Abstract
Curcumin is a natural anti-inflammatory agent that has been used for treating medical conditions for many years. Several experimental and pharmacologic trials have demonstrated its efficacy in the role as an anti-inflammatory agent. Curcumin has been shown to be effective in treating chronic conditions like rheumatoid arthritis, inflammatory bowel disease, Alzheimer's and common malignancies like colon, stomach, lung, breast, and skin cancers. As treatments in medicine become more and more complex, the answer may be something simpler. This is a review article written with the objective to systematically analyze the wealth of information regarding the medical use of curcumin, the “curry spice”, and to understand the existent gaps which have prevented its widespread application in the medical community.
Keywords: Curcumin, Chemoprophylaxis, Turmeric, Anti-inflammatory, Curry, Cancer
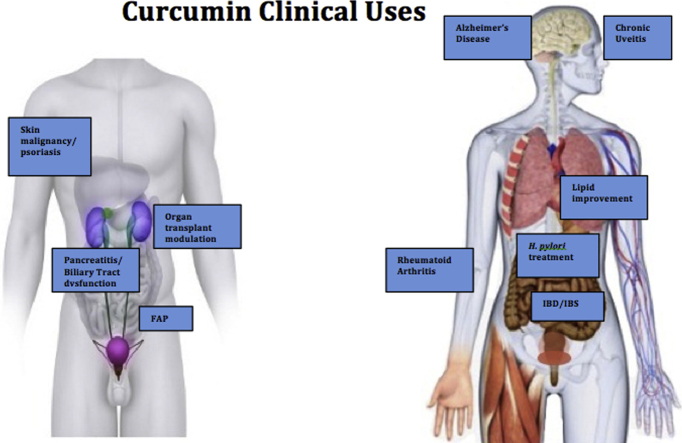
Graphical abstract
1. Introduction
Natural plant products have been used as the foundation of several medical treatments in humans.1 Although modern aspects of Western medicine have become the forefront of clinical practice today, natural plant products continue to be used as remedies in alternative medicine throughout the world. It is estimated that 80% of individuals in developing countries depend primarily on natural products to meet their healthcare needs.1 Even in the United States it has been found that approximately one in three Americans uses natural medicinal products daily.1 It has been estimated that of the 877 small-molecule drugs introduced worldwide between 1981 and 2002, approximately 61% can be traced back to their origins in natural products.1 Natural products are not only effective, but are relatively non-toxic and have therapeutic doses well below their toxic levels.1 Curcumin is one such molecule that has shown promise since time immemorial. Nonetheless, there exists a significant barrier towards the utilization of these natural plant products in modern healthcare due to stigmatization of these “natural” remedies. Although the mechanisms of natural plant products and other plant-based drugs may not be well understood, it is important to uncover their mechanisms of action and determining their effectiveness. This will lead to a much more widespread acceptance of these alternative forms of treatment and allow it to be used in mainstream medicine.
2. Methods
The purpose of this article is to comprehensively review the literature on curcumin and its application in the field of medicine. Literature search was performed using Pubmed, Medline and Google Scholar to search for articles published in English language. The following key words were used – “curcumin,” “turmeric,” “curry,” “chemoprophylaxis,” “cancer chemoprevention” and “anti-inflammatory.” All the papers were reviewed by two authors. The objective of this review was to present the published data on Curcumin to date and explore the lacunae in our current understanding which has withheld the medical community from its clinical use.
3. Results
Curcumin is the principle component of turmeric, a curry spice used as an edible component through different parts of Asia, mainly for its flavor and color profile and less so for its medicinal properties. In Ayurvedic medicine, curcumin is used as treatment for a variety of health conditions, including respiratory illness, liver disorders, inflammatory disorders and diabetic wounds.1 In ancient Hindu medicine, it was used topically to treat sprains and swelling. In traditional Chinese medicine, curcumin is mainly used in treatment for conditions associated with abdominal pain.2 Current evidence suggests that curcumin is a highly pleiotropic molecule with numerous targets and mechanisms of action. It has properties that alter the activity of enzymes, growth factor receptors, cofactors, and other molecules. Curcumin has been confirmed by scientific research to be anticarcinogenic, antimicrobial, hepatoprotective, cardioprotective and thrombosuppresive.1
Curcumin is traditionally an Eastern spice, and is consumed in great quantities in certain regions. One epidemiologic survey found that turmeric consumption in Nepal was up to 1500 mg per person per day.3 In India, the average intake of curcumin can be as high as 2000–2500 mg per day.4 In the 13th century, Marco Polo introduced turmeric to Europe, and only in the recent decades has scientific attention been given to its medicinal properties in the Western world.5
Curcumin was first isolated in 1815 and formulated into its crystalline form in 1870, and ultimately identified as 1,6-heptadiene-3,5-dione-1,7-bis(4-hydroxy-3-methoxyphenyl)-(1E,6E) or diferuloylmethane.6 The first article published regarding the use of curcumin in human disease was in 1937. This article found that healthy persons injected with an intravenous solution containing curcumin had rapid emptying of the gallbladder, which demonstrated that curcumin could treat subacute, recurrent, or chronic cholecystitis.7
Today the United States Food and Drug Administration has approved Curcumin as “Generally Recognized As Safe” (GRAS), showing that the experts have determined that curcumin as a food additive is safe and tolerable under its intended use, and does not need to be subjected to pre-market review and approval by the FDA. It can be found worldwide not just as a medical treatment in the form of capsules and tablets, but as a supplement in ointments, energy drinks, soaps, and cosmetics.7
Treatment of all types of human disease, whether it is chronic, acute, or malignant, has evolved over time. In particular many of the drugs that have been developed recently over the last decade act at very specific pathways, modulating one particular aspect of a disease process. However many diseases today do not operate in such a unilateral fashion. These new mono-targeted drugs may also be expensive and carry large side effect profiles, in addition to lacking efficacy as well. A paradigm shift towards therapies that target multiple signaling pathways rather than therapies that target only one specific pathway may be on the horizon, especially given that many human diseases encountered in medicine are systemic in nature.7 With this understanding, Curcumin is unique for medical treatments in that it has multiple targets and mechanisms of action.
4. Mechanism of action
Curcumin is a highly pleiotropic molecule with numerous targets and mechanisms of action, including altering the activity of enzymes, growth factor receptors, cofactors, and other molecules. Curcumin acts to modulate several pathways as enlisted in Table 1.7 The wide range of action of curcumin can be demonstrated by its activity in inhibiting lipoxygenase by binding lipoxygenase itself or binding to phosphatidylcholine micelles.8 Curcumin also inhibits tumor invasion and angiogenesis by irreversibly binding CD13/aminopeptidase.9 It has also shown both in-vitro and in-vivo to block aggregation and fibril formation by directly binding small β-amyloid species.10
Table 1.
Mechanism of action of curcumin.
| Curcumin mechanism of action2, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20 |
|---|
| Anti-inflammatory |
| Down-regulates activity of COX-2, lipoxygenase and inducible iNOS enzymes |
| Inhibits production of TNF-alpha, IL-1, -2, -6, -8, and -12, MCP, migration inhibitory protein |
| Down-regulates mitogen-activated and Janus kinases |
| Anti-neoplastic via cell-cycle arrest |
| Inhibits expression of cyclin D1 and CDK4 via acetylation and upregulation of p53 |
| ATP-competitive inhibitor by down-regulating mRNA & protein expression of cyclin D1 |
| Induction of CDK inhibitors p16(/INK4a), p21(/WAF1/CIP1), and p27(/KIP1) |
| Inhibits cyclin E/cyclin D1 expression |
| Hyperphosphorylation of retinoblastoma (Rb) protein (CDK2 substrate) |
| Induction of apoptotic signals |
| Induced upregulation of Fas, FasL, and DR5 expression |
| Enhances cleavage of procaspases and poly(ADP-ribose) polymerase |
| Upregulates the expression of DR 4 and 5 |
| Inhibits the TNF-α-induced production of IL-6/IL-8 in HaCaT cells |
| p38-dependent upregulation of FasL in Huh7 cells |
| Inhibits TNF-α-induced activation of NF-κB, including NF-κB-P65 |
Curcumin affects tumor growth by disrupting the activity of several enzymes that allow for growth and proliferation. Its anti-fibrotic effects in glomerular disease is suggested in its action of blocking fibrosis in anti-Thy1 glomerulonephritis through up-regulation of hemoxygenase-1 gene expression.11 Hemoxygenase-1 gene expression can also be induced by curcumin through the generation of reactive oxygen species (ROS), p38 activation, and phosphatase inhibition.12 Another pathway of tumor growth is the Ras pathway in which its proteins must be isoprenylated to be activated. The intermediate in the mevalonate pathway, farnesyl pyrophosphate, donates this isoprenyl group to activate Ras. Curcumin was shown in a study to strongly inhibit FPTase activity, thereby inhibiting the mevalonate pathway and blocking the transforming effects of Ras oncogenes expression.2 Curcumin has also been shown to inhibit xanthine oxidase activity, an enzyme that generates ROS, in PMA-treated NIH3T3 cells to inhibit PMA-mediated tumor promotion.13
Mutations in tyrosine kinases cause uncontrolled activations that result in malignant transformation, growth, and metastasis of human cancers.14 For instance, the overexpression of epidermal growth factor receptor (EGFR) and HER2/neu in cells stimulates the proliferation of cancer cells.14 Both of these pathways act via Tyrosine kinase activation. Curcumin's effect on the activity of multiple kinases furthers the suggestion of its role in cancer therapy. Research shows that curcumin inhibits EGFR kinase activity and EGFR-induced tyrosine phosphorylation of EGFR in A431 cells and degrades cells of Her2/neu protein in-vitro.15 Curcumin has also demonstrated that it has the ability to induce apoptosis in acute T-cell leukemia through inhibition of the phosphatidylinositol-3 kinase/AKT pathway and has also shown to induce G2/M arrest and non-apoptotic autophagic cell death in malignant glioma cells by abrogating Akt and Erk signaling pathways.16 Additionally Curcumin can inhibit many pathways that contribute to its anti-inflammatory and anti-carcinogenic effects, such as various MAPK pathways leading to activation of the p44/42 MAPK (aka ERK1/ERK2), JNK, or p38 MAPK pathway.6, 13
Other mechanisms of cancer proliferation are involved in inhibition of apoptosis, cell invasion, and adhesion for metastasis. Curcumin affects these pathways by being a potent inhibitor of TNF-α induced expression of intracellular cell adhesion molecule-1 (ICAM-1), vascular cell adhesion molecule-1 (VCAM-1), and E-selectin in a study using human umbilical vein endothelial cells. In human prostate cancer, curcumin can activate p53 and simultaneously down-regulate MDM2 oncogene expression via the PI3K/mTOR/ETS2 pathway in human prostate cancer (PC3) and colon cancer (HT-29) cell lines. It can also induce apoptosis and nuclear translocation and activation of p53 in human neuroblastoma cells.17, 18, 19
By inhibiting the activation of transcription factors, curcumin can affect the expression of genes that contribute to carcinogenesis, inflammation, cell survival, cell proliferation, invasion, and angiogenesis. These factors include nuclear factor-kB (NF-kB), activated protein-1 (AP-1), signal transducer and activator of transcription (STAT) proteins, peroxisome proliferator-activated receptor-γ (PPAR-γ), and β-catenin.13 The anti-inflammatory properties of curcumin are through inhibition of COX-1 and COX-2 to prevent the production the eicosanoids prostaglandin E2 and 5-hydroxyeicosatetraenoic acid. The inhibition of these eicosanoids is also associated with reduction of carcinogenesis in rodent models of colorectal cancer.20
5. Pharmacokinetics and pharmacodynamics of curcumin
Prior studies have discussed the difficulty in achieving optimum therapeutic concentrations of the molecule due to low solubility and poor bioavailability of curcumin. Studies suggest that curcumin is first biotransformed to dihydrocurcumin and tetrahydrocurcumin, and subsequently converted to monoglucuronide conjugates.21 Preliminarily animal studies demonstrate that curcumin is rapidly metabolized and conjugated in the liver, and then excreted in feces with limited systemic bioavailability. A 40 mg/kg intravenous dose of curcumin given to rats resulted in complete plasma clearance at one hour post-dose. An oral dose of 500 mg/kg given to rats resulted in a peak plasma concentration of only 1.8 ng/mL.22
A common method that has been employed to increase the bioavailability of curcumin is to use agents that block the metabolic pathway of curcumin. One study exploring methods to increase the bioavailability of curcumin found that co-administration of oral curcumin with piperine, an alkaloid found in black pepper (Piper nigrum) and long pepper (Piper longa), increased serum concentrations of curcumin in rodents, as piperine is a known inhibitor of hepatic and intestinal glucoronidation. With high doses of oral curcumin (2000 mg/kg) and co-administration of piperine, systemic bioavailability was increased by as much as 154%.23
Several phase I clinical trials report data on the pharmacokinetics, metabolites, and systemic bioavailability of curcumin in humans, mainly conducted on cancer patients. A trial conducted of 25 patients with various pre-cancerous lesions administered oral doses of 4, 6, and 8 g curcumin daily for three months yielded serum curcumin concentrations of only 0.51 ± 0.11, 0.63 ± 0.06, and 1.77 ± 1.87 μM, respectively. However safety and patient tolerance was appreciated even at 8 g of curcumin. Serum levels peaked between one and two hours post-dose and declined rapidly; urinary excretion of curcumin was undetectable.24 Another study of 15 patients with advanced colorectal cancer reported even lower serum curcumin concentrations.25 In this study curcumin doses between 0.45 and 3.6 g were given daily for four months. In three of six patients given the 3.6 g dose, mean plasma curcumin measured at all points during the first month of curcumin therapy was consistently 11.1 ± 0.6 nmol/L. Curcumin was not detected in the plasma of patients taking lower doses.25
Due to the low bioavailability of curcumin, Theracurmin, a synthetically derived nano-particle form of curcumin was developed that has a higher bioavailability.26 Previous studies exploring the pharmacokinetics of Theracurmin in healthy patients achieved satisfactory plasma concentrations after one dose.26 Other studies to evaluate the safety of curcumin in cancer patients have yielded similar findings. In one study, Theracurmin was orally administered every day with standard gemcitabine-based chemotherapy. Peak plasma curcumin levels (median) after 200 mg of Theracurmin administration were 324 ng/mL and at 400 mg of Theracurmin peak plasma level was 440 ng/mL with no unexpected adverse events during the 9 months of drug administration.26
Another study of 24 patients aimed to quantify levels of curcumin and its metabolites in colorectal mucosa of patients rather than measuring serum concentration.27 Curcumin C3-complex (2.35 g) was administered daily for 14 days prior to endoscopic biopsy or colonic resection. Curcumin and its metabolites were detectable in 9/24 plasma samples, 24/24 urine samples and in the colonic mucosa of all 23 biopsied participants with mean tissue levels at 48.4 μg/g. The only adverse event reported was mild abdominal discomfort in six patients, and 67% expressed acceptability of the therapy long-term should it be of proven benefit.27
6. Clinical applications of curcumin
More recently there has been a significant increase in the number of clinical trials testing the efficacy of curcumin in treating a variety of diseases, including malignancy, chronic diseases, and psychiatric conditions (Table 2). As of July 2012, there have been observations from 67 clinical trials that have been published, with another 35 clinical trials which were in progress at that time.7
Table 2.
Applications of curcumin in the form of a Clinical Trial.
| Anti-inflammatory/Anti-rheumatic |
| Immune modulator for organ transplant |
| Improving lipid profile |
| Slows progression of Alzheimer's disease |
| Inflammatory bowel disorder |
| Irritable bowel syndrome |
| Cancerous skin lesions |
| Psoriasis |
| Chronic uveitis |
| Pancreatitis |
| Familial adenomatous polyposis |
| Biliary tract dysfunction |
| Anti-H. pylori |
6.1. Rheumatoid arthritis
One of the most promising properties of Curcumin is its ability as an anti-inflammatory agent. One disease that is very common and is associated with an ongoing inflammatory process is rheumatoid arthritis. Rheumatoid arthritis has historically been a debilitating disease until the advent of DMARDs in the 1990s. Although these new disease-modifying drugs have proven quite effective, their use is limited by cost and immune-modulating side effects. Treating rheumatoid arthritis with curcumin has been studied recently.27 The safety and effectiveness of curcumin make it an attractive option for treating some rheumatic diseases, especially given that some studies have found curcumin to have an anti-rheumatic effect comparable to some NSAIDs.1
6.2. Organ transplantation
Curcumin can be used to modulate the immune response after organ transplantation, as one trial demonstrated curcumin's ability to improve early graft function post-renal transplant.28 Studies have demonstrated that curcumin has the ability to up-regulate the antioxidant hemoxygenase-1, which improves outcomes in kidney graft function. A randomized, placebo-controlled trial demonstrated that patients given curcumin for one month after a cadaveric kidney transplant demonstrated better early graft function, in particular decreased creatinine levels after two and thirty days of treatment. High doses of curcumin in this trial also reduced the incidence of acute graft rejection at six months post-transplantation.28
6.3. Cardiovascular disease
Another common medical condition that can be treated with curcumin is atherosclerosis, which is widely prevalent in the Western society. Although there are numerous explanations for this pattern of atherosclerotic disease, one of the factors that may play a role is the decreased consumption of natural plant-based products such as curcumin in the Western diet. Curcumin has demonstrated some efficacy in treating hypercholesterolemia. One small study found that daily administration of 500 mg of curcumin for one week led to a significant 33% decrease in lipid peroxides, a 29% increase in HDL cholesterol, and a 12% decrease in total body cholesterol. Another study also had consistent findings, demonstrating that only 10 mg of curcumin administered twice daily lowered serum LDL and increased HDL.29
6.4. Neurodegenerative disorders
Curcumin is also believed to play a role in preventing the pathogenesis of some psychiatric conditions as well. There has been some evidence that curcumin possesses the ability to bind beta-amyloid plaques and reduce the plaque burden, thus slowing the progression of early Alzheimer's disease.30 One study of 1010 elderly Asians without any serious cognitive defects found that those who consumed curry (curcumin) “occasionally,” “often,” or “very often” scored significantly higher on the mini-mental status examination (screening questionnaire used to detect early signs of dementia) compared to those who “never” or “rarely consumed curcumin.” Although the design of this study may be vague and generally unspecific towards the association of curcumin and cognitive functioning, it certainly can act as a catalyst for other studies to find a stronger relationship between the two. Another current study is examining the efficacy and tolerability of curcumin to treat mild and moderate cases of Alzheimer's dementia.31
6.5. Gastrointestinal disorders
Curcumin has demonstrated therapeutic effects in patients suffering from inflammatory bowel disease (IBD). Inflammation of the digestive tract seen in Crohn's disease and Ulcerative colitis can be a debilitating disease and longstanding inflammation may also increase the risk of colorectal cancer. One preliminary study of nine patients, although small, demonstrated considerable findings regarding curcumin consumption and IBD.32 Five patients with ulcerative colitis on standard treatments of 5-aminosalicyclic acid and corticosteroids were given curcumin at a dose of 550 mg twice daily for a month and then three times daily for another month. After this intervention for two months, all five patients reported significant symptom improvement. Four of the five patients either discontinued their corticosteroids, discontinued their 5-aminosalicylcic acid, or lowered their dose of 5-aminosalicylcic acid as the result of their symptom improvement. The small cohort of patients with Crohn's disease in the same study had very similar findings, as all experienced clinical improvement demonstrated by Crohn's disease activity index. The patients with Crohn's disease also continued to have decreased symptoms at follow-up months later, describing more formed stools, less frequent bowel movements, and decreased abdominal pain and cramping.1 These subjective findings of improvement in both cohorts of patients with IBD were further supported by evidence of laboratory results. It was shown that after two months of treatment with curcumin, inflammatory markers such as erythrocyte sedimentation rate and C-reactive protein levels returned to normal limits.33 Another study demonstrated the ability of curcumin to effectively prevent relapse of ulcerative colitis when curcumin is used as maintenance therapy for six months. This randomized, double-blind placebo-controlled, multicenter study demonstrated that curcumin in addition to maintenance therapy with sulfasalazine or mesalamine had a relapse rate of only 4.7% compared to 20.5% without curcumin.34
Another very common gastrointestinal ailment that curcumin has shown to be effective in treating is irritable bowel syndrome (IBS). IBS is associated with abdominal pain, constipation, diarrhea, and an overall poor quality of life. One randomized study of 207 adults with IBS found that of those who took curcumin daily for eight weeks had a significant improvement in their symptoms.32 Studies such as these not only demonstrate the importance of curcumin for gastrointestinal diseases such as IBS and IBD, but also challenge some of the findings that some of the most common side effects of curcumin are gastrointestinal in nature.
7. Curcumin and cancer treatment
Some of the most exciting aspects of recent research have been curcumin's ability to treat malignancies, either through its own inherent mechanisms or by augmenting other cancer treatments. Given the complexity of cancer medicine, treatments for malignancy still remain one of the most pressing issues in medicine today. Malignancy can result from dys-regulation of hundreds of genes in cell signaling pathways, highlighting the importance of the aforementioned need for treatments that target multiple pathways, much like curcumin.
Today there are clinical trials using curcumin to treat pancreatic, hepatocellular, gastric, breast, prostate, skin, lung and colon cancer, as well as multiple myeloma. For example in-vivo animal studies examining curcumin's chemosensitizing and radiosensiziting properties have favorably demonstrated the effect of curcumin on Gemcitabine for pancreatic cancer.35 A recent clinical trial also demonstrated that a curcumin dose of 8 g per day when taken with Gemcitabine is safe and well tolerated as a supplement.7 Other studies have demonstrated similar effects of curcumin and Docetaxel for ovarian cancer,33 as well as curcumin and oxaliplatin for colon cancer.33, 37 Studies investigating the use of Docetaxel and curcumin as potential treatments for breast cancer have also shown that curcumin can be well tolerated in addition to the chemotherapy.36
One interesting study of 85 men who underwent prostate biopsies because of elevated prostate specific antigen (PSA) but later had negative biopsies showed that those who took a combination of curcumin and flavonoids for six months had a significantly decreased level of PSA. This study demonstrated that curcumin may play a role in suppressing the production of PSA.37
Curcumin was also well tolerated in doses up to 12 g per day in patients who were being treated for multiple myeloma.33 Curcumin has also been shown to decrease risk factors for lung cancer. One study demonstrated in 16 chronic smokers, in addition to 6 non-smokers as control, that when given 1.5 g curcumin a day for 30 days, there was a significant reduction in urinary mutagens found, whereas in the control group there was no change in the excretion of mutagens that was observed. Treatment with curcumin in this study was well tolerated, and there were no changes in serum AST, ALT, blood glucose, creatinine or lipid profile observed.38 This study suggested that not only is curcumin safe, but it could also be used as a dietary modification to decrease the risk of lung cancer.
8. Curcumin and colorectal cancer
The morbidity and mortality from colorectal cancer in affluent countries is striking, especially when compared to Eastern and developing countries.39 In addition to the Western lifestyle and diet that contributes to the discrepancy with colorectal cancer rates, it has been hypothesized that the powerful anti-inflammatory characteristics of curcumin, which is a staple in Eastern diets, may be linked to the decreased colorectal cancer incidence. This appears to have suggest the chemopreventive effect of curcumin.
The efficacy of various chemotherapy regimes for colorectal cancer such as FOLFOX have significantly improved over the last two decades but there remains scope for getting better in eliminating the resistant colorectal cancer cells in circulation.40, 41 The resistance to chemotherapy demonstrates a need to either augment the current therapy, or to find alternative strategies. Augmenting chemotherapy with natural anti-inflammatories such as curcumin could present a novel approach to improving outcomes in treating malignancies. Curcumin's role in the treatment of colorectal cancer is especially important because the postulated mechanism of its efficacy could revolutionize the approach to treating malignancies.
In an attempt to redefine colorectal cancer treatment, research in the last few years has focused attention to the colorectal cancer stem cells (CSCs), which are suspected to account for cancer recurrence, relapse, and metastasis. The stem-cell theory postulates that only a very small number of cells are responsible for driving malignancies. It is estimated that these CSCs may account for only 0.04% of all colorectal cancer cells.42 However failure to eliminate the CSCs could explain recurrence, as the CSCs have self-renewing properties and drive the expansion of malignancy.43, 44 CSCs have similar properties to physiologic stem cells, and also maintain the tumor microenvironment, which in itself enhances carcinogenesis, metastasis, and invasion.42, 45, 46, 47 In theory, therapies that target CSCs should limit tumor growth, relapse and metastasis.
In addition to the CSCs, research has also examined the tumor-microenvironment and the signaling that occurs within it. The initiation and progression of colorectal cancer is associated with epigenetic and genetic alterations which are the result of interactions of transformed cells in the tumor microenvironment, including stromal cells, tumor cells, and surveying immune cells.47, 48
A 2014 study examined the “cross-talk” that occurs between CSCs and the stromal fibroblasts associated in the tumor microenvironment. It was found that there was an in-vitro synergistic relationship between the two types of cells when cultured together compared to monoculture, resulting in a massive release of pro-inflammatory cytokines extremely important to tumor initiation and carcinogenesis.49 This cytokine-induced upregulation of metastatic active adhesion molecules and proliferation-associated proteins promotes tumor development and metastasis, as well as CSC survival.50 This same 2014 study found that in-vitro curcumin administration with 5-FU not only profoundly modulated communication between fibroblasts and CSCs, but also demonstrated a significant decrease in CSCs. Chemoresistant stem cells were identified by CD markers that were found to survive treatments with the traditional FOLFOX chemotherapy regime. These CSCs were positive for CD44, CD133, CD166, and EGFR (epithelial growth factor receptor). It was then found that the CSCs which were treated with FOLFOX and curcumin had a marked reduction in stem cells expressing CD 44, CD133, CD166, and EGFR, demonstrating the ability of curcumin to augment traditional chemotherapies by decreasing the number of colorectal stem cells.42 By inhibiting this synergistic cross-talk in the tumor microenvironment, there is a significant decrease in cell surface adhesion molecules, matrix metalloproteinases, and inflammatory cytokines which all lead to increase tumor development.50 The chemosensitizing ability of curcumin to FOLFOX was demonstrated in another study as well which showed that colorectal cancer cells treated with FOLFOX alone significantly decreased after treatment, but there was a ten-fold greater proportion of CSCs among those surviving, demonstrating the resistance to chemotherapy of the stem cells.42 However treatment with either curcumin alone or in addition to FOLFOX demonstrated a marked reduction in the CSCs, much like the 2014 study demonstrated.
Curcumin may also be particularly effective in decreasing colorectal cancer rates in patients with Familial Adenomatous Polyposis (FAP), an autosomal dominant condition associated with the development of hundreds or thousands of polyps that develop invariably into colorectal cancer at a median age of 39 years. Patients diagnosed with FAP are often recommended to undergo prophylactic proctocolectomy due to this risk. Patients with FAP treated with NSAIDs and COX-2 inhibitors have shown decreased development of adenomas, but there is particular concern about side effects of patients on these medications long-term. One study looked to determine if three doses of 480 mg of curcumin in combination with 20 mg quercetin (a common supplemental flavanol) could suppress adenoma formation in FAP. In the study of five patients diagnosed with FAP who had undergone previous colectomy, it was found that the number and mean size of polyps had decreased after six months by 60.4% and 50.9%, respectively.46
9. Adverse effects of curcumin
The risks associated with curcumin in clinical studies appear to be minimal, and some are often isolated findings (see Table 3). These include transient rise in liver enzymes and anticoagulant properties due to suppression of platelet aggregation.51 In 2011, it was found that there were no significant toxicities of curcumin reported from almost 40 clinical trials involving over 800 participants.1 Other studies have shown that patients have tolerated up to 8 g a day of curcumin for three months with minimal adverse events. One study in 2008 found that Curcumin can be tolerated in doses as high as 12 g per day, with few dose-dependent side effects found in 30% of subjects.1 Escalation beyond a dose of 8 g of curcumin is more limited by the number of capsules that would be required to deliver the dose, making the dose impractical.
Table 3.
Outline of the adverse effects of curcumin at high doses.
As with most supplements and medications, the tolerability and acceptability of curcumin decreases with the increase in dose, as side effects tend to increase and the capsule size and number increases as well in order to deliver the dose.52 The dose-dependent side effects (Table 3) that have been reported appear to be exclusively gastrointestinal in nature, including loose stools, reflux, bloating, and abdominal discomfort. Recently it has been found that most adverse events with daily curcumin intake occur at amounts greater than 4 g a day.24, 53 Not only are the adverse events increased after 4 g a day due to which compliance is also reduced. Compliance is found to be highest between doses of 2–4 g per day, as increasing capsule size becomes clinically impractical, especially in the elderly population.23, 54, 55
In more recent research, a 2013 study of 26 patients examined curcumin pharmacokinetics and adverse events after a 14-day trial of 2.35 g daily curcumin administration. This study found no serious adverse events attributable to curcumin and no changes in overall activity or general health. There were some adverse gastrointestinal disturbances, which were mild and self-resolving.52 Patients in the study actually self-reported a decrease in gastrointestinal disturbances including nausea, vomiting, constipation, diarrhea, flatulence, and abdominal pain following two weeks of daily curcumin intake. The gastrointestinal disturbances that are attributed to curcumin in this study and other studies in the past may not accurately reflect the side effect profile, given the tendency of the selected cohorts to the adverse events.25, 56 The findings in this 2013 study could suggest that curcumin may even be therapeutic for gastrointestinal symptoms, consistent with previous clinical trials of IBD and IBS which found curcumin to improve symptoms in both. This study also found no difference in the overall general health in patients taking curcumin, as well as no serious adverse side effects.
Attention also needs to be paid to some other reported adverse effects of curcumin. In 2013 it was found that curcumin demonstrated a concentration-dependent inhibition of sperm motility in-vitro, with a total block of motility with increased concentration.58 Curcumin has been shown to inhibit the synthesis of Hepcidin,58 which is a protein involved in systemic iron balance. It was found that curcumin caused a dose-dependent drop in hematocrit, hemoglobin, serum iron, and transferrin saturation especially with an underlying subclinical iron deficiency or anemia of chronic disease. Curcumin should therefore be taken with caution among those with marginally low iron stores or other diseases associated with iron such as anemia of chronic disease. In cultured cells curcumin exhibits the properties of an iron chelator, making it likely that it could induce a subclinical or clinical iron deficiency anemia.58 Other side effects of curcumin include potential contact dermatitis and urticaria.1, 60, 61
10. Avenues for future research
Research on curcumin for its chemoprophylaxis and anti-inflammatory properties has been on the rise rapidly in the last decade. In 2008 there were at least twelve active clinical trials of curcumin in the United States, Israel, and Hong Kong.1 As of July 2012, there have been observations from 67 clinical trials that have been published, with another 35 clinical trials which were in progress at that time.7 Curcumin trials are focused on colorectal cancer, hepatocellular carcinoma, gastric carcinoma, Familial Adenomatous Polyposis, multiple myeloma, myelodysplastic syndrome, Alzheimer's, and many more.
With extensive research on curcumin's efficacy, safety, and pharmacokinetics, there are many outlets suggested for future research. There are some concerning issues, in particular poor bioavailability. There is also a very limited set of data regarding any long-term adverse effects of curcumin, and the amount of clinical data is still relatively limited compared to the research involving pharmacologic studies and toxological studies.
Future research in improving the bioavailability of curcumin is a must. Curcumin undergoes extensive metabolism in the liver and intestines, making therapeutic levels of curcumin difficult to achieve.61 However there have been several studies in recent years that have aimed to reduce the toxicity of curcumin by dramatically decreasing the dose needed for therapeutic measures. Decreasing the dose will not only decrease adverse events, but also increase compliance.
One of the criticisms in Curcumin research is that most evidence for the therapeutic potential of curcumin is based on findings from in-vitro studies.51 In these studies curcumin was tested in the concentrations in the micromolar range, although most reports suggest that the plasma concentrations of patients taking oral curcumin remain in the nanomolar range, which may not be sufficient for therapeutic doses.62, 63 These in-vitro studies have shown that cancer cells do not die unless they have been exposed to curcumin concentrations of 5–50 μm for several hours.63, 64 Because of the poor bioavailability of curcmin these concentrations are rarely achieved in humans, let alone maintained for hours, perhaps limiting the chemotherapeutic potential of curcumin, it has been criticized that too many trials are translating in-vitro data into potential clinical outcomes.
Although it has been recognized that curcumin does not cause any significant adverse events in the short-term, there are no large-scale trials that examine adverse effects of curcumin in the long-term. Most trials have only examined high doses of curcumin in short timespans, only weeks to months. Although epidemiologic data from India, where it is estimated that the average person consumes 2500 mg a day,4 has not found any major toxicity with long-term use, there has been no trial to prove that it is devoid of long-term toxicity.60 Another interesting finding among adverse effects of curcumin is that there is significant variability in reporting of these adverse effects among different countries. Interesting research could be done to examine any differences in the pharmacodynamics among different ethnic groups, especially given that certain areas of the world consume significant amounts of curcumin a day compared to others.
Increased research into the tumor microenvironment could also prove to be quite beneficial. Given the findings of curcumin's abilities to modulate molecular targets such as transcription factors, pro-inflammatory cytokines, cell surface adhesion molecules and other targets which enhance carcinogenesis, research could be driven into finding additional agents which may act in a similar fashion. Additional therapies that are similar to curcumin that can modulate the cross talk between the tumor and the stromal environment could find alternative and safer measures to improve the efficacy and safety of treatment of malignancies today.
11. Conclusion
The historical use of curcumin as a therapeutic natural plant product dates back hundreds of years ago, but the most recent advances regarding this agent have extended the possibilities of its use as therapy. The novel idea of supplementing chemotherapy or treating common medical conditions with a traditional kitchen spice is an exciting yet challenging step in medicine. With more clinical trials in addition to the current toxologic and pharmacologic trials, the future of using curcumin not only in the kitchen but in the clinics is becoming a real possibility. With so many traditional treatments today ending up in failure or relapse, new approaches must be considered. It is hoped that the results of the current laboratory and clinical trials not only help prove the effectiveness of curcumin, but also that they may serve as catalysts for future research in large-scale clinical trials to demonstrate the efficacy and safety of curcumin for the treatment of a multitude of human diseases.
Conflict of interests disclosure
The authors have neither conflicts of interests nor any sources of funding to disclose.
Footnotes
Peer review under responsibility of The Center for Food and Biomolecules, National Taiwan University.
References
- 1.Goel A., Kunnumakkara A.B., Aggarwal B.B. Curcumin as “Curecumin”: from kitchen to clinic. Biochem Pharmacol. 2007 doi: 10.1016/j.bcp.2007.08.016. [DOI] [PubMed] [Google Scholar]
- 2.Aggarwal B.B., Takada Y., Oommen O.V. From chemoprevention to chemotherapy: common targets and common goals. Expert Opin Investig Drugs. 2004;13:1327–1338. doi: 10.1517/13543784.13.10.1327. [DOI] [PubMed] [Google Scholar]
- 3.Eigner D., Scholz D. Ferula asa-foetida and Curcuma longa in traditional medical treatment and diet in Nepal. J Ethnopharmacol. 1999;67:1–6. doi: 10.1016/s0378-8741(98)00234-7. [DOI] [PubMed] [Google Scholar]
- 4.Basnet Purusotam, Skalko-Basnet Natasa. Curcumin: an anti-inflammatory molecule from a curry spice on the path to cancer treatment. Molecules. 2011:4567–4598. doi: 10.3390/molecules16064567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang Ke, Fan Hua, Chen Qingsen. Curcumin inhibits aerobic glycolysis and induces mitochondrial-mediated apoptosis through hexokinase II in human colorectal cancer cells in vitro. Anti-Cancer Drugs. 2015;26(1):15–24. doi: 10.1097/CAD.0000000000000132. [DOI] [PubMed] [Google Scholar]
- 6.Aggarwal B.B., Surh Y.J., Shishodia S. The molecular targets and therapeutic uses of curcumin in health and disease. Adv Exp Med Biol. 2007:595. Springer publication. [Google Scholar]
- 7.Gupta Subash C., Patchva Sridevi, Aggarwal Bharat B. Therapeutic roles of curcumin: lessons learned from clinical trials. AAPS J. 2012;15(1):195–218. doi: 10.1208/s12248-012-9432-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Skrzypczak-Jankun E., Zhou K., McCabe N.P., Selman S.H., Jankun J. Structure of curcumin in complex with lipoxygenase and its significance in cancer. Int J Mol Med. 2003;12:17–24. [PubMed] [Google Scholar]
- 9.Shim J.S., Kim J.H., Cho H.Y. Irreversible inhibition of CD13/aminopeptidase N by the antiangiogenic agent curcumin. Chem Biol. 2003;10:695–704. doi: 10.1016/s1074-5521(03)00169-8. [DOI] [PubMed] [Google Scholar]
- 10.Yang F., Lim G.P., Begum A.N. Curcumin inhibits formation of amyloid beta oligomers and fibrils, binds plaques, and reduces amyloid in vivo. J Biol Chem. 2005;280:5892–5901. doi: 10.1074/jbc.M404751200. [DOI] [PubMed] [Google Scholar]
- 11.Gaedeke J., Noble N.A., Border W.A. Curcumin blocks fibrosis in anti-Thy 1 glomerulonephritis through up-regulation of heme oxygenase 1. Kidney Int. 2005;68:2042–2049. doi: 10.1111/j.1523-1755.2005.00658.x. [86] McNally SJ, Harrison EM, Ross JA, Garden OJ, Wigmore SJ. [DOI] [PubMed] [Google Scholar]
- 12.Mcnally Stephen, Harrison Ewen, Ross James, Garden O., Wigmore Stephen. Curcumin induces heme oxygenase 1 through generation of reactive oxygen species, P38 activation and phosphatase inhibition. Int J Mol Med. 2007;19(1) [PubMed] [Google Scholar]
- 13.Shishodia S., Singh T., Chaturvedi M.M. Modulation of transcription factors by curcumin. Adv Exp Med Biol. 2007;595:127–148. doi: 10.1007/978-0-387-46401-5_4. [DOI] [PubMed] [Google Scholar]
- 14.Lengyel E., Sawada K., Salgia R. Tyrosine kinase mutations in human cancer. Curr Mol Med. 2007;7:77–84. doi: 10.2174/156652407779940486. [DOI] [PubMed] [Google Scholar]
- 15.Tikhomirov O., Carpenter G. Identification of ErbB-2 kinase domain motifs required for geldanamycin-induced degradation. Cancer Res. 2003;63:39–43. [PubMed] [Google Scholar]
- 16.Aoki H., Takada Y., Kondo S., Sawaya R., Aggarwal B.B., Kondo Y. Evidence that curcumin suppresses the growth of malignant gliomas in vitro and in vivo through induction of autophagy: role of Akt and ERK signaling pathways. Mol Pharmacol. 2007;72(1):29–39. doi: 10.1124/mol.106.033167. [DOI] [PubMed] [Google Scholar]
- 17.Li M., Zhang Z., Hill D.L., Wang H., Zhang R. Curcumin, a dietary component, has anticancer, chemosensitization, and radiosensitization effects by down-regulating the MDM2 oncogene through the PI3K/mTOR/ETS2 pathway. Cancer Res. 2007;67:1988–1996. doi: 10.1158/0008-5472.CAN-06-3066. [DOI] [PubMed] [Google Scholar]
- 18.Song G., Mao Y.B., Cai Q.F., Yao L.M., Ouyang G.L., Bao S.D. Curcumin induces human HT-29 colon adenocarcinoma cell apoptosis by activating p53 and regulating apoptosisrelated protein expression. Braz J Med Biol Res. 2005;38:1791–1798. doi: 10.1590/s0100-879x2005001200007. [DOI] [PubMed] [Google Scholar]
- 19.Liontas A., Yeger H. Curcumin and resveratrol induce apoptosis and nuclear translocation and activation of p53 in human neuroblastoma. Anticancer Res. 2004;24:987–998. [PubMed] [Google Scholar]
- 20.Huang M., Lysz T., Ferraro T., Abidi T., Laskin J., Conney A. Inhibitory effects of curcumin on in vitro lipoxygenase and cyclooxygenase activity. Cacner Res. 1991;51:813–819. [PubMed] [Google Scholar]
- 21.Pan M.H., Huang T.M., Lin J.K. Biotransformation of curcumin through reduction and glucuronidation in mice. Drug Metab Dispos. 1999;27:486–494. [PubMed] [Google Scholar]
- 22.Ireson C., Orr S., Jones D.J. Characterization of metabolites of the chemopreventive agent curcumin in human and rat hepatocytes and in the rat in vivo, and evaluation of their ability to inhibit phorbolester-induced prostaglandin E2 production. Cancer Res. 2001;61:1058–1064. [PubMed] [Google Scholar]
- 23.Shoba G., Joy D., Joseph T., Majeed M., Rajendran R., Srinivas P.S. Influence of piperine on the pharmacokinetics of curcumin in animals and human volunteers. Planta Med. 1998;64:353–356. doi: 10.1055/s-2006-957450. [DOI] [PubMed] [Google Scholar]
- 24.Cheng A.L., Hsu C.H., Lin J.K. Phase I clinical trial of curcumin, a chemopreventive agent, in patients with high-risk or pre-malignant lesions. Anticancer Res. 2001;21:2895–2900. [PubMed] [Google Scholar]
- 25.Sharma R.A., Euden S.A., Platton S.L. Phase I clinical trial of oral curcumin: biomarkers of systemic activity and compliance. Clin Cancer Res. 2004 Oct 15;10:6847–6854. doi: 10.1158/1078-0432.CCR-04-0744. [DOI] [PubMed] [Google Scholar]
- 26.Kanai M., Imaizumi A., Otsuka Y. Dose-escalation and pharmacokinetic study of nanoparticle curcumin, a potential anticancer agent with improved bioavailability, in healthy human volunteers. Cancer Chemother Pharmacol. 2012;69:65–70. doi: 10.1007/s00280-011-1673-1. [DOI] [PubMed] [Google Scholar]
- 27.Chandran B., Goel A. A randomized, pilot study to assess the efficacy and safety of curcumin in patients with active rheumatoid arthritis. Phytother Res Phytother Res. 2012;26(11):1719–1725. doi: 10.1002/ptr.4639. [DOI] [PubMed] [Google Scholar]
- 28.Gerrits J., Wetering J., Weimar W., Besouw N. T-Cell reactivity during tapering of immunosuppression to low-dose monotherapy prednisolone in HLA-identical living-related renal transplant recipients. Transplantation. 2010;8(2):907–914. doi: 10.1097/TP.0b013e31819b3df2. [DOI] [PubMed] [Google Scholar]
- 29.Kang Q., Chen A. Curcumin suppresses expression of low-density lipoprotein (LDL) receptor, leading to the inhibition of LDL-induced activation of hepatic stellate cells. Br J Pharmacol. 2009;157(8):1354–1367. doi: 10.1111/j.1476-5381.2009.00261.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Caesar I., Jonson M., Nilsson K., Thor S., Hammarström P. Curcumin promotes A-beta fibrillation and reduces neurotoxicity in transgenic Drosophila. PLoS One. 2012;7(2) doi: 10.1371/journal.pone.0031424. http://dx.doi.org/10.1371/journal.pone.0031424 Retrieved September 25, 2015, from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mathew A., Fukuda T., Nagaoka Y. Curcumin loaded-PLGA nanoparticles conjugated with Tet-1 peptide for potential use in Alzheimer's disease. PLoS One. 2012;7(3) doi: 10.1371/journal.pone.0032616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Midura-Kiela M., Radhakrishnan V., Larmonier C., Laubitz D., Ghishan F., Kiela P. Curcumin inhibits interferon- signaling in colonic epithelial cells. AJP Gastrointest Liver Physiol. 2011;302(1):G85–G96. doi: 10.1152/ajpgi.00275.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ravindranath V., Chandrasekhara N. Metabolism of curcumin—studies with [3H]curcumin. Toxicology. 1982;22(no. 4):337–344. doi: 10.1016/0300-483x(81)90027-5. [DOI] [PubMed] [Google Scholar]
- 34.Kumar S., Ahuja V., Vishnubhatla S., Prasad K., Kumar A. Curcumin for maintenance of remission in ulcerative colitis. Protoc Cochrane Database Syst Rev. 1996;10 doi: 10.1002/14651858.CD008424.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Epelbaum R., Schaffer M., Vizel B., Badmaev V., Bar-Sela G. Curcumin and gemcitabine in patients with advanced pancreatic cancer. Nutr Cancer. 2010 Nov;62:1137–1141. doi: 10.1080/01635581.2010.513802. [DOI] [PubMed] [Google Scholar]
- 36.Bayet-Robert M., Morvan D. Metabolomics reveals metabolic targets and biphasic responses in breast cancer cells treated by curcumin alone and in association with docetaxel. PLoS One. 2013;8(3) doi: 10.1371/journal.pone.0057971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhou D., Ding N., Du Z. Curcumin analogues with high activity for inhibiting human prostate cancer cell growth and androgen receptor activation. Mol Med Rep Mol Med Rep. 2014;10(3):1315–1322. doi: 10.3892/mmr.2014.2380. [DOI] [PubMed] [Google Scholar]
- 38.Gupta S., Patchva S., Aggarwal B. Therapeutic roles of curcumin: lessons learned from clinical trials. APPS J. January 2013;15(No 1) doi: 10.1208/s12248-012-9432-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Polasa K., Raghuram T.C., Krishna T.P., Krishnaswamy K. Effect of turmeric on urinary mutagens in smokers. Mutagenesis. 1992;7(2):107–109. doi: 10.1093/mutage/7.2.107. [DOI] [PubMed] [Google Scholar]
- 40.Jemal A., Siegel R., Ward E. Cancer statistics, 2008. CA Cancer J Clin. 2008;58(2):71–96. doi: 10.3322/CA.2007.0010. [DOI] [PubMed] [Google Scholar]
- 41.Todaro M., Francipane M.G., Medema J.P., Stassi G. Colon cancer stem cells: promise of targeted therapy. Gastroenterology. 2010;138:2151–2162. doi: 10.1053/j.gastro.2009.12.063. [DOI] [PubMed] [Google Scholar]
- 42.Abdul Khalek F.J., Gallicano G.I., Mishra L. Colon cancer stem cells. Gastrointest Cancer Res. 2010:S16–S23. [PMC free article] [PubMed] [Google Scholar]
- 43.Yu Y., Kanwar S.S., Patel B.B., Nautiyal J., Sarkar F.H., Majumdar A.P. Elimination of colon cancer stem-like cells by the combination of curcumin and FOLFOX. Transl Oncol. 2009;2(4):321–328. doi: 10.1593/tlo.09193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dick J.E. Stem cell concepts renew cancer research. Blood. 2008;112(13):4793–4807. doi: 10.1182/blood-2008-08-077941. [DOI] [PubMed] [Google Scholar]
- 45.Wang J.C., Dick J.E. Cancer stem cells: lessons from leukemia. Trends Cell Biol. 2005;15(9):494–501. doi: 10.1016/j.tcb.2005.07.004. [DOI] [PubMed] [Google Scholar]
- 46.Boman B.M., Huang E. Human colon cancer stem cells: a new paradigm in gastrointestinal oncology. J Clin Oncol. 2008;26:2828–2838. doi: 10.1200/JCO.2008.17.6941. [DOI] [PubMed] [Google Scholar]
- 47.Schiavoni G., Gabriele L., Mattei F. The tumor microenvironment: a pitch for multiple players. Front Oncol. 2013;3 doi: 10.3389/fonc.2013.00090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Buhrmann C., Kraehe P., Lueders C., Shayan P., Goel A., Shakibaei M. Curcumin suppresses crosstalk between colon cancer stem cells and stromal fibroblasts in the tumor microenvironment: potential role of EMT. Sethi G., editor. PLoS One. 2014;9(9):e107514. doi: 10.1371/journal.pone.0107514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gout S., Huot J. Role of cancer microenvironment in metastasis: focus on colon cancer. Cancer Microenviron. 2008;1:69–83. doi: 10.1007/s12307-008-0007-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Boral D., Nie D. Cancer stem cells and niche mircoenvironments. Front Biosci (Elite Ed) 2012;4:2502–2514. doi: 10.2741/e561. [DOI] [PubMed] [Google Scholar]
- 51.Pin A.L., Houle F., Huot J. Recent advances in colorectal cancer research: the microenvironment impact. Cancer Microenviron. 2011;4:127–131. doi: 10.1007/s12307-011-0070-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Irving G.R., Karmokar A., Berry D.P., Brown K., Steward W.P. Curcumin: the potential for efficacy in gastrointestinal diseases. Best Pract Res Clin Gastroenterol. 2011;25:519–534. doi: 10.1016/j.bpg.2011.09.005. [DOI] [PubMed] [Google Scholar]
- 53.Irving G.R., Howells L.M., Sale S. Prolonged biologically active colonic tissue levels of curcumin achieved after oral administration—a clinical pilot study including assessment of patient acceptability. Cancer Prev Res (Phila) 2013;6:119–128. doi: 10.1158/1940-6207.CAPR-12-0281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Li L., Ahmed B., Mehta K., Kurzrock R. Liposomal curcumin 1570 with and without oxaliplatin: effects on cell growth, 1571 apoptosis, and angiogenesis in colorectal cancer. Mol Cancer Ther. 2007;6:1276–1282. doi: 10.1158/1535-7163.MCT-06-0556. [DOI] [PubMed] [Google Scholar]
- 55.Garcea G., Jones D.J., Singh R. Detection of curcumin and its metabolites in hepatic tissue and portal blood of patients following oral administration. Br J Cancer. 2004 Mar 8;90:1011–1015. doi: 10.1038/sj.bjc.6601623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Carroll R.E., Benya R.V., Turgeon D.K. Phase IIa clinical trial of curcumin for the prevention of colorectal neoplasia. Cancer Prev Res. 2011;4:354–364. doi: 10.1158/1940-6207.CAPR-10-0098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ireson C.R., Jones D.J., Orr S. Metabolism of the cancer chemopreventive agent curcumin in human and rat intestine. Cancer Epidemiol Biomarkers Prev. 2002;11:105–111. [PubMed] [Google Scholar]
- 58.Naz R.K., Lough M.L. Curcumin as a potential non-steroidal contraceptive with spermicidal and microbicidal properties. Eur J Obstet Gynecol Reprod Biol. 2014;176:142–148. doi: 10.1016/j.ejogrb.2014.01.024. [DOI] [PubMed] [Google Scholar]
- 59.Jiao Y., Wilkinson J., Di X. Curcumin, a cancer chemopreventive and chemotherapeutic agent, is a biologically active iron chelator. Blood. 2009;113:462–469. doi: 10.1182/blood-2008-05-155952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hata M., Sasaki E., Ota M., Fujimoto K., Yajima J., Shichida T. Allergic contact dermatitis from curcumin 1827 (turmeric) Contact Dermat. 1997;36:107–108. doi: 10.1111/j.1600-0536.1997.tb00426.x. [DOI] [PubMed] [Google Scholar]
- 61.Burgos-Moron E., Calderon-Montano J.M., Salvador J., Robles A., Lopez-Lazaro M. The dark side of curcumin. Int J Cancer. 2010;126(7):1771–1775. doi: 10.1002/ijc.24967. [DOI] [PubMed] [Google Scholar]
- 62.Kanai M., Otsuka Y., Otsuka K. A phase I study investigating the safety and pharmacokinetics of highly bioavailable curcumin (Theracurmin) in cancer patients. Cancer Chemother Pharmacol. 2013;71:1521–1530. doi: 10.1007/s00280-013-2151-8. [DOI] [PubMed] [Google Scholar]
- 63.Lopez-Lazaro M. Anticancer and carcinogenic properties of curcumin: considerations for its clinical development as a cancer chemopreventive and chemotherapeutic agent. Mol Nutr Food Res. 2008;52(suppl 1):S103–S127. doi: 10.1002/mnfr.200700238. [DOI] [PubMed] [Google Scholar]
- 64.Syng-Ai C., Kumari A.L., Khar A. Effect of curcumin on normal and tumor cells: role of glutathione and bcl-2. Mol Cancer Ther. 2004;3:1101–1108. [PubMed] [Google Scholar]