Abstract
Abnormal anterior translation of the femur on the tibia has been observed in mid flexion (20–60°) following posterior stabilized total knee arthroplasty. The underlying biomechanical causes of this abnormal motion remain unknown. The purpose of this study was to isolate the effects of posterior cruciate ligament removal on knee motion after total knee arthroplasty. We posed two questions: Does removing the posterior cruciate ligament introduce abnormal anterior femoral translation? Does implanting a posterior stabilized prosthesis change the kinematics from the cruciate deficient case? Using a navigation system, we measured passive knee kinematics of ten male osteoarthritic patients during surgery after initial exposure, after removing the anterior cruciate ligament, after removing the posterior cruciate ligament, and after implanting the prosthesis. Passively flexing and extending the knee, we calculated anterior femoral translation and the flexion angle at which femoral rollback began. Removing the posterior cruciate ligament doubled anterior translation (from 5.1±4.3 mm to 10.4±5.1 mm) and increased the flexion angle at which femoral rollback began (from 31.2±9.6° to 49.3±7.3°). Implanting the prosthesis increased the amount of anterior translation (to 16.1±4.4 mm), and did not change the flexion angle at which femoral rollback began. Abnormal anterior translation was observed in low and mid flexion (0–60°) after removing the posterior cruciate ligament, and normal motion was not restored by the posterior stabilized prosthesis.
Keywords: surgical navigation, total knee replacement, biomechanics, kinematics
Posterior stabilized (PS) total knee prostheses are designed to stabilize anterior–posterior (AP) knee motion by mechanical interaction between the tibial post and the femoral cam after removal of the posterior cruciate ligament (PCL).1 The PCL resists anterior femoral translation,2 particularly between 30 and 90° of knee flexion.3 The cam–post interaction is designed to engage near 75° of flexion4 to prevent anterior femoral translation and produce femoral rollback in deeper flexion, mimicking the normal motion of the knee.1,5 Femoral rollback increases quadriceps moment arm6 and increases range of motion by increasing the flexion angle at which the femur impinges on the posterior tibial plateau.7–11
Measurements of knee motions in total knee arthroplasty (TKA) patients and cadavers have revealed abnormal knee kinematics after PS knee arthroplasty. In particular, researchers have observed greater than normal anterior femoral translation in mid flexion (20–60°) during stair climbing,12–14 deep knee bend,5 the stance phase of gait,15 and under passive motion.16 Anterior translation of the medial femoral condyle was observed at 30 and 60° of knee flexion under passive motion and simulated muscle loads in cadaver studies.17 This abnormal translation implies sliding, which could accelerate prosthesis wear.18,19 An anterior position of the femur on the tibia may also decrease the moment arms of the knee extensors.6,12,20
In other studies, however, no anterior translation was observed in PS knees during quasi-static deep knee bend,21,22 stepup,23 and kneeling24 in patients, or with simulated muscle loads in cadaver studies.25 Simulations of a stepup activity with a PS knee26 predicted larger translations than were observed for stepup tasks in vivo.23
The kinematics following TKA are variable and are influenced by several factors,27 including muscle and external forces,12 prosthesis type (cruciate retaining or PS),14,15 prosthesis design (placement of the cam and post,28 tilt or slope of the tibial component,4,29 contour of the polyethylene insert30), and surgical variables, such as ligament release31 and restoration of the joint line.32 The contributions of individual factors to knee kinematics are difficult to measure postoperatively, and factors leading to the observed abnormal anterior femoral translation may be significant in some locomotor tasks and not in others.
One possible cause of anterior femoral translation in low to mid flexion is removal of the PCL. The purpose of this study was to examine the effects of PCL removal on the passive kinematics of the knee after implantation of a PS prosthesis. We addressed two questions: does PCL removal introduce abnormal anterior translation of the femur? Does PS prosthesis implantation change the kinematics from the cruciate deficient case? We answered these questions by measuring knee kinematics throughout the range of flexion and extension during TKA. From these measurements we calculated anterior femoral translation and the knee flexion angle at which femoral rollback began. Recording kinematics during surgery allowed us to make paired comparisons between the cruciate ligament deficient knee and both the osteoarthritic knee prior to ligament removal and the knee after prosthesis implantation in each subject. A single implant design was used throughout the study, and was installed with consistent technique by the same surgeon. We measured kinematics without large muscle or external forces, allowing us to isolate the effects of PCL removal on passive knee motions.
MATERIALS AND METHODS
Knee kinematics were measured in 10 male subjects during primary TKA for osteoarthritis. Pilot data indicated that nine subjects were required to detect a difference in anterior translation of 3.5 mm with a power of 0.8. Institutional review boards at Stanford University and Veterans Affairs Palo Alto Health Care System approved the protocol, and subjects gave informed consent.
A custom-built surgical navigation system was used to record knee kinematics during surgery16 (Fig. 1). The tourniquet was inflated with the subject’s knee maximally flexed. After the initial surgical exposure through a medial parapatellar approach, infrared reflective trackers (Traxtal Inc, Toronto, Ontario) were affixed directly to the femur and tibia. The position and orientation of the trackers were recorded by an optical tracking system (Polaris, Northern Digital, Waterloo, Ontario). Using an infrared reflective stylus, the surgeon digitized anatomic landmarks to establish the transformations for the anatomic femur and tibia reference frames relative to the femoral and tibial trackers. The origin of the femur reference frame was the anterolateral edge of the PCL attachment. The origin of the tibia reference frame was the center of the anterior cruciate ligament (ACL) attachment. The anterior tibial axis was the cross product of the vector containing the most lateral and medial points on the tibial plateau with the vector containing the midpoint of the lateral and medial malleoli and the origin. The anterior direction was defined to be positive. Diagrams and details of the anatomic reference frame conventions16 were published previously.
Figure 1.
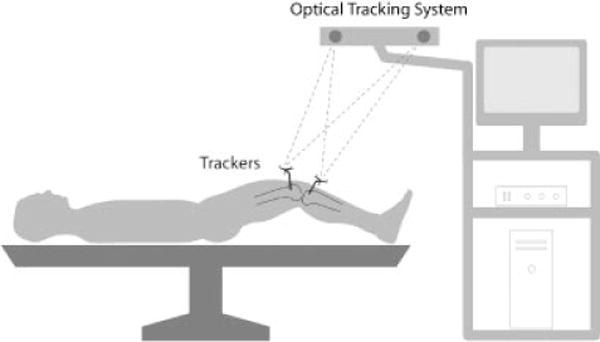
Intraoperative experimental setup. An optical tracking system recorded knee motions using the positions and orientations of trackers affixed to the femur and tibia. At four surgical stages, knee motions were recorded as the surgeon moved the knee through its range of flexion and extension. (see methods for details)
Knee kinematics were recorded at four surgical stages. The first stage was after initial surgical exposure but before cruciate ligament removal (Intact). Next, the surgeon sequentially removed the ACL and then the PCL, and recorded the kinematics after each ligament removal (No ACL, No ACL No PCL). The order of cruciate ligament removal was not randomized. The surgery progressed normally, using conventional instrumentation supplied by the manufacturer to implant the prosthesis and restore the joint line. Kinematics were recorded a final time after cementing the prosthesis (TKA). A NexGen Legacy PS Knee (Zimmer Inc., Warsaw, IN) was used in each case. No releases of the lateral or medial collateral ligaments were performed.
At each surgical stage, knee motions were recorded as the surgeon moved the knee through a range of flexion and extension three times.16 The subject was supine on the operating table, and the patella was reduced in the trochlear groove. To reach maximum extension, the subject’s leg was supported at the heel by the surgeon’s open palm. To flex the knee, the surgeon used his other hand to raise the subject’s thigh, while still supporting the heel with an open palm, flexing both the knee and the hip. To reach maximum knee flexion, the foot was released once the hip was flexed beyond 90°. Gravity pulled the knee into deeper flexion. To extend the knee, the surgeon supported the subject’s heel with an open palm while the thigh was slowly lowered, extending both the knee and the hip.
During this motion, the optical tracking system recorded the positions and orientations of the femoral tracker with respect to the tibial tracker at 30 Hz. From these data and the femur and tibia reference frames, we calculated the knee flexion angle33 and anterior position of the femur16 over the range of flexion and extension. Knee flexion angle was calculated according to Grood and Suntay.33 The anterior position of the femur was defined by the projection of the origin of the femur frame onto the anterior axis of the tibia. A fifth order polynomial was fit to each of the plots of anterior position of the femur versus flexion (Fig. 2). The mean root-mean-square (RMS) error between the polynomials and the experimental data was 0.81 mm over all subjects. From the polynomials, we calculated the anterior translation of the femur, which was defined as the difference between the anterior position at maximum extension, and the most anterior position (Fig. 3, arrow). We also calculated the knee flexion angle at which the most anterior position occurred; this was considered to be the knee flexion angle at which femoral rollback began.
Figure 2.
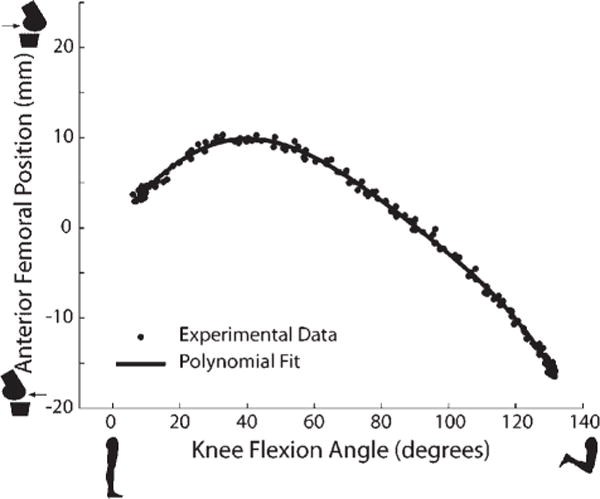
Anterior femoral position throughout the range of knee flexion for one subject after removal of the ACL and PCL. Experimental data represent three trials of flexion extension. Data were fit with a fifth-order polynomial.
Figure 3.
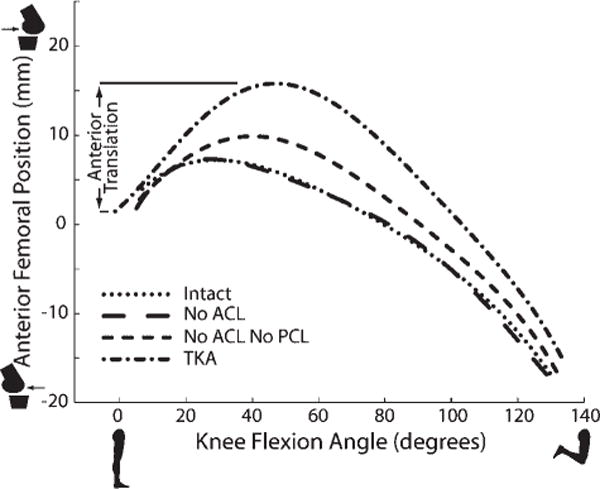
Anterior femoral position throughout the range of knee flexion for one subject at the four surgical stages (Intact, No ACL, No ACL No PCL, TKA. Arrow indicates anterior femoral translation.
Differences in anterior femoral translation among the four surgical stages were identified using repeated-measures analysis of variance. Surgical stages were compared with paired student’s t-tests with Bonferroni correction for multiple comparisons. We made three comparisons to investigate the role of PCL removal. Comparing the Intact and No ACL stages showed the contribution of removing the ACL. Comparing the Intact and No ACL No PCL stages showed the contribution of removing the PCL. Comparing the No ACL No PCL and TKA stages showed the contribution of prosthesis implantation. Differences in flexion angle at initiation of femoral rollback were identified using the same tests.
RESULTS
Removing the PCL introduced abnormal anterior femoral translation, doubling the amount compared to the intact knee (p < 0.001, Fig. 4 Intact vs. No ACL No PCL). PCL removal also caused femoral rollback to begin at a deeper flexion angle, 49.3±7.3° (p < 0.001, Fig. 5 Intact vs. No ACL No PCL). Removing the ACL did not change anterior translation (p = 0.21, Fig. 4 Intact vs. No ACL), nor did it change the flexion angle at which femoral rollback began (p = 0.54, Fig. 5 Intact vs. No ACL).
Figure 4.
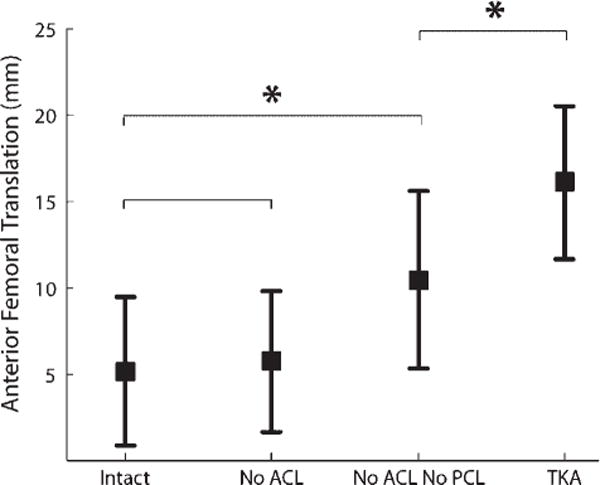
Anterior femoral translation at the four surgical stages (mean±SD). The mean anterior femoral translation significantly increased with PCL removal (No ACL No PCL) and with prosthesis implantation (TKA). *p < 0.05.
Figure 5.
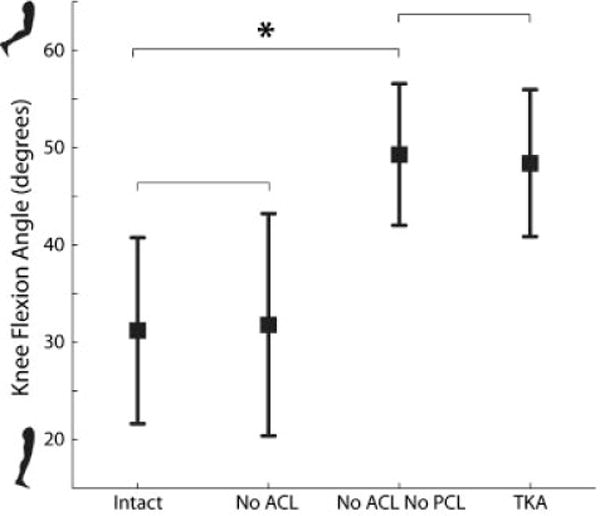
Knee flexion angle at which femoral rollback began at the four surgical stages (mean±SD). Femoral rollback angle occurred in deeper flexion after removal of the PCL (No ACL No PCL). Normal femoral rollback angle was not restored with the prosthesis (TKA). *p < 0.05.
Implanting the PS total knee prosthesis changed the kinematics from the cruciate deficient stage. Implanting the prosthesis further increased anterior translation (p = 0.01, Fig. 4 No ACL No PCL vs. TKA). The mean anterior translation after prosthesis implantation (16.1 mm) was three times that of the intact knee. We did not detect a difference in the flexion angle at which femoral rollback began (p = 0.74, Fig. 5 No ACL No PCL vs. TKA).
DISCUSSION
Several studies have reported abnormal anterior translation of the femur on the tibia in mid flexion (20–60°) after PS TKA.5,12–16 This abnormal anterior translation may reduce the quadriceps moment arm and increase wear of polyethylene inserts. We investigated a possible cause of this anterior translation: removal of the PCL. Measurements of passive knee kinematics throughout the range of flexion and extension during TKA revealed that abnormal anterior translation of the femur throughout low and mid flexion was introduced immediately after removal of the PCL, and that normal motion was not restored by implantation of a PS prosthesis.
The changes in anterior femoral translation between stages must be interpreted in terms of our experimental protocol and the orientations of the ligaments. At full extension, the lower extremity was horizontal and was supported at the thigh and heel16,34 such that the weight of the tibia caused a posteriorly directed force on the tibia that would move the femur anterior relative to the tibia. As the knee flexed, the tibia rotated toward vertical, decreasing the force component in the posterior tibial direction. This differs from passive loading conditions used in robotic cadaver studies,17,25 in which the passive path was defined by zero forces and moments applied to the joint.35 In the Intact stage, our results are consistent with previous results,16 which showed that the AP motion of osteoarthritic knees during TKA was not significantly different from the motion of normal cadaver knees during a similar passive motion. After ACL removal, the anterior femoral position throughout flexion of each knee was indistinguishable from the Intact stage (Fig. 3), despite the body of literature describing kinematic changes in ACL deficient knees during various functional activities.36,37 The ACL is positioned to resist anterior tibial loads, particularly in low flexion (0–30°).38,39 The posterior directed weight of the tibia that occurred in our protocol likely unloaded the ACL. After removing the PCL, anterior femoral translation increased. The PCL is positioned to resist posterior tibial loads (anterior femoral loads), particularly from 30 to.2,39,40 When the ACL is absent, PCL function may be altered. Because ACL removal caused no detectable changes to passive kinematics measured in our experiments, we considered the changes to PCL function negligible. Thus, the changes between the intact stage and the cruciate deficient stage were considered to result primarily from PCL removal. After the PS prosthesis was implanted, anterior femoral translation began at full extension and continued into mid flexion (Fig. 3, arrow), consistent with previous results using the same implant and same experimental protocol.16
In the initiation angle of femoral rollback, we detected no difference between the cruciate deficient stage and postimplantation stage (Fig. 5, No ACL No PCL vs. TKA). In the cruciate deficient stage (No ACL No PCL), femoral rollback is initiated by the geometry of the articulating surfaces and by the remaining soft tissue structures of the knee, including the medial and lateral collateral ligaments, posterior capsule, and hamstrings. These same mechanisms may be initiating femoral rollback during passive motion after implantation of the PS prosthesis. We did not measure cam–post engagement directly, but noted that after prosthesis implantation, femoral rollback began on average at 48° flexion (Fig. 5). This is below the expected flexion angle of cam–post engagement. The cam–post mechanism in this PS prosthesis was reported to engage between 60 and 90° of flexion17 or between 80 and 90° of flexion.25 A model of the Insall-Burstein PS prosthesis, a precursor to the NexGen prosthesis, predicted that the cam–post mechanism would engage at 75° of flexion.4 The weight of the tibia created a small posterior tibial load, which may have caused the cam–post mechanism to engage at a lower flexion angle.
Our study has several limitations. We used a single implant design, and therefore could not test for differences between implants. Other implants designed to limit anterior translation in low flexion could yield different results.6 Only one surgeon participated in the study; thus, we could not test for differences arising from individual surgical technique. Cruciate ligament removal was not randomized; in all 10 subjects, the surgeon removed the ACL first, and then the PCL. The ACL is not positioned to resist anterior translation of the femur,39,41 which was the effect under investigation. Because the anterior attachment of the meniscus was detached as part of the surgical approach, meniscal stabilization of AP motion may have been altered. All data were collected with the lower extremity under tourniquet pressure, which may have altered knee kinematics. Implantation of the prosthesis offsets the relative positions of the origins of the femur and tibia reference frames, which was analyzed in detail previously.16 This offset has minimal effect results because we measured the anterior femoral translation, which subtracts this offset.
Intraoperative measurements present both advantages and limitations. Intraoperative measurement allowed us to rigidly affix trackers to the femur and tibia, which eliminated measurement errors due to soft tissue motion and allowed accurate tracking of bone motion. Intraoperative measurements also allowed direct comparisons of knee motions before and after cruciate ligament removal, and after prosthesis implantation. Using trackers fixed to the bones allowed consistent comparison of flexion angles even with altered geometry following implantation of the prosthesis. However, intraoperative measurements are inherently limited to studying passive motions. Studying passive kinematics allowed us to separate the effects of implant geometry and passive structures from the effects of large muscle forces and large external loads that occur during locomotion and other activities. Although knee kinematics during walking are likely different from passive kinematics, the observation of anterior femoral translation in both passive16 and active5,12–15 motions implies that joint geometry and passive structures, such as the PCL, influence AP motion. Future work is needed to link passive kinematics recorded during surgery to loaded kinematics measured after surgery.
PCL retaining prostheses have also demonstrated abnormal anterior translation of the femur. Anterior femoral translation was observed in mid flexion in patients with cruciate retaining prostheses during stepups and stair climbing8,13,42 and deep knee bends21,43 In studies that directly compared cruciate retaining and PS designs, the knees with cruciate retaining prostheses sometimes showed greater anterior femoral translation and/or greater kinematic variability.8,13,21,44 The PCL may be unable to resist anterior femoral translation in low and mid flexion in a PCL retaining prosthesis if the PCL is not tensioned properly or if the collateral ligaments are not properly balanced. These findings highlight the complexity of the interaction between soft tissues, implant design, surgical technique, and muscle coordination in determining postoperative kinematics. A challenge for the future is to develop new implant designs and surgical techniques to better control anterior femoral translation in low and mid flexion.
Acknowledgments
Support was received from an NDSEG Fellowship and from the Powell Foundation.
References
- 1.Insall JN, Lachiewicz PF, Burstein AH. The posterior stabilized condylar prosthesis: a modification of the total condylar design. Two to four-year clinical experience. J Bone Joint Surg Am. 1982;64:1317–1323. [PubMed] [Google Scholar]
- 2.Papannagari R, DeFrate LE, Nha KW, et al. Function of posterior cruciate ligament bundles during in vivo knee flexion. Am J Sports Med. 2007;35:1507–1512. doi: 10.1177/0363546507300061. [DOI] [PubMed] [Google Scholar]
- 3.Li G, Most E, DeFrate LE, et al. Effect of the posterior cruciate ligament on posterior stability of the knee in high flexion. J Biomech. 2004;37:779–783. doi: 10.1016/j.jbiomech.2003.09.031. [DOI] [PubMed] [Google Scholar]
- 4.Piazza SJ, Delp SL, Stulberg SD, et al. Posterior tilting of the tibial component decreases femoral rollback in posterior-substituting knee replacement: a computer simulation study. J Orthop Res. 1998;16:264–270. doi: 10.1002/jor.1100160214. [DOI] [PubMed] [Google Scholar]
- 5.Dennis DA, Komistek RD, Colwell CE, Jr, et al. In vivo anteroposterior femorotibial translation of total knee arthroplasty: a multicenter analysis. Clin Orthop Relat Res. 1998;346:47–57. doi: 10.1097/00003086-199811000-00009. [DOI] [PubMed] [Google Scholar]
- 6.Draganich LF, Piotrowski GA, Martell J, et al. The effects of early rollback in total knee arthroplasty on stair stepping. J Arthroplasty. 2002;17:723–730. doi: 10.1054/arth.2002.33558. [DOI] [PubMed] [Google Scholar]
- 7.Banks S, Bellemans J, Nozaki H, et al. Knee motions during maximum flexion in fixed and mobile-bearing arthroplasties. Clin Orthop Relat Res. 2003;410:131–138. doi: 10.1097/01.blo.0000063121.39522.19. [DOI] [PubMed] [Google Scholar]
- 8.Victor J, Banks S, Bellemans J. Kinematics of posterior cruciate ligament-retaining and -substituting total knee arthroplasty: a prospective randomised outcome study. J Bone Joint Surg Br. 2005;87:646–655. doi: 10.1302/0301-620X.87B5.15602. [DOI] [PubMed] [Google Scholar]
- 9.Massin P, Gournay A. Optimization of the posterior condylar offset, tibial slope, and condylar roll-back in total knee arthroplasty. J Arthroplasty. 2006;21:889–896. doi: 10.1016/j.arth.2005.10.019. [DOI] [PubMed] [Google Scholar]
- 10.Dennis DA, Komistek RD, Stiehl JB, et al. Range of motion after total knee arthroplasty: the effect of implant design and weight-bearing conditions. J Arthroplasty. 1998;13:748–752. doi: 10.1016/s0883-5403(98)90025-0. [DOI] [PubMed] [Google Scholar]
- 11.Bellemans J, Banks S, Victor J, et al. Fluoroscopic analysis of the kinematics of deep flexion in total knee arthroplasty. Influence of posterior condylar offset. J Bone Joint Surg Br. 2002;84:50–53. doi: 10.1302/0301-620x.84b1.12432. [DOI] [PubMed] [Google Scholar]
- 12.Andriacchi TP, Dyrby CO, Johnson TS. The use of functional analysis in evaluating knee kinematics. Clin Orthop Relat Res. 2003;410:44–53. doi: 10.1097/01.blo.0000062383.79828.f5. [DOI] [PubMed] [Google Scholar]
- 13.Uvehammer J, Karrholm J, Brandsson S. In vivo kinematics of total knee arthroplasty. Concave versus posterior-stabilised tibial joint surface. J Bone Joint Surg Br. 2000;82:499–505. doi: 10.1302/0301-620x.82b4.10651. [DOI] [PubMed] [Google Scholar]
- 14.Banks SA, Hodge WA. Implant design affects knee arthroplasty kinematics during stair-stepping. Clin Orthop Relat Res. 2004;426:187–193. doi: 10.1097/01.blo.0000138956.04316.ac. [DOI] [PubMed] [Google Scholar]
- 15.Dennis DA, Komistek RD, Mahfouz MR, et al. Multi-center determination of in vivo kinematics after total knee arthroplasty. Clin Orthop Relat Res. 2003;416:37–57. doi: 10.1097/01.blo.0000092986.12414.b5. [DOI] [PubMed] [Google Scholar]
- 16.Siston RA, Giori NJ, Goodman SB, et al. Intraoperative passive kinematics of osteoarthritic knees before and after total knee arthroplasty. J Orthop Res. 2006;24:1607–1614. doi: 10.1002/jor.20163. [DOI] [PubMed] [Google Scholar]
- 17.Li G, Most E, Otterberg E, et al. Biomechanics of posterior-substituting total knee arthroplasty: an in vitro study. Clin Orthop Relat Res. 2002;404:214–225. doi: 10.1097/00003086-200211000-00035. [DOI] [PubMed] [Google Scholar]
- 18.Blunn GW, Walker PS, Joshi A, et al. The dominance of cyclic sliding in producing wear in total knee replacements. Clin Orthop Relat Res. 1991;273:253–260. [PubMed] [Google Scholar]
- 19.Harman MK, Banks SA, Hodge WA. Polyethylene damage and knee kinematics after total knee arthroplasty. Clin Orthop Relat Res. 2001;392:383–393. doi: 10.1097/00003086-200111000-00050. [DOI] [PubMed] [Google Scholar]
- 20.D’Lima DD, Poole C, Chadha H, et al. Quadriceps moment arm and quadriceps forces after total knee arthroplasty. Clin Orthop Relat Res. 2001;392:213–220. doi: 10.1097/00003086-200111000-00026. [DOI] [PubMed] [Google Scholar]
- 21.Yoshiya S, Matsui N, Komistek RD, et al. In vivo kinematic comparison of posterior cruciate-retaining and posterior stabilized total knee arthroplasties under passive and weight-bearing conditions. J Arthroplasty. 2005;20:777–783. doi: 10.1016/j.arth.2004.11.012. [DOI] [PubMed] [Google Scholar]
- 22.Ranawat CS, Komistek RD, Rodriguez JA, et al. In vivo kinematics for fixed and mobile-bearing posterior stabilized knee prostheses. Clin Orthop Relat Res. 2004;418:184–190. doi: 10.1097/00003086-200401000-00030. [DOI] [PubMed] [Google Scholar]
- 23.Banks SA, Markovich GD, Hodge WA. In vivo kinematics of cruciate-retaining and -substituting knee arthroplasties. J Arthroplasty. 1997;12:297–304. doi: 10.1016/s0883-5403(97)90026-7. [DOI] [PubMed] [Google Scholar]
- 24.Incavo SJ, Mullins ER, Coughlin KM, et al. Tibiofemoral kinematic analysis of kneeling after total knee arthroplasty. J Arthroplasty. 2004;19:906–910. doi: 10.1016/j.arth.2004.03.020. [DOI] [PubMed] [Google Scholar]
- 25.Li G, Most E, Sultan PG, et al. Knee kinematics with a high-flexion posterior stabilized total knee prosthesis: an in vitro robotic experimental investigation. J Bone Joint Surg Am. 2004;86-A:1721–1729. doi: 10.2106/00004623-200408000-00017. [DOI] [PubMed] [Google Scholar]
- 26.Piazza SJ, Delp SL. Three-dimensional dynamic simulation of total knee replacement motion during a step-up task. J Biomech Eng. 2001;123:599–606. doi: 10.1115/1.1406950. [DOI] [PubMed] [Google Scholar]
- 27.Dennis DA, Komistek RD, Scuderi GR, et al. Factors affecting flexion after total knee arthroplasty. Clin Orthop Relat Res. 2007 doi: 10.1097/BLO.0b013e31812f785d. [DOI] [PubMed] [Google Scholar]
- 28.Delp SL, Kocmond JH, Stern SH. Tradeoffs between motion and stability in posterior substituting knee arthroplasty design. J Biomech. 1995;28:1155–1166. doi: 10.1016/0021-9290(94)00172-z. [DOI] [PubMed] [Google Scholar]
- 29.Bellemans J, Robijns F, Duerinckx J, et al. The influence of tibial slope on maximal flexion after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2005;13:193–196. doi: 10.1007/s00167-004-0557-x. [DOI] [PubMed] [Google Scholar]
- 30.Matsuda S, Whiteside LA, White SE, et al. Knee kinematics of posterior cruciate ligament sacrificed total knee arthroplasty. Clin Orthop Relat Res. 1997;341:257–266. [PubMed] [Google Scholar]
- 31.Saragaglia D, Chaussard C, Rubens-Duval B. Navigation as a predictor of soft tissue release during 90 cases of computer-assisted total knee arthroplasty. Orthopedics. 2006;29:S137–S138. [PubMed] [Google Scholar]
- 32.Mountney J, Karamfiles R, Breidahl W, et al. The position of the joint line in relation to the trans-epicondylar axis of the knee complementary radiologic and computer-based studies. J Arthroplasty. 2007;22:1201–1207. doi: 10.1016/j.arth.2006.11.023. [DOI] [PubMed] [Google Scholar]
- 33.Grood ES, Suntay WJ. A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. J Biomech Eng. 1983;105:136–144. doi: 10.1115/1.3138397. [DOI] [PubMed] [Google Scholar]
- 34.Siston RA, Giori NJ, Goodman SB, et al. Surgical navigation for total knee arthroplasty: a perspective. J Biomech. 2007;40:728–735. doi: 10.1016/j.jbiomech.2007.01.006. [DOI] [PubMed] [Google Scholar]
- 35.Li G, Rudy TW, Allen C, et al. Effect of combined axial compressive and anterior tibial loads on in situ forces in the anterior cruciate ligament: a porcine study. J Orthop Res. 1998;16:122–127. doi: 10.1002/jor.1100160121. [DOI] [PubMed] [Google Scholar]
- 36.Andriacchi TP, Dyrby CO. Interactions between kinematics and loading during walking for the normal and acl deficient knee. J Biomech. 2005;38:293–298. doi: 10.1016/j.jbiomech.2004.02.010. [DOI] [PubMed] [Google Scholar]
- 37.Papadonikolakis A, Cooper L, Stergiou N, et al. Compensatory mechanisms in anterior cruciate ligament deficiency. Knee Surg Sports Traumatol Arthrosc. 2003;11:235–243. doi: 10.1007/s00167-003-0367-6. [DOI] [PubMed] [Google Scholar]
- 38.Jordan SS, DeFrate LE, Nha KW, et al. The in vivo kinematics of the anteromedial and posterolateral bundles of the anterior cruciate ligament during weightbearing knee flexion. Am J Sports Med. 2007;35:547–554. doi: 10.1177/0363546506295941. [DOI] [PubMed] [Google Scholar]
- 39.Li G, Zayontz S, Most E, et al. In situ forces of the anterior and posterior cruciate ligaments in high knee flexion: an in vitro investigation. J Orthop Res. 2004;22:293–297. doi: 10.1016/S0736-0266(03)00179-7. [DOI] [PubMed] [Google Scholar]
- 40.Li G, Papannagari R, Li M, et al. Effect of posterior cruciate ligament deficiency on in vivo translation and rotation of the knee during weightbearing flexion. Am J Sports Med. 2007 doi: 10.1177/0363546507310075. [DOI] [PubMed] [Google Scholar]
- 41.Li G, Defrate LE, Rubash HE, et al. In vivo kinematics of the acl during weight-bearing knee flexion. J Orthop Res. 2005;23:340–344. doi: 10.1016/j.orthres.2004.08.006. [DOI] [PubMed] [Google Scholar]
- 42.Nozaki H, Banks SA, Suguro T, et al. Observations of femoral rollback in cruciate-retaining knee arthroplasty. Clin Orthop Relat Res. 2002;404:308–314. doi: 10.1097/00003086-200211000-00046. [DOI] [PubMed] [Google Scholar]
- 43.Stiehl JB, Komistek RD, Dennis DA. Detrimental kinematics of a flat on flat total condylar knee arthroplasty. Clin Orthop Relat Res. 1999;369:139–148. doi: 10.1097/00003086-199908000-00019. [DOI] [PubMed] [Google Scholar]
- 44.Dennis DA, Komistek RD, Hoff WA, et al. In vivo knee kinematics derived using an inverse perspective technique. Clin Orthop Relat Res. 1996;331:107–117. doi: 10.1097/00003086-199610000-00015. [DOI] [PubMed] [Google Scholar]


