Abstract
Objective
To examine the extent to which a clinical intervention resulted in reduced body mass index (BMI) z-scores among 2–12 year old children compared to routine practice (treatment as usual, TAU).
Methods
The Massachusetts Childhood Obesity Research Demonstration project (MA-CORD) is a multifaceted initiative to prevent childhood obesity among low-income children. In the federally qualified community health centers (FQHC) of two communities (Intervention Site #1 and #2), we implemented (1) pediatric weight management training; (2) electronic decision supports for clinicians; (3) on-site Healthy Weight Clinics; (4) community health worker integration; and (5) healthful clinical environment changes. One FQHC in a demographically-matched community served as the TAU site. Using electronic health records, we assessed BMI z-scores and used linear mixed models to examine BMI z-score change over 2 years in each intervention site compared to a TAU site.
Results
Compared to children in the TAU site (n=2286), children in Intervention site #2 (n=1368) had a significant decline in BMI z-scores following the start of the intervention (−0.16 units/year; 95% CI: −0.21, −0.12). We found no evidence of an effect in Intervention site #1 (n=111).
Conclusions
The MA-CORD clinical interventions were associated with modest improvement in BMI z-scores in one of two intervention communities compared to a TAU community.
Keywords: childhood obesity, clinical care, intervention, community health
Introduction
After increasing steadily for three decades, the national childhood obesity prevalence in the United States (US) appears to have leveled off among children <12 years of age.1 Yet, childhood obesity prevalence remains at historically high levels and progress has not been equitably distributed. Racial and ethnic minority children, and children from low-income families and neighborhoods continue to bear a disproportionate share of the burden of obesity.2, 3 In 2011, in an effort to reduce the substantial disparities in obesity prevalence among its underserved pediatric populations, Massachusetts launched the MA Childhood Obesity Research Demonstration (MA-CORD) project, a multifaceted initiative, funded by the Centers for Disease Control and Prevention,4 to prevent and manage obesity among children ages 2–12 years living in low-income communities.5 The study implemented evidence-informed interventions across several sectors working with low-income children including pediatric clinical care delivered in federally qualified community health centers (FQHCs).5, 6
Health centers in low-income communities are well-positioned to have an impact on childhood obesity. FQHCs often serve as patient-centered medical homes offering valuable opportunities for screening and detection of overweight and obesity as well as services to manage the subsequent course of health and disease for children diagnosed with obesity.7 The increasing use of electronic health records in community-based health centers have been shown to improve the quality of care for children with obesity and for accelerating the use of Expert Committee evidence on obesity screening and management practices by primary care providers.8, 9 Mounting evidence also suggests that community health workers (CHWs), who are increasingly embedded into chronic disease prevention teams in FQHCs, can link clinical and community systems and programs and support family behavior change for obesity management.10–13
This manuscript reports the main outcomes of a quasi-experimental trial examining the extent to which a comprehensive clinical intervention delivered at two FQHCs as part of MA-CORD improved body mass index (BMI) outcomes among low-income children ages 2–12 years. We hypothesized that children receiving care in the two intervention FQHCs would demonstrate improved age- and sex-specific BMI z-scores over a 2-year period, compared to those receiving routine care (treatment as usual [TAU]) in a FQHC of a demographically-matched Massachusetts community.
Methods
Study overview
We conducted a quasi-experimental trial in two FQHCs — one in each of two Massachusetts communities selected to participate as intervention sites for MA-CORD based on size, per capita income, and prevalence of childhood overweight and obesity. The conceptual framework, intervention design and evaluation methods for the larger MA-CORD initiative have been described in detail.4–6 Briefly, MA-CORD spanned several sectors including FQHCs; the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC); public elementary and middle schools; after-school settings; and the broader community. In each sector in both communities, we implemented evidence-based programs to promote childhood obesity prevention.
Here we summarize the clinical intervention components that were part of MA-CORD and their effectiveness. In the two intervention FQHCs we implemented a systematic, comprehensive clinical intervention. One FQHC in a demographically-matched Massachusetts community served as the comparison. The primary outcome was improvement in child age- and sex-specific BMI z-score over a two-year intervention period using electronic health records from the two intervention and one TAU FQHC. Secondary outcomes included changes in BMI z-score and percent of the 95th percentile (BMIp95) among children referred to the Healthy Weight Clinics in the intervention FQHCs.
Eligibility and Recruitment
The study protocol was approved by the human subjects committees of the participating institutions. All well-children aged 2–12 years receiving care at the three FQHCs and residing in the community were eligible for the longitudinal analyses of BMI changes. Children with severe chronic health conditions (e.g. congenital and chromosomal anomalies) were excluded. Children with a BMI ≥ 85th percentile were eligible for referral to the Healthy Weight Clinics. We received a waiver of informed consent to use longitudinal electronic health record data.
Clinical Intervention
Evidence-informed interventions were implemented across both intervention FQHCs (Figure 1).14–16 Intervention components aimed to improve primary and secondary prevention of childhood obesity and included: 1) advanced training to FQHC staff on clinical quality improvement and obesity prevention, assessment, and management; 2) computerized, point-of-care decision support tools for clinicians on obesity management; 3) implementation of multi-disciplinary weight management programs within the FQHCs, e.g. Healthy Weight Clinics; 4) integrating CHWs into the primary care and Healthy Weight Clinic teams; and 5) health center environmental changes to support behavior change modification.
Figure 1.
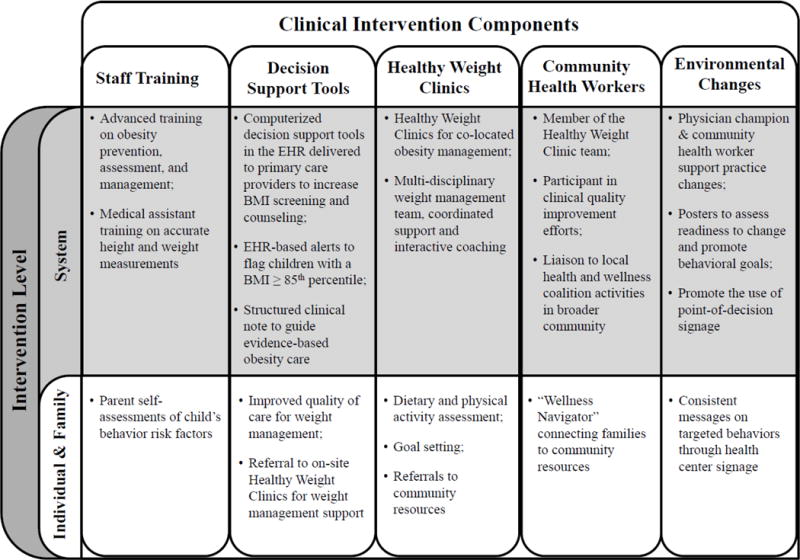
Clinical Intervention Components in the MA-CORD Study
Staff Training
Staff from the two intervention FQHCs received advanced training on obesity prevention, assessment, and management through a combination of a modified Breakthrough Series™ Collaborative17 and individualized team coaching to assist with implementation of evidence based practices.5 Participants included a physician champion, clinical staff such as nurses or medical assistants, administrative leaders, CHWs, and representatives from local health and wellness coalitions. Training included: 1) quality improvement methods; 2) methods of encouraging health behavior change, including motivational interviewing; 3) best practices in treating childhood obesity; and 4) Be Our Voice™18 Advocacy training, which engages and trains clinicians to be advocates of children in the fight against childhood obesity. Full-day live learning sessions were held every 6 months supplemented by monthly interactive webinars and individualized coaching.
Point-of-Care Clinical Decision Support Tools
To support evidence-based management of pediatric obesity, existing electronic health records in each health center were modified to deploy a computerized, point-of-care, decision support alert to pediatricians at the time of a well-child care visit for a child with a BMI ≥ 85th percentile shown to be effective in improving quality of care for overweight children.8,9 The alert contained links to the child’s growth chart and a link to a pre-populated, standardized note specific for obesity that included the ability to: 1) document and code for BMI percentile and weight status diagnosis; 2) document and code for nutrition and physical activity counseling; 3) place referrals to the on-site Healthy Weight Clinics for weight management support; and 4) place orders for obesity-related laboratory studies, if appropriate.
Healthy Weight Clinics
In each intervention FQHC, we worked to develop a multi-disciplinary Healthy Weight Clinic.15 The Healthy Weight Clinics were staffed by a physician, a nutritionist, and a CHW who met with each patient and family in tandem during a single, in-person, 90-minute clinical encounter. Primary care providers referred eligible patients (BMI ≥ 85th percentile, ages 2–18) to this specially trained, primary care team. Patients participating in the Healthy Weight Clinic engaged in dietary and physical activity assessment, goal-setting, and were referred to community resources to support healthy lifestyles. We aimed for patients to be followed in the Healthy Weight Clinic bi-monthly for six months, followed by monthly for an additional six months for a total of approximately 27 hours of contacts during the 1-year period. Clinicians used the Next Steps Guide from the National Institute for Children’s Health Quality to guide their counseling at each follow up visit.19
Community Health Workers
Each intervention FQHC employed a full-time CHW as a member of the primary care and multi-disciplinary obesity management teams.5 The purpose of the CHWs was to: 1) serve as a member of the Healthy Weight Clinic, counseling patients referred to the program; 2) participate in the health center’s quality improvement efforts; 3) serve as “Wellness Navigators” connecting children and families with community resources for behavior change; and 4) act as a liaison to local health and wellness coalition activities in the broader community. They also catalogued local community resources to refer patients to and conducted parent education and training sessions on the MA-CORD target behaviors. The five target behaviors of MA-CORD were: 1) replacement of water for sugary drinks; 2) ≤2 hours of screen time per day; 3) ≥1 hour of physical activity per day; 4) replacement of sugary, salty, fried and fast food with fruits and vegetables; and 5) ≥11 hours of sleep per day for 2–5 year olds and ≥10 hours for 6–12 year olds.
Environmental Changes
To improve the healthfulness of the clinical environment we worked with health center administrators and the CHWs to implement clinical environmental changes. Changes were intended to support lifestyle modifications and the health of patients, visitors and staff. Following a physical space environmental assessment completed by research staff and health center staff, we developed a menu of options in which the center could improve. These included signage related to targeted behavior changes and promotion of water, access to healthy food options within the building, and walking challenges.
Treatment as Usual Site
TAU participants at the comparison FQHC received the current standard of care offered by their pediatric office. No new decision support tools, trainings, Healthy Weight Clinics, or patient educational materials for obesity were made available in the TAU site during the intervention period. All new patient educational materials were made available free of charge to the comparison community at study completion.
Outcome Measurements
The primary outcome of the trial was change in age- and sex-specific BMI z-score throughout the two-year intervention period obtained from children’s electronic health record from well-child care visits. Medical assistants at each health center measured height and weight according to the written standardized protocol of the health centers and entered the information into the electronic health record. BMI and age- and sex-specific BMI z-score were calculated at each clinical visit. We culled longitudinal data from the electronic health records of all three health centers for 6,624 children, ages 2–12 years, who received care at any of the three health centers between October 2010 (approximately two years prior to the start of the intervention) through August 2015 (approximately twenty months after the start of the intervention and the date of our final electronic health record data pull). To be included in the analyses, children needed to reside in the community, have vital demographic information available (e.g. age, sex, and race/ethnicity), and have at least two visits in which height and weight were measured. These included at least one visit prior to intervention start in the fall of 2013 and at least one visit after intervention start. The sample size for our longitudinal analyses included these 3,765 children with 14,452 weight and height measures (Figure 2).
Figure 2.

Participant Flow for the MA-CORD Clinical Quasi-Experimental Trial
The secondary outcomes of the study were changes in BMI z-score and percent of the 95th percentile (BMIp95)20–23 among children referred and seen for at least 2 visits in the Healthy Weight Clinic. We refer to a BMI that is expressed as a percentage of the 95th percentile as BMIp95; values can range from <50 (for very thin children) to >220 (for very heavy children), and a child with a BMI equal to the 95th percentile would have a BMIp95 of 100%.20
Other Measures
From the electronic health record we also extracted information on clinical visit dates, child’s date of birth, sex, and race/ethnicity. To assess families’ exposure to the MA-CORD interventions outside of the clinical setting, we conducted a survey at baseline of parents with children ages 2.0 to 12.9 years of age who received their well-child care at Intervention Sites 1 and 2. The surveys were available in English, Spanish and Portuguese and were administered by trained research assistants during well-child visits or by telephone immediately following the visits. The survey assessed whether the family had a child that was enrolled in WIC, enrollment of the child in the local public elementary or middle school, and enrollment of the child in an after-school program in the community.
Statistical Analysis
We used a quasi-experimental design with a TAU group and assessed longitudinal changes in BMI z-score of individual children at each of the FQHCs in the two intervention communities compared to children in the TAU site. To assess BMI z-score, we used linear mixed-effects regression models to account for clustering of observations over time within individual and within community. The model for BMI z-score included indicator variables for time, intervention arm (Intervention site #1, Intervention site #2, or TAU), child age, child race/ethnicity and sex, as well as a time-after variable indicating a change after the intervention begins, with interactions for each intervention arm. These interaction terms test for changes in BMI z-scores after the intervention starts in the intervention sites compared to the TAU site. We present minimally unadjusted (child age and sex only) and fully adjusted (child age, sex, and race/ethnicity) multiple regression estimates.
The Healthy Weight Clinic study used a quasi-experimental design, where each child served as their own control, and measured BMI changes over time. The Healthy Weight Clinic analyses did not have a control site because these multidisciplinary clinics were not implemented in the TAU site. To assess BMI z-score and BMIp95 we used linear mixed-effects models to account for clustering of visits by child. Models were adjusted for child age, sex and race/ethnicity. All analyses were performed using the SAS System, Version 9.3 (Cary, NC) using PROC MIXED.
Results
Figure 2 shows the participant flow of the study. The sample size for our main analyses and outcomes included 3,765 children with 14,452 weight and height measures. Table 1 shows baseline characteristics of the study sample across the three FQHCs. Compared to children in the TAU site, both Intervention sites had a higher percentage of Hispanic children, and children in Intervention Site #1 were slightly older.
Table 1.
Baseline Characteristics of Children Receiving Care in the MA-CORD Federally Qualified Community Health Centers, by Intervention Assignment.
| Baseline Participant Characteristics | Intervention Site #1 N=111 |
Intervention Site #2 N=1,368 |
TAU Site N=2,286 |
P-value |
|---|---|---|---|---|
| Mean (SD) or N (%) | ||||
| Age at baseline, years | 6.5 (2.9) | 5.8 (3.0) | 6.0 (3.0) | 0.03 |
| Male, n (%) | 55 (49.5) | 689 (50.4) | 1203 (52.6) | 0.37 |
| Race/ethnicity, n (%) | < 0.0001 | |||
| White, non-Hispanic | 15 (13.5) | 240 (17.5) | 441 (19.3) | |
| Hispanic/Latino | 84 (75.7) | 892 (65.2) | 1100 (48.1) | |
| Black, non-Hispanic | 6 (5.4) | 221 (16.5) | 236 (10.3) | |
| Asian | 6 (5.4) | 8 (0.6) | 507 (22.2) | |
| Other, non-Hispanic | 0 (0) | 7 (0.5) | 2 (0.1) | |
| BMI z-score | 0.81 (1.2) | 0.83 (1.1) | 0.86 (1.1) | 0.73 |
| BMI Percentile | 0.29 | |||
| < 85th percentile | 71 (64.0) | 781 (57.0) | 1270 (55.5) | |
| ≥ 85th to < 95th percentile | 12 (10.8) | 252 (18.5) | 450 (19.7) | |
| ≥ 95th percentile | 28 (25.2) | 335 (24.5) | 566 (24.8) | |
Program Implementation
Throughout the study period, Intervention site #1 faced several institutional challenges that prevented full implementation of the intervention and led to substantially fewer children receiving primary care at the FQHC.24 Over the two-year intervention period, the FQHC in Intervention Site #1 experienced a high level of attrition in their senior leadership and clinical providers, re-located their facility, and ended their accredited family medicine residency program. These challenges prevented the FQHC from attracting and retaining pediatric patients and prevented the full implementation of the Healthy Weight Clinic in their practice. Thus, our evaluation of the Healthy Weight Clinic only included children in Intervention Site #2.
Overlap with MA-CORD Multi-Sectoral Interventions
From July 2012 through April 2013, we sampled 92 parents of children in Intervention Site #1 and 240 parents in Intervention Site #2 to assess potential overlap with the MA-CORD activities in WIC, schools, and after-school programs. In Intervention site #1, 15/22 (68%) families with children aged 2 to < 5 years reported receiving WIC benefits. Among parents with school aged (≥ 6 years) children in Intervention Site #1, 60/62 (97%) reported their child was enrolled in the communities’ public school and 10/62 (16%) reported their child attended an after-school program. In Intervention site #2, 80/103 (78%) families with children aged 2 to < 5 years reported receiving WIC benefits. Among parents with school aged children (≥ 6 years) in Intervention Site #2, 108/114 (95%) reported that their child was enrolled in the communities’ public school and 7/114 (6%) reported their child attended an after-school program.
Main Outcomes
Prior to the start of the intervention, the mean (SD) BMI z-score of children was 0.81 (1.2) in Intervention Site #1, 0.83 (1.1) in Intervention Site #2, and 0.86 (1.1) in the TAU site. In models adjusted for child age and sex, we found that compared to children in the TAU site, children in Intervention Site #2 had lower BMI z-scores after the intervention start (−0.16 units/year; 95% Confidence Interval: −0.21, −0.12) (Table 2). Further adjustments for child race/ethnicity did not change the estimates. Compared to children in the TAU site, children in Intervention Site #1 did not have a significant difference in their BMI z-scores over time (−0.02 units/year; 95% CI: − 0.16, 0.12).
Table 2.
Changes in Body Mass Index Z-Score from Pre-Intervention to Post-Intervention Implementation, by Intervention Assignment (N=3,765 patients, 14,452 visits).
| Main Outcome | Unadjusted change in BMI z-score/year after intervention start β (95% CI)* | P-value‡ | Adjusted change in BMI z-score/year after intervention start** β (95% CI) | P-value‡ |
|---|---|---|---|---|
| BMI z-score (units) | ||||
| Intervention Site #2 | −0.16 −0.21,−0.12) | < 0.0001 | −0.16 −0.21,−0.12) | < 0.0001 |
| Compared to TAU Site | Reference | Reference |
Generalized linear mixed effects models with all models corrected for clustering by community and correlation within individual.
Adjusted for child age, sex, and race/ethnicity.
Type 3 overall p-value evaluates equality of effects across interventions as obtained from the time*arm interaction term.
Healthy Weight Clinic Outcomes
Approximately 187 children, ages 2.0 to 12.9 years were referred to the Healthy Weight Clinic at Intervention Site #2 and completed a mean (SD) of 2.56 (1.9) visits with the multi-disciplinary team (Table 3). At the time of referral, the mean (SD) age of children was 7.9 (3.0) years; mean (SD) BMI z-score was 2.01 (0.63), and mean (SD) BMIp95 was 111.2% (17.6). In minimally- and fully-adjusted models, we observed a decrease in BMI z-score among children in the Healthy Weight Clinic. In models adjusted for child age, sex, and race/ethnicity, BMI z-score decreased by −0.07 units (95% CI: −0.10, −0.03; p <0.001) over the course of children’s visits to the clinic (Table 4). Similarly, in models adjusted for child age, sex, and race/ethnicity, we observed a non-significant decrease of 0.87% (95% CI: −1.82, 0.09; p=0.07) in BMIp95 over the course of the visits to the clinic.
Table 3.
Sociodemographic characteristics of 187 children seen in the Healthy Weight Clinic between November 1, 2012 and June 30, 2014.
| Healthy Weight Clinic Patients (n = 187 patients/1288 visits) |
|
|---|---|
| Child Level Characteristics | Mean (SD) or N (%) |
| Age, mean ± SD, years | 7.9 (3.0) |
| Age, 2–5 years, n (%) | 36 (19.3%) |
| Boy, n (%) | 94 (48.1%) |
| Race/ethnicity, n (%) | |
| White, non-Hispanic | 21 (11.2%) |
| Black, non-Hispanic | 21 (11.2%) |
| Hispanic/Latino | 145 (77.5%) |
| MassHealth/Medicaid, n (%) | 61 (32.6%) |
| BMI (kg/m2) at referral, mean ± SD | 23.2 (4.8) |
| BMI z-score at referral, mean ± SD | 2.01 (0.63) |
| BMIp95 at referral, mean ± SD | 111.2 (17.6) |
| Number of Healthy Weight Clinic visits, mean ± SD | 2.56 (1.9) |
| Time after referral at the last visit in days, mean ± SD | 102.63 (115.8) |
Table 4.
Change in BMI z-score and BMIp95 for 187 children referred to the Healthy Weight Clinic in Intervention Site #2 between November 1, 2012 and June 30, 2014.
| Main Outcomes | Unadjusted change in BMI z-score/year after intervention start β (95% CI) | P-value | Adjusted change in BMI z-score/year after intervention start** β (95% CI) | P-value |
|---|---|---|---|---|
| BMI z-score | −0.10 (−0.13,−0.10) | < 0.001 | −0.07 (−0.10,−0.03) | < 0.001 |
| BMIp95 | −0.18 (−0.68, 0.32) | 0.48 | −0.87 (−1.82, 0.09) | 0.07 |
Adjusted for child age, sex, and race/ethnicity.
Discussion
In this multi-level intervention to prevent and manage childhood obesity in Massachusetts FQHCs, we observed a modest improvement in BMI z-scores in one of two intervention communities versus a TAU site. The magnitude of improvement in BMI z-score was −0.16 units/year and the effects were robust to adjustment for child age, sex, and race/ethnicity. In this same intervention site, we implemented a Healthy Weight Clinic to manage children with a BMI ≥ 85th percentile and found that BMI z-score decreased by −0.07 units over the course of children’s visits to the clinic. We did not observe differences in BMI z-score among children in the other intervention site versus the TAU site, but substantial institutional challenges led to fewer children being seen for primary care during the intervention period and other barriers prevented the site from fully adhering to the intervention protocol. Despite the challenges to implementation, our findings lend support to a growing body of evidence that improving the quality of obesity-related care in community-based settings that see a large percentage of low-income children could lead to improvements in BMI for all children and reduction in BMI among those with overweight and obesity.
Our findings also extend the existing literature by showing that the components we implemented at the intervention FQHCs may be feasible and effective in low-resource settings. For example, Expert Committee guidelines and systematic reviews recommend universal childhood obesity screening, provision of specific nutrition and physical activity counseling, and encouraging structured weight management strategies in pediatric primary care.25,26 We implemented universal screening of BMI in the two intervention primary care settings and developed educational materials to assist with nutrition and physical activity counseling. Second, clinical decision support tools delivered to clinicians at the point-of-care that flag children with overweight or obesity and provide a standardized note template specific for obesity management have been shown to increase the quality of obesity-related care and improve BMI outcomes.27, 28 In the MA-CORD intervention FQHC’s we worked to optimize the electronic health records to plot BMI on appropriate growth charts, flag children with overweight and obesity, and provide structured, obesity-specific note templates to guide primary care management. Third, evidence suggests that multidisciplinary Healthy Weight Clinics that reorganize care to provide access to a trained team consisting of a pediatric provider, nutritionist, and case manager during dedicated weight management visits are effective.15,29 Two recent studies showed that healthy weight clinics improved obesity care and BMI outcomes among low-income children in Massachusetts.15,29 Our findings show that the Healthy Weight Clinic model did improve obesity care by promoting local specialization and increasing capacity for specialized care and improved child BMI outcomes.
While our study had many strengths including the systematic, multi-level approach to clinical obesity management, the study also had limitations and we faced several challenges. First, given the nature of the multi-level, multi-sector community intervention, we were not able to use a randomized or blinded design. While a randomized controlled trial provides the highest level of internal validity, in many settings — particularly low resource settings serving vulnerable populations — randomization to a control group is not acceptable as it conflicts with the organization’s objective to serve vulnerable families.30 As a viable alternative, we used a longitudinal, quasi-experimental design with a TAU group and collected outcome data from groups before and after the study implementation. Second, the MA-CORD clinical intervention activities were embedded within other MA-CORD interventions in WIC, public schools, and after-school programs.31,32 Our process measures indicated that a large majority of eligible families were enrolled in WIC and school-age children were enrolled in the local public schools. A much lower percentage of children interacted with the after-school programs. Thus, it is possible that our intervention effects could be partially attributed to activities in the WIC and public school settings. Third, we selected a representative comparison community and it is possible that other wellness interventions were undertaken by that community during the study period. To our knowledge, there were no systematic childhood obesity interventions implemented in the comparison community during the study period. Finally, our study faced substantial implementation challenges as previously described and several of the barriers we encountered likely reflect the socioeconomic instability of the communities we were working in, the timing of this intervention which began during a financial recession, and leadership turmoil in the health centers as they worked to implement the intervention. Despite these limitations, we believe our study reflects best practice in the design and evaluation of a multi-level intervention and our results could add to the knowledge base in addressing childhood obesity in low-income communities.
In conclusion, the clinical interventions delivered through MA-CORD were associated with significant improvement in BMI z-scores in one of two intervention communities. Our findings suggest that multi-level interventions to improve childhood obesity prevention and management in low-income, primary care settings could have beneficial effects on BMI and reach the very segments of the US population who need it most.
Study Importance Questions.
- What is already known about this subject?
- Decision support tools in electronic health records have been shown to improve the quality of care for children with obesity and for accelerating the use of Expert Committee evidence on obesity screening and management practices by primary care providers.
- Community health workers are increasingly being embedded into chronic disease prevention teams serving to link clinical and community systems for obesity management.
- Few interventions to improve obesity-related quality of care have been developed in low resource settings like federally qualified community health centers or have incorporated systematic changes to prevent and manage obesity.
- What does your study add?
- In this quasi-experimental trial, body mass index (BMI) outcomes were improved for low-income children ages 2–12 years in a comprehensive clinical intervention delivered at two federally qualified community health centers as part of the MA-CORD initiative.
- This study highlights intervention implementation challenges often faced in federally-qualified health centers, including staff and provider turnover and transient patient populations. This study highlights these challenges and the effect on implementation fidelity.
Acknowledgments
We thank the families, institutions, faculty, research staff, and students that participated in the MA-CORD study.
Funding: This study was supported by the Centers for Disease Control and Prevention National Center for Chronic Disease Prevention and Health Promotion (Award no.: U18DP003370). Dr. Taveras is supported by grant K24 DK10589 from the National Institute of Diabetes and Digestive and Kidney Diseases. This work is solely the responsibility of the authors and does not represent the official views of the CDC or any of the other funders.
Footnotes
Clinical Trials Registration: NCT02110615
Disclosure: The authors declared no conflict of interest.
References
- 1.Ogden CL, Carroll MD, Lawman HG, et al. Trends in Obesity Prevalence Among Children and Adolescents in the United States, 1988–1994 Through 2013–2014. JAMA. 2016;315:2292–9. doi: 10.1001/jama.2016.6361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Singh GK, Siahpush M, Kogan MD. Neighborhood socioeconomic conditions, built environments, and childhood obesity. Health Aff (Millwood) 2010;29:503–12. doi: 10.1377/hlthaff.2009.0730. [DOI] [PubMed] [Google Scholar]
- 3.Singh GK, Siahpush M, Kogan MD. Rising social inequalities in US childhood obesity, 2003–2007. Ann Epidemiol. 2010;20:40–52. doi: 10.1016/j.annepidem.2009.09.008. [DOI] [PubMed] [Google Scholar]
- 4.Dooyema CA, Belay B, Foltz JL, et al. The childhood obesity research demonstration project: a comprehensive community approach to reduce childhood obesity. Child Obes. 2013;9:454–9. doi: 10.1089/chi.2013.0060. [DOI] [PubMed] [Google Scholar]
- 5.Taveras EM, Blaine RE, Davison KK, et al. Design of the Massachusetts Childhood Obesity Research Demonstration (MA-CORD) study. Child Obes. 2015;11:11–22. doi: 10.1089/chi.2014.0031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Davison KK, Falbe J, Taveras EM, et al. Evaluation overview for the Massachusetts Childhood Obesity Research Demonstration (MA-CORD) project. Child Obes. 2015;11:23–36. doi: 10.1089/chi.2014.0059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Henke RM, Johann J, Senathirajah M, et al. Implementation of the Patient-Centered Medical Home Model in Facilities Providing Comprehensive Care to Medically Underserved Populations. J Health Care Poor Underserved. 2016;27:1638–1646. doi: 10.1353/hpu.2016.0152. [DOI] [PubMed] [Google Scholar]
- 8.Ayash CR, Simon SR, Marshall R, et al. Evaluating the impact of point-of-care decision support tools in improving diagnosis of obese children in primary care. Obesity (Silver Spring) 2013;21:576–82. doi: 10.1002/oby.20161. [DOI] [PubMed] [Google Scholar]
- 9.Taveras EM, Marshall R, Horan CM, et al. Improving children’s obesity-Related health care quality: Process outcomes of a cluster-Randomized controlled trial. Obesity (Silver Spring) 2013 doi: 10.1002/oby.20612. [DOI] [PubMed] [Google Scholar]
- 10.Dietz WH, Solomon LS, Pronk NP, et al. An integrated framework for the prevention and treatment of obesity and its related chronic diseases. Health Aff (Millwood) 2015;34:1456–1463. doi: 10.1377/hlthaff.2015.0371. [DOI] [PubMed] [Google Scholar]
- 11.Viswanathan M, Kraschnewski J, Nishikawa B, et al. Outcomes of community health worker interventions. Evid Rep Technol Assess (Full Rep) 2009:1–144. A1–2, B1–14. passim. [PMC free article] [PubMed] [Google Scholar]
- 12.Viswanathan M, Kraschnewski JL, Nishikawa B, et al. Outcomes and costs of community health worker interventions: a systematic review. Med Care. 2010;48:792–808. doi: 10.1097/MLR.0b013e3181e35b51. [DOI] [PubMed] [Google Scholar]
- 13.National Center for Chronic Disease Prevention and Health Promotion. A Policy Brief on Community Health Workers. In: Centers for Disease Control and Prevention, editor. Addressing Chronic Disease through Community Health Workers: A Policy and Systems-Level Approach. Second. Atlanta, GA: 2015. [Google Scholar]
- 14.Taveras EM, Marshall R, Horan CM, et al. Rationale and design of the STAR randomized controlled trial to accelerate adoption of childhood obesity comparative effectiveness research. Contemp Clin Trials. 2013;34:101–8. doi: 10.1016/j.cct.2012.10.005. [DOI] [PubMed] [Google Scholar]
- 15.Anand SG, Adams WG, Zuckerman BS. Specialized care of overweight children in community health centers. Health Aff (Millwood) 2010;29:712–7. doi: 10.1377/hlthaff.2009.1113. [DOI] [PubMed] [Google Scholar]
- 16.Huh SY, Rifas-Shiman SL, Taveras EM, et al. Timing of solid food introduction and risk of obesity in preschool-aged children. Pediatrics. 2011;127:e544–51. doi: 10.1542/peds.2010-0740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Langley GL, Nolan KM, Nolan TW, et al. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. San Francisco, California: Jossey-Bass Publishers; 2009. [Google Scholar]
- 18.McPherson ME, Mirkin R, Heatherley PN, et al. Educating health care professionals in advocacy for childhood obesity prevention in their communities: integrating public health and primary care in the Be Our Voice project. Am J Public Health. 2012;102:e37–43. doi: 10.2105/AJPH.2012.300833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.National Initiative for Children’s Health Care Quality. Next Steps: A Practitioner’s Guide For Themed Follow-up Visits For Their Patients to Achieve a Healthy Weight. American Academy of Pediatrics; 2013. [Google Scholar]
- 20.Flegal KM, Wei R, Ogden CL, et al. Characterizing extreme values of body mass index-for-age by using the 2000 Centers for Disease Control and Prevention growth charts. Am J Clin Nutr. 2009;90:1314–20. doi: 10.3945/ajcn.2009.28335. [DOI] [PubMed] [Google Scholar]
- 21.Fox CK, Kaizer AM, Rudser KD, et al. Meal replacements followed by topiramate for the treatment of adolescent severe obesity: A pilot randomized controlled trial. Obesity (Silver Spring) 2016;24:2553–2561. doi: 10.1002/oby.21633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Garnett SP, Gow M, Ho M, et al. Improved insulin sensitivity and body composition, irrespective of macronutrient intake, after a 12 month intervention in adolescents with pre-diabetes; RESIST a randomised control trial. BMC Pediatr. 2014;14:289. doi: 10.1186/s12887-014-0289-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ho M, Gow M, Halim J, et al. Effect of a prescriptive dietary intervention on psychological dimensions of eating behavior in obese adolescents. Int J Behav Nutr Phys Act. 2013;10:119. doi: 10.1186/1479-5868-10-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ganter C, Aftosmes-Tobio A, Chuang E, et al. Lessons Learned by Community Stakeholders in the Massachusetts Childhood Obesity Research Demonstration (MA-CORD) Project, 2013–2014. Prev Chronic Dis. 2017;14:E08. doi: 10.5888/pcd14.160273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.U. S. Preventive Services Task Force. Screening for Obesity in Children and Adolescents: US Preventive Services Task Force Recommendation Statement. Pediatrics. 2010;125:361–367. doi: 10.1542/peds.2009-2037. [DOI] [PubMed] [Google Scholar]
- 26.Oude Luttikhuis H, Baur L, Jansen H, et al. Interventions for treating obesity in children. Cochrane Database Syst Rev. 2009:CD001872. doi: 10.1002/14651858.CD001872.pub2. [DOI] [PubMed] [Google Scholar]
- 27.Taveras EM, Marshall R, Horan CM, et al. Improving children’s obesity-related health care quality: process outcomes of a cluster-randomized controlled trial. Obesity (Silver Spring) 2014;22:27–31. doi: 10.1002/oby.20612. [DOI] [PubMed] [Google Scholar]
- 28.Taveras EM, Marshall R, Kleinman KP, et al. Comparative effectiveness of childhood obesity interventions in pediatric primary care: a cluster-randomized clinical trial. JAMA Pediatr. 2015;169:535–42. doi: 10.1001/jamapediatrics.2015.0182. [DOI] [PubMed] [Google Scholar]
- 29.Cheng JK, Wen X, Coletti KD, et al. 2-Year BMI Changes of Children Referred for Multidisciplinary Weight Management. Int J Pediatr. 2014;2014:152586. doi: 10.1155/2014/152586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Glasgow RE, Magid DJ, Beck A, et al. Practical clinical trials for translating research to practice: design and measurement recommendations. Med Care. 2005;43:551–7. doi: 10.1097/01.mlr.0000163645.41407.09. [DOI] [PubMed] [Google Scholar]
- 31.Woo Baidal JA, Nelson CC, Perkins ME, et al. Childhood Obesity Prevention in the Women, Infants, and Children Program: Outcomes of the MA-CORD Study. Obesity (Silver Spring) 2017 doi: 10.1002/oby.21865. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Franckle RL, Falbe J, Gortmaker S, et al. Student Obesity Prevalence and Behavioral Outcomes for the Massachusetts Childhood Obesity Research Demonstration Project. Obesity (Silver Spring) 2017 doi: 10.1002/oby.21867. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]


