Abstract
Background
Currently there is a lot of debate about the advantages and disadvantages of for-profit health care delivery. We examined staffing ratios for direct-care and support staff in publicly funded not-for-profit and for-profit nursing homes in British Columbia.
Methods
We obtained staffing data for 167 long-term care facilities and linked these to the type of facility and ownership of the facility. All staff were members of the same bargaining association and received identical wages in both not-for-profit and for-profit facilities. Similar public funding is provided to both types of facilities, although the amounts vary by the level of functional dependence of the residents. We compared the mean number of hours per resident-day provided by direct-care staff (registered nurses, licensed practical nurses and resident care aides) and support staff (housekeeping, dietary and laundry staff) in not-for-profit versus for-profit facilities, after adjusting for facility size (number of beds) and level of care.
Results
The nursing homes included in our study comprised 76% of all such facilities in the province. Of the 167 nursing homes examined, 109 (65%) were not-for-profit and 58 (35%) were for-profit; 24% of the for-profit homes were part of a chain, and the remaining homes were owned by a single operator. The mean number of hours per resident-day was higher in the not-for-profit facilities than in the for-profit facilities for both direct-care and support staff and for all facility levels of care. Compared with for-profit ownership, not-for-profit status was associated with an estimated 0.34 more hours per resident-day (95% confidence interval [CI] 0.18–0.49, p < 0.001) provided by direct-care staff and 0.23 more hours per resident-day (95% CI 0.15–0.30, p < 0.001) provided by support staff.
Interpretation
Not-for-profit facility ownership is associated with higher staffing levels. This finding suggests that public money used to provide care to frail eldery people purchases significantly fewer direct-care and support staff hours per resident-day in for-profit long-term care facilities than in not-for-profit facilities.
Nnursing homes provide long-term housing, support and direct care to members of the community who are unable to function independently because of medical, physical and cognitive disabilities. Although only a small proportion of older Canadians reside in nursing homes (18% of those ≥ 80 years), the majority (81%) of long-term care residents are frail elderly people over the age of 65.1
Government-funded long-term care in Canada has been provided for many years by a mix of not-for-profit (nonproprietary) and for-profit (proprietary) facilities. The ratio of this mix varies greatly by province. For example, in Ontario 52% of publicly funded nursing homes are for-profit, as compared with 15% in Manitoba.2
Previous studies from the United States have shown that having more direct-care personnel is associated with better care in nursing homes.3,4,5,6,7 Specifically, higher numbers of registered-nurse hours per resident-day have been associated with fewer violations of care standards4 and improved functional ability of residents.7 Schnelle and colleagues examined 21 nursing homes in California and found that the homes with the highest number of nurse aides performed significantly better in 13 of 16 quality-of-care measures than the homes with fewer nurse aides.6 Although there has been little research on staffing levels and nursing home care in other countries, health policy-makers in the United Kingdom8 and Australia9 have begun to call for greater accountability for public resources spent in this area.
The American literature has also shown that, compared with for-profit nursing homes, not-for-profit facilities have higher direct-care staffing levels4 and lower staff turnover rates.10,11 However, the majority of nursing home care in the United States is delivered by the for-profit sector, whereas in Canada the not-for-profit sector constitutes the majority. This may result in a difference in the informal benchmarks for staffing levels between the 2 countries. There also may be a wider variation in wages and working conditions among nursing homes in the United States, which potentially confounds the comparison between for-profit and not-for-profit facilities.
We compared staffing levels of nursing and support staff in publicly funded long-term care facilities by ownership type (not-for-profit v. for-profit) in British Columbia at a time when the majority of publicly funded not-for-profit and for-profit facilities employed a unionized labour force with standardized wages and benefits set by a master collective agreement.
In British Columbia, approximately 70% of publicly funded nursing homes are nonproprietary (not-for-profit) and 30% are proprietary (for-profit). Both not-for-profit and for-profit facilities receive global funding from the provincial government on the basis of (a) the level of functional dependence of facility residents and (b) the percentage of fees borne by residents according to their income levels. At the time of the study (2001), there was no regulation by government or the regional health authorities as to how individual facilities allocated funding between staffing, administration or property costs.
Not-for-profit long-term care in British Columbia is delivered by religious, cultural or other community-based societies, by regional health authorities or by publicly owned acute care hospitals. For-profit care is delivered by sole operators or by facilities that are part of larger business entities (chains). Nursing homes are grouped by levels of care according to the residents' case-mix: intermediate care only (IC), intermediate and extended care (IC & EC), multi-level care, or extended care only. IC facilities provide care for people with relatively more functional ability, whereas extended care facilities accommodate the most functionally dependent people. The other 2 facility types provide care for people with a mix of functional abilities.
Methods
After obtaining ethics approval from the University of British Columbia Behavioural Research Ethics Board, we collected all available data for publicly funded long-term care facilities (nursing homes) in British Columbia. We included all long-term care facilities providing care to primarily frail, older residents with a designation of IC, IC & EC, or multilevel care (Fig. 1). Facilities providing extended care only (n = 24) were excluded, as data on facilities in this sector were incomplete. Four other facilities (3 IC and 1 IC & EC) attached to hospitals were also excluded, as it was not possible to disaggregate staffing data from the acute care side of the hospital.
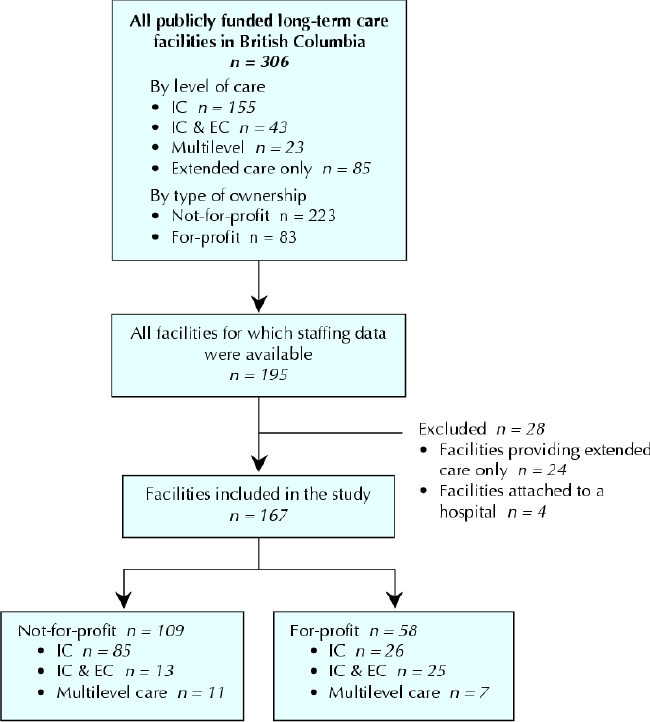
Fig. 1: Publicly funded long-term care facilities in British Columbia included in the study. IC = intermediate care, IC & EC = intermediate and extended care.
Information on nursing home staffing levels was obtained from the British Columbia Labour Relations Board. The board collected staffing information from each long-term care facility before the expiry of the 1998–2001 master collective agreement between the Health Employers Association of British Columbia and the health sector unions.12 The information was agreed upon by both union and management and was submitted to the board so that they could determine essential staffing levels in the event of a strike.
Staffing data were linked to the ownership status of a facility, as determined by the registered facility's legal name. Facilities registered as “societies” or as part of a regional health authority were classified as not-for-profit. Facilities registered as “corporations” were classified as for-profit. We also determined whether for-profit facilities were part of a larger corporate chain. This information was collected from a variety of sources, including government agencies and long-term care facility Web sites.13,14
The facility's level of care (IC, IC & EC, or multilevel) was used as a surrogate measure to control for resident case-mix. Data on levels of care were collected from the British Columbia Labour Relations Board registry (and then cross-referenced with Ministry of Health data), Web sites set up by the various regional health authorities and several other sources.13,14,15,16,17,18,19 Facility size was measured by bed numbers, information that was gathered from the same data sources used to determine the facility's level of care. Full occupancy was assumed on the basis of a waitlist of several months for all nursing homes at the time of the study.
We calculated the mean number of staff hours per resident-day by multiplying the number of full-time equivalent positions for a given job classification by 7.2 hours (the standard full-time shift designated by the collective agreement) and dividing the value by the number of beds in a given facility. We then created a composite variable for direct-care hours by adding up the mean number of hours per resident-day provided by registered nurses (RNs), licensed practical nurses (LPNs) and resident care aides (RCAs). Similarly, we calculated a composite variable for support staff hours by adding up the hours of work per resident-day provided by housekeeping, dietary and laundry staff. We also calculated the mean number of hours per resident-day provided by activity aides (employees who organize recreational programs).
The unit of analysis was the long-term care facility. Descriptive statistics were calculated for the mean staffing hours per resident-day — stratified by facility level of care and ownership type — for each job classification (RN, LPN, RCA, activity aide, and dietary, housekeeping and laundry staff) and for the composite measures of direct-care and support staff hours. We used one-way analysis of variance (ANOVA) and univariate linear regression, where appropriate, to examine the association of individual characteristics of facilities (ownership, levels of care and size) with the outcome variables (number of direct-care and support staff hours per resident-day). We used two-way ANOVA and analysis of covariance (ANCOVA) to calculate estimates and 95% confidence intervals (CIs) for the difference in the total mean number of direct-care and support staff hours in not-for-profit facilities compared with for-profit facilities, after adjusting for nursing home size (bed numbers) and facility level of care.
Results
The nursing homes in our study represented 76% (167/221) of the facilities in British Columbia with a level-of-care designation of IC, IC & EC, or multilevel (Fig. 1). Of the 167 nursing homes examined, 109 (65%) were not-for-profit and 58 (35%) were for-profit facilities (Fig. 1). Of the 58 for-profit facilities, 14 (24%) were part of a chain.
Fig. 1 shows the distribution of not-for-profit and for-profit nursing homes by level of care. The mean number of beds in the total sample of facilities was 87 (standard deviation [SD] 52.4, range 18–300). The mean number of beds in not-for-profit facilities was 91 (SD 52.7), as compared with 81 in for-profit facilities (SD 51.6), a difference that was not statistically significant (p = 0.24).
The mean number (and SD) of hours per resident-day provided by direct-care staff differed significantly by facility level of care: it was 2.46 (0.33) in IC facilities, 3.06 (0.64) in IC & EC facilities, and 3.18 (0.64) in multilevel facilities (p < 0.001). The corresponding numbers for hours per resident-day provided by support staff were 1.05 (0.22), 1.11 (0.28) and 1.17 (0.26) (p = 0.08). There was no significant association between facility size and direct-care or support staff hours in the univariate analysis (p = 0.43 and p = 0.36 respectively).
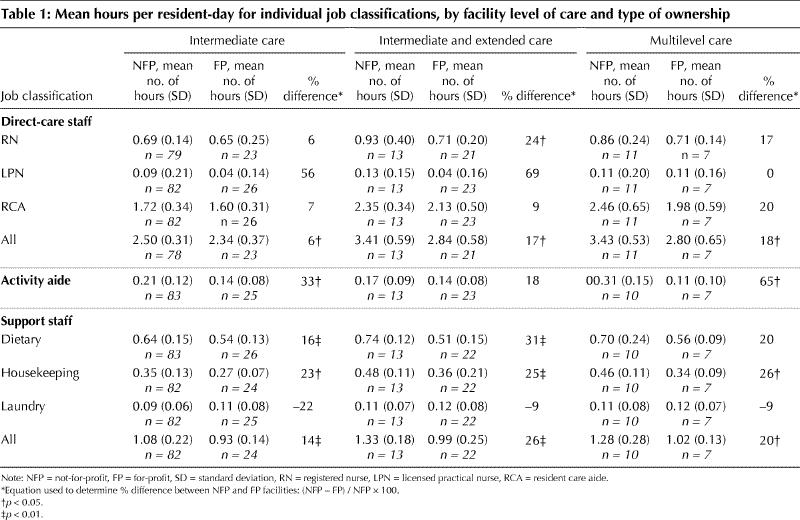
Table 1 shows the mean number of staff hours stratified by facility level of care, ownership and individual occupations. For almost all occupations, the mean number of hours per resident-day was higher in the not-for-profit than in the for-profit facilities.
Table 1
The mean number (and SD) of hours per resident-day provided by direct-care staff did not differ significantly between the single-operator for-profit facilities and the corporate chain facilities (unadjusted for level of care: 2.63 [0.56] and 2.56 [0.55] respectively, p = 0.70). The same was true for the mean number of hours provided by support staff (0.98 [0.21] and 0.94 [0.14] respectively, p = 0.57).
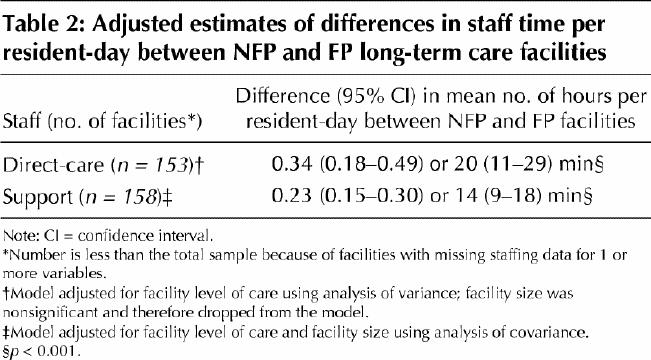
Compared with for-profit ownership, not-for-profit status was associated with an estimated 0.34 more hours per resident-day (95% CI 0.18–0.49, p < 0.001) provided by direct-care staff after adjustment for facility level of care. Facility size was initially included in the analysis of direct-care hours but was determined to be nonsignificant and was therefore dropped from the final model (Table 2). Not-for-profit status was associated with an estimated 0.23 more hours per resident-day (95% CI 0.15–0.30, p < 0.001) provided by support staff after adjustment for facility size and level of care (Table 2).
Table 2
Interpretation
We found that the number of hours per resident-day provided by direct-care staff and support staff was significantly higher in the not-for-profit facilities than in the for-profit facilities after adjusting for facility size and level of care. The adjusted difference between not-for-profit and for-profit facilities was 20 minutes (95% CI 11–29 minutes) per resident-day for direct-care staff and 14 minutes (95% CI 9–18 minutes) per resident-day for support staff.
Although it is difficult to quantify the clinical impact of this difference, previous research has shown that it takes about 8 minutes to provide 1 episode of toiletting assistance,20 and protocols that increase residents' independence in morning activities of daily living take about 7 to 11 minutes.21 Group feeding assistance at a ratio of 1 RCA to 3 residents is estimated to take 18 minutes.5
Although staffing differences do not necessarily imply differences in quality of care, an extensive body of research in the United States links higher direct-care staffing levels in long-term care facilities to better care outcomes.3,4,6 A recent study commissioned by the US Congress examined over 5000 long-term care facilities in 10 states and determined that higher staffing continued to predict improved care outcomes (eg., maintenance of skin integrity, good nutritional status) up to certain thresholds. Beyond these thresholds no further improvements could be demonstrated.5 These thresholds were 1.3 RN- and LPN-hours and 2.8 RCA-hours per resident-day — levels that are considerably higher than the mean staffing levels reported in our study. Although the role of activity aides has not been studied extensively, Reid and colleagues found that higher ratios of activity aides to residents had beneficial effects on residents' cognitive function and social and language skills.22
The finding that not-for-profit ownership was associated with a higher mean number of hours per resident-day is consistent with US findings10,23 and suggests that in both countries the financial imperatives of for-profit ownership in nursing home care operate in a similar manner. One of these imperatives may be the higher property costs associated with private investment. In all of the facilities in our study, the staff had similar wages and benefits set by a master collective agreement. Because lower staffing levels are likely to be one of the options available to generate profit in a system with fixed costs for wages, it is not surprising that staffing levels were lower in the for-profit facilities.
Although a possible association has been proposed between nosocomial infection and the availability of cleaning staff,24 there has been no research in the United States, Canada or elsewhere into the relation between non-nursing support staff (cleaners, laundry and dietary workers), type of ownership and patient outcomes. Further research exploring the effect of staffing levels of support staff on the quality of direct-care and resident outcomes is needed.
Our study was limited by its retrospective design. As with all retrospective studies, there is the possibility of misclassification and missing data resulting in unintended bias. It is also possible that the care demands of residents in for-profit facilities are lower in ways that are not measurable at the facility level of care. However, we think that this is unlikely given that managers of both facility types have an interest in maintaining a certain volume of more functionally dependent clients within the limits of their care designation in order to ensure adequate funding levels. Finally, our study has limited generalizability both in British Columbia, because of the exclusion of facilities offering only extended care from the sample, and in the rest of Canada, because of possible differences in wages and provincial regulation of nursing home care between provinces. However, the facilities studied represented 76% of all IC, IC & EC, and multilevel facilities in British Columbia. In addition, we used a novel method for collecting staffing data that was likely quite accurate, given that both local union and management were required by the Labour Relations Board to agree on staffing levels in their respective facilities before their submission to the board.
Similar funding formulas applied to not-for-profit and for-profit long-term care facilities in British Columbia purchase significantly more direct-care and support staff hours per resident-day in the not-for-profit sector. This difference between the 2 sectors may have implications for quality of care. Further research is needed to understand whether these differences in staffing levels are present in other provinces and whether they translate into differences in health outcomes among residents in nursing homes.
Acknowledgments
We gratefully acknowledge the assistance of Evelyn Shapiro, Manitoba Centre for Health Policy, University of Manitoba, who provided information on the background and context for the study and helped to review the manuscript; Edwin Mak, who assisted in the data analysis; and Sam Sheps from the Department of Healthcare and Epidemiology, University of British Columbia, who assisted with critical review of the manuscript.
Footnotes
This article has been peer reviewed.
Contributors: Margaret McGregor contributed to the research design, coordinated the implementation of the research and played a mjaor role in writing the manuscript. Marcy Cohen assisted with the study design and implementation, interpretion of the results and writing the manuscript. Kimberlyn McGrail assisted with supervision of the data collection, interpretation of the data analysis and writing the manuscript. Anne Marie Broemeling assisted with data interpretation and writing the manuscript. Reva Adler helped to obtain the research funding and assisted with writing the manuscript. Michael Schulzer performed the data analysis. Lisa Ronald, Mary Beck and Yuri Cvitkovich assisted with the data collection and classification of nursing homes. All of the authors gave final approval of the version to be published.
The study was funded by the Vancouver Foundation (FY 02-03).
Competing interests: Marcy Cohen is a researcher for the Hospital Employees Union, and Anne Marie Broemeling is Director of Research and Evaluation for the Interior Health Authority.
Correspondence to: Dr. Margaret J. McGregor, Mid-Main Community Health Centre, 3998 Main St., Vancouver BC V5V 3P2; fax 604-875-8790; mrgret@interchange.ubc.ca
References
- 1.Tully P, Mohl C. Older residents of health care institutions. Health Rep 1995;7(3):27-30. [PubMed]
- 2.Ontario Health Coalition. Ownership matters — lessons from Ontario's long-term care facilities. Toronto: The Coalition; 2002. p. 1-17. Available: www.web.net/ohc/docs/may2702.htm (accessed 2005 Jan 24).
- 3.Spector WD, Takada HA. Characteristics of nursing homes that affect resident outcomes. J Aging Health 1991;3(4):427-54. [DOI] [PubMed]
- 4.Harrington C, Zimmerman D, Karon SL, Robinson J, Beutel P. Nursing home staffing and its relationship to deficiencies. J Gerontol B Psychol Sci Soc Sci 2000;55(5):S278-87. [DOI] [PubMed]
- 5.Centers for Medicare & Medicaid Services. Report to Congress: Appropriateness of minimum nurse staffing ratios in nursing homes phase II final report. Baltimore: The Centers; 2001. Available: www.cms.hhs.gov/medicaid/reports/rp1201home.asp (accessed 2003 June 30).
- 6.Schnelle JF, Simmons SF, Harrington C, Cadogan M, Garcia E, M Bates-Jensen B. Relationship of nursing home staffing to quality of care. Health Serv Res 2004;39(2):225-50. [DOI] [PMC free article] [PubMed]
- 7.Linn MW, Gurel L, Linn BS. Patient outcome as a measure of quality of nursing home care. Am J Public Health 1977;67(4):337-44. [DOI] [PMC free article] [PubMed]
- 8.Kerrison SH, Pollock AM. Regulating nursing homes: caring for older people in the private sector in England. BMJ 2001;323(7312):566-9. [DOI] [PMC free article] [PubMed]
- 9.Braithwaite J. Regulating nursing homes: the challenge of regulating care for older people in Australia. BMJ 2001;323(7310):443-6. [DOI] [PMC free article] [PubMed]
- 10.Aaronson WE, Zinn JS, Rosko MD. Do for-profit and not-for-profit nursing homes behave differently? Gerontologist 1994;34(6):775-86. [DOI] [PubMed]
- 11.Banaszak-Holl J, Hines MA. Factors associated with nursing home staff turnover. Gerontologist 1996;36(4):512-7. [DOI] [PubMed]
- 12.BC Labour Relations Board. BC Labour Relations Essential Services Staffing Level Agreement 2001. Vancouver: The Board.
- 13.Canadian Healthcare Association. Guide to Canadian healthcare facilities 2000–2001. Vol 10. Ottawa: The Association; 2000. p. 53-86.
- 14.British Columbia Health Industries Network. Health-related agencies. Available: www.hinetbc.org/database/findit.asp?t=sector&r1=5 (accessed 2003 June 10).
- 15.Fraser Health Authority & Vancouver Coastal Health Authority. Continuing care facilities in the lower mainland. Available: www2.vpl.vancouver.bc.ca/DBs/Redbook/htmlPgs/home.html (accessed 2003 May 30).
- 16.Interior Health Authority. Appendix K — Summary by health service area: residential care. Available: www.interiorhealth.ca/Media+Centre/Documents/Redesign_Interior_Health.htm (accessed 2003 May 30).
- 17.Northern Health Authority. Communities and facilities. Available: northernhealth.ca/nha/health/facilities (acessed 2003 June 3).
- 18.Vancouver Coastal Health Authority. Residential care facilities. Available: www.vcha.net/Programs/programs.asp?service=005 (accessed 2003 June 3).
- 19.Victoria Gerontology Association. Continuing care facilities — Vancouver Island. Available: www.guide4seniors.com/content/?go=housing&type=4 (accessed 2003 May 30).
- 20.Schnelle JF, Sowell VA, Traughber B, Hu TW. A behavioral analysis of the labor cost of managing continence and incontinence in nursing home patients. J Organizational Behav Management 1988;9(2):137-53.
- 21.Centers for Medicare & Medicaid Services. Report to Congress: Appropriateness of minimum nurse staffing ratios in nursing homes [phase I report]. Baltimore: The Centers; 2000. Available: www.cms.hhs.gov/medicaid/reports/rp700hmp.asp (accessed 2004 Sept 4).
- 22.Reid RC, Chappell NL. Outcomes in special care units: Do activity aides make a difference? J Appl Gerontol 2003;22(1):89-103.
- 23.Harrington C, Woolhandler S, Mullan J, Carrillo H, Himmelstein DU. Does investor ownership of nursing homes compromise the quality of care? Am J Public Health 2001;91(9):1452-5. [DOI] [PMC free article] [PubMed]
- 24.Dancer SJ. Mopping up hospital infections. J Hosp Infect 1999;43(2):85-100. [DOI] [PubMed]


