Abstract
Objective
To provide information on the prevalence and treatment of methicillin-resistant Staphylococcus aureus (MRSA) infections and the distinction between community-associated MRSA and health care–associated MRSA.
Quality of evidence
The MEDLINE and EMBASE databases were searched from 2005 to 2016. Epidemiologic studies were summarized and the relevant treatment literature was based on level I evidence.
Main message
The incidence of community-associated MRSA infection is rising. Certain populations, including indigenous Canadians and homeless populations, are particularly affected. Community-associated MRSA can be distinguished from health care–associated MRSA based on genetic, epidemiologic, or microbiological profiles. It retains susceptibility to some oral agents including trimethoprim-sulfamethoxazole, clindamycin, and tetracyclines. Community-associated MRSA typically presents as purulent skin and soft tissue infection, but invasive infection occurs and can lead to severe, complicated disease. Treatment choices and the need for empiric MRSA coverage are influenced by the type and severity of infection.
Conclusion
Community-associated MRSA is a common cause of skin and soft tissue infections and might be common in populations where overcrowding and limited access to clean water exist.
Résumé
Objectif
Fournir des renseignements sur la prévalence et le traitement des infections aux Staphylococcus aureus résistants à la méticilline (SARM), de même que sur la distinction entre les SARM d’origine communautaire et les SARM associés aux soins de santé.
Qualité des données
Une recension dans les bases de données MEDLINE et EMBASE a été effectuée, portant sur la période de 2005 à 2016. Les études épidémiologiques ont été résumées, et les ouvrages pertinents sur les traitements se fondaient sur des données probantes de niveau I.
Message principal
L’incidence des infections aux SARM d’origine communautaire est à la hausse. Certaines populations, dont les Canadiens autochtones et les sans-abri, sont particulièrement touchées. Les SARM d’origine communautaire se distinguent des SARM associés aux soins de santé d’après leurs profils génétiques, épidémiologiques ou microbiologiques. Ils demeurent susceptibles à certains agents oraux, notamment la combinaison triméthoprimesulfaméthoxazole, la clindamycine et les tétracyclines. Les SARM d’origine communautaire se présentent habituellement sous la forme d’une infection purulente de la peau et des tissus mous, mais une infection invasive peut se produire et entraîner une maladie plus sévère et compliquée. Les choix de traitement et la nécessité d’une approche empirique aux SARM sont influencés par le type et la gravité de l’infection.
Conclusion
Les SARM d’origine communautaire sont une cause fréquente d’infection de la peau et des tissus mous et peuvent être courants dans les populations surpeuplées et où l’accès à l’eau potable est limité.
Methicillin-resistant Staphylococcus aureus (MRSA) is recognized in the popular press as a “superbug.” Medically, it is a common bacterium that can affect clinical care in important ways. Much of what we know about MRSA has been discovered in the past 30 years. The purpose of this literature review is to describe the evolving knowledge about MRSA and its associated risk factors and epidemiology, and to provide an update on best practices for family physicians.
Quality of evidence
In MEDLINE and EMBASE (2005 to 2016), the term methicillin-resistant Staphylococcus aureus was combined with the MeSH terms abscess or synovial fluid or cerebrospinal fluid or shock, septic or bacteremia or skin diseases, bacterial or soft tissue infections or skin and soft tissue infections, and incidence.
The abstracts or titles of generated papers were read for relevance to the review topic. Additional papers were extracted from reference lists. A total of 85 relevant articles were chosen for this review. Most of the recommendations of the Infectious Diseases Society of America were based on level II or level III evidence. We have identified any level I evidence support for treatment-related findings.
Main message
Staphylococcus aureus is a common component of skin flora, and 30% to 50% of healthy adults are colonized with it at any given time.1 Preferred colonization sites include the axillae, anterior nares, pharynx, vagina, rectum, and perineum, and damaged skin.1,2 Colonization with S aureus is a commensal, asymptomatic relationship.1 Symptomatic S aureus infection is less common and might occur following breaks in skin or mucosal barriers. Its severity is influenced by isolate virulence and host factors.1,3 Diseases caused by S aureus range from superficial skin and soft tissue infections (SSTIs) to life-threatening invasive disease, including bacteremia, endocarditis, and toxic shock syndrome.1 Most S aureus infections are caused by methicillin-sensitive S aureus (MSSA), which responds to penicillin.4 Methicillin-sensitive S aureus infections predominate (75%) in tertiary care centre staphylococcal infections, while some rural hospitals report MRSA accounts for slightly more than half (56%) of staphylococcal infections.4,5 This review will concentrate on strains that are resistant to penicillin (MRSA), for which methicillin (or oxacillin) is the term used by laboratories to identify penicillin resistance.
Methicillin-resistant S aureus: 2 distinct origins
Methicillin-resistant S aureus was first identified at a hospital in the United Kingdom in 1961, shortly after the introduction of methicillin.6–9 In Canada, MRSA was first documented in 1964 and the first outbreak occurred in 1978 at the Royal Victoria Hospital in Montreal, Que.9 From the time of its emergence until the 1980s, MRSA was essentially a hospital-acquired pathogen.8 Today, these isolates of MRSA are called health care–associated MRSA (HA-MRSA) and are highly resistant to most oral antibiotics.
In the late 1980s and early 1990s cases of MRSA in young and otherwise healthy patients without any health care–related risk factors were reported.2,7,8,10 Some of the earliest reports of such infections in Canada and Australia came from isolated indigenous communities.11–14 Today, these isolates of MRSA have been identified as community-associated (previously community-acquired) MRSA (CA‑MRSA).
Community-associated MRSA and HA-MRSA can be differentiated in several ways. These include presumed location of acquisition (ie, community or hospital),15 antibiotic susceptibility pattern,16 and genotyping,17–19 the latter being the most definitive. Our review included many articles with genotyped definitions, but some smaller studies use antibiotic susceptibility patterns.
Some newer, highly resistant strains have arisen, but they are rare in Canada and are currently limited to tertiary care centres. They include vancomycin-intermediate S aureus (VISA), heterogeneous VISA, and vancomycin-resistant S aureus.20,21
Comparing CA‑MRSA and HA-MRSA.
Community-associated MRSA and HA-MRSA are genetically, epidemiologically, and phenotypically distinct (Table 1).2,4,6–8,10–15,19,22–34
Table 1.
Comparison of CA‑MRSA and HA-MRSA
| CHARACTERISTIC | CA‑MRSA | HA-MRSA |
|---|---|---|
| Time and location of emergence2,6–8,10–14,22,23 | 1980s–1990s, in the community | 1960s, in hospitals |
| Genotype2,23–27 | SCCmec types IV and V | SCCmec types I, II, and III |
| Virulence factors23,26–30 | Panton-Valentine leukocidin often present; other virulence factors believed to exist | Uncommon |
| Common subtypes19,24,25,27,29 | CMRSA-10 (USA300), CMRSA-7 (USA400) | CMRSA-2 (USA100) |
| Predominant type of infection2,7,27,28,31 | Skin and soft tissue infections | Respiratory tract, urinary tract, bloodstream, and postsurgical infections |
| Infection onset2,8,15,30,32 | Typically in the community in young, healthy individuals | Typically in hospital, often associated with older age, intensive care unit stay, and central lines |
| Antibiotic susceptibility4,27,30,33 | Susceptible to a range of antibiotics | Limited range of antibiotic susceptibility |
| Risk factors | Community risk factors25,34
|
Health care risk factors26,27
|
CA‑MRSA—community-associated methicillin-resistant Staphylococcus aureus, CMRSA—Canadian epidemic strain, HA-MRSA—health care–associated methicillin-resistant Staphylococcus aureus, SCCmec—staphylococcal chromosomal cassette mec.
Contemporary advances in laboratory technology have demonstrated that methicillin resistance was acquired through different genes in CA‑MRSA and HA-MRSA isolates. Specifically, staphylococcal chromosomal cassette mec (SCCmec) types I, II, and III confer methicillin resistance in HA-MRSA whereas SCCmec types IV and V confer methicillin resistance in CA‑MRSA.2,23–27
The SCCmec types carried by HA-MRSA are larger than those carried by CA‑MRSA and confer resistance to additional non–β-lactam antibiotics. Community-associated MRSA is therefore susceptible to a broader range of antibiotics than HA-MRSA is.4,27,30,33 A study of pathogens isolated at Canadian hospitals between 2007 and 2009 found the susceptibility of CA‑MRSA to trimethoprim-sulfamethoxazole (100.0%), gentamicin (98.7%), and clindamycin (86.1%) to be greater than that of HA-MRSA (86.5%, 85.5%, and 27.8%, respectively).4 Antibiotic sensitivity profiles can consequently be used as an inexpensive means of classifying MRSA as health care associated or community associated.16,35 For example, clindamycin susceptibility is predictive of CA‑MRSA with 95% sensitivity, 80% specificity, and a likelihood ratio of 4.86.35 Methicillin-resistant S aureus isolates that are resistant to 3 or more non–β-lactam antibiotics can safely be categorized as HA-MRSA.16
Before advances were made in laboratory genetic technologies, epidemiologic risk factors were used to differentiate cases of HA-MRSA and CA‑MRSA infection: the location of acquisition (ie, community or hospital) provided its designation.26,27 In the contemporary context, this method of differentiating HA-MRSA and CA‑MRSA no longer aligns with clinical reality, as CA‑MRSA has found its way into hospitals and is becoming an increasingly prevalent hospital pathogen.2,32 An American study found that community-associated strains of MRSA are increasing both in communities and in hospitals.15 In Canada, more than 20% of nosocomial MRSA infections are caused by CA‑MRSA.17,30 A recent study from Alberta found 27.6% of such hospital-onset MRSA infections were caused by CA‑MRSA and 27.5% of community-associated infections were caused by HA-MRSA.36 Both communities and hospitals have become antibiotic-rich environments and are apparently exchanging bacterial isolates.
There is consistent evidence that CA‑MRSA is more likely than HA-MRSA to be associated with SSTIs.2,7,9,10,12,17,19,22,23,25–28,30,31,37–44 Community-associated MRSA is more likely than HA-MRSA to carry Panton-Valentine leukocidin, a known virulence factor23,26–30 often associated with tissue necrosis SSTIs.16,23,28,31,45
Methicillin-resistant S aureus SSTIs are associated with higher mortality rates, longer hospital admissions, and greater hospital costs than SSTIs caused by MSSA strains are.31,46 The reason for this is unclear, but might involve greater virulence of MRSA relative to MSSA,46,47 or increased effectiveness of β-lactam antibiotics against MSSA.48
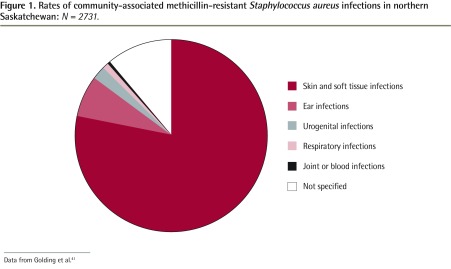
In 2012, Golding reported a high rate of CA‑MRSA infection in northern Saskatchewan (168.1 cases per 10 000 population in 2006). A compilation of 8 years of data from this region, including 2731 cases, shows that most cases (78.2%) are SSTIs, followed distantly by ear infections (6.7%), urogenital infections (2.4%), respiratory infections (1.1%), and joint or blood infections (0.4%) (Figure 1).41
Figure 1.
Rates of community-associated methicillin-resistant Staphylococcus aureus infections in northern Saskatchewan: N = 2731.
A community and hospital study done in northern Ontario documented that 56% of the burden of staphylococcal illness was caused by CA‑MRSA.5
The predominant strains of CA‑MRSA identified are Canadian epidemic strain (CMRSA) 10 (also known as USA300) and CMRSA-7 (also known as USA400). The predominant strain of HA-MRSA is CMRSA-2 (also known as USA100).19,24,25,27,29 Health care–associated MRSA is more likely to be associated with respiratory tract, urinary tract, bloodstream, and postsurgical infections.2,7,27,28,31
Risk factors
The original epidemiologic definition of HA-MRSA infection captures its principal risk factors: hospitalization, other prolonged exposure to a health care environment, or the presence of a percutaneous device such as a central line.17,26,27
Predisposing factors for CA‑MRSA infection are more varied and are intimately associated with social determinants of health.9,47 Frequent skin-to-skin contact, wound contact, and poor sanitation facilitate the transmission of CA‑MRSA.2 Crowded living environments, including military barracks, homeless shelters, subsidized housing, and prisons, are associated with increased risk of CA‑MRSA infection.10,12,23,25 A study of the relationship between in-home pressurized water service and infectious diseases among Alaska Natives found that regions with limited access to clean water had significantly higher rates of MRSA infections (rate ratio = 7.1; 95% CI 3.6 to 14.0) and hospitalization for skin infections (rate ratio = 2.7; 95% CI 1.8 to 4.1).34 Socially disadvantaged minority populations are consistently associated with higher rates of CA‑MRSA infection,47 including African Americans,40,49 Canadian First Nations communities,5,9,19,22,37,50,51 and the indigenous populations of Australia and New Zealand.16,52 Homelessness is another recognized risk factor for CA‑MRSA infection,9,10,23,26,30,32,47 as is intravenous drug use.8,17,23,27,31,32,47
Epidemiology
During the 2000s, increasing incidence rates of CA‑MRSA infections were widely reported by researchers in the United States and Canada,10,15,17,19,24,30,32,38–41,43,53,54 along with a corresponding increase in SSTIs caused by S aureus.10,19,43,52,54–58 Rates of CA‑MRSA infection are increasing, while HA-MRSA infection rates are generally reported to be in decline.19,53,57
Several studies documenting the epidemiology of MRSA in indigenous populations have been published. Studies from communities in the United States,6,34 Canada,5,19,39,41,50,51 Australia,11,16 and New Zealand 52 demonstrate high and increasing rates of CA‑MRSA infection in the indigenous populations, where HA-MRSA is rare.
In Canada, Muileboom et al found the proportion of S aureus isolates demonstrating methicillin resistance isolated from cultures obtained in one northern Ontario laboratory increased from 31% in 2008 to 56% in 2012.5 Kirlew et al reported an incidence rate of MRSA bacteremia of 41.1 cases per 100 000 person-years in northwestern Ontario.51 In northern Saskatchewan, Golding et al found that the rate of CA‑MRSA infection increased from 8.2 cases per 10 000 person-years in 2001 to 168.1 cases per 10 000 person-years in 2006.41 A previous study found that 99.5% of MRSA isolates from these remote communities were CA‑MRSA.50 A 1-year study at the Children’s Hospital of Winnipeg in Manitoba found that 79% of patients from outside of Winnipeg who presented with community-onset S aureus infection lived in rural communities in northern Manitoba, southern Nunavut, or northwestern Ontario.39 Among these patients, the rate of MRSA infection was relatively high (61%).39 A large study assessing MRSA infection rates among children across Canada between 1995 and 2007 found that 25% of all cases occurred in First Nations children.19
Like their counterparts in Canada, indigenous populations in the United States, Australia, and New Zealand face disproportionately high rates of MRSA-associated infection and hospitalization.6,11,16,52
The confluence of environmental and host factors might explain the disproportionate MRSA burden in indigenous communities. Environmental conditions associated with social and material deprivation, such as overcrowding and inadequate access to in-home pressurized water service, are associated with the transmission of MRSA and the development of MRSA-associated SSTIs.34 These same environmental conditions are pressing concerns in indigenous communities around the world.11,16,34,51 Additionally, the prevalence of host factors increasing vulnerability to infection by modulating the immune response (such as diabetes mellitus) or providing a portal of entry (skin disease, injection drug use) might be elevated in some indigenous communities.59–63
Treatment
Empiric treatment is the norm for infections and must take into consideration information about likely infecting agents, severity of illness, access to follow-up, patient adherence, and other factors. Published guidelines, original research, and knowledge of local epidemiology might assist clinicians in making clinical judgments that adhere to principles of antimicrobial stewardship.52,63–65 The current clinical practice guidelines for CA‑MRSA and HA-MRSA treatment from the Infectious Diseases Society of America recommend increasingly aggressive treatment with increased severity of infection.65
A distinction is made between purulent and nonpurulent SSTIs. Uncomplicated abscesses without evidence of systemic toxicity might be treated by incision and drainage without antibiotics (level I evidence).2,22,28,65 Evidence from 3 randomized controlled trials and a systematic review indicates not providing antibiotics to patients who undergo incision and drainage for uncomplicated abscesses is associated with lower reinfection rates and comparable wound healing (level I evidence).22,66–69 Empiric treatment of purulent cellulitis, when needed, might include oral clindamycin, trimethoprim-sulfamethoxazole, tetracyclines, or linezolid (level II evidence).65 Nonpurulent cellulitis is generally caused by Streptococcus (group A, C, or G), while purulent cellulitis is substantially more likely to be caused by S aureus, most commonly CA‑MRSA.70–73 Treatment of nonpurulent cellulitis should therefore target streptococcal species with a β-lactam antibiotic, without routine addition of an agent active against MSSA or MRSA. Most, if not all, MRSA encountered by family physicians will be CA‑MRSA, as it occurs primarily in the community context and is distinct from its highly drug-resistant relative, HA-MRSA (Table 2).65,74
Table 2.
Treatment of outpatient SSTI in the era of CA‑MRSA
| SSTI | TREATMENT* |
|---|---|
| Simple cutaneous abscess (in a low-risk patient not involving face, hands, or genitalia) | Incision and drainage alone; obtain culture |
| Purulent cellulitis (without abscess): treat for CA‑MRSA if risk factors present | Tetracycline, trimethoprim-sulfamethoxazole, or clindamycin |
| Purulent cellulitis (without abscess): treat for CA‑MRSA if risk factors present | β-Lactam antibiotic (cloxacillin or first-generation cephalosporin) |
CA‑MRSA—community-associated methicillin-resistant Staphylococcus aureus, SSTI—skin and soft tissue infection.
Complicated SSTIs and invasive MRSA infections, including bacteremia, septic arthritis, endocarditis, meningitis, and pneumonia, are typically treated with parenteral vancomycin (level I and III evidence).28,65 Susceptibility to clindamycin, trimethoprim-sulfamethoxazole, and tetracyclines is often retained in CA‑MRSA isolates4,75 and these agents can be considered in nonsevere infection or as step-down therapy. These agents have good oral bioavailability.
Alternatives to vancomycin for the treatment of severe or invasive MRSA infection include linezolid, daptomycin, and tigecycline.4,28 Newer agents recently approved or developed that have shown promise are the cephalosporins ceftaroline and ceftobiprole; the lipoglycopeptides telavancin, dalbavancin, and oritavancin; and the oxazolidinone tedizolid.75–81 Pharmacologic and clinical considerations for each antimicrobial agent are listed in Table 3. Telavancin, oritavancin, and dalbavancin might be of particular interest to community-based health care services because of their once-daily, one-time, and weekly dosing, respectively (only dalbavancin is currently available in Canada).78–80 Table 4 provides a list of additional agents active against MRSA that are not available in Canada.
Table 3.
Antibiotics relevant in the treatment of MRSA
| AGENT | ROUTE | ACTIVITY | DOSAGE FOR MRSA INFECTIONS | COMMENTS |
|---|---|---|---|---|
| Lincosamides | ||||
| • Clindamycin | Oral or IV | Bacteriostatic | 300‑450 mg orally 4 times daily or 600‑900 mg IV every 8 h | Increasing resistance among community-associated MRSA and methicillin-sensitive Staphylococcus aureus; inducible resistance in MRSA |
| Sulfonamides | ||||
| • Trimethoprim-sulfamethoxazole | Oral | Bactericidal | 1–2 double-strength tablets (160 mg and 800 mg) orally twice daily | Contraindicated in severe renal or hepatic dysfunction; multiple drug interactions (including ACEIs and ARBs) |
| Tetracyclines | ||||
| • Tetracycline | Oral | Bacteriostatic | 250–500 mg orally 4 times daily | Caution about teratogenicity |
| • Doxycycline | Oral | Bacteriostatic | 100 mg orally twice daily | Caution about teratogenicity |
| • Minocycline | Oral | Bacteriostatic | 100 mg orally twice daily | Caution about teratogenicity |
| • Tigecycline | IV | Bacteriostatic | 100-mg IV loading dose, then 50 mg IV every 12 h | Caution about teratogenicity; indicated for SSTI and intra-abdominal infections (unfavourable outcomes in community-associated pneumonia) |
| Oxazolidinones | ||||
| • Linezolid | Oral or IV | Bacteriostatic | 600 mg orally twice daily or 600 mg IV every 12 h | Indicated for SSTI; multiple drug interactions, risk of myelosuppression if used 2 wk or longer; high cost |
| Lipopeptides | ||||
| • Daptomycin | IV | Bactericidal | 4 mg/kg IV every 24 h for SSTI; 6 mg/kg IV every 24 h for bacteremia or right-sided endocarditis, up to 12 mg/kg IV every 24 h | Indicated for SSTI, endocarditis, and bloodstream infection; not indicated for pneumonia unless from hematogenous origin; might cause eosinophilic pneumonia, abnormal coagulation, myopathy, and rhabdomyolysis |
| Lipoglycopeptides | ||||
| • Vancomycin | IV | Bactericidal | 15–20 mg/kg per dose every 8–12 h; consider loading dose of 25–30 mg/kg in seriously ill patients | Dose monitoring; target levels vary with site and severity of infection |
| •Telavancin | IV | Bactericidal | 10 mg/kg IV every 24 h (if creatinine clearance > 50 mL/min) | Indicated for SSTI; increased mortality observed in chronic kidney disease |
ACEI—angiotensin-converting enzyme inhibitor, ARB—angiotensin receptor blocker, IV—intravenous, MRSA—methicillin-resistant Staphylococcus aureus, SSTI—skin and soft tissue infection.
Table 4.
Additional agents active against MRSA not available in Canada
| AGENT | ROUTE | STATUS (AT TIME OF WRITING) |
|---|---|---|
| Tedizolid | Oral or IV | Received NOC; not yet marketed |
| Ceftobiprole medocaril | IV | Received NOC; never marketed |
| Ceftaroline | IV | Not available |
| Dalbavancin | IV (weekly) | Not available |
| Oritavancin | IV (1-time dose) | Not available |
IV—intravenous, MRSA—methicillin-resistant Staphylococcus aureus, NOC—Health Canada Notice of Compliance.
Failure of vancomycin therapy has been documented in the context of resistant strains (heterogeneous VISA, vancomycin-resistant S aureus), but these are unlikely to be commonly encountered.20,22 Treatment of these infections is beyond the scope of this article.52,82
For patients colonized with MRSA, decolonization treatment can be considered under special circumstances, such as recurrent infections in an individual or household (level III evidence).22,28,65 Decolonization regimens might involve nasal administration of mupirocin, daily 4% chlorhexidine soap baths, and a course of doxycycline and rifampin (level I).22,83 Success rates are modest (< 50%) at best and largely influenced by comorbidities, and thus decolonization is not routinely recommended.3,47,84,85 It is recommended that household contacts and patients exercise good hand-washing practices. Household members should avoid sharing razors and other personal hygiene equipment; however, family bedding, clothing, and dishes can be washed together as usual. Aside from covering open wounds, there is no need to isolate persons colonized with MRSA within a household or to wear personal protective equipment when engaging with the colonized individual. However, gloves should be used when handling wounds.47
Future research directions
This is an evolving science, and there is much to learn about community spread of CA‑MRSA. As HA-MRSA primarily involves inpatients, it lends itself more easily to study. As CA‑MRSA began entering the hospital setting it now lends itself to hospital-based research. While specific clinical questions around initial drug choice and duration remain, regional population studies are needed to inform empirical treatment for the community-based clinician.
Conclusion
The prevalence of CA‑MRSA appears to be on the rise globally, and disadvantaged communities with overcrowded housing and homeless populations are disproportionally affected. Community-associated MRSA can be found in both hospitals and the community and is predominantly associated with purulent SSTIs. Treatment of endemic CA‑MRSA infections needs to be balanced with the principles of antibiotic stewardship.
EDITOR’S KEY POINTS
Isolates of methicillin-resistant Staphylococcus aureus (MRSA) that were first identified as hospital acquired are called health care–associated MRSA and are highly antibiotic resistant. Isolates of MRSA that appear in young and otherwise healthy patients are identified as community-associated (previously community-acquired) MRSA (CA‑MRSA). Neither of these bacteria exist solely in the community or in hospitals.
Empiric treatment is the norm for these typically purulent skin and soft tissue infections and includes consideration of severity of illness, access to follow-up, and patient adherence. Clinical practice guidelines for CA‑MRSA treatment recommend increasingly aggressive treatment with increased severity of infection.
Predisposing factors for CA‑MRSA infection are varied and include living in a group setting, participation in sports teams, and social determinants of health. Crowded living environments and lack of access to clean water are also associated with increased risk of CA‑MRSA infection.
POINTS DE REPÈRE DU RÉDACTEUR
Les isolats des Staphylococcus aureus résistants à la méticilline (SARM), initialement identifiés comme étant d’origine nosocomiale, sont appelés les SARM associés aux soins de santé et ont une forte résistance aux antibiotiques. Les isolats des SARM détectés chez des patients jeunes et autrement en santé sont connus sous le nom de SARM d’origine communautaire (auparavant acquis dans la communauté – SARM-AC). Ni l’une ni l’autre de ces bactéries n’existe que dans la communauté ou dans les hôpitaux.
Un traitement empirique est la norme pour ces infections de la peau et des tissus mous, typiquement purulentes; il comporte la prise en compte de la gravité de la maladie, l’accès à un suivi et l’observance du traitement par le patient. Les guides de pratique clinique concernant le traitement des SARM d’origine communautaire recommandent une thérapie proportionnelle à la sévérité de l’infection.
Parmi les divers facteurs qui prédisposent à une infection aux SARM d’origine communautaire figurent la vie en groupe, la participation à des sports d’équipe et les déterminants de la santé. La vie dans un environnement surpeuplé et le manque d’accès à de l’eau potable sont aussi associés à un risque accru d’infection aux SARM d’origine communautaire.
Footnotes
This article has been peer reviewed.
Contributors
All authors contributed to the literature review and interpretation, and to preparing the manuscript for submission.
Competing interests
None declared
References
- 1.Lowy FD. Staphylococcus aureus infections. N Engl J Med. 1998;339(8):520–32. doi: 10.1056/NEJM199808203390806. [DOI] [PubMed] [Google Scholar]
- 2.NeVille-Swensen M, Clayton M. Outpatient management of community-associated methicillin-resistant Staphylococcus aureus skin and soft tissue infections. J Pediatr Health Care. 2011;25(5):308–15. doi: 10.1016/j.pedhc.2010.05.005. Epub 2010 Jul 17. [DOI] [PubMed] [Google Scholar]
- 3.Jiménez-Truque N, Saye EJ, Soper N, Saville BR, Thomsen I, Edwards KM, et al. Longitudinal assessment of colonization with Staphylococcus aureus in healthy collegiate athletes. J Pediatric Infect Dis Soc. 2016;5(2):105–13. doi: 10.1093/jpids/piu108. Epub 2014 Nov 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhanel GG, Adam HJ, Low DE, Blondeau J, DeCorby M, Karlowsky JA, et al. Antimicrobial susceptibility of 15,644 pathogens from Canadian hospitals: results of the CANWARD 2007–2009 study. Diagn Microbiol Infect Dis. 2011;69(3):291–306. doi: 10.1016/j.diagmicrobio.2010.10.025. [DOI] [PubMed] [Google Scholar]
- 5.Muileboom J, Hamilton M, Parent K, Makahnouk D, Kirlew M, Saginur R, et al. Community-associated methicillin-resistant Staphylococcus aureus in northwest Ontario: a five-year report of incidence and antibiotic resistance. Can J Infect Dis Med Microbiol. 2013;24(2):e42–4. doi: 10.1155/2013/169409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Byrd KK, Holman RC, Bruce MG, Hennessy TW, Wenger JD, Bruden DL, et al. Methicillin-resistant Staphylococcus aureus–associated hospitalizations among the American Indian and Alaska Native population. Clin Infect Dis. 2009;49(7):1009–15. doi: 10.1086/605560. [DOI] [PubMed] [Google Scholar]
- 7.Peebles E, Morris R, Chafe R. Community-associated methicillin-resistant Staphylococcus aureus in a pediatric emergency department in Newfoundland and Labrador. Can J Infect Dis Med Microbiol. 2014;25(1):13–6. doi: 10.1155/2014/267901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stenstrom R, Grafstein E, Romney M, Fahimi J, Harris D, Hunte G, et al. Prevalence of and risk factors for methicillin-resistant Staphylococcus aureus skin and soft tissue infection in a Canadian emergency department. CJEM. 2009;11(5):430–8. doi: 10.1017/s1481803500011623. Erratum in: CJEM 2009;11(6):570. [DOI] [PubMed] [Google Scholar]
- 9.Cimolai N. Methicillin-resistant Staphylococcus aureus in Canada: a historical perspective and lessons learned. Can J Microbiol. 2010;56(2):89–120. doi: 10.1139/w09-109. [DOI] [PubMed] [Google Scholar]
- 10.Meddles-Torres C, Hu S, Jurgens C. Changes in prescriptive practices in skin and soft tissue infections associated with the increased occurrence of community acquired methicillin resistant Staphylococcus aureus. J Infect Public Health. 2013;6(6):423–30. doi: 10.1016/j.jiph.2013.04.010. Epub 2013 Jun 15. [DOI] [PubMed] [Google Scholar]
- 11.Tong SY, Varrone L, Chatfield MD, Beaman M, Giffard PM. Progressive increase in community-associated methicillin-resistant Staphylococcus aureus in indigenous populations in northern Australia from 1993 to 2012. Epidemiol Infect. 2015;143(7):1519–23. doi: 10.1017/S0950268814002611. Epub 2014 Oct 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vayalumkal JV, Suh KN, Toye B, Ramotar K, Saginur R, Roth VR. Skin and soft tissue infections caused by methicillin-resistant Staphylococcus aureus (MRSA): an affliction of the underclass. CJEM. 2012;14(6):335–43. [PubMed] [Google Scholar]
- 13.Udo EE, Pearman JW, Grubb WB. Genetic analysis of community isolates of methicillin-resistant Staphylococcus aureus in western Australia. J Hosp Infect. 1993;25(2):97–108. doi: 10.1016/0195-6701(93)90100-e. [DOI] [PubMed] [Google Scholar]
- 14.Taylor G, Kirkland T, Kowalewska-Grochowska K, Wang Y. A multistrain cluster of methicillin-resistant Staphylococcus aureus based in a native community. Can J Infect Dis. 1990;1(4):121–6. doi: 10.1155/1990/618630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hadler JL, Petit S, Mandour M, Cartter ML. Trends in invasive infection with methicillin-resistant Staphylococcus aureus, Connecticut, USA, 2001–2010. Emerg Infect Dis. 2012;18(6):917–24. doi: 10.3201/eid1806.120182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tong SY, Bishop EJ, Lilliebridge RA, Cheng AC, Spasova-Penkova Z, Holt DC, et al. Community-associated strains of methicillin-resistant Staphylococcus aureus and methicillin-susceptible S. aureus in indigenous northern Australia: epidemiology and outcomes. J Infect Dis. 2009;199(10):1461–70. doi: 10.1086/598218. [DOI] [PubMed] [Google Scholar]
- 17.Lévesque S, Bourgault AM, Galarneau LA, Moisan D, Doualla-Bell F, Tremblay C. Molecular epidemiology and antimicrobial susceptibility profiles of methicillin-resistant Staphylococcus aureus blood culture isolates: results of the Quebec Provincial Surveillance Programme. Epidemiol Infect. 2015;143(7):1511–8. doi: 10.1017/S095026881400209X. Epub 2014 Aug 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ponce-de-Léon A, Camacho-Ortiz A, Macías AE, Landín-Larios C, Villanueva-Walbey C, Trinidad-Guerrero D, et al. Epidemiology and clinical characteristics of Staphylococcus aureus bloodstream infections in a tertiary-care center in Mexico City: 2003–2007. Rev Invest Clin. 2010;62(6):553–9. [PubMed] [Google Scholar]
- 19.Matlow A, Forgie S, Pelude L, Embree J, Gravel D, Langley JM, et al. National surveillance of methicillin-resistant Staphylococcus aureus among hospitalized pediatric patients in Canadian acute care facilities, 1995–2007. Pediatr Infect Dis J. 2012;31(8):814–20. doi: 10.1097/INF.0b013e31825c48a0. [DOI] [PubMed] [Google Scholar]
- 20.Zhang S, Sun X, Chang W, Dai Y, Ma X. Systematic review and meta-analysis of the epidemiology of vancomycin-intermediate and heterogeneous vancomycin-intermediate Staphylococcus aureus isolates. PLoS One. 2015;10(8):e0136082. doi: 10.1371/journal.pone.0136082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Holmes NE, Johnson PDR, Howden BP. Relationship between vancomycin-resistant Staphylococcus aureus, vancomycin-intermediate S. aureus, high vancomycin MIC, and outcome in serious S. aureus infections. J Clin Microbiol. 2012;50(8):2548–52. doi: 10.1128/JCM.00775-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Muileboom J, Hamilton M, Kelly L. The changing face of cellulitis and MRSA in rural Canada: a clinical update. Can J Rural Med. 2013;18(4):137–9. [PubMed] [Google Scholar]
- 23.Harrison B, Ben-Amotz O, Sammer DM. Methicillin-resistant Staphylococcus aureus infection of the hand. Plast Reconstr Surg. 2015;135(3):826–30. doi: 10.1097/PRS.0000000000000952. [DOI] [PubMed] [Google Scholar]
- 24.Nichol KA, Adam HJ, Hussain Z, Mulvey MR, McCracken M, Mataseje LF, et al. Comparison of community-associated and health care-associated methicillin-resistant Staphylococcus aureus in Canada: results of the CANWARD 2007–2009 study. Diagn Microbiol Infect Dis. 2011;69(3):320–5. doi: 10.1016/j.diagmicrobio.2010.10.028. [DOI] [PubMed] [Google Scholar]
- 25.Borgundvaag B, Ng W, Rowe B, Katz K, Emergency Department Emerging Infectious Disease Surveillance Network (EMERGENT) Working Group Prevalence of methicillin-resistant Staphylococcus aureus in skin and soft tissue infections in patients presenting to Canadian emergency departments. CJEM. 2013;15(3):141–60. [PubMed] [Google Scholar]
- 26.Achiam CC, Fernandes CM, McLeod SL, Salvadori MI, John M, Seabrook JA, et al. Methicillin-resistant Staphylococcus aureus in skin and soft tissue infections presenting to the emergency department of a Canadian academic health care center. Eur J Emerg Med. 2011;18(1):2–8. doi: 10.1097/MEJ.0b013e328337901a. [DOI] [PubMed] [Google Scholar]
- 27.Al-Rawahi G, Reynolds S, Porter SD, Forrester L, Kishi L, Chong T, et al. Community-associated CMRSA-10 (USA-300) is the predominant strain among methicillin-resistant Staphylococcus aureus strains causing skin and soft tissue infections in patients presenting to the emergency department of a Canadian tertiary care hospital. J Emerg Med. 2010;38(1):6–11. doi: 10.1016/j.jemermed.2007.09.030. Epub 2008 Mar 6. [DOI] [PubMed] [Google Scholar]
- 28.Abrahamian F, Snyder EW. Community-associated methicillin-resistant Staphylococcus aureus: incidence, clinical presentation, and treatment decisions. Curr Infect Dis Rep. 2007;9(5):391–7. doi: 10.1007/s11908-007-0061-9. [DOI] [PubMed] [Google Scholar]
- 29.Adam HJ, Allen VG, Currie A, McGeer AJ, Simor AE, Richardson SE, et al. Community-associated methicillin-resistant Staphylococcus aureus: prevalence in skin and soft tissue infections at emergency departments in the greater Toronto area and associated risk factors. CJEM. 2009;11(5):439–46. doi: 10.1017/s1481803500011635. [DOI] [PubMed] [Google Scholar]
- 30.Nichol KA, Adam HJ, Roscoe DL, Golding GR, Lagacé-Wiens PR, Hoban DJ, et al. Changing epidemiology of methicillin-resistant Staphylococcus aureus in Canada. J Antimicrob Chemother. 2013;68(Suppl 1):i47–55. doi: 10.1093/jac/dkt026. [DOI] [PubMed] [Google Scholar]
- 31.Dryden M. Complicated skin and soft tissue infections caused by methicillin-resistant Staphylococcus aureus: epidemiology, risk factors, and presentation. Surg Infect (Larchmt) 2008;9(Suppl 1):s3–10. doi: 10.1089/sur.2008.066.supp. [DOI] [PubMed] [Google Scholar]
- 32.Kim J, Ferrato C, Golding GR, Mulvey MR, Simmonds KA, Svenson LW, et al. Changing epidemiology of methicillin-resistant Staphylococcus aureus in Alberta, Canada: population-based surveillance, 2005–2008. Epidemiol Infect. 2011;139(7):1009–18. doi: 10.1017/S0950268810002128. Epub 2010 Sep 21. [DOI] [PubMed] [Google Scholar]
- 33.Simor AE, Louie L, Watt C, Gravel D, Mulvey MR, Campbell J, et al. Antimicrobial susceptibilities of health care-associated and community-associated strains of methicillin-resistant Staphylococcus aureus from hospitalized patients in Canada, 1995 to 2008. Antimicrob Agents Chemother. 2010;54(5):2265–8. doi: 10.1128/AAC.01717-09. Epub 2010 Mar 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hennessy TW, Ritter T, Holman RC, Bruden DL, Yorita KL, Bulkow L, et al. The relationship between in-home water service and the risk of respiratory tract, skin, and gastrointestinal tract infections among rural Alaska Natives. Am J Public Health. 2008;98(11):2072–8. doi: 10.2105/AJPH.2007.115618. Epub 2008 Apr 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Popovich K, Hota B, Rice T, Aroutcheva A, Weinstein RA. Phenotypic prediction rule for community-associated methicillin-resistant Staphylococcus aureus. J Clin Microbiol. 2007;45(7):2293–5. doi: 10.1128/JCM.00044-07. Epub 2007 May 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Taylor G, Bush K, Leal J, Henderson E, Chui L, Louie M. Epidemiology of methicillin-resistant Staphylococcus aureus bloodstream infections in Alberta, Canada. J Hosp Infect. 2015;89(2):132–5. doi: 10.1016/j.jhin.2014.11.008. Epub 2014 Dec 16. [DOI] [PubMed] [Google Scholar]
- 37.Irvine J, Canadian Paediatric Society, First Nations, Inuit and Métis Health Committee Community-associated methicillin-resistant Staphylococcus aureus in indigenous communities in Canada. Paediatr Child Health. 2012;17(7):395–8. [PMC free article] [PubMed] [Google Scholar]
- 38.Casey JA, Cosgrove SE, Stewart WF, Pollak J, Schwartz BS. A population-based study of the epidemiology and clinical features of methicillin-resistant Staphylococcus aureus infection in Pennsylvania, 2001–2010. Epidemiol Infect. 2013;141(6):1166–79. doi: 10.1017/S0950268812001872. Epub 2013 Apr 23. Erratum in: Epidemiol Infect 2013;141(6):1180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fanella S, Embree J. Pediatric Staphylococcus aureus infections: impact of methicillin resistance at a Canadian center. South Med J. 2015;108(5):254–7. doi: 10.14423/SMJ.0000000000000274. [DOI] [PubMed] [Google Scholar]
- 40.Gerber JS, Coffin SE, Smathers SA, Zaoutis TE. Trends in the incidence of methicillin-resistant Staphylococcus aureus infection in children’s hospitals in the United States. Clin Infect Dis. 2009;49(1):65–71. doi: 10.1086/599348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Golding GR, Quinn B, Bergsrom K, Stockdale D, Woods S, Nsungu M, et al. Community-based educational intervention to limit the dissemination of community-associated methicillin-resistant Staphylococcus aureus in northern Saskatchewan, Canada. BMC Public Health. 2012;12:15. doi: 10.1186/1471-2458-12-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hassan S, Gashau W, Balchin L, Orange G, Wilmshurst A. Incidence of community-acquired methicillin resistant Staphylococcus aureus hand infections in Tayside, Scotland: a guide to appropriate antimicrobial prescribing. J Hand Surg Eur. 2011;36(3):226–9. doi: 10.1177/1753193410394520. Epub 2010 Dec 17. [DOI] [PubMed] [Google Scholar]
- 43.May AK. Skin and soft tissue infections: the new Surgical Infection Society guidelines. Surg Infect (Larchmt) 2011;12(3):179–84. doi: 10.1089/sur.2011.034. Epub 2011 Jul 18. [DOI] [PubMed] [Google Scholar]
- 44.Leifso KR, Gravel D, Mounchili A, Kaldas S, Le Saux N. Clinical characteristics of pediatric patients hospitalized with methicillin-resistant Staphylococcus aureus in Canadian hospitals from 2008 to 2010. Can J Infect Dis Med Microbiol. 2013;24(3):e53–6. doi: 10.1155/2013/627871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hota B, Lyles R, Rim J, Popovich KJ, Rice T, Aroutcheva A, et al. Predictors of clinical virulence in community-onset methicillin-resistant Staphylococcus aureus infections: the importance of USA300 and pneumonia. Clin Infect Dis. 2011;53(8):757–65. doi: 10.1093/cid/cir472. Epub 2011 Aug 31. [DOI] [PubMed] [Google Scholar]
- 46.Kaye KS, Engemann JJ, Mozaffari E, Carmeli Y. Reference group choice and antibiotic resistance outcomes. Emerg Infect Dis. 2004;10(6):1125–8. doi: 10.3201/eid1006.020665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.David MZ, Daum RS. Community-associated methicillin-resistant Staphylococcus aureus: epidemiology and clinical consequences of an emerging epidemic. Clin Microbiol Rev. 2010;23(3):616–87. doi: 10.1128/CMR.00081-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Engemann JJ, Carmeli Y, Cosgrove SE, Fowler VG, Bronstein MZ, Trivette SL, et al. Adverse clinical and economic outcomes attributable to methicillin resistance among patients with Staphylococcus aureus surgical site infection. Clin Infect Dis. 2003;36(5):592–8. doi: 10.1086/367653. Epub 2003 Feb 7. [DOI] [PubMed] [Google Scholar]
- 49.Ray GT, Suaya JA, Baxter R. Incidence, microbiology, and patient characteristics of skin and soft-tissue infections in a U.S. population: a retrospective population-based study. BMC Infect Dis. 2013;13:252. doi: 10.1186/1471-2334-13-252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Golding GR, Levett PN, McDonald RR, Irvine J, Quinn B, Nsungu M, et al. High rates of Staphylococcus aureus USA400 infection, northern Canada. Emerg Infect Dis. 2011;17(4):722–5. doi: 10.3201/eid1704.100482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kirlew M, Rea S, Schroeter A, Makahnouk D, Hamilton M, Brunton N, et al. Invasive CA‑MRSA in northwestern Ontario: a 2-year prospective study. Can J Rural Med. 2014;19(3):99–102. [PubMed] [Google Scholar]
- 52.Williamson DA, Ritchie SR, Lennon D, Roberts SA, Stewart J, Thomas MG, et al. Increasing incidence and socioeconomic variation in community-onset Staphylococcus aureus skin and soft tissue infections in New Zealand children. Pediatr Infect Dis J. 2013;32(8):923–5. doi: 10.1097/INF.0b013e3182905f3d. [DOI] [PubMed] [Google Scholar]
- 53.David MZ, Daum RS, Bayer AS, Chambers HF, Fowler VG, Jr, Miller LG, et al. Staphylococcus aureus bacteremia at 5 US academic medical centers, 2008–2011: significant geographic variation in community-onset infections. Clin Infect Dis. 2014;59(6):798–807. doi: 10.1093/cid/ciu410. Epub 2014 May 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Karamatsu ML, Thorp AW, Brown L. Changes in community-associated methicillin-resistant Staphylococcus aureus skin and soft tissue infections presenting to the pediatric emergency department: comparing 2003 to 2008. Pediatr Emerg Care. 2012;28(2):131–5. doi: 10.1097/PEC.0b013e318243fa36. [DOI] [PubMed] [Google Scholar]
- 55.Suaya JA, Mera RM, Cassidy A, O’Hara P, Amrine-Madsen H, Burstin S, et al. Incidence and cost of hospitalizations associated with Staphylococcus aureus skin and soft tissue infections in the United States from 2001 through 2009. BMC Infect Dis. 2014;14:296. doi: 10.1186/1471-2334-14-296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Miller LG, Eisenberg DF, Liu H, Chang CL, Wang Y, Luthra R, et al. Incidence of skin and soft tissue infections in ambulatory and inpatient settings, 2005–2010. BMC Infect Dis. 2015;15:362. doi: 10.1186/s12879-015-1071-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Khatib R, Sharma M, Iyer S, Fakih MG, Obeid KM, Venugopal A, et al. Decreasing incidence of Staphylococcus aureus bacteremia over 9 years: greatest decline in community-associated methicillin-susceptible and hospital-acquired methicillin-resistant isolates. Am J Infect Control. 2013;41(3):210–3. doi: 10.1016/j.ajic.2012.03.038. Epub 2012 Oct 4. [DOI] [PubMed] [Google Scholar]
- 58.Song X, Cogen J, Singh N. Incidence of methicillin-resistant Staphylococcus aureus infection in a children’s hospital in the Washington metropolitan area of the United States, 2003–2010. Emerg Microbes Infect. 2013;2(10):e69. doi: 10.1038/emi.2013.69. Epub 2013 Oct 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Canadian Diabetes Association Clinical Practice Guidelines Expert Committee. Harris SB, Bhattacharyya O, Dyck R, Hayward MN, Toth EL. Type 2 diabetes in aboriginal peoples. Can J Diabetes. 2013;37(Suppl 1):S191–6. doi: 10.1016/j.jcjd.2013.01.046. Epub 2013 Mar 26. [DOI] [PubMed] [Google Scholar]
- 60.Kelly L, Guilfoyle J, Dooley J, Antone I, Gerber-Finn L, Dooley R, et al. Incidence of narcotic abuse during pregnancy in northwestern Ontario. Three-year prospective cohort study. Can Fam Physician. 2014;60:e493–8. Available from: www.cfp.ca/content/cfp/60/10/e493.full.pdf. Accessed 2017 May 1. [PMC free article] [PubMed] [Google Scholar]
- 61.Balfour-Boehm J, Rea S, Gordon J, Dooley J, Kelly L, Robinson A. The evolving nature of narcotic use in northwestern Ontario. Can J Rural Med. 2014;19(4):158–60. [PubMed] [Google Scholar]
- 62.Kearns TM, Speare R, Cheng AC, McCarthy J, Carapetis JR, Holt DC, et al. Impact of ivermectin mass drug administration on scabies prevalence in a remote Australian aboriginal community. PLoS Negl Trop Dis. 2015;9(10):e0004151. doi: 10.1371/journal.pntd.0004151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Jenkins TC, Knepper BC, Moore SJ, Saveli CC, Pawlowski SW, Perlman DM, et al. Microbiology and initial antibiotic therapy for injection drug users and non-injection drug users with cutaneous abscesses in the era of community-associated methicillin-resistant Staphylococcus aureus. Acad Emerg Med. 2015;22(8):993–7. doi: 10.1111/acem.12727. Epub 2015 Jul 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Tosas Auguet O, Betley JR, Stabler RA, Patel A, Ioannou A, Marbach H, et al. Evidence for community transmission of community-associated but not health-care-associated methicillin-resistant Staphylococcus aureus strains linked to social and material deprivation: spatial analysis of cross-sectional data. PLoS Med. 2016;13(1):e1001944. doi: 10.1371/journal.pmed.1001944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Liu C, Bayer A, Cosgrove SE, Daum RS, Fridkin SK, Gorwitz RJ, et al. Clinical practice guidelines by the Infectious Diseases Society of America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children. Clin Infect Dis. 2011;52(3):e18–55. doi: 10.1093/cid/ciq146. Epub 2011 Jan 4. Erratum in: Clin Infect Dis 2011;53(3):319. [DOI] [PubMed] [Google Scholar]
- 66.Rajendran PM, Young D, Maurer T, Chambers H, Perdreau-Remington F, Ro P, et al. Randomized, double-blind, placebo-controlled trial of cephalexin for treatment of uncomplicated skin abscesses in a population at risk for community-acquired methicillin-resistant Staphylococcus aureus infection. Antimicrob Agents Chemother. 2007;51(11):4044–8. doi: 10.1128/AAC.00377-07. Epub 2007 Sep 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Schmitz G, Bruner D, Pitotti R, Olderog C, Livengood T, Williams J, et al. Randomized controlled trial of trimethoprim-sulfamethoxazole for uncomplicated skin abscesses in patients at risk for community-associated methicillin-resistant Staphylococcus aureus. Ann Emerg Med. 2010;56(3):283–7. doi: 10.1016/j.annemergmed.2010.03.002. Epub 2010 Mar 26. Erratum in: Ann Emerg Med 2010;56(5):588. [DOI] [PubMed] [Google Scholar]
- 68.Duong M, Markwell S, Peter J, Barenkamp S. Randomized controlled trial of antibiotics in the management of community-acquired skin abscesses in the pediatric patient. Ann Emerg Med. 2010;55(5):401–7. doi: 10.1016/j.annemergmed.2009.03.014. Epub 2009 May 5. [DOI] [PubMed] [Google Scholar]
- 69.Forcade NA, Wiederhold NP, Ryan L, Talbert RL, Frei CR. Antibacterials as adjunct to incision and drainage for adults with purulent methicillin-resistant Staphylococcus aureus (MRSA) skin infections. Drugs. 2012;72(3):339–51. doi: 10.2165/11599510-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 70.Jenkins TC, Knepper BC, Sabel AL. Decreased antibiotic utilization after implementation of a guideline for inpatient cellulitis and cutaneous abscess. Arch Intern Med. 2011;171(12):1072–9. doi: 10.1001/archinternmed.2011.29. [DOI] [PubMed] [Google Scholar]
- 71.Jeng A, Beheshti M, Li J, Nathan R. The role of beta-hemolytic streptococci in causing diffuse, nonculturable cellulitis: a prospective investigation. Medicine (Baltimore) 2010;89(4):217–26. doi: 10.1097/MD.0b013e3181e8d635. [DOI] [PubMed] [Google Scholar]
- 72.Moran GJ, Krishnadasan A, Gorwitz RJ, Fosheim GE, McDougal LK, Carey RB, et al. Methicillin-resistant S. aureus infections among patients in the emergency department. N Engl J Med. 2006;355(7):666–74. doi: 10.1056/NEJMoa055356. [DOI] [PubMed] [Google Scholar]
- 73.Talan DA, Krishnadasan A, Gorwitz RJ, Fosheim GE, Limbago B, Albrecht V, et al. Comparison of Staphylococcus aureus from skin and soft-tissue infections in US emergency department patients, 2004 and 2008. Clin Infect Dis. 2011;53(2):144–9. doi: 10.1093/cid/cir308. [DOI] [PubMed] [Google Scholar]
- 74.Stevens D, Bisno A, Chambers H, Patchen Dellinger E, Goldstein E, Gorbach S, et al. Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America. Clin Infect Dis. 2014;59(2):147–59. doi: 10.1093/cid/ciu296. Epub 2014 Jun 18. [DOI] [PubMed] [Google Scholar]
- 75.Cavalcante F, Schuenck RP, Caboclo RM, de Carvalho Ferreira D, Nouér SA, Santos KR. Tetracycline and trimethoprim/sulfamethoxazole at clinical laboratory: can they help to characterize Staphylococcus aureus carrying different SCCmec types? Rev Soc Bras Med Trop. 2013;46(1):100–2. [PubMed] [Google Scholar]
- 76.Saravolatz LD, Stein GE, Johnson LB. Ceftaroline: a novel cephalosporin with activity against methicillin-resistant Staphylococcus aureus. Clin Infect Dis. 2011;52(9):1156–63. doi: 10.1093/cid/cir147. [DOI] [PubMed] [Google Scholar]
- 77.Lodise TP, Low DE. Ceftaroline fosamil in the treatment of community-acquired bacterial pneumonia and acute bacterial skin and skin structure infections. Drugs. 2012;72(11):1473–93. doi: 10.2165/11635660-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 78.Corey GR, Good S, Jiang H, Moeck G, Wikler M, Green S, et al. Single-dose oritavancin versus 7–10 days of vancomycin in the treatment of Gram-positive acute bacterial skin and skin structure infections: the SOLO II noninferiority study. Clin Infect Dis. 2015;60(2):254–62. doi: 10.1093/cid/ciu778. Epub 2014 Oct 6. [DOI] [PubMed] [Google Scholar]
- 79.Cardona AF, Wilson SE. Skin and soft tissue infections: a critical review and the role of telavancin in their treatment. Clin Infect Dis. 2015;61(Suppl 2):S69–78. doi: 10.1093/cid/civ528. [DOI] [PubMed] [Google Scholar]
- 80.Chen AY, Zervos MJ, Vazquez JA. Dalbavancin: a novel antimicrobial. Int J Clin Pract. 2007;61(5):853–63. doi: 10.1111/j.1742-1241.2007.01318.x. Epub 2007 Mar 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Wong E, Rab S. Tedizolid phosphate (Sivextro): a second-generation oxazolidinone to treat acute bacterial skin and skin structure infections. P T. 2014;39(8):555–79. [PMC free article] [PubMed] [Google Scholar]
- 82.Brink AJ. Does resistance in severe infections caused by methicillin-resistant Staphylococcus aureus give you the ‘creeps’? Curr Opin Crit Care. 2012;18(5):451–9. doi: 10.1097/MCC.0b013e3283578968. [DOI] [PubMed] [Google Scholar]
- 83.Jennings JE, Timm NL, Duma EM. Methicillin-resistant Staphylococcus aureus: decolonization and prevention prescribing practices for children treated with skin abscesses/boils in a pediatric emergency department. Pediatr Emerg Care. 2015;31(4):266–8. doi: 10.1097/PEC.0000000000000377. [DOI] [PubMed] [Google Scholar]
- 84.Schmid H, Romanos A, Schiffl H, Lederer SR. Persistent nasal methicillin-resistant Staphylococcus aureus carriage in hemodialysis outpatients: a predictor of worse outcome. BMC Nephrol. 2013;14:93. doi: 10.1186/1471-2369-14-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Baratz MD, Hallmark R, Odum SM, Springer BD. Twenty percent of patients may remain colonized with methicillin-resistant Staphylococcus aureus despite a decolonization protocol in patients undergoing total joint arthroplasty. Clin Orthop Relat Res. 2015;473(7):2283–90. doi: 10.1007/s11999-015-4191-3. [DOI] [PMC free article] [PubMed] [Google Scholar]