Abstract
The Advisory Committee on Immunization Practices recommended immunization schedule for adolescents includes three vaccines (Tdap, HPV, and MCV4) and annual influenza vaccination. Given the increasing number of recommended vaccines for adolescents and health and economic costs associated with non-vaccination, it is imperative that effective strategies for increasing vaccination rates among adolescents be developed. This article describes the development, theoretical framework, and initial first-year evaluation of an intervention designed to promote vaccine acceptance among a middle- and high-school based sample of adolescents and their parents in eastern Georgia. Adolescents, parents, and teachers were active participants in the development of the intervention. The intervention, which consisted of a brochure for parents and a teacher-delivered curriculum for adolescents, was guided by constructs from the Health Belief Model and Theory of Reasoned Action. Evaluation results indicated that our intervention development methods were successful in creating a brochure that met cultural relevance and literacy needs of parents. We also demonstrated an increase in student knowledge of and attitudes toward vaccines. To our knowledge, this study is the first to extensively engage middle- and high-school students, parents, and teachers in the design and implementation of key theory-based educational components of a school-based, teacher-delivered adolescent vaccination intervention.
INTRODUCTION
Between 2005 and 2008, the Advisory Committee on Immunization Practices recommended three vaccines that are specifically targeted to adolescents (tetanus, diphtheria, and acellular pertussis (Tdap) vaccine; human papillomavirus (HPV) vaccine; and meningococcal conjugate vaccine (MCV4)), as well as annual influenza vaccination (Centers for Disease Control and Prevention, June 2012). However, vaccination rates among adolescents for most of these four recommended vaccines remain below the Healthy People 2020 objective of 80% coverage (Centers for Disease Control and Prevention, June 2012). The 2012 national coverage for Tdap vaccine was 84.6%, MCV4 was 74.0%, and for at least one dose of HPV vaccine among females was 53.8%; of those only 66.7% completed the HPV series; among males only 20.8% received at least one dose of the HPV vaccine and of those only 45.1% completed the three dose series (Centers for Disease & Prevention, 2013). The morbidity, mortality, and costs associated with vaccine-preventable diseases emphasize the need to develop and implement effective strategies for increasing vaccination rates among adolescents (Caro, Getsios, El-Hadi, Payne, & O’Brien, 2005; Caro et al., 2007; Insinga, Dasbach, Elbasha, Puig, & Reynales-Shigematsu, 2007; Zhou et al., 2005).
Because adolescents in middle- and high-school have consistently been shown to be the most difficult group to reach for vaccination (Carpenter et al., 2007; Monto, Davenport, Napier, & Francis, 1969, 1970), more targeted approaches may be necessary to increase vaccination rates among these populations. Nearly all U.S. children attend school daily, with attendance rates ranging from 92.0% to 98.2% among students aged 10–18 years (US Census Bureau, 2011). Consequently, school-based intervention programs may be an efficient, effective strategy to reach large numbers of adolescents compared to individually-scheduled physician visits (Luce et al., 2001). Because students have already established a sense of trust and rapport with classroom teachers, teacher-delivered interventions have the potential to be highly effective. Teacher-delivered interventions have been effectively utilized to impact health-related attitudes and behaviors for several health outcomes, including sexual activity (Henderson et al., 2007), nutrition (Fahlman, Dake, McCaughtry, & Martin, 2008), asthma (Henry, Gibson, Vimpani, Francis, & Hazell, 2004), and anxiety (Neil & Christensen, 2009). To date, teacher-delivered interventions have not been extensively utilized to impact vaccination behavior. Such interventions may be particularly important for increasing vaccine acceptance among adolescents (Painter, Sales, Pazol, Wingood, et al., 2010; Painter et al., 2011).
Adolescence is a stage characterized by development of social and emotional maturity, an increasing sense of self, and development of autonomy (Lind, Anderson, & Oberle, 2003). Adolescents are more likely to take control of their own health-related attitudes and behaviors than younger children (Coates TJ, 1982). The relative importance of parental versus adolescent attitudes toward vaccination and vaccine uptake has not been well studied. Research suggests that both parental and adolescent attitudes may be important in determining vaccine uptake.
Studies have shown that for parents, knowledge, perceived susceptibility, perceived barriers to vaccination, social norms and concerns about vaccine safety are important predictors of vaccine acceptance (Allison et al., 2010; Carpenter et al., 2007; Daley et al., 2009; Sales et al., 2011; Woodhall et al., 2007). Among adolescents, perceived susceptibility to infection, perceived barriers to vaccination, and perceived benefit of vaccination have been identified as important predictors of vaccination (Chan, Yan Ng, Lo, Cheung, & Hung Chung, 2009; Kahn et al., 2008; Painter, Sales, Pazol, Wingood, et al., 2010; Painter et al., 2011; Roberts, Gerrard, Reimer, & Gibbons, 2010).
The purpose of this article is to describe the development of a comprehensive approach to promoting adolescent vaccine acceptance among parents and adolescents attending middle- and high-schools in eastern Georgia. Specifically, this article focuses on the (a) theoretical framework, (b) educational intervention development, and (c) initial evaluation of the first year of implementation of the project.
PROJECT OVERVIEW
Beginning in 2010, we initiated a project to determine the effectiveness of two interventions designed to enhance adolescent vaccination rates among a sample of adolescents attending middle- or high-schools in Georgia. The first year was for development of methods for the intervention, years two and three are for intervention implementation, and year four is for analysis and dissemination of final results. The study used a randomized, three-armed controlled design across two years (Figure 1). The three arms consist of 1) an educational brochure targeted to parents, 2) the parent brochure and a science teacher-delivered intervention targeted to students, and 3) a control arm (no intervention). Each intervention arm comprises two middle-schools and two high-schools, and the control arm comprises two middle-schools and one high-school.
Figure 1.
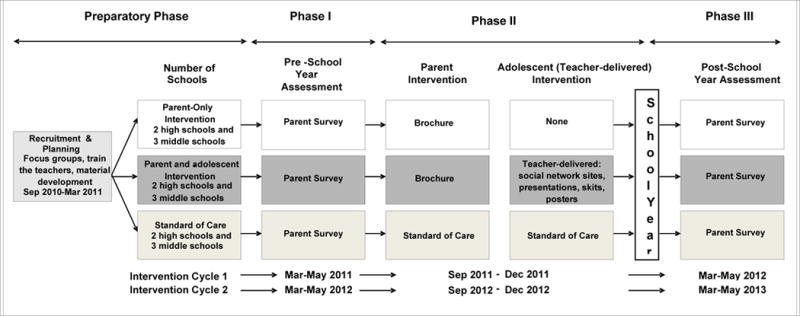
Study Design for “Enhancing Adolescent Immunization through Parent and Teacher Interventions
The first year of the project was utilized for development of methods for the intervention. As part of this formative phase, focus groups and piloting testing were conducted among parents, adolescents and teachers. Similar procedures were utilized across focus groups and are herein described. A convenience sample was taken for all focus groups with assistance from the schools to identify and invite participants. Participants of focus group received $20 and were notified in advance that they would be compensated for their time. All focus group and pilot participants resided in our intervention county but did not attend schools participating in our study. Grounded theory was used to develop all focus group questions. Focus groups were recorded and transcribed verbatim by an independent transcription company. Content analysis was performed using NVivo9 qualitative analysis software. The analysis included line-by-line coding of statements and responses from two independent researchers. Researchers met to review the codes and evaluate their meaning. The coded data were organized to identify themes and understand the behavior and attitudes among the participants. The themes were cross-referenced among the coders and percent agreement was determined. Disagreements about themes were discussed and resolved among coders until 100% agreement on themes was achieved.
The study was approved by the institutional review boards at Emory University and Georgia Department of Community Health.
PARTICIPANT POPULATION
This intervention was implemented in a county in eastern Georgia that was selected because it has a relatively large population, includes a mix of urban and rural schools, and has substantial low income and high minority population. Fiscal Year 2010 enrollment data indicated that there were 5,734 middle-school students and 8,586 high-school students in the participating county. The percentage of African-American students ranged from 29% to 98% in the middle-schools and 59% to 96% in the high-schools; 72.3% of students were eligible for a free or reduced price meal (Data Center, 2012).
THEORETICAL FRAMEWORK
The Health Belief Model (HBM) was originally developed to explain the failure of participation in tuberculosis screenings, and it is still considered to be salient for use with one-time behaviors, such as vaccination (Champion V, 2008; Noar & Zimmerman, 2005). However, additional research indicates that alternative theories, such as the Theory of Reasoned Action (TRA), may also be appropriate for understanding vaccination behavior (Montano, 1986). We have successfully employed a framework using HBM and TRA in a previous school-based intervention to increase the uptake of influenza vaccine among middle- and high-school students (Gargano et al., 2011). An illustration of the conceptual framework used to guide our intervention for the current study is presented in Figure 2. In this study, we designed our educational intervention materials to target the six major constructs from HBM, including: attitudes toward perceived threat of disease [(1) perceived susceptibility and (2) perceived severity], attitudes regarding perceived expectations of vaccination [(3) perceived benefits and (4) perceived barriers], (5) cues to action to vaccinate, and (6) self-efficacy for obtaining vaccinations against HPV, influenza, tetanus, diphtheria, pertussis, and meningococcal disease. We also included a key construct from the TRA, social norms, (both injunctive and descriptive norms) (Table 1).
Figure 2.
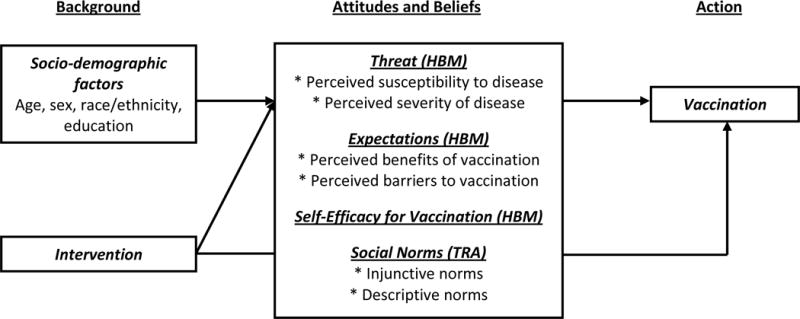
Theoretical Framework Employing Constructs from the Health Belief Model and Theory of Reasoned Action in the Context of Our Educational Intervention
Table 1.
Application of Health Belief Model and Theory of Reasoned Action to Educational Intervention Content
| HBM/ TRA Constructs | Translating Constructs to the Intervention | Parent Brochure Content | Student Curriculum Content |
|---|---|---|---|
| HBM Constructs | |||
| Perceived susceptibility | Parents and adolescents must feel at risk for tetanus, diphtheria, pertussis, meningococcal, influenza and human papillomavirus | Information about how tetanus, diphtheria, pertussis, meningitis, influenza, and human papillomavirus are spread
|
Information about how tetanus, diphtheria, pertussis, meningitis, influenza, and human papillomavirus are spread
|
| Perceived severity | Parents and students must feel that the consequences of tetanus, diphtheria, pertussis, meningococcal, influenza and human papillomavirus are serious | Information about the seriousness of tetanus, diphtheria, pertussis, meningitis, influenza, and human papillomavirus
|
Information about the seriousness of tetanus, diphtheria, pertussis, meningitis, influenza, and human papillomavirus |
| Perceived benefits | Parents and adolescents must believe that Tdap, MCV4, flu and HPV vaccination will be beneficial in terms of preventing disease | Information about how adolescent vaccines can help prevent adolescents from getting these diseases
|
Information about how the vaccines can help prevent adolescents from getting tetanus, diphtheria, pertussis, meningitis, influenza, and human papillomavirus Information about how to prevent spreading diseases to others
|
| Perceived barriers | Parents and adolescents must believe that they can overcome barriers that would prevent them from being vaccinated | Information dispelling myths about vaccines Visual images of parents accompanying teens, who are receiving vaccines |
Information about vaccines safety
|
| Cues to action | Parents’ and adolescents’ decision to obtain the vaccines will be influenced by various factors | The brochure serves as a cue to action
|
Visual images of teens receiving vaccines |
| Self efficacy | Parents and adolescents must feel confident in their ability to get vaccinated | Motivational testimony from parents and a nurse practitioner on the importance of vaccination
|
Visual images of teens receiving vaccines Information about where to get vaccinated |
| TRA Constructs | |||
| Social norms |
Injunctive norms: Parents and adolescents must feel that their peers would approve of vaccination Descriptive norms: Parent and adolescents must believe that their peers receive vaccination |
Pictures of multiethnic parents and adolescents receiving vaccines Motivational testimony from parents and a nurse practitioner |
Students ask questions and answer to demonstrate their understanding of adolescent vaccines |
INTERVENTION DEVELOPMENT
Preliminary Research – Parent Brochure
We designed a tailored educational brochure to be distributed to parents as one part of this intervention. Studies have shown that educational brochures are an acceptable format to disseminate information to parents and are capable of enhancing vaccine acceptance among parents and high-minority populations (Clayton, Hickson, & Miller, 1994; Jacobson et al., 1999; Sales et al., 2011). Before developing the educational brochure we ascertained existing attitudes and beliefs related to adolescent vaccines and the diseases they protect against by conducting a series of focus groups among parents of middle- and high-school students. We conducted four focus groups, drawing from two middle-schools and two high-schools. All focus groups were held at the respective schools, and contained 8 to 12 participants each.
Focus group results indicated that, in general, parents knew that there were vaccines recommended specifically for adolescents. They also believed that HPV-associated conditions, influenza, diphtheria, tetanus, pertussis, and meningitis are serious illnesses and that vaccination is an important prevention strategy. However, they were uncertain about why adolescents are at particular risk for these diseases. When asked whether getting their adolescent vaccinated with HPV, influenza, Tdap, or MCV4 vaccine would cause the illness the vaccine is designed to prevent, only the influenza vaccine was thought to cause the disease. Concerns about side-effects and lack of knowledge about the vaccines were the leading reasons why parents would not have their adolescent vaccinated. Parents also indicated that they would discuss information about vaccines sent from the school with their physicians.
Brochure Development
We developed a draft brochure based on our theoretical framework, literature review, previous work, and focus group findings. We developed the prototype in two formats: a booklet format and a fold-out format. Two pilot testing groups were conducted with parents of middle- and high-school students to obtain feedback regarding the prototype brochure. Each group included 8 to 12 participants. During these sessions, with direction from facilitator, participants systematically evaluated the brochure page by page discussing both the text layout, information in the brochure, and pictures and indicated which aspects of the brochure they liked or disliked.
Aspects of the brochure appealing to participants included the “eye-catching” layout and color scheme; photographs of multiethnic parents, adolescents, and doctors; easy to read language; use of bullet points; the testimonials; and the “Did you know” sections, that gave additional facts about each disease. Key aspects of the brochure that required changes included the pictures on the outside and inside of the front cover and adding phone numbers for the Vaccines for Children program and the local health department. Parents were polled and all participants preferred the booklet format instead of the fold-out format because it was more convenient and easier to read.
Final Brochure
The final brochure consisted of eight pages of information in a booklet format. Page 1 was a cover panel with a photo of a multiethnic group of adolescents, a statement indicating the partnership between Emory University, Georgia Regents University and the County Board of Health, and the phrases “Vaccines aren’t just for babies, Vaccinate your teen”, and “Learn about vaccines for teens”. Page 2 contained information about CDC’s adolescent vaccine recommendations and why it is important to get adolescents vaccinated. There was also an additional photo of multiethnic adolescents. The next four pages were specific for each vaccine. Each page contained information on complications from disease, a “How is it spread?” section for perceived disease susceptibility, a “Did you know?” section giving facts about the diseases the vaccine protects against and complications and symptoms of those diseases for perceived disease severity and vaccine benefit, and a “What should I do?” section containing the recommendation for vaccination to promote self-efficacy. There were also pictures of adolescents getting vaccinated, a family, and a high-school football player. For social norms, there were also several testimonials from parents and healthcare providers on the importance of vaccination. Page 7 consisted of “Mythbusters” which addressed some of the common myths about vaccines. Page 8 gave a picture of medical personnel, along with sources for more information (telephone numbers and websites), a recommendation to see their healthcare provider or local health department for more information or to get vaccinated to decrease barriers to vaccination, and our message that “Vaccines aren’t just for babies, Vaccinate your teen” (Supplementary Figure 1).
Preliminary Research – Teacher-delivered Adolescent Curriculum
Before developing the teacher-delivered adolescent curriculum, we conducted a series of four focus groups with middle- and high-school students, parents, and health and science teachers. Each focus group included 6 to 12 participants and was held in the respective school. During the adolescent focus groups, we evaluated existing knowledge and attitudes related to the four specific adolescent vaccines, infectious diseases, and types of teaching tools they preferred. For the teacher focus groups, we ascertained existing knowledge of these specific infectious diseases and comfort level in teaching material about infectious diseases and vaccines.
Participants in the adolescent focus groups knew that there were vaccines recommended for adolescents; the high-school students could name more of the recommended vaccines than middle-school students. Overall, students knew that vaccination is an important tool for disease prevention and that adolescents were at risk for these specific diseases. Students said they would want to know about side-effects and how the vaccines are manufactured before they would get them. They reported that they would be interested in learning about infectious diseases and vaccines in school, these lessons would benefit people their age, and their parents would be supportive of such a curriculum. They recommended that the lesson plan be interactive with games, projects, and hands on activities, in addition to utilizing colorful and animated PowerPoint slides.
Results from the parent focus group indicated that parents would be comfortable with their child learning about the specific infectious diseases and their corresponding vaccines in school and that this would be beneficial for them. They indicated that discussion of HPV and how it spread would not bother them; however, they preferred that science or health teachers deliver the material rather than English or history teachers.
In general, participants in the teacher focus groups were aware that there were vaccines recommended for adolescents, and most were able to name them. They knew the importance of vaccination for disease prevention and that adolescents were at risk for these specific diseases. Participants were comfortable delivering a curriculum on infectious diseases and vaccines, as long as it was approved by the school board, and felt that the topic would fit into their existing curriculum. The teachers were especially supportive if all of the supplies were provided and if they were given a training session before implementation. They said tools that would be helpful when teaching this topic would be hands-on activities, use of graphics and multimedia, having a speaker discuss a personal experience, and games and competitions.
Teacher-delivered Adolescent Curriculum Development
We developed an initial curriculum based on our theoretical framework, literature review, and initial focus group findings that identified knowledge gaps, specific concerns, and areas of uncertainty. We then conducted a pilot test with four middle-school students and five high-school students. Participants systematically evaluated each part of the curriculum and indicated which aspects of the curriculum they liked or disliked. The curriculum comprised a PowerPoint presentation, a video on how vaccines work, a disease-spread activity, pre- and post-test, and a car racing PowerPoint game. Overall, participants liked the curriculum. Participants said they understood the test questions and felt that students would take the lesson more seriously if the test was included. Aspects of the PowerPoint slides that required changes included adding more colors and pictures throughout the PowerPoint to help sustain the students’ attention and adding “gross” (graphic) pictures to drive home the severity and consequences of these diseases.
We also held a mock training session with science teachers in our intervention schools who would be delivering the curriculum to explain and demonstrate the initial version of the curriculum materials and collect any final suggestions. The teachers felt the curriculum was well organized and structured. They were comfortable with the topics covered in the PowerPoint presentations. Teachers felt activities and games were especially engaging and would be enjoyed by students. Teachers felt that the pre- and post-test did a good job of assessing students understanding of the materials and that it did not take up too much time. Some teachers requested the scores from the tests be given to them so the students could use it for extra credit. Technical difficulties were experienced by two of the schools which had a block on the website hosting the video on how vaccines work. To overcome this barrier, we requested and used the video on a CD from Colorado Children’s Immunization Coalition (http://www.childrensimmunization.org).
Final Teacher-delivered Adolescent Curriculum
The final curriculum consisted of several parts. The total intervention time was approximately 120 minutes delivered in segments over two to three days, depending on the length of class periods. Each teacher was given a package with all the materials they would need, including copies of a pre-test and post-test; a CD with presentations and videos; instructions and lesson plans with objectives; supplies for the activities; and prizes for the game winning team. The pre- and post-test had ten questions, five assessing vaccine-related knowledge and four attitude questions that followed the HBM (disease susceptibility, disease severity, barriers to vaccination, benefit to vaccination), and one question on intention to be vaccinated. The Day 1 curriculum included the baseline pre-test; a PowerPoint presentation on infectious diseases, how they spread (perception of disease susceptibility), ways to prevent infection (perceived benefit to vaccination), and what vaccines are recommended for adolescents; the video on how vaccines work; and an interactive session to demonstrate how infectious diseases spread (perceived disease susceptibility). The Day 2 curriculum consisted of a re-cap of the previous day’s lesson; a PowerPoint presentation specifically related to the vaccines recommended for adolescents, the complications of those diseases including an audio of a child with pertussis coughing (perceived disease severity), and how the diseases spread (perceived disease susceptibility); and a PowerPoint-based car racing game for which the winning team received a plush microbe toy representing chickenpox, influenza, or pertussis. The Day 3 curriculum comprised students working in teams to develop a poster on one of the topics they learned about and present it to the class. Lastly, students completed the post-test.
EVALUATION FROM THE FIRST YEAR IMPLEMENTATION
Parent Brochure Evaluation
After our first-year implementation cycle (school year 2011–2012), we identified 184 out of 208 (88.5%) parents in the intervention schools who were willing to participate in a brief phone survey regarding the educational intervention. Of the respondents, 67% recalled receiving the brochure. Of those who reported receiving the brochure, 90% reported reading it, with 23% reading some, 37% reading most, and 40% reading the entire brochure. Most respondents believed that they understood the brochure (97%), that it was relevant to them (91%), and that it increased their knowledge about adolescent vaccination (93%). Fifty-six percent reported discussing the brochure with family or friends.
Teacher-delivered Adolescent Curriculum Outcome Evaluation
Students were given a pre- and post-test to assess changes in knowledge and attitudes after participating in the curriculum. We had a total of 667 out of 787 middle-school students (84.8%) and 401 out of 569 high-school students (70.5%) complete both tests (Table 2). A chi-square analysis was conducted to compare pre- and post-test responses. Among middle-school students, there was a significant increase from pre- to post-test in knowledge regarding how vaccines are produced (from 14% to 25.3%, p<0.001). There was a significant increase in students’ knowledge of the four recommended teen vaccines for both middle- (21% to 66.4%, p<0.001) and high-school students (38.7% to 67.6%, p<0.001) (Table 2). There were significant increases in students’ knowledge that by being vaccinated they could protect others, for middle-school (76.3% to 91.3%, p<0.001) and high school (86.8% to 93.8%, p=0.001). At baseline, a high percentage of middle- and high-school students had a positive attitude toward vaccines. Among middle-school students, there was a significant increase in the belief that vaccines could prevent people from getting sick (78.6% to 87.4%, p<0.001) (Table 2). At post-test, there was a slight increase in the number of students in both middle- and high-schools who responded that vaccines could make them sick. Of importance, there was a significant increase in in the proportion of both middle- (from 70.0% to 82.9%, p<0.001) and high-school (from 77.3% to 84.8%, p=0.01) students who were interested in getting the adolescent vaccinations (Table 2).
Table 2.
Pre- and Post-test Scores Assessing Vaccine Knowledge and Attitudes among Middle and High School Students
| Questions | Middle School (N=667) | High School (N=401) | ||||
|---|---|---|---|---|---|---|
| Knowledge | Pre-test N (%) correct* |
Post-test N (%) correct* |
p-value** | Pre-test N (%) correct* |
Post-test N (%) correct* |
p-value** |
| Which is true about vaccines? | 331 (49.6) | 357 (53.5) | 0.15 | 282 (70.3) | 283 (70.6) | 0.94 |
| Vaccines are constantly studies and monitored to make sure they are safe | 617 (92.5) | 625 (93.7) | 0.39 | 381 (95.0) | 388 (96.8) | 0.21 |
| Which of the following is NOT a way vaccines are made? | 92 (14.0) | 167 (25.3) | <0.001 | 73 (18.2) | 57 (14.2) | 0.13 |
| By getting a vaccination, you protect others as well as yourself | 509 (76.3) | 609 (91.3) | <0.001 | 348 (86.8) | 376 (93.8) | 0.001 |
| What are the 4 vaccines recommended for teens age 11–18? | 140 (21.0) | 443 (66.4) | <0.001 | 155 (38.7) | 271 (67.6) | <0.001 |
| Attitudes | ||||||
| Infectious diseases, like the flu, could make me sick | 625 (93.7) | 643 (96.4) | 0.02 | 384 (95.8) | 394 (98.3) | 0.04 |
| Infectious diseases, like the flu, can be serious | 561 (84.1) | 602 (90.2) | 0.001 | 366 (91.3) | 381 (95.0) | 0.04 |
| Vaccines, like the flu vaccine, could make me sick | 373 (55.9) | 397 (59.5) | 0.18 | 170 (42.4) | 202 (50.4) | 0.02 |
| Vaccines can stop me from getting sick | 524 (78.6) | 583 (87.4) | <0.001 | 314 (78.3) | 310 (77.3) | 0.73 |
| I am interested in getting the vaccines for teenagers | 467 (70.0) | 553 (82.9) | <0.001 | 310 (77.3) | 340 (84.8) | 0.01 |
Percent answering the question correctly
Bolded p-values are statistically significant at alpha=0.05
DISCUSSION
The aims of this project were to 1) develop a theory-based intervention to increase adolescent vaccination rates among middle- and high-school students in eastern Georgia and 2) increase vaccine-related knowledge and positive attitudes regarding vaccination among students and parents. This project is currently ongoing and the primary outcome of adolescent vaccine coverage will be reported at a later date. Development of an effective, theory-based educational intervention that was well received by the target audience was a fundamental step toward achieving our study goals. Year two evaluation results indicated that our intervention development methods were successful in creating a theory-based educational intervention that was culturally relevant, developmentally appropriate for adolescents, met the literacy needs of our target parent audience, and was acceptable and feasible to implement with teachers in schools. The brochure seemed to resonate positively among parents who recalled receiving it. We found that parents reported that the brochure increased their knowledge of adolescent vaccination and facilitated further discussion about adolescent vaccines with their friends and family. We found that there was a high baseline level of knowledge about infectious diseases and vaccines in both the middle- and high-school students. We speculate that the increase in students responding that vaccines could make them sick may be because of an increase in the knowledge of potential side-effects of vaccines, such as fever which they may have interpreted as being “made sick”. We found that our teacher-delivered adolescent curriculum improved adolescents’ knowledge and attitudes toward vaccination. While scare tactics, such as the “gross” pictures used in the curriculum may not be effective behavior change tools (Peters, Ruiter, & Kok, 2013) we elected to retain these features since they were recommended by students in our focus group as a way to keep students’ attention.
This research was distinctive in multiple respects. First, no previous interventions have been designed to improve uptake and attitudes toward all four vaccines recommended for adolescents. In light of low vaccination rates of adolescents, particularly for HPV and influenza vaccine, in the U.S., lessons learned from this project are particularly important. We have previously demonstrated that educational interventions targeting adolescents and their parents serve to improve uptake of influenza vaccine among adolescents (Gargano et al., 2011) and attitudes toward influenza vaccine in both parents and adolescents (Painter, Sales, Pazol, Grimes, et al., 2010; Painter, Sales, Pazol, Wingood, et al., 2010; Painter et al., 2011; Sales et al., 2011). Second, there are relatively few interventions described in the literature that apply health behavior theory to the fullest extent (Painter, Borba, Hynes, Mays, & Glanz, 2008; Painter, Sales, Pazol, Grimes, et al., 2010). Finally, to our knowledge, this study is the first to extensively engage middle- and high-school students through a science teacher-delivered curriculum to increase knowledge and positive attitudes toward all recommended adolescent vaccines.
Implementation of this project is ongoing. Future work will address how the parent brochure impacts parental attitudes and receipt or intention for their adolescent to receive the recommended vaccines. Also, future work will assess if there was a difference in receipt or intention to receive the recommended adolescent vaccines between the parent only intervention arm and the parent and adolescent intervention arm.
Limitations
This intervention has several limitations. First is the compromise of intervention fidelity, which is the degree to which the delivery of instruction in the way that it was designed to be delivered was the same in all classrooms, a common limitation in intervention research when interventions are implemented in multiple venues (Kilbourne, Neumann, Pincus, Bauer, & Stall, 2007). Second, we had an overall low response rate for the parent survey. Third, no evaluation data were collected from the teachers. Fourth, since a convenience sample was taken those that were interested in vaccines may have been more likely to participate than those who were not, potentially biasing our focus group findings. Finally, this intervention may not be generalizable beyond a high minority population in eastern Georgia. Future research is needed to determine whether the educational components of our intervention could be easily adapted and disseminated among other populations.
Conclusions
We believe that the degree of theory use was an important strength of this study and that practitioners could benefit from an example of how to use the HBM and TRA as tools to guide intervention curriculum and educational material development for their respective audiences. As the number of vaccines recommended for adolescents increases, the need to develop better ways to increase adolescent vaccination coverage will become even more important. The conceptual framework and materials developed should assist public health practitioners and healthcare providers in devising strategies that increase vaccination coverage and improve general acceptance of vaccines by adolescents.
Supplementary Material
Acknowledgments
We would like to thank Dr. Ketty M. Gonzalez, District Health Director for the East Central Health District, school district, schools that assisted us in our focus groups and schools that participated in our interventions. This project is funded by the Centers for Disease Control and Prevention grant 5UO1IP000413. Dr. Painter was also supported by grant Award Number T32AI074492 from the National Institute of Allergy and Infectious Disease, National Institutes of Health. Dr. Sales was supported by grant K01 MH085506 from the National Institutes of Mental Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Centers for Disease Control and Prevention.
References
- Allison MA, Reyes M, Young P, Calame L, Sheng X, Weng HY, Byington CL. Parental attitudes about influenza immunization and school-based immunization for school-aged children. Pediatr Infect Dis J. 2010;29(8):751–755. doi: 10.1097/INF.0b013e3181d8562c. [DOI] [PubMed] [Google Scholar]
- Caro JJ, Getsios D, El-Hadi W, Payne K, O’Brien JA. Pertussis immunization of adolescents in the United States: an economic evaluation. Pediatr Infect Dis J. 2005;24(5 Suppl):S75–82. doi: 10.1097/01.inf.0000160918.72953.51. doi: 00006454-200505001-00015 [pii] [DOI] [PubMed] [Google Scholar]
- Caro JJ, Moller J, Getsios D, Coudeville L, El-Hadi W, Chevat C, Caro I. Invasive meningococcal disease epidemiology and control measures: a framework for evaluation. BMC Public Health. 2007;7:130. doi: 10.1186/1471-2458-7-130. doi: 1471-2458-7-130[pii] 10.1186/1471-2458-7-130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpenter LR, Lott J, Lawson BM, Hall S, Craig AS, Schaffner W, Jones TF. Mass distribution of free, intranasally administered influenza vaccine in a public school system. Pediatrics. 2007;120(1):e172–178. doi: 10.1542/peds.2006-2603. doi: peds.2006-2603[pii] 10.1542/peds.2006-2603. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Immunization Schedules. 2012 Jun; Retrieved October 16, 2012, from http://www.cdc.gov/vaccines/schedules/hcp/child-adolescent.html.
- Centers for Disease Control and Prevention. National and state vaccination coverage among adolescents aged 13–17 years - United States, 2012. MMWR Morb Mortal Wkly Rep. 2013;62(34):685–693. [PMC free article] [PubMed] [Google Scholar]
- Champion V, Skinner C. The Health Belief Model. 4. San Franisco: Jossey-Bass; 2008. [Google Scholar]
- Chan SS, Yan Ng BH, Lo WK, Cheung TH, Hung Chung TK. Adolescent girls’ attitudes on human papillomavirus vaccination. J Pediatr Adolesc Gynecol. 2009;22(2):85–90. doi: 10.1016/j.jpag.2007.12.007. doi: S1083-3188(07)00375-0 [pii] 10.1016/j.jpag.2007.12.007. [DOI] [PubMed] [Google Scholar]
- Clayton EW, Hickson GB, Miller CS. Parents’ responses to vaccine information pamphlets. Pediatrics. 1994;93(3):369–372. [PubMed] [Google Scholar]
- Coates TJ, Peterson AC, Perry C. Promoting Adolescent Health A Dialog on Research and Practice. New York: Academic Press; 1982. [Google Scholar]
- Daley EM, Buhi ER, Baldwin J, Lee JH, Vadaparampil S, Abrahamsen M, Giuliano A. Men’s responses to HPV test results: development of a theory-based survey. Am J Health Behav. 2009;33(6):728–744. doi: 10.5555/ajhb.2009.33.6.728 [pii] [PMC free article] [PubMed] [Google Scholar]
- Data Center, Kids Count. Georgia, Students eligible to receive free or reduced price lunch (Percent) - 2012. 2012 Retrieved November 26, 2012, from http://datacenter.kidscount.org/data/bystate/Rankings.aspx?state=GA&ind=696.
- Fahlman MM, Dake JA, McCaughtry N, Martin J. A pilot study to examine the effects of a nutrition intervention on nutrition knowledge, behaviors, and efficacy expectations in middle school children. J Sch Health. 2008;78(4):216–222. doi: 10.1111/j.1746-1561.2008.00289.x. doi: JOSH289 [pii] 10.1111/j.1746-1561.200800289.x. [DOI] [PubMed] [Google Scholar]
- Gargano LM, Pazol K, Sales JM, Painter JE, Morfaw C, Jones LM, Hughes JM. Multicomponent interventions to enhance influenza vaccine delivery to adolescents. Pediatrics. 2011;128(5):e1092–1099. doi: 10.1542/peds.2011-0453. doi: peds.2011-0453[pii] 10.1542/peds.2011-0453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henderson M, Wight D, Raab GM, Abraham C, Parkes A, Scott S, Hart G. Impact of a theoretically based sex education programme (SHARE) delivered by teachers on NHS registered conceptions and terminations: final results of cluster randomised trial. BMJ. 2007;334(7585):133. doi: 10.1136/bmj.39014.503692.55. doi: bmj.39014.503692.55 [pii] 10.1136/bmj.39014.503692.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henry RL, Gibson PG, Vimpani GV, Francis JL, Hazell J. Randomized controlled trial of a teacher-led asthma education program. Pediatr Pulmonol. 2004;38(6):434–442. doi: 10.1002/ppul.20095. [DOI] [PubMed] [Google Scholar]
- Insinga RP, Dasbach EJ, Elbasha EH, Puig A, Reynales-Shigematsu LM. Cost-effectiveness of quadrivalent human papillomavirus (HPV) vaccination in Mexico: a transmission dynamic model-based evaluation. Vaccine. 2007;26(1):128–139. doi: 10.1016/j.vaccine.2007.10.056. doi: S0264-410X(07)01226-1 [pii] 10.1016/j.vaccine.2007.10.056. [DOI] [PubMed] [Google Scholar]
- Jacobson TA, Thomas DM, Morton FJ, Offutt G, Shevlin J, Ray S. Use of a low-literacy patient education tool to enhance pneumococcal vaccination rates. A randomized controlled trial. JAMA. 1999;282(7):646–650. doi: 10.1001/jama.282.7.646. doi: joc90357 [pii] [DOI] [PubMed] [Google Scholar]
- Kahn JA, Rosenthal SL, Jin Y, Huang B, Namakydoust A, Zimet GD. Rates of human papillomavirus vaccination, attitudes about vaccination, and human papillomavirus prevalence in young women. Obstet Gynecol. 2008;111(5):1103–1110. doi: 10.1097/AOG.0b013e31817051fa. 111/5/1103 [pii] 10.1097/AOG.0b013e31817051fa. [DOI] [PubMed] [Google Scholar]
- Kilbourne AM, Neumann MS, Pincus HA, Bauer MS, Stall R. Implementing evidence-based interventions in health care: application of the replicating effective programs framework. Implement Sci. 2007;2:42. doi: 10.1186/1748-5908-2-42. doi: 1748-5908-2-42 [pii] 10.1186/1748-5908-2-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lind C, Anderson B, Oberle K. Ethical issues in adolescent consent for research. Nurs Ethics. 2003;10(5):504–511. doi: 10.1191/0969733003ne632oa. [DOI] [PubMed] [Google Scholar]
- Luce BR, Zangwill KM, Palmer CS, Mendelman PM, Yan L, Wolff MC, Belshe RB. Cost-effectiveness analysis of an intranasal influenza vaccine for the prevention of influenza in healthy children. Pediatrics. 2001;108(2):E24. doi: 10.1542/peds.108.2.e24. [DOI] [PubMed] [Google Scholar]
- Montano DE. Predicting and understanding influenza vaccination behavior. Alternatives to the health belief model. Med Care. 1986;24(5):438–453. doi: 10.1097/00005650-198605000-00007. [DOI] [PubMed] [Google Scholar]
- Monto AS, Davenport FM, Napier JA, Francis T., Jr Effect of vaccination of a school-age population upon the course of an A2-Hong Kong influenza epidemic. Bull World Health Organ. 1969;41(3):537–542. [PMC free article] [PubMed] [Google Scholar]
- Monto AS, Davenport FM, Napier JA, Francis T., Jr Modification of an outbreak of influenza in Tecumseh, Michigan by vaccination of schoolchildren. J Infect Dis. 1970;122(1):16–25. doi: 10.1093/infdis/122.1-2.16. [DOI] [PubMed] [Google Scholar]
- Neil AL, Christensen H. Efficacy and effectiveness of school-based prevention and early intervention programs for anxiety. Clin Psychol Rev. 2009;29(3):208–215. doi: 10.1016/j.cpr.2009.01.002. doi: S0272-7358(09)00003-8 [pii] 10.1016/j.cpr.2009.01.002. [DOI] [PubMed] [Google Scholar]
- Noar SM, Zimmerman RS. Health Behavior Theory and cumulative knowledge regarding health behaviors: are we moving in the right direction? Health Educ Res. 2005;20(3):275–290. doi: 10.1093/her/cyg113. doi: cyg113 [pii] 10.1093/her/cyg113. [DOI] [PubMed] [Google Scholar]
- Painter JE, Borba CP, Hynes M, Mays D, Glanz K. The use of theory in health behavior research from 2000 to 2005: a systematic review. Ann Behav Med. 2008;35(3):358–362. doi: 10.1007/s12160-008-9042-y. [DOI] [PubMed] [Google Scholar]
- Painter JE, Sales JM, Pazol K, Grimes T, Wingood GM, DiClemente RJ. Development, theoretical framework, and lessons learned from implementation of a school-based influenza vaccination intervention. Health Promot Pract. 2010;11(3 Suppl):42S–52S. doi: 10.1177/1524839909360171. doi: 11/3_suppl/42S [pii] 10.1177/1524839909360171. [DOI] [PubMed] [Google Scholar]
- Painter JE, Sales JM, Pazol K, Wingood GM, Windle M, Orenstein WA, DiClemente RJ. Psychosocial correlates of intention to receive an influenza vaccination among rural adolescents. Health Educ Res. 2010;25(5):853–864. doi: 10.1093/her/cyq037. doi: cyq037 [pii] 10.1093/her/cyq037. [DOI] [PubMed] [Google Scholar]
- Painter JE, Sales JM, Pazol K, Wingood GM, Windle M, Orenstein WA, DiClemente RJ. Adolescent attitudes toward influenza vaccination and vaccine uptake in a school-based influenza vaccination intervention: a mediation analysis. J Sch Health. 2011;81(6):304–312. doi: 10.1111/j.1746-1561.2011.00595.x. [DOI] [PubMed] [Google Scholar]
- Peters GJ, Ruiter RA, Kok G. Threatening communication: a critical re-analysis and a revised meta-analytic test of fear appeal theory. Health Psychol Rev. 2013;7(Suppl 1):S8–S31. doi: 10.1080/17437199.2012.703527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts ME, Gerrard M, Reimer R, Gibbons FX. Mother-daughter communication and human papillomavirus vaccine uptake by college students. Pediatrics. 2010;125(5):982–989. doi: 10.1542/peds.2009-2888. doi: peds.2009-2888 [pii] 10.1542/peds.2009-2888. [DOI] [PubMed] [Google Scholar]
- Sales JM, Painter JE, Pazol K, Gargano LM, Orenstein W, Hughes JM, DiClemente RJ. Rural parents’ vaccination-related attitudes and intention to vaccinate middle and high school children against influenza following educational influenza vaccination intervention. Hum Vaccin. 2011;7(11):1146–1152. doi: 10.4161/hv.7.11.17891. doi: 17891 [pii] 10.4161/hv.7.11.17891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- US Census Bureau. School Enrollment - Social and Economic Characteristics fo Students. 2011 October 2011. Retrieved October 16, 2012, from http://www.census.gov/hhes/school/data/cps/2011/tables.html.
- Woodhall SC, Lehtinen M, Verho T, Huhtala H, Hokkanen M, Kosunen E. Anticipated acceptance of HPV vaccination at the baseline of implementation: a survey of parental and adolescent knowledge and attitudes in Finland. J Adolesc Health. 2007;40(5):466–469. doi: 10.1016/j.jadohealth.2007.01.005. doi: S1054-139X(07)00022-5 [pii] 10.1016/j.jadohealth.2007.01.005. [DOI] [PubMed] [Google Scholar]
- Zhou F, Santoli J, Messonnier ML, Yusuf HR, Shefer A, Chu SY, Harpaz R. Economic evaluation of the 7-vaccine routine childhood immunization schedule in the United States, 2001. Arch Pediatr Adolesc Med. 2005;159(12):1136–1144. doi: 10.1001/archpedi.159.12.1136. doi: 159/12/1136 [pii] 10.1001/archpedi.159.12.1136. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


