Abstract
Introduction
Previous studies have reported associations between prenatal cell phone use and child behavioral problems, but findings have been inconsistent and based on retrospective assessment of cell phone use. This study aimed to assess this association in a multi-national analysis, using data from three cohorts with prospective data on prenatal cell phone use, together with previously published data from two cohorts with retrospectively collected cell phone use data.
Methods
We used individual participant data from 83,884 mother-child pairs in the five cohorts from Denmark (1996–2002), Korea (2006–2011), the Netherlands (2003–2004), Norway (2004–2008), and Spain (2003–2008). We categorized cell phone use into none, low, medium, and high, based on frequency of calls during pregnancy reported by the mothers. Child behavioral problems (reported by mothers using the Strengths and Difficulties Questionnaire or Child Behavior Checklist) were classified in the borderline/clinical and clinical ranges using validated cut-offs in children aged 5–7 years. Cohort specific risk estimates were meta-analyzed.
Results
Overall, 38.8% of mothers, mostly from the Danish cohort, reported no cell phone use during pregnancy and these mothers were less likely to have a child with overall behavioral, hyperactivity/inattention or emotional problems. Evidence for a trend of increasing risk of child behavioral problems through the maternal cell phone use categories was observed for hyperactivity/inattention problems (OR for problems in the clinical range: 1.11, 95%CI 1.01, 1.22; 1.28, 95%CI 1.12, 1.48, among children of medium and high users, respectively). This association was fairly consistent across cohorts and between cohorts with retrospectively and prospectively collected cell phone use data.
Conclusions
Maternal cell phone use during pregnancy may be associated with an increased risk for behavioral problems, particularly hyperactivity/inattention problems, in the offspring. The interpretation of these results is unclear as uncontrolled confounding may influence both maternal cell phone use and child behavioral problems.
Keywords: Attention Deficit Disorder with Hyperactivity, Cell Phones, Child Behavior, Child Health, Electromagnetic Radiation, Pregnancy
1. INTRODUCTION
Cell phone use is widespread throughout the world (World Bank, 2014) and radio frequency electromagnetic field (RF-EMF) exposure from cell phone use has been well documented (Cardis et al., 2011). Health consequences regarding this exposure have been researched but strong conclusions are not yet justified (Kostoff and Lau, 2013; Swerdlow, 2012). While short term exposure to RF-EMF is generally considered safe in adults, long term exposure have not been thoroughly explored (World Health Organization, 2002). If long-term RF-EMF exposure does in fact impact human health, there is concern that fetuses or children would be more vulnerable than adults to this potential influence, given the rapid development of neurological and organ systems in early life and the extended exposure over the entire lifespan (Kheifets et al., 2005; Leung et al., 2011). Therefore, cohort studies with prospective data on RF-EMF exposure and neuropsychological development in children have been identified as a high-priority research need (National Research Council, 2008; van Deventer et al., 2011). Some studies in rats or mice have shown that extended RF-EMF exposure in pregnant dams was linked to hyperactivity, altered neurons, or impaired cognition in offspring (Aldad et al., 2012; Haghani et al., 2013; Zhang et al., 2015), while another study in rats did not support these findings (Shirai et al., 2014); but the relevance of these studies to human health is not clear.
Recently, in a large prospective cohort study, researchers in Denmark produced two independent analyses (n=12,796 and n=28,745) showing that mothers who more often used cell phones (the main sources of RF-EMF exposure to the head) during pregnancy were more likely to have children with behavioral problems at age 7 (Divan et al., 2012, 2008). These results were corroborated in a further analysis (n=51,190) where cell phone use (during pregnancy and at age 7) was associated with emotional and behavioral difficulties at age 11 (Sudan et al., 2016). In a smaller sample (n=2,532), researchers in The Netherlands did not find associations between prenatal cell phone use and behavioral problems in children at age 5 in their cohort (Guxens et al., 2013), but confidence intervals overlapped with estimates in the Danish analyses (Sudan et al., 2013). A main limitation in both studies was potential recall bias since mothers recalled their prenatal cell phone use when the child was 7 years old.
Considering that a true association would have a large health impact worldwide given the ubiquity of cell phones, it is necessary to explore this association among cohorts wherein mothers reported cell phone use prospectively during pregnancy, i.e. long before the onset of any behavioral symptoms in the child. Therefore, the aim of this study was to assess the association between maternal cell phone use during pregnancy and behavioral problems in children ages 5–7 using data from three birth cohorts from Korea, Norway, and Spain where mothers reported cell phone use prospectively at 1st and/or 3rd trimester of pregnancy, together with the data from the Danish and Dutch cohorts where maternal cell phone use during pregnancy was reported retrospectively when children were 7 years old.
2. METHODS
2.1 Study Population
As part of the Generalized EMF Research using Novel Methods (GERoNiMO) Project (“Generalized EMF research using novel methods,” 2014), five population-based prospective birth cohorts spanning Europe and Asia (Table 1) were harmonized for analysis regarding maternal cell phone use during pregnancy. These were: the Amsterdam Born Children and their Development Study (ABCD) (Eijsden et al., 2011), the Danish National Birth Cohort (DNBC) (Olsen et al., 2001), the Spanish Environment and Childhood Project (INMA) (Guxens et al., 2012), the Norwegian Mother and Child Cohort Study (MoBa) (Magnus et al., 2006), and the Korean Mothers and Children’s Environment Health Study (MOCEH) (Kim et al., 2009). Informed consent was obtained from all participants in accordance with each study’s institutional review board or ethics committee. Enrollment in the five cohorts spanned 1996–2011 with more than 190,000 mother-child pairs (Table 1). Across all cohorts, 83,884 mother-child pairs met our inclusion criteria of having information on frequency of maternal cell phone use during pregnancy and having collected a behavioral assessment of the child at 5–7 years (Table 1).
Table 1.
Description of participating birth cohorts, exposures, and outcomes in analysis
| Cohort | Location | Enrollment
|
Cell phone use during pregnancy
|
Behavioral problems
|
N included in analysisa | ||||
|---|---|---|---|---|---|---|---|---|---|
| Time period | N | Time of collection | N collected | Assessment | Age at assessment | N collected | |||
|
|
|
|
|
||||||
| ABCD | The Netherlands | 2003–2004 | 8,266 | Postnatal 7 years | 2,611 | SDQ | 5 years | 4,511 | 2,420 |
| DNBC | Denmark | 1996–2002 | 91,661 | Postnatal 7 years | 50,040 | SDQ | 7 years | 54,907 | 50,039 |
| INMA | Spain | 2003–2008 | 2,270 | Pregnancy | 1,993 | SDQ | 4–7 years | 1,288 | 1,205 |
| MoBa | Norway | 2004–2008 | 93,891 | Pregnancy | 93,891 | Adapted CBCL | 5 years | 32,587 | 29,720 |
| MOCEH | Korea | 2006–2011 | 1,751 | Pregnancy | 1,435 | CBCL | 5 years | 500 | 500 |
|
| |||||||||
| Total N | 197,839 | 149,970 | 93,793 | 83,884 | |||||
Abbreviations: CBCL, child behavior checklist; SDQ, strengths and difficulties questionnaire.
With data on cell phone use and behavioral problems
2.2 Maternal cell phone use during pregnancy
When children were 7 years old in the Dutch and Danish cohorts, mothers were asked to recall frequency of cell phone use during pregnancy. In Spain, Norway, and Korea, mothers were asked during pregnancy to report frequency of cell phone use (Table 1). In each cohort, questionnaires captured frequency of maternal cell phone use using different questions and number of calls categorization (Table 2 and Supplemental Table S1). Mothers in the Dutch cohort were also asked to recall cordless phone use during pregnancy. For the purpose of this study, we created a frequency of use variable (none, low, medium, and high) to classify maternal cell phone use during pregnancy in all cohorts (Table 2). We created the same categories for maternal cordless phone use during pregnancy. The creation of these classifications was blind to child behavioral problems.
Table 2.
Maternal cell phone use during pregnancy by cohort [% (n)]
| Categorization used in analysis | Netherlands | Denmark | Spaina | Norway | Koreaa | Total | |||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|
|||||
| None | none | 6.7 (163) | 60.8 (30,419) | 2.9 (35) | Seldom/neverb | 6.5 (1,938) | none | 0.8 (4) | 38.8 (32,564) |
| Low (reference) | 0–1 calls/day | 43.4 (1,051) | 21.9 (10,947) | 37.6 (451) | A few times a week | 38.9 (11,572) | 1–2 calls/day | 17.5 (85) | 28.7 (24,191) |
| Medium | 2–3 calls/day 4 calls or |
27.4 (662) | 12.4 (6,207) | 38.3 (459) | Daily | 50.0 (14,855) | 3–5 calls/day 6 or more |
52.0 (253) | 26.8 (22,518) |
| High | more/day | 22.5 (544) | 4.9 (2,466) | 21.3 (255) | More than an hour a day | 4.6 (1,355) | calls/day | 29.8 (145) | 5.7 (4,804) |
In the INMA and MOCEH cohorts, 5 and 13 women, respectively, reported using a cell phone during pregnancy but did not report frequency and therefore were excluded from frequency of calls analyses.
Seldom/never was the lowest call frequency category collected in the MoBa cohort.
2.3 Behavioral problems
In all cohorts, overall behavioral problems, hyperactivity/inattention problems, and emotional problems were assessed. In the Danish, Dutch, and Spanish cohorts, child behavioral problems were assessed by using the parental Strength and Difficulties Questionnaire (SDQ) (Goodman, 1997) at ages 5–7, depending on cohort (Table 1). The SDQ is a short screening form, in this case completed by parents, consisting of 25 items with 5 for each dimension: emotional problems, conduct problems, hyperactivity/inattention problems, peer/social problems, and pro-social behavior (Goodman, 1997). Each item has a scaled response (very true, partly true, not true). Each dimension yields a score, and summation of 4 dimensions (pro-social behavior is excluded) yields an overall behavior difficulties score (Goodman, 1997). In the Spanish cohort, hyperactivity/inattention problems were also assessed by teachers at 5 years using the Attention Deficit and Hyperactivity Disorder criteria of the Diagnostic and Statistical Manual of Mental Disorders-IV (ADHD DSM-IV) (American Academy of Pediatrics, 2004). The ADHD DSM-IV consists of 18 symptoms, nine for inattention and nine for hyperactivity/impulsivity. Each symptom is rated on a 4-point scale (never or rarely, sometimes, often, or very often) (American Academy of Pediatrics, 2004). For the Spanish cohort, the SDQ assessment was used in our main analysis to be comparable with other cohorts, while the ADHD DSM-IV was used for a sensitivity analysis.
In the Korean cohort, children’s behavioral problems were assessed at 5 years by the parental Child Behavior Checklist (CBCL) (Achenbach, 2011). The CBCL is a standardized form that parents fill out to describe their children’s behavioral and emotional problems. The version for ages 1½ to 5 years includes 99 competence items and problems, asking the parent to indicate how each item applies to the child (not true, somewhat or sometimes true, and very true or often true) (Achenbach, 2011). The CBCL’s questions are associated with various disorders from the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR) (American Academy of Pediatrics, 2004) and syndrome scales, including overall behavioral problems, hyperactivity/inattention problems, and emotional problems. The Norwegian cohort used an adapted 25-item version of the CBCL with selected items of five subscales of the full CBCL (Garthus-Niegel et al., 2010). In this adapted CBCL, almost all items from the complete CBCL are present for the attention deficit/hyperactivity problems subscale. After administering this shorter CBCL from years 2004–2009, in 2010 MoBa added two items to this adapted version in order to complete the anxious/depressed subscale to assess emotional problems.
For all tests, higher scores indicated more behavioral problems. For cohorts in the Netherlands, Denmark, Spain, and Korea we used validated cut-offs to yield proxies for overall behavioral problems, hyperactivity/inattention problems, and emotional problems within the borderline/clinical range and within the clinical range only, specific for each test (Achenbach, 2011; American Academy of Pediatrics, 2004; Goodman, 1997) (Supplemental Table S2). For Norway’s adapted version of the CBCL we applied the cohort’s 93rd and 98th percentiles as cut-off scores to classify children with overall problems, hyperactivity/inattention problems and anxious/depressed problems (from here on referred to as emotional problems) within the borderline/clinical range and the clinical range, respectively (Supplemental Table S2). These percentile cutoffs were chosen based on the expected prevalence in the population if the full CBCL had been used, as the score cutoffs for the full CBCL are designed to select the 93rd and 98th percentiles (Achenbach, 2011).
2.4 Covariate data
Covariate information was collected in all cohorts during pregnancy or after birth through questionnaires or medical registries. Covariates for this analysis were identified based on previous studies (Divan et al., 2012, 2008; Guxens et al., 2013; Sudan et al., 2016). Covariates included age of child at time of assessment, geographical region (in Spain and Korea where this was heterogeneous), and the following maternal characteristics: age at birth, parity, country of birth (in the Netherlands, Denmark, and Spain where this was heterogeneous), marital status during pregnancy (living with the father or living alone), education (highest level completed: primary, secondary, university or higher), history of psychopathology (defined within cohorts, Supplemental Table S3), smoking during pregnancy (yes or no), secondhand smoking during pregnancy (defined within cohorts, Supplemental Table S4) alcohol consumption during pregnancy (yes or no), pre-pregnancy body mass index (BMI), and height.
2.5 Statistical Analysis
Differences in covariates between included and not-included subjects were compared using chi-square test or Student’s t-test. Among children with available data on exposure and outcome variables (n=83,884), we performed multiple imputation of missing covariate values using chained equations where 15 completed datasets were generated and analyzed using the standard combination rules for multiple imputation (Graham et al., 2007; Sterne et al., 2009). Distributions in imputed datasets were very similar to those observed (data not shown).
Maternal and child characteristics according to categories of the prenatal cell phone use were described using means (standard deviation) or proportions, with chi-square or ANOVA tests applied.
For behavioral problems scores, we used the SDQ for the Danish, Dutch and Spanish cohorts and the CBCL and adapted CBCL for Korea and Norway, respectively. Logistic regression models were used in order to examine the association between prenatal cell phone use and each one of the child behavior problem scales (normal vs. borderline/clinical range and normal vs. clinical range). We considered mothers that were low cell phone users during pregnancy as the reference category since only a small proportion of mothers reported no cell phone use in all cohorts, except Denmark.
First, models were adjusted for child’s age at time of behavioral assessment (minimally-adjusted models). Then, models were additionally adjusted for all the potential confounding variables described above (fully-adjusted models). Cohort specific risk estimates were then meta-analyzed and evaluated for heterogeneity using the Q test and the I2 statistic (Higgins et al., 2003; Thompson and Sharp, 1999). If estimates were heterogeneous (Cochran’s Q test p<0.05 and/or I2≥25%), random effects analysis was used.
We performed the following sensitivity analyses: i) meta-analysis excluding one cohort at a time to determine the influence of a particular cohort, ii) meta-analysis of associations among mothers who were very high cell phone users (10 or more calls a day in the Netherlands and Spain, 11 or more calls a day in Korea) during pregnancy in cohorts where this data was available (the Netherlands, Korea, and Spain), iii) meta-analysis of no prenatal cell phone use in the mother versus any prenatal cell phone use and behavioral problems in children, iv) meta-analysis stratified by timing of maternal cell phone use data collection (prospectively vs retrospectively), v) analysis of cohort specific associations in the Dutch cohort of maternal cordless phone use during pregnancy and behavioral problems, vi) analysis of cohort specific associations in the Spanish cohort using Attention Deficit and Hyperactivity Disorder criteria of the Diagnostic and Statistical Manual of Mental Disorders-IV (ADHD DSM-IV) (American Academy of Pediatrics, 2004) to assess hyperactivity/inattention problems instead of the SDQ, vii) and analysis of children born from 1996–2004 and those born from 2005–2011 to investigate possible time trends in cell phone use and behavioral problems.
All analyses were performed using Stata 14 statistical software (Stata Corporation, College Station, Texas). Data from all cohorts was sent to and analyzed at ISGlobal, except those from the Norwegian cohort which was analyzed onsite in Norway and summary results sent to ISGlobal for the joint meta-analysis. A consensus protocol was followed for all the analyses.
3. RESULTS
Compared with excluded mothers (those with cell phone use or child’s behavioral problems missing), mothers included in the present analysis were generally older, more often primiparous, more often had university education or higher, and were generally taller (data not shown). In the Norwegian cohort, mothers of children with the CBCL including the emotional subscale versus mothers of those without had higher education, were less likely to smoke or use alcohol and had lower BMI (data not shown).
In this study population of 83,884 mother-child pairs, 6.6% of children scored for having overall behavioral problems in the borderline/clinical range with 2.7% scoring within the clinical range (Table 3). For hyperactivity/inattention problems, 8.3% and 4.1% of children scored within the borderline/clinical range and clinical range, respectively. For emotional problems, 12.0% of children scored within the borderline/clinical range and 6.0% scored within the clinical range.
Table 3.
Child behavioral problems within borderline and clinical ranges among cohorts [%(n)]
| Cohort | Assessment | n | Overall problems
|
Hyperactivity/inattention problems
|
Emotional problemsa
|
|||
|---|---|---|---|---|---|---|---|---|
| borderline/clinical range | clinical range | borderline/clinical range | clinical range | borderline/clinical range | clinical range | |||
|
|
|
|
||||||
| Netherlands | SDQ | 2,420 | 3.2 (77) | 1.5 (36) | 7.9 (192) | 4.4 (107) | 4.0 (97) | 2.1 (50) |
| Denmark | SDQ | 50,039 | 6.3 (3,141) | 3.0 (1,511) | 8.6 (4,312) | 5.1 (2,555) | 13.9 (6,945) | 7.4 (3,706) |
| Spain | SDQ | 1,205 | 16.9 (204) | 8.5 (103) | 25.1 (302) | 15.5 (187) | 18.3 (220) | 9.9 (119) |
| Norway | CBCLb | 29,720 | 7.0 (2,080) | 2. 0 (594) | 7.0 (2,080) | 2. 0 (594) | 7.0 (1,136) | 2.0 (324) |
| Korea | CBCL | 500 | 8.0 (40) | 3.6 (18) | 7.2 (36) | 2.0 (10) | 9.6 (48) | 1.8 (9) |
|
|
|
|
||||||
| Total | 6.6 (5,542) | 2.7 (2,262) | 8.3 (6,922) | 4.1 (3,453) | 12.0 (8,446) | 6.0 (4,208) | ||
Abbreviations: CBCL, child behavior checklist; SDQ, strength and difficulties questionnaire.
Norway cohort collected this subscale only for subset of n=16,229.
Norway cohort administered adapted version of CBCL
Overall, 38.8% of mothers reported no cell phone use during pregnancy (Table 2). This was largely driven by 30,419 mothers in the Danish cohort reporting no cell phone use (60.8%), due to recruitment period that started prior to ubiquitous use of cell phones. Other use categories were classified as low or medium frequency cell phone users during pregnancy with 28.7% of mothers classified as low and 26.8% classified as medium. The remaining 5.7% of mothers were classified as high frequency cell phone users.
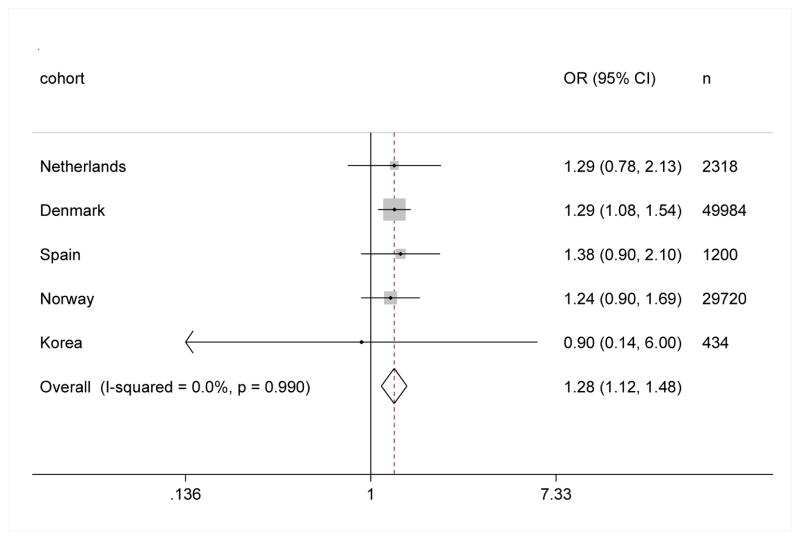
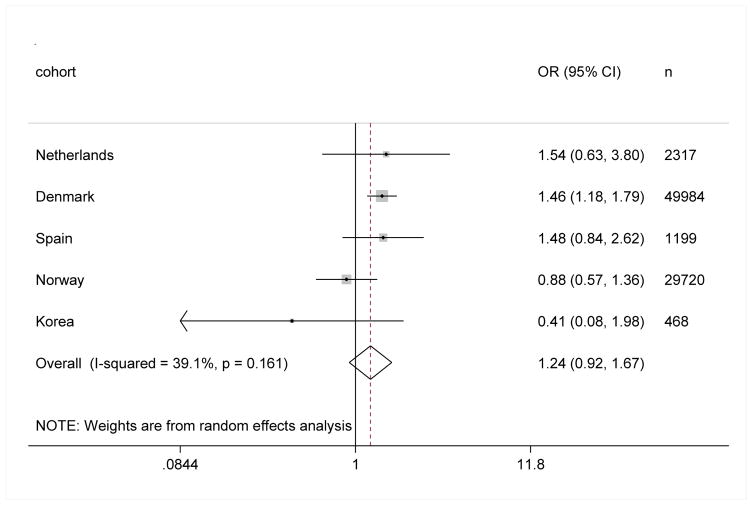
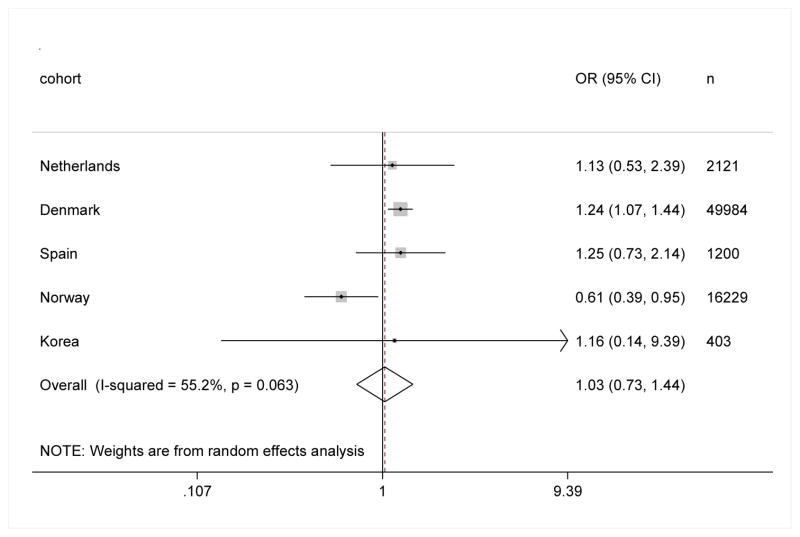
For overall behavioral problems, hyperactivity/inattention problems, and emotional problems within the borderline/clinical range and clinical range, non-users were at a lower risk than low cell phone users (OR 0.76 95%CI 0.68, 0.87 for overall behavioral problems within the clinical range) (Table 4). For hyperactivity/inattention problems within the borderline/clinical and clinical ranges, mothers who were medium or high cell phone users during pregnancy were at higher risk compared to low cell phone users (medium users: OR 1.07 95%CI 1.00, 1.14 and OR 1.11 95%CI 1.01, 1.22; high users: OR1.24 95%CI 1.12, 1.37 and OR 1.28 95%CI 1.12, 1.48 for hyperactivity/inattention problems in the borderline/clinical and clinical ranges, respectively) (Table 4, QFigure 1). This resulted in trends of increasing risk for hyperactivity/inattention problems through the cell phone categories (p for trend <0.001 for problems within borderline/clinical and clinical ranges, Supplemental Table S5). For overall behavioral problems this comparison of risk between high and low users did not reach statistical significance (OR 1.24 95%CI 0.92, 1.67 for overall behavioral problems within clinical range) (Table 4, Figure 2) nor did the trend (Supplemental Table S5). For emotional problems, high cell phone users were at an increased risk in DNBC, but a decreased risk in Norway (Figure 3), giving rise to heterogeneity between cohorts (Cochran’s test p<0.05 and/or I2≥25%) and no increase in the risk of these problems in the meta-analysis result (Table 4, Figure 3). None of the other heterogeneous associations were statistically significant. For forest plots not shown here, please see supplemental figures for all other fully adjusted associations (Supplemental Figures 1–15).
Table 4.
Meta-analyses of maternal cell phone use during pregnancy and associations with behavioral problems in children ages 5–7 in five cohorts
| Behavioral problems | Frequency of maternal cell phone use during pregnancy | cases | OR (95%CI) for problems within the borderline/clinical range | cases | OR (95%CI) for problems within the clinical range | ||
|---|---|---|---|---|---|---|---|
|
|
|
|
|||||
| minimally adjusteda | fully adjustedb | minimally adjusteda | fully adjustedb | ||||
| Overall problems | None | 1,690 | 0.77 (0.70, 0.83) | 0.82 (0.75, 0.89) | 755 | 0.78 (0.58, 1.05) c | 0.76 (0.68, 0.87) |
| Low | 1,621 | ref | ref | 628 | ref | ref | |
| medium | 1,726 | 1.02 (0.82, 1.28) c | 1.03 (0.91, 1.16) c | 632 | 1.17 (0.94, 1.45) c | 1.07 (0.95, 1.21) | |
| High | 436 | 1.09 (0.75, 1.60) c | 1.10 (0.81, 1.50) c | 203 | 1.25 (0.86, 1.82) c | 1.24 (0.92, 1.67) c | |
| Hyperactivity/inattention problems | None | 2,495 | 0.83 (0.78, 0.89) | 0.87 (0.81, 0.93) | 1,407 | 0.82 (0.75, 0.90) | 0.87 (0.79, 0.96) |
| Low | 2,252 | ref | ref | 993 | ref | ref | |
| medium | 2,425 | 1.11 (1.00, 1.23) c | 1.07 (1.00, 1.14) | 992 | 1.19 (1.09, 1.31) | 1.11 (1.01, 1.22) | |
| High | 604 | 1.31 (1.18, 1.44) | 1.24 (1.12, 1.37) | 317 | 1.39 (1.21, 1.59) | 1.28 (1.12, 1.48) | |
| Emotional problems | None | 3,893 | 0.81 (0.76, 0.86) | 0.89 (0.84, 0.95) | 1,980 | 0.87 (0.62, 1.21) c | 0.84 (0.78, 0.92) |
| low | 2,411 | ref | ref | 1,165 | ref | ref | |
| medium | 2,304 | 1.04 (0.93, 1.16) c | 1.00 (0.90, 1.11) c | 984 | 1.07 (0.98, 1.18) | 1.01 (0.92, 1.10) | |
| high | 621 | 0.99 (0.81, 1.22) c | 1.00 (0.84, 1.19) c | 331 | 1.02 (0.70, 1.47) c | 1.03 (0.73, 1.44) c | |
Models adjusted for age of child at behavior assessment
Models adjusted for age of child at behavior assessment, region (where applicable) and the following maternal characteristics: age at birth, parity, country of origin (where applicable), marital status during pregnancy, education, history of psychopathology, smoking during pregnancy, secondhand smoking during pregnancy, alcohol consumption during pregnancy, pre-pregnancy BMI, and height. Missing covariates have been imputed.
Heterogeneity existed among cohorts (Cochran’s Q test p<0.05 and/or I2≥25%), weights are from random effects analysis.
Abbreviations: CI, confidence interval; OR, odds ratio; ref, reference category.
Figure 1.
Meta-analysis of high frequency maternal cell phone use during pregnancy and risk for hyperactivity/inattention problems within the clinical range in children ages 5–7, as compared to low frequency maternal cell phone use.
Figure 2.
Meta-analysis of high frequency maternal cell phone use during pregnancy and risk for overall behavioral problems within the clinical range in children ages 5–7, as compared to low frequency maternal cell phone use.
Figure 3.
Meta-analysis of high frequency maternal cell phone use during pregnancy and risk for emotional problems within the clinical range in children ages 5–7, as compared to low frequency maternal cell phone use.
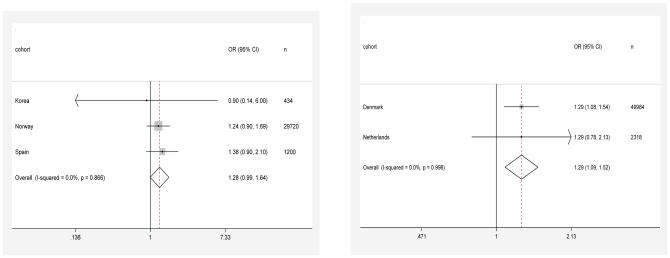
Sensitivity analysis revealed that when excluding Denmark (the largest cohort with the largest proportion of non-users) from the main analysis, the reduced effect estimate remained among mothers who reported no cell phone use during pregnancy but lost statistical significance; while ORs remained significant for hyperactivity/inattention problems in the borderline/clinical and clinical ranges among children of high users (Supplemental Table S6). When excluding the Norwegian cohort, ORs became statistically significant for overall clinical behavioral problems and emotional clinical problems among high users and heterogeneity disappeared. Children of very high cell phone users (10 or more calls/day in cohorts the Netherlands, Spain, and 11 or more calls/day in Korea, where this data was available) had the highest risk for both overall and hyperactivity/inattention problems (ORs ranging from 1.30 to 1.73), but the estimates were not statistically significant (Supplemental Table S7). Comparing no cell phone use to any cell phone use during pregnancy, we found a statistically significant risk for overall behavioral problems, hyperactivity/inattention problems, and emotional problems; but after excluding Denmark, this risk only remained statistically significant for hyperactivity/inattention problems (Supplemental Table S8). In sensitivity analysis stratified by timing of maternal cell phone use data collection (prospectively vs retrospectively), prospectively collected data had fewer statistically significant results (Figures 4A & 4B, Supplemental Table S9).
Figure 4.
Figure 4A: Meta-analysis of high frequency maternal cell phone use during pregnancy and risk for hyperactivity problems within the clinical range in children ages 5–7, as compared to low frequency maternal cell phone use in cohorts where cell phone data was collected prospectively.
Figure 4B: Meta-analysis of high frequency maternal cell phone use during pregnancy and risk for hyperactivity problems within the clinical range in children ages 5–7, as compared to low frequency maternal cell phone use in cohorts where cell phone data was collected retrospectively.
In analysis of cordless phone use in the Dutch cohort, we found children of mothers who were high cell phone users or high cordless phone users had similar cohort specific risks for hyperactivity/inattention problems. Children of mothers who did not use cordless phones had high risks for all outcomes (Supplemental Table S10). In analyses of risk for hyperactivity/inattention problems in the Spanish cohort as assessed by the ADHD-DSM-IV tool, risks among high cell phone users were consistent with cohort specific results regarding risk for hyperactivity/inattention as scored by the SDQ (Supplemental Table S11). In analyses of children born 1996–2004 and those born 2005–2011, risk for hyperactivity/inattention problems was slightly diminished among children born later (2005–2011). However the reduced risk for overall or hyperactivity/inattention problems among children of non-users was persistent during both time periods (Supplemental Table S12). For a summary of sensitivity analysis results regarding hyperactivity/inattention problems in the clinical range, see Table 5.
Table 5.
Summary of sensitivity analyses for risk of hyperactivity/inattention problems in the clinical range for children among mothers who were high cell phone users during pregnancy compared to low usersa
| Analysis | Number of cases with high cell phone useb | Fully adjusted OR (95% CI) among high cell phone usersb |
|---|---|---|
| All cohorts - main analysis | 317 | 1.28 (1.12, 1.48) |
| Excluding one cohort at a time: | ||
| Excluding Netherlands | 286 | 1.28 (1.11, 1.48) |
| Excluding Denmark | 130 | 1.28 (1.02, 1.60) |
| Excluding Spain | 269 | 1.27 (1.10, 1.48) |
| Excluding Norway | 269 | 1.30 (1.11, 1.51) |
| Excluding Korea | 314 | 1.29 (1.12, 1.48) |
| By timing of cell phone use data collection: | ||
| Prospective (Spain, Norway, Korea) | 99 | 1.28 (0.99, 1.64) |
| Retrospective (Netherlands, Denmark) | 218 | 1.29 (1.09, 1.52) |
| By years of birth: | ||
| 1996–2004 (Netherlands, Denmark, part Spain, part Norway) | 234 | 1.34 (1.14, 1.57) |
| 2005–2011 (part Spain, part Norway, Korea) | 83 | 1.17 (0.88, 1.54) |
| Very high cell phone use versus low cell phone use (Netherlands, Spain, and Korea) | 78 | 1.55 (0.94, 2.56) |
| Any cell phone use versus no cell phone use | 2,302 | 1.24 (1.14, 1.34) |
All models adjusted for age of child at behavioral assessment, region (where applicable) and the following maternal characteristics: age at birth, parity, country of birth (where applicable), marital status during pregnancy, education, history of psychopathology, smoking during pregnancy, secondhand smoking during pregnancy, alcohol consumption during pregnancy, pre-pregnancy BMI, and height. Missing covariates have been imputed.
Except in the analyses of very high cell phone use versus low cell phone use and any cell phone use versus no cell phone use.
4. DISCUSSION
In this meta-analysis of individual participant data among five birth cohorts, children whose mothers did not use cell phones during pregnancy had a lower risk of overall behavioral problems, hyperactivity/inattention problems, and emotional problems. Increased use of cell phones during pregnancy was associated with increased risk for hyperactivity/inattention problems in offspring. The association for hyperactivity/inattention problems was fairly consistent across cohorts and was observed both in cohorts with retrospective assessment of cell phone use and in those with prospective assessment.
The increased risks observed in cell phone users compared to non-users are in line with previous studies published using data from the Danish and Dutch cohorts (Divan et al., 2012, 2008; Guxens et al., 2013; Sudan et al., 2016), though results from the previous Dutch study were not statistically significant. In our study, the group of pregnant women who did not use cell phones during pregnancy largely consisted of mothers from Denmark (93% of non-users). This makes sense, as the Danish cohort is the oldest, beginning enrollment in 1996 and ending in 2002, before cell phones were as ubiquitous as they are today. During those years, cell phone users in Denmark were more likely to be younger and have less education, while in later cohorts this trend was reversed (Supplemental Table S13). In sensitivity analyses without Denmark, cell phone users were still at an increased risk at a similar magnitude for overall problems and hyperactivity/inattention problems in children, but statistical significance was only maintained among high users. In a previous publication from the Danish cohort, authors explored the possibility that cell phone use was indicative of a mother’s inattention to the child and used proxy measures (breastfeeding, hours per day spent with child, hours per day that child spent in daycare) to capture attentiveness, but accounting for these factors did not diminish associations between prenatal cell phone use and behavioral problems (Divan et al., 2012). It has also been proposed that recall bias in the mother could influence this association, but in our sensitivity analysis the increased risk among cell phone users was still present at a similar magnitude, though borderline statistically significant, for overall problems and hyperactivity/inattention problems in cohorts where cell phone use data was collected prospectively (at time of pregnancy).
Pregnant women who were medium and high frequency cell phone users during pregnancy were more likely to have a child with hyperactivity/inattention problems within both borderline/clinical and clinical ranges. In a 2008 study with Danish data, an increase in risk for hyperactivity was also found among mothers who used cell phones ever during pregnancy (Divan et al., 2008). In Guxens et al.’s analysis of the Dutch cohort, the main analysis reported no associations with hyperactivity/inattention problems, but supplemental materials showed an increased risk for hyperactivity/inattention problems within the borderline/clinical range among prenatal cell phone users making five or more calls per day, without statistical significance (Guxens et al., 2013). Similarity of results for hyperactivity/inattention problems across cohorts with retrospective and prospective data collection indicates that biased recall of cell phone use is an unlikely explanation of the association, though the association in cohorts with prospective data collection was borderline statistically significant. Further, this association was hardly influenced by the one-by-one exclusion of cohorts (ORs for clinical hyperactivity/inattention problems ranging between 1.27 and 1.30), indicating that cohort-specific biases are unlikely to explain the overall result. In the Spanish cohort, prevalences of hyperactivity/inattention problems within borderline/clinical and clinical ranges were particularly high. Past studies evaluating SDQ scores in Spanish children have shown similar results (Marzocchi et al., 2004, 2011), and found that cross-national differences in SDQ scores do not actually reflect differences in rates of disorders (Goodman et al., 2012). However, sensitivity analysis revealed that even when hyperactivity/inattention was assessed more strictly using the ADHD-DSM-IV administered by teachers, borderline/clinical and clinical prevalences were cut in half but cohort specific associations with high cell phone use remained the same.
The interpretation of our results is as yet unclear, mainly due to the small RF-EMF exposure expected to reach the fetus from maternal cell phone use and to the potential presence of residual confounding. Firstly, specific absorption rate (SAR) models indicate that RF-EMF from the mother holding the cell phone to her head or near the body would only result in very low SAR levels to reach the fetus (below the basic restriction of 0.08 W kg−1)(Varsier et al., 2014); and these SAR models vary depending on pregnancy stage and position of the fetus, relying on many assumptions and extrapolations (Dimbylow, 2007; Dimbylow et al., 2009; Varsier et al., 2014). Also, RF-EMF exposure to the fetus could depend on where the mother carries her cell phone (Sudan et al., 2016), data which was not available for this analysis. Secondly, RF-EMF is also emitted from cordless phones, therefore it has been argued that similar associations should be seen in children of high cordless phone users if the association were due to RF-EMF exposure in the mother (Guxens et al., 2013; Swerdlow, 2012). However, it should be noted that 1) cordless phone users also use cell phones; 2) RF-EMF emitted from cordless phones is comparable to that from third generation (3G) phones, but lower than that emitted from second generation (2G) phones (Cardis et al., 2011; Schüz et al., 2006), which were used by the vast majority of pregnant women in this study (pregnancies through 2008, (Cardis et al., 2011)); and 3) cordless phone use habits should be expected to differ from cell phone use habits, such as longer duration of calls, possibly resulting in higher overall exposure per call. Therefore comparisons of cell phone use with cordless phone use should be approached with caution. Nevertheless, sensitivity analysis in the Dutch cohort revealed similar cohort specific coefficients for hyperactivity/inattention problems among children of high prenatal cordless phone users. Curiously, children of mothers who did not use cordless phones saw the same increased risk for hyperactivity/inattention problems and very high risk for overall behavioral problems. We cannot explain this finding, but we should note that 25% of non-cordless phone users included high cell phone users, again cautioning the interpretation of this sensitivity analysis. Furthermore, researchers in the Danish cohort found evidence that childhood (postnatal) cell phone use is linked to behavioral problems, but more so for older children (11 years) and less for the age group in our study (5–7 years) (Sudan et al., 2016). Indeed, very few children in this age group use phones, with recent data showing less than 10% of children with cell phone ownership at age 7 (GSM Association et al., 2015). Therefore, childhood cell phone use was not used in our models. Finally, there is concern that over time both cell phone use and prevalence of child behavioral problems have increased (Sudan et al., 2013), introducing a bias in our results. In fact, the sensitivity analysis of children born earlier (1996–2004) versus later (2005–2011) found that the reduced risk for overall behavioral and hyperactivity/inattention problems among children of non-users was consistent during both time periods, while increased risk for hyperactivity/inattention problems for children of high users was slightly diminished in later years. We suspect that this is due to a dilution of our exposure assessment, since in more recent years, exposure to other sources of RF-EMF such as nearby cell phone users, wifi networks, or newly constructed cell phone base stations, would be more likely. Confounding by various unmeasured factors could explain our findings. The factors linked to maternal cell phone use (pre and postnatally) and behavioral problems in the child are numerous and complex. One important aspect, parenting style, could account for some of these factors, capturing parental responsiveness and demandingness through a four category typology: indulgent, authoritarian, authoritative, or uninvolved (Maccoby and Martin, 1983). While research shows parenting styles to be related with various outcomes in the child, including behavioral problems (Baumrind, 1991), studies have yet to demonstrate their associations with maternal cell phone use, though it is not difficult to imagine a correlation. Unfortunately, neither parenting styles nor postnatal maternal cell phone were collected in any cohorts in this study. This type of uncontrolled confounding may explain the similar decreases in risk observed among non-users compared to any users for overall, emotional, and hyperactivity/inattention problems. In the Danish cohort, they have previously performed a sibling analysis to account for unmeasured in-family confounding in the associations between maternal cell phone use and child behavior problems, but found it hard to isolate the influence of rapidly changing cell phone use from birth order and time period effects; they concluded that in-family confounding could not fully explain associations (Sudan et al., 2014). Also, in our analysis of non-users, the reduced risk hardly varies from unadjusted to fully adjusted models, suggesting that confounding may not fully explain these findings. Regarding the persistent increased risks for hyperactivity/inattention problems among children of cell phone users in our analysis, it is possible that mothers with adult hyperactivity/inattention problems were more likely to make more cell phone calls or cordless phone calls and also passed hyperactivity/inattention problems to their child through genetics, as hyperactivity/inattention problems are some of the most heritable psychiatric traits (Faraone and Mick, 2010). While cohorts in this analysis have accounted for history of psychopathology in the mother as possible confounders, adult hyperactivity/inattention is largely untreated or undiagnosed (Asherson et al., 2016; Faraone SV et al., 2004) and thus mostly unaccounted for in these prospective cohorts. Furthermore, associations in our unadjusted models for hyperactivity/inattention problems slightly varied from adjusted models, indicating the influence of uncontrolled confounding. This is also demonstrated in Supplemental Table S13, showing the strong correlations between covariates and cell phone use. It should be noted that maternal history of psychopathogy was assessed differently at different times in each cohort. Even so, prevalences of maternal psychopathology were more or less comparable for four cohorts, but not in the case of the Dutch. The Dutch cohort’s method of collecting this information may have been the most exhaustive, asking the mother if she had ever/never had nine disorders. Despite this, we can assume an over-estimation of maternal psychological disorders in the Netherlands would bias towards a null effect in our associations of interest. Overall, to improve our interpretation of observed associations between prenatal cell phone use and behavioral problems, further studies would need to include postnatal cell phone use, adjust for parenting styles, possible other social and behavioral determinants of cell phone use, and maternal hyperactivity/inattention problems.
We observed no statistically significant increased risk for overall or emotional problems in children of mothers who used cell phones at medium or high frequencies as compared to low frequency users, but there was heterogeneity among cohorts. One of the previous studies in the Danish cohort reported a small increased risk for emotional problems among children of cell phone users (Divan et al., 2008) while the previous Dutch study found no associations (Guxens et al., 2013). In our study, risks in the Danish and other cohorts were negated by the Norwegian cohort where mothers who used cell phones were less likely to have children with emotional problems. This heterogeneity could be due to confounding factors related to hyperactivity/inattention problems but not related to emotional problems. Upon exclusion of Norway from meta-analyses, our main results remained intact, but statistically significant risks emerged for overall clinical behavioral problems, and clinical emotional problems among high frequency users.
Our study has some important strengths, including its large sample size and the harmonized and detailed information regarding individual maternal characteristics, enabling adjustment across cohorts for possible confounders collected prospectively, protecting from recall bias. Furthermore, this is the first study on this association to include cohorts that collected cell phone use prospectively.
Our study has several limitations. While the cell phone use frequency categorizations we used were useful for combining these five cohorts, it was not precise in categorizing number of calls made per day by the mother during pregnancy. Still, studies have shown that cell phone users are not exact estimators of use (Shum et al., 2011; Vrijheid et al., 2006), therefore we felt that classifying mothers in different exposure groups from no use to high use within each cohort would better capture the variability of cell phone use specific to that cohort. It should be noted that for three of the cohorts, our exposure categories referred to the same number of calls in the Netherlands, Denmark, and Spain. It was only for Norway and Korea that the frequency categories differed in exact number of calls. Norway’s classification of high cell phone users was difficult to compare with other cohorts. While all other cohorts’ high users were classified by frequency of calls, Norway’s high users were classified by duration of calls (“more than an hour a day”), which was quite restrictive. Only 5% of Norwegian mothers reported high use, versus 20–30% in other cohorts (the Netherlands, Spain, and Korea) where women were pregnant during the same technology era (2004–2008). In excluding Norway and Korea from analyses (also the only cohorts not using the SDQ to evaluate outcomes), associations were statistically significant or borderline significant for all outcomes among high frequency users. Misclassification of calls, due to errors in self-reports or due to our imperfect categorization, would most likely have resulted in an attenuation of associations and is unlikely to explain the associations we observed (Blair et al., 2007). Even if we assumed errors in self-reports, we believe the difference of calls per day between low and high users is considerable. In Denmark, the Netherlands, and Spain low users made 0–1 calls per day, as compared to high users making 4 or more calls per day. In Norway low users (a few times a week) were compared to high users (more than an hour a day) and in Korea, low users were making 1–2 calls/day and high users were making 6 or more calls/day. In the Netherlands, Spain, and Korea analysis of very high cell phone use in mothers during pregnancy compared to low use showed that children of these very high users were at the highest risk for all behavioral problems (overall, hyperactivity/inattention, and emotional). These associations had wide confidence intervals, perhaps due to small number of cases included in this sensitivity analysis, but this increased risk among children of very high users provides further evidence for this association with the added strength that the exposure groups were even less likely to overlap.
While our outcome assessments varied across cohorts, various studies have shown the SDQ and CBCL overall scales and subscales to be comparable (Goodman and Scott, 1999; Klasen et al., 2000; Koskelainen et al., 2000). However, ours would be the first study to use Norway’s adapted CBCL scores with the SDQ and complete CBCL, presenting an important limitation in our study and possible explanation for the inconsistency between Norway and other cohorts for risks for overall behavioral problems and emotional problems. Even so, prevalences of borderline/clinical and clinical scores were very similar between Norway and Korea, suggesting Norway’s adapted format would not be the reason for this inconsistency in associations. Furthermore, the SDQ and CBCL are valuable screening tools used internationally for pediatric behavioral issues but are not a substitute for diagnosis by a physician, which would be the most reliable, but perhaps under diagnosed measure of behavioral outcomes (Stone et al., 2010).
5. CONCLUSIONS
Maternal cell phone use during pregnancy may be associated with an increased risk of behavioral problems, particularly hyperactivity/inattention problems, in the offspring. This is the largest study to date to evaluate these associations and to show mostly consistent results across cohorts with retrospectively and prospectively assessed maternal cell phone use. Still, the interpretation of these results is unclear and should take into consideration that uncontrolled confounding by social factors or maternal hyperactivity may influence both maternal cell phone use and child behavioral problems.
Supplementary Material
Highlights.
Largest study to date to use prenatal cell phone use data collected prospectively
High prenatal cell phone use linked to hyperactivity/inattention problems in child
No prenatal cell phone use linked to low risk for any behavioral problems in child
Analysis adjusted for many confounders, but associations cannot be judged causal
Future research should adjust for parenting style, maternal hyperactivity, and more
Acknowledgments
Funding sources:
GERoNiMO project: This work is supported by the European Union (grant 603794).
ABCD, The Netherlands: This work was supported by the Netherlands Organization for Health Research and Development (grant 2100.0076) and within the programme Electromagnetic Fields and Health Research (grants 85600004 and 85800001)
DNBC, Denmark: This work was supported by the Danish Epidemiology Science Centre; The Lundbeck Foundation; Egmont Foundation; March of Dimes Birth Defect Foundation; Agustinus Foundation; and the Medical Research Council.
INMA, Spain: This work was supported by the European Union (grants FP7-ENV-2011, 282957, HEALTH.2010.2.4.5-1); Instituto de Salud Carlos III (grants G03/176, CB06/02/0041, FIS-FEDER 03/1615, 04/1509, 04/1112, 04/1931, 05/1079, 05/1052, 06/1213, 07/0314, 09/02647, 11/01007, 11/02591, CP11/00178, FIS-PI06/0867, FIS-PS09/00090, FIS-PI041436, FIS-PI081151, FIS-PI042018, FIS-PI09/02311, FIS-PI13/1944, FIS-PI13/2429, FIS-PI14/0981, FIS-PI13/141687, CP13/00054 incl. FEDER funds, and MS13/00054); Conselleria de Sanitat Generalitat Valenciana; Generalitat de Catalunya (grants CIRIT1999SGR, 00241); Obra Social Cajastur; Universidad de Oviedo; Department of Health of the Basque Government (grants 2005111093112009111069); and the Provincial Government of Gipuzkoa (grants DFG06/004, DFG08/001).
MoBa, Norway: This work was supported by the Norwegian Ministry of Health; National Institutes of Health; National Institute of Environmental Health Sciences (grant N01-ES–85433); National Institute of Neurological Disorders and Stroke (grant 1 UO1 NS 047537); Norwegian Research Council; and Functional Genomics (grant 151918/S10).
MOCEH, Korea: This work was supported by the National Institute of Environmental Research and Korean Ministry of Environment and IT R&D program of MSIP/IITP. [B0138-16-1002, Study on the EMF exposure control in smart society]
The authors would particularly like to thank all participants for their generous collaboration.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Achenbach TM. Child Behavior Checklist. In: Kreutzer JS, DeLuca J, Caplan B, editors. Encyclopedia of Clinical Neuropsychology. Springer; New York: 2011. pp. 546–552. [Google Scholar]
- Aldad TS, Gan G, Gao XB, Taylor HS. Fetal radiofrequency radiation exposure from 800–1900 mhz-rated cellular telephones affects neurodevelopment and behavior in mice. Sci Rep. 2012;2:312. doi: 10.1038/srep00312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Academy of Pediatrics. Diagnostic And Statistical Manual Of Mental Disorders DSM-IV-TR Fourth Edition. Amer Psychiatric Pub; Washington, D.C: 2004. [Google Scholar]
- Asherson P, Buitelaar J, Faraone SV, Rohde LA. Adult attention-deficit hyperactivity disorder: key conceptual issues. Lancet Psychiatry. 2016;3:568–578. doi: 10.1016/S2215-0366(16)30032-3. [DOI] [PubMed] [Google Scholar]
- Baumrind D. The Influence of Parenting Style on Adolescent Competence and Substance Use. J Early Adolesc. 1991;11:56–95. doi: 10.1177/0272431691111004. [DOI] [Google Scholar]
- Blair A, Stewart P, Lubin JH, Forastiere F. Methodological issues regarding confounding and exposure misclassification in epidemiological studies of occupational exposures. Am J Ind Med. 2007;50:199–207. doi: 10.1002/ajim.20281. [DOI] [PubMed] [Google Scholar]
- Cardis E, Varsier N, Bowman JD, Deltour I, Figuerola J, Mann S, Moissonnier M, Taki M, Vecchia P, Villegas R, Vrijheid M, Wake K, Wiart J. Estimation of RF energy absorbed in the brain from mobile phones in the Interphone Study. Occup Environ Med. 2011;68:686–693. doi: 10.1136/oemed-2011-100065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimbylow P. SAR in the mother and foetus for RF plane wave irradiation. Phys Med Biol. 2007;52:3791–3802. doi: 10.1088/0031-9155/52/13/009. [DOI] [PubMed] [Google Scholar]
- Dimbylow PJ, Nagaoka T, Xu XG. A comparison of foetal SAR in three sets of pregnant female models. Phys Med Biol. 2009;54:2755–2767. doi: 10.1088/0031-9155/54/9/011. [DOI] [PubMed] [Google Scholar]
- Divan HA, Kheifets L, Obel C, Olsen J. Cell phone use and behavioural problems in young children. J Epidemiol Community Health. 2012;66:524–529. doi: 10.1136/jech.2010.115402. [DOI] [PubMed] [Google Scholar]
- Divan HA, Kheifets L, Obel C, Olsen J. Prenatal and postnatal exposure to cell phone use and behavioral problems in children. Epidemiol Camb Mass. 2008;19:523–529. doi: 10.1097/EDE.0b013e318175dd47. [DOI] [PubMed] [Google Scholar]
- van Eijsden M, Vrijkotte TG, Gemke RJ, van der Wal MF. Cohort Profile: The Amsterdam Born Children and their Development (ABCD) Study. Int J Epidemiol. 2011;40:1176–1186. doi: 10.1093/ije/dyq128. [DOI] [PubMed] [Google Scholar]
- Faraone SV, Mick E. Molecular Genetics of Attention Deficit Hyperactivity Disorder. Psychiatr Clin North Am, Psychiatric Genetics. 2010;33:159–180. doi: 10.1016/j.psc.2009.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faraone SV, Spencer TJ, Montano C, Biederman J. Attention-deficit/hyperactivity disorder in adults: A survey of current practice in psychiatry and primary care. Arch Intern Med. 2004;164:1221–1226. doi: 10.1001/archinte.164.11.1221. [DOI] [PubMed] [Google Scholar]
- Garthus-Niegel S, Hagtvet KA, Vollrath ME. A prospective study of weight development and behavior problems in toddlers: the Norwegian Mother and Child Cohort Study. BMC Public Health. 2010;10:626. doi: 10.1186/1471-2458-10-626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GERoNiMO [WWW Document] Gen EMF Res Using Nov Methods. 2014 http://crealradiation.com/index.php/en/project-description/geronimo-projectdescription.
- Goodman A, Heiervang E, Fleitlich-Bilyk B, Alyahri A, Patel V, Mullick MSI, Slobodskaya H, Dos Santos DN, Goodman R. Cross-national differences in questionnaires do not necessarily reflect comparable differences in disorder prevalence. Soc Psychiatry Psychiatr Epidemiol. 2012;47:1321–1331. doi: 10.1007/s00127-011-0440-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman R. The Strengths and Difficulties Questionnaire: A Research Note. J Child Psychol Psychiatry. 1997;38:581–586. doi: 10.1111/j.1469-7610.1997.tb01545.x. [DOI] [PubMed] [Google Scholar]
- Goodman R, Scott S. Comparing the Strengths and Difficulties Questionnaire and the Child Behavior Checklist: is small beautiful? J Abnorm Child Psychol. 1999;27:17–24. doi: 10.1023/a:1022658222914. [DOI] [PubMed] [Google Scholar]
- Graham JW, Olchowski AE, Gilreath TD. How Many Imputations are Really Needed? Some Practical Clarifications of Multiple Imputation Theory. Prev Sci. 2007;8:206–213. doi: 10.1007/s11121-007-0070-9. [DOI] [PubMed] [Google Scholar]
- GSM Association, Mobile Society Research, Institute within NTT DOCOMO, Inc. Japan. Children’s Use of Mobile Phones - GSMA. 2015. [Google Scholar]
- Guxens M, Ballester F, Espada M, Fernández MF, Grimalt JO, Ibarluzea J, Olea N, Rebagliato M, Tardón A, Torrent M, Vioque J, Vrijheid M, Sunyer J. Cohort Profile: The INMA—INfancia y Medio Ambiente—(Environment and Childhood) Project. Int J Epidemiol. 2012;41:930–940. doi: 10.1093/ije/dyr054. [DOI] [PubMed] [Google Scholar]
- Guxens M, Eijsden M, van Vermeulen R, Loomans E, Vrijkotte TGM, Komhout H, Strien RT, van Huss A. Maternal cell phone and cordless phone use during pregnancy and behaviour problems in 5-year-old children. J Epidemiol Community Health jech–2012–201792. 2013 doi: 10.1136/jech-2012-201792. [DOI] [PubMed] [Google Scholar]
- Haghani M, Shabani M, Moazzami K. Maternal mobile phone exposure adversely affects the electrophysiological properties of Purkinje neurons in rat offspring. Neuroscience. 2013;250:588–598. doi: 10.1016/j.neuroscience.2013.07.049. [DOI] [PubMed] [Google Scholar]
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kheifets L, Repacholi M, Saunders R, van Deventer E. The Sensitivity of Children to Electromagnetic Fields. Pediatrics. 2005;116:e303–e313. doi: 10.1542/peds.2004-2541. [DOI] [PubMed] [Google Scholar]
- Kim BM, Ha M, Park HS, Lee BE, Kim YJ, Hong YC, Kim Y, Chang N, Roh YM, Kim BN, Oh S, Ha EH MOCEH Study Group. The Mothers and Children’s Environmental Health (MOCEH) study. Eur J Epidemiol. 2009;24:573–583. doi: 10.1007/s10654-009-9370-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klasen H, Woerner W, Wolke D, Meyer R, Overmeyer S, Kaschnitz W, Rothenberger A, Goodman R. Comparing the German versions of the Strengths and Difficulties Questionnaire (SDQ-Deu) and the Child Behavior Checklist. Eur Child Adolesc Psychiatry. 2000;9:271–276. doi: 10.1007/s007870070030. [DOI] [PubMed] [Google Scholar]
- Koskelainen M, Sourander A, Kaljonen A. The Strengths and Difficulties Questionnaire among Finnish school-aged children and adolescents. Eur Child Adolesc Psychiatry. 2000;9:277–284. doi: 10.1007/s007870070031. [DOI] [PubMed] [Google Scholar]
- Kostoff RN, Lau CGY. Combined biological and health effects of electromagnetic fields and other agents in the published literature. Technol Forecast Soc Change. 2013;80:1331–1349. doi: 10.1016/j.techfore.2012.12.006. [DOI] [Google Scholar]
- Leung S, Croft RJ, McKenzie RJ, Iskra S, Silber B, Cooper NR, O’Neill B, Cropley V, Diaz-Trujillo A, Hamblin D, Simpson D. Effects of 2G and 3G mobile phones on performance and electrophysiology in adolescents, young adults and older adults. Clin Neurophysiol Off J Int Fed Clin Neurophysiol. 2011;122:2203–2216. doi: 10.1016/j.clinph.2011.04.006. [DOI] [PubMed] [Google Scholar]
- Maccoby EE, Martin JA. Socialization in the context of the family: parent-child interaction. In: Mussen Paul H., editor. Handb Child Psychol Former Carmichaels Man Child Psychol. 1983. [Google Scholar]
- Magnus P, Irgens LM, Haug K, Nystad W, Skjærven R, Stoltenberg C, Group TMS. Cohort profile: The Norwegian Mother and Child Cohort Study (MoBa) Int J Epidemiol. 2006;35:1146–1150. doi: 10.1093/ije/dyl170. [DOI] [PubMed] [Google Scholar]
- Marzocchi GM, Capron C, Di Pietro M, Duran Tauleria E, Duyme M, Frigerio A, Gaspar MF, Hamilton H, Pithon G, Simões A, Thérond C. The use of the Strengths and Difficulties Questionnaire (SDQ) in Southern European countries. Eur Child Adolesc Psychiatry. 2004;13(Suppl 2):II40–46. doi: 10.1007/s00787-004-2007-1. [DOI] [PubMed] [Google Scholar]
- National Research Council. Identification of Research Needs Relating to Potential Biological or Adverse Health Effects of Wireless Communication. National Academies Press; Washington, D.C: 2008. [Google Scholar]
- Olsen J, Melbye M, Olsen SF, Sørensen TI, Aaby P, Andersen AM, Taxbøl D, Hansen KD, Juhl M, Schow TB, Sørensen HT, Andresen J, Mortensen EL, Olesen AW, Søndergaard C. The Danish National Birth Cohort--its background, structure and aim. Scand J Public Health. 2001;29:300–307. doi: 10.1177/14034948010290040201. [DOI] [PubMed] [Google Scholar]
- Schüz J, Böhler E, Berg G, Schlehofer B, Hettinger I, Schlaefer K, Wahrendorf J, Kunna-Grass K, Blettner M. Cellular Phones, Cordless Phones, and the Risks of Glioma and Meningioma (Interphone Study Group, Germany) Am J Epidemiol. 2006;163:512–520. doi: 10.1093/aje/kwj068. [DOI] [PubMed] [Google Scholar]
- Shirai T, Imai N, Wang J, Takahashi S, Kawabe M, Wake K, Kawai H, Watanabe SI, Furukawa F, Fujiwara O. Multigenerational effects of whole body exposure to 2.14 GHz W-CDMA cellular phone signals on brain function in rats. Bioelectromagnetics. 2014;35:497–511. doi: 10.1002/bem.21871. [DOI] [PubMed] [Google Scholar]
- Shum M, Kelsh MA, Sheppard AR, Zhao K. An evaluation of self-reported mobile phone use compared to billing records among a group of engineers and scientists. Bioelectromagnetics. 2011;32:37–48. doi: 10.1002/bem.20613. [DOI] [PubMed] [Google Scholar]
- Sterne JAC, White IR, Carlin JB, Spratt M, Royston P, Kenward MG, Wood AM, Carpenter JR. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ. 2009;338:b2393. doi: 10.1136/bmj.b2393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone LL, Otten R, Engels RCME, Vermulst AA, Janssens JMAM. Psychometric Properties of the Parent and Teacher Versions of the Strengths and Difficulties Questionnaire for 4- to 12-Year-Olds: A Review. Clin Child Fam Psychol Rev. 2010;13:254–274. doi: 10.1007/s10567-010-0071-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sudan M, Kheifets L, Arah OA, Olsen J. On the association of cell phone exposure with childhood behaviour. J Epidemiol Community Health jech–2013–202495. 2013 doi: 10.1136/jech-2013-202495. [DOI] [PubMed] [Google Scholar]
- Sudan M, Kheifets LI, Arah OA, Divan HA, Olsen J. Complexities of sibling analysis when exposures and outcomes change with time and birth order. J Expo Sci Environ Epidemiol. 2014;24:482–488. doi: 10.1038/jes.2013.56. [DOI] [PubMed] [Google Scholar]
- Sudan M, Olsen J, Arah OA, Obel C, Kheifets L. Prospective cohort analysis of cellphone use and emotional and behavioural difficulties in children. J Epidemiol Community Health jech–2016–207419. 2016 doi: 10.1136/jech-2016-207419. [DOI] [PubMed] [Google Scholar]
- Swerdlow A. Radiofrequency electromagnetic fields: health effects - Publications. 2012. [Google Scholar]
- Thompson SG, Sharp SJ. Explaining heterogeneity in meta-analysis: a comparison of methods. Stat Med. 1999;18:2693–2708. doi: 10.1002/(SICI)1097-0258(19991030)18:20<2693::AID-SIM235>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- Unitat d’Epidemiologia i de Diagnòstic en Psicopatologia del Desenvolupament. [accessed 7.14.16];Spanish norms for the Strength & Difficulties Questionnaire (SDQ) for 3 and 4-year-old schoolchildren: Parents’ and teachers’ versions [WWW Document] 2011 http://www.sdqinfo.com/norms/Spanish_norms_for_3-4_year-old.pdf.
- Van Deventer E, van Rongen E, Saunders R. WHO research agenda for radiofrequency fields. Bioelectromagnetics. 2011;32:417–421. doi: 10.1002/bem.20660. [DOI] [PubMed] [Google Scholar]
- Varsier N, Dahdouh S, Serrurier A, De la Plata JP, Anquez J, Angelini ED, Bloch I, Wiart J. Influence of pregnancy stage and fetus position on the whole-body and local exposure of the fetus to RF-EMF. Phys Med Biol. 2014;59:4913–4926. doi: 10.1088/0031-9155/59/17/4913. [DOI] [PubMed] [Google Scholar]
- Vrijheid M, Cardis E, Armstrong BK, Auvinen A, Berg G, Blaasaas KG, Brown J, Carroll M, Chetrit A, Christensen HC, Deltour I, Feychting M, Giles GG, Hepworth SJ, Hours M, Iavarone I, Johansen C, Klæboe L, Kurttio P, Lagorio S, Lönn S, McKinney PA, Montestrucq L, Parslow RC, Richardson L, Sadetzki S, Salminen T, Schüz J, Tynes T, Woodward A. Validation of short term recall of mobile phone use for the Interphone study. Occup Environ Med. 2006;63:237–243. doi: 10.1136/oem.2004.019281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Bank. Mobile Cellular Subscriptions (per 100 people) (World Development Indicators) The World Bank Group; 2014. [Google Scholar]
- World Health Organization. Electromagnetic Fields (EMF): Publications and Information Resources. 2002. Establishing a Dialogue on Risks From Electromagnetic Fields. [Google Scholar]
- Zhang Y, Li Z, Gao Y, Zhang C. Effects of fetal microwave radiation exposure on offspring behavior in mice. J Radiat Res (Tokyo) 2015;56:261–268. doi: 10.1093/jrr/rru097. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.