Abstract
Peer victimization increases the risk of experiencing psychotic symptoms among clinical and general populations, but the mechanism underlying this association remains unclear. Dissociation, which is related to peer victimization and hallucinatory experiences, has been demonstrated as a significant mediator in the relation between childhood victimization and hallucinatory experience among adult patients with psychosis. However, no studies have examined the mediating effect of dissociation in a general early adolescent population. We examined whether dissociation mediates the relationship between peer victimization and hallucinatory experiences among 10-year-old adolescents using a population-based cross-sectional survey of early adolescents and their main parent (Tokyo Early Adolescence Survey; N = 4478). We examined the mediating effect of dissociation, as well as external locus of control and depressive symptoms, on the relationship between peer victimization and hallucinatory experiences using path analysis. The model assuming mediation effects indicated good model fit (comparative fit index = .999; root mean square error of approximation = .015). The mediation effect between peer victimization and hallucination via dissociation (standardized indirect effect = .038, p < .001) was statistically significant, whereas the mediation effects of depressive symptoms (standardized indirect effect = −.0066, p = 0.318) and external locus of control (standardized indirect effect = .0024, p = 0.321) were not significant. These results suggest that dissociation is a mediator in the relation between peer victimization and hallucinatory experiences in early adolescence. For appropriate intervention strategies, assessing dissociation and peer victimization as they affect hallucinatory experiences is necessary.
Keywords: Bullying, Trauma, Psychotic-like experience, Mediator
1. Introduction
Peer victimization in adolescence has long-term adverse effects on mental health (Takizawa et al., 2014, Lereya et al., 2015), including psychotic symptoms (Schreier et al., 2009). A recent meta-analysis demonstrated that adolescents who experienced peer victimization in childhood and adolescence had a twofold greater risk of experiencing psychotic symptoms as compared to those who did not (Van Dam et al., 2012). Further, the causal relationship between adolescent peer victimization and psychotic symptoms has been suggested in a prospective cohort study (Kelleher et al., 2013). However, the mechanism explaining how peer victimization increases the risk for psychotic symptoms remains unclear.
Dissociation is defined as the “lack of normal integration of thoughts, feelings and experiences into the stream of consciousness and memory” (Bernstein et al., 1993). Dissociation can be caused by peer victimization in childhood and adolescence (van Ijzendoorn and Schuengel, 1996, Campbell and Morrison, 2007, Teicher et al., 2010) and lead to loosening reality discrimination (Allen et al., 1997), as well as psychotic symptoms, particularly hallucination (Anketell et al., 2010.; Escher et al., 2002a, Escher et al., 2002b, Pilton et al., 2015, Varese et al., 2011), because dissociation due to peer victimization undermines a person's grounding in the outer world and weakens their ability to reality test (Allen et al., 1997). Hallucination can be conceptualized as dissociated components of the self arising from the failure to integrate adverse and traumatic sensory and psychological experiences into the context of the self-identity (Longden et al., 2012), which develops during adolescence (Kasai, 2013, Sawyer et al., 2012).
A recent meta-analysis suggested that traumatic experience induced dissociative experiences (Dalenberg et al., 2012, Dalenberg et al., 2014) and that dissociative experiences are particularly related to hallucinatory experiences, in both clinical and non-clinical samples (Pilton et al., 2015), even after controlling for depressive symptoms (Altman et al., 1997). Previous studies have suggested that the relationship between peer victimization and hallucinatory experiences could be accounted for by dissociation (Pilton et al., 2015. Longden et al., 2012, Varese et al., 2012, Perona-Garcelan et al., 2012, Perona-Garcelan et al., 2014, Kisiel and Lyons, 2014). However, clinical studies have had small samples and assessed childhood victimization retrospectively when participants were approximately 40 years of age (Varese et al., 2012, Perona-Garcelan et al., 2012). A non-clinical study also showed the mediating effect of dissociation in young adulthood, although childhood victimization was recalled after 15 years and potential mediating factors were not controlled for (Perona-Garcelan et al., 2014).
Further, a study conducted on victimized adolescents demonstrated the mediating effect of dissociation on the relationship between victimization and overall mental health (Kisiel and Lyons, 2014), but this study was also limited by small sample size. Additionally, it did not focus specifically on peer victimization or hallucinatory experiences. A notable study attempted to examine the pathway between peer victimization and psychotic symptoms among early adolescents: Fisher et al. (2013) found that external locus of control, which can lead to misattributions of perceptual anomalies (Garety et al., 2007), and depressive symptoms had a significant mediation effect on the relationship between peer victimization and psychotic symptoms among 7000 adolescents aged 13 (Fisher et al., 2013). About 30% of the association between peer victimization and psychotic symptoms could be explained by the mediating effects of external locus of control and depressive symptoms. The unexplained portion of the association might represent other mediating factors. However, they did not examine the effect of dissociation on the relationship between peer victimization and hallucinatory experience.
Thus, to our knowledge, no previous research has examined whether dissociation mediates the relationship between peer victimization and hallucinatory experiences in early adolescence. We hypothesized that dissociation mediates the relationship between peer victimization and hallucinatory experiences. The aim of the present study was to test this hypothesis and further examine the mediation effect of dissociation while controlling for external locus of control and depressive symptoms among 10-year-old adolescents. We used path modeling, which allows us to infer a mediating relationship between peer victimization and hallucinatory experiences via dissociation while controlling for possible confounders.
2. Methods
2.1. Study design, sample, and survey procedures
This study used data from the Tokyo Early Adolescence Survey (T-EAS), which was originally designed as a baseline cross-sectional survey for the subsequent longitudinal cohort study (Tokyo Teen Cohort), which is currently ongoing (URL: http://ttcp.umin.jp/index.html). The T-EAS is a multidisciplinary survey of 10-year-old adolescents aimed at investigating their health and development. We randomly sampled early adolescents by using the resident register in three municipalities: Setagaya-ku, Mitaka-shi, and Chofu-shi in the metropolitan area of Tokyo. Eligible residents were those born between September 2002 and August 2004. The survey was carried out between October 2012 and January 2015. We sent letters of invitation to participants around their 10th birthday. Then, a trained interviewer visited their home. The survey was completed twice over two visits. At the first visit, written informed consent from the adolescent and his/her main parent (generally mothers) was obtained, and they were asked to complete the questionnaires at home by the second visit. At the second visit, the adolescent and his/her main parent were asked to answer the self-report questionnaires separately. The questionnaires were enclosed in envelopes by the respondents immediately after completion. Also during the second visit, the interviewer measured the adolescent's height and weight. Concurrently, the main parent responded to a semi-structured interview. All data were collected anonymously. T-EAS is based at three research institutes: Tokyo Metropolitan Institute of Medical Science, The University of Tokyo, and SOKENDAI (The Graduate University for Advanced Studies). This survey was approved by the ethics committees of the above three institutes.
2.2. Participants
Among 18,830 eligible pairs of adolescents and parents, 14,553 were randomly selected. Of these, 4319 could not be contacted. Out of the 10,234 children who were accessible, 5756 adolescents and/or their parents refused to participate. Therefore, 4478 pairs participated in the survey (response rate: 43.8%). Among the consenting pairs, 201 (4.5%) were excluded from the analyses due to incomplete responses to questions of interest. Hence, the remaining 4277 cases were analyzed (mean age = 9.8 years, SD = 0.4; 53% boys).
2.3. Measures
2.3.1. Hallucinatory experiences
Hallucinatory experiences were assessed by the main parent of the participant using 2 items derived from the Child Behavior Check List (Achenbach, 1991, Itani et al., 2001). The following factors were assessed: (i) auditory hallucination (“hears sounds or voices that aren't there”) and (ii) visual hallucination (“sees things that aren't there”). Responses were provided on a 3-point scale: not true = 0, somewhat or sometimes true = 1, very true or often true = 2. The hallucinatory experiences score was defined as the sum of these 2-item scores (possible range: 0–4).
2.3.2. Dissociation
Dissociation was assessed by the main parent of the participant using 6 items from the Child Behavior Check List based on previous studies demonstrating acceptable internal consistency (Malinosky-Rummell and Hoier, 1991, Becker-Blease et al., 2004). We used the following questions: i) “acts too young for his/her age,” ii) “can't concentrate, can't pay attention for long,” iii) “confused or seems to be in a fog,” iv) “daydreams or gets lost in his/her thoughts,” v) “stares blankly,” and vi) “sudden changes in mood or feeling.” All responses were given on a 3-point scale: not true = 0, somewhat or sometimes true = 1, very true or often true = 2. The dissociation score was defined as the sum of these 6-item scores (possible range: 0–12).
2.3.3. Peer victimization
Participants' peer victimization in the previous 2 months was assessed by main parents using a global scale that adopted questions from the Olweus Bully/Victims Questionnaire (Solberg and Olweus, 2013). The definition of bullying was shown and participants were asked, “How often has your child been bullied at school in the past 2 months?” Responses were based on a 5-point Likert scale: it hasn't happened to my child in the past couple months = 0, only once or twice = 1, two or three times a month = 2, about once a week = 3, and several times a week = 4. Scores of 1–4 were defined as being bullied.
2.3.4. Depressive symptoms
Participants' depressive symptoms were assessed using the Short Mood and Feelings Questionnaire (SMFQ), which is a 13-item self-report questionnaire and screening measure for severity of depression (Kuo et al., 2005).
2.3.5. External locus of control
Participants' external locus of control was assessed using the shortened version of the Childhood Nowicki–Strickland Internal–External (CNSIE) questionnaire (Nowicki, 1976, Nowicki and Duke, 1974, Nowicki and Strickland, 1973), which is a 12-item self-report questionnaire that has been used in a previous population-based survey of 8-year-old children (Thompson et al., 2011).
2.4. Statistical analysis
Cross-tabulation and chi-square tests were performed to test the association between peer victimization and hallucinatory experiences. By using structural equation modeling, the mediating effect of dissociation on the relation between hallucinatory experiences and peer victimization was examined after investigating the presence of a direct effect between peer victimization and hallucinatory experiences. Model fit was assessed using two common indices, comparative fit index (CFI) and root mean square error of approximation (RMSEA). Models with a CFI value greater than 0.9 and an RMSEA less than 0.05 indicate good model fit. Potential mediating effects were assessed by calculating indirect effects of each mediator on the relationship between peer victimization and hallucinatory experiences. Indirect effects were calculated by multiplying the path coefficient between peer victimization and each mediator and between each mediator and hallucinatory experiences. The Sobel test (Sobel, 1982, Bollen and Stine, 1990, Preacher and Hayes, 2004) was performed to test the mediation effect of dissociation as well as that of depression and external locus of control. A z-test was used to compare the size of the mediation effect of dissociation with that of depressive symptoms as well as external locus of control. The significance level was set to 0.05. IBM SPSS 21.0 and Amos 20.0 (IBM Corp, New York, USA) were used for statistical analyses.
3. Results
Descriptive statistics are shown in Table 1. Approximately 2% of adolescents experienced auditory hallucinations, and about 2% experienced visual hallucination, according to parent ratings. Further, 12% of the total sample experienced peer victimization in the last 2 months. Adolescents with hallucinatory experiences were more likely to experience peer victimization than those without hallucinatory experiences (20.5% and 12.5%, respectively; χ2 = 8.35, p = .004), indicating a significant positive correlation between hallucinatory experiences and peer victimization.
Table 1.
Demographic characteristics of participants.
| N = 4277 | |
|---|---|
| Females, n (%) | 2005 (46.9) |
| Age, mean (SD) | 9.8 (0.4) |
| Dissociative behavior, mean (SD) | 2.17 (1.80) |
| Auditory hallucinatory experiences, n (%) | |
| Not true | 4189 (97.9) |
| Somewhat or sometimes true | 83 (1.9) |
| Very true or often true | 5 (0.1) |
| Visual Hallucinatory experiences, n (%) | |
| not true | 4199 (98.2) |
| somewhat or sometimes true | 67 (1.6) |
| very true or often true | 11 (0.3) |
| Peer victimization in past 2 months, n (%) | |
| None | 3755 (87.8) |
| Once or twice | 334 (7.8) |
| Two or three times a month | 79 (1.8) |
| Once a week | 56 (1.3) |
| Several times a week | 53 (1.2) |
| Depression,a mean (SD) | 4.78 (4.58) |
| Locus of control,b mean (SD) | 4.66 (1.89) |
Total scores of Short Mood and Feeling Questionnaire (range 0–26).
Total scores of Childhood Nowicki–Strickland Internal–External questionnaire (range 0–12).
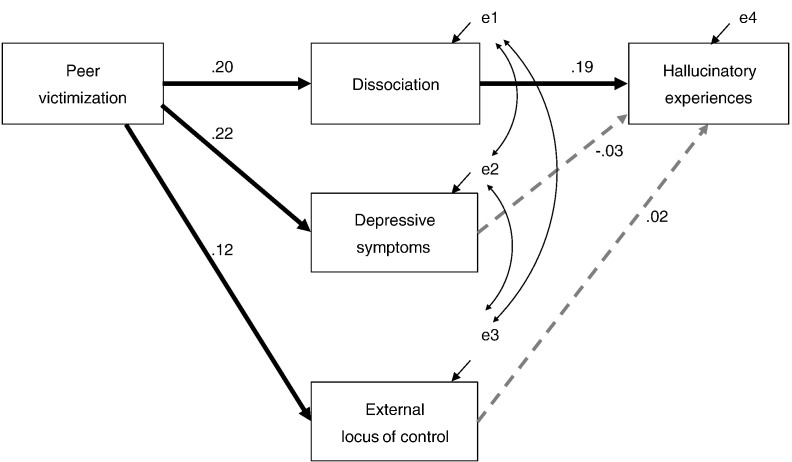
A direct path between peer victimization and hallucinatory experiences was not statistically significant in a saturated path model (β = .02, p = .149), which assumes both direct and indirect paths between peer victimization and hallucinatory experiences. Thus, the direct path between peer victimization and hallucinatory experiences was excluded from the path model. Fig. 1 shows the path diagram describing the mediating effects of dissociation, depressive symptoms, and external locus of control on the relationship between peer victimization and hallucinatory experiences. This model demonstrated a good model fit (CFI = .999, RMSEA = .015).
Fig. 1.
Path diagram describing the mediating effect of dissociation on the relationship between peer victimization and hallucinatory experiences.
Note. Solid black line: path coefficient is statistically significant (p < .001); dotted line: path coefficient is not significant (p > .05).
Peer victimization was significantly associated with dissociation (β = .20, p < .001) as well as depressive symptoms and external locus of control (β = .22, p < .001; β = .12, p < .001, respectively). Hallucinatory experience was significantly associated with dissociation (β = .19, p < .001), whereas the path between depressive symptoms and hallucinatory experiences (β = −.03, p = .123) and that between external locus of control and hallucinatory experiences (β = .02, p = .319) were not significant. The mediation effect of dissociation on the relationship between peer victimization and hallucinatory experiences was significant (standardized indirect effect = .038, p < .001). The mediation effects of depressive symptoms and external locus of control were not (standardized indirect effect = −.0066, p = 0.318; standardized indirect effect = .0024, p = 0.321, respectively). The z-test revealed that the mediating effect of dissociation was significantly larger than the mediating effect of both depressive symptoms (z = 6.285, p < .001) and external locus of control (z = 8.531, p < .001).
4. Discussion
The present study was the first to investigate whether dissociation mediates the relationship between peer victimization and hallucinatory experiences among young adolescents. The present findings from a path analysis support our hypothesis that dissociation mediates the association between peer victimization and hallucinatory experiences.
About 2% of young adolescents experienced hallucinatory experiences as rated by their main parent, comparable to a previous study demonstrating a rate of 3%–4% using the same measurement with children under 11 years of age (Ferdinand et al., 2004). The mean score on the dissociation scale was slightly higher than the mean score reported in a previous study assessing 11-year-old children (mean scores = 1.16–1.48; Becker-Blease et al., 2004). This is consistent with the previous finding that the normative age for peak dissociation is 10, and that it experiences a decline through adolescence and adulthood (Putnam, 1993). One in eight participants experienced peer victimization, which is comparable to a previous epidemiological study showing rates of 5%–20% among young adolescents aged 11–15 years across 25 countries (Nansel et al., 2004).
Further consistent with previous studies, the mediating effect of dissociation in the relation between peer victimization and hallucinatory experiences was statistically significant (Varese et al., 2012, Perona-Garcelan et al., 2012, Perona-Garcelan et al., 2014, Kisiel and Lyons, 2014), proposing that dissociation may be a potential mechanism linking victimization and psychopathology. Recent studies have revealed that dissociation arises from HPA axis dysregulation (Simeon et al., 2007), which could be caused by peer victimization in childhood and adolescence (Ouellet-Morin et al., 2011). Recent studies have also suggested that HPA axis dysregulation increases the risk of having psychotic symptoms, including hallucinations (Walker et al., 2008, Corcoran et al., 2003). To integrate these findings, HPA axis dysregulation may be a biological factor mediating the relationship between peer victimization and hallucinatory experiences. The other recent studies revealed that victimized experience in early life may lead to cognitive dysfunction in adulthood among people without psychopathology (Gould et al., 2012, Berthelot et al., 2015). These results may also suggest that we should focus on a neuropsychological mediator between peer victimization and hallucinatory experiences among adolescents in future study. However, this issue is beyond the scope of this article and further evidence is needed to elucidate the biological and neuropsychological influence on the link between peer victimization and hallucinatory experiences among adolescents.
The mediating effects of depressive symptoms and external locus of control were not significant. This is inconsistent with a previous population-based study (Fisher et al., 2013); however, the inconsistency might be due to the difference in study design. The previous study did not adopt dissociation as a mediator in the mediation model. The present results indicate that dissociation could explain a greater proportion of the association between peer victimization and hallucinatory experience than depressive symptoms and external locus of control. Moreover, the results of the current study provided evidence that the mediating effect of dissociation in the relationship between peer victimization and hallucinatory experiences may be larger in comparison with the effect of depressive symptoms and of locus of control.
The prevalence of hallucinatory experiences was less frequent than that of peer victimization in this adolescent population. Peer victimization may lead not only to hallucinatory experiences but also to other possible psychopathologies (e.g. anxiety symptoms). In addition, there may be some adolescents who would not experience any psychopathology in later life even though they experienced peer victimization. We need to examine the pathways from peer victimization to other outcomes, and need to explore resilient factors against developing psychopathology even if experienced peer victimization.
In terms of intervention for hallucinatory experiences in early adolescence, dissociation linked with peer victimization might be an important factor. The present study results suggest that it is important to specify hallucinatory experience as it relates to dissociation and peer victimization. It is possible that psychosocial interventions (e.g., trauma-focused cognitive behavioral therapy for youth (Cohen et al., 2011), cognitive–behavioral intervention for trauma in school; Stein et al., 2003) rather than antipsychotic medication could be effective in managing hallucinatory experiences associated with peer victimization in early adolescence. For appropriate intervention strategies, assessing dissociation and peer victimization as they affect hallucinatory experiences is necessary.
Several limitations in the present study should be noted. First, we used the main parent's ratings on hallucinatory experiences, dissociation, and peer victimization, not adolescent self-reports. It is possible that parents underestimated their children's experiences of peer victimization and hallucination. Second, we used data from a cross-sectional survey and could not clarify the direction of pathways between peer victimization and hallucinatory experience, though large prospective studies have previously determined a causal relationship between peer victimization and hallucinatory experiences in adolescence (Schreier et al., 2009, Kelleher et al., 2013). We are currently conducting a subsequent longitudinal cohort study (Tokyo Teen Cohort Study), which will further clarify causality. Third, our findings in the general population may not be directly applicable to pathological hallucinations in clinical samples. Hallucinatory experiences in general adolescents would not necessarily lead to the onset of clinical psychosis, although subclinical psychotic experiences increase the risk of having psychotic disorders after 3–24 years by 3.5-fold (Kaymaz et al., 2012). Future studies need to clarify the mediation effect of dissociation on the relationship between peer victimization and the onset of psychotic disorders in adolescence with a longitudinal cohort study. The definition of dissociative symptoms in this study was broader than the clinical diagnosis of dissociative disorders, although previous epidemiological studies adopted and validated the measure (Malinosky-Rummell and Hoier, 1991, Becker-Blease et al., 2004). We need to be careful to apply the present findings to clinical samples and further clinical studies would be needed. Fourth, other potential path models might be considered, and we cannot eliminate the possibility of other models being a better fit. The present path model, which controlled for potential confounders, showed acceptable model fit, suggesting a mediating relationship between victimization and hallucinatory experiences via dissociation. Fifth, although this is not uncommon in estimating mediation in behavioral data, the observed size of the mediating effect of dissociation was not large. Further, we did not test other potential mediating factors (e.g., attachment style (Sitko et al., 2014), post-traumatic stress disorder re-experiencing symptoms (Gracie et al., 2007), and source monitoring; Bentall et al., 2014) in the relation between peer victimization and hallucinatory experiences. However, previous studies have shown no association between source monitoring and childhood victimization (Varese et al., 2012, Bendall et al., 2011), and only 1%–3% of the association between victimization and hallucinatory experiences could be explained by attachment style and post-traumatic stress disorder re-experiencing symptoms (Sitko et al., 2014, Gracie et al., 2007). We will overcome this limitation through the Tokyo Teen Cohort Study.
In conclusion, our investigation suggests that dissociation significantly mediates the relationship between peer victimization and hallucinatory experiences among early adolescents. Understanding developmental epidemiology in general early adolescence, which is the critical life-stage for the emergence of psychiatric disorders, will deepen our understanding of psychopathology in psychosis, and ultimately serve as a compass for early interventions.
Role of Funding Sources
This work was supported by a Japan Scientific Research Grant on an Innovative Area (MEXT KAKENHI Grant Numbers 23118002, 23118004; Adolescent Mind & Self-Regulation) from the Ministry of Education, Culture, Sports, Science and Technology; a Japanese Society for the Promotion of Science Scientific Research Grant (Strategic Young Researcher Overseas Visits Program for Accelerating Brain Circulation; Grant-in-Aid for Scientific Research(B): JSPS KAKENHI Grant Number 16H03745); a Tokyo Metropolitan Institute of Medical Science Project Grant (Kokoronokenko H21-H26); and an International Early Psychosis Association 2014 poster award. However, neither the bodies nor the institutions with which the authors are affiliated with have any financial interest or conflict with the subject matter of this manuscript.
Contributors
SY, SA, SK, PF, KE, TS, TF, MH, KK, AN conceptualized the study and wrote the first draft of the manuscript. SY, SU conducted the statistical analyses. SY, KE, SK, AS, AN helped in the design of the study and the management of database. All authors have approved the final manuscript.
Conflict of Interest
None.
Acknowledgements
We are extremely grateful for the cooperation and assistance of all of the adolescents and their parents who participated in this study.
References
- Achenbach T.M. University of Vermont Burlington; 1991. Integrative Guide for the 1991 CBCL/4-18, YSR, and TRF Profiles: Department of Psychiatry. [Google Scholar]
- Allen J.G., Coyne L., Console D.A. Dissociative detachment relates to psychotic symptoms and personality decompensation. Compr. Psychiatry. 1997;38:327–334. doi: 10.1016/s0010-440x(97)90928-7. [DOI] [PubMed] [Google Scholar]
- Altman H., Collins M., Mundy P. Subclinical hallucinations and delusions in nonpsychotic adolescents. J. Child Psychol. Psychiatry. 1997;38:413–420. doi: 10.1111/j.1469-7610.1997.tb01526.x. [DOI] [PubMed] [Google Scholar]
- Anketell C., Dorahy M.J., Shannon M., Elder R., Hamilton G., Corry M., MacSherry A., Curran D., O'Rawe B. An exploratory analysis of voice hearing in chronic PTSD: potential associated mechanisms. J. Trauma Dissociation. 2010;11:93–107. doi: 10.1080/15299730903143600. [DOI] [PubMed] [Google Scholar]
- Becker-Blease K.A., Deater-Deckard K., Eley T., Freyd J.J., Stevenson J., Plomin R. A genetic analysis of individual differences in dissociative behaviors in childhood and adolescence. J. Child Psychol. Psychiatry. 2004;45:522–532. doi: 10.1111/j.1469-7610.2004.00242.x. [DOI] [PubMed] [Google Scholar]
- Bendall S., Jackson H.J., Hulbert C.A. What self-generated speech is externally misattributed in psychosis? Testing three cognitive models in a first-episode sample. Schizophr. Res. 2011;129:36–41. doi: 10.1016/j.schres.2011.03.028. [DOI] [PubMed] [Google Scholar]
- Bentall R.P., de Sousa P., Varese F., Wickham S., Sitko K., Haarmans M., Read J. From adversity to psychosis: pathways and mechanisms from specific adversities to specific symptoms. Soc. Psychiatry Psychiatr. Epidemiol. 2014;49:1011–1022. doi: 10.1007/s00127-014-0914-0. [DOI] [PubMed] [Google Scholar]
- Bernstein E., Putnam F.W., Ross C.A., Torem M., Coons P., Dill D. Validity of the dissociative experiences scale in screening for multiple personality disorder: a multicenter study. Am. J. Psychiatry. 1993;150:1030–1036. doi: 10.1176/ajp.150.7.1030. [DOI] [PubMed] [Google Scholar]
- Berthelot N., Paccalet T., Gilbert E., Moreau I., Merette C., Gingras N., Rouleau N., Maziade M. Childhood abuse and neglect may induce deficits in cognitive precursors of psychosis in high-risk children. J. Psychiatry Neurosci. 2015;40:336–343. doi: 10.1503/jpn.140211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bollen K.A., Stine R. Direct and indirect effects: classical and bootstrap estimates of variability. Sociol. Methodol. 1990;20(1):15–140. [Google Scholar]
- Campbell M.L.C., Morrison A.P. The relationship between bullying, psychotic-like experiences and appraisals in 14–16-year olds. Behav. Res. Ther. 2007;45:1579–1591. doi: 10.1016/j.brat.2006.11.009. [DOI] [PubMed] [Google Scholar]
- Cohen J.A., Mannarino A.P., Murray L.K. Trauma-focused CBT for youth who experience ongoing traumas. Child Abuse Negl. 2011;35:637–646. doi: 10.1016/j.chiabu.2011.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corcoran C., Walker E., Huot R., Mittal V., Tessner K., Kestler L., Malaspina D. The stress cascade and schizophrenia: etiology and onset. Schizophr. Bull. 2003;29:671–692. doi: 10.1093/oxfordjournals.schbul.a007038. [DOI] [PubMed] [Google Scholar]
- Dalenberg C.J., Brand B.L., Gleaves D.H., Dorahy M.J., Loewenstein R.J., Cardeña E., Frewen P.A., Carlson E.B., Spiegel D. Evaluation of the evidence for the trauma and fantasy models of dissociation. Psychol. Bull. 2012;138:550–588. doi: 10.1037/a0027447. [DOI] [PubMed] [Google Scholar]
- Dalenberg C.J., Brand B.L., Loewenstein R.J., Gleaves D.H., Dorahy M.J., Cardeña E., Frewen P.A., Carlson E.B., Spiegel D. Reality versus fantasy: reply to Lynn et al. (2014) Psychol. Bull. 2014;140:911–920. doi: 10.1037/a0036685. [DOI] [PubMed] [Google Scholar]
- Escher S., Romme M., Buiks A., Delespaul P., van Os J. Formation of delusional ideation in adolescents hearing voices: a prospective study. Am. J. Med. Genet. 2002;114:913–920. doi: 10.1002/ajmg.10203. [DOI] [PubMed] [Google Scholar]
- Escher S., Romme M., Buiks A., Delespaul P., van Os J. Independent course of childhood auditory hallucinations: a sequential 3-year follow-up study. Br. J. Psychiatry. 2002;181:S10–S18. doi: 10.1192/bjp.181.43.s10. [DOI] [PubMed] [Google Scholar]
- Ferdinand R.F., van der Ende J., Verhulst F.C. Associations between visual and auditory hallucinations in children and adolescents, and tobacco use in adulthood. Soc. Psychiatry Psychiatr. Epidemiol. 2004;39:514–520. doi: 10.1007/s00127-004-0777-x. [DOI] [PubMed] [Google Scholar]
- Fisher H.L., Schreier A., Zammit S., Maughan B., Munafò M.R., Lewis G., Wolke D. Pathways between childhood victimization and psychosis-like symptoms in the ALSPAC birth cohort. Schizophr. Bull. 2013;39:1045–1055. doi: 10.1093/schbul/sbs088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garety P.A., Bebbington P., Fowler D., Freeman D., Kuipers E. Implications for neurobiological research of cognitive models of psychosis: a theoretical paper. Psychol. Med. 2007;37:1377–1391. doi: 10.1017/S003329170700013X. [DOI] [PubMed] [Google Scholar]
- Gould F., Clarke J., Heim C., Harvey P.D., Majer M., Nemeroff C.B. The effects of child abuse and neglect on cognitive functioning in adulthood. J. Psychiatr. Res. 2012;46:500–506. doi: 10.1016/j.jpsychires.2012.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gracie A., Freeman D., Green S., Garety P.A., Kuipers E., Hardy A., Ray K., Dunn G., Bebbington P., Fowler D. The association between traumatic experience, paranoia and hallucinations: a test of the predictions of psychological models. Acta Psychiatr. Scand. 2007;116:280–289. doi: 10.1111/j.1600-0447.2007.01011.x. [DOI] [PubMed] [Google Scholar]
- Itani T., Kanbayashi Y., Nakata Y., Kita M., Fujii H., Kuramoto H., Negishi K., Teduka K., Okada A., Natori H. Standardization of the Japanese version of the child behavior checklist/4-18. Psychiatr. Neurol. Paediatr. Jpn. 2001;41:243–252. [Google Scholar]
- Kasai K. Toward an interdisciplinary science of adolescence: insights from schizophrenia research. Neurosci. Res. 2013;75:89–93. doi: 10.1016/j.neures.2012.12.001. [DOI] [PubMed] [Google Scholar]
- Kaymaz N., Drukker M., Lieb R., Wittchen H.-U., Werbeloff N., Weiser M., Lataster T., van Os J. Do subthreshold psychotic experiences predict clinical outcomes in unselected non-help-seeking population-based samples? A systematic review and meta-analysis, enriched with new results. Psychol. Med. 2012;42:2239–2253. doi: 10.1017/S0033291711002911. [DOI] [PubMed] [Google Scholar]
- Kelleher I., Keeley H., Corcoran P., Ramsay H., Wasserman C., Carli V., Sarchiapone M., Hoven C., Wasserman D., Cannon M. Childhood trauma and psychosis in a prospective cohort study: cause, effect, and directionality. Am. J. Psychiatry. 2013;170:734–741. doi: 10.1176/appi.ajp.2012.12091169. [DOI] [PubMed] [Google Scholar]
- Kisiel C.L., Lyons J.S. Dissociation as a mediator of psychopathology among sexually abused children and adolescents. Am. J. Psychiatry. 2014;158:1034–1039. doi: 10.1176/appi.ajp.158.7.1034. [DOI] [PubMed] [Google Scholar]
- Kuo E.S., Vander Stoep A., Stewart D.G. Using the short mood and feelings questionnaire to detect depression in detained adolescents. Assessment. 2005;12:374–383. doi: 10.1177/1073191105279984. [DOI] [PubMed] [Google Scholar]
- Lereya S.T., Copeland W.E., Costello E.J., Wolke D. Adult mental health consequences of peer bullying and maltreatment in childhood: two cohorts in two countries. Lancet Psychiatry. 2015;2:1–8. doi: 10.1016/S2215-0366(15)00165-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Longden E., Madill A., Waterman M.G. Dissociation, trauma, and the role of lived experience: toward a new conceptualization of voice hearing. Psychol. Bull. 2012;138:28–76. doi: 10.1037/a0025995. [DOI] [PubMed] [Google Scholar]
- Malinosky-Rummell R., Hoier T.S. Validating measures of dissociation in sexually abused and nonabused children. Behav. Assess. 1991;13:341–357. [Google Scholar]
- Nansel T.R., Craig W., Overpeck M.D., Saluja G., Ruan W.J. Cross-national consistency in the relationship between bullying behaviors and psychosocial adjustment. Arch. Pediatr. Adolesc. Med. 2004;158:730–736. doi: 10.1001/archpedi.158.8.730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nowicki S., Duke M.P. A preschool and primary internal-external control scale. Dev. Psychol. 1974;10:874. [Google Scholar]
- Nowicki S., Strickland B.R. A locus of control scale for children. J. Consult. Clin. Psychol. 1973;40:148–155. doi: 10.1037/h0034499. [DOI] [PubMed] [Google Scholar]
- Nowicki S. Factor structure of locus of control in children. J. Genet. Psychol. 1976;129:13–17. doi: 10.1080/00221325.1976.10534005. [DOI] [PubMed] [Google Scholar]
- Ouellet-Morin I., Odgers C.L., Danese A., Bowes L., Shakoor S., Papadopoulos A.S., Caspi A., Moffitt T.E., Arseneault L. Blunted cortisol responses to stress signal social and behavioral problems among maltreated/bullied 12-year-old children. Biol. Psychiatry. 2011;70:1016–1023. doi: 10.1016/j.biopsych.2011.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perona-Garcelan S., Carrascoso-Lopez F., Garcia-Montes J.M., Ductor-Recuerda M.J., López Jiménez A.M., Vallina-Fernández O., Pérez-Álvarez M., Gómez-Gómez M.T. Dissociative experiences as mediators between childhood trauma and auditory hallucinations. J. Trauma Stress. 2012;25:323–329. doi: 10.1002/jts.21693. [DOI] [PubMed] [Google Scholar]
- Perona-Garcelan S., Garcia-Montes J.M., Rodriguez-Testal J.F., López-Jiménez A.M., Ruiz-Veguilla M., Ductor-Recuerda M.J., Benítez-Hernández Mdel M., Arias-Velarde M.Á., Gómez-Gómez M.T., Pérez-Álvarez M. Relationship between childhood trauma, mindfulness, and dissociation in subjects with and without hallucination proneness. J. Trauma Dissociation. 2014;15:35–51. doi: 10.1080/15299732.2013.821433. [DOI] [PubMed] [Google Scholar]
- Pilton M., Varese F., Berry K., Bucci S. The relationship between dissociation and voices: a systematic literature review and meta-analysis. Clin. Psychol. Rev. 2015;40:138–155. doi: 10.1016/j.cpr.2015.06.004. [DOI] [PubMed] [Google Scholar]
- Preacher K.J., Hayes A.F. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav. Res. Methods Instrum. Comput. 2004;36:717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- Putnam F.W. Dissociative disorders in children—behavioral profiles and problems. Child Abuse Negl. 1993;17:39–45. doi: 10.1016/0145-2134(93)90006-q. [DOI] [PubMed] [Google Scholar]
- Sawyer S.M., Afifi R.A., Bearinger L.H., Blakemore S.J., Dick B., Ezeh A.C., Patton G.C. Adolescence: a foundation for future health. Lancet. 2012;379:1630–1640. doi: 10.1016/S0140-6736(12)60072-5. [DOI] [PubMed] [Google Scholar]
- Schreier A., Wolke D., Thomas K., Horwood J., Hollis C., Gunnell D., Lewis G., Thompson A., Zammit S., Duffy L., Salvi G., Harrison G. Prospective study of peer victimization in childhood and psychotic symptoms in a nonclinical population at age 12 years. Arch. Gen. Psychiatry. 2009;66:527–536. doi: 10.1001/archgenpsychiatry.2009.23. [DOI] [PubMed] [Google Scholar]
- Simeon D., Knutelska M., Yehuda R., Putnam F., Schmeidler J., Smith L.M. Hypothalamic–pituitary–adrenal axis function in dissociative disorders, post-traumatic stress disorder, and healthy volunteers. Biol. Psychiatry. 2007;61:966–973. doi: 10.1016/j.biopsych.2006.07.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sitko K., Bentall R.P., Shevlin M., Sellwood W. Associations between specific psychotic symptoms and specific childhood adversities are mediated by attachment styles: an analysis of the National Comorbidity Survey. Psychiatry Res. 2014;217:202–209. doi: 10.1016/j.psychres.2014.03.019. [DOI] [PubMed] [Google Scholar]
- Sobel M.E. Asymptotic confidence intervals for indirect effects in structural equation models. Sociol. Methodol. 1982;13:290–312. [Google Scholar]
- Solberg M.E., Olweus D. Prevalence estimation of school bullying with the Olweus bully/victim questionnaire. Aggress. Behav. 2013;29:239–268. [Google Scholar]
- Stein B.D., Jaycox L.H., Kataoka S.H., Wong M., Tu W., Elliott M.N., Fink A. A mental health intervention for schoolchildren exposed to violence: a randomized controlled trial. JAMA. 2003;290:603–611. doi: 10.1001/jama.290.5.603. [DOI] [PubMed] [Google Scholar]
- Takizawa R., Maughan B., Arseneault L. Adult health outcomes of childhood bullying victimization: evidence from a five-decade longitudinal British birth cohort. Am. J. Psychiatry. 2014;171:777–784. doi: 10.1176/appi.ajp.2014.13101401. [DOI] [PubMed] [Google Scholar]
- Teicher M.H., Samson J.A., Sheu Y.S., Polcari A., McGreenery C.E. Hurtful words: association of exposure to peer verbal abuse with elevated psychiatric symptom scores and corpus callosum abnormalities. Am. J. Psychiatry. 2010;167:1464–1471. doi: 10.1176/appi.ajp.2010.10010030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson A., Sullivan S., Lewis G., Zammit S., Heron J., Horwood J., Thomas K., Gunnell D., Hollis C., Wolke D., Harrison G. Association between locus of control in childhood and psychotic symptoms in early adolescence: results from a large birth cohort. Cogn. Neuropsychiatry. 2011;16:385–402. doi: 10.1080/13546805.2010.546077. [DOI] [PubMed] [Google Scholar]
- Van Dam D., Van Der Ven E., Velthorst E., Selten J., Morgan C., De Haan L. Childhood bullying and the association with psychosis in non-clinical and clinical samples: a review and meta-analysis. Psychol. Med. 2012;42:2463–2474. doi: 10.1017/S0033291712000360. [DOI] [PubMed] [Google Scholar]
- van Ijzendoorn M.H., Schuengel C. The measurement of dissociation in normal and clinical populations: meta-analytic validation of the Dissociative Experiences Scale (DES) Clin. Psychol. Rev. 1996;16:365–382. [Google Scholar]
- Varese F., Barkus E., Bentall R.P. Dissociation mediates the relationship between childhood trauma and hallucination-proneness. Psychol. Med. 2012;42:1025–1036. doi: 10.1017/S0033291711001826. [DOI] [PubMed] [Google Scholar]
- Varese F., Udachina A., Myin-Germeys I., Oorschot M., Bentall R.P. The relationship between dissociation and auditory verbal hallucinations in the flow of daily life of patients with psychosis. Psychosis. 2011;3:14–28. [Google Scholar]
- Walker E., Mittal V., Tessner K. Stress and the hypothalamic pituitary adrenal axis in the developmental course of schizophrenia. Annu. Rev. Clin. Psychol. 2008;4:189–216. doi: 10.1146/annurev.clinpsy.4.022007.141248. [DOI] [PubMed] [Google Scholar]