Abstract
Background and Objectives:
Every year ∼20 million inguinal hernia repairs are completed worldwide. Increased patient access to medical information and education has elicited interest in minimally invasive surgical techniques that obtain improved surgical outcomes and cosmesis. Because of these factors, there is a growing interest in single-incision surgery. Laparoscopic totally extraperitoneal (TEP) single-incision hernia repair technique has been reported with different meshes used in a tack fixation system. Recently, self-fixating mesh technology has offered the possibility of avoiding tack fixation and potentially avoiding chronic postoperative pain. Self-fixating mesh technology employs monofilament polylactic acid (PLA) creating a microgrip system that provides self-adherence of the mesh to adjacent tissue. This tack-free fixation system provides coverage over the entire myopectineal orifice and surrounding areas where traditional tacks cannot be placed. Self-fixating mesh has also been safely applied in laparoscopic TEP procedures, but this mesh has not been described in single site TEP surgery; possibly because of the potential difficulty with mesh deployment. We sought to determine the technical feasibility of a single-site laparoscopic TEP repair of inguinal hernias and to discuss our techniques and patient short-term outcomes.
Methods:
Review of a prospectively maintained database of patients who received single-site laparoscopic TEP herniorrhaphy from August 2012 through August 2015. Patient characteristics and demographics and perioperative and postoperative data were analyzed.
Results:
Thirty-four patients (aged 55.2 ±14.2; 17.6% women) with a mean body mass index of 26.2 ± 3.9 were analyzed. Mean operative time was 99.5 ± 30.5 minutes, 41.2% were left-side repairs, and 50% were bilateral. Estimated blood loss was 18.4 ± 14.1 mL. Recurrent hernias accounted for 14.7% of cases; 32.4% of cases were combination surgeries, most commonly a concurrent umbilical hernia repair. The most common short-term postoperative complication was urinary retention (4 patients). The median length of follow-up was 25 days (IQR 18.75–61.75). Complications occurring at >30 days included hydrocele (2 patients) and stitch abscess (1 patient). Eight (23.5%) patients had complications (surgical or during follow-up). No recurrences or deaths were reported.
Conclusions:
With comparable operative times, perioperative outcomes, and safety profile, SS-TEP appears to be a safe and effective surgical approach for the management of inguinal hernias in the short term. Furthermore, SS-TEP with a self-fixating mesh is a feasible approach.
Keywords: Laparoscopic single-site inguinal hernia repair, Self-fixating mesh
INTRODUCTION
Inguinal hernias are a common prevalent condition worldwide, with >20 million repairs performed annually.1 Recently, the proportion of laparoscopic inguinal hernia repairs have increased to nearly 40%.2–4 Furthermore, multiple studies have demonstrated safety and efficacy of laparoscopic inguinal hernia repair, and the 2 most common laparoscopic approaches include transabdominal preperitoneal (TAPP) and totally extraperitoneal (TEP), each with its own complication profile and learning curve.
The TAPP approach by definition entails entry into the peritoneal cavity and the creation of a peritoneal flap, with subsequent closure, typically using tacks. This method raises the potential for formation of intra-abdominal adhesions. In addition, tacks have been implicated in the development of postoperative pain. Some prefer the TEP approach, because it avoids violation of the peritoneum, and others have even used self-gripping meshes along with TEP to completely overcome some of the limitations of TAPP.5 However, regardless of surgical approach, both techniques typically use 3 laparoscopic incisions to accommodate its working ports.
Recently, patient-driven factors such as the desire for earlier return to activity, less postoperative pain, and an increasing demand in decreased incisions for improved cosmetic results have promoted interest in single-site (SS) laparoscopic surgery. The SS laparoscopic approach has been applied to various different operations with relative success.6
We sought to report the technical feasibility and short-term results of an SS-TEP approach using a self-fixating mesh or the repair of inguinal hernias.
PATIENTS AND METHODS
With institutional review board (IRB) approval, we conducted a review of a prospectively maintained database of patients who underwent SS laparoscopic TEP herniorrhaphy from August 2012 through August 2015. All patients who underwent SS laparoscopic TEP herniorrhaphy were included in the study. All procedures were performed by trained fellowship surgeons trained in minimally invasive techniques.
Patient characteristics, demographics data, and perioperative data were analyzed. Collected data included preoperative symptoms leading to the initial surgical evaluation and information regarding location or laterality of the hernia. Perioperative data included estimated blood loss, operative times, hospital length of stay, and surgical complications. Follow-up data involved office visits where pertinent data were obtained as needed. Continuous variables were summarized with mean, standard deviation, median, and IQR and categorical variables with frequency counts and percentages. Operative times of bilateral or unilateral left- or right-side procedures were compared by the Kruskal-Wallis test. The Mann-Whitney-Wilcoxon test was used to compare operative times between patients with and without surgical complications. Fisher's exact test was used to examine the associations of laterality and recurrence in laparoscopic inguinal hernia repair with surgical complications. Times to the first complication event (can be surgical or long-term) were measured from the date of operative procedure to the first event date, or censored at the end of the study, August 11, 2015, or 1 year, whichever occurred first. First complication 1-year survival times were estimated with the Kaplan-Meier method. Statistical significance was assessed at α = 0.05. Data analysis was conducted using R (R Core Team 2015, Vienna, Austria).
Operative procedure
In brief, after induction of general anesthesia, the patient is positioned supine with both arms tucked. We routinely place a Foley catheter, and a single 1.5–2-cm incision is made along a crease within the umbilicus. Dissection is carried down to the level of the anterior fascia with electrocautery, and the anterior rectus sheath is sharply incised along the horizontal axis. The rectus abdominis muscle is retracted laterally, and a small retrorectal tunnel is then created with careful blunt dissection. A TEP balloon dissector is inserted into the space of Retzius and activated under direct laparoscopic visualization, allowing visualization of the hernia and anatomic landmarks. The balloon dissector is removed and replaced with a single-incision laparoscopic surgery (SILS) 3-channel foam port (Covidien/Medtronic, New Haven, Connecticut, USA).
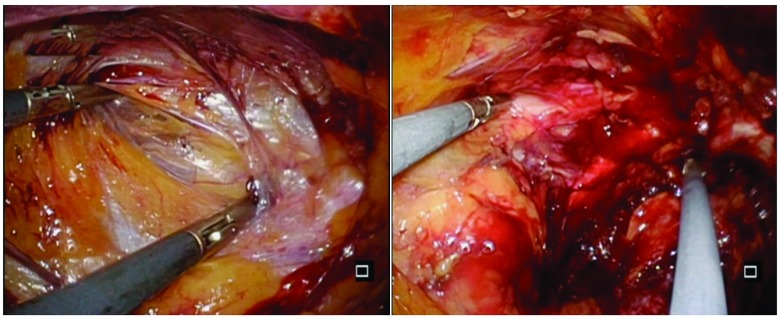
Insufflation is established at a pressure of 15 mm Hg, and, with a flexible-tip laparoscope and two 5-mm laparoscopic instruments held in criss-cross fashion (Figure 1), dissection and reduction of the inguinal hernia are performed in typical TEP fashion.
Figure 1.
Criss-cross instrument placement.
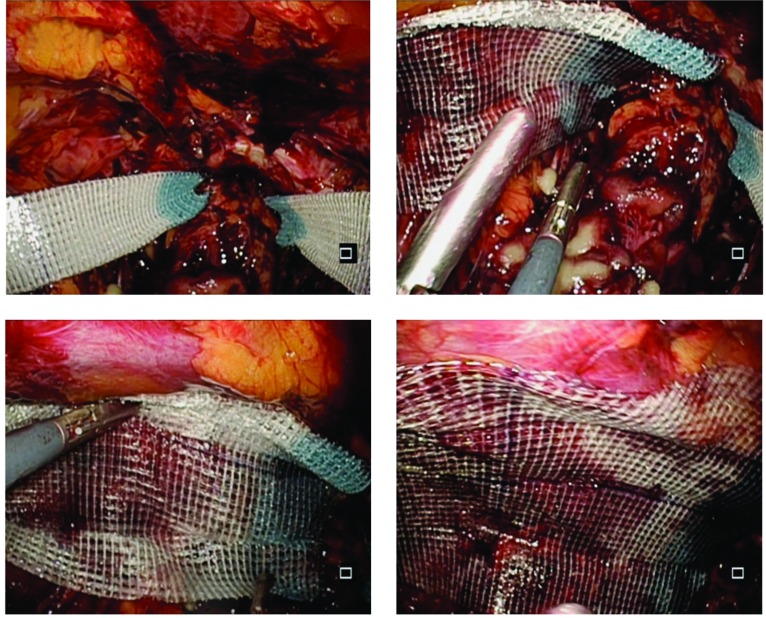
Once the hernia is completely reduced, and a satisfactory dissection has been completed a self-fixating mesh (Progrip; Covidien/Medtronic) is placed into the preperitoneal space. We typically fold the mesh in quarters (along its longitudinal axis) to facilitate placement of the mesh into a limited preperitoneal working space. The mesh is then carefully unfolded, ensuring complete coverage of the hernia defect with ample overlap (Figure 2). In the same manner as described, the contralateral groin can be explored and treated if necessary.
Figure 2.
Mesh placement.
Insufflation is then discontinued, the SILS Port is removed, and the anterior rectus sheath is closed with braided absorbable suture in figure-of-eight fashion. The single skin incision is closed with keen attention paid to cosmesis.
RESULTS
Thirty-four patients underwent SS laparoscopic hernia repair; demographic characteristics, operative details, and short-term outcomes are summarized in Table 1. Eleven patients (32.4%) underwent combination surgeries (2 femoral, 1 pantaloon, and 8 umbilical hernias). Seventeen patients (50%) underwent bilateral inguinal hernia repair, and 14 patients (41.2%) had unilateral left-side and 3 patients (8.8%) received unilateral right side hernia repair. The average operative time was 99.5 (SD = 30.5) minutes, and the median was 100 (IQR = 75–114). The average operative time for bilateral procedures was 102.12 (SD = 28.32) minutes (median = 99; IQR = 79–114. Mean time was 93.08 (SD = 33.64) minutes for left-side operations (median = 104, IQR = 70–112) and 112.00 (SD = 33.87) minutes for right-side operations (median = 123; IQR = 98.5–131). The Kruskal-Wallis test showed no significant difference in operative times for bilateral, unilateral left-side, and unilateral right-side hernia repair (Kruskal-Wallis χ2 = 0.89; df = 2; P = .64). We further combined unilateral right-side and left-side operations into a single category for analysis. The average operative time for unilateral operation was 96.6 (SD = 33.4) minutes (median = 104.5, IQR: 73–114.8). No significant differences were found in operative time between unilateral and bilateral hernia repairs (Wilcoxon's rank-sum test W = 141; P = .87).
Table 1.
Demographic Characteristics and Baseline Operative Details
| Characteristic | Total N = 34 |
|---|---|
| Age, years | |
| Mean (SD) | 55.2 (14.2) |
| Median (IQR) | 57.5 (46.2–64.8) |
| Gender, n (%) | |
| Female | 6 (17.6) |
| Male | 28 (82.4) |
| Body mass index | |
| Mean (SD) | 26.2 (3.9) |
| Median (IQR) | 26.3 (23.6–28.8) |
| Estimated blood loss (mL) | |
| Mean (SD) | 18.4 (14.1) |
| Median (IQR) | 10.0 (10.0–20.0) |
| Operative time (min) | |
| Mean (SD) | 99.5 (30.5) |
| Median (IQR) | 100.0 (75.0–114.0) |
| Missing, n (%) | 1 (2.9) |
| Laterality, n (%) | |
| Bilateral | 17 (50.0) |
| Left-side unilateral | 14 (41.2) |
| Right-side unilateral | 3 (8.8) |
| Recurrent hernia, n (%) | |
| No | 29 (85.3) |
| Yes | 5 (14.7) |
| Combined procedure, n (%) | |
| No | 23 (67.6) |
| Yes | 11 (32.4) |
| Combined procedure type, n (%) | |
| Femoral | 2 (5.9) |
| Pantaloon | 1 (2.9) |
| Umbilical | 8 (23.5) |
| Not applicable | 23 (67.6) |
| Surgical complications, n (%) | |
| No | 30 (88.2) |
| Yes | 4 (11.8) |
| Complications during postoperative follow-up, n (%) | |
| No | 30 (88.2) |
| Yes | 4 (11.8) |
| Postoperative (surgical or postoperative) complications), n (%) | |
| No | 26 (76.5) |
| Yes | 8 (23.5) |
Four patients (11.8%) had surgical complications, and urinary retention was the most common. The average operative time for procedures without surgical complications was 99.83 (SD = 29.62) minutes (median = 102, IQR = 75–114) and was 96.75 (SD = 41.76) minutes (median = 95.5, IQR = 80.8–111.5) for proceduress with surgical complications. There was no significant difference in operative time between patients with and without surgical complications (Wilcoxon's rank-sum test W = 64; P = .76).
Twenty-nine cases (85.3%) involved primary hernia and 5 were recurrent (14.7%). The average operative time for primary hernia was 99.93 (SD = 32.1) minutes (median = 99.5, IQR = 74.8–116.5) and 96.8 (SD = 22.13) minutes (median = 104; IQR = 88–105) for recurrent hernia. Wilcoxon's rank-sum test showed no significant difference in operative time between primary and recurrent hernias (W = 75; P = .82).
The association of surgical complications and laterality was examined by Fisher's exact test, and there was no evidence of an association (P = 1). We also tested the association of surgical complications and primary/recurrent hernias, and there was no significant relationship.
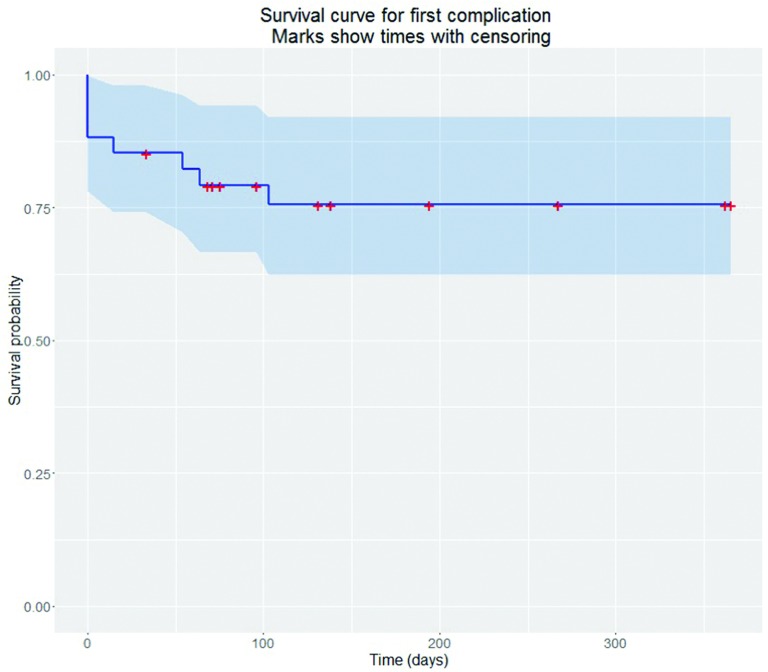
Thirty-two patients had at least 1 follow-up encounter after the operation; the median first follow-up visit was at 19 days (IQR = 18.8–22.5). One patient presented with persistent swelling, and 3 had inguinal or scrotal pain that did not require surgical intervention. The median length of follow-up was 25 days (IQR = 18.75–61.75). Complications that occurred later than 30 days included hydrocele (2 patients) and stitch abscess/wound drainage (1 patient). Two patients had 4 office visits related to pain. A total of 8 (23.5%) patients had any complication (surgical or during postoperative follow-up). The estimated Kaplan-Meier 1-year survival time to first complication event is shown in Figure 3 and Table 2. The curve was flat after 103 days, suggesting that patients no longer had complication events. No recurrences or deaths were reported.
Figure 3.
Kaplan-Meier survival curve for first complication event.
Table 2.
Kaplan-Meier Estimate for First Complication Event Within 1 Year
| Time, min | Number at Risk | Events, n | Survival | SE | Lower 95% CL | Upper 95% CL |
|---|---|---|---|---|---|---|
| 0 | 34 | 4 | 0.882 | 0.0553 | 0.78 | 0.998 |
| 15 | 30 | 1 | 0.853 | 0.0607 | 0.742 | 0.981 |
| 54 | 28 | 1 | 0.822 | 0.0658 | 0.703 | 0.962 |
| 64 | 27 | 1 | 0.792 | 0.07 | 0.666 | 0.942 |
| 103 | 22 | 1 | 0.756 | 0.0755 | 0.622 | 0.92 |
CL, confidence limits.
DISCUSSION
The 2 recognized types of laparoscopic approaches for inguinal hernia repair approaches are totally extraperitoneal preperitoneal (TEPP) and transabdominal preperitoneal (TAPP). Both have their advantages and disadvantages. Totally extraperitoneal (TEP) repairs have been shown to have a lower incidence of port-site incisional hernias or bowel-related complications and are associated with less pain and greater patient satisfaction.7 TEP is considered a technically difficult procedure to learn, with a more demanding learning curve because of the unfamiliar visualization of the inguinal anatomy; however, it is advantageous because it allows direct access to the myopectineal orifice without entering the abdominal cavity and disrupting the peritoneum.8
During laparoscopic inguinal hernia repair, mesh fixation is traditionally performed, to minimize displacement of the prosthesis as a preventive measure to reduce recurrence. This fixation when performed with staples or tacks has been associated with the development of chronic inguinal pain. Kaul et al9 found no difference in inguinal hernia recurrence when reviewing 662 procedures and comparing fixation methods including staple/tack versus fibrin glue during laparoscopic TEP inguinal hernia repair. The incidence of chronic inguinal pain was significantly increased in the staple/tack fixation group (n = 394 vs 268 in the fibrin glue group). Operative time, seroma formation, hospital stay, or time to return to normal activities showed no differences between the 2 groups.9 Antoniuo et al10 reported an increased likelihood of postoperative pain beyond 3 months with the use of penetrating mesh fixation techniques when compared with bioglue fixation. We acknowledge that chronic pain is a multifactorial problem in which multiple variables, such as operative technique, nerve injury, degree of mesh innervation11 and mechanisms of fixation16, have been implicated.
The characteristics of the mesh used for prosthetic reinforcement have evolved over the past 15 years, as well as the methods and techniques for their fixation, ranging from simple stitching to various stapling or tacking systems. Newer methods include mesh materials with self-adhering or self-gripping properties that have been designed to appose to tissue with monofilament polylactic acid (PLA) technology that creates a microgrip system providing self-adherence to the adjacent tissue, potentially reducing the risk of the chronic pain associated with suture or tack fixation. Decreased postoperative pain during the early recovery period has been reported during tension-free Lichtenstein repair with this self-fixating mesh.12 Zhang et al13 reviewed the differences between self-gripping mesh and sutured mesh in open inguinal repair. There were no differences in chronic pain, recurrence, wound infection, hematoma, or seroma formation between 2 groups; however the mean operative time was shorter in the self-adhering mesh.
The self-gripping mesh has been criticized for its potential to adhere to itself, consequently increasing handling and placement difficulties. We typically fold the mesh in quarters along the longitudinal axis. The mesh is held by the corners with a blunt grasper and is introduced through the 10-mm trocar aiming laterally. The remainder of the mesh is subsequently pushed with graspers into the preperitoneal space. As this is a small space, we find it easiest to move the mesh while it is still folded in half. Grasping the folded edge allows us to position the medial aspect overlying Cooper's ligament and the defect. Medially, the mesh is unfolded upward first and secured to Cooper's ligament. We then unfurl the first quarter of the mesh and proceed to unfurl it completely.
The TEP approach avoids violation of the peritoneum, thus decreasing intra-abdominal adhesions. Also no repair of the peritoneal layer is needed, therefore minimizing chances of bowel obstruction with defects in the repaired peritoneum. The TEP technique is an ideal foundation for an SS approach, because there is no risk of future incisional hernias, and the SS approach maintains all working instruments well away from the hernia defect and minimizes encroachment on the already small working space. Disadvantages include limited laparoscopic working space in TEP. Also, once the mesh is introduced, the trocars and other instruments can block the surgeon's view.
The average operative time for bilateral hernias was 102.12 minutes (SD = 28.32), and 96.63 minutes (SD = 33.41) for unilateral repairs. In a meta-analysis, Siddiqui et al14 reported that unilateral repair took a little less than 100 minutes (range, 40–98), whereas bilateral repairs were reported to take up to 2 hours (range, 41–121 minutes). Our operative times are similar to those reported in the literature confirming no prolonged operative time with our newly devised technique. All our procedures were same-day procedures, and no hospital admission was necessary. Other studies reported a hospital stay of <1 day to 2.15 days.14
In our study, there were no conversions and no intraoperative complications. Intraoperative complications involving bleeding or a peritoneal tear have been reported.14 The most common short-term postoperative complication was urinary retention—in particular, failure to void (4 patients; 11.7%). None of our patients required Foley catheter reinsertion. Other studies reported a 3.2% to 22% incidence of urinary retention.5,15 Risk factors associated with this complication include narcotics use and age >50. Another study reported only minor complications: epididymitis, wound infection, dehiscence, ileus, and seromas or hematomas in laparoendoscopic single-site (LESS) TEP.14
Follow-up ranged from 2 weeks to 14 months. Patients reported only minimal discomfort or ache. We did not record narcotic use or pain scores on a comfort scale to assess pain and quality of life. Bresnahan et al5 reported 4.8% symptomatic pain at the first postoperative visit and no symptomatic pain at 14.8 months' mean follow-up. The SS-TEP technique is very safe and efficacious when compared to outcomes in published reports.
Our results are similar to previously reported data in regard to technical aspects and outcomes of traditional laparoscopic inguinal hernia repair and demonstrate the equivalence of the SS-TEP approach. The SS approach is not difficult, does not prolong operative time, and does not incur complications and recurrences in the short term. Self-fixating mesh can be used with SS-TEP. We believe that SS-TEP affords some key benefits over the traditional TEP approach.
CONCLUSIONS
The duration of surgery for unilateral and bilateral repairs was comparable with other reports. There were no conversions. There were no deaths or recurrences. Postoperative recovery was largely uneventful, and very few complications were noted.
With comparable operative times, perioperative outcomes, and patient results, SS-TEP appears to be a safe and effective surgical approach for the management of inguinal hernias. Furthermore, we describe the feasibility of the SS-TEP approach with a self-fixating mesh, and we believe that it may have technical benefits with regard to mesh placement and intraoperative deployment of instruments.
Contributor Information
Alfredo D. Guerron, Department of General Surgery, Duke University Health System, Durham, North Carolina..
Hui-Jie Lee, Department of Biostatistics and Bioinformatics, Duke University Medical Center, Durham, North Carolina..
Jin Yoo, Department of General Surgery, Duke University Health System, Durham, North Carolina..
Keri Seymour, Department of General Surgery, Duke University Health System, Durham, North Carolina..
Ranjan Sudan, Department of General Surgery, Duke University Health System, Durham, North Carolina..
Dana Portenier, Department of General Surgery, Duke University Health System, Durham, North Carolina..
Chan Park, Department of General Surgery, Duke University Health System, Durham, North Carolina..
References:
- 1. Kingsnorth A, LeBlanc K. Hernias: inguinal and incisional. Lancet. 2003;362:1561–1571. [DOI] [PubMed] [Google Scholar]
- 2. Rutkow IM. Demographic and socioeconomic aspects of hernia repair in the United States in 2003. Surg Clin North Am. 2003;83:1045–1051, v–vi. [DOI] [PubMed] [Google Scholar]
- 3. Corbitt JD., Jr Laparoscopic herniorrhaphy. Surg Laparosc Endosc. 1991;1:23–25. [PubMed] [Google Scholar]
- 4. Zendejas B, Ramirez T, Jones T, et al. Trends in the utilization of inguinal hernia repair techniques: a population-based study. Am J Surg. 2012;203:313–317; discussion 317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bresnahan E, Bates A, Wu A, Reiner M, Jacob Bl. The use of self-gripping (Progrip) mesh during laparoscopic total extraperitoneal (TEP) inguinal hernia repair: a prospective feasibility and long-term outcomes study (published correction in Surg Endosc. 2015;29:2697). Surg Endosc. 2015;29:2690–2696. [DOI] [PubMed] [Google Scholar]
- 6. Romanelli JR, Roshek TB, 3rd, Lynn DC, Earle DB. Single-port laparoscopic cholecystectomy: initial experience. Surg Endosc. 2010;24:1374–1379. [DOI] [PubMed] [Google Scholar]
- 7. Krishna A, Misra MC, Bansal VK, Kumar S, Rajeshwari S, Chabra A. Laparoscopic inguinal hernia repair: transabdominal preperitoneal (TAPP) versus totally extraperitoneal (TEP) approach: a prospective randomized controlled trial. Surg Endosc. 2012;26:639–649. [DOI] [PubMed] [Google Scholar]
- 8. Misra MC, Bansal VK, Kumar S, Prashant B, Bhattacharjee HK. Total extra-peritoneal repair of groin hernia: prospective evaluation at a tertiary care center. Hernia 2008;12:65–71. [DOI] [PubMed] [Google Scholar]
- 9. Kaul A, Hutfless S, Le H, et al. Staple versus fibrin glue fixation in laparoscopic total extraperitoneal repair of inguinal hernia: a systematic review and meta-analysis. Surg Endosc. 2012;26:1269–1278. [DOI] [PubMed] [Google Scholar]
- 10. Antoniou SA, Köhler G, Antoniou GA, Muysoms FE, Pointner R, Granderath FA. Meta-analysis of randomized trials comparing nonpenetrating vs mechanical mesh fixation in laparoscopic inguinal hernia repair. Am J Surg. 2016;211:239–249-e2. [DOI] [PubMed] [Google Scholar]
- 11. Bendavid R, Lou W, Grischkan D. A mechanism of mesh-related post-herniorrhaphy neuralgia. Hernia.2016;20:357–365. [DOI] [PubMed] [Google Scholar]
- 12. Kosai N, Sutton PA, Evans J, Varghese J. Laparoscopic preperitoneal mesh repair using a novel self-adhesive mesh. J Minim Access Surg. 2011;7:192–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Zhang C, Li F, Zhang H, Zhong W, Shi D, Zhao Y. Self-gripping versus sutured mesh for inguinal hernia repair: a systematic review and meta-analysis of current literature. J Surg Res. 2013;185:653–660. [DOI] [PubMed] [Google Scholar]
- 14. Siddiqui MR, Kovzel M, Brennan SJ, Priest OH, Preston SR, Soon Y. The role of the laparoendoscopic single site totally extraperitoneal approach to inguinal hernia repairs: a review and meta-analysis of the literature. Can J Surg, 2014;57:116–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Koch CA, Grinberg GG, Farley DR. Incidence and risk factors for urinary retention after endoscopic hernia repair. Am J Surg, 2006;191:381–385. [DOI] [PubMed] [Google Scholar]
- 16. Andresen K, Fenger AQ, Burcharth J, Pommergaard HC, Rosenberg J. Mesh fixation methods and chronic pain after transabdominal preperitoneal (TAPP) inguinal hernia surgery: a comparison between fibrin sealant and tacks. Surg Endosc. 2017. February 23 doi: 10.1007/s00464-017-5454-8. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]