Abstract
Common mental disorders, including depression, anxiety, and posttraumatic stress, are leading causes of disability worldwide. Treatment for these disorders is limited in low- and middle-income countries. This systematic review synthesizes the implementation processes and examines the effectiveness of psychological treatments for common mental disorders in adults delivered by nonspecialist providers in low- and middle-income countries. In total, 27 trials met the eligibility criteria; most treatments targeted depression or posttraumatic stress. Treatments were commonly delivered by community health workers or peers in primary care or community settings; they usually were delivered with fewer than 10 sessions over 2–3 months in an individual, face-to-face format. Treatments included common elements, such as nonspecific engagement and specific domains of behavioral, interpersonal, emotional, and cognitive elements. The pooled effect size was 0.49 (95% confidence interval = 0.36–0.62), favoring intervention conditions. Our review demonstrates that psychological treatments—comprising a parsimonious set of common elements and delivered by a low-cost, widely available human resource—have moderate to strong effects in reducing the burden of common mental disorders.
Keywords: global mental health, psychological treatments, low- and middle-income countries, implementation processes, common elements, systematic review, meta-analysis
INTRODUCTION
Common mental disorders (CMDs), which include depressive, anxiety, and posttraumatic stress disorders, represent one of the leading causes of disability worldwide (Whiteford et al. 2013). Global prevalence rates are estimated at 4.7% for depressive disorders (Ferrari et al. 2013) and 7.3% for anxiety disorders (Baxter et al. 2013). Among populations affected by political violence and displacement, which primarily occur in low- and middle-income countries (LMICs), the prevalence rates of depression and posttraumatic stress average, respectively, 30.6% and 30.8% (Steel et al. 2009). Twelve-month prevalence rates are estimated at 17.6% for all CMDs worldwide, and 29.2% of adults will experience a CMD at some point during their life (Steel et al. 2014). CMDs also account for 41.9% of the burden of all mental and substance use disorders (Whiteford et al. 2013). CMDs significantly impair the quality of life, social functioning, and workforce participation of sufferers and their family members and larger communities (Chisholm et al. 2016, Whiteford et al. 2015). Consequently, the annual global cost attributable to CMDs is estimated at $1.15 trillion (Chisholm et al. 2016).
Empirically supported psychological treatments are among the most effective mental health interventions for treating CMDs (Patel et al. 2016a). However, they are not accessible for most populations in most countries. This is particularly true in LMICs, where intervention coverage for CMDs is estimated at 7% to 28%, resulting in a treatment gap of up to 93% (Chisholm et al. 2016). A recent review observed a treatment gap of more than 90% for CMDs in India and China, two relatively well-resourced middle-income countries (Chisholm et al. 2016, Patel et al. 2016b). There are many reasons for the poor coverage of psychological treatment including a reliance on a limited number of specialists to provide or supervise treatments, as well as to train therapists (Kohrt et al. 2015); the use of highly specific disorder-based treatment packages (England et al. 2015, Kazdin 2016, Murray et al. 2014, Weisz et al. 2012); and the stigma of seeking help for CMDs and other mental illnesses (Semrau et al. 2015).
The dissemination and implementation of empirically supported psychological treatments in any setting can be challenging (Kazdin 2016). The barriers are, in part, due to the nature of how these treatments develop, which typically begins in highly specialized academic centers and involves individuals who are attending mental health clinics (and, therefore, already have a psychological explanatory model) and who are drawn from a narrow sociocultural group. Additionally, these psychological treatments rely on expensive but scarce mental health professionals for delivery. Moving to real-world, LMIC-based settings, in which the vast majority of individuals with CMDs will pursue treatment options through primary health-care or other community platforms, requires psychological treatments to be delivered by nonspecialist providers (NSPs; i.e., through task sharing) and addresses explanatory models distinct from those of mental health practitioners. Thus, although the World Health Organization’s (WHO’s) Mental Health Gap Action Program (mhGAP; WHO 2015) recommends psychological treatments as first-line treatment for CMDs, the challenge lies in determining how these can be delivered in real-world settings.
During the past 15 years, global mental health researchers have developed innovative approaches to reduce psychological treatment gaps by addressing some of the barriers to implementation. Examples include aligning the treatment content with prevailing illness beliefs; delivering the treatment in accessible settings, such as in primary care and in community settings; and using NSPs to enhance the availability of human resources for delivery (van Ginneken et al. 2013). Systematic reviews (Clarke et al. 2013, van Ginneken et al. 2013) have demonstrated that these innovations have been associated with moderate to large effects on clinical and social outcomes in individuals with CMDs. More recently, global mental health has followed trends from high-income countries (HICs), moving toward transdiagnostic, or common element, approaches that address the barrier of focusing on treating a single disorder (Bolton et al. 2014a,b; Murray et al. 2014). Transdiagnostic treatments teach a set of common practice elements that can be delivered in varying combinations to address a range of problems. Decision rules based on research conducted on effective psychological treatments guide the selection and sequencing of elements, but allow for flexibility in addressing an individual’s symptom presentation (Chorpita & Daleiden 2009). Identifying which common elements are used in psychological treatments is an implementation strategy that is likely to help with dissemination, scale-up, and, ultimately, sustainability.
Despite the growing evidence that testifies to the success of psychological treatments in the global context, there is no review of relevant implementation processes or the common elements utilized when delivering psychological treatment to adults in LMICs. Such a synthesis has relevance for the scaling-up of these approaches, not just in LMICs but also for HICs, which are also struggling to reduce treatment gaps.
Aims
The aim of this review is to synthesize key implementation processes related to the delivery of psychological treatment in LMICs by NSPs and to update the evidence on their effectiveness for treating adults with CMDs. The primary research questions we address are
what was the composition of the psychological treatments for CMDs in terms of their components (i.e., elements and techniques);
who delivered the psychological treatments (i.e., a description of the NSPs and their supervisors);
where were the psychological treatments delivered;
how were NSPs trained and supervised and how were psychological treatments delivered, including a description of training and supervision procedures, and how were sessions delivered; and
what is the relative effectiveness of these psychological treatments on clinical outcomes, and what are the effects of the components on effectiveness.
The ultimate goal of our systematic review was to generate knowledge to inform the design of psychological treatments for scalability and effective delivery to the large proportion of individuals with CMDs in resource-constrained contexts. We also intended to identify knowledge gaps for future research.
Guiding Principles
Our approach to reviewing the evidence base is consistent with the US Institute of Medicine’s recent framework for psychosocial interventions, which calls for independent systematic reviews followed by the selection and development of quality measures to enhance the implementation of these psychological treatments in routine care (England et al. 2015). Three principles guided our approach in this review.
First, we focused only on articles in which psychological treatments for CMDs had been evaluated through a randomized controlled trial (RCT) to ensure that we assessed high-quality data and to enable us to examine implementation processes, including treatment elements, in relation to effectiveness. Also, we focused on depression, anxiety, and posttraumatic stress for the following reasons: CMDs are the leading mental health cause of the global burden of disease (Chisholm et al. 2016); WHO’s guidelines recommend psychological treatment as first-line treatment for CMDs (WHO 2015); and the vast majority of trials in LMICs target CMDs (van Ginneken et al. 2013).
Second, we included only articles in which the front-line delivery of psychological treatment was carried out by NSPs. Task-sharing, also known as task-shifting, refers to collaborating with NSPs to deliver health-care services that have been traditionally relegated to experts with professional degrees or certifications (WHO 2008). In the context of global mental health, an NSP is defined as anyone who provides, or intends to provide, mental health care but has not had specialized professional clinical training in a field closely related to mental health (van Ginneken et al. 2013). NSPs may include, but are not limited to, community health volunteers, peers from the same community, social workers, midwives, auxiliary health staff, teachers, primary care doctors and nurses, and persons without a professional service role. The rationale for the principle of involving NSPs is that it is extremely unlikely that there will ever be sufficient mental health professionals to deliver psychological treatment in any country; thus, dissemination hinges on delivery by NSPs. Our criteria did not, however, imply there was no role for mental health professionals who could be engaged in capacities such as being a supervisor or trainer.
Third, we carried out our analysis of the treatment content by adopting the distillation approach of dismantling the psychological treatment packages into their common elements. Based on several studies (Chorpita & Daleiden 2009, Chorpita et al. 2007), the recent IOM report (England et al. 2015) called for identifying the therapeutic elements that are common across effective psychological treatments. Such an approach lies at the heart of some transdiagnostic treatments in which a set of common elements can be delivered in varying combinations to address diverse mental health conditions (Farchione & Bullis 2014, Kaehler et al. 2016, McHugh et al. 2009). Transdiagnostic treatments may be particularly suitable for CMDs because these disorders share genetic, familial, and environmental risk factors (Kendler 1996, Kessler et al. 2005) and, unsurprisingly, are often comorbid conditions (Brown et al. 2001). Furthermore, it is not feasible to train NSPs to deliver multiple types of psychological treatments, given limited funding and scarce personnel (Murray & Jordans 2016); also, the use of multiple treatment manuals can lead to confusion and redundancy (Kazdin & Blase 2011). Thus, by using existing blueprints (e.g., Chorpita & Daleiden 2009, Michie et al. 2013, Murray et al. 2014) we aimed to develop a taxonomy of common elements that pertains to adults in LMICs.
METHODS
Protocol and Registration
We conducted a systematic review and meta-analysis in accordance with PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines (Moher et al. 2009). The protocol was developed following the procedures outlined in the Cochrane handbook for systematic reviews (Higgins et al. 2011) and registered with PROSPERO (the international prospective register of systematic reviews; CRD42016029451).
Search Strategy
We used search strategies from the most recent Cochrane review of mental health treatments delivered by nonspecialist health workers in LMICs (van Ginneken et al. 2013). All articles retrieved using these strategies that met the eligibility criteria (described in the next section) were included in the current review. To update the review with recent publications, we extended the search from January 2012 to March 2016, utilizing the following databases: CINAHL (search date of March 15, 2016), Ovid MEDLINE (March 15, 2016), Ovid MEDLINE In-Process (March 15, 2016), WHO’s Global Index Medicus (March 15, 2016), PsychINFO (March 15, 2016), Web of Science (full catalogue) (March 16, 2016), Cochrane CENTRAL (March 18, 2016), and EMBASE (March 18, 2016). The search strategies are available in the Supplemental Appendix. In addition, the bibliographies of systematic reviews of psychological treatments delivered by NSPs in LMICs were also considered (Chowdhary et al. 2014, Clarke et al. 2013, Rahman et al. 2013, van’t Hof et al. 2011, van der Waerden et al. 2011, van Ginneken et al. 2013).
Eligibility Criteria
Articles eligible for inclusion were required to demonstrate the following five characteristics:
The trials were conducted in an LMIC as defined by The World Bank Group in 2015 (World Bank 2015) or at the time of the trial (e.g., trials conducted in Chile prior to Chile becoming a high-income country). Consistent with prior reviews in LMICs (van Ginneken et al. 2013), Taiwan was grouped with China, even though Taiwan is categorized as an HIC.
The psychological treatment was delivered by an NSP.
The psychological treatment outcomes included CMDs: depression, anxiety, and posttraumatic stress disorder.
The participants were adults, defined as individuals aged 18–65 years (no articles were found that exclusively targeted persons older than 65 years).
The trial was an RCT.
There were two exclusion criteria:
The trials included only self-help treatments without an NSP delivery component.
The trials were feasibility or pilot trials; however, if the feasibility or pilot trial was tied to a published RCT, then data were extracted from these secondary sources.
Trial Selection
Two researchers (D.R.S. and B.A.K.) and two research assistants independently identified eligible articles by systematically screening titles and abstracts to determine whether an article met the eligibility criteria. Each abstract that was deemed ineligible was screened by the second researcher and, if necessary, by a third researcher (V.P.) to reach a final consensus. Next, eligible articles were distributed among the researchers (D.R.S., B.A.K., L.K.M., and A.A.) and the full-text was screened. At this stage, articles that were deemed ineligible were verified by two additional researchers. Once eligible trials had been identified, their bibliographies were reviewed to identify any related articles, including those describing protocols for the development or adaptation of the tested treatment, or secondary analyses, and these additional articles were drawn upon as secondary publications to enrich the data sources for the eligible trials. Although most articles reported only one trial, two articles each reported two trials, so data extraction and analysis were conducted for each specific trial.
Development of Taxonomy of Treatment Components
Our aim was to develop a taxonomy of treatment components, comprising elements and techniques, that cut across treatment packages. We defined an element as a therapeutic activity or strategy (Chorpita & Daleiden 2009, Chorpita et al. 2007, England et al. 2015), and a technique as skills that the therapist implements during a session to deliver an element. We further categorized elements into nonspecific elements (also referred to as engagement elements), which are universal to the therapy experience and reflective of the approach used by the therapist to engage a patient or implement the therapy, or both (Becker et al. 2015, Duncan et al. 2010, Wampold 2015). We defined specific elements as those that are grounded in specific psychological mechanisms; these were grouped into four broad domains to facilitate heuristic understanding: emotional, behavioral, cognitive, and interpersonal. These domains were not synonymous with a particular class of treatment.
We conducted a systematic, multistep analysis of existing taxonomies of common psychological treatment elements and behavioral change techniques used for CMDs (Chorpita & Daleiden 2009, Chorpita et al. 2007, Michie et al. 2013, Murray et al. 2014, PracticeWise 2015). Next, we compiled a list of eligible elements and reviewed these for duplication and redundancy. After that, each element was operationalized and reviewed by the researchers. Four rounds of pilot testing followed, whereby four researchers independently coded two or more eligible trials to test and iteratively adapt the existing taxonomy. During this phase, interrater reliability was estimated using an intraclass correlation (ICC). After each round of coding, similarities and discrepancies were discussed among the coders, and modifications were made to the taxonomy. Our final round of coding indicated a high degree of agreement among coders (ICC = 0.77–0.85). At this stage, an expert panel of psychological treatment researchers (see Acknowledgments) was invited to review the taxonomy to comment, for example, on the classification of elements and techniques, missing elements, or redundancies.
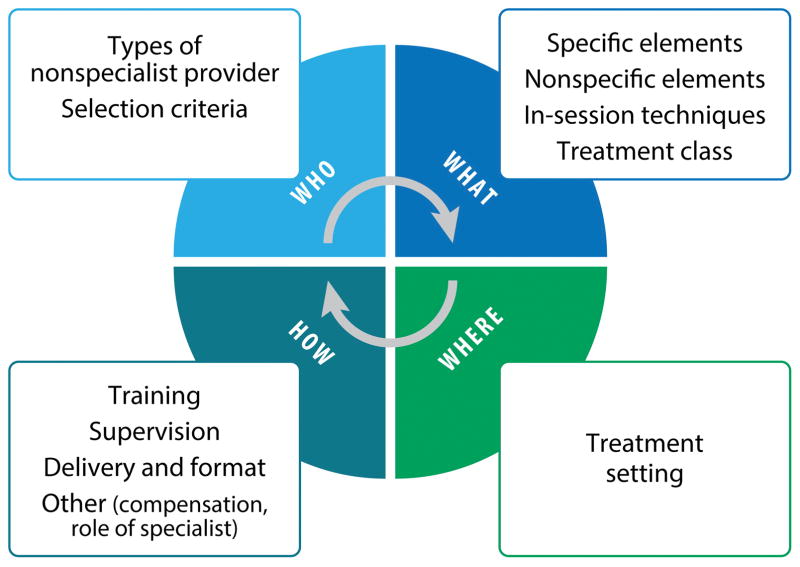
Next, primary authors were contacted via email and asked to complete an online survey and select which elements and techniques from the taxonomy comprised components of their treatment, as well as to select the treatment class (or classes) to which their psychological treatments belonged (a copy of the author survey is available in the Supplemental Appendix). In the event that trial authors perceived that the existing taxonomy did not accurately capture the elements in their treatment package, they were also given the option of using the Other category to elaborate upon existing elements or add elements. Finally, for those trials in which the authors did not respond, two researchers independently coded the same article with high interrater reliability (ICC = 0.90). Discrepancies were discussed and, when necessary, a third researcher was consulted. A final review of the taxonomy took place following responses from the authors of the eligible trials, resulting in the current taxonomy, which includes 18 specific elements in four domains (behavioral, interpersonal, cognitive, and emotional); 9 nonspecific engagement elements; and 12 in-session techniques (Figure 1).
Figure 1.
The taxonomy of treatment components of psychological treatments for common mental disorders delivered to adults in low- and middle-income countries.
Data Extraction
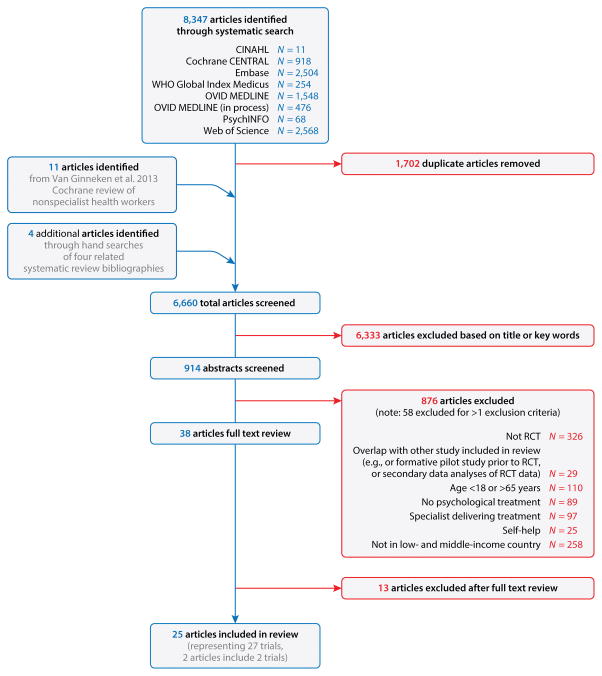
Apart from the data on treatment components described above, two other types of data were extracted by the review authors: (a) those related to other implementation processes (Figure 2), and (b) data for the meta-analyses.
Figure 2.
Implementation processes related to the who, what, where, and how of delivering psychological treatments in low- and middle-income countries.
For other implementation processes, data extraction was conducted by distributing the articles to four researchers (D.R.S., B.A.K., L.K.M., and A.A.). We extracted data relevant to the themes of the analysis, both from the primary RCT publications and, when available, from linked articles describing how the treatment was developed and delivered (a copy of the implementation coding is available in the Supplemental Appendix). Linked articles included trial protocols, articles about developing the treatments, or secondary analyses, and they were utilized to supplement the descriptions in the primary trial article (see Table 1 for citations to these articles).
Table 1.
Trial characteristics
| Reference | Secondary papers | Country | Sample size | Trial design | Population (mean age; range) | Recruitment setting | Intervention | Control group |
|---|---|---|---|---|---|---|---|---|
| Ali 2003 | Gul & Ali 2004, Naeem et al. 2003 | Pakistan | 161 | RCT | Women in the local community (32.6; 18–50) | Home | 8 sessions of supportive, cognitive, and problem-solving counseling | Usual treatment |
| Araya 2003 | Araya et al. 2006 | Chile | 211 | RCT | Primary care attendees (42.6; 18–70) | Primary care | 7 weekly sessions and 2 booster sessions of psychoeducational group and pharmacotherapy program for patients with severe or persistent depression | Usual treatment |
| Bass et al. 2013 | Hall et al. 2014 | Congo | 313 | RCT | Female survivors of sexual violence (<35; *) | Mental health clinics | 1 individual session and 11 group sessions of cognitive processing therapy | Individual support |
| Bolton et al. 2014a | Magidson et al. 2015, Murray et al. 2014; Weiss et al. 2016 | Iraq | 347 | RCT | Survivors of systematic violence (>17; 39.8*) | Home, community | 12 sessions of brief behavioral activation treatment for depression (psychotherapy); 12 sessions of cognitive processing therapy | Wait-list control |
| Bolton et al. 2014b | Murray et al. 2014; Weiss et al. 2016 | Thailand | 180 | RCT | Burmese refugees and survivors of violence (35.5; >17*) | Home, community | 7–13 sessions of cognitive behavioral therapy | Wait-list control |
| Bolton et al. 2003 | Bass et al. 2006, Verdeli et al. 2003 | Uganda | 326 | cRCT | Local men and women (46.5; 26.7–66.1) | Home, community | 16 sessions of interpersonal psychotherapy | Usual treatment |
| Chen et al. 2000 | NA | Taiwan | 60 | RCT | Primary care attendees (29.1; 19–40) | Primary care | 4 sessions of support group | Usual treatment |
| Chibanda et al. 2014 | Chibanda et al. 2011 | Zimbabwe | 49 | RCT | Postpartum mothers (25; 18*) | Primary care | 12 sessions of group problem-solving therapy | Usual treatment |
| Dybdahl 2001 | Dybdahl & Pasagic 2000 | Bosnia | 87 | RCT | Bosnian displaced mother–child dyads (30.7; 20–44) | Home, community, refugee camp | Weekly psychosocial discussion groups | Enhanced usual care |
| Fritsch 2007 | NA | Chile | 274 | RCT | Primary care attendees (NA; 18–70) | Primary care | Regular telephone contact with patients | Usual treatment |
| Gao et al. 2010 | Gao et al. 2012 | China | 194 | RCT | New mothers (28.4; 21–35) | Primary care | 2 groups sessions of IPT | Enhanced usual care |
| Gao et al. 2015 | Gao et al. 2014 | China | 180 | RCT | Pregnant mothers (28.6; *) | Primary care | 1 session of psychoeducation | Usual treatment |
| Hirani et al. 2010a | Hirani et al. 2010b | Pakistan | 15 | cRCT | Local women (NA; 25–35) | Community | 8 sessions of behavioral group counseling; 8 sessions of economic skill-building | Usual treatment |
| Ho 2009 | NA | Taiwan | 163 | RCT | Primary care attendees (29.3; 20–35) | Primary care | 1 session of education program | Usual treatment |
| Kaaya 2013 | Antelman et al. 2007 | Tanzania | 188 | RCT | HIV-positive pregnant mothers (26.0, >17*) | Primary care and antenatal clinics | 6 sessions of problem-solving therapy | Usual treatment |
| Milani et al. 2015 | NA | Iran | 54 | RCT | Postpartum mothers (28.0; *) | Primary care | 12–18 sessions of telephone support | Usual treatment |
| Patel et al. 2010 | Buttorff et al. 2012, Chatterjee et al. 2008 | India | 1,961 | cRCT | Primary care attendees (26.3; >16*) | Primary care | 6–12 sessions of IPT | Enhanced usual care |
| Rahman et al. 2008 | (Rahman 2007, Rahman & Creed 2007 | Pakistan | 798 | cRCT | Pregnant mothers (26.7; 16–45) | Home | 16 sessions of CBT | Enhanced usual care |
| Rojas 2007 | Araya 2003 | Chile | 230 | RCT | Primary care attendees (26.6; *) | Primary care | 8 sessions of group CBT | Usual treatment |
| Rotheram-Borus, 2014 | Richter et al. 2014, Rotheram-Borus et al. 2011 | South Africa | 287 | cRCT | HIV-infected women (26.5; *) | Primary care and HIV clinics | 8 sessions of CBT | Usual treatment |
| Singla et al. 2015 | Singla & Kumbakumba 2015 | Uganda | 291 | cRCT | Mothers with children <3 years (27.4; 21–49) | Home, community | 12 sessions of an integrated parenting program; 6 focused on common maternal mental disorders using IPT, CBT, and MI-based techniques | Wait-list control |
| Tiwari et al. 2010 | NA | China | 200 | RCT | Chinese women survivors of intimate partner violence (38.1; >17*) | Schools, community | 12 sessions of telephone social support | Usual treatment |
| Weiss et al. 2015 | Murray et al. 2014 | Iraq | 218 | RCT | Torture survivors (CPT, 40.3; CETA-42.8) | Community | 8–12 sessions of CBT; 12 sessions of CPT | Wait-list control |
| Wijesinghe 2015 | NA | Sri Lanka | 133 | RCT | Patients with a recent snakebite (42.1; >17*) | Emergency department | 1 session of CBT; 1 session of psychological first aid and psychoeducation | Usual treatment |
| Yeomans et al. 2010 | NA | Burundi | 76 | RCT | Internally displaced persons (38.6; *) | Community | 3-day psychoeducation workshop | Wait-list control |
Range not available.
Abbreviations: CBT, cognitive behavioral therapy; CETA, common elements treatment approach; CMD, common mental disorder; CPT, cognitive processing therapy; cRCT, cluster randomized controlled trial; IPT, interpersonal psychotherapy; MI, motivational interviewing; NA, not available; RCT, randomized controlled trial.
Trial characteristics
To conduct meta-analyses of the effects of the psychological treatments on continuous outcomes of CMDs, we extracted the means and standard deviations of primary endpoints for both the intervention and control arms and their respective sample sizes. When multiple control groups were available, data from the active control group were prioritized for extraction. When relevant information was not available for either type of data, we contacted the primary authors for clarification.
Analyses
We estimated the frequency of the use of each specific implementation process and treatment component. All frequencies are represented by a percentage in which the denominator is the total number of eligible trials (N = 27), unless otherwise indicated (e.g., if data were not specified or missing for a particular variable). We also estimated the total number of individual treatment elements and in-session techniques for each trial and further grouped them according to the primary disorder outcome as defined by the trial’s author. For some variables, there was the option to choose the category Other (e.g., for the treatment setting), whereby authors could insert a category that was not included in the response options. When variables were labeled Other, they were analyzed qualitatively by two researchers, and this analysis was then used to generate frequencies for each code. When possible, the mean was calculated along with the 95% confidence interval (CI). When ranges were provided for a particular trial (e.g., 6 to 10 sessions), the average was used (e.g., 8 sessions). Outliers were identified and, when applicable, analyses were repeated without these outliers.
For the meta-analyses, we utilized all available outcome data for CMDs in each trial (any CMD; depression, posttraumatic stress, anxiety, or mixed anxiety/depression). Analyses were carried out using Cochrane Review Manager version 5.3 (Cochrane Collab. 2014). This program requires means and standard deviations for both the intervention and control groups to calculate the standardized mean difference (SMD). A forest plot of the SMDs with summary statistics (pooled effect sizes) was calculated. Those trials without available data (e.g., trials that presented results as odds or risk ratios) were not included in our meta-analyses. We employed a random-effects analysis because we expected heterogeneity arising from the presence of cluster randomized controlled trials for which the random-effects model is the method of choice (Hayes & Moulton 2009). Heterogeneity among trials was calculated using the I2 measure of inconsistency. One forest plot with a pooled estimate was calculated using all primary outcomes. Additional forest plots with pooled estimates were calculated separately by condition (depression, posttraumatic stress, anxiety, mixed anxiety/depression), employing both primary and secondary outcomes. A test for subgroup differences was conducted among conditions. We did post hoc subgroup analyses using leave-one-out analyses to test the impact of excluding single trials that had a disproportionately large effect.
Finally, we conducted exploratory analyses of the domains of treatment elements and in-session techniques by calculating the simple summative score for the diversity of elements per subcategory. Again, treatment elements and in-session techniques were calculated for each eligible trial (N = 27). Thus, larger scores reflect a greater number of elements per subcategory (e.g., a treatment in which collaboration and empathy were used as the nonspecific elements would be scored 2 compared with a treatment that used only empathy as a nonspecific element, which would receive a 1). Correlations among the total number of element domains were estimated using Pearson’s r. Effect sizes were calculated using the SMDs for the primary continuous outcomes when relevant data were available. Additionally, we were able to transform the binary outcome data using an online calculator to estimate the effect size (https://www.campbellcollaboration.org/effect-size-calculato.html, Campbell Collab., Oslo, Norway). Thus, we were able to include results from all trials in these analyses.
To estimate the independent effects of specific and nonspecific domains on trial effectiveness, we analyzed two separate models using forward multiple regressions: (a) in the first model the dependent variable was the effect size (as described above) as predicted by two independent variables—the summed score of all treatment-specific elements and the summed score of the nonspecific elements; and (b) in the second model the dependent variable was the effect size as predicted by five independent variables, each representing one summed score for each domain of engagement, behavioral, cognitive, interpersonal, and emotional elements. For these analyses, we selected only one outcome estimate for each trial, prioritizing the continuous outcome defined as primary by the authors to estimate the effect size. Model fit and the variance accounted for by the model was estimated (F, R2). The variance inflation factor (VIF) was calculated for each model to assess multicollinearity among independent variables, with a conservative estimate (VIF ≥ 5). These quantitative analyses were conducted using SAS 9.3 (SAS Inst. 2011).
RESULTS
Trial Selection and Participant Response
Figure 3 presents the flowchart describing the inclusion of articles. We began our review by identifying 11 articles from the latest Cochrane Review (van Ginneken et al. 2013). Our systematic review of publications since the publication of van Ginneken et al. (2013) yielded 6,645 eligible articles, after removal of duplicate references. Our review of other systematic reviews yielded 4 articles that had not been found during our systematic search. After title, abstract, and full paper review, our final review included 25 articles, which included 27 trials (two articles included data on two trials). Among the 25 authors who were contacted to enter their treatment data, 21 (84%) completed the online survey used to distill treatment components.
Figure 3.
Flow chart for identifying eligible articles. Abbreviation: RCT, randomized controlled trial.
Trial Characteristics
Eligible trials and their characteristics are displayed in Table 1. Among these, 22 were individual RCTs and 5 were cluster randomized controlled trials. The trials were conducted in 17 countries, most commonly in sub-Saharan Africa (n = 7, including 2 in Uganda), East Asia (n = 6, including 5 from China or Taiwan), South Asia (n = 5, including 3 from Pakistan) and 3 each from Chile and Iraq. Almost half of the trials took place among urban populations, with the remainder equally distributed among rural and semiurban populations. The target population in most trials was primary care attendees (77.8%), followed by torture survivors (14.8%), persons living with HIV (7.4%), and refugees (7.4%). The majority of trials (62.9%) targeted only women, almost half of whom were mothers in the pre- or postnatal phase. Trial participants were most likely to be recruited from primary health-care settings, notably those providing maternal and reproductive services (n = 12), followed by community settings (n = 8), and participants’ homes (n = 6). Home-based recruitment typically took place in refugee camps or communities in which house-to-house screening was used to identify potential participants who had a CMD. Other settings included specialty services in HIV facilities. The median sample size inclusive of intervention and control arms was 194 participants (range = 15 to 1,961). Excluding the outliers of the largest and smallest trials (Patel et al. 2010, n = 1,961; Hirani et al. 2010a, n = 15), the average sample size for the trials was 219 participants (range = 49–798). The average age of participants was 33.9 years (95% CI = 31.1–36.9). The majority of participants were from low socioeconomic backgrounds—for example, they had relatively low levels of education or did not have formal employment outside of the home, or both.
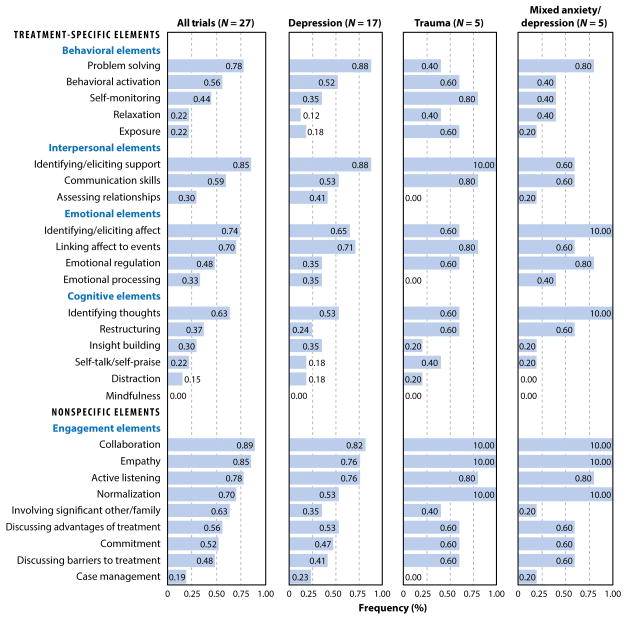
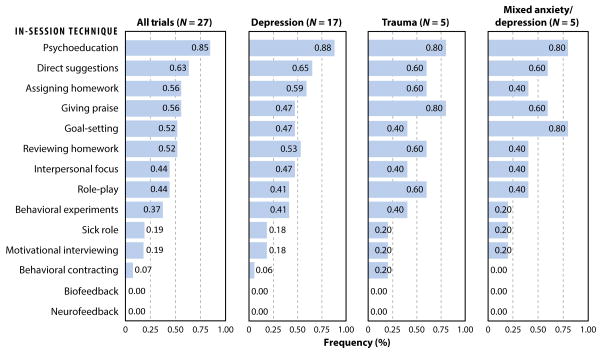
What: Implementation Processes Related to Treatment Components
The five most commonly endorsed nonspecific elements were empathy (88.9%); collaboration (85.2%); active listening (77.8%); normalizing treatment or aspects of the illness (70.4%), or both; and involving family members or a significant other (63.0%). The five most commonly used specific elements were eliciting or identifying social support (85.2%); engaging in problem-solving (80.8%); identifying or eliciting affect (76.9%), or both; linking affect to events (76.9%); and identifying thoughts (63.0%). At least one behavioral, interpersonal, and emotional element was used in 23 trials (85%); at least one cognitive element was used in 20 trials (74.1%). The specific elements least often used were mindfulness (0%), distraction (14.8%), self-talk (22.2%), exposure (22.2%), and relaxation (22.2%). The least commonly used nonspecific element was case management (18.5%). Among the additional nonspecific elements suggested by trial authors, one author suggested “giving hope” and another suggested “making eye contact.” Figures 4 and 5 present, respectively, the frequencies of the use of elements and techniques.
Figure 4.
Specific and nonspecific elements used to address common mental disorders in 27 trials in low- and middle-income countries.
Figure 5.
Techniques used in sessions to address common mental disorders in 27 trials in low- and middle-income countries.
Overall, treatments included an average of 5.22 out of 9 nonspecific elements and 7.81 out of 18 specific elements. On average, treatments comprised 2.24 out of 5 behavioral elements, 2.26 out of 4 emotional elements, 1.71 out of 3 interpersonal elements, and 1.74 out of 6 cognitive elements. The contribution of the domains of elements (nonspecific versus specific, and the domains of specific elements) on treatment outcomes are described in the section titled The Effectiveness of Treatments for Common Mental Disorders Delivered by Nonspecialist Providers in Low- And Middle-Income Countries. The most common in-session techniques used were psychoeducation (85.2%), providing direct suggestions (59.2%), assigning homework (59.2%), giving praise (55.6%), and goal setting (55.6%). The least common in-session techniques used were biofeedback or neurofeedback (0%), behavioral contracting (7.4%), and giving the sick role or using motivational interviewing (18.5% each). When asked, most authors (63%) indicated they used more than one class of treatments, with 2.26 classes being the average (95% CI = 1.76–2.77). The most commonly used treatment class was psychoeducation (33.3%), followed by problem-solving (23.1%), cognitive behavioral therapy (17.9%), and behavioral activation or interpersonal psychotherapy (12.8%). No additional classes of psychological treatments were proposed by authors.
We measured the internal consistency of the taxonomy by using Cronbach’s α (Cronbach 1988), which indicated modest to good reliability within the domains of specific elements (cognitive: α = 0.593; behavioral: α = 0.601; emotional: α = 0.662; interpersonal: α = 0.673), within nonspecific elements (α = 0.781), and within in-session techniques (α = 0.842). We observed significant correlations between these domains, in particular between the behavioral and cognitive domains (r = 0.611, p < 0.001) and between the emotional and interpersonal domains (r = 0.474, p < 0.01). Similarly, the domain of nonspecific elements was significantly correlated with the specific element domains (r = 0.425–0.483, p < 0.01), with the exception of the cognitive element domain (r = 0.235, p = 0.240).
Almost half of the trials targeted parenting (n = 13); typically, those trials targeted mothers by providing psychoeducation related to childcare for parents or by focusing on parent–child interactions. Approximately one-quarter of all trials (22.2%) targeted substance abuse; 18.5% included the ability to prescribe psychotropic medications. These components were not included in our final taxonomy as they did not primarily target the CMD outcome.
Who: Implementation Processes Related to Who Delivered the Treatment
The most common NSPs were community health workers employed through the health system (33.3%). The other frequently used personnel were peers or individuals specifically recruited for the trial from the same community (29.6%), nurses (18.5%), and midwives (14.8%). The rationale for selecting a given NSP was described by about half of the trials (n = 13): The most common rationale was that the NSPs were close to and had frequent contact with the target community (46.2%); also important were acknowledging the value of peer support (30.7%) and seeing the chosen individuals as a sustainable resource (23.1%) (e.g., by being employed at a local health center). Selection criteria for NSPs typically reflected their language proficiency or communication skills, or both, including their general interpersonal skills and fluency in local dialects. Among the 13 trials that reported education levels for NSPs, 30.8% reported that NSPs had up to a postgraduate education, but nearly one-quarter (23.1%) reported NSPs had only primary education (23.1%). One trial included literate NSPs as the criteria for selecting delivery agents, although they had had no formal schooling. Only half of the trials (n = 14) reported the gender of the NSPs; of these, all included females (100%) and the majority included only females (64.3%). Only three trials reported the age of the NSPs, which averaged 35 years (range = 30–50).
Mental health specialists had diverse roles in these treatments, most commonly during trial evaluation (100%), followed by training and supervising NSPs (66.7%), receiving referrals (25.9%), providing medication (14.8%), and sending referrals (11.1%) to another specialist to address physical health concerns (e.g., an obstetrician for pregnancy complications).
How: Implementation Processes Related to How Treatment Was Delivered
Training methods were reported by 18 trials. The majority of programs (77.8%) used a mixed methods approach to train NSPs; others reported only using didactics. The mixed approach typically involved an intensive period of didactics led by a trainer in face-to-face format, allowing the NSP to learn about the program or counseling skills, or both, which was followed by the opportunity to practice skills through role plays with other NSPs or patients, or both, during a pilot phase. A total of 17 trials specified the duration of their training period, which varied from 3 hours to 2 months. Overall, training lasted a mean of 78.82 hours (95% CI = 21.81–135.84); it lasted a mean of 53.80 hours (95% CI = 31.72–75.84) when the one outlier (Patel et al. 2010) was excluded in which training lasted 2 months because it covered skills that went beyond psychological treatment (e.g., case management). No trials reported conducting a formal evaluation to examine the competency of NSPs, or whether certification was provided. Only five trials reported compensating NSPs, which typically involved providing either a per diem or reimbursement for relevant costs, such as travel; in two trials, the NSP role was voluntary.
The format for supervision was reported by 15 trials. All trials conducted supervision in person, and almost half of these supplemented this supervision with telephone (46.7%) or Skype (40.0%) support. Supervision was conducted in groups (86.7%) and/or individually (66.7%)—some trials included both group and individual supervision. Supervision methods were reported in 19 trials and typically involved discussing a particular case (63.1%), observing a session (26.3%), or listening to an individual session via audio (10.5%), or some combination of these methods. Seventeen trials reported who conducted supervision and how often. These trials reported that an expert specialist provided supervision, either alone (76.5%) or with others (17.6%), such as other lay counselors or staff from nongovernmental organizations; only one trial exclusively used peers to conduct supervision (5.9%). Supervision was most often conducted weekly (76.5%); in other trials, ad hoc supervision was conducted when required (17.6%) or supervision occurred monthly (5.9%).
Almost three-quarters of trials (n = 18) reported using a manualized treatment strategy; 65% of trials used a phase- or session-specific sequence; and 40% used booster sessions. In all trials, treatment was delivered face to face; two (7.4%) also used the telephone. The majority of trials exclusively used an individual (51.9%) format; 37.0% used group formats; 11.1% used both.
Twenty-six trials provided information on treatment duration. When all 26 trials were included, the mean duration was 10.19 weeks (95% CI = 6.92 to 13.51); when the four outliers were excluded, treatment duration was 9.05 weeks (95% CI = 7.43 to 10.58) (Dybdahl 2001; Gao et al. 2015, 2010; Rahman et al. 2008). A total of 22 trials (81.5%) reported on the mean number of intended sessions, which was 9.59 (95% CI = 7.61–11.59); one trial (Bolton et al. 2014b) explicitly stated that sessions were intentionally varied (i.e., because they were based on an individual’s symptoms) and, therefore, it was not included in these analyses. Analyses of the number of intended sessions without the outliers (Bolton et al. 2003; Gao et al. 2015, 2010; Milani et al. 2015; Patel et al. 2010; Tiwari et al. 2010) showed a slight decrease to 9.30 sessions (95% CI = 7.94–10.78). Twenty-one trials reported the intended duration of each session, which was approximately 1 hour (mean = 63.45 min, 95% CI = 52.51–74.42); without the outliers (Bass et al. 2013, Bolton et al. 2003, Chen et al. 2000, Gao et al. 2010, Tiwari et al. 2010), this decreased to 56.88 min (95% CI = 50.12–63.78). However, the actual indicators of treatment delivery were described by only a handful of trials: 7 trials reported the number of sessions actually delivered (mean = 6.84, 95% CI = 3.11–10.61) and the duration of sessions was reported by one group-based therapy, which ranged from 60 to 90 minutes (Singla et al. 2015). A total of 23 trials reported the proportion of individuals who completed the entire or a significant amount of the psychological treatment (mean = 79.6% participants).
Where: Implementation Processes Related to Treatment Setting
The psychological treatment setting was reported by 26 trials. Half of the treatments were delivered in the community (50.0%)—for example in schools, at community meetings, and outdoors; 38.4% were delivered at primary care centers; and 26.9% were delivered in homes. Forty percent of the 26 trials provided a rationale for why a particular setting was selected, and most reasons related to enhancing accessibility for the target population. Three trials reported the relevant barriers and facilitators of their settings: The convenience of a location was cited as facilitating psychological treatment; barriers cited were interruptions from the community, weather, and a lack of privacy for conducting individual sessions.
The Effectiveness of Psychological Treatments for Common Mental Disorders Delivered by Nonspecialist Providers in Low- And Middle-Income Countries
The most common outcome assessment tools used for depression were the Hopkins Symptom Checklist (Derogatis et al. 1974) and the Edinburgh Postnatal Depression Scale (Cox et al. 1987), each of which were used in 6 of the 19 (32%) assessments of depression outcome. The tool most commonly used to assess posttraumatic stress was the Harvard Trauma Questionnaire (Mollica et al. 1992), which was used in 6 of the 8 (75%) assessments of outcomes for patients with posttraumatic stress disorder. The most common assessment tool for mixed anxiety/depression was the Hopkins Symptom Checklist, which was used in 2 of the 5 (40%) assessments. The most commonly used tool for assessing outcomes among patients with anxiety was the Hopkins Symptom Checklist, which was used in all three (100%) assessments. The average primary endpoint was reached in 3.33 months (95% CI = 2.52–4.19), with a range from 2 weeks to 6 months.
Because we restricted our analyses to continuous outcomes, consistent with our alignment with the transdiagnostic approaches that are implicit as the guiding principles of this review, authors whose publications included only dichotomous outcomes or had missing information on means or standard deviations were asked to provide details. Three trials were subsequently dropped from the meta-analyses due to incomplete information, leaving a total of 24 trials for these analyses. The final comparisons included 19 outcomes for depression, 8 for trauma, 5 for mixed anxiety/depression, and 3 for anxiety.
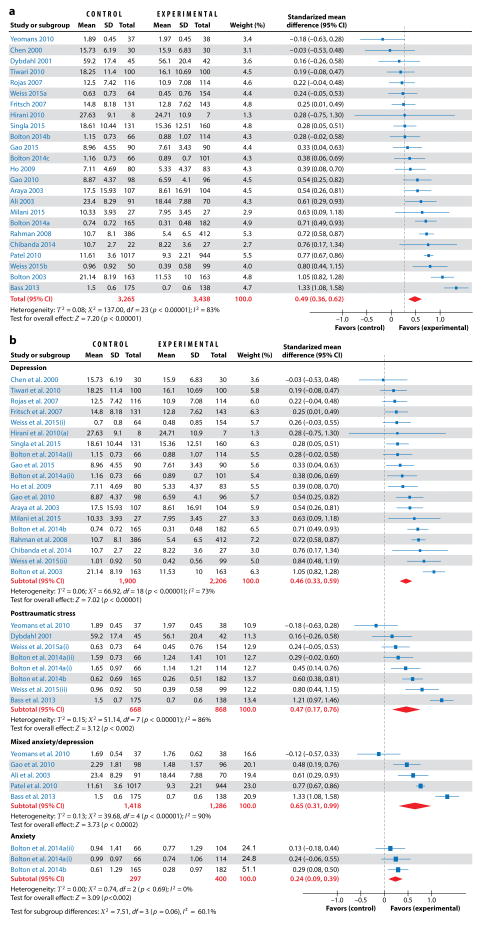
Figure 6 presents the forest plots of the effectiveness analyses. The SMD for the 24 primary outcomes was 0.49 (95% CI = 0.36–0.62), favoring the intervention with the inconsistency measure I2 = 83%, suggesting substantial heterogeneity among trials (Figure 6a). Additional pooled estimates were calculated for each CMD (Figure 6b) for 35 primary and secondary outcomes. For the 19 depression outcomes, the SMD was 0.46 (95% CI = 0.33–0.59, I2 = 73%). For the 8 trauma outcomes, the SMD was 0.47 (95% CI = 0.17–0.76, I2 = 86%). For the 5 mixed anxiety/depression outcomes, the SMD was 0.65 (96% CI = 0.31–0.99, I2 = 90%). For the 3 anxiety outcomes, the SMD was 0.24 (95% CI = 0.09–0.39, I2 = 0%). The test of subgroup differences among the outcomes was not significant (χ2 = 7.51, p = 0.06, I2 = 60.1%). In the leave-one-out analyses, the removal of the largest trial (Patel et al. 2010) did not substantially change the SMD for all outcomes (0.46, 95% CI = 0.34–0.58) or for mixed anxiety/depression (0.59, 95% CI = 0.02–1.16). The removal of the trial with largest effect sizes (cognitive processing therapy in the Democratic Republic of the Congo, Bass et al. 2013) reduced the SMD for posttraumatic stress (0.37, 95% CI = 0.16–0.57) and mixed anxiety/depression (0.48, 95% CI = 0.17–0.80); its removal also moderately reduced inconsistency (overall I2 = 77%; posttraumatic stress I2 = 65%). Removal of the Burundi posttraumatic stress trial (Yeomans et al. 2010), which compared trauma-related psychoeducation with reconciliation workshops and which was the only trial that showed poorer outcomes for the psychological treatment arm, improved the SMD for mixed anxiety/depression (0.80, 95% CI = 0.49–1.12, I2 = 88%).
Figure 6.
(a) Forest plot of the effects of psychological treatments on primary outcomes for common mental disorders in 24 trials in low- and middle-income countries. (b) Forest plot of the effects of psychological treatments on outcomes for common mental disorders in low- and middle-income countries by condition (N = 35). Abbreviation: CI, confidence interval; df, degrees of freedom; SD, standard deviation. Bolton 2014a(i): BMC Psychiatry, behavioral activation experimental condition versus control; Bolton 2014a(ii): BMC Psychiatry, cognitive processing therapy experimental condition versus control; Bolton 2014b, PLoS Medicine, common elements treatment approach (CETA) experimental condition versus control; Weiss 2015(i): BMC Psychiatry, cognitive processing therapy experimental condition versus control; Weiss 2015(ii): BMC Psychiatry, common elements treatment approach (CETA) experimental condition versus control.
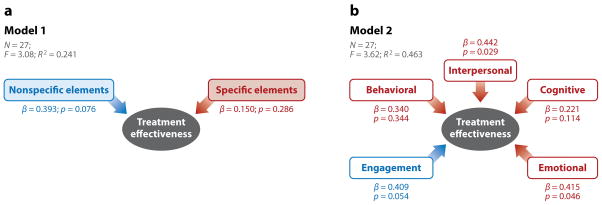
Exploratory analyses showed that the trial effect size was significantly related to the summed score of the number of all specific elements (Pearson’s r=0.383, p=0.048) and nonspecific elements (r = 0.474, p = 0.012). We evaluated the relative contribution of element domains to the effect sizes in two regression models. The first model (Figure 7a) examined the influence of two independent variables on effect size: the summed score of all specific element domains and the summed score of nonspecific elements. This model (F = 3.08, p = 0.037) accounted for 24.1% of the variance in effect size. Although neither variable showed a statistically significant association with effect size, the nonspecific elements domain showed trend-level effects (β = 0.393, p = 0.076). The second model (Figure 7b) evaluated the effects of five independent variables (total summed scores for four specific element and one non-specific element domain) on trial effectiveness. This model was more robust (F = 3.62, p = 0.016) and the five domains explained 46.3% of the variance (R2) in trial effectiveness. The strongest associations were observed for the interpersonal elements (β = 0.442, p = 0.029), emotional elements (β = 0.415, p = 0.046), and nonspecific (engagement) elements (β = 0.409, p = 0.052). None of the independent variables in either model showed evidence of multicollinearity (VIF < 2). Figure 7 shows the full results of both models.
Figure 7.
The effects of treatment-specific and nonspecific elements on trial effectiveness. (a) Model 1: comparison of specific and nonspecific elements on treatment effectiveness. (b) Model 2: comparison of nonspecific element domain with specific element domain showing effects on treatment effectiveness. β represents standardized beta. Treatment effectiveness is the effect size or standardized mean difference between the intervention and control groups at the primary endpoint.
DISCUSSION
The objective of this systematic review was to synthesize the evidence base for implementation processes and the effectiveness of psychological treatments for common CMDs in adults delivered by NSPs in LMICs. We identified 27 trials that met our eligibility criteria, with 35 primary and secondary outcomes. The majority of these trials targeted depression or posttraumatic stress in both urban and rural populations and across 17 LMICs. Two-thirds of the selected trials targeted only women, and many focused on perinatal CMDs. We intended for this synthesis to help inform the ultimate goal of disseminating psychological treatments globally.
Implementation Processes and Effectiveness
The most common NSPs were community health workers or peers with no formal health-care role who typically belonged to the same community as the beneficiary population. The selection of this type of NSP reflects attempts to utilize local, affordable, and sustainable resources (Fairburn & Patel 2014); the pragmatic considerations inherent to the goal of integrating mental health care into primary care (Patel et al. 2010); and community attitudes regarding preferred and accepted providers (Singla et al. 2014a). Mental health specialists had diverse roles related to building competency, maintaining quality, assuring safety, and (as researchers) evaluating psychological treatments. On average, the NSPs had approximately 10 days of face-to-face training, and supervision was typically conducted weekly in person, during which individual cases were reviewed with an expert supervisor. Most commonly, treatments were delivered in primary care or community settings in less than 10 sessions, each lasting up to 1 hour and delivered during 2 to 3 months. Most treatments were delivered individually and face to face, with about one-third including a group component. We conclude that these psychological treatments delivered in this way had medium to strong effects on improving outcomes in a range of CMDs.
In addition, the treatments distilled in this review comprised a set of elements, including nonspecific (engagement) elements and specific elements, spanning behavioral, interpersonal, cognitive, and emotional domains. The ultimate goal of dissemination is to identify a parsimonious set of elements that can, either alone or in combination, produce optimal clinical outcomes and are backed by a sound theory of change and some evidence of mediation (Murray & Jordans 2016). One or more nonspecific elements, typically empathy or collaboration, were included in all treatments. The five most commonly used specific elements across domains were (a) eliciting or identifying social support; (b) engaging in problem-solving; (c) identifying or eliciting affect, or both; (d) linking affect to events; and (e) identifying thoughts. Our taxonomy cuts across treatment classes, as intended, and is aligned with both the distillation literature on common elements and the methodologies used in other studies (Becker et al. 2015, Bolton et al. 2014b, Chorpita & Daleiden 2009, Chorpita et al. 2007, Michie et al. 2013). The taxonomy we developed showed modest to good internal consistency within domains, strong interrater reliability, and covered both nonspecific and domain-specific elements. The completeness and face validity of the list of elements and their organization was confirmed by trial authors and experts in psychological treatment. Our exploratory analyses of the contribution of elements to the effect sizes of psychological treatments found that the five domains of elements explained 46% of the variance in effect size. Both specific and nonspecific elements independently predicted trial effectiveness, highlighting the importance of both types of elements in treatment. The most common in-session techniques used were psychoeducation, giving praise, and assigning homework. Psychoeducation by itself constituted a treatment class in some trials but also was used as a technique in many more trials.
Implications for the Dissemination of Psychological Treatments
This review highlights several key implementation processes for treating CMDs. These include using a limited number of nonspecific and specific elements delivered by briefly trained NSPs over a few sessions in routine health-care and community settings to populations with large treatment gaps resulting from both demand and supply-side barriers. These findings have important implications for disseminating psychological treatments globally, including in HICs where these treatments are typically packaged by theoretical classes (e.g., interpersonal psychotherapy or cognitive behavioral therapy) for specific disorders; require long periods of training, which is delivered by mental health professionals in mental health facilities; and where brief manualized treatments typically range from 12 to 20 sessions. Despite these differences, our effect sizes in targeting CMDs are similar to effect sizes from a review of predominantly HIC trials with specialist-delivered treatments (Huhn et al. 2014).In addition, nonspecific elements—sometimes referred to as common factors (Barth et al. 2011, Webb et al. 2010)—were related to treatment effectiveness. These results are consistent with recent findings that showed among therapists in training, nonspecific skills (e.g., collaboration, empathy, and warmth) are independent contributors to patients’ outcomes (Anderson et al. 2015), in particular for brief treatments (Anderson et al. 2016). The competencies that providers need to deliver these nonspecific elements must be emphasized as a foundation for delivering psychological treatment. Additionally, our regression models highlight the benefits of examining specific elements domains, in particular those targeting interpersonal and emotional mediators. Others (e.g., Cuijpers et al. 2012) have typically aggregated treatment-specific elements and examined their effects as one variable. Although conceptually sound, this may omit some of the variance explained by treatment-specific elements, thus overstating the role of common factors (Webb et al. 2010). Therefore, our findings strongly indicate the need to expand the orthodox definitions of who is considered a mental health-care provider, what constitutes a psychological treatment, and where treatments can be delivered. Our findings point to using relatively simpler treatment protocols as the basis for more widely disseminating empirically supported psychological treatments.
Limitations of the Evidence
Our review identified an important gender gap in the evidence—that is, the relative lack of psychological treatments for men with CMDs. Two-thirds of the trials in this review exclusively focused on women, with a significant proportion in the remaining one-third also predominantly targeting women. The lack of treatment for men is especially concerning given that men’s mental health and behavior, in particular substance abuse and interpersonal violence, have a strong adverse impact on women’s mental health (Nayak et al. 2010), and suicide is a more frequent cause of death in men (WHO 2014b). In addition, including both genders may be beneficial, given the mediating pathway of perceived spousal support on psychological well-being (Singla et al. 2015).
Some of the methods used by global mental health innovators to implement psychological treatment in resource-constrained environments may pose challenges for wider dissemination. Thus, there are significant barriers to the wider adoption of such NSP-delivered psychological treatments, including the need for ongoing, structured supervision and adequate training and compensation (Mendenhall et al. 2014). The subgroup of trials that reported on these processes showed a continuing reliance on orthodox, face-to-face methods for training and supervision delivered by experts, which, although reported to be critical to changing behavior in therapy (Beidas et al. 2014), is a significant barrier to scale-up (Fairburn & Patel 2014). The use of digital platforms for training and supervision (Fairburn & Cooper 2011, Fairburn & Patel 2014), the development of standardized measures of competence for NSPs (Kohrt et al. 2015), and demonstration of the reliability and validity of peer supervision (Singla et al. 2014b) all point to potential solutions to addressing some of these barriers. Sustaining NSP-delivered treatments and motivating NSPs also need attention by developing compensation mechanisms that may work by, for example, professionalizing community health workers, as has been implemented by some countries (Maes & Kalofonos 2013).
An unexpected gap in the literature was the limited utilization of indigenous elements. For example, mindfulness, a practice rooted in South and East Asian culture, was not used by any of the trials. Although this may reflect a bias toward treatments developed in so-called Western contexts, recent research suggests that the effectiveness of treatment does not differ significantly among “homegrown” or “transported” treatments and that their elements are similar (Leijten et al. 2016). Also, adapting psychological treatments for use with culturally distinct populations shows effectiveness similar to that of the original treatments when changes are made in implementation while preserving the treatment’s content (Chowdhary et al. 2014). We did not find any trials of psychological treatments delivered by NSPs that used treatments from the third wave of psychotherapy [such as acceptance and commitment therapy (known as ACT) or mindfulness-based cognitive therapy (known as MBCT)]. These gaps may reflect the fact that these therapies have been delivered by specialists—for example, mindfulness-based stress reduction has been delivered by psychologists in Iran (Seyed-Alinaghi et al. 2012)—or manualized as a self-help therapy—for example, acceptance and commitment therapy is discussed in WHO’s Self Help Plus (WHO 2014a).
There are also limitations to our approach to distilling common elements from treatment packages. First, there are alternative methods for categorizing and coding elements of psychological treatments (e.g., Dickens et al. 2013, Weiss et al. 2016). Although our taxonomy was feasible and had strong face validity and good psychometric properties, there are other approaches that could have been utilized for parsing and coding treatment elements. Second, we do not capture the dose or extent to which elements are applied in the treatments. A psychological treatment that is centered on problem-solving elements (e.g., Chibanda et al. 2014) and a psychological treatment in which problem solving is one of many elements would have been coded similarly in our taxonomy; therefore, our approach does not distinguish between the number of times that problem solving was used and the degree to which it was used singly or in combination with other techniques. Third, although we have been able to extract descriptive information, we cannot infer whether these elements, when dismantled from their original treatment packages, would continue to have a therapeutic effect independent of the other elements in those packages. Thus, we must be cautious about our interpretations regarding significant associations among element domains that were based on summed scores of elements. At best, our analyses of treatment components can help the reader identify which elements are frequently used for psychological treatments delivered by NSPs, thus helping to set a research agenda to identify which elements, or combinations and sequences of elements, exert optimal effects.
Finally, the evidence in this review has been further bolstered by other recent trials (e.g., Chibanda et al. 2016; Patel et al. 2016; Rahman et al. 2016) that demonstrate the value of brief psychological treatments comprising a parsimonious set of elements for adult common mental disorders and delivered by NSPs in routine care settings in diverse populations.
CONCLUSIONS
This review confirms that innovations in global mental health to improve access to psychological treatments by using low-cost and widely available NSPs are more effective than usual care in LMIC-based settings. These innovations share a number of key treatment components and implementation processes, including the types of elements and techniques, the training and supervision formats for NSPs, and the number of sessions and duration during which the treatment is delivered. These common implementation processes could act as a blueprint for scaling-up these psychological treatments, not just in the LMICs from where our evidence base was generated but globally, with implications for the science of the dissemination of such treatments. Our review also highlights the gap in reporting on relevant implementation processes. Only two trials (Araya et al. 2006, Buttorff et al. 2012) reported an economic evaluation of their psychological treatments, and only one reported on mediators of the treatment’s effectiveness (Singla et al. 2015). Given the dearth of information on treatment elements and implementation processes, we recommend that authors of trials systematically report additional details (see Table 2), as has been proposed for complex public health treatments (Hoffmann et al. 2014).
Table 2.
Checklist of Key Implementation Processes for Psychological Treatments
Where?
|
What?
|
|
Who? Delivery agent
|
How? Training
|
Checklist of Key Implementation Processes for Psychological Treatments
Future research could evaluate the effectiveness of a parsimonious set of elements bound together by a theoretically sound framework and delivered in a transdiagnostic or stepped-care format; it could also evaluate the mediating pathways of the effectiveness of such composite treatments. Issues that require further examination are which elements may be most effective, including those elements that may be derived from indigenous approaches to mental health problems (Hinton & Kirmayer 2013); to what degree they may be effective; and in which combinations they influence trial effectiveness. Other key research issues include developing and evaluating strategies to address barriers to training and supervision, determining how best to scale-up the dissemination of psychological treatments—for example, possibly by using technology platforms— and evaluating the effectiveness of stepped-care systems based on the severity of the CMD and response of patients (Murray & Jordans 2016). Dissemination and implementation research will be critical during the next decade to translate the wealth of knowledge generated by global mental health innovators and use it to reduce the large gaps in the effective coverage of psychological treatments in populations around the world. We hope this review will stimulate the ongoing debate and research on the innovations needed to disseminate some of the most effective types of mental health care, with the ultimate goal of greatly enhancing their coverage and reducing treatment gaps for CMDs globally.
Supplementary Material
SUMMARY POINTS.
Global mental health researchers have developed innovative delivery frameworks for psychological treatments to reduce the clinical, social, and economic burdens of common mental disorders.
This article assesses the effectiveness of psychological treatments delivered by nonspecialist providers in low- and middle-income countries and innovative implementation processes for addressing common mental disorders in adults.
Our taxonomy of treatment components cuts across treatment modalities, as trial authors used a variety of common elements and in-session techniques, irrespective of the reported class or classes of psychological treatments.
Innovations reflect attempts to utilize local, affordable, and sustainable resources, including delivery agents from the same community, brief treatments with fewer than 10 sessions, and accessible settings.
These common implementation processes could act as a blueprint for scaling-up psychological treatments, not just in the low- and middle-income countries from where our evidence base was generated but globally, with implications for the science of the dissemination of psychological treatment.
FUTURE ISSUES.
It will be important to explore which elements, including indigenous elements, influence the effectiveness of psychological treatments for common mental disorders, and to determine to what degree and in which combinations they are most effective.
This examination of treatment components should be extended to psychological treatments for children and adolescents.
Key underlying processes should be examined, including conducting trials of treatment mechanisms and mediators of effectiveness, and their potential relationships to treatment elements.
Strategies to address barriers to disseminating psychological treatment delivered by nonspecialist providers need to be evaluated—for example, by evaluating digital platforms for treatment implementation and for training and supervising nonspecialist providers; scalable incentives for motivating nonspecialist providers to deliver psychological treatments also need to be determined.
The assessment of how a common-elements approach to delivering psychological treatments can be integrated with stepped-care approaches to maximize recovery in patients with common mental disorders.
Acknowledgments
The authors of this systematic review thank the generous efforts of their research assistants, Andi Schmidt and Anvita Bhardwaj, who assisted in screening the abstracts, as well as Dr. Brieanne Kohrt and Angela Leocata, who contributed to data extraction with conscientious precision. We thank our expert panel of advisers (Professors Steven D. Hollon, Paula Ravitz, and Holly Swartz) for their technical advice and reviewing our taxonomy of common elements. D.R.S. and B.A.K. were supported by National Institute of Mental Health grants U19MH095687 (D.R.S.) and K01MH104310 (B.A.K.). V.P. was supported by a Wellcome Trust Principal Research Fellowship (106919/Z/15). Finally, we appreciate the responses of the trial authors who completed the online survey and contributed data to this systematic review.
Footnotes
disclosure statement
The authors are not aware of any affiliations, memberships, funding, or financial holdings that might be perceived as affecting the objectivity of this review.
literature cited
- Ali BS, Rahbar MH, Naeem S, Gul A, Mubeen S, Iqbal A. The effectiveness of counseling on anxiety and depression by minimally trained counselors: a randomized controlled trial. Am J Psychother. 2003;57:324–36. doi: 10.1176/appi.psychotherapy.2003.57.3.324. [DOI] [PubMed] [Google Scholar]
- Anderson T, Crowley ME, Himawan L, Holmberg JK, Uhlin BD. Therapist facilitative interpersonal skills and training status: a randomized clinical trial on alliance and outcome. Psychother Res. 2015;26:511–29. doi: 10.1080/10503307.2015.1049671. [DOI] [PubMed] [Google Scholar]
- Anderson T, McClintock AS, Himawan L, Song X, Patterson CL. A prospective study of therapist facilitative interpersonal skills as a predictor of treatment outcome. J Consult Clin Psychol. 2016;84:57–66. doi: 10.1037/ccp0000060. [DOI] [PubMed] [Google Scholar]
- Antelman G, Kaaya S, Wei R, Mbwambo J, Msamanga GI, et al. Depressive symptoms increase risk of HIV disease progression and mortality among women in Tanzania. J Acquir Immune Defic Syndr. 2007;44:470–77. doi: 10.1097/QAI.0b013e31802f1318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Araya R, Flynn T, Rojas G, Fritsch R, Simon G. Cost-effectiveness of a primary care treatment program for depression in low-income women in Santiago, Chile. Am J Psychiatry. 2006;163(8):1379–87. doi: 10.1176/ajp.2006.163.8.1379. [DOI] [PubMed] [Google Scholar]
- Araya R, Rojas G, Fritsch R, Gaete J, Rojas M, et al. Treating depression in primary care in low-income women in Santiago, Chile: a randomised controlled trial. Lancet. 2003;361:995–1000. doi: 10.1016/S0140-6736(03)12825-5. [DOI] [PubMed] [Google Scholar]
- Barth RP, Lee BR, Lindsey MA, Collins KS, Strieder F, et al. Evidence-based practice at a crossroads: the emergence of common elements and factors. Res Soc Work Pract. 2011;22(1):108–19. [Google Scholar]
- Bass JK, Annan J, McIvor Murray S, Kaysen D, Griffiths S, et al. Controlled trial of psychotherapy for Congolese survivors of sexual violence. N Engl J Med. 2013;368:2182–91. doi: 10.1056/NEJMoa1211853. [DOI] [PubMed] [Google Scholar]
- Bass JK, Neugebauer R, Clougherty KF, Verdeli H, Wickramaratne P, et al. Group interpersonal psychotherapy for depression in rural Uganda: 6-month outcomes. Br J Psychiatry. 2006;188:567–73. doi: 10.1192/bjp.188.6.567. [DOI] [PubMed] [Google Scholar]
- Baxter A, Scott K, Vos T, Whiteford H. Global prevalence of anxiety disorders: a systematic review and meta-regression. Psychol Med. 2013;43:897–910. doi: 10.1017/S003329171200147X. [DOI] [PubMed] [Google Scholar]
- Becker KD, Lee BR, Daleiden EL, Lindsey M, Brandt NE, Chorpita BF. The common elements of engagement in children’s mental health services: which elements for which outcomes? J Clin Child Adolesc Psychol. 2015;44:30–43. doi: 10.1080/15374416.2013.814543. [DOI] [PubMed] [Google Scholar]
- Beidas RS, Cross W, Dorsey S. Show me, don’t tell me: behavioral rehearsal as a training and analogue fidelity tool. Cogn Behav Pract. 2014;21:1–11. doi: 10.1016/j.cbpra.2013.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolton P, Bass J, Neugebauer R, Verdeli H, Clougherty KF, et al. Group interpersonal psychotherapy for depression in rural Uganda: a randomized controlled trial. JAMA. 2003;289(23):3117–24. doi: 10.1001/jama.289.23.3117. [DOI] [PubMed] [Google Scholar]
- Bolton P, Bass JK, Zangana GAS, Kamal T, Murray SM, et al. A randomized controlled trial of mental health interventions for survivors of systematic violence in Kurdistan, Northern Iraq. BMC Psychiatry. 2014a;14:360. doi: 10.1186/s12888-014-0360-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolton P, Lee C, Haroz EE, Murray L, Dorsey S, et al. A transdiagnostic community-based mental health treatment for comorbid disorders: development and outcomes of a randomized controlled trial among Burmese refugees in Thailand. PLOS Med. 2014b;11:e1001757. doi: 10.1371/journal.pmed.1001757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown TA, Campbell LA, Lehman CL, Grisham JR, Mancill RB. Current and lifetime comorbidity of the DSM-IV anxiety and mood disorders in a large clinical sample. J Abnorm Psychol. 2001;110:585. doi: 10.1037//0021-843x.110.4.585. [DOI] [PubMed] [Google Scholar]
- Buttorff C, Hock RS, Weiss HA, Naik S, Araya R, et al. Economic evaluation of a task-shifting intervention for common mental disorders in India. Bull World Health Organ. 2012;90:813–21. doi: 10.2471/BLT.12.104133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chatterjee S, Chowdhary N, Pednekar S, Cohen A, Andrew G, et al. Integrating evidence-based treatments for common mental disorders in routine primary care: feasibility and acceptability of the MANAS intervention in Goa, India. World Psychiatry. 2008;7:39–46. doi: 10.1002/j.2051-5545.2008.tb00151.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen C-H, Tseng Y-F, Chou F-H, Wang S-Y. Effects of support group intervention in postnatally distressed women: a controlled study in Taiwan. J Psychosom Res. 2000;49:395–99. doi: 10.1016/s0022-3999(00)00180-x. [DOI] [PubMed] [Google Scholar]
- Chibanda D, Mesu P, Kajawu L, Cowan F, Araya R, Abas MA. Problem-solving therapy for depression and common mental disorders in Zimbabwe: piloting a task-shifting primary mental health care intervention in a population with a high prevalence of people living with HIV. BMC Public Health. 2011;11:828. doi: 10.1186/1471-2458-11-828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chibanda D, Shetty AK, Tshimanga M, Woelk G, Stranix-Chibanda L, Rusakaniko S. Group problemsolving therapy for postnatal depression among HIV-positive and HIV-negative mothers in Zimbabwe. J Int Assoc Provid AIDS Care. 2014;13:335–41. doi: 10.1177/2325957413495564. [DOI] [PubMed] [Google Scholar]
- Chibanda D, Weiss HA, Verhey R, Simms V, Munjoma R, et al. Effect of a primary care–based psychological intervention on symptoms of common mental disorders in Zimbabwe: a randomized clinical trial. JAMA. 2016;316:2618–26. doi: 10.1001/jama.2016.19102. [DOI] [PubMed] [Google Scholar]
- Chisholm D, Sweeny K, Sheehan P, Rasmussen B, Smit F, et al. Scaling-up treatment of depression and anxiety: a global return on investment analysis. Lancet Psychiatry. 2016;3:415–24. doi: 10.1016/S2215-0366(16)30024-4. [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Becker KD, Daleiden EL, Hamilton JD. Understanding the common elements of evidence-based practice. J Am Acad Child Adolesc Psychiatry. 2007;46:647–52. doi: 10.1097/chi.0b013e318033ff71. [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Daleiden EL. Mapping evidence-based treatments for children and adolescents: application of the distillation and matching model to 615 treatments from 322 randomized trials. J Consult Clin Psychol. 2009;77:566–79. doi: 10.1037/a0014565. [DOI] [PubMed] [Google Scholar]
- Chowdhary N, Sikander S, Atif N, Singh N, Ahmad I, et al. The content and delivery of psychological interventions for perinatal depression by non-specialist health workers in low and middle income countries: a systematic review. Best Pract Res Clin Obstet Gynaecol. 2014;28:113–33. doi: 10.1016/j.bpobgyn.2013.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke K, King M, Prost A. Psychosocial interventions for perinatal commonmental disorders delivered by providers who are not mental health specialists in low- and middle-income countries: a systematic review and meta-analysis. PLOS Med. 2013;10:e1001541. doi: 10.1371/journal.pmed.1001541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cochrane Collab. Review Manager 5 (RevMan 5): version 5.3. 2014 http://tech.cochrane.org/revman.
- Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression: development of the 10-item Edinburgh Postnatal Depression Scale. Brit J Psychiatry. 1987;150:782–86. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- Cronbach LJ. Internal consistency of tests: analyses old and new. Psychometrika. 1988;53:63–70. [Google Scholar]
- Cuijpers P, Driessen E, Hollon SD, van Oppen P, Barth J, Andersson G. The efficacy of non-directive supportive therapy for adult depression: a meta-analysis. Clin Psychol Rev. 2012;32:280–91. doi: 10.1016/j.cpr.2012.01.003. [DOI] [PubMed] [Google Scholar]
- Derogatis LR, Lipman RS, Rickels K, Uhlenhuth EH, Covi L. The Hopkins Symptom Checklist (HSCL): a self-report symptom inventory. Behav Sci. 1974;19:1–15. doi: 10.1002/bs.3830190102. [DOI] [PubMed] [Google Scholar]
- Dickens C, Cherrington A, Adeyemi I, Roughley K, Bower P, et al. Characteristics of psychological interventions that improve depression in people with coronary heart disease: a systematic review and meta-regression. Psychosom Med. 2013;75:211–21. doi: 10.1097/PSY.0b013e31827ac009. [DOI] [PubMed] [Google Scholar]
- Duncan BL, Miller SD, Wampold BE, Hubble MA, editors. The Heart and Soul of Change: Delivering What Works in Therapy. Washington, DC: Am. Psychol. Assoc; 2010. [Google Scholar]
- Dybdahl R. Children and mothers in war: an outcome study of a psychosocial intervention program. Child Dev. 2001;72:1214–30. doi: 10.1111/1467-8624.00343. [DOI] [PubMed] [Google Scholar]
- Dybdahl R, Pasagic I. Traumatic experiences and psychological reactions among women in Bosnia during the war. Medicine Confl Surviv. 2000;16:281–90. doi: 10.1080/13623690008409525. [DOI] [PubMed] [Google Scholar]
- England MJ, Butler AS, Gonzalez ML Comm. Dev. Evidence-Based Stand. Psychos. Interv. Ment. Disord. Inst. Medicine Board Health Sci. Policy. Psychosocial Interventions for Mental and Substance Use Disorders: A Framework for Establishing Evidence-Based Standards. Washington, DC: Natl. Acad. Press; 2015. [PubMed] [Google Scholar]
- Fairburn CG, Cooper Z. Therapist competence, therapy quality, and therapist training. Behav Res Ther. 2011;49:373–78. doi: 10.1016/j.brat.2011.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn CG, Patel V. The global dissemination of psychological treatments: a road map for research and practice. Am J Psychiatry. 2014;171(5):124–26. doi: 10.1176/appi.ajp.2013.13111546. [DOI] [PubMed] [Google Scholar]
- Farchione TJ, Bullis JR. Addressing the global burden of mental illness: why transdiagnostic and common elements approaches to evidence-based practice might be our best bet. Cogn Behav Pract. 2014;21:124–26. [Google Scholar]
- Ferrari AJ, Charlson FJ, Norman RE, Patten SB, Freedman G, et al. Burden of depressive disorders by country, sex, age, and year: findings from the global burden of disease study 2010. PLOS Med. 2013;10:e1001547. doi: 10.1371/journal.pmed.1001547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fritsch R, Araya R, Solis J, Montt E, Pilowsky D, Rojas G. A randomized trial of pharmacotherapy with telephone monitoring to improve treatment of depression in primary care in Santiago, Chile. Rev Med Chil. 2007;135:587–95. [PubMed] [Google Scholar]
- Gao LL, Chan SW, Li X, Chen S, Hao Y. Evaluation of an interpersonal-psychotherapy-oriented childbirth education programme for Chinese first-time childbearing women: a randomised controlled trial. Int J Nurs Stud. 2010;47:1208–16. doi: 10.1016/j.ijnurstu.2010.03.002. [DOI] [PubMed] [Google Scholar]
- Gao LL, Luo Sy, Chan SWC. Interpersonal psychotherapy-oriented program for Chinese pregnant women: delivery, content, and personal impact. Nurs Health Sci. 2012;14:318–24. doi: 10.1111/j.1442-2018.2012.00722.x. [DOI] [PubMed] [Google Scholar]
- Gao LL, Sun K, Chan SW-C. Social support and parenting self-efficacy among Chinese women in the perinatal period. Midwifery. 2014;30:532–38. doi: 10.1016/j.midw.2013.06.007. [DOI] [PubMed] [Google Scholar]
- Gao LL, Xie W, Yang X, Chan SW-C. Effects of an interpersonal-psychotherapy-oriented postnatal programme for Chinese first-time mothers: a randomized controlled trial. Int J Nurs Stud. 2015;52:22–29. doi: 10.1016/j.ijnurstu.2014.06.006. [DOI] [PubMed] [Google Scholar]
- Gul A, Ali B. The onset and duration of benefit from counselling by minimally trained counsellors on anxiety and depression in women. J Pak Med Assoc. 2004;54:549–52. [PubMed] [Google Scholar]
- Hall BJ, Bolton PA, Annan J, Kaysen D, Robinette K, et al. The effect of cognitive therapy on structural social capital: results from a randomized controlled trial among sexual violence survivors in the Democratic Republic of the Congo. Am J Public Health. 2014;104:1680–86. doi: 10.2105/AJPH.2014.301981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes RJ, Moulton LH. Cluster Randomised Trials. London: CRC Press; 2009. [Google Scholar]
- Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinton DE, Kirmayer LJ. Local responses to trauma: symptom, affect, and healing. Transcult Psychiatry. 2013;50:607–21. doi: 10.1177/1363461513506529. [DOI] [PubMed] [Google Scholar]
- Hirani SS, Karmaliani R, McFarlane J, Asad N, Madhani F, Shehzad S. Testing a community derived intervention to promote women’s health: preliminary results of a 3-arm randomized controlled trial in Karachi. South Online J Nurs Res. 2010a;10:6. http://www.resourcenter.net/images/snrs/files/sojnr_articles2/Vol10Num03Art06.html. [Google Scholar]
- Hirani SS, Karmaliani R, McFarlane J, Asad N, Madhani F, et al. Development of an economic skill building intervention to promotewomen’s safety and child development in Karachi, Pakistan. Issues Mental Health Nurs. 2010b;31:82–88. doi: 10.3109/01612840903254859. [DOI] [PubMed] [Google Scholar]
- Ho SM, Heh SS, Jevitt CM, Huang LH, Fu YY, Wang LL. Effectiveness of a discharge education program in reducing the severity of postpartum depression: a randomized controlled evaluation study. Patient Educ Couns. 2009;77:68–71. doi: 10.1016/j.pec.2009.01.009. [DOI] [PubMed] [Google Scholar]
- Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ. 2014;348:g1687. doi: 10.1136/bmj.g1687. [DOI] [PubMed] [Google Scholar]
- Huhn M, Tardy M, Spineli LM, Kissling W, Förstl H, et al. Efficacy of pharmacotherapy and psychotherapy for adult psychiatric disorders: a systematic overview of meta-analyses. JAMA Psychiatry. 2014;71:706–15. doi: 10.1001/jamapsychiatry.2014.112. [DOI] [PubMed] [Google Scholar]
- Kaaya SF, Blander J, Antelman G, Cyprian F, Emmons KM, et al. Randomized controlled trial evaluating the effect of an interactive group counseling intervention for HIV-positive women on prenatal depression and disclosure of HIV status. AIDS Care. 2013;25:854–62. doi: 10.1080/09540121.2013.763891. [DOI] [PubMed] [Google Scholar]
- Kaehler LA, Jacobs M, Jones DJ. Distilling common history and practice elements to inform dissemination: Hanf-Model BPT programs as an example. Clin Child Fam Psychol Rev. 2016;19:236–58. doi: 10.1007/s10567-016-0210-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazdin AE. Closing the research–practice gap: how, why, and whether. Clin Psychol. 2016;23:201–6. [Google Scholar]
- Kazdin AE, Blase SL. Rebooting psychotherapy research and practice to reduce the burden of mental illness. Perspect Psychol Sci. 2011;6:21–37. doi: 10.1177/1745691610393527. [DOI] [PubMed] [Google Scholar]
- Kendler KS. Major depression and generalised anxiety disorder same genes, (partly) different environments—revisited. Br J Psychiatry. 1996;30:68–75. [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kohrt BA, Jordans MJD, Rai S, Shrestha P, Luitel NP, et al. Therapist competence in global mental health: development of the ENhancing Assessment of Common Therapeutic factors (ENACT) rating scale. Behav Res Ther. 2015;69:11–21. doi: 10.1016/j.brat.2015.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leijten P, Melendez-Torres G, Knerr W, Gardner F. Transported versus homegrown parenting interventions for reducing disruptive child behavior: a multilevel meta-regression study. J Am Acad Child Adolesc Psychiatry. 2016;55(7):610–17. doi: 10.1016/j.jaac.2016.05.003. [DOI] [PubMed] [Google Scholar]
- Maes K, Kalofonos I. Becoming and remaining community health workers: perspectives from Ethiopia and Mozambique. Soc Sci Med. 2013;87:52–59. doi: 10.1016/j.socscimed.2013.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magidson J, Lejuez C, Kamal T, Blevins E, Murray L, et al. Adaptation of community health worker–delivered behavioral activation for torture survivors in Kurdistan, Iraq. Glob Mental Health. 2015;2:e24. doi: 10.1017/gmh.2015.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHugh RK, Murray HW, Barlow DH. Balancing fidelity and adaptation in the dissemination of empirically-supported treatments: the promise of transdiagnostic interventions. Behav Res Ther. 2009;47:946–53. doi: 10.1016/j.brat.2009.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendenhall E, De Silva MJ, Hanlon C, Petersen I, Shidhaye R, et al. Acceptability and feasibility of using non-specialist health workers to deliver mental health care: stakeholder perceptions from the PRIME district sites in Ethiopia, India, Nepal, South Africa, and Uganda. Soc Sci Med. 2014;118:33–42. doi: 10.1016/j.socscimed.2014.07.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michie S, Richardson M, Johnston M, Abraham C, Francis J, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med. 2013;46:81–95. doi: 10.1007/s12160-013-9486-6. [DOI] [PubMed] [Google Scholar]
- Milani HS, Azargashb E, Beyraghi N, Defaie S, Asbaghi T. Effect of telephone-based support on postpartum depression: a randomized controlled trial. Int J Fertil Steril. 2015;9:247–53. doi: 10.22074/ijfs.2015.4246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:264–69. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- Mollica RF, Caspi-Yavin Y, Bollini P, Truong T, Tor S, Lavelle J. The Harvard Trauma Questionnaire: validating a cross-cultural instrument for measuring torture, trauma, and posttraumatic stress disorder in Indochinese refugees. J Nerv Ment Dis. 1992;180:111–16. [PubMed] [Google Scholar]
- Murray LK, Dorsey S, Haroz E, Lee C, Alsiary MM, et al. A common elements treatment approach for adult mental health problems in low- and middle-income countries. Cogn Behav Pract. 2014;21:111–23. doi: 10.1016/j.cbpra.2013.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray LK, Jordans M. Rethinking the service delivery system of psychological interventions in low and middle income countries. BMC Psychiatry. 2016;16:234. doi: 10.1186/s12888-016-0938-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naeem S, Ali B, Mubeen S, Iqbal A. The transformative effect of training in counselling and its application, on the community counsellors themselves. J Pak Med Assoc. 2003;53:388–90. [PubMed] [Google Scholar]
- Nayak MB, Patel V, Bond JC, Greenfield TK. Partner alcohol use, violence and women’s mental health: population-based survey in India. Br J Psychiatry. 2010;196:192–99. doi: 10.1192/bjp.bp.109.068049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel V, Chisholm D, Parikh R, Charlson FJ, Degenhardt L, et al. Addressing the burden of mental, neurological, and substance use disorders: key messages from Disease Control Priorities, 3rd edition. Lancet. 2016a;387:1672–85. doi: 10.1016/S0140-6736(15)00390-6. [DOI] [PubMed] [Google Scholar]
- Patel V, Weiss HA, Chowdhary N, Naik S, Pednekar S, et al. Effectiveness of an intervention led by lay health counsellors for depressive and anxiety disorders in primary care in Goa, India (MANAS): a cluster randomised controlled trial. Lancet. 2010;376:2086–95. doi: 10.1016/S0140-6736(10)61508-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel V, Weobong B, Weiss HA, Anand A, Bhat B, et al. The Healthy Activity Program (HAP), a lay counsellor-delivered brief psychological treatment for severe depression, in primary care in India: a randomised controlled trial. Lancet. 2017;389:176–85. doi: 10.1016/S0140-6736(16)31589-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel V, Xiao S, Chen H, Hanna F, Jotheeswaran A, et al. The magnitude of and health system responses to the mental health treatment gap in adults in India and China. Lancet. 2016b;388:3074–84. doi: 10.1016/S0140-6736(16)00160-4. [DOI] [PubMed] [Google Scholar]
- PracticeWise. Psychosocial and combined treatments coding manual. Satellite Beach, FL: PracticeWise; 2015. [Google Scholar]
- Rahman A. Challenges and opportunities in developing a psychological intervention for perinatal depression in rural Pakistan—a multi-method study. Arch Women’s Mental Health. 2007;10:211–19. doi: 10.1007/s00737-007-0193-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman A, Creed F. Outcome of prenatal depression and risk factors associated with persistence in the first postnatal year: prospective study from Rawalpindi, Pakistan. J Affect Disord. 2007;100:115–21. doi: 10.1016/j.jad.2006.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman A, Fisher J, Bower P, Luchters S, Tran T, et al. Interventions for common perinatal mental disorders in women in low- and middle-income countries: a systematic review and meta-analysis. Bull World Health Organ. 2013;91:593–601I. doi: 10.2471/BLT.12.109819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman A, Hamdani SU, Awan NR, Bryant RA, Dawson KS, et al. Effect of a multicomponent behavioral intervention in adults impaired by psychological distress in a conflict-affected area of Pakistan: a randomized clinical trial. JAMA. 2016;316:2609–17. doi: 10.1001/jama.2016.17165. [DOI] [PubMed] [Google Scholar]
- Rahman A, Malik A, Sikander S, Roberts C, Creed F. Cognitive behaviour therapy–based intervention by community health workers for mothers with depression and their infants in rural Pakistan: a cluster randomised controlled trial. Lancet. 2008;372:902–9. doi: 10.1016/S0140-6736(08)61400-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richter L, Rotheram-Borus MJ, Van Heerden A, Stein A, Tomlinson M, et al. Pregnant women living with HIV (WLH) supported at clinics by peer WLH: a cluster randomized controlled trial. AIDS Behav. 2014;18:706–15. doi: 10.1007/s10461-014-0694-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rojas G, Fritsch R, Solis J, Jadresic E, Castillo C, et al. Treatment of postnatal depression in low-income mothers in primary-care clinics in Santiago, Chile: a randomised controlled trial. Lancet. 2007;370:1629–37. doi: 10.1016/S0140-6736(07)61685-7. [DOI] [PubMed] [Google Scholar]
- Rotheram-Borus M-J, Richter L, Van Rooyen H, Van Heerden A, Tomlinson M, et al. Project Masihambisane: a cluster randomised controlled trial with peer mentors to improve outcomes for pregnant mothers living with HIV. Trials. 2011;12:2. doi: 10.1186/1745-6215-12-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotheram-Borus MJ, Tomlinson M, le Roux IM, Harwood JM, Comulada S, et al. A cluster randomised controlled effectiveness trial evaluating perinatal home visiting among South African mothers/infants. PLoS One. 2014;9:e105934. doi: 10.1371/journal.pone.0105934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAS Institute Inc. SAS/STAT 9.3. Cary, North Carolina: SAS Inst; 2011. [Google Scholar]
- Semrau M, Evans-Lacko S, Koschorke M, Ashenafi L, Thornicroft G. Stigma and discrimination related to mental illness in low- and middle-income countries. Epidemiology Psychiatr Sci. 2015;24:382–94. doi: 10.1017/S2045796015000359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seyed-Alinaghi S, Jam S, Foroughi M, Imani A, Mohraz M, et al. Randomized controlled trial of mindfulness-based stress reduction delivered to human immunodeficiency virus-positive patients in Iran: effects on CD4+ T lymphocyte count and medical and psychological symptoms. Psychosom Med. 2012;74:620. doi: 10.1097/PSY.0b013e31825abfaa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singla DR, Kumbakumba E. The development and implementation of a theory-informed, integrated mother–child intervention in rural Uganda. Soc Sci Med. 2015;47:242–51. doi: 10.1016/j.socscimed.2015.10.069. [DOI] [PubMed] [Google Scholar]
- Singla DR, Kumbakumba E, Aboud FE. Effects of a parenting intervention to address maternal psychological well being and child development and growth in rural Uganda: a community-based, cluster randomised trial. Lancet Glob Health. 2015;3:e458–69. doi: 10.1016/S2214-109X(15)00099-6. [DOI] [PubMed] [Google Scholar]
- Singla DR, Lazarus A, Atif N, Sikander S, Bhatia U, et al. “Someone like us”: Delivering maternal mental health through peers in two South Asian contexts. J Affect Disord. 2014a;168:452–58. doi: 10.1016/j.jad.2014.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singla DR, Weobong B, Nadkarni A, Chowdhary N, Shinde S, et al. Improving the scalability of psychological treatments in developing countries: an evaluation of peer-led therapy quality assessment in Goa, India. Behav Res Ther. 2014b;60:53–59. doi: 10.1016/j.brat.2014.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steel Z, Chey T, Silove D, Marnane C, Bryant RA, Van Ommeren M. Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement: a systematic review and meta-analysis. JAMA. 2009;302:537–49. doi: 10.1001/jama.2009.1132. [DOI] [PubMed] [Google Scholar]
- Steel Z, Marnane C, Iranpour C, Chey T, Jackson JW, et al. The global prevalence of common mental disorders: a systematic review and meta-analysis 1980–2013. Int J Epidemiology. 2014;43:476–93. doi: 10.1093/ije/dyu038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiwari A, Fong DYT, Yuen KH, Yuk H, Pang P, et al. Effect of an advocacy intervention on mental health in Chinese women survivors of intimate partner violence: a randomized controlled trial. JAMA. 2010;304:536–43. doi: 10.1001/jama.2010.1052. [DOI] [PubMed] [Google Scholar]
- van der Waerden JE, Hoefnagels C, Hosman CM. Psychosocial preventive interventions to reduce depressive symptoms in low-SES women at risk: a meta-analysis. J Affect Disord. 2011;128:10–23. doi: 10.1016/j.jad.2010.02.137. [DOI] [PubMed] [Google Scholar]
- van Ginneken N, Tharyan P, Lewin S, Rao GN, Meera S, et al. Non-specialist health worker interventions for the care of mental, neurological and substance-abuse disorders in low-and middle-income countries. Cochrane Database Syst Rev. 2013;19(11):CD009149. doi: 10.1002/14651858.CD009149.pub2. [DOI] [PubMed] [Google Scholar]
- van’t Hof E, Cuijpers P, Waheed W, Stein DJ. Psychological treatments for depression and anxiety disorders in low- and middle-income countries: a meta-analysis. Afr J Psychiatry. 2011;14:200–7. doi: 10.4314/ajpsy.v14i3.2. [DOI] [PubMed] [Google Scholar]
- Verdeli H, Clougherty K, Bolton P, Speelman L, Lincoln N, et al. Adapting group interpersonal psychotherapy for a developing country: experience in rural Uganda. World Psychiatry. 2003;2:114–20. [PMC free article] [PubMed] [Google Scholar]
- Wampold BE. How important are the common factors in psychotherapy? An update. World Psychiatry. 2015;14:270–77. doi: 10.1002/wps.20238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webb CA, DeRubeis RJ, Barber JP. Therapist adherence/competence and treatment outcome: a metaanalytic review. J Consult Clin Psychol. 2010;78:200–11. doi: 10.1037/a0018912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss WM, Murray LK, Zangana GAS, Mahmooth Z, Kaysen D, et al. Community-based mental health treatments for survivors of torture and militant attacks in Southern Iraq: a randomized control trial. BMC Psychiatry. 2015;15:249. doi: 10.1186/s12888-015-0622-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss WM, Ugueto AM, Mahmooth Z, Murray LK, Hall BJ, et al. Mental health interventions and priorities for research for adult survivors of torture and systematic violence: a review of the literature. Torture. 2016;26:17–44. [PubMed] [Google Scholar]
- Weisz JR, Chorpita BF, Palinkas LA, Schoenwald SK, Miranda J, et al. Testing standard and modular designs for psychotherapy treating depression, anxiety, and conduct problems in youth: a randomized effectiveness trial. Arch Gen Psychiatry. 2012;69:274–82. doi: 10.1001/archgenpsychiatry.2011.147. [DOI] [PubMed] [Google Scholar]
- Whiteford HA, Degenhardt L, Rehm J, Baxter AJ, Ferrari AJ, et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet. 2013;382:1575–86. doi: 10.1016/S0140-6736(13)61611-6. [DOI] [PubMed] [Google Scholar]
- Whiteford HA, Ferrari AJ, Degenhardt L, Feigin V, Vos T. The global burden of mental, neurological and substance use disorders: an analysis from the Global Burden of Disease Study 2010. PLOS ONE. 2015;10:e0116820. doi: 10.1371/journal.pone.0116820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO (World Health Organ.) Task Shifting: Rational Redistribution of Tasks Among Health Workforce Teams: Global Recommendations and Guidelines. Geneva: WHO; 2008. [Google Scholar]
- WHO(World Health Organ.) Low-Intensity Psychological Interventions for People in Communities Affected by Adversity: A New Area of Mental Health and Psychosocial Work at WHO. Geneva: WHO; 2014a. [Google Scholar]
- WHO (World Health Organ.) Preventing Suicide: A Global Imperative. Geneva: WHO; 2014b. [Google Scholar]
- WHO (World Health Organ.) mhGAP Humanitarian Intervention Guide (mhGAP-HIG): Clinical Management of Mental, Neurological and Substance Use Conditions in Humanitarian Emergencies. Geneva: WHO; 2015. [Google Scholar]
- World Bank Group. World Bank Country and Data Groups. World Bank; Washington, DC: 2015. [Accessed Oct 15]. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-countryand-lending-groups. [Google Scholar]
- Wijesinghe CA, Williams SS, Kasturiratne A, Dolawaththa N, Wimalaratne P, et al. A randomized controlled trial of a brief intervention for delayed psychological effects in snakebite victims. PLoS Negl Trop Dis. 2015;9:e0003989. doi: 10.1371/journal.pntd.0003989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeomans PD, Forman EM, Herbert JD, Yuen E. A randomized trial of a reconciliation workshop with and without PTSD psychoeducation in Burundian sample. J Trauma Stress. 2010;23:305–12. doi: 10.1002/jts.20531. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.