Abstract
Background
Adolescent smoking is a major public health concern, and current treatments are only somewhat effective in promoting abstinence. One way to improve treatments is to identify psychosocial characteristics that impede cessation, allowing development of targeted treatments. This study examined the influence of two such characteristics, life event stressors and coping, on initiation of cessation treatment and end-of-treatment abstinence status.
Methods
One-hundred five adolescent smokers were eligible to participate in a validated contingency management (CM) and cognitive-behavioral (CBT) cessation treatment; of those, 72 completed at least one treatment session. Data included sociodemographic characteristics, questionnaires assessing past year life events and coping behavior use, and abstinence status at the end of the 4-week treatment. Logistic regression was used to predict treatment initiation and abstinence status, with life event stressor number, coping or their interaction as predictors.
Results
Higher levels of cognitive and peer support coping predicted treatment initiation, while life events were unrelated. End-of-treatment abstinence was predicted by higher numbers of life events and greater use of avoidant coping. The interaction of helpless coping and life events also predicted abstinence, with greater increases in helpless coping as total life events rose in abstinent but not non-abstinent participants. Finally, greater use of behavioral coping predicted abstinence in participants exposed to only CM treatment, while lesser use of behavioral coping predicted abstinence in participants receiving combined CM/CBT treatment.
Conclusions
Exposure to life event stressors may promote cessation by forcing use of self-control resources prior to the quit attempt, which may strengthen such resources. Techniques that improve self-control resources may improve cessation outcome, and prevention programs may want to emphasize behavioral coping to improve rates of treatment initiation.
Introduction
Despite improvements, adolescent smoking remains a notable public health concern. Rates of adolescent smoking have decreased since peaks in the late 1990s1, but rates remain unacceptably high. In 2010, 19.2% of US high school seniors had smoked in the past month, with over half of those smoking daily. Almost 90% of adult smokers initiated smoking before the age of 18,2 indicating the importance of prevention and efforts to promote cessation in adolescence. Adolescent tobacco use is associated with symptoms of nicotine dependence,3 nicotine withdrawal4 and a host of physical health-related consequences.2, 5, 6 Adolescent smoking often co-occurs with,7, 8 and may lead to, other addictive substance use.9 Ultimately, conservative estimates indicate that 32% of current adolescent smokers will die from a smoking-related cause later in adulthood.10
The consequences of smoking may underlie findings that most adolescent smokers want to quit,11 with roughly 60% having attempted past year cessation .12 Natural rates of adolescent smoking cessation are low, however, as no more than 10% making a quit attempt achieve longer-term cessation.11 Abstinence rates are improved by treatment, but even with validated treatments, end-of-treatment cessation is usually achieved by less than 20% of adolescents, with continued declines at follow-up assessments.13, 14 Thus, there is a need for improvements in current treatments, perhaps by targeting specific characteristics that impede adolescent cessation. The first step, though, is to identify barriers to treatment initiation and cessation among adolescent smokers.
Two such characteristics could be exposure to a high level of life event stressors and coping behavior. Theoretically, life stressors increase distress, reduce self-control and motivation to undertake difficult tasks, and prompt coping.15, 16 While more adaptive coping (e.g., behavioral strategies) may ameliorate the stressor and associated distress, maladaptive coping (e.g., anger) may have no effect or even worsen distress. Substance use, including smoking, can be seen as coping, and may become a primary strategy in entrenched users. Life stressors may indirectly entrench smoking, as adolescents become reliant on the overlearned coping response of tobacco use,17 particularly if they are prone to other forms of ineffective coping. In adults, higher levels of past year life stressors increase the likelihood of relapse among former smokers and prevent abstinence in current smokers.18, 19 The role of coping in adulthood on cessation is equivocal, with evidence indicating that use of many different coping strategies20 and planning specific coping strategies prior to the quit attempt21 may aid cessation; conversely, no single type of coping is most effective,20 and real-time data point to a limited role for coping during quit attempts.22
In adolescents, higher numbers of life events and/or a greater likelihood of specific life events are found in smokers, as compared to non-smokers,23, 24 and initiation and persistence of smoking is predicted by higher numbers of life events.25, 26 For coping, lesser use of adaptive (e.g., cognitive) and greater use of maladaptive strategies (e.g., helplessness) differentiated adolescents by smoking status.27 Wills and colleagues24 found parental support and behavioral strategies were associated with a decreased likelihood of smoking, while use of anger as a coping strategy was associated with an increased likelihood. However, searches of relevant databases revealed no studies examining the influence of life stressors or coping strategies on adolescent cessation attempts. Furthermore, no relevant studies could be found that examined adolescent coping in smokers by more specific use indicators, such as nicotine dependence status or severity of smoking. That said, sex may affect adolescent coping, as females tend to use greater social support resources and avoidance than males.28
Aims and Hypotheses
The first aim of this work was to examine whether past year stressful life events and coping behavior use predicted entry into cessation treatment among adolescents who were eligible to enter treatment following an initial screening appointment. The second aim was to examine the effects of pre-treatment life events and coping on abstinence at the end of a school-based smoking cessation research intervention.29, 30 Finally, there were two exploratory aims: one, to evaluate the interaction of life events and coping on smoking cessation outcome and treatment initiation; and two, to evaluate whether number of past year life events or coping behavior interacted with treatment type (i.e., Cognitive-Behavioral Therapy [CBT] only, Contingency Management [CM] only or combined CM/CBT) to predict cessation outcome.
For the first aim, we hypothesized that fewer past year life events, higher levels of adaptive coping (e.g., behavioral) and lower levels of less adaptive coping (e.g., anger) would predict treatment initiation. For the second aim, we anticipated a similar pattern of results, with a lower number of life events, higher levels of adaptive coping and lower levels of less adaptive coping predicting end-of-treatment abstinence. Finally, we did not posit a priori hypotheses for the exploratory aims, given the lack of any research on the examined interactions.
Methods
Participants
For this investigation, participants were grouped in one of two ways, with all adolescents who were eligible to participate included in one set of analyses, and participants who initiated treatment included in a separate set. One-hundred fifty-seven adolescents consented to enter treatment, with 51 deemed ineligible because of below threshold smoking or significant psychiatric illness. One individual did not have an age listed, excluding this person from analyses. Nine (8.6%) of the eligible 105 participants had one missing Life Events Questionnaire for Adolescents (LEQ-A) item; that item was imputed using the average of other subscale items or, for those items not in a subscale, the entire scale. Five eligible individuals (4.8%) did not complete the Response–based Coping Inventory (RBCI) and were excluded from RBCI-based analyses, and two others (1.9%) were missing one subscale and were excluded from analyses involving that subscale.
Across the eligible sample of 105 adolescents, 45.9% were female and 91.4% were Caucasian, with a mean age of 16.53 (SD= 1.32, range= 14-20 years). Seventy-two adolescents entered treatment, with four not completing any of the RBCI (5.6%). In the treatment sample, 52.8% were female and 91.7% were Caucasian, with a mean age of 16.50 (SD= 1.41, range= 14-20 years). Twenty-one (29.2%) received CM-only, 23 (31.9%) received CBT-only and 28 (38.9%) received combined treatment. Participant characteristics by group are listed in Table 1.
Table 1. Sociodemographic, Tobacco Use and Other Substance Use Characteristics by Group.
| Non-Initiators (n = 33) |
Treatment Initiators (n = 72) |
Abstinent (n = 17) |
Non-Abstinent (n = 55) |
|
|---|---|---|---|---|
| Female (%) | 42.4% (n = 14) | 42.8% (n = 38) | 41.2% (n = 7) | 56.4% (n = 31) |
| Age | 16.63 ± 1.13 | 16.55 ± 1.41 | 16.69 ± 1.20 | 16.51 ± 1.48 |
| Caucasian (%) | 90.9% (n = 30) | 91.7% (n = 66) | 82.4% (n = 14) | 94.5% (n = 52) |
| mFTQ score | 3.49 ± 1.32 | 3.47 ± 1.44 | 2.77 ± 1.28 | 3.69 ± 1.43 |
| CPD | 13.75 ± 5.25 | 14.08 ± 6.28 | 11.61 ± 5.20 | 14.83 ± 6.43 |
| Alcohol Use Days | 2.28 ± 2.45 | 2.00 ± 2.51 | 2.94 ± 2.93 | 1.72 ± 2.32 |
| Marijuana Use Days | 9.16 ± 11.80 | 10.20 ± 11.43 | 8.75 ± 9.67 | 10.64 ± 11.95 |
Procedures
Data for this study came from an investigation into the efficacy of a CM and CBT based smoking cessation intervention for adolescent smokers. Intervention details are described in detail elsewhere.29-31 Participants attended selected high schools in Northeastern region of the U.S., with assent/consent obtained through passive parental permission. Adolescents who appeared eligible to participate were met at their school for an initial screening session where they completed the self-report questionnaires of interest for this study in a school office with only the research assistant present. Adolescents were eligible for participation in the cessation study if they were treatment-seeking daily cigarette smokers with baseline urine cotinine levels of 350 ng/ml or greater. Eligible participants were randomized to one of three treatment groups: (1) CM-only; (2) CBT-only; or (3) combined CM/CBT. CM meetings occurred daily, while CBT sessions were once weekly for 30 minutes.
Measures
All measures used in this study, with the exception of one-week point prevalence abstinence, were collected at the initial screening session (see above), prior to randomization to treatment group and treatment initiation.
One-Week Point Prevalence Abstinence at 4 Weeks
Participants were abstinent if they denied past week cigarette smoking with a qualitative urine cotinine of 100 ng/μL or lower (Graham-Massey Laboratories, Shelton, CT).
Life Events Questionnaire for Adolescents32 (LEQ-A)
The LEQ-A 67-item is a self-report measure of the presence or absence of past year stressful life events. We combined items 33 and 34, which assess pregnancy differentially by gender. The LEQ-A provides a total score and six subscales, coded by discreteness of event onset (chronic or discrete), desirability (positive, negative or ambiguous) and level of control the adolescent had (none/independent or some control/non-independent). Across the sample, the internal consistency (Cronbach's α of the LEQ-A was .82; Cronbach's α values for the subscales were all below .65. Because of the low internal consistencies of the original LEQ-A subscales, these were excluded from analyses. Instead, subscales were created to examine events labeled as independent, non-independent, chronic, discrete-onset or negative (other types had too few questions). The independent (.72) and negative events (.76) had acceptable internal consistencies and were used in analyses.
Coping
The Response–based Coping Inventory (RBCI) is a 47-item self-report 33 that uses intention-based assessment.34 The RBCI contains eight coping subscales: behavioral, cognitive, avoidant, angry, helpless, substance use, seeking peer support and seeking parental support. Unpublished factor analysis by this research group in a different sample indicates that the RBCI generally fit this subscale structure. The substance use subscale was omitted here because of low internal consistency (.44). For the other subscales, Cronbach's α values ranged between .95 (parental support) and .88 (avoidant) in the entire sample.
Sociodemographic Information
Participants provided information about age, sex and race/ethnicity.
Modified Fagerstrom Tolerance Questionnaire (mFTQ) 35, 36 and Timeline Follow-back37 measured nicotine dependence and number of days of alcohol or marijuana use in the past 28 days. These were included as covariates in regression models.
Data Analysis
Participants who were eligible to participate but did not enter treatment were compared to those who entered treatment on sociodemographic characteristics. Chi-square was used to compare sex, Mann-Whiney U was used to compare ethnicity and an independent samples t-test was used to compare age. Two sets of primary analyses were conducted, following the same plan (below): one to examine differences between those who did and did not initiate treatment and one to examine differences in end-of-treatment abstinence status among those entering treatment.
First, we examined differences in number of past year stressful life events (i.e., LEQ-A score) based on treatment initiation or cessation outcome. If significant differences between groups were found, follow-up analyses tested for differences in LEQ-A independent or negative events. Second, we examined differences in the RBCI subscales based on treatment initiation or cessation outcome. If a significant difference was found for LEQ-A score, interaction analyses examined whether total number of stressful life events interacted with the RBCI subscales. Finally, the interaction of LEQ-A score or RCBI subscale and treatment type was examined in terms of cessation outcome at 4 weeks.
Analyses used the LOGISTIC REGRESSION command in IBM SPSS Statistics version 20, with treatment initiation group or cessation outcome as the dependent variable and LEQ-A or RBCI score as primary predictor (independent) variable. RCBI analyses were multivariate (i.e., all subscales were included) while the LEQ-A analysis was univariate. All analyses controlled for sex, age, mFTQ score and days of alcohol and marijuana use in the past 28 days; race/ethnicity was not controlled for since Caucasian participants composed over 90% of both samples. Analyses that examined cessation outcome also included treatment group (e.g., CM-only, CBT-only or combined treatment) as a between-subject factor. Interactions between LEQ-A score and RBCI subscale entered control variables in block one, LEQ-A score and RBCI subscale of interest in block two, and the interaction term in block three.
Results
Differences Based on Treatment Initiation: Sociodemographics
Of eligible participants, 72 (68.6%) initiated treatment, while 33 (31.4%) did not. No differences were found in any sociodemographic characteristics by treatment initiation status: sex, χ 2(1, N= 105)= .97, p= .33; race/ethnicity, Mann-Whitney U= 1181.5, Z= -.09, p= .93; or age, t(103)= .38, p= .71).
Differences Based on Treatment Initiation: Stressful Life Events
All means, standard deviations and inferential statistics (excluding odds ratios and 95% confidence intervals) for differences based on treatment initiation are in Table 2. No difference in total LEQ-A score was found between those who did and those who did not initiate treatment, odds ratio (OR)= 1.01, 95% confidence interval (95%CI)= 0.94-1.08.
Table 2. Differences in Life Events and Coping between Treatment Initiators and Non-initiators.
| Initiator M (n = 72; 68.6%) |
Non-Initiator M (n = 33; 31.4%) |
B | SE | Wald χ2 | p | Odds Ratio | 95% CI | |
|---|---|---|---|---|---|---|---|---|
| LEQ (life events) | 12.36 ± 7.55 | 11.55 ± 5.59 | .007 | .035 | .040 | .842 | 1.007 | 0.94-1.08 |
| RCBI (coping) | ||||||||
| Behavioral | 20.11 ± 5.63 | 16.35 ± 6.09 | .108 | .043 | 6.421 | .011 | 1.114 | 1.03-1.21 |
| Cognitive | 18.88 ± 5.95 | 16.47 ± 6.78 | .065 | .036 | 3.153 | .076 | 1.067 | 0.99-1.15 |
| Parental Support | 10.94 ± 5.32 | 8.88 ± 5.20 | .070 | .044 | 2.485 | .115 | 1.073 | 0.98-1.17 |
| Peer Support | 13.82 ± 4.56 | 11.50 ± 4.91 | .119 | .052 | 5.214 | .022 | 1.127 | 1.02-1.25 |
| Avoidant | 32.12 ± 8.82 | 28.79 ± 11.30 | .036 | .024 | 2.240 | .134 | 1.037 | 0.99-1.09 |
| Anger | 13.18 ± 5.50 | 13.16 ± 5.68 | .002 | .044 | .003 | .959 | 1.00 | 0.92-1.09 |
| Helpless | 7.53 ± 3.57 | 7.34 ± 3.60 | .014 | .065 | .045 | .832 | 1.014 | 0.89-1.15 |
Notes: LEQ = Life Events Questionnaire – Adolescent; RCBI = Response-based Coping Inventory; M = Mean (± Standard Deviation); SE = Standard Error; CI = Confidence Interval
Bolded, italicized text denotes significant findings at a p ≤ .05 level
Differences Based on Treatment Initiation: Coping
Two significant differences were found on RBCI subscales between treatment initiators and non-initiators. First, initiators had higher levels of behavioral coping than non-initiators, OR= 1.11, 95%CI= 1.03-1.21, with an 11% increase in odds of treatment enrollment for every point increase in behavioral coping. Also, initiators made greater use of peer support than non-initiators OR= 1.13, 95%CI= 1.02-1.25, with a 13% increase in enrollment odds for each point increase in peer support. Also cognitive coping displayed a trend-level difference, OR= 1.07, 95%CI= 0.99-1.15, with higher levels of cognitive coping in treatment initiators.
Differences Based on Cessation Outcome at 4 Weeks: Stressful Life Events
Statistics for differences by end-of-treatment abstinence status (except for ORs and 95%CIs) are in Table 3. Seventeen (23.6%) of the 72 participants who initiated treatment were abstinent at the end of treatment, with 10 abstinent in the CM/CBT group (35.7% of the group) and 7 in the CM-only group (33.3% of the group); no participants in the CBT-only group were abstinent at 4 weeks. No significant difference (p < .05) was found between treatment groups in number of stressful life events. Participants who achieved one-week of point prevalence abstinence at week 4 had a greater number of total life events than those who did not achieve abstinence, OR= 0.89, 95%CI= 0.80-0.98, with an 11% increase in cessation odds with each past year stressful life event. Follow-up analyses of the LEQ-A indicated that abstinent participants had more independent stressful events, OR= 0.74, 95%CI= 0.59-0.92, and more negative stressful events, OR= 0.83, 95%CI= 0.71-0.98. Each independent event increased odds of cessation by 23%, and each negative event increased odds by 17%.
Table 3. Differences in Life Events and Coping based on End-of-Treatment (4-week) Cessation Status.
| Abstinent M (n = 17; 23.6%) |
Non-Abstinent M (n = 55; 76.4%) |
B | SE | Wald χ2 | p | Odds Ratio | 95% CI | |
|---|---|---|---|---|---|---|---|---|
| LEQ (life events) | 15.71 ± 10.07 | 11.32 ± 6.35 | -.122 | .052 | 5.494 | .019 | 0.885 | 0.80-0.98 |
| Negative Events | 9.41 ± 6.37 | 7.03 ± 4.37 | -.186 | .083 | 5.096 | .024 | 0.830 | 0.71-0.98 |
| Independent Events | 6.18 ± 5.43 | 3.59 ± 2.74 | -.308 | .114 | 7.276 | .007 | 0.735 | 0.59-0.92 |
| RCBI (coping) | ||||||||
| Behavioral | 19.81 ± 6.05 | 20.20 ± 5.55 | .080 | .085 | 0.877 | .349 | 1.083 | 0.92-1.28 |
| Cognitive | 18.00 ± 4.03 | 19.15 ± 6.44 | .112 | .086 | 1.706 | .191 | 1.118 | 0.95-1.32 |
| Parental Support | 11.25 ± 5.63 | 10.85 ± 5.28 | -.046 | .083 | 0.305 | .581 | 0.955 | 0.81-1.12 |
| Peer Support | 13.44 ± 3.67 | 13.94 ± 4.83 | -.010 | .118 | 0.007 | .933 | 0.990 | 0.79-1.25 |
| Avoidant | 36.00 ± 6.61 | 30.92 ± 9.12 | -.152 | .059 | 6.524 | .011 | 0.859 | 0.77-0.97 |
| Anger | 12.81 ± 4.64 | 13.29 ± 5.78 | .064 | .095 | 0.456 | .499 | 1.066 | 0.89-1.28 |
| Helpless | 7.81 ± 3.27 | 7.44 ± 3.69 | .092 | .142 | 0.413 | .520 | 1.096 | 0.83-1.45 |
Notes: LEQ = Life Events Questionnaire – Adolescent; RCBI = Response-based Coping Inventory; M = Mean (± Standard Deviation); SE = Standard Error; CI = Confidence Interval
Bolded, italicized text denotes significant findings at a p ≤ .05 level
Differences Based on Cessation Outcome at 4 Weeks: Coping
No significant differences (ps < .05) were found between treatment groups in coping behavior. Analyses of coping differences on the RBCI indicated that only scores on the avoidant coping subscale differed between abstinent and non-abstinent participants, OR= 0.86, 95%CI= 0.77-0.97. Abstinent participants engaged in higher levels of avoidant coping, with a 14% increase in odds of cessation for each point on the avoidant subscale.
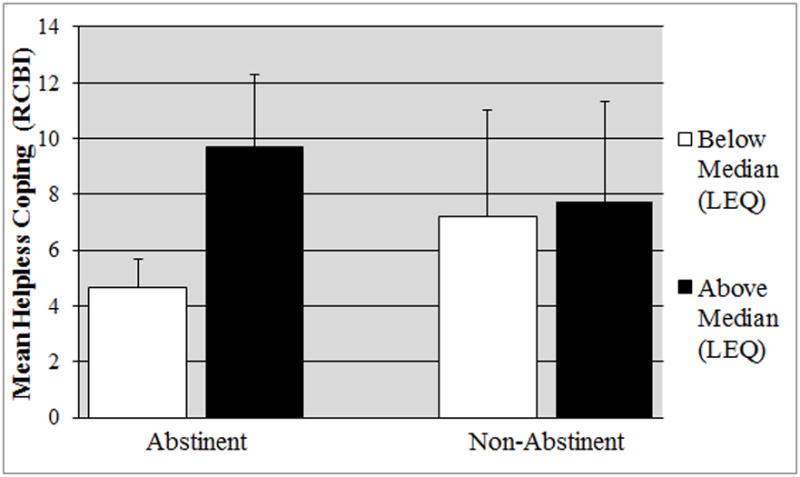
Interaction of Coping and Stressful Life Events on Cessation Outcome at 4 Weeks
Only one interaction between number of past year stressful life events and RBCI subscale was found. Helpless coping interacted with LEQ score, B= -.06, SE= .03, Wald χ 2= 4.12, p= .042, such that abstinent individuals engaged in relatively little helpless coping if they had a below median number of life events (4.67±1.03) and a much higher amount of helpless coping when they had an above median number of stressful life events (9.70±2.58). Non-abstinent participants had an intermediate use of helpless coping whether they experienced a below median number (7.21±3.80) or an above median number of life events (7.74±3.60). This is illustrated in Figure 1.
Figure 1.
Interaction between helpless coping and stressful life events on smoking cessation outcome.
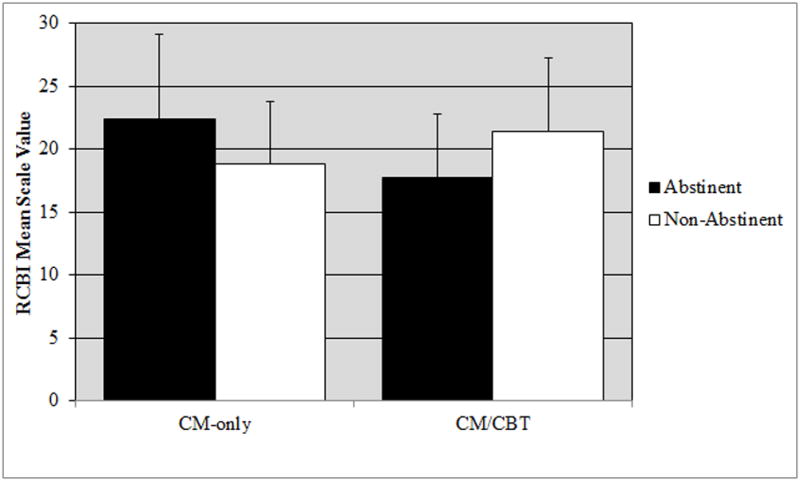
Interaction of Coping or Stressful Life Events and Treatment Group on Cessation Outcome at 4 Weeks
Since no participants in the CBT-only group achieved cessation at 4 weeks, only the CM-only and CM/CBT treatment groups were examined for the interaction of coping or stressful life events and treatment on cessation outcome. These analyses indicated that behavioral coping interacted with treatment type, B= -.352, SE= .16, Wald χ 2= 4.87, p= .027. Cessation was more likely in CM-only participants with greater behavioral coping (abstinent: 22.43±6.66; non-abstinent: 18.79±4.95), while the opposite was true in CM/CBT participants (abstinent: 17.78±4.97; non-abstinent: 21.41±5.85). This is illustrated in Figure 2.
Figure 2.
Interaction between treatment type and behavioral coping on smoking cessation outcome.
Also, peer support and cognitive coping had trend-level interactions with treatment type (peer support: B= -.408, SE= .21, Wald χ 2= 3.63, p= .057; peer support: B= -.303, SE= .17, Wald χ 2= 3.10, p= .078). Abstinent CM-only participants used greater levels of peer support than non-abstinent participants (abstinent: 14.71±3.40; non-abstinent: 13.00±4.72), while abstinent CM/CBT participants used less peer support than non-abstinent participants (abstinent: 12.44±3.75; non-abstinent: 16.29±3.41). For cognitive coping, CM-only participants were similar in cognitive coping use across abstinence status (abstinent: 18.00±3.90; non-abstinent: 18.71±6.62), while abstinent CM/CBT participants used greater levels than non-abstinent participants (abstinent: 17.89±4.57; non-abstinent: 21.71±5.00).
Discussion
In general, the hypotheses were not supported. While initiation of cessation treatment was more likely in those who used higher levels of behavioral coping, no support was found for many of the predicted effects of life event stressors and coping on treatment initiation or cessation outcome. Unexpectedly, end-of-treatment abstinence was predicted by higher levels of past year life events and avoidant coping. Exploratory analyses indicated that abstinence was predicted by higher levels of stressful life events combined with higher levels of baseline helpless coping or lower levels of past year life event stressors and lower levels of helpless coping; non-abstinent adolescents had intermediate levels of helpless coping, regardless of level of past year life events. Finally, behavioral coping interacted with treatment type for cessation at 4 weeks, with abstinent participants in the CM-only group using behavioral coping more frequently than non-abstinent participants; this pattern was reversed in CM/CBT participants.
Contrary to work in adults,18, 19 higher levels of life event stressors predicted abstinence at the end of a 4-week CM/CBT smoking cessation treatment. One explanation may be that adolescents with greater life stressors may value either the monetary rewards of CM or the therapeutic interaction of CBT more than other adolescents because of the likely reduction in other reinforcing events occurring in the environment of teens with greater numbers of stressful life events. CM-based reinforcers may replace some of the unavailable contingent rewards in adolescents with greater numbers of stressful life events, particularly incentivizing cessation success in order to maintain reinforcer availability. Alternatively, the work of Baumeister and colleagues38 indicates that willpower or self-control is a dynamic resource that can be depleted, restored and, through use of the resource, strengthened. Adolescents with higher levels of past year life events may have had greater opportunities to exercise self-control, strengthening it. This is quite speculative, however, and further research would need to better evaluate this possibility.
Many of the coping results for treatment initiation were predicted (e.g., behavioral), but the peer support result was not necessarily anticipated. Peer support is an equivocal coping strategy vis-à-vis helping individuals resist maladaptive behaviors. Abstinent peers can promote cessation,39, 40 but peers who smoke discourage abstinence.41, 42 More unexpected was that greater use of avoidant coping encouraged cessation success. Examination of the specific avoidant coping questions indicates that many of these questions tap distraction (e.g., “I try to distract myself from the problem”), which is a relatively common adolescent cessation coping strategy.43 Distraction may help adolescents attempting cessation avoid focusing on the adverse symptoms of nicotine withdrawal and craving, as has been posited about similar results in adult substance users.15 Furthermore, while greater use of behavioral coping in abstinent CM-only participants was understandable given the intensity of behavioral intervention in CM, the increased use of peer support in abstinent CM-only participants was surprising. Perhaps peer support replaces the relationship between therapist and participant, supplying empathic support in the cessation attempt.
Clinical Implications
As noted previously, avoidance may serve as a proxy for distraction. While not a perfect analogue, mindfulness strategies could help adolescents attempting cessation by increasing their ability to disengage from nicotine withdrawal sensations and craving. Indeed, mindfulness appears to help adults attempting cessation.44 Assessing behavioral coping prior to the quit attempt may also help improve cessation rates, as CM-only treatment was most effective in those with greater behavioral coping and treatment including CBT was most effective in those with lesser levels of behavioral coping. Finally, the finding that initiation of treatment was more likely in those with higher levels of peer support coping may indicate that use of peers to encourage treatment enrollment may help teens who are considering cessation.
Limitations and Strengths
Five limitations should be noted. First, coping strategy use may have changed during treatment with CBT in some adolescents, confounding the results slightly. One of the major aims of CBT for substance use is to promote adaptive coping,45 so coping changes are somewhat likely. Second, some data was missing for roughly 12% of individuals, potentially affecting results. Third, the sample was over 90% Caucasian, limiting generalizability to similar samples. Fourth, factors associated with entry into research-based cessation interventions may differ from those for naturalistic treatment, arguing for some caution in interpreting the treatment initiation results. Finally, post hoc power analyses indicated that the analyses of interaction effects are likely to be underpowered to detect significant results with small effect sizes. That said, this work was also strengthened by its use of a validated smoking cessation intervention, through having a wide age range of adolescents, a nearly even number of male and female participants, and its prospective design.
Conclusion
This investigation found that higher numbers of life event stressors and greater use of avoidant coping predicted smoking cessation in adolescents participating in a validated CM/CBT cessation treatment. These findings may indicate that use of distraction techniques (similar to avoidance) may help adolescents attempting cessation. Both of these hypotheses need to be evaluated in future research. More expected was that use of more adaptive coping, especially behavioral coping, promoted entry to the cessation intervention. Together, it is hoped that these results will help refine current adolescent smoking cessation treatments, reducing the significant harm and societal cost of adolescent smoking.
Acknowledgments
Funding: Preparation of this manuscript was supported by NIH grant P50 DA009421. NIH (National Institute on Drug Abuse) had no further role in study design, the collection, analysis or interpretation of data, the writing of the report, or the decision to submit the paper for publication. The authors declare that they have no conflicts of interest.
Footnotes
Author Contributions: This manuscript was derived from a parent study designed by SKS and DAC, with conception and design of this particular investigation by TSS. TSS, DAC, GK, TL and AL participated in the data collection for this study. All analyses were performed by TSS, and TSS was also the primary author of this manuscript. All authors participated in the editing process for this manuscript, and all authors approved of its final submission.
References
- 1.Johnston LD, O'Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future national survey results on drug use, 1975–2010: Volume I, Secondary school students. Ann Arbor, MI: Institute for Social Research, The University of Michigan; 2011. [Google Scholar]
- 2.U.S. Department of Health and Human Services. Preventing Tobacco Use Among Youth and Young Adults: A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2012. [Google Scholar]
- 3.Zhan W, Dierker LC, Rose JS, Selya A, Mermelstein RJ. The Natural Course of Nicotine Dependence Symptoms Among Adolescent Smokers. Nicotine Tob Res. 2012 doi: 10.1093/ntr/nts031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Smith AE, Cavallo DA, McFetridge A, Liss T, Krishnan-Sarin S. Preliminary examination of tobacco withdrawal in adolescent smokers during smoking cessation treatment. Nicotine Tob Res. 2008;10(7):1253–1259. doi: 10.1080/14622200802219357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Martinez JA, Mota GA, Vianna ES, Filho JT, Silva GA, Rodrigues AL., Jr Impaired quality of life of healthy young smokers. Chest. 2004;125(2):425–428. doi: 10.1378/chest.125.2.425. [DOI] [PubMed] [Google Scholar]
- 6.Prokhorov AV, Emmons KM, Pallonen UE, Tsoh JY. Respiratory response to cigarette smoking among adolescent smokers: a pilot study. Prev Med. 1996;25(5):633–640. doi: 10.1006/pmed.1996.0099. [DOI] [PubMed] [Google Scholar]
- 7.O'Cathail SM, O'Connell OJ, Long N, et al. Association of cigarette smoking with drug use and risk taking behaviour in Irish teenagers. Addictive behaviors. 2011;36(5):547–550. doi: 10.1016/j.addbeh.2011.01.012. [DOI] [PubMed] [Google Scholar]
- 8.McCambridge J, Strang J. Age of first use and ongoing patterns of legal and illegal drug use in a sample of young Londoners. Substance Use and Misuse. 2005;40(3):313–319. doi: 10.1081/ja-200049333. [DOI] [PubMed] [Google Scholar]
- 9.Mayet A, Legleye S, Chau N, Falissard B. Transitions between tobacco and cannabis use among adolescents: a multi-state modeling of progression from onset to daily use. Addictive behaviors. 2011;36(11):1101–1105. doi: 10.1016/j.addbeh.2011.06.009. [DOI] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. Projected smoking-related deaths among youth - United States. MMWR Morb Mortal Wkly Rep. 1996;45(44):971–974. [PubMed] [Google Scholar]
- 11.Burt RD, Peterson AV., Jr Smoking cessation among high school seniors. Preventive Medicine. 1998;27(3):319–327. doi: 10.1006/pmed.1998.0269. [DOI] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention. High school students who tried to quit smoking cigarettes - United States, 2007. Morbidity and Mortality Weekly Report. 2009;58(16):428–431. [PubMed] [Google Scholar]
- 13.Schepis TS, Rao U. Smoking cessation for adolescents: a review of pharmacological and psychosocial treatments. Current Drug Abuse Reviews. 2008;1(2):142–154. doi: 10.2174/1874473710801020142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sussman S. Effects of sixty six adolescent tobacco use cessation trials and seventeen prospective studies of self-initiated quitting. Tobacco Induced Diseases. 2002;1(1):35–81. doi: 10.1186/1617-9625-1-1-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moos RH. Theory-based processes that promote the remission of substance use disorders. Clinical psychology review. 2007;27(5):537–551. doi: 10.1016/j.cpr.2006.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moos RH. Theory-based active ingredients of effective treatments for substance use disorders. Drug Alcohol Depend. 2007;88(2-3):109–121. doi: 10.1016/j.drugalcdep.2006.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schepis TS, Adinoff B, Rao U. Neurobiological processes in adolescent addictive disorders. The American journal on addictions / American Academy of Psychiatrists in Alcoholism and Addictions. 2008;17(1):6–23. doi: 10.1080/10550490701756146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McKee SA, Maciejewski PK, Falba T, Mazure CM. Sex differences in the effects of stressful life events on changes in smoking status. Addiction. 2003;98(6):847–855. doi: 10.1046/j.1360-0443.2003.00408.x. [DOI] [PubMed] [Google Scholar]
- 19.Siahpush M, Carlin JB. Financial stress, smoking cessation and relapse: results from a prospective study of an Australian national sample. Addiction. 2006;101(1):121–127. doi: 10.1111/j.1360-0443.2005.01292.x. [DOI] [PubMed] [Google Scholar]
- 20.O'Connell KA, Hosein VL, Schwartz JE, Leibowitz RQ. How does coping help people resist lapses during smoking cessation? Health psychology : official journal of the Division of Health Psychology, American Psychological Association. 2007;26(1):77–84. doi: 10.1037/0278-6133.26.1.77. [DOI] [PubMed] [Google Scholar]
- 21.van Osch L, Lechner L, Reubsaet A, Wigger S, de Vries H. Relapse prevention in a national smoking cessation contest: effects of coping planning. British journal of health psychology. 2008;13(Pt 3):525–535. doi: 10.1348/135910707X224504. [DOI] [PubMed] [Google Scholar]
- 22.Minami H, McCarthy DE, Jorenby DE, Baker TB. An Ecological Momentary Assessment analysis of relations among coping, affect and smoking during a quit attempt. Addiction. 2011;106(3):641–650. doi: 10.1111/j.1360-0443.2010.03243.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ozge C, Toros F, Bayramkaya E, Camdeviren H, Sasmaz T. Which sociodemographic factors are important on smoking behaviour of high school students? The contribution of classification and regression tree methodology in a broad epidemiological survey. Postgraduate medical journal. 2006;82(970):532–541. doi: 10.1136/pgmj.2005.040360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wills TA, Resko JA, Ainette MG, Mendoza D. Smoking onset in adolescence: a person-centered analysis with time-varying predictors. Health psychology : official journal of the Division of Health Psychology, American Psychological Association. 2004;23(2):158–167. doi: 10.1037/0278-6133.23.2.158. [DOI] [PubMed] [Google Scholar]
- 25.Booker CL, Unger JB, Azen SP, Baezconde-Garbanati L, Lickel B, Johnson CA. Stressful life events and smoking behaviors in Chinese adolescents: a longitudinal analysis. Nicotine Tob Res. 2007;9(11):1085–1094. doi: 10.1080/14622200701491180. [DOI] [PubMed] [Google Scholar]
- 26.Rao U, Hammen CL, London ED, Poland RE. Contribution of hypothalamic-pituitary-adrenal activity and environmental stress to vulnerability for smoking in adolescents. Neuropsychopharmacology. 2009;34(13):2721–2732. doi: 10.1038/npp.2009.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Siqueira L, Diab M, Bodian C, Rolnitzky L. Adolescents becoming smokers: the roles of stress and coping methods. The Journal of adolescent health : official publication of the Society for Adolescent Medicine. 2000;27(6):399–408. doi: 10.1016/s1054-139x(00)00167-1. [DOI] [PubMed] [Google Scholar]
- 28.Recklitis CJ, Noam GG. Clinical and developmental perspectives on adolescent coping. Child psychiatry and human development. 1999;30(2):87–101. doi: 10.1023/a:1021998217862. [DOI] [PubMed] [Google Scholar]
- 29.Cavallo DA, Cooney JL, Duhig AM, et al. Combining cognitive behavioral therapy with contingency management for smoking cessation in adolescent smokers: a preliminary comparison of two different CBT formats. American Journal on Addictions. 2007;16(6):468–474. doi: 10.1080/10550490701641173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Krishnan-Sarin S, Duhig AM, McKee SA, et al. Contingency management for smoking cessation in adolescent smokers. Experimental and clinical psychopharmacology. 2006;14(3):306–310. doi: 10.1037/1064-1297.14.3.306. [DOI] [PubMed] [Google Scholar]
- 31.Krishnan-Sarin S, Cavallo DA, Cooney JL, et al. An exploratory randomized controlled trial of a novel high-school-based smoking cessation intervention for adolescent smokers using abstinence-contingent incentives and cognitive behavioral therapy. Drug Alcohol Depend. 2013;132(1-2):346–351. doi: 10.1016/j.drugalcdep.2013.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Masten AS, Neemann J, Andenas S. Life events and adjustment in adolescents: The significance of event independence, desirability and chronicity. Journal of Research on Adolescence. 1994;4(1):71–97. [Google Scholar]
- 33.Wills TA. Stress and coping in early adolescence: relationships to substance use in urban school samples. Health psychology : official journal of the Division of Health Psychology, American Psychological Association. 1986;5(6):503–529. doi: 10.1037//0278-6133.5.6.503. [DOI] [PubMed] [Google Scholar]
- 34.Stone AA, Neale JM. New measure of daily coping: Development and preliminary results. Journal of personality and social psychology. 1984;46(4):892–906. [Google Scholar]
- 35.Prokhorov AV, Pallonen UE, Fava JL, Ding L, Niaura R. Measuring nicotine dependence among high-risk adolescent smokers. Addictive behaviors. 1996;21:117–127. doi: 10.1016/0306-4603(96)00048-2. [DOI] [PubMed] [Google Scholar]
- 36.Pomerleau CS, Carton SM, Lutzke ML, Flessland KA, Pomerleau OF. Reliability of the Fagerstrom Tolerance Questionnaire and the Fagerstrom Test for Nicotine Dependence. Addictive behaviors. 1994;19:33–39. doi: 10.1016/0306-4603(94)90049-3. [DOI] [PubMed] [Google Scholar]
- 37.Sobell LC, Sobell MB. Timeline Follow-back: A technique for assessing self-reported alcohol consumption. In: Litten R, Allen J, editors. Measuring alcohol consumption. Rockville, MD: The Humana Press Inc; 1992. pp. 207–224. [Google Scholar]
- 38.Baumeister RF, Alquist JL. Self-regulation as a limited resource: Strength model of control and depletion. In: Forgas JP, Baumeister RF, Tice DM, editors. Psychology of self-regulation: Cognitive, affective, and motivational processes. New York, NY US: Psychology Press; 2009. pp. 21–33. [Google Scholar]
- 39.Chen PH, White HR, Pandina RJ. Predictors of smoking cessation from adolescence into young adulthood. Addictive behaviors. 2001;26(4):517–529. doi: 10.1016/s0306-4603(00)00142-8. [DOI] [PubMed] [Google Scholar]
- 40.Fagan P, Eisenberg M, Frazier L, Stoddard AM, Avrunin JS, Sorensen G. Employed adolescents and beliefs about self-efficacy to avoid smoking. Addictive behaviors. 2003;28(4):613–626. doi: 10.1016/s0306-4603(02)00227-7. [DOI] [PubMed] [Google Scholar]
- 41.Pallonen UE, Prochaska JO, Velicer WF, Prokhorov AV, Smith NF. Stages of acquisition and cessation for adolescent smoking: an empirical integration. Addictive behaviors. 1998;23(3):303–324. doi: 10.1016/s0306-4603(97)00074-9. [DOI] [PubMed] [Google Scholar]
- 42.Wills TA, Windle M, Cleary SD. Temperament and novelty seeking in adolescent substance use: convergence of dimensions of temperament with constructs from Cloninger's theory. Journal of personality and social psychology. 1998;74(2):387–406. doi: 10.1037//0022-3514.74.2.387. [DOI] [PubMed] [Google Scholar]
- 43.Myers MG, MacPherson L, Jones LR, Aarons GA. Measuring adolescent smoking cessation strategies: instrument development and initial validation. Nicotine Tob Res. 2007;9(11):1131–1138. doi: 10.1080/14622200701648466. [DOI] [PubMed] [Google Scholar]
- 44.Brewer JA, Mallik S, Babuscio TA, et al. Mindfulness training for smoking cessation: results from a randomized controlled trial. Drug Alcohol Depend. 2011;119(1-2):72–80. doi: 10.1016/j.drugalcdep.2011.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Carroll KM, Onken LS. Behavioral therapies for drug abuse. Am J Psychiatry. 2005;162(8):1452–1460. doi: 10.1176/appi.ajp.162.8.1452. [DOI] [PMC free article] [PubMed] [Google Scholar]


