Abstract
Background
Patients with schizophrenia have deficits in social cognition (SC), a construct that includes emotion perception (EP), social perception (SP), theory of mind (ToM) and attributive style (AS). The aim of our study was to assess the applicability, identify potential problems and obtain preliminary data on the efficacy of a new online training program on SC called e-Motional Training (ET®), which can be remotely administered and remotely supervised by a clinician.
Materials and methods
A pre/post intervention pilot study was conducted with 21 patients with schizophrenia in the healthcare area of Ourense, Spain (12 patients were assigned to the intervention group and 9 in the control group). The control group received standard treatment (TAU) (occupational therapy and leisure group). The intervention group received TAU plus 12 sessions (1 hour per week) with ET® (including training modules on emotional perception and a short animated cartoon for ToM and AS training, including automated metacognitive feedback).
Endpoints: EP (Ekman 60 Faces Test), ToM (Hinting Task, Faux Pas, Happé), AS (Ambiguous Intentions Hostility Questionnaire).
Results
ET® was shown to be an understandable, viable and pleasant program for the participants. After the intervention, statistically significant data (p < 0.05) were obtained for the EP, ToM and AS variables.
Conclusion
ET® enables self-training in SC and online follow-up by the therapist, thereby covering the lack of online intervention instruments validated for patients with SC deficits. Our preliminary results demonstrate the feasibility of ET® and its possible efficacy in improving emotion recognition, ToM and AS.
Keywords: Social cognition, Schizophrenia, Computerized training, Cognitive remediation, Theory of mind
1. Background
Social cognition (SC) is a psychological construct that refers to a collection of mental operations that underlie social interactions. SC includes the processes involved in the perception, interpretation and generation of responses when faced with the intentions, dispositions and behavior of others (Green et al., 2008, Penn et al., 2008).
SC includes emotion perception, both in people’s faces and voices (Kohler et al., 2010, Tseng et al., 2013); social perception (Couture et al., 2006, Pinkham, 2014) i.e., the interpretation of clues about what happens in a certain social context and the application of this social understanding to develop more appropriate behavior; theory of mind (ToM) (Brüne, 2005b, Sarfati et al., 1999), which is defined as the ability to be aware that others have different ideas and intentions than ours; and attributive style (AS), which refers to people’s tendency to explain events that have occurred in their life and that sometimes leads them to consider the negative events as caused by the misconduct of others (Green et al., 2008, Hasson-Ohayon et al., 2014, Langdon et al., 2013, Mizrahi et al., 2008). In recent years, this topic has been the subject of intense study, revealing disorders in emotion perception, ToM, AS and social perception in patients with schizophrenia (Chung et al., 2014, Kurtz and Richardson, 2012, Lahera et al., 2014, Savla et al., 2013). The study of these deficits and of strategies for improving them is important because SC appears to have a greater repercussion on social function than neurocognition itself (Bigelow et al., 2006, Brüne, 2005a, Green et al., 2008) and is considered to be a mediator between neurocognition and functional performance (Casacchia et al., 2004, Penn et al., 1996, Pinkham and Penn, 2006). SC rehabilitation has been made possible by various therapeutic models (Addington et al., 2006, Addington et al., 2010). These rehabilitation models initially focused on the construct’s specific subdomains (Combs et al., 2009, Frommann et al., 2003, Kayser et al., 2006, Penn and Combs, 2000, Roberts and Penn, 2009, Roder et al., 2011, Russell et al., 2006, Silver et al., 2004). More ambitious models subsequently emerged that included all components of SC (Horan et al., 2009, Roberts et al., 2014, Rocha and Queirós, 2013). However, all of these models required a significant number of sessions (between 12 and 45), were typically applied in a group setting and required specific training by the therapists, factors that hindered their application in the clinical setting (Roberts et al., 2010). With this objective in mind, we designed an online rehabilitation program for SC, limited to just 12 sessions (the minimum number of face-to-face sessions reported in previous studies.)
Computerized training, conversely, allows for their application with minimal supervision, which enables access by the entire target population and produces clear financial savings (Ventura et al., 2013).
Computer-based programs can be classified into three groups:
-
(1)
Slide-based tutorials oriented toward group treatment, focused on a single domain such as Metacognitive Training (Aghotor et al., 2010) or with a more comprehensive aim, such as the Social Cognition Training Program (PECS) (Gil Sanz et al., 2009, Gil-Sanz et al., 2014).
-
(2)
Programs devoted to improving emotion recognition, such as MRIGE (Mind Reading: An Interactive Guide to Emotions) (Lindenmayer et al., 2012) or METT (Micro-Expression Training Tool) (Russell et al., 2008).
-
(3)
A heterogeneous group of recently developed programs including Neuropersonal Trainer-Mental Health (TNP-SM) (Fernandez-Gonzalo et al., 2015), a cognitive rehabilitation program focused on attention, memory and executive functions including a module on social cognition; Soskitrain (Rus-Calafell et al., 2014), a virtual reality program for social skills training; R2CS (Peyroux & Franck, 2014) a French program on which has been published a description of the technology and Social Ville (Nahum et al., 2014, Rose et al., 2015), an online rehabilitation program focused on speeding processing, on which preliminary results have been published.
However, apart from improvements in emotion recognition, to date none of these strategies has demonstrated robust improvements in ToM or AS, and with the exception of Social Ville none is intended for self-training.
e-Motional Training® (ET®) allows online self-training and stores the data of each individual session. ET® is designed following the basic principles of neuropsychological rehabilitation in this domain (Brenner et al., 1987, Ochsner, 2008, Zubin and Spring, 1977). The program aims to deliver realistic and natural but attractive exercises of short duration without irrelevant stimuli or distractions, while offering continuous feedback. Emotion recognition tasks are designed with increasing difficulty, starting with tutorials, following with eyes and mouths recognition and finally scaling to microexpression training. An animated short film with 33 scenes is the vehicle for ToM, social perception and attributional style stories. After each scene, a series of questions including ToM, AS and control questions are posed. When the answer is incorrect, the patient receives metacognitive suggestions, which lead the user to think about the situation from a different perspective or prompts the user to pay attention to specific aspects of the film.
The program was composed of 12 1-hour sessions (the minimum number of face-to-face sessions reported in previous studies).
In this study, we present the feasibility and applicability results of our SC rehabilitation program: e-Motional Training® (ET®).
1.1. Objective
To assess the applicability and to explore the efficacy of a new online training program on SC in patients with chronic schizophrenia: e-Motional Training®.
Based on the characteristics of our program and the previous literature, we hypothesized that ET® would improve the three assessed SC domains (emotional recognition, ToM, EA) in the patients with schizophrenia but would not change the patients’ symptoms (PANSS).
2. Methodology
A pilot, pre/post intervention study on patients with chronic schizophrenia was performed. The patients were recruited at 3 centers: The University Hospital of Ourense (CHUO), the Association of Persons and Families with Mental Illness of Ourense (MOREA) and the Ceboliño Community Residence (Ourense).
Inclusion criteria: We included patients who voluntarily agreed to participate in the study, aged 18–50 years with a diagnosis of schizophrenia (DSM-IV TR), who were clinically stable (no acute psychotic symptoms and not hospitalized during the last three months), and who had no comorbidity with other psychiatric or neurological diseases (International Neuropsychiatric Interview-MINI) and excluding current substance abuse (except nicotine).
2.1. Description of the intervention
The control group received standard treatment (TAU) (occupational therapy and leisure group).
The intervention group received TAU plus 12 sessions (1 hour per week) with ET® (including training modules on emotional perception and a short animated cartoon for ToM and AS training, including automatic metacognitive feedback). Some 30% of the participants participated in the intervention from their homes, visiting the center only for the assessments and for the first session of the intervention. The rest of the participants (70%) performed the intervention at the healthcare center under direct supervision. All participants in the intervention group (regardless of mode: clinical or online) completed the same number of sessions.
To start the intervention, the patient accessed the website www.e-motionaltraining.com and registered with a username and password.
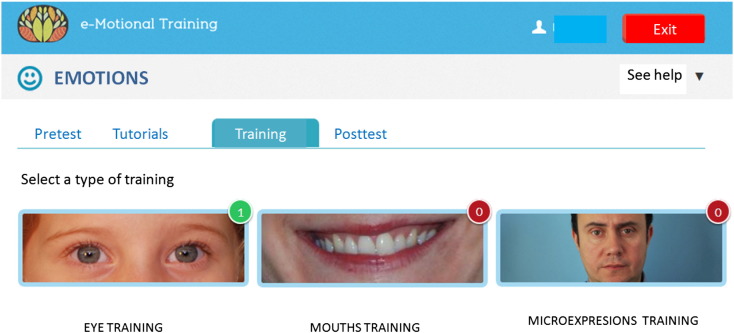
The first 4 meetings (1 h each session) are dedicated to recognizing facial emotions. This section includes a pre and post test, tutorials, and scaling minigames starting with eyes and mouths and finally microexpression (< 250 ms) training (Fig. 1).
Fig. 1.
Training module on emotions.
The next 8 sessions (1 h each) include watching a short, interactive animated cartoon in which a couple invites their friends to their home for a party. As the story unfolds, instances of miscommunication occur among the actors, causing various emotions and mental conditions such as anger, affection, appreciation and jealousy. After each scene, the user is queried about what happened, with questions about ToM (interpreting irony, insinuations, faux pas, 2nd-order false beliefs, etc.), social perception (interpretation and analysis of the social situation through the visual content of each scene) and attributive style (the individuals’ attributions to the events, and questions such as, “What kind of thinking would result in Cristina getting better results in this situation?”), as well as control questions. The game provides user feedback and, in the event of errors, can display a hyperlink with information and metacognitive strategies, whose objective is to help users understand the scene that they just watched (Fig. 2).
Fig. 2.
Training module on ToM and AS.
In our study, the researcher (MVC) monitored the patients’ performance and resolved the initial questions regarding computer and software use, but did not provide any assistance with the training tasks.
Apart from offering immediate feedback and a progress summary, e-Motional Training® stores the results of each session individually in a database with access restricted to the therapist or researcher.
2.2. Instruments
The post training assessment was performed during the month following the end of treatment at patients’ convenience, using the following battery of tests1:
-
(a)
Ekman 60 Faces Test (r = 0.62; v = 0.81) (Ekman and Friesen, 1976): a computer test based on the facial recognition of emotional expressions. The test contains 60 photographs of faces with expressions of the 6 basic emotions: anger, disgust, sadness, fear, surprise and happiness.
-
(b)
Hinting Task (r = 2.5 ± 0.53; v = 6.60 ± 0.84) (Corcoran et al, 1995) (Spanish version of Gil, 2012): the individual must identify what the story character really meant to say.
-
(c)
Recognition of Faux Pas (r = 7.00 ± 2.16; v = 3.73 ± 1.42) (Baron-Cohen, 1997): the participant must identify the embarrassing situations or gaffes.
-
(d)
Strange Stories of Happé (Spanish version of Pousa, 1999): the participant must understand the emotions, intentions and thoughts of the characters in the various stories.
-
(e)
Ambiguous Intentions Hostility Questionnaire (AIHQ) (r = 6.27 ± 1.27; v = 2.73 ± 1.19) (Combs et al., 2007b): which explores the attributional cognitive biases (hostility, intent, guilt, anger and aggressiveness) in 3 types of situations: ambiguous (AIHQ-AM), intentional (AIHQ-INT) and accidental (AIHQ-AC).
-
(f)
Mayer-Salovey-Caruso Emotional Intelligence Test (MSCEIT) (r = 0.95; v = 0.83) (Spanish version of Extremera and Fernández-Berrocal, 2009): an emotional intelligence test recommended by the MATRICS initiative (Measurement and Treatment Research to Improve Cognition in Schizophrenia). The MSCEIT provides one total score and four branch scores (Perceiving Emotions, Facilitating Thought, Understanding Emotions, Managing Emotions).
-
(g)
Positive and Negative Symptom Scale (PANSS) (Kay et al., 1987): assesses positive and negative symptom severity.
-
(h)
The Wechsler Adult Intelligence Scale (WAIS-IV, 2012): includes a total intelligence score (IQ), verbal comprehension index (VCI), working memory index (WMI), perceptual information index (POI) and processing speed index (PSI).
-
(i)
Semistructured, self-designed interview and direct observation of the participants to assess their tolerability and opinion of the intervention, as well as potential difficulties related to the intervention.
MVC was responsible for pre and post testing.
3. Statistical analysis
A descriptive analysis was first performed. The qualitative variables are presented with their absolute frequency and percentage. The quantitative Gaussian variables are presented as mean and standard deviation, and the non-Gaussian variable is presented as median [minimum–maximum]. To compare 2 qualitative variables we used the chi-squared test.
To compare the quantitative variables, we used Student’s t-test for independent samples and for paired samples (in Gaussian variables) and U–Mann Whitney, Wilcoxon (in non-Gaussian). The accepted α risk was 0.05. The data were analyzed using SPSS 15.0 software.
4. Results
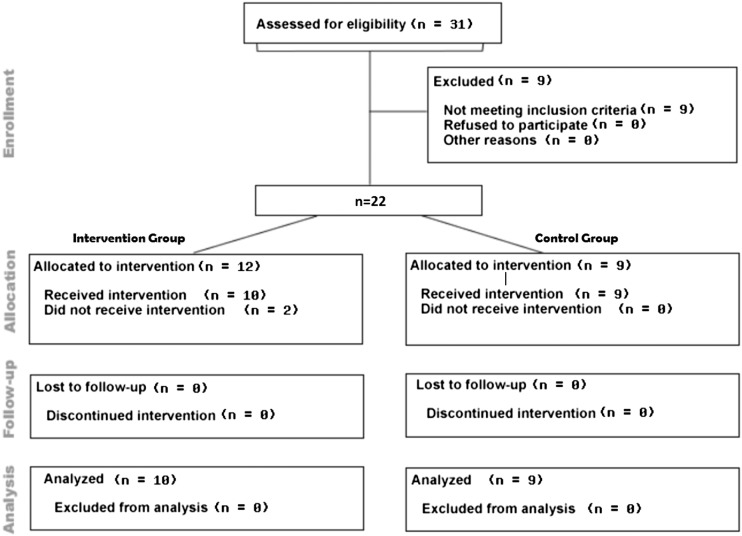
A total of 31 participants were recruited during a 6-month period, 22 of whom met the selection criteria. Twelve participants were included in the intervention group, and 9 were included in the control group. There were two patients lost to follow-up in the intervention group (both occurred before the ET training), one was a relapse and the other committed suicide (Fig. 3).
Fig. 3.
Flowchart.
All patients provided informed consent (both verbal and written) to participate in this study.
All variables followed a normal distribution, except for happiness in Ekman’s 60 faces, due to ceiling effects.
There were no significant differences in the demographic and clinical characteristics between the 2 groups. At baseline, there were statistically significant differences in the total results from Faux Pas (p = 0.044), thus the control group demonstrated poorer performance.
At the start of the study, the participants were a mean age of 39.47 (± 9.10) years. Table 1 shows the characteristics and demographic variables of the 2 groups.
Table 1.
Participant characteristics.
| Control Group | Intervention Group | p | ||
|---|---|---|---|---|
| Mean age years (SD) | 41.78 (9.39) | 37.40 (8.79) | 0.31 | |
| Sex | Male, n | 5 | 7 | 0.51 |
| Female, n | 4 | 3 | ||
| Education level | Primary, n | 4 | 3 | 0.38 |
| Secondary, n | 4 | 7 | ||
| Tertiary, n | 1 | 0 | ||
| Occupation | Unemployed, n | 1 | 2 | 0.46 |
| Retired, n | 8 | 6 | ||
| Employed, n | 0 | 1 | ||
| Student, n | 0 | 1 | ||
| Marital status | Single, n | 8 | 9 | 0.93 |
| Married, n | 0 | 0 | ||
| Separated, n | 1 | 1 | ||
| Widowed/Other, n | 0 | 0 | ||
| Computer skills | None, n | 2 | 3 | 0.46 |
| User, n | 6 | 4 | ||
| Expert, n | 1 | 3 | ||
| Mean age at diagnosis (SD) | 24.56 (10) | 23.40 (7.24) | 0.78 | |
| Mean treatment, mg of chlorpromazine (SD) | 380.56 (101.37) | 463.80 (105.92) | 0.10 | |
| Hospital admissions, n (SD) | 0.78 (1.09) | 1.1 (0.99) | 0.51 | |
| WAIS-Total | 68.68 (10.95) | 77.50 (13.89) | 0.18 | |
| WAIS-VC | 80.33 (18.46) | 86.30 (12.79) | 0.40 | |
| WAIS-PR | 71.44 (17.40) | 76.10 (16.51) | 0.44 | |
| WAIS-WM | 74.67 (11.03) | 83.10 (14.07) | 0.09 | |
| WAIS-PS | 73.33 (5.87) | 82.60 (13.42) | 0.09 |
VC: Verbal Comprehension. PR: Perceptual Reasoning. WM: Working Memory. PS: Processing Speed.
The enrolled patients were diagnosed with schizophrenia at the age of approximately 24 (± 8.42) years, were taking a dosage equivalent to 424 mg of chlorpromazine per day and had been hospitalized once due to exacerbations of their psychiatric disease (Table 1).
4.1. Feasibility
Except for the 2 patients lost to follow-up before starting the intervention, all participants in the intervention group completed the training at the scheduled meetings. Ninety percent of the participants stated that they found the game to be easy, and all declared that ET was entertaining and amusing, suggesting their interest in performing similar computer activities in the future. Some 70% found the program useful for improving their social relations and 30% found it very useful. Regarding online self-treatment, 57% of patients trained at the health facility stated their willingness to play it at home. Some 90.9% of the patients expressed their interest in participating in similar online interventions.
4.2. Emotion recognition
At baseline, both groups had difficulties with fear, sadness and anger whereas normal results were obtained for happiness and surprise (Table 2). One month after the intervention, the intervention group showed a statistically significant improvement in total perception scores, with greater improvements in the emotions more affected at baseline. The control group showed a significant decline in total perception scoring.
Table 2.
Scores pre and post intervention.
| Control Group |
Intervention Group |
|||||
|---|---|---|---|---|---|---|
| Pre Mean (SD) | Post Mean (SD) | p⁎ | Pre Mean (SD) | Post Mean (SD) | p⁎ | |
| Ekman Total | 38.44 (7.40) | 35.78 (7.53) | 0 .025⁎⁎ | 44 (4.47) | 55.60 (2.17) | < 0 .001⁎⁎ |
| Happiness + | 10[6–10] | 9 .92[6–10] | 0 .999 | 10[9–10] | 10[9–10] | 0 .317 |
| Surprise | 7.56 (2.60) | 7 (2.92) | 0 .139 | 8.30 (1.16) | 9.70 (0.48) | 0 .007⁎⁎ |
| Fear | 4.22 (2.68) | 3.44 (2.70) | 0 .133 | 5.90 (2.33) | 8.60 (1.77) | 0 .002⁎⁎ |
| Sadness | 5.89 (2.03) | 5.11 (2.26) | 0 .133 | 5.30 (1.56) | 9 (0.94) | 0 .001⁎⁎ |
| Disgust | 6 (2.92) | 6 (2.29) | 0 .999 | 7.80 (2.15) | 9.80 (0.42) | 0 .010⁎⁎ |
| Anger | 5 (2.69) | 4.11 (2.42) | 0 .069 | 5.90 (1.52) | 1.16 | 0 .001⁎⁎ |
p-value: Paired samples t-test. +: Median [min–max] and p-value: Wilcoxon test.
p < 0.05 = statistical significance.
4.3. ToM
Baseline scores on the Faux Pas test were under the standard cutoff point of 54 out of 60 points. After training, the intervention group showed a significant improvement in Faux Pas detection question scores (p < 0.001)
Baseline scores on Happé’s Strange Stories were under the standard cutoff point of 14 out of 16. After training, the intervention group showed a statistically significant improvement (p = 0.01), and there were no changes were in the control group.
Baseline scores on the Hinting Task test revealed a deficit in this area, with a score of 14.56 for the control group and 12.70 for the intervention group, respectively (maximum score is 20 points). Patients in the intervention group showed a significant improvement in comparison with the control group (p = 0.006).
Regarding attributive style, we used the Ambiguous Intent Attribution Questionnaire (AIHQ), which explores the attributional cognitive biases (hostility, intent, guilt, anger and aggressiveness) in 3 types of situations: ambiguous (AIHQ-AM), intentional (AIHQ-INT) and accidental (AIHQ-AC). Both groups showed improved performance in the total AIHQ scores after completing the study (Table 3). These differences were more pronounced in the intervention group, with a significant improvement in the answers for ambiguous (p = 0.002) and intentional (p = 0.031) situations.
Table 3.
Scores pre and post intervention.
| Control Group |
Intervention Group |
|||||
|---|---|---|---|---|---|---|
| Pre Mean (SD) | Post Mean (SD) | p⁎ | Pre Mean (SD) | Post Mean (SD) | p⁎ | |
| Happé | 6.67 (4.27) | 6.89 (4.31) | 0.512 | 8.20 (3.58) | 11.20 (4.68) | 0.010⁎⁎ |
| Faux Pas | 18.78 (12.89) | 20.56 (15.33) | 0.353 | 31.40 (12.43) | 38.30 (19.20) | 0.131 |
| Detect. FP | 3.67 (2.39) | 3.67 (2.59) | 0.999 | 5.90 (2.37) | 8 (2.98) | < 0.001⁎⁎ |
| Hinting | 14.56 (3.28) | 14.56 (3.94) | 0.999 | 12.70 (4.45) | 16.90 (4.82) | 0.006⁎⁎ |
| AIAQ-T | 172.56 (21.11) | 166.22 (20.56) | 0.076 | 178.40 (54.98) | 167.40 (51.01) | 0.131 |
| AIAQ-AM | 62.56 (7.76) | 62.89 (7.97) | 0.814 | 69.20 (25.34) | 61 (22.70) | 0.002⁎⁎ |
| AIAQ-INT | 65.78 (10.47) | 65 (8.60) | 0.622 | 74.80 (19.60) | 72.70 (21.25) | 0.031⁎⁎ |
| AIAQ-AC | 44.22 (10.95) | 40.44 (12.46) | 0.062 | 44.50 (15.75) | 41.30 (13.50) | 0.064 |
| MSCEIT | 86.56 (13.50) | 82.78 (9.06) | 0.124 | 96.10 (14.36) | 95.60 (10.45) | 0.763 |
| PANSS-T | 26.11 (6.27) | 26 (6.44) | 0.729 | 36.40 (14.54) | 29.80 (9.88) | 0.012⁎⁎ |
| PANSS-P | 11.89 (4.34) | 11.78 (4.23) | 0.347 | 17.30 (7.18) | 16.40 (7.60) | 0.753 |
| PANSS-N | 14.22 (3.66) | 14.22 (3.76) | 0.999 | 19.80 (8.67) | 14.40 (6.72) | 0.098 |
p-value: Paired samples t-test.
p < 0.05 = statistical significance.
The patients included in the study (control and intervention groups) showed responses at baseline within the normal range in emotional intelligence as measured with the MSCEIT. There were no improvements in MSCEIT scores after the intervention or TAU.
No differences were found between the participants in the intervention group who performed the intervention from their homes and those who were directly supervised at healthcare facilities.
Finally, there were statistically significant improvements in the PANSS scores in the intervention group (Table 3).
5. Discussion
The results of this pilot study suggest that ET® is an attractive intervention, with a wide age range, and it is feasible and reliable for use, even if the user has no previous experience with information technology.
Following the intervention with ET®, the difficulties in recognizing facial emotions were reduced, with patients achieving scores within the normal range and similar to those of the general population (Dodich et al., 2014, Young et al., 1997). These results are consistent with those achieved by similar strategies for rehabilitating emotional perception, such as the strategy performed with METT (Russell et al., 2008) or NPT-SM (Fernandez-Gonzalo et al., 2015). After a single training session for identifying microexpressions, these researchers found an improvement in emotional recognition, results that are similar to those of a study performed with Emotion Management Therapy (EMT) (Hodel et al., 1998). A pilot study was conducted with Training of Affect Recognition (TAR) (Frommann et al., 2003) a program that includes training on differentiating the 6 basic emotions, as well as training for integrating facial expressions into overall processing. The study results were not statistically significant, but subsequent results of clinical trials with TAR showed improvements in terms of emotion recognition skills (Wo et al., 2005) and a certain generalization on other measures of social cognition, including ToM (Wölwer and Frommann, 2011).
After training with ET®, the patients with chronic schizophrenia had a statistically significant improvement in emotional perception, detection of gaffes (Faux Pas) and other ToM scales (Hinting Task and Happé tests). However, their final scores did not reach the performance ranges of the general population. A number of studies conducted with the Social Cognition and Interaction Training (SCIT) group intervention (Lahera et al., 2013, Penn et al., 2005) and with Metacognitive and Social Cognition Training (Rocha and Queirós, 2013) have also demonstrated improved emotional perception and ToM. However, with regard to the latter, other studies performed with SCIT had conflicting results (Roberts et al., 2014).
We found differences in our pilot study regarding attributive style between the groups. The vast majority of published studies using SCIT (Lahera et al., 2013, Penn et al., 2005), Emotion and ToM Imitation Training (Mazza et al., 2010), Social Cognitive Skills Training (SCST) (Horan et al., 2009) and Metacognitive and Social Cognition Training (Rocha and Queirós, 2013), found no differences in this variable. Only one study, using SCIT (Combs et al., 2007a), showed a reduction in hostile attributions toward others, with a medium to large effect size.
Our study found no differences regarding emotional intelligence (as assessed with MSCEIT) following the intervention; this was also the case in other studies (Lindenmayer et al., 2012, Nahum et al., 2014, Rocha and Queirós, 2013). Additionally, the patients had baseline scores close to or within the normal range, which contradicts the data from the other SC scales and their own clinical impression. These facts prompt us to doubt on the validity of MSCEIT for the assessment of schizophrenia patients.
Finally, our results showed a significant improvement in PANSS scores, which can be attributed to an amelioration of negative symptoms. It can be argued that PANSS improvement is on the basis of the SC reported changes, but despite its occurrence, this association was not reported in previous studies (Kayser et al., 2006, Rus-Calafell et al., 2014), or in a meta-analysis of 19 clinical trials that assessed the efficacy of various SC interventions (Kurtz and Richardson, 2012).
ET® was feasible and well accepted, allowing individual self-training and online follow-up, favoring accessibility and autonomy. Moreover, we have shown improvements in all the subdomains of SC except for social perception (which was not assessed).
5.1. Limitations of the study
The study was not randomized. The patients were assigned to the various treatments as convenient in a consecutive manner. The first 12 patients were assigned to the intervention group and the remainder to the control group. Due to the study’s exploratory nature, we did not add assessments that measured generalization, using scales that assessed functionality, but perhaps this fact might have provided relevant information. The patient assessments were not blinded, and a number of these tests have no objective scoring methods.
Contributors
MVC, AAGC and YMS devised and designed the study and acquired and interpreted the data. They also drafted the article.
GLF and RMA performed the critical review of the intellectual content and approved the final version of the submitted article.
Conflict of interest
The authors declare no conflicts of interest.
Acknowledgments
This study was made possible with the help of the College of Physicians of Ourense, by granting Cabaleiro Goas-Prize and the College of Psychologists of Galicia for the award of the Siota grant.
Footnotes
The reliability (r) and validity (v) values for the AIHQ, Faux Pas and Hinting Task scales are expressed as mean and standard deviation (on a scale from 1 to 9, according to expert consensus), and the other measures are expressed according to the corresponding coefficient. The Happe test, despite being one of the classical tasks in assessing ToM, has no data on r or v.
References
- Addington J., Saeedi H., Addington D. Influence of social perception and social knowledge on cognitive and social functioning in early psychosis. Br. J. Psychiatry. 2006;189:373–378. doi: 10.1192/bjp.bp.105.021022. [DOI] [PubMed] [Google Scholar]
- Addington J., Girard T.A., Christensen B.K., Addington D. Social cognition mediates illness-related and cognitive influences on social function in patients with schizophrenia-spectrum disorders. J. Psychiatry Neurosc. 2010;35(1):49–54. doi: 10.1503/jpn.080039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aghotor J., Pfueller U., Moritz S., Weisbrod M., Roesch-Ely D. Metacognitive training for patients with schizophrenia (MCT): feasibility and preliminary evidence for its efficacy. J. Behav. Ther. Exp. Psychiatry. 2010;41(3):207–211. doi: 10.1016/j.jbtep.2010.01.004. [DOI] [PubMed] [Google Scholar]
- Baron-Cohen S. Hey! It was just a joke! Understanding propositions and propositional attitudes by normally developing children and children with autism. Isr. J. Psychiatry Relat. Sci. 1997;34(3):174–178. [PubMed] [Google Scholar]
- Bigelow N.O., Paradiso S., Adolphs R., Moser D.J., Arndt S., Heberlein A.…Andreasen N.C. Perception of socially relevant stimuli in schizophrenia. Schizophr. Res. 2006;83:257–267. doi: 10.1016/j.schres.2005.12.856. [DOI] [PubMed] [Google Scholar]
- Brenner H.D., Hodel B., Kube G., Roder V. Cognitive therapy of schizophrenic patients: problem analysis and empirical results. Nervenarzt. 1987;58(2):72–83. [PubMed] [Google Scholar]
- Brüne M. Emotion recognition, “theory of mind”, and social behavior in schizophrenia. Psychiatry Res. 2005;133(2–3):135–147. doi: 10.1016/j.psychres.2004.10.007. [DOI] [PubMed] [Google Scholar]
- Brüne M. “Theory of mind” in schizophrenia: a review of the literature. Schizophr. Bull. 2005;31(1):21–42. doi: 10.1093/schbul/sbi002. [DOI] [PubMed] [Google Scholar]
- Casacchia M., Mazza M., Roncone R. Theory of mind, social development, and psychosis. Curr. Psychiatry Rep. 2004;6(3):183–189. doi: 10.1007/s11920-004-0063-3. [DOI] [PubMed] [Google Scholar]
- Chung Y.S., Barch D., Strube M. A meta-analysis of mentalizing impairments in adults with schizophrenia and autism spectrum disorder. Schizophr. Bull. 2014;40(3):602–616. doi: 10.1093/schbul/sbt048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Combs D.R., Adams S.D., Penn D.L., Roberts D., Tiegreen J., Stem P. Social Cognition and Interaction Training (SCIT) for inpatients with schizophrenia spectrum disorders: preliminary findings. Schizophr. Res. 2007;91:112–116. doi: 10.1016/j.schres.2006.12.010. [DOI] [PubMed] [Google Scholar]
- Combs D.R., Penn D.L., Wicher M., Waldheter E. The Ambiguous Intentions Hostility Questionnaire (AIHQ): a new measure for evaluating hostile social-cognitive biases in paranoia. Cogn. Neuropsychiatry. 2007;12(2):128–143. doi: 10.1080/13546800600787854. [DOI] [PubMed] [Google Scholar]
- Combs D.R., Penn D.L., Tiegreen J.A., Nelson A., Ledet S.N., Basso M.R., Elerson K. Stability and generalization of Social Cognition and Interaction Training (SCIT) for schizophrenia: six-month follow-up results. Schizophr. Res. 2009;112(1–3):196–197. doi: 10.1016/j.schres.2009.04.010. [DOI] [PubMed] [Google Scholar]
- Corcoran R., Mercer G., Frith C.D. Schizophrenia, symptomatology and social inference: investigating “theory of mind” in people with schizophrenia. Schizophr. Res. 1995;17(1):5–13. doi: 10.1016/0920-9964(95)00024-g. [DOI] [PubMed] [Google Scholar]
- Couture S.M., Penn D.L., Roberts D.L. The functional significance of social cognition in schizophrenia: a review. Schizophr. Bull. 2006;32:44–63. doi: 10.1093/schbul/sbl029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dodich A., Cerami C., Canessa N., Crespi C., Marcone A., Arpone M.…Cappa S.F. Emotion recognition from facial expressions: a normative study of the Ekman 60-Faces Test in the Italian population. Neurol. Sci. 2014;35(7):1015–1021. doi: 10.1007/s10072-014-1631-x. [DOI] [PubMed] [Google Scholar]
- Ekman P., Friesen W. Consulting Psychologists Press; Palo Alto, CA: 1976. Pictures of facial affect. [Google Scholar]
- Extremera N., Fernández-Berrocal P. 2009. Adaptación española del test de inteligencia emocional de Mayer-Salovey-Caruso (MSCEIT): manual y cuadernillo. (TEA, Ed.). Madrid. [Google Scholar]
- Fernandez-Gonzalo S., Turon M., Jodar M., Pousa E., Hernandez Rambla C., García R., Palao D. A new computerized cognitive and social cognition training specifically designed for patients with schizophrenia/schizoaffective disorder in early stages of illness: a pilot study. Psychiatry Res. 2015;228(3):501–509. doi: 10.1016/j.psychres.2015.06.007. [DOI] [PubMed] [Google Scholar]
- Frommann N., Streit M., Wölwer W. Remediation of facial affect recognition impairments in patients with schizophrenia: a new training program. Psychiatry Res. 2003;117(3):281–284. doi: 10.1016/s0165-1781(03)00039-8. [DOI] [PubMed] [Google Scholar]
- Gil D. Adaptación al español de la prueba de teoría de la mente Hinting Task. Rev. Psiquiatr. Salud Ment. (Barc) 2012;5(5):79–88. doi: 10.1016/j.rpsm.2011.11.004. [DOI] [PubMed] [Google Scholar]
- Gil Sanz D., Diego Lorenzo M., Bengochea Seco R., Arrieta Rodríguez M., Lastra Martínez I., Sánchez Calleja R., Alvarez Soltero A. Efficacy of a social cognition training program for schizophrenic patients: a pilot study. Span. J. Psychol. 2009;12(1):184–191. doi: 10.1017/s1138741600001591. [DOI] [PubMed] [Google Scholar]
- Gil-Sanz D., Fernández-Modamio M., Bengochea-Seco R., Arrieta-Rodríguez M., Pérez-Fuentes G. Efficacy of the Social Cognition Training Program in a sample of schizophrenic outpatients. Clin. Schizophr. Relat. Psychoses. 2014 doi: 10.3371/CSRP.GIFE.013114. [DOI] [PubMed] [Google Scholar]
- Green M.F., Penn D.L., Bentall R., Carpenter W.T., Gaebel W., Gur C.…Park S. Social cognition in schizophrenia: an NIMH workshop on definitions, assessment, and research opportunities. Schizophr. Bull. 2008;34(6):1211–1220. doi: 10.1093/schbul/sbm145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasson-Ohayon I., Mashiach-Eizenberg M., Avidan M., Roberts D.L., Roe D. Social cognition and interaction training: preliminary results of an RCT in a community setting in Israel. Psychiatr. Serv. 2014;65(4):555–558. doi: 10.1176/appi.ps.201300146. [DOI] [PubMed] [Google Scholar]
- Hodel B., Brenner H.D., Merlo M.C., Teuber J.F. Emotional management therapy in early psychosis. Br. J. Psychiatry Suppl. 1998;172(33):128–133. [PubMed] [Google Scholar]
- Horan W.P., Kern R.S., Shokat-fadai K., Sergi M.J., Wynn J.K., Green M.F. Social cognitive skills training in schizophrenia: an initial efficacy study of stabilized outpatients. Schizophr. Res. 2009;107(1):47–54. doi: 10.1016/j.schres.2008.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kay S.R., Fiszbein A., Opler L.A. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr. Bull. 1987;13(2):261–276. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- Kayser N., Sarfati Y., Besche C., Hardy-Baylé M.-C. Elaboration of a rehabilitation method based on a pathogenetic hypothesis of “theory of mind” impairment in schizophrenia. Neuropsychol. Rehabil. 2006;16(1):83–95. doi: 10.1080/09602010443000236. [DOI] [PubMed] [Google Scholar]
- Kohler C.G., Walker J.B., Martin E.A., Healey K.M., Moberg P.J. Facial emotion perception in schizophrenia: a meta-analytic review. Schizophr. Bull. 2010;36(5):1009–1019. doi: 10.1093/schbul/sbn192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurtz M.M., Richardson C.L. Social cognitive training for schizophrenia: a meta-analytic investigation of controlled research. Schizophr. Bull. 2012;38(5):1092–1104. doi: 10.1093/schbul/sbr036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahera G., Benito A., Montes J.M., Fernández-Liria A., Olbert C.M., Penn D.L. Social cognition and interaction training (SCIT) for outpatients with bipolar disorder. J. Affect. Disord. 2013;146(1):132–136. doi: 10.1016/j.jad.2012.06.032. [DOI] [PubMed] [Google Scholar]
- Lahera G., Herrera S., Fernández C., Bardón M., de los Ángeles V., Fernández-Liria A. Familiarity and face emotion recognition in patients with schizophrenia. Compr. Psychiatry. 2014;55(1):199–205. doi: 10.1016/j.comppsych.2013.06.006. [DOI] [PubMed] [Google Scholar]
- Langdon R., Still M., Connors M.H., Ward P.B., Catts S.V. Attributional biases, paranoia, and depression in early psychosis. Br. J. Clin. Psychol. 2013;52(4):408–423. doi: 10.1111/bjc.12026. [DOI] [PubMed] [Google Scholar]
- Lindenmayer J.-P., McGurk S.R., Khan A., Kaushik S., Thanju A., Hoffman L.…Herrmann E. Improving social cognition in schizophrenia: a pilot intervention combining computerized social cognition training with cognitive remediation. Schizophr. Bull. 2012;64:1–11. doi: 10.1093/schbul/sbs120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazza M., Lucci G., Pacitti F., Pino M.C., Mariano M., Casacchia M., Roncone R. Could schizophrenic subjects improve their social cognition abilities only with observation and imitation of social situations? Neuropsychol. Rehabil. 2010;20:675–703. doi: 10.1080/09602011.2010.486284. [DOI] [PubMed] [Google Scholar]
- Mizrahi R., Addington J., Remington G., Kapur S. Attribution style as a factor in psychosis and symptom resolution. Schizophr. Res. 2008;104(1–3):220–227. doi: 10.1016/j.schres.2008.05.003. [DOI] [PubMed] [Google Scholar]
- Nahum M., Fisher M., Loewy R., Poelke G., Ventura J., Nuechterlein K.H.…Vinogradov S. A novel, online social cognitive training program for young adults with schizophrenia: a pilot study. Schizophr. Res. Cogn. 2014;1(1):e11–e19. doi: 10.1016/j.scog.2014.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ochsner K. The social-emotional processing stream: five core constructs and their translational potential for schizophrenia and beyond. Biol. Psychiatry. 2008;64(1):48–61. doi: 10.1016/j.biopsych.2008.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penn D.L., Combs D. Modification of affect perception deficits in schizophrenia. Schizophr. Res. 2000;46(2–3):217–229. doi: 10.1016/s0920-9964(00)00005-0. [DOI] [PubMed] [Google Scholar]
- Penn D.L., Spaulding W., Reed D., Sullivan M. The relationship of social cognition to ward behavior in chronic schizophrenia. Schizophr. Res. 1996;20(3):327–335. doi: 10.1016/0920-9964(96)00010-2. [DOI] [PubMed] [Google Scholar]
- Penn D., Roberts D.L., Munt E.D., Silverstein E., Jones N., Sheitman B. A pilot study of social cognition and interaction training (SCIT) for schizophrenia. Schizophr. Res. 2005;80(2–3):357–359. doi: 10.1016/j.schres.2005.07.011. [DOI] [PubMed] [Google Scholar]
- Penn D.L., Sanna L.J., Roberts L. Social cognition in schizophrenia: an overview. Schizophr. Bull. 2008;34(3):408–411. doi: 10.1093/schbul/sbn014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peyroux E., Franck N. RC2S: A Cognitive Remediation Program to Improve Social Cognition in Schizophrenia and Related Disorders. Frontiers in Human Neuroscience. 2014;8:400. doi: 10.3389/fnhum.2014.00400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinkham A.E. Social cognition in schizophrenia. J. Clin. Psychiatry. 2014;75(Suppl. 2):14–19. doi: 10.4088/JCP.13065su1.04. [DOI] [PubMed] [Google Scholar]
- Pinkham A.E., Penn D.L. Neurocognitive and social cognitive predictors of interpersonal skill in schizophrenia. Psychiatry Res. 2006;143(2–3):167–178. doi: 10.1016/j.psychres.2005.09.005. [DOI] [PubMed] [Google Scholar]
- Pousa E. Universidad Autónoma de Barcelona; 1999. Measurement of Theory of Mind in healthy adolescents: translation and cultural adaptation of F. Happé’s Theory of Mind Stories. [Google Scholar]
- Roberts D.L., Penn D.L. Social cognition and interaction training (SCIT) for outpatients with schizophrenia: a preliminary study. Psychiatry Res. 2009;166(2–3):141–147. doi: 10.1016/j.psychres.2008.02.007. [DOI] [PubMed] [Google Scholar]
- Roberts D.L., Penn D.L., Labate D., Margolis S.A., Sterne A. Transportability and feasibility of Social Cognition And Interaction Training (SCIT) in community settings. Behav. Cogn. Psychother. 2010;38:35–47. doi: 10.1017/S1352465809990464. [DOI] [PubMed] [Google Scholar]
- Roberts D.L., Combs D.R., Willoughby M., Mintz J., Gibson C., Rupp B., Penn D.L. A randomized, controlled trial of Social Cognition and Interaction Training (SCIT) for outpatients with schizophrenia spectrum disorders. Br. J. Clin. Psychol. 2014;53(3):281–298. doi: 10.1111/bjc.12044. [DOI] [PubMed] [Google Scholar]
- Rocha N.B.F., Queirós C. Metacognitive and social cognition training (MSCT) in schizophrenia: a preliminary efficacy study. Schizophr. Res. 2013;150(1):64–68. doi: 10.1016/j.schres.2013.07.057. [DOI] [PubMed] [Google Scholar]
- Roder V., Mueller D.R., Schmidt S.J. Effectiveness of integrated psychological therapy (IPT) for schizophrenia patients: a research update. Schizophr. Bull. 2011;37(Suppl. 2):S71–S79. doi: 10.1093/schbul/sbr072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose A., Vinogradov S., Fisher M., Green M.F., Ventura J., Hooker C.…Nahum M. Randomized controlled trial of computer-based treatment of social cognition in schizophrenia: the TRuSST trial protocol. BMC Psychiatry. 2015;15(1):142. doi: 10.1186/s12888-015-0510-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rus-Calafell M., Gutiérrez-Maldonado J., Ribas-Sabaté J. A virtual reality-integrated program for improving social skills in patients with schizophrenia: a pilot study. J. Behav. Ther. Exp. Psychiatry. 2014;45(1):81–89. doi: 10.1016/j.jbtep.2013.09.002. [DOI] [PubMed] [Google Scholar]
- Russell T.A., Chu E., Phillips M.L. A pilot study to investigate the effectiveness of emotion recognition remediation in schizophrenia using the micro-expression training tool. Br. J. Clin. Psychol. 2006;45(Pt 4):579–583. doi: 10.1348/014466505X90866. [DOI] [PubMed] [Google Scholar]
- Russell T.A., Green M.J., Simpson I., Coltheart M. Remediation of facial emotion perception in schizophrenia: concomitant changes in visual attention. Schizophr. Res. 2008;103(1–3):248–256. doi: 10.1016/j.schres.2008.04.033. [DOI] [PubMed] [Google Scholar]
- Sarfati Y., Hardy-Baylé M.C., Brunet E., Widlöcher D. Investigating theory of mind in schizophrenia: influence of verbalization in disorganized and non-disorganized patients. Schizophr. Res. 1999;37(2):183–190. doi: 10.1016/s0920-9964(98)00154-6. [DOI] [PubMed] [Google Scholar]
- Savla G.N., Vella L., Armstrong C.C., Penn D.L., Twamley E.W. Deficits in domains of social cognition in schizophrenia: a meta-analysis of the empirical evidence. Schizophr. Bull. 2013;39(5):979–992. doi: 10.1093/schbul/sbs080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silver H., Goodman C., Knoll G., Isakov V. Brief emotion training improves recognition of facial emotions in chronic schizophrenia. A pilot study. Psychiatry Res. 2004;128(2):147–154. doi: 10.1016/j.psychres.2004.06.002. [DOI] [PubMed] [Google Scholar]
- Tseng H.-H., Chen S.-H., Liu C.-M., Howes O., Huang Y.-L., Hsieh M.H.…Hwu H.-G. Facial and prosodic emotion recognition deficits associate with specific clusters of psychotic symptoms in schizophrenia. PLoS One. 2013;8(6):e66571. doi: 10.1371/journal.pone.0066571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ventura J., Wilson S.A., Wood R.C., Hellemann G.S. Cognitive training at home in schizophrenia is feasible. Schizophr. Res. 2013;143(2–3):397–398. doi: 10.1016/j.schres.2012.11.033. [DOI] [PubMed] [Google Scholar]
- WAIS-IV . Pearson; Madrid: 2012. Escala de inteligencia de Wechsler para adultos-IV. [Google Scholar]
- Wo W., Frommann N., Halfmann S., Piaszek A., Gil-Sanz D., Gaebel W. Remediation of impairments in facial affect recognition in schizophrenia : efficacy and specificity of a new training program. Schizophr. Res. 2005;80:295–303. doi: 10.1016/j.schres.2005.07.018. [DOI] [PubMed] [Google Scholar]
- Wölwer W., Frommann N. Social-cognitive remediation in schizophrenia: generalization of effects of the Training of Affect Recognition (TAR) Schizophr. Bull. 2011;37(Suppl. 2):S63–S70. doi: 10.1093/schbul/sbr071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young A.W., Rowland D., Calder A.J., Etcoff N.L., Seth A., Perrett D.I. Facial expression megamix: tests of dimensional and category accounts of emotion recognition. Cognition. 1997;63(3):271–313. doi: 10.1016/s0010-0277(97)00003-6. [DOI] [PubMed] [Google Scholar]
- Zubin J., Spring B. Vulnerability — a new view of schizophrenia. J. Abnorm. Psychol. 1977;86(2):103–126. doi: 10.1037//0021-843x.86.2.103. [DOI] [PubMed] [Google Scholar]