Abstract
Objective:
Human immunodeficiency virus (HIV) partner services are an integral part of comprehensive HIV prevention programs. We examined the patterns of HIV testing and positivity among partners of HIV-diagnosed people who participated in partner services programs in CDC-funded state and local health departments.
Methods:
We analyzed data on 21 484 partners submitted in 2013-2014 by 55 health departments. We conducted descriptive and multivariate analyses to examine patterns of HIV testing and positivity by demographic characteristics and geographic region.
Results:
Of 21 484 partners, 16 275 (75.8%) were tested for HIV; 4503 of 12 886 (34.9%) partners with test results were identified as newly HIV-positive. Compared with partners aged 13-24, partners aged 35-44 were less likely to be tested for HIV (adjusted odds ratio [aOR] = 0.86; 95% confidence interval [CI], 0.78-0.95) and more likely to be HIV-positive (aOR = 1.35; 95% CI, 1.20-1.52). Partners who were male (aOR = 0.89; 95% CI, 0.81-0.97) and non-Hispanic black (aOR = 0.68; 95% CI, 0.63-0.74) were less likely to be tested but more likely to be HIV-positive (male aOR = 1.81; 95% CI, 1.64-2.01; non-Hispanic black aOR = 1.52; 95% CI, 1.38-1.66) than partners who were female and non-Hispanic white, respectively. Partners in the South were more likely than partners in the Midwest to be tested for HIV (aOR = 1.56; 95% CI, 1.35-1.80) and to be HIV-positive (aOR = 2.18; 95% CI, 1.81-2.65).
Conclusions:
Partner services programs implemented by CDC-funded health departments are successful in providing HIV testing services and identifying previously undiagnosed HIV infections among partners of HIV-diagnosed people. Demographic and regional differences suggest the need to tailor these programs to address unique needs of the target populations.
Keywords: partner services programs, HIV testing, HIV positivity, partners
An estimated 1.2 million people in the United States are living with human immunodeficiency virus (HIV) infection, 13% of whom are unaware of their infection.1,2 Advances in treatment and care since the late 1990s have decreased the mortality rate of those infected with HIV, which has increased the overall prevalence of people living with HIV or AIDS. Prevention efforts have helped stabilize the rate of new infections, but approximately 40 000 people continue to be newly diagnosed with HIV infection each year,3 highlighting the need for prevention, care, and treatment efforts.
Sexual and/or needle-sharing partners (hereinafter referred to as partners) of HIV-infected people who are not virally suppressed are at the greatest risk for acquiring HIV infection. The National HIV/AIDS Strategy (NHAS) recommends that partner services be provided to all people with diagnosed HIV infection as part of a comprehensive HIV prevention program.4,5 As part of its High-Impact HIV Prevention approach,6 CDC considers partner services a cost-effective prevention strategy and funds state and local health departments to implement HIV partner services. Partner services include an array of prevention activities offered to people with HIV and their partners to help reduce the spread of infection. The primary goals of partner services are to (1) interview HIV-diagnosed people (hereinafter referred to as index patients) and identify their partners, (2) notify partners of their potential HIV exposure and offer HIV testing, and (3) link HIV-positive partners to HIV medical services. In 2008, CDC published the revised recommendations for partner services implementation based on the 1998 HIV Partner Counseling and Referral Services Guide and the 2001 Program Operations Guidelines for STD Prevention7,8 that encouraged the coordination of prevention activities for HIV, syphilis, gonorrhea, and chlamydia.9
HIV partner services are an efficient approach to reach people at risk for HIV, identify undiagnosed infections,10,11 and provide a cost-effective HIV prevention and control strategy.12 For example, a study by the San Francisco Department of Public Health partner services program using data from 2005-2011 showed HIV testing rates among partners ranging from 27.4% to 44.9% and an HIV positivity rate ranging from 13.2% to 50.0%, with an overall positivity rate of 28.3%.13 Similarly, a study by the New York City Department of Health and Mental Hygiene found that 61% of notified partners were tested for HIV, and 13% of those tested were newly diagnosed with HIV infection.14 A systematic review of 9 studies that examined the effectiveness of provider notifications found that 63% of notified partners were tested for HIV, and 20% of partners had previously undiagnosed HIV infection (range, 14%-26%).11
Health departments play a key role in partner services. Partner notification by the health department, instead of by the index patients themselves, is the most effective way to inform partners of their exposure to infection.15–19 One study in New York City showed that disease intervention specialists were more successful than were clinicians at notifying partners (70.9% vs 48.3%).20 Another study showed that when public health workers spend time counseling index patients about the importance of notifying partners, the partners are more likely to be notified.21 Yet one more study showed that index patients who received HIV partner services were more likely to initiate medical care within 3 months of diagnosis and retain in medical care than those who were not engaged in partner services programs.22
The wide range of HIV testing rates from the various partner services programs may reflect the availability of resources and the maturity of the partner services programs, along with accessibility of HIV testing services. Similarly, various factors contribute to HIV positivity rates among partners of index patients.23–27 For example, differences in HIV positivity rates of tested partners from partner services programs may be attributed to a community’s HIV prevalence and the implementation and accessibility of HIV prevention programs. Biomedical factors that are associated with the likelihood of HIV positivity of partners include the viral load and antiretroviral treatment status of the index patient, whether one or both partners have a sexually transmitted disease coinfection, and whether one or both people inject drugs.28–32
Limited information about the patterns of HIV testing and positivity among partners is available at the national level. This study examined the demographic and regional patterns of HIV testing and positivity among partners of index patients using client-level data from partner services programs in CDC-funded state and local health departments.
Methods
Data Source and Analytical Sample
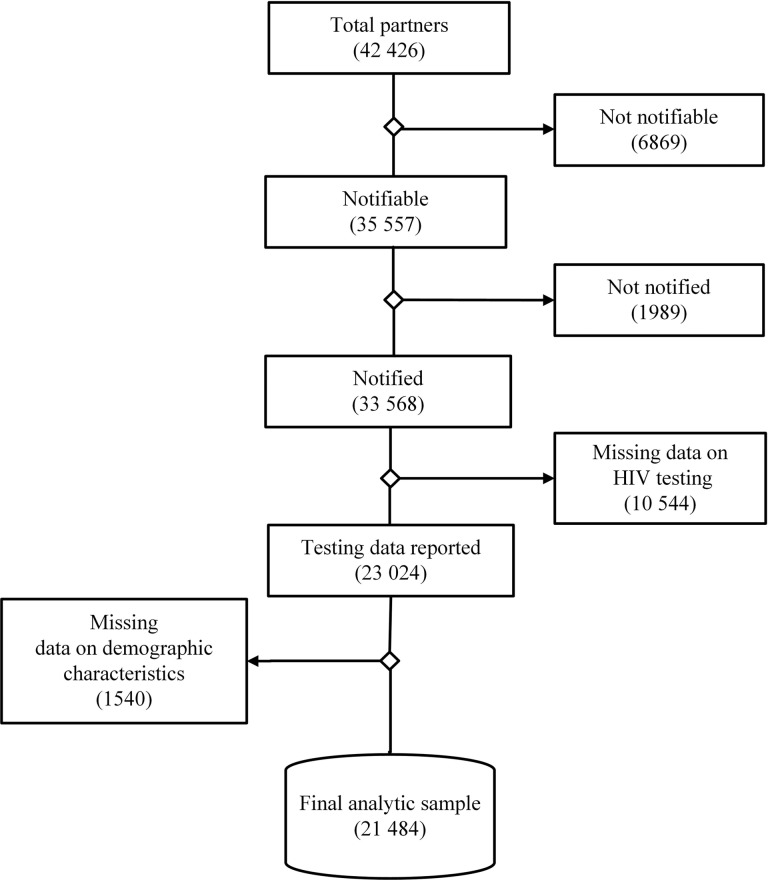
CDC provides funds to 61 health departments (50 state health departments and 11 local and city health departments) to implement comprehensive HIV prevention programs, including partner services. We focused on the 55 health departments that successfully reported data in 2013 and 2014 through CDC’s National HIV Prevention Program Monitoring and Evaluation system. We examined client-level data collected from 42 426 partners who were identified during this period through partner services programs, including those named by index patients (primary partners) and the partners of HIV-positive partners (secondary partners). Of these, 35 557 (83.8%) were deemed notifiable after excluding those who were deceased, were out of jurisdiction, had a risk for domestic violence, or were previously reported as HIV-positive. Among them, 33 568 (94.4%) were notified of their potential HIV exposure. HIV testing data were reported for 23 024 (68.6%) notified partners; of these, 1540 (6.7%) had missing data on demographic characteristics. The final analytic sample consisted of 21 484 partners from 55 jurisdictions with valid data on HIV testing, demographic characteristics, and geographic region (Figure). Because data collection for this effort was determined to be a program evaluation activity and classified as not human subjects research by CDC, institutional review board approval was not required.
Figure.
Flowchart describing analytical sample of partners from 55 partner services programs in the United States, 2013-2014. Abbreviation: HIV, human immunodeficiency virus.
Variables Analyzed
The outcomes of interest were HIV testing status (ie, whether the partners were tested for HIV) and HIV positivity (ie, whether the partners tested were newly diagnosed HIV-positive). We defined newly diagnosed partners as partners who tested HIV-positive through partner services–initiated testing and had not previously self-reported as HIV-positive or had never been tested for HIV infection. We analyzed the following demographic characteristics: partners’ age (13-24, 25-34, 35-44, and ≥45 y); race/ethnicity (non-Hispanic white [hereinafter referred to as white], non-Hispanic black or African American [hereinafter referred to as black], Hispanic/Latino, and non-Hispanic other race [hereinafter referred to as other race]); and gender (male, female, or other [ie, transgender and those who did not specify their current gender]). In addition, we categorized the state in which partners received partner services into geographic regions: South, Northeast, Midwest, and West.33
Analysis
We conducted descriptive and multivariate analyses on the reported partner services data. We first examined the patterns of HIV testing by partners’ demographic characteristics and geographic region. Then we assessed the patterns of HIV positivity by partners’ demographic characteristics and geographic region. We used univariate logistic regression analysis to calculate crude odds ratios (ORs) and 95% confidence intervals (CIs) for each independent variable to assess its association with the likelihood of being tested for HIV infection and being HIV-positive. We then constructed a multivariate logistic regression model with stepwise selection to assess the adjusted association of the demographic characteristics and geographic region with HIV testing and HIV positivity of partners. We used adjusted ORs (aORs) and their 95% CIs to interpret the final model. We conducted all statistical analyses using SAS version 9.3.34
Results
A total of 21 484 sexual and/or needle-sharing partners of index patients with HIV testing data were reported by partner services programs from 55 CDC-funded state and local health departments during 2013-2014. Of these, 16 275 (75.8%) were tested for HIV, and 12 886 (79.2%) of them had HIV test results. Among those who had HIV test results, 4503 (34.9%) were newly diagnosed with HIV infection (Table 1).
Table 1.
Characteristics of partners tested for HIV in partner services programs (n = 55), United States, 2013-2014
| Characteristics | Total Partners, No. (Column %) | Partners Tested for HIV, No. (Row % of Total Partners) | Tested Partners With Test Results, No. (Row % of Partners Tested for HIV) | Newly Diagnosed HIV-Positive Partners, No. (Row % of Partners With Test Results) |
|---|---|---|---|---|
| Age group, y | ||||
| 13-24 | 4596 (21.4) | 3525 (76.7) | 2734 (77.6) | 880 (32.2) |
| 25-34 | 7606 (35.4) | 5721 (75.2) | 4506 (78.8) | 1571 (34.9) |
| 35-44 | 4666 (21.7) | 3502 (75.1) | 2768 (79.0) | 1005 (36.3) |
| ≥45 | 4616 (21.5) | 3527 (76.4) | 2878 (81.6) | 1047 (36.4) |
| Gender | ||||
| Male | 16 872 (78.5) | 12 987 (77.0) | 10 168 (78.3) | 3824 (37.6) |
| Female | 4028 (18.8) | 3123 (77.5) | 2556 (81.8) | 648 (25.4) |
| Othera | 584 (2.7) | 165 (28.3) | 162 (98.2) | 31 (19.1) |
| Race/ethnicity | ||||
| Non-Hispanic white | 6023 (28.0) | 4784 (79.4) | 3686 (77.0) | 1083 (29.4) |
| Non-Hispanic black | 11 294 (52.6) | 8420 (74.6) | 6696 (79.5) | 2681 (40.1) |
| Hispanic/Latino | 3665 (17.1) | 2660 (72.6) | 2239 (84.2) | 674 (30.1) |
| Non-Hispanic otherb | 502 (2.3) | 411 (81.9) | 265 (64.5) | 65 (24.5) |
| Geographic regionc | ||||
| Northeast | 3330 (15.5) | 1618 (48.6) | 1431 (88.4) | 234 (16.4) |
| Midwest | 1249 (5.8) | 978 (78.3) | 659 (67.4) | 145 (22.0) |
| South | 14 148 (65.9) | 11 613 (82.1) | 9704 (83.6) | 3920 (40.4) |
| West | 2757 (12.8) | 2066 (74.9) | 1092 (52.9) | 204 (18.7) |
| Total | 21 484 (100.0) | 16 275 (75.8) | 12 886 (79.2) | 4503 (34.9) |
Abbreviation: HIV, human immunodeficiency virus.
aIncludes transgender and those who did not specify their current gender.
bIncludes Asian, American Indian/Alaska Native, Native Hawaiian/other Pacific Islander, and multi-race.
cUS geographic regions: Northeast: Connecticut, Maine, Massachusetts, New Hampshire, New Jersey, New York, New York City (New York), Pennsylvania, Philadelphia (Pennsylvania), and Rhode Island. Midwest: Indiana, Iowa, Kansas, Michigan, Minnesota, Missouri, Nebraska, North Dakota, Ohio, South Dakota, and Wisconsin; South: Alabama, Arkansas, Atlanta (Georgia), Baltimore (Maryland), Chicago (Illinois), Delaware, Florida, Georgia, Kentucky, Louisiana, Maryland, Mississippi, North Carolina, Oklahoma, South Carolina, Tennessee, Virginia, Washington DC, and West Virginia. West: Alaska, Arizona, California, Colorado, Hawaii, Idaho, Los Angeles (California), Montana, Nevada, New Mexico, Oregon, San Francisco, Utah, Washington, and Wyoming. Illinois, Vermont, Texas, Houston, Puerto Rico, and the US Virgin Islands were not included either because data were not received from them or because their data had missing information on demographic characteristics or HIV test results.
HIV Testing Patterns
Partners aged 35-44 (aOR = 0.86; 95% CI, 0.78-0.95) were less likely to be tested for HIV than those aged 13-24. Partners who were male (aOR = 0.89; 95% CI, 0.81-0.97) and other gender (aOR = 0.08; 95% CI, 0.06-0.09) were less likely than female partners to be tested for HIV. Compared with white partners, partners who were black (aOR = 0.68; 95% CI, 0.63-0.74) and Hispanic/Latino (aOR = 0.79; 95% CI, 0.71-0.88) were less likely to be tested for HIV, and partners who were other race (aOR = 1.28; 95% CI, 1.01-1.64) were more likely to be tested for HIV. Finally, partners who received partner services in the South (aOR = 1.56; 95% CI, 1.35-1.80) were more likely than partners who received partner services in the Midwest to be tested for HIV. Partners who received partner services in the Northeast (aOR = 0.28; 95% CI, 0.24-0.32) and the West (aOR = 0.78; 95% CI, 0.66-0.92) were less likely than those who received partner services in the Midwest to be tested for HIV (Table 2).
Table 2.
Demographic characteristics and geographic regions associated with HIV testing of partners in partner services programs (n = 55), United States, 2013-2014
| Characteristics | Total No. of Partners | OR (95% CI) | aOR (95% CI) |
|---|---|---|---|
| Age group, y | |||
| 13-24 | 4596 | 1.00 (Ref) | 1.00 (Ref) |
| 25-34 | 7606 | 0.92 (0.85-1.01) | 0.92 (0.84-1.01) |
| 35-44 | 4666 | 0.91 (0.83-1.01) | 0.86 (0.78-0.95) |
| ≥45 | 4616 | 0.98 (0.89-1.08) | 0.90 (0.81-1.00) |
| Gender | |||
| Female | 4028 | 1.00 (Ref) | 1.00 (Ref) |
| Male | 16 872 | 0.97 (0.89-1.05) | 0.89 (0.81-0.97) |
| Othera | 584 | 0.11 (0.09-0.14) | 0.08 (0.06-0.09) |
| Race/ethnicity | |||
| Non-Hispanic white | 6023 | 1.00 (Ref) | 1.00 (Ref) |
| Non-Hispanic black | 11 294 | 0.76 (0.70-0.82) | 0.68 (0.63-0.74) |
| Hispanic/Latino | 3665 | 0.69 (0.62-0.75) | 0.79 (0.71-0.88) |
| Non-Hispanic otherb | 502 | 1.17 (0.92-1.48) | 1.28 (1.01-1.64) |
| Geographic regionc | |||
| Midwest | 1249 | 1.00 (Ref) | 1.00 (Ref) |
| Northeast | 3330 | 0.26 (0.23-0.30) | 0.28 (0.24-0.32) |
| South | 14 148 | 1.27 (1.10-1.46) | 1.56 (1.35-1.80) |
| West | 2757 | 0.83 (0.71-0.97) | 0.78 (0.66-0.92) |
Abbreviation: aOR, adjusted odds ratio; CI, confidence interval; HIV, human immunodeficiency virus; OR, odds ratio; Ref, reference group.
aIncludes transgender and those who did not specify their current gender.
bIncludes Asian, American Indian/Alaska Native, Native Hawaiian/other Pacific Islander, and multi-race.
cUS geographic regions: Northeast: Connecticut, Maine, Massachusetts, New Hampshire, New Jersey, New York, New York City (New York), Pennsylvania, Philadelphia (Pennsylvania), and Rhode Island. Midwest: Indiana, Iowa, Kansas, Michigan, Minnesota, Missouri, Nebraska, North Dakota, Ohio, South Dakota, and Wisconsin; South: Alabama, Arkansas, Atlanta (Georgia), Baltimore (Maryland), Chicago (Illinois), Delaware, Florida, Georgia, Kentucky, Louisiana, Maryland, Mississippi, North Carolina, Oklahoma, South Carolina, Tennessee, Virginia, Washington DC, and West Virginia. West: Alaska, Arizona, California, Colorado, Hawaii, Idaho, Los Angeles (California), Montana, Nevada, New Mexico, Oregon, San Francisco, Utah, Washington, and Wyoming. Illinois, Vermont, Texas, Houston, Puerto Rico, and the US Virgin Islands were not included either because data either were not received from them or because their data had missing information on demographic characteristics or HIV test results.
HIV Positivity Patterns
Demographic characteristics and geographic region were significantly associated with HIV positivity of partners in multivariate analyses. Partners aged 25-34 (aOR = 1.19; 95% CI, 1.07-1.32), 35-44 (aOR = 1.35; 95% CI, 1.20-1.52), and ≥45 (aOR = 1.30; 95% CI, 1.16-1.46) were more likely than those aged 13-24 to test HIV-positive. Compared with partners who were female, partners who were male (aOR = 1.81; 95% CI, 1.64-2.01) were more likely to test HIV-positive and partners who were other gender (aOR = 0.63; 95% CI, 0.41-0.93) were less likely to test HIV-positive. Partners who were black (aOR = 1.52; 95% CI, 1.38-1.66) were more likely to test HIV-positive than partners who were white. Finally, compared with partners who received partner services in the Midwest, partners who received partner services in the South (aOR = 2.18; 95% CI, 1.81-2.65) were more likely to test HIV-positive and those in the Northeast (aOR = 0.68; 95% CI, 0.54-0.86) were less likely to test HIV-positive (Table 3).
Table 3.
Demographic characteristics associated with HIV positivity of partners in partner services programs (n = 55), United States, 2013-2014
| Characteristics | Tested Partners With Test Results | OR (95% CI) | aOR (95% CI) |
|---|---|---|---|
| Age group | |||
| 13-24 | 2734 | 1.00 (Ref) | 1.00 (Ref) |
| 25-34 | 4506 | 1.13 (1.02-1.25) | 1.19 (1.07-1.32) |
| 35-44 | 2768 | 1.20 (1.07-1.34) | 1.35 (1.20-1.52) |
| ≥45 | 2878 | 1.21 (1.08-1.35) | 1.30 (1.16-1.46) |
| Gender | |||
| Female | 2556 | 1.00 (Ref) | 1.00 (Ref) |
| Male | 10 168 | 1.77 (1.61-1.96) | 1.81 (1.64-2.01) |
| Othera | 162 | 0.70 (0.47-1.04) | 0.63 (0.41-0.93) |
| Race/ethnicity | |||
| Non-Hispanic white | 3686 | 1.00 (Ref) | 1.00 (Ref) |
| Non-Hispanic black | 6696 | 1.61 (1.47-1.75) | 1.52 (1.38-1.66) |
| Hispanic/Latino | 2239 | 1.04 (0.92-1.16) | 1.05 (0.93-1.18) |
| Non-Hispanic otherb | 265 | 0.78 (0.59-1.04) | 0.97 (0.71-1.30) |
| Geographic regionc | |||
| Midwest | 659 | 1.00 (Ref) | 1.00 (Ref) |
| Northeast | 1431 | 0.69 (0.55-0.87) | 0.68 (0.54-0.86) |
| South | 9704 | 2.40 (1.99-2.90) | 2.18 (1.81-2.65) |
| West | 1092 | 0.81 (0.64-1.03) | 0.85 (0.67-1.09) |
Abbreviation: aOR, adjusted odds ratio; CI, confidence interval; HIV, human immunodeficiency virus; OR, odds ratio; Ref, reference group.
aIncludes transgender and those who did not specify their current gender.
bIncludes Asian, American Indian/Alaska Native, Native Hawaiian/other Pacific Islander, and multi-race.
cUS geographic regions: Northeast: Connecticut, Maine, Massachusetts, New Hampshire, New Jersey, New York, New York City (New York), Pennsylvania, Philadelphia (Pennsylvania), and Rhode Island. Midwest: Indiana, Iowa, Kansas, Michigan, Minnesota, Missouri, Nebraska, North Dakota, Ohio, South Dakota, and Wisconsin; South: Alabama, Arkansas, Atlanta (Georgia), Baltimore (Maryland), Chicago (Illinois), Delaware, Florida, Georgia, Kentucky, Louisiana, Maryland, Mississippi, North Carolina, Oklahoma, South Carolina, Tennessee, Virginia, Washington DC, and West Virginia. West: Alaska, Arizona, California, Colorado, Hawaii, Idaho, Los Angeles (California), Montana, Nevada, New Mexico, Oregon, San Francisco, Utah, Washington, and Wyoming. Illinois, Vermont, Texas, Houston, Puerto Rico, and the US Virgin Islands were not included either because data were not received from them or because their data had missing information on demographic characteristics or HIV test results.
Discussion
Partner services implemented by CDC-funded local and state health departments in the United States appear successful in providing HIV testing services and identifying previously undiagnosed HIV infection among sexual and/or needle-sharing partners of people with HIV infection. One indication of success was the high proportion of partners tested for HIV (75.8%) compared with the rates reported by other partner services programs (range, 50%-63%).11,13,14 However, there is room for improvement. Nearly 25% of partners were not tested, implying that they were potentially at risk for getting infected (if negative) or exposing their other partners to infection (if positive). The problem is likely to be more pronounced if those not tested for HIV represent a sector of the population who may have limited access to testing services, are marginalized, or are more vulnerable to HIV infection for various socioeconomic reasons. Given these potential problems, it is important that health department partner services programs strive to identify and address the underlying barriers for not testing among partners.
Among partners with test results, 34.9% were newly diagnosed as HIV-positive. Although the high rate of HIV positivity among partners is disturbing and reflects the vulnerability of partners of HIV-diagnosed people, it is also an indication of the success of partner services programs. The result is consistent with previous findings that partner services programs are more effective in identifying a higher proportion of undiagnosed HIV infections than are targeted or routine HIV testing programs.15–17,35 This finding was close to the San Francisco Department of Health’s finding of a 28.3% HIV positivity rate among partners.13 In addition, a study among index patients with acute and early HIV infection found that 33% of partners were newly HIV-positive.36 However, other studies, including a survey of partner services programs among 44 local health departments from 10 states and a systematic review of 9 studies, reported newly diagnosed HIV-positive partners at ≤20%.11,37 These differences in HIV positivity reflect variations in data collection methods, target population covered, and ascertainment of new HIV-positive partners. Most of these studies relied on small samples or were limited to specific geographic areas; our study depended on routinely collected program data from 47 state health departments and 8 local health departments. In our study, newly diagnosed HIV-positive partners were those who self-reported no prior HIV-positive test results; in other studies, newly diagnosed HIV-positive people were determined by cross-checking the person’s HIV status with HIV surveillance records.13,36
Overall, older, black, and male partners were more likely to test HIV-positive than their counterparts. This finding is also consistent with the pattern of HIV prevalence3 and CDC-funded HIV testing programs nationally.35,38 Partners who received partner services in the South accounted for 66% of total partners and had the highest HIV testing rate (82%) compared with other regions. This higher rate might be due to efforts by CDC and other public health agencies to expand HIV testing in regions that are most affected by HIV.4–6,39 Partners who received partner services in the South had the highest rate of HIV positivity (40%), which is consistent with the disproportionate prevalence of HIV in this region. The South had the highest HIV diagnosis rate of any US region in 2014, with 51% of all HIV diagnoses reported, despite accounting for only 38% of the US population.3,40
Demographic and regional differences in HIV testing rates suggest that barriers exist that prevent some groups from accessing partner services–initiated HIV testing services. People with HIV who know they are infected can get treatment to help keep them healthy for many years. Studies indicate that all people living with HIV, including those with early infection, benefit from antiretroviral therapy.41 Treatment with antiretroviral medications lowers the level of HIV viral load in the bloodstream, reduces HIV-related illness, and reduces the spread of HIV to others.42 People living with HIV who know their status can also make other decisions that lower their risk of transmitting HIV to a partner. Adherence to antiretroviral therapy by an HIV-positive person can reduce the chance of transmitting the virus to sexual/needle-sharing partners by as much as 96%.43 This finding reinforces the importance of partner services in identifying new infections among partners of HIV-positive people for timely linkage to HIV medical care.
Nearly two-thirds of partners tested did not have HIV and may continue to be at risk for infection. Pre-exposure prophylaxis (PrEP) has proven to be a highly effective HIV prevention strategy, particularly among people at substantial risk for HIV acquisition, including serodiscordant partners of people living with HIV.44 As such, partner services programs have a unique opportunity to facilitate linkage to PrEP services for HIV-negative partners of HIV-positive people. CDC-funded health departments were not required to collect data on PrEP services in the past; as a result, the extent to which partner services programs facilitated entry to PrEP services for partners at risk for HIV infection is unknown. It will be important for state and local health departments to capture information on these efforts in the future to help monitor and improve PrEP services.
Limitations
Our study had several limitations. First, although CDC provided recommendations outlining the basic requirements for implementing partner services programs, funded health departments employ different methods and models of partner services, which depend on legislation, local service delivery systems, and/or available resources. A national survey study37 identified that partner services programs vary in several ways, including (1) whether partner services are integrated for HIV and other sexually transmitted diseases, (2) the degree of collaboration with surveillance, and (3) who is involved in implementing partner services activities (eg, health department only vs health department in collaboration with community-based organizations or private providers). Unfortunately, our current data requirements did not capture these patterns. The variability in models of partner services can differentially affect some of the outcomes discussed in our study. The newly diagnosed HIV-positive rate may, in part, reflect a jurisdiction’s ability to effectively use its surveillance system.
Second, we determined a new HIV-positive status based on self-report of no prior positive test results. As such, the HIV positivity rate may have been overestimated in those jurisdictions that do not routinely check their laboratory or surveillance records. Lack of this information in current CDC partner services data requirements suggests an area of improvement for future data collection efforts. Third, although CDC’s partner services program evaluation data requirements are standardized, data collection approaches and systems vary among grantees. Data systems may not be programmed to capture the complete set of required elements, or extracting and reporting the data to CDC may be challenging. All of these limitations could potentially introduce data biases. Among tested partners in this analysis, 3389 (20.8%) lacked HIV test results. When we compared people with and without HIV test results, we found no difference by demographic characteristics. However, the patterns of missing data on HIV test results varied by geography: 16.4% of people tested in the South, 11.6% in the Northeast, 32.6% in the Midwest, and 47.1% in the West had missing data. Although the effect of this variability is unclear, it is unlikely that HIV positivity is underestimated in the South given the lower proportion of missing data in the region that has the highest HIV prevalence. Finally, the data for this study were limited to CDC-funded state and local health departments and may not reflect the totality of partner services programs implemented nationally.
Conclusions
Our analysis revealed that partner services programs implemented by CDC-funded health departments are successful in providing HIV testing services to more than three-fourths of partners of HIV-positive people. In addition, compared with other routine or targeted testing initiatives, partner services programs have identified higher levels of undiagnosed HIV infection among partners and paved the way for efforts to link HIV-positive partners to care, improve their health outcomes, and interrupt further transmission of HIV infection to others. Demographic and regional differences in partner services-initiated HIV testing and diagnosis of HIV infection suggest differences in the delivery of partner services programs and population-level vulnerabilities to HIV infection. Further analysis may help identify underlying factors contributing to demographic and regional differences in HIV testing and diagnosis of new HIV infection among partners and help improve partner services programs.
Footnotes
Authors’ Note: The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The Centers for Disease Control and Prevention provides funding to health departments in states, territories, and selected US cities to develop and implement comprehensive HIV prevention programs, including partner services.
References
- 1. Centers for Disease Control and Prevention. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data: United States and 6 dependent areas—2013. HIV Surveill Suppl Rep. 2015;20(2):1–70. [Google Scholar]
- 2. Centers for Disease Control and Prevention. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data: United States and 6 dependent areas—2014. HIV Surveill Suppl Rep. 2016;21(4):1–87. [Google Scholar]
- 3. Centers for Disease Control and Prevention. Diagnoses of HIV infection in the United States and dependent areas, 2014. HIV Surveill Rep. 2015;26:1–123. [Google Scholar]
- 4. White House (US), Office of National AIDS Policy. National HIV/AIDS strategy for the United States. 2010. https://www.aids.gov/federal-resources/national-hiv-aids-strategy/nhas-fact-sheet.pdf. Accessed February 19, 2016.
- 5. White House (US), Office of National AIDS Policy. National HIV/AIDS strategy for the United States: updated to 2020. 2015. https://www.aids.gov/federal-resources/national-hiv-aids-strategy/nhas-update.pdf. Accessed February 19, 2016.
- 6. Centers for Disease Control and Prevention. High-impact HIV Prevention: CDC’s approach to reducing HIV infections in the United States. https://www.cdc.gov/hiv/pdf/policies_nhpc_booklet.pdf. 2011. Accessed December 10, 2015.
- 7. Centers for Disease Control and Prevention. HIV partner counseling and referral services: guidance. 1998. https://stacks.cdc.gov/view/cdc/5150/cdc_5150_DS1.pdf. Accessed December 10, 2015.
- 8. Centers for Disease Control and Prevention. Program operations guidelines for STD prevention. 2001. http://www.cdc.gov/std/program/progevaluation.pdf. Accessed December 10, 2015.
- 9. Centers for Disease Control and Prevention. Recommendations for partner services programs for HIV infection, syphilis, gonorrhea, and chlamydial infection. MMWR Recomm Rep. 2008;57(RR-9):1–63. [PubMed] [Google Scholar]
- 10. Ahrens K, Kent CK, Kohn RP, et al. HIV partner notification outcomes for HIV-infected patients by duration of infection, San Francisco, 2004 to 2006. J Acquir Immune Defic Syndr. 2007;46(4):479–484. [DOI] [PubMed] [Google Scholar]
- 11. Hogben M, McNally T, McPheeters M, et al. ; Task Force on Community Preventive Services. The effectiveness of HIV partner counseling and referral services in increasing identification of HIV-positive individuals: a systematic review. Am J Prev Med. 2007;33(suppl 2):S89–S100. [DOI] [PubMed] [Google Scholar]
- 12. Lin F, Farnham PG, Shrestha RK, et al. Cost effectiveness of HIV prevention interventions in the U.S. Am J Prev Med. 2016;50(6):699–708. [DOI] [PubMed] [Google Scholar]
- 13. Bernstein KT, Stephens SC, Moss N, et al. Partner services as targeted HIV screening: changing the paradigm. Public Health Rep. 2014;129(suppl 1):50–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Udeagu CC, Shah D, Shepard CW, et al. Impact of a New York City Health Department initiative to expand HIV partner services outside STD clinics. Public Health Rep. 2012;127(1):107–114. [PMC free article] [PubMed] [Google Scholar]
- 15. Varghese B, Peterman TA, Holtgrave DR. Cost-effectiveness of counseling and testing and partner notification: a decision analysis. AIDS. 1999;13(13):1745–1751. [DOI] [PubMed] [Google Scholar]
- 16. Shrestha RK, Begley EB, Hutchinson AB, et al. Costs and effectiveness of partner counseling and referral services with rapid testing for HIV in Colorado and Louisiana, United States. Sex Transm Dis. 2009;36(10):637–641. [DOI] [PubMed] [Google Scholar]
- 17. Jones JL, Wykoff RF, Hollis SL, et al. Partner acceptance of health department notification of HIV exposure, South Carolina. JAMA. 1990;264(10):1284–1286. [PubMed] [Google Scholar]
- 18. Passin WF, Kim AS, Hutchinson AB, et al. ; HIV/AIDS Prevention Research Synthesis Project Team. A systematic review of HIV partner counseling and referral services: client and provider attitudes, preferences, practices, and experiences. Sex Transm Dis. 2006;33(5):320–328. [DOI] [PubMed] [Google Scholar]
- 19. Henley C, Forgwei G, Welty T, et al. Scale-up and case-finding effectiveness of an HIV partner services program in Cameroon: an innovative HIV prevention intervention for developing countries. Sex Transm Dis. 2013;40(12):909–914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Malave MC, Shah D, Sackoff JE, et al. Human immunodeficiency virus partner elicitation and notification in New York City: public health does it better. Sex Transm Dis. 2008;35(10):869–876. [DOI] [PubMed] [Google Scholar]
- 21. Wilson TE, Hogben M, Malka ES, et al. A randomized controlled trial for reducing risks for sexually transmitted infections through enhanced patient-based partner notification. Am J Public Health. 2009;99(suppl 1):S104–S110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Bocour A, Renaud TC, Udeagu CC, et al. HIV partner services are associated with timely linkage to HIV medical care. AIDS. 2013;27(18):2961–2963. [DOI] [PubMed] [Google Scholar]
- 23. Weller SC, Davis-Beaty K. Condom Effectiveness in Reducing Heterosexual HIV Transmission (Review): The Cochrane Collaboration. Hoboken, NJ: John Wiley and Sons; 2007;4:1–22. [DOI] [PubMed] [Google Scholar]
- 24. Patel P, Borkowf CB, Brooks JT, et al. Estimating per-act HIV transmission risk: a systematic review. AIDS. 2014;28(10):1509–1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Tripathi A, Gardner L, Ogbuanu I, et al. Predictors of time to enter medical care after a new HIV diagnosis: a statewide population-based study. AIDS Care. 2011;23(11):1366–1373. [DOI] [PubMed] [Google Scholar]
- 26. Page-Shafer K, Veugelers PJ, Moss AR, et al. Sexual risk behavior and risk factors for HIV-1 seroconversion in homosexual men participating in the Tricontinental Seroconverter Study, 1982-1994 [published erratum appears in Am J Epidemiol. 1997;146(12):1076]. Am J Epidemiol. 1997;146(7):531–542. [DOI] [PubMed] [Google Scholar]
- 27. Ostrow DG, DiFranceisco WJ, Chmiel JS, et al. A case-control study of human immunodeficiency virus type 1 seroconversion and risk-related behaviors in the Chicago MACS/CCS cohort, 1984-1992 [published erratum appears in Am J Epidemiol. 1996;143(1):104]. Am J Epidemiol. 1995;142(8):875–883. [DOI] [PubMed] [Google Scholar]
- 28. Quinn TC, Wawer MJ, Sewankambo N, et al. Viral load and heterosexual transmission of human immunodeficiency virus type 1. Rakai Project Study Group. N Engl J Med. 2000;342(13):921–929. [DOI] [PubMed] [Google Scholar]
- 29. Gray RH, Wawer MJ, Brookmeyer R, et al. Probability of HIV-1 transmission per coital act in monogamous, heterosexual, HIV-1-discordant couples in Rakai, Uganda. Lancet. 2001;357(9263):1149–1153. [DOI] [PubMed] [Google Scholar]
- 30. Wawer MJ, Gray RH, Sewankambo NK, et al. Rates of HIV-1 transmission per coital act, by stage of HIV-1 infection, in Rakai, Uganda. J Infect Dis. 2005;191(1):1403–1409. [DOI] [PubMed] [Google Scholar]
- 31. Freeman EE, Weiss HA, Glynn JR, et al. Herpes simplex virus 2 infection increases HIV acquisition in men and women: systematic review and meta-analysis of longitudinal studies. AIDS. 2006;20(1):73–83. [DOI] [PubMed] [Google Scholar]
- 32. Macdonald N, Elam G, Hickson F, et al. Factors associated with HIV seroconversion in gay men in England at the start of the 21st century. Sex Transm Infect. 2008;84(1):8–13. [DOI] [PubMed] [Google Scholar]
- 33. US Census Bureau. Census regions and divisions of the United States. 2013. https://www2.census.gov/geo/pdfs/maps-data/maps/reference/us_regdiv.pdf. Accessed October 25, 2015.
- 34. SAS Institute Inc. SAS Version 9.3. Cary, NC: SAS Institute Inc; 2011. [Google Scholar]
- 35. Centers for Disease Control and Prevention. CDC-funded HIV testing: United States, Puerto Rico, and the U.S. Virgin Islands, 2013. https://www.cdc.gov/hiv/pdf/library/reports/cdc-hiv-CDCFunded_HIV_Testing_UnitedStates_Puerto_Rico_USVI_2013.pdf. Accessed April 14, 2017.
- 36. Green N, Hoenigl M, Chaillon A, et al. Partner services in adults with acute and early HIV infection. AIDS. 2017;31(2):287–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Katz DA, Hogben M, Dooley SW, Jr, et al. Increasing public health partner services for human immunodeficiency virus: results of a second national survey. Sex Transm Dis. 2010;37(8):469–475. [DOI] [PubMed] [Google Scholar]
- 38. Centers for Disease Control and Prevention. CDC-funded HIV testing: United States, Puerto Rico, and the U.S. Virgin Islands, 2014. https://www.cdc.gov/hiv/pdf/library/reports/cdc-hiv-funded-testing-us-puerto-rico-2014.pdf. Accessed April 14, 2017.
- 39. Centers for Disease Control and Prevention. PS12-1201: comprehensive HIV prevention programs for health departments: monitoring and evaluation report, 2012. –2013. https://www.cdc.gov/hiv/pdf/funding/announcements/ps12-1201/cdc-hiv-ps12-1201_monitoring_and_evaluation_report.pdf. Accessed April 14, 2017.
- 40. US Census Bureau. United States population growth by region. 2015. https://www.census.gov/popclock/data_tables.php?component=growth. Accessed October 20, 2015.
- 41. Reynolds SJ, Makumbi F, Nakigozi G, et al. HIV-1 transmission among HIV-1 discordant couples before and after the introduction of antiretroviral therapy. AIDS. 2011;25(4):473–477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Cohen MS, Gay CL. Treatment to prevent transmission of HIV-1. Clin Infect Dis. 2010;50(suppl 3):S85–S95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Cohen MS, Chen YQ, McCauley M, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365(6):493–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. McMahon JM, Myers JE, Kurth AE, et al. Oral pre-exposure prophylaxis (PrEP) for prevention of HIV in serodiscordant heterosexual couples in the United States: opportunities and challenges. AIDS Patient Care STDS. 2014;28(9):462–474. [DOI] [PMC free article] [PubMed] [Google Scholar]