R, Graves J, Head GA, Imai Y, Kario K, Lurbe E, Mallion JM, Mancia G, Mengden T, Myers M, Ogedegbe G, Ohkubo T, Omboni S, Palatini P, Redon J, Ruilope LM, Shennan A, Staessen JA, Vanmontfrans G, Verdecchia P, Waeber B, Wang J, Zanchetti A, Zhang Y, , European Society of Hypertension Working Group on Blood Pressure Monitoring. European Society of Hypertension position paper on ambulatory blood pressure monitoring. J Hypertens 2013; 31: 1731–1768. [DOI] [PubMed] [Google Scholar]
- Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN, Jones DW, Kurtz T, Sheps SG, Roccella EJ. Recommendations for blood pressure measurement in humans and experimental animals: part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Circulation 2005; 111: 697–716. [DOI] [PubMed] [Google Scholar]
- Boivin JM, Tsou-Gaillet TJ, Fay R, Dobre D, Rossignol P, Zannad F. Influence of the recommendations on the implementation of home blood pressure measurement by French general practitioners: a 2004-2009 longitudinal survey. J Hypertens 2011; 29: 2105–2115. [DOI] [PubMed] [Google Scholar]
- Manzoli L, Simonetti V, D'Errico MM, De Vito C, Flacco ME, Forni C, La Torre G, Liguori G, Messina G, Mezzetti A, Panella M, Pizzi C, Siliquini R, Villari P, Cicolini G. (In)accuracy of blood pressure measurement in 14 Italian hospitals. J Hypertens 2012; 30: 1955–1960. [DOI] [PubMed] [Google Scholar]
- Omron Model M3 Instruction Manualwww.omron-healthcare.com/en/support/manuals/download/m3-hem-7131-e-en. Accessed on 24 December 2016.
- Microlife BP A6 BT Manualhttp://www.microlife.com/media/1006/download/IB%20BP%20A6%20BT%20S-V10-1%201516.pdf. Accessed on 24 December 2016.
- Mourad JJ, Lopez-Sublet M, Aoun-Bahous S, Villeneuve F, Jaboureck O, Dourmap-Collas C, Denolle T, Fourcade J, Baguet JP. Impact of miscuffing during home blood pressure measurement on the prevalence of masked hypertension. Am J Hypertens 2013; 26: 1205–1209. [DOI] [PubMed] [Google Scholar]
- Sprafka JM, Strickland D, Gómez-Marín O, Prineas RJ. The effect of cuff size on blood pressure measurement in adults. Epidemiology 1991; 2: 214–217. [DOI] [PubMed] [Google Scholar]
- Parati G, Omboni S, Bilo G. Why is out-of-office blood pressure measurement needed? Home blood pressure measurements will increasingly replace ambulatory blood pressure monitoring in the diagnosis and management of hypertension. Hypertension 2009; 54: 181–187. [DOI] [PubMed] [Google Scholar]
- Takahashi H, Yokoi T, Yoshika M. Validation of the OMRON M6 Comfort (HEM-7321-E) upper arm blood pressure monitor, in oscillometry mode, for clinic use and self measurement in a general population, according to the European Society of Hypertension International Protocol revision. 2010. www.dableducational.org/Publications/2014/ESH-IP%202010%20Validation%20of%20Omron%20M6%20Comfort%20%28HEM-7321-E%29.pdf. Accessed on 24 December 2016.
- Bland JM, Altman DG. Measuring agreement in method comparison studies. Stat Methods Med Res 1999; 8: 135–160. [DOI] [PubMed] [Google Scholar]
- Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull 1979; 86: 420–428. [DOI] [PubMed] [Google Scholar]
- Mitchell PL, Parlin RW, Blackburn H. Effect of vertical displacement of the arm on indirect blood-pressure measurement. N Engl J Med 1964; 271: 72–74. [DOI] [PubMed] [Google Scholar]
- Silverberg DS, Shemesh E, Jaina A. The unsupported arm: a cause of falsely raised blood pressure readings. BMJ 1977; 2: 1331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cushman WC, Cooper KM, Horne RA, Meydrech EF. Effect of back support and stethoscope head on seated blood pressure determinations. Am J Hypertens 1990; 3: 240–241. [DOI] [PubMed] [Google Scholar]
- Peters GL, Binder SK, Campbell NR. The effect of crossing legs on blood pressure: a randomized single-blind cross-over study. Blood Press Monit 1999; 4: 97–101. [PubMed] [Google Scholar]
- Mengden T, Hernandez Medina RM, Beltran B, Alvarez E, Kraft K, Vetter H. Reliability of reporting self-measured blood pressure values by hypertensive patients. Am J Hypertens 1998; 11: 1413–1417. [DOI] [PubMed] [Google Scholar]
- El Tahlawi M, Abdelbaset M, Gouda M, Hussein I. Can we predict the presence of coronary lesions from blood pressure measurement? A new clinical method. Hypertens Res 2015; 38: 260–263. [DOI] [PubMed] [Google Scholar]
- O’Brien E, O’Malley K. The ABC of blood pressure measurement: the sphygmomanometer. BMJ 1979; 2: 851–853.509127 [Google Scholar]
- Stryker T, Wilson M, Wilson TW. Accuracy of home blood pressure readings: monitors and operators. Blood Pressure Monit 2004; 9: 143–147. [DOI] [PubMed] [Google Scholar]
- Manning DM, Kuchirka C, Kaminski J. Miscuffing: inappropriate blood pressure cuff application. Circulation 1983; 68: 763–766. [DOI] [PubMed] [Google Scholar]
- Graves JW, Darby CH, Bailey K, Sheps SG. The changing prevalence of arm circumferences in NHANES III and NHANES 2000 and its impact on the utility of the ‘standard adult’ blood pressure cuff. Blood Press Monit 2003; 8: 223–227. [DOI] [PubMed] [Google Scholar]
- Patyna WD, Borsch B, Patyna M, Mitrovic V. Information deficits concerning blood pressure self-measurement. Dtsch Med Wochenschr 2004; 129: 2466–2469. [DOI] [PubMed] [Google Scholar]
- Wiliński J, Kusiak A, Wiliński B, Smolik P, Klima Ł, Chmielewska J, Czarnecka D. Selection and maintenance of the blood pressure monitor for self-blood pressure monitoring (SBPM). Przegl Lek 2013; 70: 900–903. [PubMed] [Google Scholar]
- Graves JW. A survey of validated automated home blood pressure monitors available for the Internet shopper. Blood Press Monit 2005; 10: 103–107. [DOI] [PubMed] [Google Scholar]
- Association for the Advancement of Medical Instrumentation. American National Standard. ANSI/AAMI/ISO 81060-2:2013 Non-invasive sphygmomanometers - Part 2: Clinical investigation of automated measurement type. 4301 N. Fairfax Drive, Suite 301, Arlington, VA 22203-1633, USA: AAMI; 2013.
- Palatini P, Benetti E, Fania C, Malipiero G, Saladini F. Rectangular cuffs may overestimate blood pressure in individuals with large conical arms. J Hypertens 2012; 30: 530–536. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.