Abstract
Despite perinatal depression (PND) being a common mental disorder affecting pregnant women and new mothers, limited attention has been paid to the heterogeneous nature of this disorder. We examined heterogeneity in PND symptom profiles and symptom trajectories. Literature searches revealed 247 relevant studies, 23 of which were included in the final review. The most common statistical approaches used to explore symptom and trajectory heterogeneity were latent class model and growth mixture model. All but one study examined PND symptom trajectories, and provide collective evidence of at least three heterogeneous patterns: low, medium or chronic-high symptom levels. Social and psychological risk factors were the most common group of predictors related to a higher burden (high sum of score) of depressive symptoms. These studies were consistent in reporting poorer health outcomes for children of mothers assigned to high burden symptom trajectories. Only one study explored heterogeneity in symptom profile, and was the only one to describe the specific constellations of depressive symptoms related to the PND heterogeneous patterns identified. Therefore, there is limited evidence on the specific symptoms and symptom configurations that make up PND heterogeneity. We suggest directions for future research to further clarify the PND heterogeneity and its related mechanisms.
Keywords: Perinatal depression, heterogeneity, profile, latent class, trajectory
Introduction
Perinatal depression (PND) — depression with onset during pregnancy and early postpartum (American Psychiatric Association, 2013) — is a common problem for women worldwide. Up to 18.4% of women experience depression during pregnancy, and as many as 19.2% suffer minor or major depression in the first three months postpartum (Gavin et al., 2005, Halbreich and Karkun, 2006). The etiology of PND is multi-faceted and complex and the dynamic interaction among depressive symptoms, biology and environment is highly idiosyncratic. This means that the onset, course and symptom configuration of PND varies widely across women; this heterogeneity hampers the accurate assessment of personalized risk and prognosis for symptom progression and remission. Our goal in this paper is to review studies examining heterogeneity of symptom profiles and trajectories in PND.
Heterogeneity: One size does not fit all
Clinical evidence has long suggested heterogeneity in the patterns and predictors of common mood disorders. Heterogeneity leads to differing symptom profiles (Fried and Nesse, 2015a, Nandi et al., 2009), which are an individual’s nature and constellation of symptoms, and symptom trajectories, which are the patterns of symptom changes over time (Nandi et al., 2009). Epidemiological studies, however, have generally addressed symptom profiles and trajectories as homogeneous, that is, that one size fits all. This one-size fit all approach is manifested in the current literature by the use of instruments indicating the absence or presence of depression, through categorical diagnosis or as symptom severity levels. Although these traditional approaches have increased our knowledge about depression, they have paid limited attention to the fact that heterogeneity in depressive disorders poses several problems, among which are: (a) the incomplete understanding of the mechanistic pathways of what appear to be “homogenous” types of depression; (b) the lack of efficacy in interventions to ameliorate depression or prevent new onsets; and (c) the lack of tailored approaches to care of individuals with depression. Understanding depression as a homogeneous latent construct in which all putative depressive symptoms are treated as unidimensional or contributing equally to the depressive state is fundamentally problematic because depression is a complex disorder with multi-level causal mechanisms and symptom interactions that we do not yet fully understand (Fried et al., 2016, Kendler, 2008, Kendler et al., 2011).
In the first systematic review to explore heterogeneity of common mood and anxiety disorders, Nandi et al. (2009) showed that the literature of symptom profiles is largely focused on major depressive disorders, synthesizing evidence of symptom profiles for the depression sub-types, including atypical, melancholic, and seasonal depression. Nandi et al. (2009) also reported substantial evidence of longitudinal trajectory heterogeneity. More recently, Musliner et al. (2016) conducted a systematic review focusing only on depression symptom trajectories, not on symptom profiles. In reviewing 25 studies from 24 separate cohorts, they found that most of the studies identified either three or four distinct trajectories, varying both in severity (low, medium, or high) and stability over time (stable, increasing, or decreasing). Of the six studies of PND, Musliner et al (2016) identified four to six distinct trajectory patterns of depressive symptoms, varying from high to low symptom severity within a time span of six to 16 years.
Neither Nandi et al. (2009) nor Musliner et al. (2016), however, identified symptom profiles specific to PND, a depression sub-type in the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5; American Psychiatric Association, 2013), with a “perinatal period” specifier, meaning a non-psychotic episode of minor or major depression with onset during pregnancy or within four weeks postpartum. This sub-typing serves to validate the assumption that PND is more homogenous than major depression outside the perinatal period.
Findings from studies exploring heterogeneity in PND, however, have yet to be reviewed systematically. The available systematic reviews on depression heterogeneity focused on major depression outside the perinatal period (Musliner et al., 2016, Nandi et al., 2009, van Loo et al., 2012). Exploring heterogeneity in PND is important for the identification of characteristics associated with distinct symptom profiles and symptom trajectories, and for the development of interventions tailored to specific PND profiles and trajectories. Furthermore, research on symptom heterogeneity may increase our understanding of the biological mechanisms underlying PND. Therefore, the purpose of this study was to identify symptom profiles and trajectories of PND and summarize the current knowledge regarding (a) the number and patterns of profiles and trajectories, (b) the analytical approaches used to identify heterogeneous patterns, and (c) the antecedents and outcomes associated with different symptom and trajectory patterns.
Method
Search Strategy
In this systematic review, we explored the available literature on PND heterogeneity—symptom profiles and symptom trajectories.
We tested different combinations of search terms and evaluated their success in finding relevant literature. The following search string allowed for the most comprehensive search: (postpartum depression OR postnatal depression OR perinatal depression OR maternal depression) AND (latent class OR trajectory). We searched three electronic databases: PubMed, Scopus, and Embase for studies published through March 2016. We used the database filters to exclude animal studies. We supplemented the search with relevant studies cited in the reference lists of the included literature plus a limited number of articles we found by hand searching.
Inclusion Criteria
For inclusion in this review, articles in peer-reviewed journals had to examine maternal PND symptoms profiles or symptom trajectories. To this purpose, we focused on articles reporting on original data and using statistical methods (e.g., latent class model) that allowed for exploration of heterogeneity through subtypes, classes, clusters or other variants of heterogeneity. We considered the perinatal period timeframe broadly, therefore, including any study that reported heterogeneity of depressive symptoms with onset during pregnancy or within the first year of the postpartum period. Rather than using strict criteria for a major depression diagnosis, we conceptualized depression as a continuum ranging from no symptoms to severe symptoms; this allowed us to include papers reporting on depression across this symptom continuum.
To limit the influence of external confounders of PND, we excluded studies that focused on (1) parents of children with developmental problems, obesity, or who are survivors of natural disasters (e.g., Hurricane Katrina survivors); (2) children greater than one year old at baseline; (3) major depression without specific focus on mothers or the childbearing period; (4) joint trajectories of multiple disorders (e.g., depression and anxiety); and (5) animal studies.
Data Extraction and Analysis
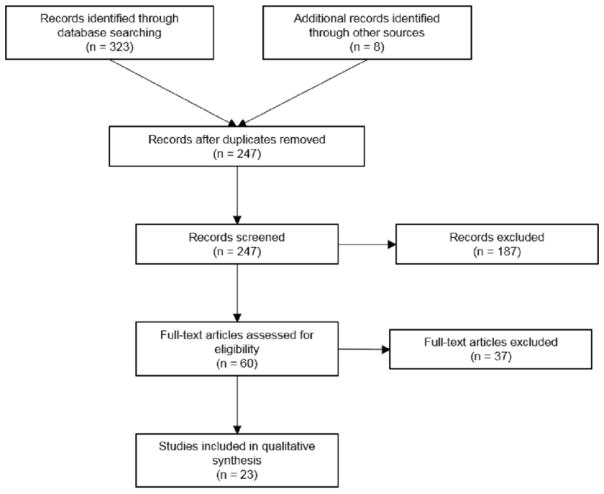
The database search returned 239 articles after duplicate citations were removed. Search in the reference lists of included articles and hand search provided another eight relevant titles, increasing the total to 247 unique titles. The first and last authors independently reviewed the titles and abstracts of all retrieved articles with an inter-rater agreement ≥90%; differing opinions about whether to include an article were discussed by the two reviewers to reach an agreement. In this initial phase, we excluded only articles that did not clearly satisfy the inclusion criteria. For the second phase, 60 articles remained, and the two researchers then completed a full text screening independently and again reviewed any disagreements; 23 articles remained for data extraction. We decided to keep multiple studies from the same cohort because they used different total sample sizes and analytical approaches. Two studies from one cohort, however, were combined because there were no clear distinctions between the two studies in terms of results related to heterogeneity of PND symptoms and analytical approach (van der Waerden et al., 2015a, van der Waerden et al., 2015b). The main reasons for excluding studies in this second stage were lack of specific analysis on heterogeneity in symptom subtype and symptom trajectory, lack of focus on mothers or the childbearing period, and joint trajectory of multiple disorders. Figure 1 details the procedure. The first and last authors extracted data from the 23 articles onto a master file for analysis. The first and second (senior statistician) authors reviewed the analyses sections and results of each included article, and as needed requested supplementary information from authors.
Figure 1.
Flow chart of the review.
Results
Study Characteristics
The 23 studies were from 20 distinct samples and 10 countries. Study characteristics, including country, sample size, data collection time points, depressive symptom measures, analytic methods, and main results are presented in Table 1 (at the end of the paper).
Table 1.
Studies Assessing Heterogeneity in Perinatal Depression Symptom Profiles and Symptom Trajectories*
| PND SYMPTOM PROFILES | |||
|---|---|---|---|
|
| |||
| Study; N; Country | Methods | Main Findings Patterns | Outcomes** |
| Putnam et al. (2015); n=10801; International Consortium1 |
Timeframe: pooled cross- sectional, varying according to original study site: prior, during and after diagnosis of PND. Measures: EPDS, HAM-D Analysis: LCA |
# of symptom profile classes: 3 1) No depressed class (53%): Mean score 3.27. 2) Symptomatic class (36%): Mean score 12.33. 3) Severe depression class (11%): Mean score 20.32. |
Psychological risk factors: poor mood, increased anxiety, onset of depressive symptoms during pregnancy, suicidal ideation. Biological risk factors: pregnancy and obstetric complications. |
|
| |||
| PND SYMPTOM TRAJECTORIES | |||
|
| |||
| Study; N ; Country | Methods | Main Findings Patterns | Predictors/Outcomes*** |
|
| |||
| Luoma et al. (2015); n=329; Finland |
Timeframe: 3rd trimester pregnancy, 1st week, 2 and 6 months, 4–5, 8–9, 16–17 years postpartum. Measures: EPDS Analysis: LGCM |
# of trajectory classes: 4 1) Very low symptoms trajectory (18%): Mean score range 0–1 across time. 2) Low-stable symptoms trajectory (53%): Mean score range 4–7 across time. 3) High-stable symptoms trajectory (27%): Mean score range 9–10 across time. 4) Intermittent symptoms trajectory (3%): Mean score range 11–19 across time. |
Social risk factors: negative life events, poor relationship with own mother. Psychological risk factors: depressive and anxiety symptoms during pregnancy, loneliness. Parenting expectation: negative expectation towards the child. |
| Matijasevich et al. (2015); n=4231; Brazil |
Timeframe: 3, 12, 24, 48 months and 6 years postpartum. Measures: EPDS Analysis: LGCM |
# of trajectory classes: 5 1) Low symptoms trajectory (34.8%): Mean score range 3 across time. 2) Moderate-low symptoms trajectory (40.9%): Mean score range 6–7 across time. 3) Increasing symptoms trajectory (9%): Mean score range 8–15 across time. 4) Decreasing symptoms trajectory (9.9%): Mean score range 13–8 across time. 5) High-chronic symptoms trajectory (5.4%): Mean score range 15–19 across time. |
Child outcome: more psychiatric disorders, and increased internalizing and externalizing problems. |
| van der Waerden et al. (2015a, 2015b);2 n=1807; France |
Timeframe: 3rd trimester pregnancy, 4, 8, 12, 24 months postpartum, 3, 4, 5 years postpartum. Measures: CES-D Analysis: LGCM |
# of trajectory classes: 5 1) No symptoms trajectory (60.2%): Mean score range 2.2–8.5 across time. 2) High pregnancy symptoms trajectory (4.7%): Mean score range 6.8–31.88 across time. 5) High preschool symptoms trajectory (4.9%): Mean score range 5.2–26.4 across time. 4) Persistent intermediate-level symptoms trajectory (25.2%): Mean score range 8.3–13.9 across time. 5) Persistent-high symptoms trajectory (5.0%): Mean score range 14.6–29.7 across time. |
Child outcome: increased emotional and behavioral difficulties, conduct disorder, and peer problems. Social risk factors: negative life events, ethnic-minority status. Psychological risk factors: anxiety during pregnancy, history of psychopathology. |
| Parade et al. (2014); n=98; US |
Timeframe: 8 and 2 weeks prior to due date, 4 and 24 weeks postpartum. Measures: CES-D Analysis: LGCM |
# of trajectory classes: 2 1) Consistent-low symptoms trajectory (57.2%): Mean score range 5.0–6.8 across time. 2) Temporary decline symptoms trajectory (42.8%): Mean score range 9.4–12.3 across time. |
Social risk factors: negative life events, conflict in partner-relationship. |
| Cents et al. (2013); n=4167; Netherlands |
Timeframe: 20 weeks pregnancy, 2, 6 and 36 months postpartum. Measures: BSI Analysis: LCGM |
# of trajectory classes: 4 1) No symptoms trajectory (34%): Mean score range 0.0 across time. 2) Low symptoms trajectory (54%): Mean score range 0.0–0.1 across time. 3) Moderate symptoms trajectory (11%): Mean score range 0.4–0.6 across time. 4) High symptoms trajectory (1.5%): Mean score range 1.2–2.5 across time. |
Social risk factors: low education, ethnic-minority status, low-income. Child outcome: increased internalizing problems. |
| Glasheen et al. (2013); n=577; US |
Timeframe: 4–5 and 7 months pregnancy, delivery, 8 and 18 months postpartum. Measures: CES-D Analysis: GMM |
# of trajectory classes: 2 1) Low pre- and postpartum symptoms trajectory (16.5%): Mean score range 14–11 across time. 2) High pre- and postpartum symptoms trajectory (83.5%): Mean score range 24–23 across time. |
Child outcome: no association between maternal pre- and postnatal depression trajectory exposure and major depression, anxiety, or conduct disorder in children. |
| Christensen et al. (2011); n=215; US |
Timeframe: 18, 28 weeks pregnancy, and 6 weeks, 4 and 12 months postpartum. Measures: BDI Analysis: GMM |
# of trajectory classes: 3 1) Low perinatal symptoms trajectory (80.0%): Mean score range 6–11 across time. 2) High postpartum symptoms trajectory (10.2%): Mean score range 14–25 across time. 3) High pregnancy symptoms trajectory (9.8%): Mean score range 6–35 across time. |
Social risk factors: unintended pregnancy. |
| Ramos-Marcuse et al. (2010); n=181; US |
Timeframe: 3 weeks, 6 and 24 months postpartum. Measures: BDI Analysis: LGCM |
# of trajectory classes: 3 1) Low symptoms trajectory (41%): Mean score range 4– 6 across time. 2) Medium symptoms trajectory (45%): Mean score range 7–11 across time. 3) High symptoms trajectory (14%): Mean score range 20–22 across time. |
Social risk factors: high negative life events. Psychological risk factors: low self- esteem. Parenting expectation: low parenting satisfaction. |
| Mora et al. (2009); n=1735; US |
Timeframe: 2nd trimester gestation, 3, 11 and 25 months postpartum. Measures: CES-D Analysis: GMM |
# of trajectory classes: 5 1) No symptoms trajectory (71%): Mean score range 8–9 across time. 2) Antepartum-only symptoms trajectory (6%): Mean score range 8–32 across time. 3) Postpartum symptoms trajectory (9%): Mean score range 16–30 across time. 4) Late, at 25 months postpartum, symptoms trajectory (7%): Mean score range 12–31 across time. 5) Chronic symptoms trajectory (7%): Mean score range 28–29 across time. |
Social risk factors: ambivalence about the pregnancy. Biological risk factors: high parity. |
| Ashman et al. (2008); n=159; US |
Timeframe: 14 months, 24 months, and 3.5, 4.5 and 6.5 years postpartum. Measures: LIFE Analysis: GMM |
# of trajectory classes: 3 1) Decreasing depression (30%): mean score range 14.9– 7.5. 2) Stable mild depression (62%): mean score range 1– 1.5. 3) Chronic depression (8%): mean score range 12.2–9.8. |
Child outcome: high levels of externalizing behavior problems, and behavior disorder diagnosis, and low social competence and decreased generalized brain activation, high respiratory sinus arrhythmia. |
|
| |||
| Avon Longitudinal Study of Children and Parents (ALSPAC) | |||
|
| |||
| Hammerton et al. (2015); n=10559; UK |
Timeframe: 18, 32 weeks pregnancy, 8 weeks and 8 months postpartum, 1 year 9 months, 2 years 9 months, 5 years 1 month, 6 years 1 month, 8 years 1 month and 11 years 2 months. Measures: EPDS Analysis: LCGM |
# of trajectory classes: 5 1) Minimal symptoms trajectory (39.6%): Mean score range 0–3.5 over time. 2) Mild symptoms trajectory (32.1%): Mean score range 5.5–7.5 over time. 3) Sub-threshold symptoms trajectory (17.6%): Mean score range 10–11 over time. 4) Increasing symptoms trajectory (5.5%): Mean score range 5–13 over time. 5) Chronic-severe symptoms trajectory (5.2%): Mean score range 14.5–16 over time. |
Child outcome: increased suicidal ideation. |
| Barker (2013); n=12151; UK |
Timeframe: 32 weeks pregnancy, 8 weeks, 8 months, 21 months and 33 months postpartum. Measures: EPDS Analysis: LLC |
# of trajectory classes: 3 1) Low symptoms trajectory (54%): Mean score range 2– 4 over time. 2) Medium symptoms trajectory (36%): Mean score range 8–9 over time. 3) Chronic symptoms trajectory (10%): Mean score range 14–15 over time. |
Child outcome: increased behavioral dysregulation. |
|
| |||
| The National Institute of Child Health and Human Development Study of Early Child Care and Youth Development | |||
|
| |||
| Campbell et al. (2009); n=1357; US |
Timeframe: 1, 6, 15, 24, 36, 54 months, and 7, 9, 11 and 12 years postpartum. Measures: CES-D Analysis: GMM |
# of trajectory classes: 5 1) Never depressed trajectory (48.7%): Mean score range 3.9–6.73 across time. 2) Early-decreasing symptoms trajectory (5.1%): Mean score range 9.8–24 across time. 3) Stable-subclinical symptoms trajectory (30.8%): Mean score range 9.1–12.5 across time. 4) Moderate-elevated symptoms trajectory (10.9%): Mean score range 12.9–20 across time. 5) Chronic symptoms trajectory (4.7%): Mean scores range 23.2–29.3 across time. |
Social risk factors: low education, unmarried. Biological risk factors: more health problems. Child outcome: increased internalizing and externalizing problems, and more risky behavior. |
| Campbell et al. (2007); n=1261; US |
Timeframe: 1, 6, 15, 24, 36 and 54 months, and 7 years postpartum. Measures: CES-D Analysis: LGCM |
# of trajectory classes: 6 1) Low-stable symptoms trajectory (45.6%): Mean score range 4.2–6 across time. 2) Moderate-stable symptoms trajectory (36.4%): Mean score range 10.5–12.2 across time. 3) Intermittent symptoms trajectory (3.6%): Mean scores range 29–9 across time. 4) Moderate-increasing symptoms trajectory (6.2%): Mean score range 14.9–25.8 over time. 5) High-decreasing symptoms trajectory (5.6%): Mean score range 13.2–25.5 across time. 6) High-chronic symptoms trajectory (2.5%): Mean score range 27–32.8 across time. |
Parenting expectation: low maternal sensitivity. Child outcome: more internalizing and externalizing symptoms. |
|
| |||
| Longitudinal Study of Australian Children (LSAC) | |||
|
| |||
| Giallo et al. (2015a); n=4164; Australia |
Timeframe: 3–12 months, 2–3, 4–5, 6–7 years postpartum. Measures: Kessler-6 Analysis: LCGM |
# of trajectory classes: 3 1) Minimal symptoms trajectory (74.6%): Mean score range 1.8–2.2 across time. 2) Subclinical symptoms trajectory (20.8%): Mean score range 5.3–6.3 across time. 3) Increasing and persistently-high symptoms trajectory (4.6%): Mean score range 9.5–12.4 across time. |
Child outcome: increased odds of asthma. |
| Giallo et al. (2015b); n=1085; Australia |
Timeframe: 10–24, 30–32 weeks gestation, 3, 6, 9, 12, and 18 months, and 4 years postpartum. Measures: EPDS Analysis: LCGM |
# of trajectory classes: 3 1) Minimal symptoms trajectory (61.0%): Mean score range 2–3 across time. 2) Subclinical symptoms trajectory (30.2%): Mean score range 6–8 over time. 3) Increasing and persistently-high symptoms trajectory (8.8 %): Mean score range 10–14 over time. |
Child outcome: increased emotional- behavioral difficulties. |
| Giallo et al. (2014); n=4879; Australia |
Timeframe: 3–12 months, 2–3, 4–5, and 6–7 years postpartum. Measures: Kessler-6 Analysis: LGM |
# of trajectory classes: 2 1) Minimal symptoms trajectory (84%): Mean score 2.1– 2.5 across time. 2) Persistently-high symptoms trajectory (16%): Mean score 7.9–8.5 across time. |
Social risk factors: low education, negative life events, ethnic-minority status. Psychological risk factors: history of psychopathology, antidepressant use during pregnancy. Biological risk factor: younger maternal age. Parenting expectations: negative expectation towards the child, low self- efficacy, and early parenting difficulty. |
|
| |||
| Mater University of Queensland Study of Pregnancy (MUSP) | |||
|
| |||
| Najman et al. (2016); n=6753; Australia |
Timeframe: 2nd trimester pregnancy, 6 months, 5, 14, 21 and 27 years postpartum. Measures: DSSI Analysis: LCGM |
# of trajectory classes: 3 1) Low symptoms trajectory (48.4%): Mean score range 0–0.5 across time. 2) Mild symptoms trajectory (41.7%): Mean score range 0.5–1.1 across time. 3) High-escalating symptoms trajectory (9.9%): Mean score range 1.6–3.5 across time. |
Biological risk factor: younger maternal age. |
| Kingsbury et al. (2015); n=2991; Australia |
Timeframe: 6 months, 5, 14 and 21 years after the birth. Measures: DSSI Analysis: K-means |
# of trajectory classes: 2 1) Low stable symptoms trajectory (78.9%): Mean score range 0.35–0.42 across time. 2) High-escalating symptoms trajectory (21.1%): Mean score range 1.34–3.45 across time. |
Social risk factors: low education, ambivalence about pregnancy, poor social support, conflict in partner- relationship. Psychological risk factors: stress and anxiety symptoms during pregnancy. Biological risk factor: younger maternal age. Parenting expectations: negative expectation towards the child. |
|
| |||
| Taiwanese Women Cohort | |||
|
| |||
| Kuo et al. (2014); n=139; Taiwan |
Timeframe: 3rd trimester pregnancy, 1, 3 days and 1 week, 1 and 6 months postpartum. Measures: EPDS Analysis: LGCM |
# of trajectory classes: 3 1) Low symptoms trajectory (30.9%): Mean score range 3–6 across time. 2) Mild symptoms trajectory (41.7%): Mean score range 9–9.5 across time. 3) High-stable symptoms trajectory (27.3%): Mean score range 14–16 across time. |
Biological risk factor: high pre- pregnancy body mass index and sleep difficulty. |
| Kuo et al. (2012); n=121; Taiwan |
Timeframe: 3rd trimester pregnancy, 1, 3 days and 1 week postpartum. Measures: EPDS Analysis: LGCM |
# of trajectory classes: 4 1) Low symptoms trajectory (23.1%): Mean score range 2–5 across time. 2) Mild symptoms trajectory (43%): Mean score range 7– 9.4 across time. 3) Moderate symptoms trajectory (25.6%): Mean score range 13.4 across time. 4) High symptoms trajectory (8.3%): Mean score range 17.6–20.3 across time. |
Biological risk factor: sleep difficulty. |
This table is organized by year of publication in decreasing order, and by study cohort with the most recent article of the cohort presented first.
Predictors significantly related to severity of depressive symptoms profile classes.
Predictors and outcomes related to high burden depressive symptom trajectories.
Represents 19 institutions in seven countries: Australia, France, Sweden, Netherlands, United Kingdom (UK), United States (US), and Denmark.
EDEN mother-child cohort study. These two manuscripts were combined because they used the same measure, analytical method and identified similar trajectories. In the predictor/outcome column we describe the findings of both reports.
Note. Analysis: LCA, latent class analysis; LLC, longitudinal latent class; LGCM, latent growth curve model; GBTM, group-based trajectory model; GMM, growth mixture model; LGM, latent growth model; LCGM, latent class growth model.
Measures used to estimate the trajectory classes: EPDS, Edinburgh Postnatal Depression Scale; HAM-D, Hamilton Depression Rating Scale; CES-D, Center for Epidemiological Studies-Depression, BSI, Brief Symptom Inventory; BDI-II, Beck Depression Inventory-version II; DSSI, Delusions-Symptoms-States Inventory, 7-item depression sub-scale; LIFE, longitudinal interval follow-up evaluation.
All but one study (Ashman et al., 2008) focused on general maternal perinatal populations, instead of clinically depressed women. Most of the samples were from high-income countries with limited attention to ethnic minorities and/or low-income populations (Christensen et al., 2011, Mora et al., 2009, Ramos-Marcuse et al., 2010). Only one study focused on symptom profile using a cross-sectional approach (n = 10,801), and the remaining studies explored symptom trajectory heterogeneity, with the length of follow-up ranging from 1 week to 27 years postpartum, and with the baseline starting either during pregnancy or postpartum. Sample size for the trajectory studies ranged from 98 to 12,151 women (Barker, 2013, Parade et al., 2014).
The depressive symptom measures most often used were the Edinburgh Postnatal Depression Scale (EPDS; 36% of the studies) and Center for Epidemiological Studies-Depression (CES-D; 27%). Both the EPDS (Cox et al., 1987) and CES-D (Radloff, 1977) measure depressive symptoms over the past week and have a 4-point scale ranging from 0 (rarely or not at all) to 3 (most or all the time). Higher scores indicate more depressive symptoms.
Analytical Approaches
As shown in Table 2, only one study (Putnam et al., 2015) explored heterogeneity in cross-sectional symptom profiles using latent class analysis (LCA), which is a statistical method for identifying unobservable classes among subjects based on multiple categorical variables (Collins and Lanza, 2010). The other 22 studies examined heterogeneity in depression trajectory based on longitudinal observations (Supplementary table S1). The most common statistical approaches used to explore symptom trajectory heterogeneity were latent class growth model (LCGM1; 65%) and growth mixture model (GMM; 22%). The LCGM models assume that the population is composed of several distinct groups defined by their symptom trajectories (Jones et al., 2001, Nagin, 2005). GMM is an extension of the LCGM in that it identifies distinct subgroups of growth trajectories and allows individuals to vary around subgroup-specific mean trajectories. This means, GMM allows a random (subject dependent) intercept to model subject effects. The two approaches, LCGM and GMM, are otherwise similar, in that both allow flexible modeling of depression trend using linear/quadratic/cubic or even piecewise linear functions of time.
Table 2.
Classification of studies (n=23) by design and analytical approach.
| Single Total | Multiple Sub-scores | |
|---|---|---|
|
|
||
| Cross-sectional | 0/23 | 1/23 LCA to study symptom profiles |
| Longitudinal | 22/23 LCGM/GMM/K-means to study heterogeneity in depression trend |
0/23 |
Note. LCA, latent class analysis; LGCM, latent growth curve model; GBTM, group-based trajectory model; GMM, growth mixture model; LGM, latent growth model; LCGM, latent class growth model
K-means approach (Hartigan, 1975) was employed in one study to cluster subjects based on repeated depression measures (Kingsbury et al., 2015). Unlike LCGM and GMM, K-means approach is a non-parametric approach, which requires no model assumptions on the shape of trend or on the distribution of depression measures, but relies on squared Euclidean distance measure to conduct clustering. Except for the study (Kingsbury et al., 2015) that conducted K-means using Stata (StataCorp, 2011), 12 of 22 remaining studies conducted trajectory analyses using Mplus (Muthén, 2004, Muthén and Muthén, 2000) and 10 used the freely available SAS procedure, PROC TRAJ (Jones et al., 2001, Nagin, 2005). All analyses using GMM, and the LCA reported in Putnam et al. (2015), were conducted in Mplus.
These three analytical approaches, though technically different, serve the same goal of uncovering population heterogeneity in trajectory of depression measures over time. After careful review of the methods sections of these studies, we believe nearly all these studies followed the “classify-and-analyze” approach (Bray et al., 2015, Clogg, 1995) to examine the relationship between risk factors and latent class memberships (trajectories), or distal outcome (e.g., children behavior) and latent class memberships. The classify-and-analyze approach assigns each subject into one of the identified classes and treats this class label as an observable outcome (in the analysis of risk factors) or a risk factor (in the analysis of distal outcome). Most of the studies (n=19) reported satisfactory class membership assignment or model entropy (Supplementary table S1); the remaining four studies referred to quality of model entropy and class membership assignment but did not provide such data either in the article or by our request.
Patterns of symptom profiles
Only one article addressing patterns of symptom profiles was identified (Putnam et al., 2015). Using common data elements from 19 international sites, the authors applied latent class analyses in a two-tiered approach to identify PND symptom profiles during the postpartum period. Tier one assessed symptom heterogeneity in women (n = 6,556) with complete data on the EPDS, and tier two in those with PND clinical case status (n = 4,245). A final model with three latent classes was considered optimum for both tiers. The most severe class, symptom profile class 3 (n = 730, 11%), had severe scores in most of the 10 symptoms assessed in the EPDS, except for positive affect: laughing and enjoyment. The moderate class (n = 2342, 36%) was the class with the least positive affect.
Patterns of symptom trajectories
The longitudinal studies reviewed (n = 22, estimated total sample of 38,779 women) indicate heterogeneity in patterns of PND symptom trajectories (Table 1). Two to six symptom trajectory classes were identified, with seven studies supporting a three-trajectory classes solution and five studies supporting a five-trajectory classes solution (Supplementary table S1). Trajectories varied in terms of time of onset, according to baseline time point (pregnancy or postpartum), severity (low, medium, or high), and stability (stable, increasing or decreasing).
Five studies described trajectories based on severity levels (two trajectories: low and high; and three trajectories-low, medium and high), and these trajectories are described as time-stable with linear trend (Barker, 2013, Giallo et al., 2014, Glasheen et al., 2013, Kuo et al., 2014, Ramos-Marcuse et al., 2010). The other studies reported symptom trajectory trends with variability — at least one trajectory having a quadratic trend. The trends most often reported were (1) a sudden drop of depressive symptoms from baseline through the first year of postpartum (Campbell et al., 2007, Christensen et al., 2011, van der Waerden et al., 2015a); (2) an increase in severity of depressive symptoms from pregnancy to postpartum followed by a decline (Campbell et al., 2009, Cents et al., 2013, Mora et al., 2009); and (3) a constant increase in symptoms over time (Hammerton et al., 2015, Matijasevich et al., 2015, van der Waerden et al., 2015a). We tested whether percentage of time-stable classes and model entropy were related to the total number of classes identified and no significant association was identified, p = 0.07 and p =0.08, respectively.
The low and high severity symptom trajectories were identified in all studies; the low trajectory was always represented by a stable pattern of low symptom levels over time, and usually represented the largest trajectory group, with 34–80% of the sample (Cents et al., 2013, Christensen et al., 2011). There was one exception: a study conducted among substance-abusing women in whom the low trajectory represented only 16.5% of the sample, in comparison to 83.5% of the high symptom trajectory (Glasheen et al., 2013). The high severity symptom trajectory was described as a stable pattern of severe symptom levels over time and was the smallest trajectory group, usually ≤10% of the sample (Cents et al., 2013, Hammerton et al., 2015, Mora et al., 2009), with few exceptions (Kingsbury et al., 2015, Kuo et al., 2014, Luoma et al., 2015).
Factors related to symptom trajectory membership assignment
Thirteen studies identified predictors of membership assignment to high symptom burden trajectories, and we classified these predictors in four categories: social, psychological, and biological risk factors, and parenting expectations (Table 1). The social risk factors most often reported were: low education (Campbell et al., 2009, Cents et al., 2013, Giallo et al., 2014, Kingsbury et al., 2015), negative life events (Giallo et al., 2014, Luoma et al., 2015, Parade et al., 2014, van der Waerden et al., 2015b), ethnic-minority status (Cents et al., 2013, Giallo et al., 2014, van der Waerden et al., 2015b), and unintended or ambivalence about pregnancy (Christensen et al., 2011, Kingsbury et al., 2015, Mora et al., 2009). Among the psychological risk factors, stress, depressive or anxiety symptoms during pregnancy (Kingsbury et al., 2015, Luoma et al., 2015, van der Waerden et al., 2015b), and history of psychopathology (Giallo et al., 2014, van der Waerden et al., 2015b), were the most described. Younger maternal age was described in three studies as a biological risk factor (Giallo et al., 2014, Kingsbury et al., 2015, Najman et al., 2016), followed by sleep difficulty (Kuo et al., 2014, Kuo et al., 2012). Parenting expectations, including negative expectation towards the child (Giallo et al., 2014, Kingsbury et al., 2015, Luoma et al., 2015), and low parenting satisfaction or self-efficacy (Giallo et al., 2014, Ramos-Marcuse et al., 2010) functioned as predictors of trajectory membership assignment in six studies.
More specifically, Cents et al. (2013) found that low education, ethnic-minority and low-income status increased the probability of mothers being assigned to the ‘moderate’ or ‘high depressive symptom trajectories. Giallo et al. (2014) found that past history of depressive symptoms was the strongest predictor associated with membership in the persistently-high depressive symptoms trajectory. Unintended pregnancy was associated with a nearly fourfold increase in risk for the postpartum high depressive symptoms trajectory (Christensen et al., 2011), while ambivalence about pregnancy was uniquely associated with the chronic and antepartum-only symptom trajectories (Mora et al., 2009).
Child outcomes related to symptom trajectory membership assignment
Nine studies explored child outcomes related to symptom trajectories (Table 1). Children of mothers assigned to any of the higher trajectories of depressive symptoms were found to have significantly more internalizing problems than children of mothers assigned to the ‘no depressive symptoms’ trajectory (Campbell et al., 2007, Campbell et al., 2009, Matijasevich et al., 2015); and, for at least one study, this relationship was maintained after controlling for sociodemographic variables and gender of the child (Cents et al., 2013). In addition, variation in maternal depressive symptom trajectory was associated with suicidal ideation at age 16 of children, with greatest risk of suicidal ideation for children of mothers with chronic-severe depressive symptom trajectory (Hammerton et al., 2015). Glasheen et al. (2013), however, found no association between maternal pre- and postnatal depression trajectory exposure and major depression, anxiety, or conduct disorder in children.
In another study, higher levels of maternal depression were associated with increased social risks, which were, in turn, associated with more negative child behavioral outcomes (Ashman et al., 2008). In terms of physical health, Giallo et al. (2015a) documented that children had approximately a threefold increase in odds of asthma at six to seven years of age, after accounting for known risk factors, including pregnancy smoking and maternal history of asthma.
Discussion
In this manuscript we reviewed studies exploring heterogeneity in PND symptom profiles and symptom trajectories over time. We identified a total of 247 relevant studies, and 23 of them were included in the final review. Twenty two studies examined PND symptom trajectories, while one study explored heterogeneity in symptom profile, identifying three PND profiles varying in terms of severity of depressive symptoms (Putnam et al., 2015). Social and psychological risk factors were the most common group of predictors related to a higher burden (high sum of score) depressive symptom trajectories. The specific risk factors most often reported were: low education, negative life events, ethnic-minority status, mood or anxiety symptoms during pregnancy, and prior history of psychopathology. Nine studies explored child outcomes related to symptom trajectories, and they were consistent in reporting poorer health outcomes for children of mothers assigned to high burden symptom trajectories. The predictors and outcomes identified in these studies, however, are not exhaustive, and future research can expand and refine this knowledge.
As shown in Table 2, we could classify studies of the heterogeneity of PND by (1) study design: cross-sectional or longitudinal; and (2) outcome definition: a single total score or multiple symptom-specific sub-scores. All of the PND symptom trajectory studies explored heterogeneity based on the sum of scores from depression screening measures; at one end were women experiencing no or low depressive symptom burden (low sum of scores) trajectories, and at the other end were women with trajectories composed of chronic levels (clinically high sum of scores) of PND symptoms. Despite referring to depressive symptoms, none of the studies in this review profiled the constellation of symptoms that compose each type of trajectory pattern; therefore, we cannot attest on the qualitative difference of the trajectories beyond the longitudinal pattern of change. Reporting only the sum of scores as proxy of depressive symptoms has no direct translation into the actual symptoms that are making up that total score (Fried and Nesse, 2015b). Only one study examined symptom profiles (Putnam et al., 2015).
We expected to find no cross-sectional study on a single total score, because such study would likely be too simple to satisfactorily reveal the inherent complexity of PND heterogeneity (Table 2), nor did we expect to find an analysis of longitudinal multiple sub-scores, because there is no well-accepted approaches or readily available software for analyzing longitudinal multivariate outcomes. However, among the 24 selected studies, the preponderance of studies with longitudinal total score as the primary outcome, and the very small proportion of studies on cross-sectional multiple sub-scores surprised us. Such an imbalance may partially reflect the popularity of the analytical methodologies: LCGM and GMM. We agree that LCGM and GMM, or similar analytical approaches are very useful exploratory analytical tools and these studies do generate very interesting findings on heterogeneous trends of PND. On the other hand, however, we think it is a missed opportunity to explore information that may only be conveyed through the inter-correlations among individual symptoms, given the readily available data in all these studies.
Whether the results identified in this review generalize to women with low income or minority groups is unknown. The sample in the majority of the studies was characterized as mostly non-immigrant Caucasian, with a college or professional degree, married or cohabitating, and middle- or higher income. Therefore, generalizability to other populations might be limited. Evidence suggests a three to four fold higher prevalence of PND for women of low socioeconomic or immigrant ethnic-minority status (Falah-Hassani et al., 2015, Halbreich and Karkun, 2006). Understanding PND heterogeneity and related underlying mechanisms in women from minority groups is of important public health relevance because of the potential to better understand maternal mental health disparities. Furthermore, different symptoms and symptom constellations of depression have shown to differ in their risk factors, underlying biology, impairment of psychosocial function, and particular adverse life events that trigger specific symptom profiles (Fried and Nesse, 2015b). This stresses the urgency of taking symptoms into account for personalized medicine, prediction and treatment.
Directions for Future Research
This review lends support to evidence of heterogeneity in PND symptom patterns. So where do we go from here? The reviewed literature explored PND heterogeneity only at the group-level, using the total sum of scores of depressive measures and categorizing heterogeneity in terms of a severity continuum, from healthy to depressed. At this macro-level, it is harder to detect symptom dynamics and how these dynamics influence the health of individuals. For example, the trajectory findings showing that chronically depressed mothers have a stable pattern of symptoms over time is problematic because the stability is defined in terms of the variation in the total sum of scores between time points; these time points were often broadly spaced from weeks to years. Although the trajectory patterns look relatively stable, the individual women have more likely experienced variation at the level and range of symptoms; to reliably capture this variation, intensive data-sampling is required, enabling a glance into the rapid nature of changing patterns (Wichers, 2014). This approach is needed to advance our understanding of PND heterogeneity and personalized insights into the underlying mechanics related to the emergence and persistence of PND.
Intensive data-sampling and re-shifting focus on symptoms configuration from total global score is a promising idea but also brings great challenges to statistical analysis. The intensive observations of an individual symptom over time offer unique opportunities to describe detailed temporal changes and identify related environmental and psychosocial antecedents and consequences at a finer level, and recent advancements in statistical modeling (Dziak et al., 2015) also provide suitable tools to uncover fine-grained information contained in such intensive data. However, it is also highly desired to simultaneously model multiple relevant symptoms using the intensively collected data to gain knowledge on the etiology paths of depressive symptoms, in addition to temporal changes of individual symptoms. This would require a more advanced statistical approach that is capable of handling intensive multivariate longitudinal observations, with the aim of untangling the complex, possibly evolving, inter-correlation structure among these symptoms; the work of Dziak et al. (2015) makes a good start in this direction. In addition, the emerging network analysis approach (Borsboom and Cramer, 2013), which has recently been employed to study intrinsic structure of mood disorders, might provide a promising complementary strategy to Dziak et al. (2015) to tackle the ambitious task of uncovering the complex dynamic inter-correlation structure among symptoms related to PND heterogeneity. Another possibility is to call for network analysis on the group level and try to derive predictors for positive vs negative distal outcomes (Boschloo et al., 2016, van Borkulo et al., 2015). Advancement analytical approach, which could combine the ideas of time-varying effect models and network analysis approach, is desired to make better use of the information contained in such longitudinal multivariate symptom scores.
The results of this review have to be considered in the light of two main limitations. First, our analysis was based on qualitative comparison of the studies. To the best of our knowledge, there is no available method to integrate the results of multiple latent class approaches. To minimize this limitation, and increase the quality of this review, we only included studies that clearly identified the analytical approach used, their rational for model selection and focused on PND heterogeneity. Second, despite the fact that PND and anxiety are common comorbidities, we chose not include studies with joint analysis of multiple disorders because in these analysis we could not identify the specific contribution of PND to the findings identified.
This systematic review integrated the emerging evidence for heterogeneity in the PND symptom profile and symptom trajectories. This heterogeneity varies from a ‘no symptoms’ to a ‘high-severe symptoms’ group of mothers with overall high depressive symptom levels. However, as a field, we have not gotten much further in understanding PND heterogeneity. There is limited evidence on the specific symptoms and symptom configurations that make up PND heterogeneity. A better understanding of the change in mood and the speed and direction in which these changes occur is essential to better comprehend the nature of PND heterogeneity and individual variations. Therefore, approaches that take into consideration individual and symptom-level approaches are desirable as the knowledge to be generated is of great need for the perinatal mental health field to move towards elucidating the possible mechanisms underlying PND, and translates group findings to knowledge that is relevant to individual women in the form of personalized health interventions.
Supplementary Material
Acknowledgments
Funding: This study was funded by the North Carolina Translational & Clinical Sciences Institute (NC TraCS), NIH Clinical and Translational Science Award (Grant # 550KR131619) and the University of North Carolina at Chapel Hill School of Nursing, small pilot program.
We would like to thank Eiko Fried and Beth Black for their comments in the early drafts of this manuscript, and Mary White for the assistance in setting up the database searches.
Footnotes
LCGM was also called semi-parametric group-based modelling, latent growth (curve) model, group-based modeling, group-based trajectory technique/modeling, in these studies.
Conflict of interest: HS, XT, and RS declare that they have no conflict of interest.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. American Psychiatric Publishing; Arlington, VA: 2013. [Google Scholar]
- Ashman SB, Dawson G, Panagiotides H. Trajectories of maternal depression over 7 years: relations with child psychophysiology and behavior and role of contextual risks. Development and Psychopatholy. 2008;20:55–77. doi: 10.1017/S0954579408000035. [DOI] [PubMed] [Google Scholar]
- Barker ED. The duration and timing of maternal depression as a moderator of the relationship between dependent interpersonal stress, contextual risk and early child dysregulation. Psychological Medicine. 2013;43:1587–96. doi: 10.1017/S0033291712002450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsboom D, Cramer AO. Network analysis: an integrative approach to the structure of psychopathology. Annual Review of Clinical Psychology. 2013;9:91–121. doi: 10.1146/annurev-clinpsy-050212-185608. [DOI] [PubMed] [Google Scholar]
- Boschloo L, van Borkulo CD, Borsboom D, Schoevers RA. A prospective study on how symptoms in a network predict the onset of depression. Psychotherapy and Psychosomatics. 2016;85:183–4. doi: 10.1159/000442001. [DOI] [PubMed] [Google Scholar]
- Bray BC, Lanza ST, Tan X. Eliminating bias in classify-analyze approaches for latent class analysis. Structural Equation Modeling. 2015;22:1–11. doi: 10.1080/10705511.2014.935265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell SB, Matestic P, von Stauffenberg C, Mohan R, Kirchner T. Trajectories of maternal depressive symptoms, maternal sensitivity, and children's functioning at school entry. Developmental Psychology. 2007;43:1202–15. doi: 10.1037/0012-1649.43.5.1202. [DOI] [PubMed] [Google Scholar]
- Campbell SB, Morgan-Lopez AA, Cox MJ, McLoyd VC. A latent class analysis of maternal depressive symptoms over 12 years and offspring adjustment in adolescence. Journal of Abnormal Psychology. 2009;118:479–93. doi: 10.1037/a0015923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cents RA, Diamantopoulou S, Hudziak JJ, Jaddoe VW, Hofman A, Verhulst FC, Lambregtse-van den Berg MP, Tiemeier H. Trajectories of maternal depressive symptoms predict child problem behaviour: the Generation R study. Psychological Medicine. 2013;43:13–25. doi: 10.1017/S0033291712000657. [DOI] [PubMed] [Google Scholar]
- Christensen AL, Stuart EA, Perry DF, Le HN. Unintended pregnancy and perinatal depression trajectories in low-income, high-risk Hispanic immigrants. Prevention Science. 2011;12:289–99. doi: 10.1007/s11121-011-0213-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clogg CC. Latent class models: recent developments and prospects for the future. In: Arminger G, Clogg CC, Sobel ME, editors. Handbook of statistical modeling for the social and behavioral sciences. Plenum Press; New York: 1995. pp. 311–359. [Google Scholar]
- Collins LM, Lanza ST. Latent class and latent transition analysis: with implications in the social, behavioral and health sciences. John Wiley & Sons, Inc; Hoboken, NJ: 2010. [Google Scholar]
- Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression: development of the 10-item Edinburgh Postnatal Depression Scale. British Journal of Psychiatry. 1987;150:782–6. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- Dziak JJ, Li R, Tan X, Shiffman S, Shiyko MP. Modeling intensive longitudinal data with mixtures of nonparametric trajectories and time-varying effects. Psychological Methods. 2015;20:444–69. doi: 10.1037/met0000048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falah-Hassani K, Shiri R, Vigod S, Dennis C-L. Prevalence of postpartum depression among immigrant women: a systematic review and meta-analysis. Journal of Psychiatric Research. 2015;70:67–82. doi: 10.1016/j.jpsychires.2015.08.010. [DOI] [PubMed] [Google Scholar]
- Fried EI, Nesse RM. Depression is not a consistent syndrome: An investigation of unique symptom patterns in the STAR*D study. Journal of Affective Disorders. 2015a;172:96–102. doi: 10.1016/j.jad.2014.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fried EI, Nesse RM. Depression sum-scores don't add up: why analyzing specific depression symptoms is essential. BMC Medicine. 2015b;13:72. doi: 10.1186/s12916-015-0325-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fried EI, van Borkulo CD, Epskamp S, Schoevers RA, Tuerlinckx F, Borsboom D. Measuring depression over time . . . or not? Lack of unidimensionality and longitudinal measurement invariance in four common rating scales of depression. Psychological Assessment. 2016 doi: 10.1037/pas0000275. [DOI] [PubMed] [Google Scholar]
- Gavin NI, Gaynes BN, Lohr KN, Meltzer-Brody S, Gartlehner G, Swinson T. Perinatal depression: a systematic review of prevalence and incidence. Obstetrics & Gynecology. 2005;106:1071–83. doi: 10.1097/01.AOG.0000183597.31630.db. [DOI] [PubMed] [Google Scholar]
- Giallo R, Bahreinian S, Brown S, Cooklin A, Kingston D, Kozyrskyj A. Maternal depressive symptoms across early childhood and asthma in school children: findings from a longitudinal Australian population based study. PLoS ONE. 2015a;10:e0121459. doi: 10.1371/journal.pone.0121459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giallo R, Cooklin A, Nicholson JM. Risk factors associated with trajectories of mothers' depressive symptoms across the early parenting period: an Australian population-based longitudinal study. Archives of Women’s Mental Health. 2014;17:115–25. doi: 10.1007/s00737-014-0411-1. [DOI] [PubMed] [Google Scholar]
- Giallo R, Woolhouse H, Gartland D, Hiscock H, Brown S. The emotional-behavioural functioning of children exposed to maternal depressive symptoms across pregnancy and early childhood: a prospective Australian pregnancy cohort study. European Child & Adolescent Psychiatry. 2015b;24:1233–44. doi: 10.1007/s00787-014-0672-2. [DOI] [PubMed] [Google Scholar]
- Glasheen C, Richardson GA, Kim KH, Larkby CA, Swartz HA, Day NL. Exposure to maternal pre- and postnatal depression and anxiety symptoms: risk for major depression, anxiety disorders, and conduct disorder in adolescent offspring. Devevelopment and Psychopathology. 2013;25:1045–63. doi: 10.1017/S0954579413000369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halbreich U, Karkun S. Cross-cultural and social diversity of prevalence of postpartum depression and depressive symptoms. Journal of Affective Disorders. 2006;91:97–111. doi: 10.1016/j.jad.2005.12.051. [DOI] [PubMed] [Google Scholar]
- Hammerton G, Mahedy L, Mars B, Harold GT, Thapar A, Zammit S, Collishaw S. Association between maternal depression symptoms across the first eleven years of their child's life and subsequent offspring suicidal ideation. PLoS One. 2015;10:e0131885. doi: 10.1371/journal.pone.0131885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartigan JA. Clustering algorithms. John Wiley & Sons, Inc; New York: 1975. [Google Scholar]
- Jones BL, Nagin DS, Roeder K. A SAS procedure based on mixture models for estimating developmental trajectories. Sociological Methods & Research. 2001;29:374–393. [Google Scholar]
- Kendler KS. Explanatory models for psychiatric illness. American Journal of Psychiatry. 2008;165:695–702. doi: 10.1176/appi.ajp.2008.07071061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Zachar P, Craver C. What kinds of things are psychiatric disorders? Psychological Medicine. 2011;41:1143–50. doi: 10.1017/S0033291710001844. [DOI] [PubMed] [Google Scholar]
- Kingsbury AM, Hayatbakhsh R, Mamun AM, Clavarino AM, Williams G, Najman JM. Trajectories and predictors of women's depression following the birth of an infant to 21 years: a longitudinal study. Maternal and Child Health Journal. 2015;19:877–88. doi: 10.1007/s10995-014-1589-6. [DOI] [PubMed] [Google Scholar]
- Kuo SY, Chen SR, Tzeng YL. Depression and anxiety trajectories among women who undergo an elective cesarean section. PLoS One. 2014;9:e86653. doi: 10.1371/journal.pone.0086653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuo SY, Yang YL, Kuo PC, Tseng CM, Tzeng YL. Trajectories of depressive symptoms and fatigue among postpartum women. Journal of Obstetric, Gynecologic & Neonatal Nursing. 2012;41:216–26. doi: 10.1111/j.1552-6909.2011.01331.x. [DOI] [PubMed] [Google Scholar]
- Luoma I, Korhonen M, Salmelin RK, Helminen M, Tamminen T. Long-term trajectories of maternal depressive symptoms and their antenatal predictors. Journal of Affective Disorders. 2015;170:30–8. doi: 10.1016/j.jad.2014.08.017. [DOI] [PubMed] [Google Scholar]
- Matijasevich A, Murray J, Cooper PJ, Anselmi L, Barros AJ, Barros FC, Santos IS. Trajectories of maternal depression and offspring psychopathology at 6 years: 2004 Pelotas cohort study. Journal of Affective Disorders. 2015;174:424–31. doi: 10.1016/j.jad.2014.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mora PA, Bennett IM, Elo IT, Mathew L, Coyne JC, Culhane JF. Distinct trajectories of perinatal depressive symptomatology: evidence from growth mixture modeling. American Journal of Epidemiology. 2009;169:24–32. doi: 10.1093/aje/kwn283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musliner KL, Munk-Olsen T, Eaton WW, Zandi PP. Heterogeneity in long-term trajectories of depressive symptoms: Patterns, predictors and outcomes. Journal of Affective Disorders. 2016;192:199–211. doi: 10.1016/j.jad.2015.12.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén B. Latent variable analysis: growth mixture modeling and related techniques for longitudinal data. In: Kaplan D, editor. In The Sage handbook of quantitative methodology for the social sciences. Sage Publications; Thousand Oaks, CA: 2004. pp. 345–370. [Google Scholar]
- Muthén B, Muthén LK. Integrating person-centered and variable-centered analyses: growth mixture modeling with latent trajectory classes. Alcoholism: Clinical and Experimental Research. 2000;24:882–91. [PubMed] [Google Scholar]
- Nagin DS. Group-based modeling of development. Harvard University Press; Cambridge: 2005. [Google Scholar]
- Najman JM, Plotnikova M, Williams GM, Alati R, Mamun AA, Scott J, Wray N, Clavarino AM. Trajectories of maternal depression: a 27-year population-based prospective study. Epidemiology and Psychiatric Sciences. 2016:1–10. doi: 10.1017/S2045796015001109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nandi A, Beard JR, Galea S. Epidemiologic heterogeneity of common mood and anxiety disorders over the lifecourse in the general population: a systematic review. BMC Psychiatry. 2009;9:31. doi: 10.1186/1471-244X-9-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parade SH, Blankson AN, Leerkes EM, Crockenberg SC, Faldowski R. Close relationships predict curvilinear trajectories of maternal depressive symptoms over the transition to parenthood. Family Relations. 2014;63:206–218. [Google Scholar]
- Putnam K, Robertson-Blackmore E, Sharkey K, Payne J, Bergink V, Munk-Olsen T, Deligiannidis K, Altemus M, Newport J, Apter G, Devouche E, Vikorin A, Magnusson P, Lichtenstein P, Penninx B, Buist A, Bilszta J, O'Hara M, Stuart S, Brock R, Roza S, Tiemeier H, Guille C, Epperson CN, Kim D, Schmidt P, Martinez P, Wisner KL, Stowe Z, Jones I, Rubinow D, Sullivan P, Meltzer-Brody S. Heterogeneity of postpartum depression: a latent class analysis. Lancet Psychiatry. 2015;2:59–67. doi: 10.1016/S2215-0366(14)00055-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Ramos-Marcuse F, Oberlander SE, Papas MA, McNary SW, Hurley KM, Black MM. Stability of maternal depressive symptoms among urban, low-income, African American adolescent mothers. Journal of Affective Disorders. 2010;122:68–75. doi: 10.1016/j.jad.2009.06.018. [DOI] [PubMed] [Google Scholar]
- StataCorp. Stata statistical software: release 12. StataCorp; College Station, TX: 2011. [Google Scholar]
- van Borkulo C, Boschloo L, Borsboom D, Penninx BW, Waldorp LJ, Schoevers RA. Association of symptom network structure with the course of longitudinal depression. JAMA Psychiatry. 2015;72:1219–26. doi: 10.1001/jamapsychiatry.2015.2079. [DOI] [PubMed] [Google Scholar]
- van der Waerden J, Galera C, Larroque B, Saurel-Cubizolles MJ, Sutter-Dallay AL, Melchior M. Maternal depression trajectories and children's behavior at age 5 years. Journal of Pediatrics. 2015a;166:1440–8. e1. doi: 10.1016/j.jpeds.2015.03.002. [DOI] [PubMed] [Google Scholar]
- van der Waerden J, Galera C, Saurel-Cubizolles MJ, Sutter-Dallay AL, Melchior M. Predictors of persistent maternal depression trajectories in early childhood: results from the EDEN mother-child cohort study in France. Psychological Medicine. 2015b;45:1999–2012. doi: 10.1017/S003329171500015X. [DOI] [PubMed] [Google Scholar]
- van Loo HM, de Jonge P, Romeijn JW, Kessler RC, Schoevers RA. Data-driven subtypes of major depressive disorder: a systematic review. BMC Medicine. 2012;10:156. doi: 10.1186/1741-7015-10-156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wichers M. The dynamic nature of depression: a new micro-level perspective of mental disorder that meets current challenges. Psychological Medicine. 2014;44:1349–60. doi: 10.1017/S0033291713001979. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.