Abstract
Objectives
To determine the variation in annual health care costs among heart failure patients in the VA system.
Background
Heart failure is associated with considerable use of health care resources, but little is known about patterns in patient characteristics related to higher costs.
Methods
We obtained VA utilization and cost records for all patients with a diagnosis of heart failure in fiscal year 2010. We compared total VA costs by patient demographic factors, comorbid conditions, and facility where they were treated in bivariate analyses. We regressed total costs on patient factors alone; VA facility alone; and all factors combined to determine the relative contribution of patient factors and facility to explaining cost differences.
Results
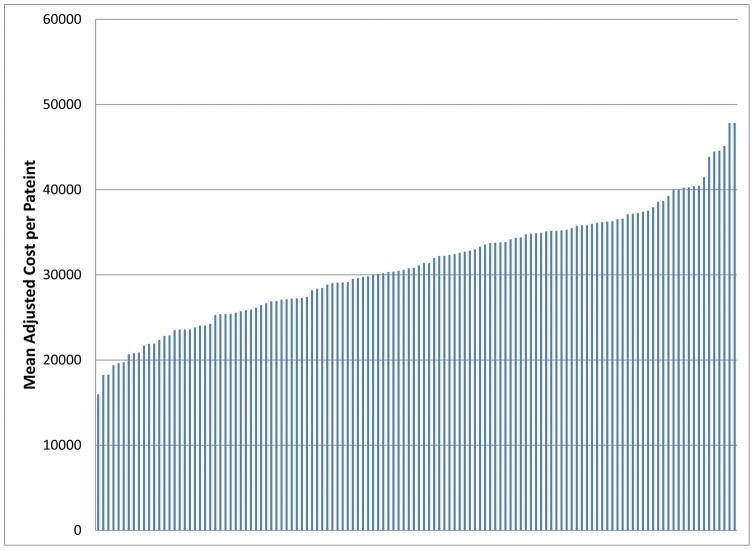
There were 117,870 patients with heart failure, and their mean annual VA costs were $30,719 (SD=49,180) with more than half of their costs due to inpatient care. Patients at younger ages, of Hispanic or black race/ethnicity, diagnosed with comorbid drug use disorders, or who died during the year had the highest costs (all P<0.01). There was variation in costs by facility as mean adjusted costs ranged from approximately $15,000 to $48,000. In adjusted analyses patient factors alone explained more of the variation in health care costs (R2=0.116) compared to the facility where the patient was treated (R2=0.018).
Conclusion
A large variation in costs of heart failure patients was observed across facilities although this was explained largely by patient factors. Improving the efficiency of VA resource utilization may require increased scrutiny of high-cost patients to determine if adequate value is being delivered to those patients.
Keywords: heart failure, costs, veterans
Introduction
Heart failure is associated with considerable morbidity and mortality, and patients diagnosed with this condition use a significant amount of health care resources. The economic burden of heart failure, especially in aging adults, is substantial: Medicare costs for all care for advanced heart failure patients has been estimated to be $36,216 in the final six months of life (1, 2). One key driver of costs for heart failure patients is the high rate of hospitalizations (3). A study of patients hospitalized for heart failure found that they had an average of $7100 in costs over the following six months with half of them being readmitted during that time (4). Among these patients, kidney failure and hypertension contributed to higher costs, so management of comorbid conditions can increase the complexity of care and resources used. In another cohort of heart failure patients, depression was found to increase costs in heart failure patients by 26–29% due to greater inpatient and outpatient utilization but not significantly greater mental health utilization (5). Other psychiatric conditions such as alcohol disorders and bipolar disorder have also been related to higher costs (6).
In addition to patient factors such as comorbidity, variation in treatment patterns by providers also contributes to the utilization of heart failure patients. Previous research looked at small-area geographic variation and between-hospital variation in quality measures for patients hospitalized for heart failure. These studies found substantial variation in quality measures as well as length of stay and mortality, and some of this variation was explained by provider and hospital characteristics such as teaching status of hospitals (7, 8).
There are several questions not yet addressed by the current literature. Most of the evidence on costs of heart failure patients has focused on those who have been hospitalized since they incur the most costs. Therefore, there have been few studies looking at costs among all heart failure patients to determine whether there are broader patterns in patient characteristics related to greater utilization and costs. While geographic variation has been documented among Medicare providers and hospitals nationally, less is known about variation within a large, integrated system such as the Veterans Affairs (VA) health care system. The VA health care system cares for more than 5 million patients each year, and heart failure is present in many multimorbid patients, especially among the highest-cost patients in the system (9). Using national performance measures of quality of care and paying providers on a salary basis may potentially minimize geographic and provider differences in the VA system.
Examining variation in health care costs between heart failure patients can shed light on the factors that are associated with higher costs that can also serve as potential areas to target for quality improvement. In this study we aimed to determine the variation in one-year, VA health care costs in a population of patients diagnosed with heart failure. We compared the differences in costs between patients by sociodemographic factors, comorbid conditions, geographic location, and the facility where patients were treated. We also determined the specific types of inpatient and outpatient health care services that patients utilized.
Methods
Cohort and Data Sources
We obtained VA inpatient and outpatient utilization records for all patients who used any VA provided or sponsored care in fiscal year (FY) 2010 (October 1, 2009-September 30, 2010). We determined which patients had a diagnosis of heart failure (ICD-9 codes: 398.91, 402.01, 402.11, 402.91, 404.01, 404.03, 404.11, 404.13, 404.91, 404.93, 428) in at least two separate encounters during the year to obtain a cohort of heart failure patients. From the VA National Patient Care Database and Fee Basis files which reported utilization, we obtained patients’ sociodemographic characteristics, diagnoses, all VA-provided or VA-sponsored inpatient (acute, long-term, and observation stays) and outpatient utilization, and costs of these services during FY2010. We also obtained VA Vital Status records for mortality information.
Costs and Utilization Measures
Costs of VA care for each patient was obtained for inpatient and outpatient care, outpatient prescription drugs, and contract care from several sources since there are no billing records in the VA. The costs of VA outpatient visits and inpatient stays were obtained from the 2010 Average Costs files, which estimate VA health care costs based on Medicare payments for similar care using information such as DRG codes in inpatient records and procedure codes in outpatient records (10–12). Inpatient care costs were also obtained for specific categories of care defined by the treating specialty of the inpatient unit and categorized as medical/surgical, behavioral, long-term, or residential/domiciliary care. Outpatient care costs were also obtained for specific categories defined by the clinic location as primary care, subspecialty, procedure-based specialty, surgical specialty, emergency department, urgent care, mental health, homeless-related, lab, or other care.
Inpatient utilization was measured by number of inpatient stays and length of each stay for each admission to an inpatient treating specialty unit. Transfers between treating specialties were considered multiple stays. Number of stays and length of stay were measured overall and by each inpatient category. Outpatient utilization was measured by number of visits which was counted by a unique combination of the clinic location and visit day for a patient. Number of visits across all categories and by specific outpatient category were estimated for each patient.
Prescription drug costs were obtained from the 2010 Decision Support System (DSS) Pharmacy files which report the supply and dispensing costs for each prescription filled in the VA. The costs of VA-sponsored care provided by non-VA providers was obtained from 2010 Fee Basis files, which report the payments per service made to providers. Total costs of VA care were estimated for each patient as the sum of all inpatient, outpatient, prescription drug, and contract care received during the year.
Costs for utilization of any services outside of the VA, including Medicare utilization and costs were not included in this study.
Patient Measures
We measured several sociodemographic characteristics of the cohort. We obtained patient’s age, gender, service connection, alternate health insurance, means test eligibility, VA facility, geographic region, marital status, race/ethnicity, and whether they had died during the year. Eligibility for VA services was categorized as service-connected if Veterans had a compensable, service-connected disability or were in the first five years after discharge from active duty, below the means test if they met an income-based means test, above the means test, or non-specified categories of eligibility. The degree of disability of a service-connected condition was rated from 0% to 100%. Patient’s alternate health insurance status was grouped into no insurance, private or public insurance other than Medicare (major medical or private HMO, PPO, Champus, or indemnity insurance), or Medicare and/or Medicare supplemental coverage. Each VA facility, also called medical center, encompasses an inpatient hospital and several outpatient clinics and is within one of 21 different regional VA Integrated Service Networks (VISNs). One facility was excluded since it had only 3 patients while the other facilities ranged in number of heart failure patients from 137 to 3,233. VISNs were grouped into 5 different geographic areas: Northeast, Southeast, Midsouth, Central, and West (see appendix for listing of VA networks in each region). Date of death, if available, was obtained from the VA Vital Status file and used to identify anyone who died during the year.
We obtained all diagnoses from inpatient and outpatient records during FY2010, and we coded 10 chronic conditions that have been identified as prevalent or previously related to high resource utilization among heart failure patients (13–19). Each VA inpatient record included fields for up to 13 conditions while each outpatient encounter included fields for up to 10 conditions. We coded conditions for alcohol use disorder, Alzheimer’s disease, chronic renal failure, depression, drug use disorder, diabetes, hypertension, ischemic heart disease (including coronary heart disease), post-traumatic stress disorder, and other psychiatric conditions (including schizophrenia and manic depression). Conditions were indicated for each patient if they had at least two separate instances of a diagnosis in inpatient or outpatient encounter records to avoid counting conditions recorded to rule out diagnoses.
Analysis
We used a generalized linear model (GLM) with a Poisson family distribution and a log-link function for all models since costs had a skewed distribution, and these are standard, recommended methods (20, 21). To compare total health care costs by patient characteristics, we conducted GLM models predicting total costs with age group as the sole predictor. We then repeated this regression for race/ethnicity alone and each comorbid condition alone. We also conducted multivariate analysis by regressing the total costs on all patient sociodemographic factors (age, gender, race/ethnicity, marital status, service connection, insurance, means test eligibility, geographic region), chronic conditions, and dummy variables for the 129 facilities in several models. Model 1 included patient factors as covariates while model 2 included facility dummies, and model 3 included all patient factors and facility dummies. We compared the R-squared and root mean squared error of the three models to determine whether the variation in health care costs was explained predominantly due to patient characteristics or facility where patients were treated (22).
We also used our fully adjusted regression model to compare the mean cost per heart failure patient in each facility after controlling for patient characteristics. For each facility, predicted cost per patient was estimated using regression model estimates for that facility and divided by the predicted cost per patient across all facilities and multiplied times the unadjusted cost per patient across all facilities to obtain the mean adjusted cost in each facility.
Results
Among the 5,233,994 patients who received any VA care in FY2010, there were 117,870 patients, or 2.3% of patients, who were identified as having heart failure. The majority of heart failure patients (56%) were 70 years and older, and few were under 50 years of age (Table 1). Patients were predominantly male (98%), and most patients were white (77%) while another 17% were black, 4% were Hispanic, and the rest were from other or unknown racial/ethnic groups. Only 53% of heart failure patients were currently married, and most patients were below the VA means test for eligibility or had a service-connected disability.
Table 1.
Patient Characteristics of All VA Patients with Heart Failure in FY2010, N=117,870
| Patient Characteristics | N (%) |
|---|---|
| Age group | |
| <50 | 2,088 (2) |
| 50–59 | 12,428 (11) |
| 60–69 | 37,014 (31) |
| 70–79 | 29,421 (25) |
| 80+ | 36,934 (31) |
| Gender | |
| Female | 2,299 (2) |
| Male | 115,586 (98) |
| Race/Ethnicity | |
| White | 90,593 (77) |
| Black | 19,516 (17) |
| Hispanic | 4,814 (4) |
| Other | 1,558 (1) |
| Unknown | 1,404 (1) |
| Marital Status | |
| Married | 62,964 (53) |
| Separated/Divorced/Widowed | 46,887 (40) |
| Single Never married | 8,034 (7) |
| Means Test | |
| Below Means Test, Not Service Connected | 50,222 (43) |
| Service Connected | 45,185 (38) |
| Above Means Test | 17,256 (15) |
| Other Eligibility | 5,222 (4) |
| Service Connected Percent | |
| 0 | 74,579 (63) |
| 1–49 | 14,887 (13) |
| 50+ | 28,419 (24) |
| Insurance | |
| No Insurance | 29,734 (25) |
| Major medical/HMO/PPO/Champus | 9,157 (8) |
| Medicare/Medicare supplemental | 76,850 (65) |
| All other | 2,144 (2) |
| Geographic region | |
| Northeast | 17,192 (15) |
| Southeast | 25,145 (21) |
| Midsouth | 29,038 (25) |
| Central | 22,721 (19) |
| West | 23,789 (20) |
| Chronic conditions | |
| Hypertension | 89,014 (76) |
| Ischemic heart disease | 62,143 (53) |
| Diabetes | 57,672 (49) |
| Renal failure | 24,187 (21) |
| Depression | 17,361 (15) |
| Post-Traumatic Stress Disorder | 8,158 (7) |
| Alcohol use disorder | 3,851 (3) |
| Other Psychiatric disorders | 4,035 (3) |
| Drug use disorder | 2457 (2) |
| Alzheimer’s disease | 854 (1) |
| Died during the year | |
| No | 105,750 (90) |
| Yes | 12,135 (10) |
Because of the older age of many heart failure patients, most were covered by Medicare. By geographic region, there was a higher percent of all heart failure patients from the Midsouth region which included the Texas network. There was high prevalence of many chronic conditions among the study cohort. Hypertension was the most prevalent condition diagnosed among 76% of heart failure patients in the current year. Ischemic heart disease (53%), diabetes (46%), and renal failure (21%) were also common diagnoses. In our cohort of heart failure patients, 10% of them died during the year.
The study cohort had mean annual VA costs of $30,719 (SD=49,180) per patient including inpatient care, outpatient care, and prescription drugs. Table 2 presents the distribution of inpatient and outpatient care spending among all heart failure patients. More than half of annual costs were due to inpatient care. The mean costs of all VA inpatient care per patient during the year was $16,313 (SD=$40,002), and most of it was for medical/surgical care. The mean costs of long-term care was $2,267 (SD=$16,004) per patient during year, and there were relatively few inpatient costs due to behavioral or residential care among all heart failure patients. Hospitalizations for medical/surgical care had the highest mean length of stay (mean= 4.6, SD=11) while the mean length of stay for long-term care was 4.2 days with considerable variation between patients (SD=27).
Table 2.
Mean VA Utilization and Costs per Patient for VA Patients with Heart Failure in FY2010, N=117,870
| Inpatient Health Care by Type | Mean (SD) |
|---|---|
| Costs | |
| Total inpatient costs | $16,313 (40,002) |
| Medical/surgical | $13,294 (31,923) |
| Behavioral | $293 (4,803) |
| Long-term care | $2,267 (16,004) |
| Residential/domiciliary | $96 (2,378) |
| Number of stays | |
| Medical/surgical | 0.83 (1.43) |
| Behavioral | 0.02 (0.21) |
| Long-term care | 0.06 (0.28) |
| Residential/domiciliary | 0.01 (0.08) |
| Length of stay | |
| Medical/surgical | 4.62 (10.59) |
| Behavioral | 0.25 (4.00) |
| Long-term care | 4.24 (26.73) |
| Residential/domiciliary | 0.26 (6.46) |
|
| |
| Outpatient Health Care by Type | |
|
| |
| Costs | |
| Medical/surgical | $6,614 (11,552) |
| Diagnostic | $1,697 (2,140) |
| Behavioral | $429 (3,472) |
| Other | $758 (9,615) |
| Pharmacy | $2,263 (4,690) |
| Number of encounters | |
| Primary care | 6.09 (6.34) |
| Subspecialty | 3.46 (5.21) |
| Procedure-based specialty | 1.32 (8.75) |
| Surgical specialty | 2.00 (3.47) |
| Emergency department | 1.32 (2.31) |
| Urgent care | 0.19 (0.85) |
| Mental health | 1.81 (9.43) |
| Homeless | 0.09 (2.44) |
| Lab | 8.51 (8.18) |
The largest component of outpatient costs was for medical/surgical care (mean=$6,614, SD=$11,552), and the next largest components were for outpatient pharmacy (mean=$2,263, SD=$4,690) and diagnostic care (mean=$1,697, SD=$2,140). Heart failure patients had an annual mean number of 6.09 primary care visits and 6.78 specialty care visits with 3.46 of them being for subspecialty care.
Health care costs not only varied by the type of care, but they also varied by demographic factors, comorbidity, and geographic location. Patients aged 50–59 years of age had the highest mean health care costs (Supplemental Figure 1), as VA health care costs declined for older ages since they were eligible for Medicare. Patients of different racial/ethnic groups also had different mean costs of care. Hispanic and black patients had mean health care costs that were more than $5,000 higher than the costs of white patients (Supplemental Figure 2). There were also differences in mean health care costs by comorbid conditions (Table 3). Patients diagnosed with comorbid drug use disorders had the highest reported costs of VA care. Other behavioral diagnoses (alcohol use disorders, depression, PSTD, and other psychiatric disorders) were also associated with higher mean costs compared to patients without these comorbid conditions. Health care costs were also relatively high for patients with renal failure.
Table 3.
Mean Costs by Comorbid Condition for VA Patients with Heart Failure in FY2010, N=117,870
| Chronic conditions | Mean Cost |
|---|---|
| Hypertension | $34,179 |
| Ischemic heart disease | $36,300 |
| Diabetes | $35,504 |
| Rental failure | $52,385 |
| Depression | $41,803 |
| Post-Traumatic Stress Disorder | $42,440 |
| Drug use disorder | $59,486 |
| Alcohol use disorder | $48,401 |
| Other Psychiatric disorders | $53,536 |
| Alzheimer’s disease | $36,116 |
Costs were obtained from a generalized linear model with a Poisson distribution and a log link function.
In adjusted analyses predicting total VA health care costs using both patient factors and facility, patient factors explained more of the variation in health care costs compared to the facility where the patient was treated (Table 4). The R2 of the regression model with patient factors including sociodemographics, and comorbid conditions was 0.116. The R2 for the regression model with facilities as the only predictors was 0.018, so little of the variation was explained by differences in care by facility. The regression model with all patient factors and facility had an R2 of 0.132.
Table 4.
Incident Rate Ratios from Generalized Linear Model Regressions of Costs in VA Patients with Heart Failure in FY2010, N=117,882
| Model (1) Patient factors only | Model (2) Facility only | Model (3) Patient and facility factors | |
|---|---|---|---|
| R-squared | 0.116 | 0.018 | 0.132 |
| Root Mean Squared Error | 46245 | 48739 | 45824 |
| Age in years | 0.991 | 0.990 | |
| Gender | |||
| Female | Ref | Ref | |
| Male | 0.942 | 0.941 | |
| Race/ethnicity | |||
| White | Ref | Ref | |
| Black | 1.015 | 1.048 | |
| Hispanic | 1.135 | 1.032 | |
| Other | 0.975 | 0.995 | |
| Unknown | 0.761 | 0.769 | |
| Marital status | |||
| Single | Ref | Ref | |
| Married | 0.801 | 0.821 | |
| Separated/divorced/widowed | 0.933 | 0.945 | |
| Service connected percent | |||
| 0 or none | Ref | Ref | |
| 1–49 | 0.930 | 0.933 | |
| 50+ | 1.163 | 1.172 | |
| Insurance coverage | |||
| None | Ref | Ref | |
| Major medical/private/CHAMPUS | 0.751 | 0.755 | |
| Medicare | 0.902 | 0.915 | |
| All other | 0.852 | 0.853 | |
| Eligibility for VA | |||
| Above means test | Ref | Ref | |
| Below means test, not service connected | 1.542 | 1.524 | |
| Service connected | 1.615 | 1.594 | |
| Other eligibility | 1.376 | 1.357 | |
| Chronic conditions | |||
| Diabetes | 1.115 | 1.117 | |
| Hypertension | 1.344 | 1.338 | |
| Ischemic heart disease | 1.393 | 1.385 | |
| Chronic renal failure | 1.901 | 1.868 | |
| Alzheimer’s disease | 1.377 | 1.363 | |
| Depression | 1.207 | 1.207 | |
| Post-traumatic stress disorder | 1.030 | 1.031 | |
| Alcohol use disorder | 1.280 | 1.282 | |
| Drug use disorder | 1.266 | 1.242 | |
| Other psychiatric conditions | 1.404 | 1.390 | |
All parameters in the table were statistically significant at p<0.001
Incident rate ratios were obtained from generalized linear regression models with a Poisson family distribution and log-link function. IRRs represent percent change in costs associated with a one-unit change in continuous variable or the percent change in costs relative to the reference category for categorical variables. Coefficients from facility dummies in models 2 and 3 are not shown in table.
In the fully adjusted model, older age was significantly associated with lower costs (P<0.001. Black patients had 5% higher costs than whites (P<0.001). Currently single marital status, higher service connection, and no other insurance were also significantly associated with higher costs (all P<0.001). All comorbid conditions were associated with higher costs for patients who had them compared to patients who did not (all P<0.001). Renal failure was associated with 87% higher mean costs compared to those who did not have this condition. After adjusting for all patient factors, the variation in mean costs of VA health care per patient ranged from $15,983 in the lowest-cost facility to $47,839 in the highest-cost facility (Figure 1).
Figure 1. Cost per Patient by VA Facility.
Average Adjusted Cost per Heart Failure Patient by VA Facility, FY2010. Average adjusted costs ranged widely between facilities, from approximately $15,000 to $48,000/patient.
Discussion
While a relatively small proportion of patients in the VA had heart failure, the annual costs of VA health care incurred by heart failure patients was high. VA costs varied considerably by patient sociodemographic characteristics, geography, comorbid conditions, and type of health services received during the year. Since most patients were elderly and covered by Medicare, mean annual VA health care costs decreased for age groups 60 years and older, in part, due to dual coverage since prior research has shown that dual enrollees shift care away from VA providers and towards Medicare providers as they age (23). Other patient factors such as being black or Hispanic, being unmarried, and more likely to have a service-connected disability were also associated with higher costs. These characteristics have been found previously to be associated with relatively more VA utilization and less non-VA utilization (24), so higher costs can represent worse health status and greater need for care or greater reliance on VA providers for health care. Patients in their last year of life also had considerably higher costs than patients who were not which was expected given the rising demand for care at the end of life.
A majority of VA costs for heart failure patients were attributed to inpatient health care, and most of this was due to medical/surgical care with patients having a mean number of one hospitalization during the year. Heart failure patients also had a substantial amount of costs from outpatient care for medical/surgical, pharmacy, and diagnostic care. Patients had both frequent primary care and specialty care visits during the year. Patient variation accounted for much of the variation in costs, so greater understanding of how certain patient characteristics influence resource utilization is needed.
High inpatient costs among heart failure patients highlights the importance of interventions to prevent hospitalizations as part of improving quality of care to heart failure patients, especially since previous work estimated that 60% of hospitalized heart failure patients have a readmission within 6 months (25, 26). Given the high rate of readmissions, there has been a lot of focus on improving post-acute care and ambulatory follow-up care in VA medical centers. Multiple studies have found that comprehensive discharge planning with discharge support and early follow up after discharge for patients with heart failure reduces readmissions (27, 28).
The high costs of patients with comorbid heart failure and renal failure highlight the challenges with co-managing renal failure and heart failure. Earlier research has also found that hospitalized patients with kidney disease are at subsequently higher risk for costly health services (4). Other comorbid conditions such as drug, alcohol, and psychiatric disorders were also associated with higher costs in our cohort which is consistent with literature on high health care use when mental health disorders are present among non-VA heart failure patients (5, 6). Currently, VA policy excludes patients with recent drug abuse from telehealth programs, so there should be alternative services or special considerations for heart failure patients with comorbid substance abuse problems to use existing services.
Since complexity of prescription drug regimens has been associated with comorbid conditions among heart failure patients (29), simplifying drug regimens and reducing inappropriate drug prescribing may both improve outcomes and reduce costs of care. VA-Medicare dual enrollees receive substantial amounts of both VA and Medicare services, so it is especially critical to monitor drug prescribing across providers and health care systems. While the VA’s national electronic medical records system can help foster some of this coordination between VA providers, additional mechanisms may be needed for coordination across health care systems.
There was significant variation in costs by VA facility where patients were treated. Although differences in costs between patients were mostly explained by patient factors, the wide variation between facilities suggests some opportunities to improve resource utilization in high-cost facilities. Previous research found that quality of care indicators varied across non-VA hospitals for heart failure patients, and several provider and hospital characteristics have been associated with treatment differences and costs (7, 8, 30). VA facilities had inter-facility differences in costs that may be due to a similar variation in treatment patterns. It is not clear whether lower performing providers are also associated with higher costs, so additional work is needed to determine this relationship. Nonetheless, quality-of-care initiatives for heart failure can be used to target care deficiencies in lower-performing facilities that can improve the efficiency of care and may ultimately decrease costs.
Limitations
We identified patients with heart failure based on diagnosis codes recorded in utilization records, so we may have undercounted patients with heart failure who did not have a diagnosis recorded in the current year. While many patients in the study were covered by Medicare, we did not include Medicare utilization and costs because we did not have this data available for our cohort. Estimating patient and facility variation in costs may be either underestimated or overestimated by not including non-VA costs of care. In this study we presented costs over a one-year period; however, the pattern in cost variation may be different over multiple years. Another limitation in this study is that we were not able to measure severity of heart failure across patients with our data, so it is possible that other patient factors were confounded with unmeasured severity and that VA facilities with more severely ill patients also had higher average costs. We did not have information on the time since diagnosis as our cohort included those newly diagnosed during the study year and those diagnosed in earlier years, so it is possible that patients newly diagnosed in the study year did not have a full year to measure heart failure treatment-related costs. While we examined inpatient and outpatient utilization in this study, we did not have access to data on laboratory tests or device use that may have provided additional information on disease severity and patterns of utilization. Our analysis also did not include specific facility factors such as size and academic affiliation that may have been important predictors of costs. Residual measured and unmeasured confounders could also influence these findings.
Conclusion
We found that among VA patients with heart failure, there is substantial variation across facilities in the VA cost of treating heart failure with close to four-fold variation between higher and lower cost facilities. Understanding how health care costs are related to both patient factors and facility can provide useful information to VA medical centers for understanding patterns in care and resource planning.
Supplementary Material
Mean Cost per VA Heart Failure Patient by Age Group, FY2010. Costs were highest for patients aged 50–59 years and lowest for patients aged 80 and above since costs decreased substantially as patients aged.
Mean Cost per VA Heart Failure Patient by Race/Ethnicity, FY2010. Costs were higher for Hispanic and Black Patients than for White Patients. Costs of Patients with Unknown Race/Ethnicity Had the Lowest Costs.
Clinical Perspectives.
Resource planning by VA medical centers can take into account the disproportionate share of resources used by patients who were younger, of Hispanic or black race/ethnicity, diagnosed with comorbid drug use disorders, and who died during the year. Since there was substantial variation across facilities in the VA cost of treating heart failure, facility-level initiatives can be used to improve the efficiency of care.
Translational Outlook.
Future work is needed to understand variation in heart failure costs and utilization across systems (e.g. Medicare), for specific patient treatment patterns (surgery and different medications), and by quality of care in different facilities.
Acknowledgments
Funding Sources
Funding/Support: This work was supported by the Chronic Heart Failure Quality Enhancement Research Initiative (QUERI) CHF 04-326 from the United States (U.S.) Department of Veterans Affairs Health Services Research and Development Service. The contents do not represent the views of the U.S. Department of Veterans Affairs or the United States Government. The funding agency had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation or review of the manuscript; or the decision to submit and approve the manuscript for publication.
The authors wish to thank Jennifer Scott for conducting data analysis.
Abbreviations
- VA
Veterans Affairs
- FY
Fiscal Year
- ICD
International Classification of Disease
- DRG
Diagnoses-Related Group
- DSS
Decision Support System
- VISN
VA Integrated Service Networks
Appendix
| Geographic Regions of Veterans Integrated Service Networks (VISN): |
|---|
| Northeast |
| VISN 1: VA New England Healthcare System |
| VISN 2: VA Health Care Upstate New York |
| VISN 3: VA NY/NJ Veterans Healthcare Network |
| VISN 4: VA Healthcare - VISN 4 |
| Southeast |
| VISN 5: VA Capitol Health Care Network |
| VISN 6: VA Mid-Atlantic Health Care Network |
| VISN7: VA Southeast Network |
| VISN 8: VA Sunshine Healthcare Network |
| Midsouth |
| VISN 9: VA Mid South Healthcare Network |
| VISN 15: VA Heartland Network |
| VISN 16: South Central VA Health Care Network |
| VISN 17: VA Heart of Texas Health Care Network |
| Central |
| VISN 10: VA Healthcare System of Ohio |
| VISN 11: Veterans In Partnership |
| VISN 12: VA Great Lakes Health Care System |
| VISN 23: VA Midwest Health Care Network |
| West |
| VISN 18: VA Southwest Health Care Network |
| VISN 19: Rocky Mountain Network |
| VISN 20: Northwest Network |
| VISN 21: Sierra Pacific Network |
| VISN 22: Desert Pacific Healthcare Network |
Footnotes
Disclosures
Fonarow reports potential conflict of interest pertaining to consulting work for Amgen (modest), Baxter (modest), Medtronic (significant), and Novartis (significant). Yoon, Groeneveld, Teerlink, Whooley, Sahay, and Heidenreich do not have any conflicts of interest to report.
References
- 1.Unroe KT, Greiner MA, Hernandez AF, et al. Resource use in the last 6 months of life among medicare beneficiaries with heart failure, 2000–2007. Arch Intern Med. 2011 Feb 14;171(3):196–203. doi: 10.1001/archinternmed.2010.371. [DOI] [PubMed] [Google Scholar]
- 2.Russo MJ, Gelijns AC, Stevenson LW, et al. The cost of medical management in advanced heart failure during the final two years of life. Journal of cardiac failure. 2008;14(8):651–8. doi: 10.1016/j.cardfail.2008.06.005. [DOI] [PubMed] [Google Scholar]
- 3.Dunlay SM, Shah ND, Shi Q, et al. Lifetime Costs of Medical Care After Heart Failure Diagnosis. Circulation: Cardiovascular Quality and Outcomes 2011. 2011 Jan 1;4(1):68–75. doi: 10.1161/CIRCOUTCOMES.110.957225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wexler DJ, Chen J, Smith GL, et al. Predictors of costs of caring for elderly patients discharged with heart failure. American heart journal. 2001;142(2):350–7. doi: 10.1067/mhj.2001.116476. [DOI] [PubMed] [Google Scholar]
- 5.Sullivan M, Simon G, Spertus J, Russo J. Depression-related costs in heart failure care. Archives of Internal Medicine. 2002;162(16):1860–6. doi: 10.1001/archinte.162.16.1860. [DOI] [PubMed] [Google Scholar]
- 6.Sayers SL, Hanrahan N, Kutney A, Clarke SP, Reis BF, Riegel B. Psychiatric comorbidity and greater hospitalization risk, longer length of stay, and higher hospitalization costs in older adults with heart failure. Journal of the American Geriatrics Society. 2007;55(10):1585–91. doi: 10.1111/j.1532-5415.2007.01368.x. [DOI] [PubMed] [Google Scholar]
- 7.Havranek EP, Wolfe P, Masoudi FA, Rathore SS, Krumholz HM, Ordin DL. PRovider and hospital characteristics associated with geographic variation in the evaluation and management of elderly patients with heart failure. Archives of Internal Medicine. 2004;164(11):1186–91. doi: 10.1001/archinte.164.11.1186. [DOI] [PubMed] [Google Scholar]
- 8.Fonarow GC, Yancy CW, Heywood J Adhere Scientific Advisory Committee Study Group and Investigators. Adherence to heart failure quality-of-care indicators in us hospitals: Analysis of the adhere registry. Archives of Internal Medicine. 2005;165(13):1469–77. doi: 10.1001/archinte.165.13.1469. [DOI] [PubMed] [Google Scholar]
- 9.Yoon J, Zulman D, Scott JY, Maciejewski ML. Costs Associated with Multimorbidity in VA Patients. Med Care. 2014;52(Suppl 3):S31–6. doi: 10.1097/MLR.0000000000000061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Phibbs CS, Bhandari A, Yu W, Barnett PG. Estimating the costs of VA ambulatory care. Med Care Res Rev. 2003 Sep;60(3 Suppl):54S–73S. doi: 10.1177/1077558703256725. [DOI] [PubMed] [Google Scholar]
- 11.Wagner TH, Chen S, Barnett PG. Using average cost methods to estimate encounter-level costs for medical-surgical stays in the VA. Med Care Res Rev. 2003 Sep;60(3 Suppl):15S–36S. doi: 10.1177/1077558703256485. [DOI] [PubMed] [Google Scholar]
- 12.Yu W, Wagner TH, Chen S, Barnett PG. Average cost of VA rehabilitation, mental health, and long-term hospital stays. Med Care Res Rev. 2003 Sep;60(3 Suppl):40S–53S. doi: 10.1177/1077558703256724. [DOI] [PubMed] [Google Scholar]
- 13.Bertoni AG, Hundley WG, Massing MW, Bonds DE, Burke GL, Goff DC. Heart failure prevalence, incidence, and mortality in the elderly with diabetes. Diabetes Care. 2004;27(3):699–703. doi: 10.2337/diacare.27.3.699. [DOI] [PubMed] [Google Scholar]
- 14.Bonneux L, Barendregt JJ, Meeter K, Bonsel GJ, van der Maas PJ. Estimating clinical morbidity due to ischemic heart disease and congestive heart failure: the future rise of heart failure. American Journal of Public Health. 1994;84(1):20–8. doi: 10.2105/ajph.84.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Evangelista LS, Doering LV, Dracup K. Usefulness of a history of tobacco and alcohol use in predicting multiple heart failure readmissions among veterans. The American Journal of Cardiology. 2000;86(12):1339–42. doi: 10.1016/s0002-9149(00)01238-8. [DOI] [PubMed] [Google Scholar]
- 16.Forman DE, Butler J, Wang Y, et al. Incidence, predictors at admission, and impact of worsening renal function among patients hospitalized with heart failure. Journal of the American College of Cardiology. 2004;43(1):61–7. doi: 10.1016/j.jacc.2003.07.031. [DOI] [PubMed] [Google Scholar]
- 17.Jiang W, Alexander J, Christopher E, et al. Relationship of depression to increased risk of mortality and rehospitalization in patients with congestive heart failure. Archives of Internal Medicine. 2001;161(15):1849–56. doi: 10.1001/archinte.161.15.1849. [DOI] [PubMed] [Google Scholar]
- 18.Lang CC, Mancini DM. Non-cardiac comorbidities in chronic heart failure. Heart. 2007;93(6):665–71. doi: 10.1136/hrt.2005.068296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Qiu C, Winblad B, Marengoni A, Klarin I, Fastbom J, Fratiglioni L. Heart failure and risk of dementia and alzheimer disease: A population-based cohort study. Archives of Internal Medicine. 2006;166(9):1003–8. doi: 10.1001/archinte.166.9.1003. [DOI] [PubMed] [Google Scholar]
- 20.Basu A, Manning WG. Issues for the next generation of health care cost analyses. Medical care. 2009;47(7_Supplement_1):S109–S14. doi: 10.1097/MLR.0b013e31819c94a1. [DOI] [PubMed] [Google Scholar]
- 21.Manning WG, Basu A, Mullahy J. Generalized modeling approaches to risk adjustment of skewed outcomes data. Journal of health economics. 2005;24(3):465–88. doi: 10.1016/j.jhealeco.2004.09.011. [DOI] [PubMed] [Google Scholar]
- 22.Zheng B, Agresti A. Summarizing the predictive power of a generalized linear model. Statistics in medicine. 2000;19(13):1771–81. doi: 10.1002/1097-0258(20000715)19:13<1771::aid-sim485>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 23.Liu C-F, Chapko M, Bryson CL, et al. Use of Outpatient Care in Veterans Health Administration and Medicare among Veterans Receiving Primary Care in Community-Based and Hospital Outpatient Clinics. Health Services Research. 2010;45(5p1):1268–86. doi: 10.1111/j.1475-6773.2010.01123.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hynes DM, Koelling K, Stroupe K, et al. Veterans’ access to and use of Medicare and Veterans Affairs health care. Med Care. 2007;45(3):214–23. doi: 10.1097/01.mlr.0000244657.90074.b7. [DOI] [PubMed] [Google Scholar]
- 25.Aranda JM, Jr, Johnson JW, Conti JB. Current trends in heart failure readmission rates: analysis of Medicare data. Clinical cardiology. 2009 Jan;32(1):47–52. doi: 10.1002/clc.20453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Krumholz HM, Parent EM, Tu N, et al. Readmission after hospitalization for congestive heart failure among Medicare beneficiaries. Archives of Internal Medicine. 1997;157(1):99–04. [PubMed] [Google Scholar]
- 27.Hernandez AF, Greiner MA, Fonarow GC, et al. Relationship between early physician follow-up and 30-day readmission among medicare beneficiaries hospitalized for heart failure. JAMA. 2010;303(17):1716–22. doi: 10.1001/jama.2010.533. [DOI] [PubMed] [Google Scholar]
- 28.Phillips CO, Wright SM, Kern DE, Singa RM, Shepperd S, Rubin HR. Comprehensive discharge planning with postdischarge support for older patients with congestive heart failure: A meta-analysis. JAMA. 2004;291(11):1358–67. doi: 10.1001/jama.291.11.1358. [DOI] [PubMed] [Google Scholar]
- 29.Masoudi FA, Baillie CA, Wang Y, et al. THe complexity and cost of drug regimens of older patients hospitalized with heart failure in the united states, 1998–2001. Archives of Internal Medicine. 2005;165(18):2069–76. doi: 10.1001/archinte.165.18.2069. [DOI] [PubMed] [Google Scholar]
- 30.Ziaeian B, Sharma PP, Yu TC, Johnson KW, Fonarow GC. Factors associated with variations in hospital expenditures for acute heart failure in the United States. Am Heart J. 2015 Feb;169(2):282–9. e15. doi: 10.1016/j.ahj.2014.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Mean Cost per VA Heart Failure Patient by Age Group, FY2010. Costs were highest for patients aged 50–59 years and lowest for patients aged 80 and above since costs decreased substantially as patients aged.
Mean Cost per VA Heart Failure Patient by Race/Ethnicity, FY2010. Costs were higher for Hispanic and Black Patients than for White Patients. Costs of Patients with Unknown Race/Ethnicity Had the Lowest Costs.