Abstract
BACKGROUND AND PURPOSE:
Men have a greater prevalence of high-risk carotid plaque features associated with stroke compared with women who have ≥50% stenosis, but little is known about these features in less significantly stenotic carotid arteries. This study aims to evaluate sex differences in complicated carotid plaque features in asymptomatic patients with <50% stenosis.
MATERIALS AND METHODS:
Ninety-six patients (50 men, 46 women) with <50% carotid stenosis on MRA who had been referred for analysis of contralateral >50% carotid stenosis were included. The associations between sex and plaque features as identified by 3T MR carotid plaque imaging were examined by using logistic and linear regression models controlling for demographic characteristics, MRA stenosis, and the presence of contralateral plaque features.
RESULTS:
The presence of a thin/ruptured fibrous cap (16% versus 2%, adjusted odds ratio = 8.57, P = .047), IPH (24% versus 6%, adjusted odds ratio = 4.53, P = .027), and American Heart Association type VI plaque (26% versus 6%, adjusted odds ratio = 5.04, P = .017) was significantly higher in men than in women. These associations remained significant following adjustment for contralateral plaque features. Men demonstrated a larger percentage volume of LR/NC (median, 1.66% versus −0.21%; P < .01). Calcification was not significantly associated with sex.
CONCLUSIONS:
There is a sex difference of higher risk carotid plaque features during the early stage of disease seen in patients recruited for MR imaging evaluation of contralateral moderate-to-severe stenosis. Given the potential of using LR/NC without or with IPH to monitor therapy, these results indicate the possible importance of sex-based management in patients with asymptomatic carotid atherosclerosis across all stages of carotid stenosis.
Histopathologic studies suggest that vulnerable plaques are characterized by the presence of a large LR/NC with a thin or ruptured fibrous cap and IPH.1,2 The American Heart Association has classified these plaques as complicated or type VI.3 MR imaging can accurately identify these carotid plaque components and classify carotid plaque according to the American Heart Association guidelines.4–6 High-risk carotid atherosclerotic plaque identified with in vivo MR imaging has recently been shown to correlate with future ipsilateral carotid stroke or transient ischemic attacks.7,8
Multiple studies have shown an increased incidence of stroke in men compared with women with moderate-severe carotid stenosis.9,10 A subgroup analysis of relevant trial data has shown that the benefit of carotid endarterectomy in symptomatic and asymptomatic severe carotid stenosis is less in women than in men.11 In a recent study of asymptomatic patients with ≥50% stenosis, in vivo MR imaging detected higher risk plaque features in men compared with women after controlling for potential confounders.12 The increased incidence of high-risk carotid plaque features in men compared with women may help explain sex differences in stroke incidence and treatment prevention in patients with ≥50% stenosis.
While these studies indicate a higher prevalence of a large LR/NC, thin/ruptured fibrous cap, and IPH in men than women with moderate-to-severe stenosis, little is known about the sex differences of these high-risk carotid plaque features in patients with mild carotid or no stenosis. This group of patients is important because of the opportunity to intervene with aggressive medical therapy early in the course of the disease and before the patients develop more severe carotid stenosis. While LR/NC occurs more frequently in patients with ≥50% stenosis, a recent study showed that the LR/NC was present in 58% of patients with asymptomatic mild stenosis.5 MR imaging has the ability to depict LR/NC size, which serves as a good carotid atherosclerotic score, which was shown to be associated with more complex plaque features such as ruptured fibrous cap or IPH and can be an effective complementary strategy to stenosis for classifying carotid atherosclerotic disease severity.13 MR imaging has also shown the ability to detect a decrease in LR/NC with aggressive statin therapy but only when an LR/NC was present at the initiation of therapy.14 It would, therefore, be useful to understand sex-based differences in carotid plaque components, especially LR/NC in patients with <50% carotid stenosis because knowledge of these components might affect the choice of medical therapy.
The aim of this study was to evaluate sex differences in the prevalence of complicated carotid plaque characteristics in asymptomatic patients with <50% stenosis who were referred by subspecialist stroke neurologists or vascular surgeons for carotid plaque MR imaging of known contralateral moderate-to-severe carotid stenosis. The presence of significant contralateral carotid stenosis may increase the prevalence of complicated carotid plaque components in these asymptomatic patients with <50% stenosis compared with patients demonstrating isolated unilateral carotid stenosis.
Materials and Methods
The study procedures were approved by the Community Research Institutional Review Board (Michigan State University, East Lansing, Michigan), and informed consent was obtained from all patients.
Subjects
Between March 2006 and October 2011, one hundred fifty-eight patients (89 men, 69 women) were referred to the Department of Radiology (Michigan State University) for evaluation of asymptomatic moderate or severe carotid stenosis by 3T MR imaging. Eighty-nine percent were referred from a vascular surgery clinic with the remainder from either neurology or cardiology outpatient services. The vascular surgeons, neurologists, and cardiologists approached all their patients with documented asymptomatic carotid stenosis about participation in this study. The analysis of the asymptomatic moderate or severe carotid stenosis has been previously reported.12 The current study evaluates the contralateral carotid bifurcation from this prior study.12 Inclusion/exclusion criteria were the following: 1) complete occlusion, prior carotid endarterectomy, or >50% stenosis involving the index carotid artery; 2) no history of stroke, transient ischemic attack, or amaurosis fugax in the distribution of either carotid artery within 4 months before enrollment; and 3) contraindications for MR imaging. Baseline clinical characteristics, including sex, age, race, body mass index, and history of hyperlipidemia, hypertension, diabetes, coronary artery disease, peripheral artery disease, statin use, and smoking, were collected by the referring physicians.
MR Imaging Protocol
Patients were imaged with a 3T whole-body scanner (Signa Excite; GE Healthcare, Milwaukee, Wisconsin) and a research 4-channel phased-array surface coil (Pathway MR Imaging, Seattle, Washington). Bilateral carotid plaque multicontrast imaging protocol included the following 5 sequences: TOF MRA, black-blood precontrast T1WI, T2WI, IR-FSPGR, and CE-T1WI performed 5 minutes after intravenous infusion of 0.15 mmol of gadobenate dimeglumine (MultiHance; Bracco Diagnostic, Princeton, New Jersey) per kilogram of body weight at rate of 3 mL/s. The 5 sequences were obtained on the basis of previously published protocols for a 3T scanner (On-line Table 1).6,15,16 After intravenous bolus contrast injection, very-high-resolution (0.28 mm3) coronal elliptic-centric carotid contrast-enhanced MRA was performed with a test bolus to time the contrast arrival.17 Approximate scanning time, including patient preparation, was 45 minutes.
MR Image Review
Two experienced reviewers who were blinded to clinical outcome reviewed all MR images, and a consensus decision was reached for each plaque feature as has been previously described.7 In brief, each reviewer primarily analyzed half of the cases and was peer-reviewed by the other reviewer. In cases in which there was disagreement between the primary and peer review, consensus agreement was reached after discussion. The quality of the overall images was scored by using an image-quality score rated on a 4-point scale (1 = poor, 4 = excellent). Arteries with an average image quality of 1 were excluded from the study.16
The extracranial carotid bifurcation level was used as a landmark for matching the 5 different weightings. Areas of the lumen, wall, and plaque components (LR/NC, IPH, and calcifications) were manually outlined. These plaque components were identified on the basis of histologically validated criteria.4,6 Details of the criteria are as follows: Lipid-rich necrotic core without hemorrhage is isointense on TOF and T1WI and hypointense on CE-T1WI and T2WI; calcification shows hypointensity on all the image weightings; and hemorrhage appears hyperintense on IR-FSPGR, TOF, and T1WI and can be hypointense to hyperintense on T2WI.
When an LR/NC was identified, the fibrous cap status was categorized as either a “thick” or “thin/ruptured” fibrous cap by using histologically validated criteria.18 Intact thick fibrous caps showed a uniform dark band adjacent to the lumen on TOF, an enhanced band adjacent to the lumen on CE-T1WI, and a smooth luminal surface on all the images. Intact thin caps showed no visible dark band adjacent to the lumen on TOF, no visible enhanced band adjacent to the lumen on CE-T1WI, and a smooth luminal surface on all the images. Ruptured fibrous cap showed a disrupted dark band or no visible dark band adjacent to the lumen on TOF, an irregular luminal surface on all the images, and a hyperintense area adjacent to the lumen on TOF images. Area measurements were obtained by using an imaging-analysis tool for carotid plaque MR imaging (MRI-Plaque View; VP Diagnostics, Seattle, Washington).
Last, 2 experienced reviewers, blinded to clinical information and carotid plaque findings, evaluated the level and degree of stenosis. The measurement of percentage diameter carotid stenosis was based on the North American Symptomatic Carotid Endarterectomy Trial criteria, using the high-resolution carotid contrast-enhanced MRA on multiplanar reformations generated by using a 3D workstation (Advantage Windows, Version 4.3; GE Healthcare).17
Statistical Analysis
Descriptive frequencies for categoric carotid plaque variables as well as means and medians (interquartile range) for continuous carotid plaque variables were generated. Sex differences in baseline clinical characteristics and MR angiographic findings were tested by using χ2 analysis or t tests. A logistic regression analysis was used to compare fibrous cap status (presence or absence of thin/ruptured fibrous cap) between the sexes. A 2-part model19 was fit to examine sex differences in the presence and size of the other plaque components, including LR/NC, IPH, and calcifications. In the first part of this model, the presence/absence of a plaque component was evaluated by using logistic regression analysis. In the second part, only subjects with values for component volumes (ie, values >0) were modeled by using linear regression analysis. Natural log transformations were performed for all percentage volume data because they were positively skewed.
Baseline characteristics demonstrating an association with sex (P < .20) were considered as potential confounding factors and included in subsequent multivariable analyses. Variables were selected into the final multivariable model by using a stepwise backward-selection method (P > .10 for removal from the model). Results were expressed as adjusted odds ratios with 95% confidence intervals for logistic regression models and as regression coefficients with 95% confidence intervals for linear regression models. The regression coefficients from the linear models indicated the increase in the log percentage volume in men versus women for each component. P < .05 was used to designate statistical significance in the multivariable models. Computation was performed by using the Statistical Package for the Social Sciences, Version 17.0 (SPSS, Chicago, Illinois).
Because of the potential that within each patient, the lesion characteristics identified in the ipsilateral <50% stenosis of the carotid artery are correlated with the contralateral >50% stenosis of the carotid artery, we undertook a sensitivity analysis in which we repeated the final multivariable models after adjusting for the presence of the identical lesion in the contralateral vessel.
Results
Of the 158 patients referred for 3T MR imaging, 62 of the 158 index carotid arteries were excluded due to poor image quality (n = 9), carotid artery occlusion (n = 14), prior carotid artery stent placement (n =1), prior carotid endarterectomy (n = 19), or stenosis >50% (n =19). Of the final 96 patients, there were 50 men and 46 women. Of their baseline clinical characteristics, the presence of hyperlipidemia (P = .1999), peripheral arterial disease (P = .11), coronary artery disease (P = .08), and statin use (P = .12) was noted more commonly in men than in women; men tended to be older (P = .07) than women. These 5 variables were selected as potential confounders in the multivariable model (On-line Table 2).
In Tables 1 and 2, the odds ratios in the univariate and the adjusted odds ratios in the multivariable models are reported for the presence of a thin/ruptured fibrous cap, LR/NC, IPH, and calcifications. For the presence of a thin/ruptured fibrous cap, odds ratios in the univariate and multivariable models remained unchanged because none of the 5 potential confounders remained in the final model. For the presence of LR/NC, statin use (adjusted odds ratio = 0.17; 95% confidence level, 0.05–0.58; P < .01) was included in the final multivariable model. For the presence of IPH, odds ratios in the univariate and multivariable models remained unchanged because none of the 5 potential confounders remained in the final model. For the presence of calcification, age (adjusted odds ratio for 10% increase = 1.83; 95% confidence level, 1.05–3.18; P = .03) was included in the final multivariable model. For the presence of type VI plaque, odds ratios in the univariate and multivariable models remained unchanged because none of the 5 potential confounders remained in the final model.
Table 1:
Prevalence of plaque components in men and women
| Presence | Men |
Women |
Univariate Model |
Multivariable Model |
||||
|---|---|---|---|---|---|---|---|---|
| % | % | Odds Ratiosa | 95% Confidence Intervals | P | Adjusted Odds Ratiosa | 95% Confidence Intervals | P | |
| Thin/ruptured fibrous cap | 16 | 2 | 8.57 | 1.03–71.48 | .047 | 8.57 | 1.03–71.48 | .047b |
| LR/NC | 50 | 40 | 1.71 | 0.75–3.86 | .198 | 2.34 | 0.95–5.74 | .064c |
| IPH | 24 | 6 | 4.53 | 1.19–17.28 | .027 | 4.53 | 1.19–17.28 | .027b |
| Calcification | 86 | 70 | 2.69 | 0.97–7.42 | .057 | 2.28 | 0.80–6.50 | .123d |
| Type VI plaque | 26 | 6 | 5.04 | 1.33–19.04 | .017 | 5.04 | 1.33–19.04 | .017b |
Odds ratios or adjusted odds ratios by logistic regression analyses.
Model also includes none.
Model includes statin use.
Model includes age.
Table 2:
Percentage volume of plaque
| Log (% Volume)a | Men |
Women |
Univariate Model |
Multivariable Model |
||||
|---|---|---|---|---|---|---|---|---|
| Median (25th–75th) | Median (25th–75th) | Coefficient | 95% Confidence Intervals | P | Adjusted Coefficient | 95% Confidence Intervals | P | |
| LR/NC (n = 42) | 1.66 (0.52–2.12) | −0.21 (−0.50–0.54) | 1.28 | 0.55–2.02 | <.01 | 1.28 | 0.55–2.02 | <.01b |
| IPH (n = 15) | 0.48 (−0.48–1.17) | 0.72 (−1.15–−0.45) | 1.21 | −0.60–3.03 | .17 | 1.21 | −0.60–3.03 | .17b |
| Calcification (n = 75) | 0.87 (−0.17–1.91) | 0.70 (−0.08–1.67) | 0.12 | −0.45–0.69 | .68 | 0.44 | −0.51–0.59 | .874c |
Coefficients for log % volume of patients with the presence of individual plaque components by linear regression analyses.
Model also includes none.
Model also includes age.
The presence of a thin/ruptured fibrous cap, IPH, and type VI plaque was significantly higher in men than in women (Tables 1 and 2 and Figs 1 and 2). In the multivariable logistic regression analysis, the adjusted odds ratio for thin/ruptured fibrous cap was 8.57 (95% confidence level, 1.03–71.48; P = .047); for the presence of IPH, it was 4.53 (95% confidence level, 1.19–17.28; P = .027); and for the presence of type VI plaque, it was 5.04 (95% confidence level, 1.33–19.04; P = .017). The presence of LR/NC was higher in men than in women but did not reach statistical significance. However, the percentage volume of LR/NC was significantly higher in men than in women (Tables 1 and 2).
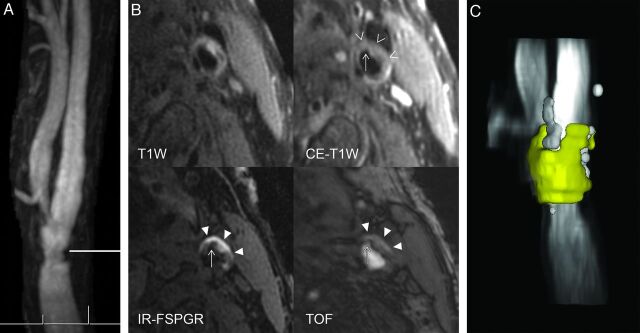
Fig 1.
A 75-year-old man with asymptomatic mild left carotid artery stenosis and complex carotid plaque. A, Maximum intensity projections from contrast-enhanced MRA show irregular narrowing of the distal left common carotid artery with stenosis of 33% diameter. The horizontal line indicates the level of transverse carotid plaque imaging. B, The chevrons demonstrate a large nonenhancing LR/NC region on CE-T1WI. Much of the LR/NC contains IPH seen as bright on IR-FSPGR and TOF. Last, a fibrous cap rupture with an ulcer penetrating into the hemorrhagic LR/NC is seen as depicted by the thin arrow. C, The large LR/NC is yellow, and calcifications are white on this volume-reformatted image generated from the multicontrast carotid plaque series. The total volume of LR/NC is 137 mL, and the percentage of the maximum area of LR/NC is 47%. Such large-volume LR/NC regions are frequently associated with other complex carotid plaque features such as IPH and/or fibrous cap rupture that correspond to American Heart Association type VI carotid plaque, which was found to occur significantly more often in men than in women.
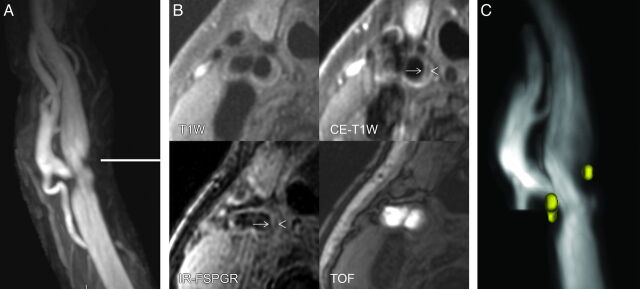
Fig 2.
A 74-year-old woman with asymptomatic mild right carotid stenosis and minimal LR/NC. A, Maximum intensity projection from contrast-enhanced MRA shows smooth narrowing of the distal right common carotid artery and proximal right internal carotid artery with a stenosis of 41% diameter. The horizontal line indicates the level of transverse carotid plaque imaging. B, The chevron demonstrates a small nonenhancing LR/NC region on CE-T1WI and IR-FSPGR. No high signal intensity on IR-FSPGR or TOF is seen to suggest IPH. The thin arrow demonstrates a thick and intact fibrous cap overlying the small deep LR/NC. These findings correspond to American Heart Association types IV and V carotid plaque. C, Two very small regions of LR/NC are seen as yellow in the volume-reformatted image generated from the multicontrast carotid plaque series. The total volume of LR/NC is 2 mL, and the percentage of maximum area of LR/NC is 8%. Women showed significantly smaller volumes of LR/NC and a significantly lower incidence of American Heart Association type VI carotid plaque compared with men in this study.
The results of the sensitivity analyses adjusting for contralateral lesions are shown in On-line Table 3. There were no major changes in the odds ratios for the sex differences, and the 3 significant associations (thin/ruptured fibrous cap, IPH, and type VI plaque) remained significant following adjustment.
When subjects having individual plaque components were examined, median (25th–75th percentile) percentage component volumes in men and women were 5.4% (3.4%–9.0%) versus 2.2% (1.3%–4.9%) for LR/NC, 1.6% (0.7%–3.2%) versus 0.49% (0.32%–0.64%) for IPH, and 2.4% (0.8%–6.7%) versus 2.0% (0.9%–5.3%) for calcifications, respectively.
The median with 25th and 75th of log percentage volumes for LR/NC, IPH, and calcifications in men and women is demonstrated in Tables 1 and 2. The size of the LR/NC was significantly larger in men than in women in both the univariate and multivariable models (Figs 1 and 2).
Discussion
The present study demonstrates that the sex difference in high-risk carotid plaque features such as the presence of thin or ruptured fibrous cap, IPH, American Heart Association type VI carotid plaque, and the size of the LR/NC recently documented in patients with moderate-to-severe carotid stenosis also occurs in patients with mild or no carotid stenosis, though at a lower incidence rate.
Given that these asymptomatic patients with <50% stenosis were referred by subspecialist stroke neurologists or vascular surgeons for carotid plaque MR imaging of known contralateral moderate-to-severe carotid stenosis, which had been previously reported,12 there is the potential for selection bias. With sensitivity analysis, the incidence of a thin/ruptured fibrous cap, IPH, and type VI plaque remained significantly higher in men compared with women, even when accounting for the presence of these complex plaque components in the contralateral carotid artery with more severe stenosis. The incidence of these complex carotid plaque components may be higher in this study due to selection bias compared with patients demonstrating isolated mild carotid stenosis.
Our current understanding of plaque biology suggests that the transition from an LR/NC with a thick intact cap (American Heart Association types IV and V) to a plaque with cap rupture (American Heart Association type VI) represents the transition from stable-to-unstable atherosclerotic disease.3 The current study extends our knowledge by revealing that 16% of men and 2% of women demonstrate a thin/ruptured fibrous cap while having only a 0%–49% carotid stenosis. It is well-documented that acute myocardial infarcts often occur in coronary arteries with <50% stenosis. It is possible that the presence of a thin/ruptured fibrous cap in patients with <50% stenosis, which occurs more often in men than women, may represent a complicated or “vulnerable” carotid plaque phenotype in patients thought to have little risk of future cerebrovascular events based on the presence of no or only mild carotid stenosis. In these patients, the carotid artery with no or mild stenosis may benefit from careful clinical follow-up in addition to the contralateral carotid artery with more severe stenosis.
Using a 3D T1-weighted fat-suppressed sequence to identify IPH, Cheung et al20 studied a group of symptomatic patients with ≤50% stenosis and noted a 13% incidence of ipsilateral carotid IPH with a significant male sex association. The present study confirmed the finding of a statistically significant increased incidence of IPH associated with mild or no carotid stenosis in a different cohort of patients, namely asymptomatic outpatients referred from subspecialty clinics for evaluation of known carotid stenosis. The present study also extends the previous findings by evaluating all the MR imaging features of American Heart Association type VI plaque, including surface disruption and IPH.21,22 All of the MR imaging findings corresponding to a complicated or potentially “vulnerable” carotid plaque, namely thin/ruptured fibrous cap, presence of IPH, and type VI plaque, demonstrate a strong male predilection in patients with 0%–49% stenosis. Similar findings have been previously documented in this same group of asymptomatic patients when reviewing their contralateral moderate-to-severe carotid stenosis, though the incidence rate of these complicated features was higher in patients with more severe stenosis.12
LR/NC was present more often in men than women, but it failed to reach statistical significance with a P = .064 in the multivariate analysis. When we evaluated the size of the LR/NC, there was clearly a significant difference, with men having a higher volume of LR/NC than women. It is possible in this cohort of patients with asymptomatic “early” atherosclerotic disease that both sexes are developing LR/NC but that men are predisposed to a larger volume of LR/NC (Tables 1 and 2). The larger LR/NC size in men compared with women may also be associated with the higher incidence of thin/ruptured fibrous cap and IPH noted in this study. While a large, prospective study would be necessary to evaluate this possibility, a recent cross-sectional study has demonstrated the association of large LR/NCs with a higher incidence of thin/ruptured fibrous cap and IPH.13
The presence of calcifications was noted in this study to be higher in men than in women in the univariate analysis that approached statistical significance, though with the multivariate analysis, the association was much less significant. The importance of calcifications in carotid plaque in patients with “early” atherosclerotic disease is unclear and warrants further study. In patients with moderate or severe carotid stenosis, carotid plaque calcifications are very prevalent, and neither their presence nor size demonstrates a sex difference.12
The current study stresses the importance of evaluating sex differences in complex carotid plaque morphology, including thin/ruptured fibrous cap, IPH, type VI plaque, and large LR/NC plaque across the entire spectrum of carotid disease as measured by carotid stenosis. These findings have possible implications for future treatment trials, including carotid endarterectomy and drug trials designed to lower the atherosclerotic burden. Reduction in stroke mortality has begun to plateau, and this change may be attributable to variations in individual responses to therapies that were derived from population-based studies.23 It was also hypothesized that further reductions in stroke mortality may require individualized care governed by direct monitoring of carotid plaque and that patients with an LR/NC with or without IPH may be the desired phenotype for monitoring treatment effects in the individual. Future drug trials may want to include patients with 0%–49% carotid stenosis in addition to those with more severe carotid stenosis. These future trials should be powered to detect a sex difference in treatment and perhaps include an imaging arm to evaluate LR/NC, which can occur in a fairly high percentage of patients with 0%–49% carotid stenosis. IPH has been shown to be associated with current and future ipsilateral carotid thromboembolic events in patients with 0%–70% stenosis.8,20 As such, IPH is a potential marker for “vulnerable” plaque. Patients with IPH may be candidates for aggressive medical treatment, though currently it is unclear whether carotid plaque with IPH will respond to statin therapy.24,25 There is likely to be a role for determining both the presence and size of LR/NC and IPH to identify patients for aggressive medical therapy across a wide spectrum of carotid stenoses.
The current study has 3 major limitations: First, there is a potential for selection bias. The current study population represents a highly selected group of patients referred to subspecialists for further evaluation of known contralateral moderate-to-severe carotid stenosis. The high incidence of cardiovascular risk factors in this study is typical of that in carotid endarterectomy clinical trials but is higher than that in the general population. The results of the current study should only be applied to similar patient groups selected from referrals for advanced carotid artery imaging by cardiovascular and/or neurology subspecialists. The presence of significant contralateral carotid stenosis may increase the prevalence of complicated carotid plaque components in these asymptomatic patients with <50% stenosis compared with patients demonstrating isolated unilateral carotid stenosis. Second, this is a cross-sectional study, and we are unable to demonstrate a direct association between plaque characteristics and subsequent stroke risk. Future prospective trials of in vivo MR imaging are underway and, hopefully, will include a sufficient percentage of women to test for sex-based differences in the treatment-outcome relationship. Last, this was a single-center study. The results should be replicated in multicenter trials.
Conclusions
This in vivo 3T MR imaging study demonstrates a sex difference in complicated American Heart Association type VI carotid plaque and the presence of a thin or ruptured fibrous cap and IPH and the size of LR/NC in patients with <50% stenosis. This sex difference of atherosclerotic plaque exists even during the early stages of the disease seen in patients recruited for MR imaging evaluation of contralateral moderate-to-severe stenosis. Combined with prior research demonstrating a higher incidence of complex plaque in men compared with women who had moderate-to-severe carotid stenosis, the results of this study indicate the possible importance of sex-based management for patients with asymptomatic carotid atherosclerosis at all stages of carotid stenosis.
Supplementary Material
Acknowledgments
We thank our research technologists, Colleen A. Hammond and Scarlett R. Doyle, for their help in acquiring the MR images.
ABBREVIATIONS:
- CE
contrast-enhanced
- IPH
intraplaque hemorrhage
- IR-FSPGR
inversion recovery fast spoiled gradient echo
- LR/NC
lipid-rich necrotic core
- TOF
time-of-flight
Footnotes
Disclosures: Arshad Majid—UNRELATED: Payment for Lectures (including service on Speakers Bureaus): Boeringer Ingelheim (Speakers Bureau), Comments: no longer on speakers bureau, Patents (planned, pending, or issued): Patent submitted for 2 neuroprotective drugs not related, Payment for Development of Educational Presentations: up-to-date on-line publication, Comments: article on pathogenesis of stroke, Travel/Accommodations/Meeting Expenses Unrelated to Activities Listed: funding to travel to the European Stroke Conference, Other: grant funding from American Heart Association and National Institutes of Health (NIH). Chun Yuan— UNRELATED: Consultancy: Imagepace LLC, Bristol-Meyers Squibb, Comments: no personal payment, Grants/Grants Pending: Philips Healthcare,* VP Diagnostics.* J. Kevin DeMarco— UNRELATED: Consultancy: Bracco Diagnostic, Comments: Speakers Bureau. *Money paid to the institution.
This work was supported by the American Heart Association Midwest Affiliate Grant-in-Aid 0855604G; Michigan State University/Office of Vice-President for Research and Graduate Studies and the Office of the Provost through the Internal Grant Program 05-IRGP-472; Bracco Diagnostic Inc; Extramural Research grant I021764; and National Institutes of Health grant HL56874.
Paper previously presented at: 49th Annual Meeting & the Foundation of the American Society of Neuroradiology Symposium, June 4–9, 2011; Seattle, Washington.
References
- 1. Spagnoli LG, Mauriello A, Sangiorgi G, et al. Extracranial thrombotically active carotid plaque as a risk factor for ischemic stroke. JAMA 2004;292:1845–52 [DOI] [PubMed] [Google Scholar]
- 2. Redgrave JN, Lovett JK, Gallagher PJ, et al. Histological assessment of 526 symptomatic carotid plaques in relation to the nature and timing of ischemic symptoms: the Oxford plaque study. Circulation 2006;113:2320–28 [DOI] [PubMed] [Google Scholar]
- 3. Stary HC, Chandler AB, Dinsmore RE, et al. A definition of advanced types of atherosclerotic lesions and a histological classification of atherosclerosis: a report from the Committee on Vascular Lesions of the Council on Arteriosclerosis, American Heart Association. Circulation 1995;92:1355–74 [DOI] [PubMed] [Google Scholar]
- 4. Saam T, Ferguson MS, Yarnykh VL, et al. Quantitative evaluation of carotid plaque composition by in vivo MRI. Arterioscler Thromb Vasc Biol 2005;25:234–39 [DOI] [PubMed] [Google Scholar]
- 5. Saam T, Underhill HR, Chu B, et al. Prevalence of American Heart Association type VI carotid atherosclerotic lesions identified by magnetic resonance imaging for different levels of stenosis as measured by duplex ultrasound. J Am Coll Cardiol 2008;51:1014–21 [DOI] [PubMed] [Google Scholar]
- 6. Ota H, Yarnykh VL, Ferguson MS, et al. Carotid intraplaque hemorrhage imaging at 3.0-T MR imaging: comparison of the diagnostic performance of three T1-weighted sequences 1. Radiology 2010;254:551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Takaya N, Yuan C, Chu B, et al. Association between carotid plaque characteristics and subsequent ischemic cerebrovascular events: a prospective assessment with MRI–initial results. Stroke 2006;37:818–23 [DOI] [PubMed] [Google Scholar]
- 8. Singh N, Moody AR, Gladstone DJ, et al. Moderate carotid artery stenosis: MR imaging-depicted intraplaque hemorrhage predicts risk of cerebrovascular ischemic events in asymptomatic men. Radiology 2009;252:502–08 [DOI] [PubMed] [Google Scholar]
- 9. Lloyd-Jones D, Adams RJ, Brown TM, et al. Executive summary: heart disease and stroke statistics—2010 update: a report from the American Heart Association. Circulation 2010;121:948–54 [DOI] [PubMed] [Google Scholar]
- 10. Rothwell PM, Eliasziw M, Gutnikov SA, et al. Endarterectomy for symptomatic carotid stenosis in relation to clinical subgroups and timing of surgery. Lancet 2004;363:915–24 [DOI] [PubMed] [Google Scholar]
- 11. den Hartog AG, Algra A, Moll FL, et al. Mechanisms of gender-related outcome differences after carotid endarterectomy. J Vasc Surg 2010;52:1062–71, 1071.e1–6 [DOI] [PubMed] [Google Scholar]
- 12. Ota H, Reeves MJ, Zhu DC, et al. Sex differences in patients with asymptomatic carotid atherosclerotic plaque: in vivo 3.0-T magnetic resonance study. Stroke 2010;41:1630–35 [DOI] [PubMed] [Google Scholar]
- 13. Underhill HR, Hatsukami TS, Cai J, et al. A noninvasive imaging approach to assess plaque severity: the carotid atherosclerosis score. AJNR Am J Neuroradiol 2010;31:1068–75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Underhill HR, Yuan C, Zhao XQ, et al. Effect of rosuvastatin therapy on carotid plaque morphology and composition in moderately hypercholesterolemic patients: a high-resolution magnetic resonance imaging trial. Am Heart J 2008;155:584.e1–8 [DOI] [PubMed] [Google Scholar]
- 15. Zhu DC, Ferguson MS, DeMarco JK. An optimized 3D inversion recovery prepared fast spoiled gradient recalled sequence for carotid plaque hemorrhage imaging at 3.0 T. Magn Reson Imaging 2008;26:1360–66 [DOI] [PubMed] [Google Scholar]
- 16. Underhill HR, Yarnykh VL, Hatsukami TS, et al. Carotid plaque morphology and composition: initial comparison between 1.5- and 3.0-T magnetic field strengths. Radiology 2008;248:550–60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. DeMarco JK, Huston J, Nash AK. Extracranial carotid MR imaging at 3T. Magn Reson Imaging Clin N Am 2006;14:109–21 [DOI] [PubMed] [Google Scholar]
- 18. Hatsukami TS, Ross R, Polissar NL, et al. Visualization of fibrous cap thickness and rupture in human atherosclerotic carotid plaque in vivo with high-resolution magnetic resonance imaging. Circulation 2000;102:959–64 [DOI] [PubMed] [Google Scholar]
- 19. Mullahy J. Much ado about two: reconsidering retransformation and the two-part model in health econometrics. J Health Econ 1998;17:247–81 [DOI] [PubMed] [Google Scholar]
- 20. Cheung HM, Moody AR, Singh N, et al. Late stage complicated atheroma in low-grade stenotic carotid disease: MR imaging depiction—prevalence and risk factors. Radiology 2011;260:841–47 [DOI] [PubMed] [Google Scholar]
- 21. Chu B, Phan BA, Balu N, et al. Reproducibility of carotid atherosclerotic lesion type characterization using high resolution multicontrast weighted cardiovascular magnetic resonance. J Cardiovasc Magn Reson 2006;8:793–99 [DOI] [PubMed] [Google Scholar]
- 22. Cai JM, Hatsukami TS, Ferguson MS, et al. Classification of human carotid atherosclerotic lesions with in vivo multicontrast magnetic resonance imaging. Circulation 2002;106:1368–73 [DOI] [PubMed] [Google Scholar]
- 23. Underhill HR, Yuan C. Carotid MRI: a tool for monitoring individual response to cardiovascular therapy? Expert Rev Cardiovasc Ther 2011;9:63–80 [DOI] [PubMed] [Google Scholar]
- 24. Underhill HR, Yuan C, Yarnykh VL, et al. Arterial remodeling in the subclinical carotid artery disease. JACC Cardiovasc Imaging 2009;2:1381–89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Takaya N, Yuan C, Chu B, et al. Presence of intraplaque hemorrhage stimulates progression of carotid atherosclerotic plaques: a high-resolution magnetic resonance imaging study. Circulation 2005;111:2768–75 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.