Fetal alcohol spectrum disorder (FASD) is a term that encompasses the wide range of physical, mental and behavioural effects that can occur when a person is exposed to ethanol during gestation. The diagnoses under the FASD umbrella are fetal alcohol syndrome (FAS), partial FAS (p-FAS) and alcohol-related neurodevelopmental disorder (ARND). The term FASD is not intended for use as a clinical diagnosis.
Like other developmental disabilities, FAS-related conditions require comprehensive assessment by a team of trained specialists. This has left many primary care physicians unclear of their role in making FASD-related diagnoses in clinical practice. This article highlights the salient messages for primary care physicians from a comprehensive guideline on FASD diagnosis that is included with this issue of CMAJ as a supplement and available online at www.cmaj.ca/content/vol172/5_suppl/index.shtml.1
Rationale for early diagnosis
Early diagnosis is associated with better long-term outcomes. Targeted interventions in childhood have been shown to reduce the risk for later secondary disabilities, such as dependent living, confinement, and addiction and mental health concerns.2
A diagnosis in early childhood may also serve as a clinical biomarker for unrecognized maternal mental health and addiction concerns and provide an opportunity to offer interventions, support and counselling for the birth mother. This, in turn, may decrease rates of maternal–child separation, facilitate recognition and intervention for other affected siblings, and prevent subsequent children from being similarly affected.3
Therefore, an FASD diagnosis should result in far more than simply providing patients and their families with a label; it should provide the impetus for early developmental interventions, family support and preventive measures to limit subsequent health problems.
The diagnosis of FAS has not been monitored consistently on a provincial or national basis, which has resulted in significant underreporting and, therefore, an inadequate allocation of resources. A standardized interdisciplinary approach to early diagnosis is essential for more accurate surveillance of FASD.4
The FASD diagnostic process
The diagnostic process for FASDs is complex, given the wide range in the type and severity of the possible effects of prenatal alcohol exposure. The best way to ensure an accurate diagnosis is through a comprehensive, multidisciplinary assessment that involves physicians (generally pediatricians, clinical geneticists, psychiatrists or neurologists) and educational psychologists or neuropsychologists, joined by other developmental specialists as indicated by the age or presentation of the patient (e.g., speech or language pathologists, occupational therapists and physiotherapists).
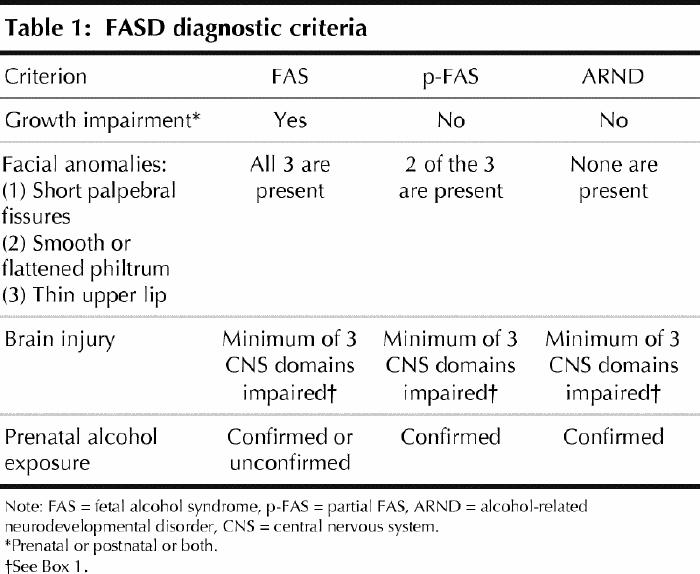
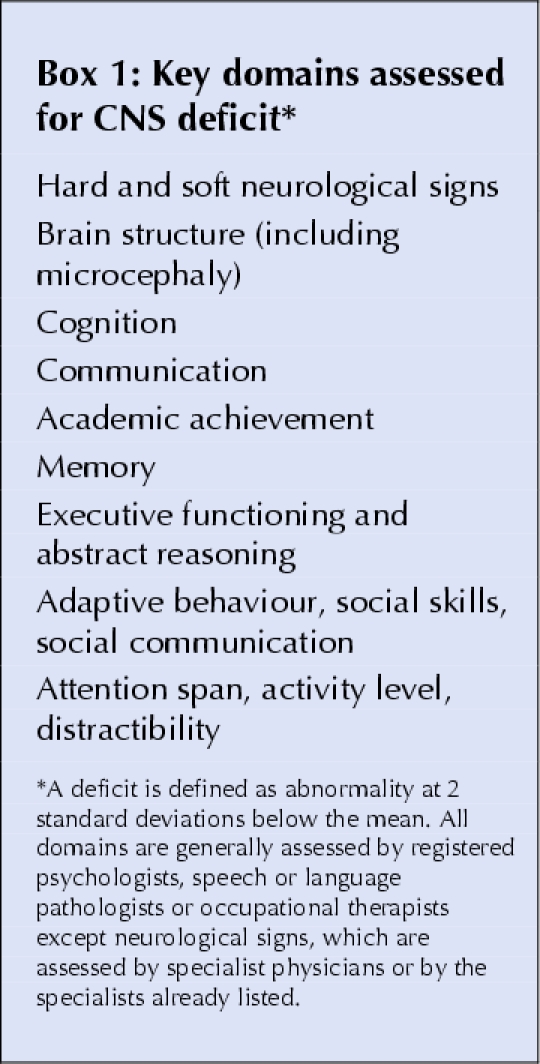
The criteria for FASD diagnoses are shown in Table 1 (a formal 4-Digit Diagnostic Code is presented in the supplement). Box 1 outlines the key domains of the central nervous system (CNS) that are assessed in the diagnostic process. Most of the domains are generally tested by registered psychologists, speech or language pathologists or occupational therapists. To make a diagnosis of brain injury, expert consensus has recommended that there be abnormalities in at least 3 domains at 2 standard deviations below that expected in the normal population.
Table 1
Box 1.
The role of the primary care physician
The primary care physician is involved in screening for alcohol use in pregnant women, referral for diagnosis, follow-up and linking patients to the community resources.
Screening
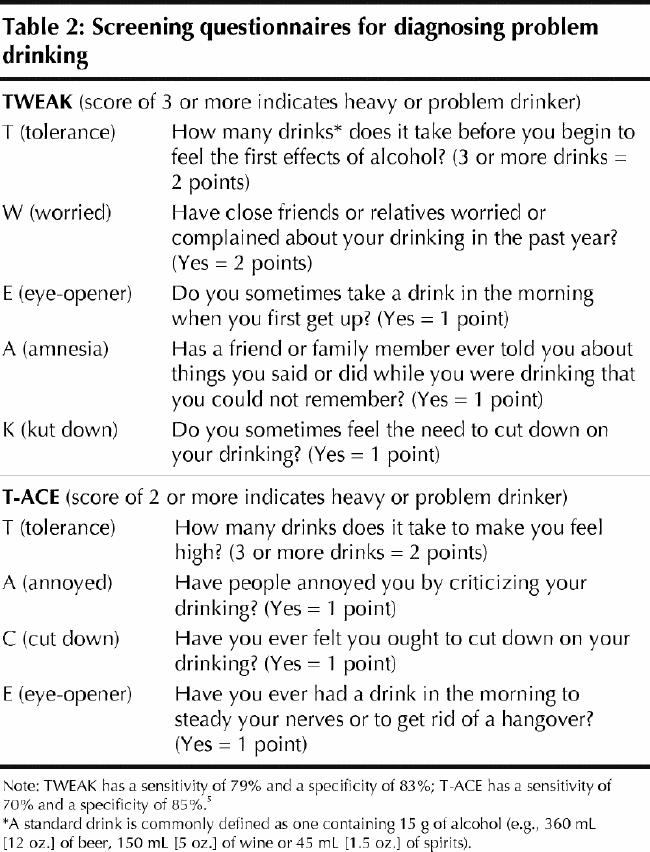
Tools for screening for alcohol misuse in women that have been found to be both sensitive and specific include CRAFFT (Box 2) for adolescent women and the modified CAGE (T-ACE and TWEAK; Table 2) for pregnant and nonpregnant women. Additional training to ask questions related to alcohol use during pregnancy in a consistent, sensitive and culturally appropriate manner may be required.
Box 2.
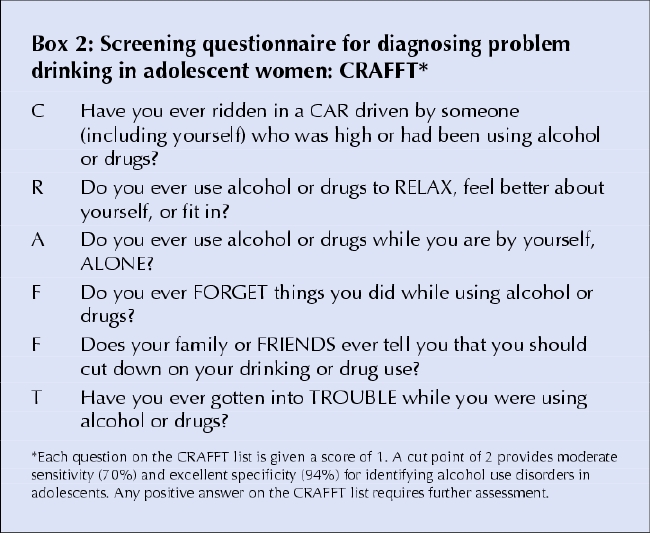
Table 2
When a patient is found to be misusing alcohol, the primary care physician is in the ideal role to obtain additional information regarding quantity and maximum frequency of alcohol use, to validate the screening, to provide support and counselling when trained in early brief intervention or motivational interviewing techniques, and to make referrals when indicated. National Institute on Alcohol Abuse and Alcoholism guidelines recommend that any woman who drinks more than 7 drinks per week or more than 3 drinks on any given day in the past month should be further assessed for risk of alcohol-related problems. Recent data suggest that prenatal exposure to small amounts of alcohol — as low as 1 standard drink per day, where a standard drink contains about 0.5 oz of ethanol alcohol (e.g., 360 mL [12 oz.] of beer, 150 mL [5 oz.] of wine or 45 mL [1.5 oz.] of spirits) — has some neurobehavioural effects on the offspring.6 Since the precise lower threshold for ethanol embryopathy is unknown, pregnant women should be advised to abstain from all alcohol use if possible.
Who should be referred for multidisciplinary assessment?
Patients should be referred for assessment in the following situations:
presence of 3 facial anomalies characteristic of prenatal alcohol exposure (see Table 1) and evidence of significant prenatal exposure to alcohol at levels known to be associated with physical and developmental effects;
presence of 1 or more facial anomalies, growth impairment and known or probable significant prenatal alcohol exposure;
presence of 1 or more facial anomalies, 1 or more CNS deficits (see Box 1) and known or probable significant prenatal alcohol exposure;
presence of 1 or more facial anomalies, growth impairment and 1 or more CNS deficits;
CNS deficits and known or probable significant prenatal alcohol exposure.
Accurate identification of facial anomalies characteristic of prenatal alcohol exposure may be challenging for many clinicians (figures showing these anomalies are provided in the supplement). Although it is unnecessary that facial anomalies be identified for patient referral, the family physician's information on pre- and postnatal growth and on maternal health and risk factors for alcohol intake during pregnancy are essential for accurate diagnosis. It is vital, therefore, that the referral include as much information as possible regarding alcohol and other potential teratogen exposure or genetic factors to assist with diagnostic accuracy and to consider and exclude other confounding or comorbid conditions.
Conclusion
The diagnostic assessment for prenatal alcohol exposure is a diagnosis for the affected individual, their mother, and other possibly affected family members. The primary care physician is a catalyst for prevention of continued exposure and subsequent affected siblings, referrals for diagnostic assessment, and links to services and resources to improve outcome.
Christine Loock Department of Pediatrics Julianne Conry Department of Educational and Counselling Psychology and Special Education University of British Columbia Vancouver, BC Jocelynn L. Cook Department of Obstetrics and Gynecology University of Ottawa Ottawa, Ont. Albert E. Chudley Departments of Pediatrics and Child Health and Biochemistry and Medical Genetics University of Manitoba Winnipeg, Man. Ted Rosales Department of Pediatrics Memorial University of Newfoundland St. John's, NL
References
- 1.Chudley AE, Conry J, Cook JL, Loock C, Rosales T, LeBlanc N. Fetal alcohol spectrum disorder: Canadian guidelines for diagnosis. CMAJ 2004;172(Suppl 5). [DOI] [PMC free article] [PubMed]
- 2.Streissguth A, Barr H, Kogan J, Bookstein F. Primary and secondary disabilities in fetal alcohol syndrome. In: Streissguth AP, Kanter J, editors. The challenge of fetal alcohol syndrome: overcoming secondary disabilities. Seattle: University of Washington Press; 1997. p. 25-39.
- 3.Astley SJ, Bailey D, Talbot C, Clarren SK. Fetal alcohol syndrome (FAS) primary prevention through FAS diagnosis: II. A comprehensive profile of 80 birth mothers of children with FAS. Alcohol Alcohol 2000;35(5):509-19. [DOI] [PubMed]
- 4.Astley SJ. Diagnostic guide for fetal alcohol spectrum disorders: The 4-Digit Diagnostic Code (3rd edition). Seattle: University of Washington Publication Services; 2004. Available: http://depts.washington.edu/fasdpnhtmls/4-digit-code.htm (accessed 2005 Feb 1).
- 5.Chang C., Wilkins-Haug L, Berman S, Goetz MA, Behr H, Hiley A. Alcohol use and pregnancy: improving identification. Obstet Gynecol 1998; 91 (6) :892-8. [DOI] [PubMed]
- 6.Sood B, Delaney-Black V, Covington C, Nordstrom-Klee B, Ager J, Templin T, et al. Prenatal alcohol exposure and childhood behaviour at age 6 to 7 years: I. dose-response effect. Pediatrics 2001;108(2):E34. [DOI] [PubMed]


