This study reviews available methodologies for evaluating human papillomavirus (HPV) status, as well as current evidence involving the prognostic and potential predictive value of p16 and HPV status in patients with locoregionally advanced or recurrent and/or metastatic squamous cell carcinoma of the head and neck treated with cetuximab combination regimens, with an emphasis placed on recent subgroup analyses of the phase III IMCL‐9815 and EXTREME trials.
Keywords: Cetuximab, p16, Human papillomavirus, Squamous cell carcinoma of the head and neck, IMCL‐9815, EXTREME
Abstract
Squamous cell carcinoma of the head and neck (SCCHN) is the sixth most common cancer worldwide. It has recently been appreciated that human papillomavirus (HPV) status (or p16 status, which is a frequently used surrogate for HPV status) is prognostic for oropharyngeal SCCHN. Here, we review and contextualize existing p16 and HPV data, focusing on the cetuximab registration trials in previously untreated, locoregionally advanced, nonmetastatic SCCHN (LA SCCHN) and in recurrent and/or metastatic SCCHN (R/M SCCHN): the IMCL‐9815 and EXTREME clinical trials, respectively. Taken together, the available data suggest that, while p16 and HPV are prognostic biomarkers in patients with LA SCCHN and R/M SCCHN, it could not be shown that they are predictive for the outcomes of the described cetuximab‐containing trial regimens. Consequently, although HPV status provides prognostic information, it is not shown to predict therapy response, and so is not helpful for assigning first‐line therapy in patients with SCCHN. In addition, we discuss assays currently used to assess p16 and HPV status, as well as the differentiation between these two biomarkers. Ultimately, we believe HPV E6/E7 polymerase chain reaction–based mRNA testing may represent the most informative technique for assessing HPV status in patients with SCCHN. While p16 is a valid surrogate for HPV status in oropharyngeal carcinoma (OPC), there is a higher risk of discordance between p16 and HPV status in non‐OPC SCCHN. Collectively, these discussions hold key implications for the clinical management of SCCHN.
Implications for Practice.
Human papillomavirus (HPV) status (or its commonly utilized surrogate p16) is a known prognostic biomarker in oropharyngeal squamous‐cell carcinoma of the head and neck (SCCHN). We evaluated implications of the available evidence, including cetuximab registration trials in previously untreated locoregionally advanced (LA) SCCHN and recurrent and/or metastatic (R/M) SCCHN. We conclude that, although p16 and HPV are prognostic biomarkers for both LA and R/M SCCHN, they have not been shown to be predictive of response to the described cetuximab‐containing regimens for either indication. Thus, current evidence suggests that benefits of cetuximab are observed in both p16‐/HPV‐positive and ‐negative SCCHN.
Introduction
Squamous‐cell carcinoma of the head and neck (SCCHN) is one of the most frequently diagnosed cancers, with an annual global incidence of more than 500,000 new cases and a death toll of approximately 300,000 patients per year [1], [2]. At the time of diagnosis, the majority of patients with SCCHN present with stage III or IVA‐B disease. Nevertheless, because relatively few patients present with incurable distant metastatic disease, most patients with locally advanced SCCHN can still be treated with curative intent.
Generally, the clinical management of patients with locally advanced stage III and stage IV SCCHN is dependent on the extent of disease and the primary site [3], [4]. Patients with previously untreated, locoregionally advanced (LA), nonmetastatic SCCHN who are treated nonsurgically should typically receive radiotherapy (RT) in combination with high‐dose cisplatin. An alternative option, RT plus cetuximab, is used in those patients for whom RT plus high‐dose cisplatin is not appropriate because of absolute or relative contraindications or in whom it is deemed unacceptable after a physician–patient discussion [5], [6], [7]. No formal comparison exists to date between cisplatin and cetuximab in combination with RT. Other treatment options for patients with LA SCCHN include, but are not limited to, surgery with or without postoperative RT and with or without cisplatin. In some selected cases, induction chemotherapy with docetaxel, cisplatin, and 5‐fluorouracil (5‐FU) followed by RT with or without platinum or cetuximab could be considered [6]. Current guidelines recommend that patients with an acceptable performance status who have recurrent and/or metastatic (R/M) SCCHN are treated with a platinum (either cisplatin or carboplatin) plus 5‐FU plus cetuximab [8].
Although the SCCHN field has historically been plagued by a dearth of informative biomarkers, it has recently been appreciated that human papillomavirus (HPV) status has prognostic value in patients with oropharyngeal SCCHN, with patients with HPV‐positive tumors characterized by improved outcomes relative to patients with HPV‐negative disease [9], [10], [11]. Indeed, HPV‐associated oropharyngeal cancer represents a distinct disease entity. p16 status has emerged as a commonly utilized surrogate biomarker for HPV status because of the cost effectiveness of testing for its presence or absence in tumor cells [12]. Although this technique is commonly deployed in oropharyngeal carcinoma (OPC), concordance between the two biomarkers is far less than 100% in non‐OPC SCCHN. It is therefore important to ensure appropriate specificity and clarity of terminology when describing p16 and HPV analyses. In the current literature, these terms are often used interchangeably, and this could lead to potentially inconsistent conclusions between studies in non‐OPC SCCHN and between analyses of OPC and non‐OPC patient populations.
Irrespective of these terminological considerations, the importance of the observed prognostic value of p16 and HPV status is further underscored by the increasing incidence of HPV‐positive SCCHN, particularly in patients with OPC. Additionally, it is now believed that HPV is a causative agent for the majority of cases of OPC in many developed countries [13], [14], [15], [16], [17]. Indeed, 45%–90% of newly diagnosed OPC is HPV‐positive, which represents nearly twice the prevalence recorded during the late 1990s [13], [15], [18], [19], [20]. In the United States, 63.8% of patients with OPC enrolled in the Radiation Therapy Oncology Group (RTOG) 0129 study had tumors that were HPV‐positive [9]. In a German prevalence rate analysis and a European validation study, 34.4% and 54.6% of patients with OPC had tumors that were p16‐positive, respectively [10], [17]. Based on recent studies in Scandinavia, incidence rates of HPV‐associated OPC have been rising by 3.5%–5% per annum, with the number of cases expected to double within a decade in this region [21], [22]. However, it is apparent that epidemiologic trends in p16 and HPV prevalence are subject to variation in geography and local economic status [13], [14], [15], [17]. Patients with p16‐positive non‐OPC SCCHN had superior outcomes relative to those of patients with p16‐negative non‐OPC SCCHN in an analysis of data from the RTOG 0129, 0234, and 0522 studies [23], suggesting that the prognostic influence of p16 status does not appear to be exclusively confined to patients with OPC; however, the generalizability of these observations in non‐OPC SCCHN remains somewhat controversial and requires further studies to confirm. Finally, it has been appreciated that the incidence of HPV‐positive SCCHN is substantially higher in LA versus R/M SCCHN, a difference that may—at least in part—reflect the superior prognosis of patients with HPV‐positive tumors (i.e., patients with HPV‐negative tumors are more likely to experience recurrences) [24], [25], [26].
In consonance with this line of thinking, there is robust empirical evidence that the biology of HPV‐positive SCCHN differs fundamentally from that of HPV‐negative SCCHN. For example, patients with HPV‐positive SCCHN are characterized by less or no tobacco exposure, more lifetime sex partners, fewer comorbidities, and a unique molecular signature compared with patients with HPV‐negative disease [14]. Furthermore, HPV‐positive tumors are more commonly characterized by loss of TNF receptor–associated factor 3 and hyperactive phosphoinositide‐3 kinase pathway, while HPV‐negative tumors present with amplifications of CDKN2A, CCND1, EGFR, and MYC and loss of TP53 [1]. Nevertheless, it should be noted that both HPV‐positive and HPV‐negative SCCHN tumors contain CD8‐positive tumor‐infiltrating lymphocytes [27]; moreover, smoking status (which has not always been collected in SCCHN clinical trials) is an important risk modifier even in HPV‐positive disease, although there is no consensus yet regarding an optimal pack‐years threshold [11], [28].
Despite the impressive progress regarding comprehension of the etiology, epidemiology, biology, and prognostic impact of HPV, the extent to which HPV status may be predictive of response to common regimens used in the treatment of LA and R/M SCCHN remains incompletely understood. As alluded to earlier, the anti–epidermal growth factor receptor (EGFR) monoclonal antibody cetuximab is used to treat both patients with LA SCCHN and those with R/M SCCHN. More specifically, in patients with LA SCCHN in the phase III IMCL‐9815 trial, the addition of cetuximab to RT improved locoregional control (LRC), overall survival (OS), and progression‐free survival (PFS) without increasing the frequency of grade 3 mucositis or dysphagia [29], [30], [31]. Furthermore, as established by the phase III EXTREME trial, adding cetuximab to first‐line platinum plus 5‐FU improved OS, PFS, disease control, and response rate in patients with R/M SCCHN and provided additional symptom relief and better physical functioning without showing a deleterious effect on quality of life [32], [33], [34]. Notably, in addition to direct receptor blockade, cetuximab can elicit antibody‐dependent cellular cytotoxicity (ADCC), and prior evidence suggests that cetuximab can synergize with RT and various chemotherapeutic agents in SCCHN model systems [35], [36], [37], [38], [39], [40]. Differences in these attributes—as well as their different affinities for EGFR—serve to distinguish cetuximab from several other monoclonal antibodies and tyrosine kinase inhibitors targeting EGFR [41], [42].
In this article, we review and discuss available methodologies for evaluating HPV status, as well as current evidence involving the prognostic and potential predictive value of p16 and HPV status in patients with LA or R/M SCCHN treated with cetuximab combination regimens, with an emphasis placed on recent subgroup analyses of the phase III IMCL‐9815 and EXTREME trials. Because very limited data on HPV analyses for cetuximab monotherapy in heavily pretreated refractory R/M SCCHN patients suggest that cetuximab may be less effective in HPV‐related disease than in HPV‐unrelated SCCHN [43], [44], [45], we focus on randomized HPV data available to assess the effect of the addition of cetuximab to standard SCCHN therapy. It must be noted that p16 and HPV analyses of IMCL‐9815 and EXTREME were performed retrospectively and are therefore subject to limitations commonly associated with such analyses. Due to the broad range and variability between available studies, we decided that this topic would be better addressed by a nonsystematic, rather than systematic, review process.
Materials and Methods
In developing this nonsystematic review, we queried PubMed, as well as American Society of Clinical Oncology and European Society for Medical Oncology annual meeting abstracts, to identify studies and review articles relevant to the prognostic and potentially predictive characteristics of HPV infection in patients with SCCHN. While there were no formal inclusion or exclusion criteria, priority was granted to clinical studies that were phase III or utilized a randomized study design. Outputs of the search results were hand‐curated. No unpublished material is included in this review.
Available Assays for the Detection of HPV Status in SCCHN
At present, there is no consensus regarding the optimal methodology for assessment of HPV status in patients with SCCHN. As mentioned earlier, p16 is commonly deployed as a surrogate biomarker for HPV status [9], [10], [11]. The biological rationale underlying this surrogacy stems from the fact that the HPV E7 viral protein triggers degradation of the retinoblastoma tumor suppressor protein in infected cells, which in turn initiates a feedback loop that results in the activation of senescence‐promoting pathways that include increased expression of p16. Hence, p16 status directly provides a general readout of retinoblastoma protein (RB) activity, leading to the possibility of discordance between p16 status and HPV status in cases in which RB is inactivated via HPV‐independent mechanisms (i.e., p16‐positive but HPV‐negative tumors).
p16 status is typically assessed via immunohistochemistry (IHC), a strategy that affords the advantages of a relatively technically and analytically straightforward assay that possesses high sensitivity [46]. Although there is a widely accepted cutoff of 70% for p16‐positive tumor cells when determining p16 status, not all studies adhere to it [31], [42], [47]. Furthermore, as with any surrogate biomarker, there is a risk of discordance between p16 status and the actual HPV status, which can be exacerbated by a failure to use a stringent cutoff (50%–70%) for percentage p16‐positive tumor cells. Current estimates posit that the discordance rate between p16 IHC and direct detection of HPV DNA/RNA may approach 25%, with p16‐positive but HPV‐negative tumors constituting the majority of discordant cases (perhaps for the reasons outlined above) [48], [49]. This discordance is generally lower for OPC SCCHN. For example, studies have shown that although the positive predictive value of p16 IHC as a surrogate for HPV status was 92.7% in patients with OPC, this value dropped to 41.3% in patients with non‐OPC SCCHN [50], [51], [52]. Accordingly, whereas utilization of p16 as a surrogate biomarker for HPV status is less of a valid approach in patients with non‐OPC, it is more valid in OPC SCCHN [53].
Because determination of p16 status does not differentiate between HPV16 and non‐HPV16 subtypes [54], several other methods for the determination of HPV status are also available. HPV DNA detection in tumors does not directly prove causal association between the viral infection and SCCHN, as HPV is ubiquitously present in humans. Therefore, HPV DNA polymerase chain reaction (PCR) is a sensitive, but not specific, method for determination of HPV status. p16 immunohistochemistry followed by PCR for HPV DNA has been proposed as a reliable algorithm for detection of HPV in fresh or paraffin‐embedded OPC specimens, combining both the specificity of p16 IHC with the sensitivity of HPV DNA PCR, and therefore helping detect higher‐risk cases by identifying the causal relationship between presence of HPV DNA and an active infection [55].
Another option is HPV DNA or RNA in situ hybridization (ISH), which can differentiate between integrated and episomal forms of HPV in tumors but also lacks sensitivity. HPV RNA‐ISH specifically affords the advantages of tumor‐specific expression of the target mRNA and the temporal advantage of pre‐neoplastic expression of viral E6 mRNA [56]. However, the ISH protocol itself is not always feasible given limited sample availability and the necessity for fresh, and not frozen or paraffin‐embedded, tissue samples. Furthermore, the HPV‐RNA ISH protocol is currently being used in clinical trials to determine HPV‐positive versus negative status only [57].
We believe that the most informative method for determining HPV status involves the direct detection of viral E6/E7 mRNA in fresh tissue samples via PCR. A drawback of this method is the potential for decreased sensitivity in lower‐quality clinical samples or samples with low E6/E7 expression [58], [59]. On the other hand, advantages of this method include generally high sensitivity, specificity, and tumor‐specific expression of the mRNA/DNA target [56]. Moreover, this assay can be deployed not only on fresh tumor samples, but also, when necessary, on formalin‐fixed, paraffin‐embedded tissue blocks (although the samples require additional quality‐control evaluation, adding a layer of complexity to the protocol) [13], [60]. Thus, we believe that HPV E6/E7 mRNA detection via PCR could evolve as a new standard for assessing HPV status in patients with SCCHN due to its overall superiority and practicality. This technology is especially important for non‐OPC SCCHN, in which the concordance between p16 and HPV status is less clear.
Overview of p16 and HPV Subgroup Analyses From the IMCL‐9815 and EXTREME Trials
The overall designs and subgroup distributions of the IMCL‐9815 and EXTREME trials are summarized in Table 1 [24, 25, 29, 30, 32, 33, 61–63]. Many North American patients were included in the IMCL‐9815 trial, whereas EXTREME included many patients from southern Europe; distinctions between these populations could account for any differences in p16/HPV status between the two trials. Additionally, although we believe that HPV E6/E7 mRNA detection via PCR is the most informative method for HPV status determination, the analyses in the IMCL‐9815 and EXTREME trials were performed using the most scientifically recognized methods available at the time.
Table 1. Trial designs for IMCL‐9815 and EXTREME.
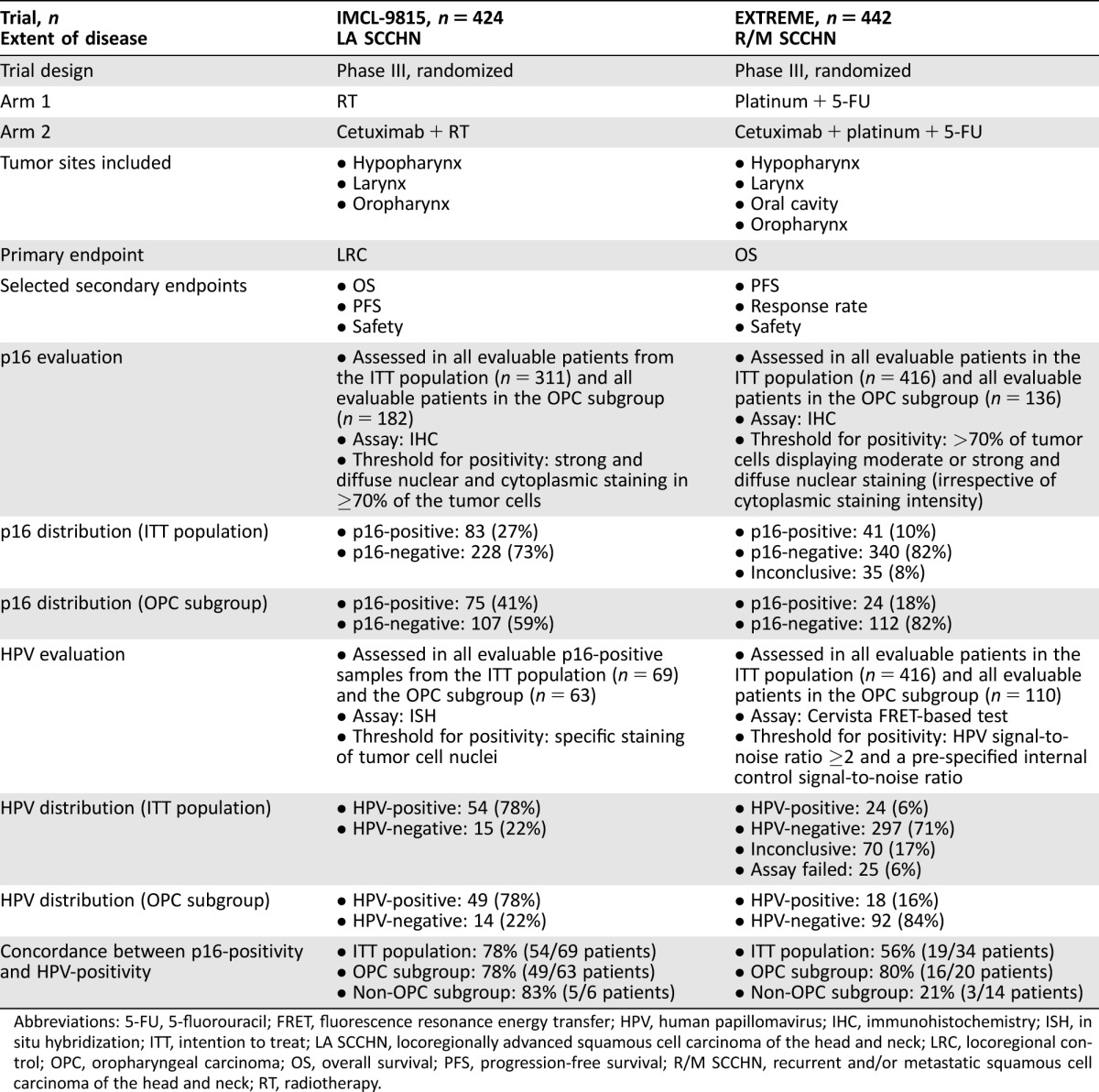
Abbreviations: 5‐FU, 5‐fluorouracil; FRET, fluorescence resonance energy transfer; HPV, human papillomavirus; IHC, immunohistochemistry; ISH, in situ hybridization; ITT, intention to treat; LA SCCHN, locoregionally advanced squamous cell carcinoma of the head and neck; LRC, locoregional control; OPC, oropharyngeal carcinoma; OS, overall survival; PFS, progression‐free survival; R/M SCCHN, recurrent and/or metastatic squamous cell carcinoma of the head and neck; RT, radiotherapy.
p16 and HPV as Potential Prognostic Biomarkers
p16 in LA SCCHN.
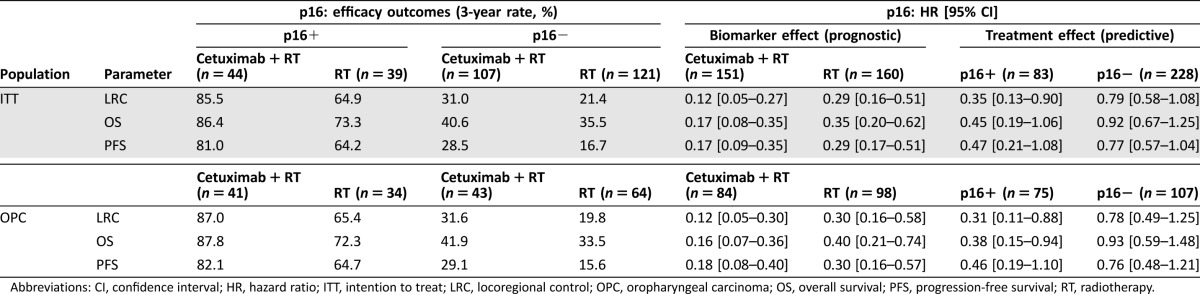
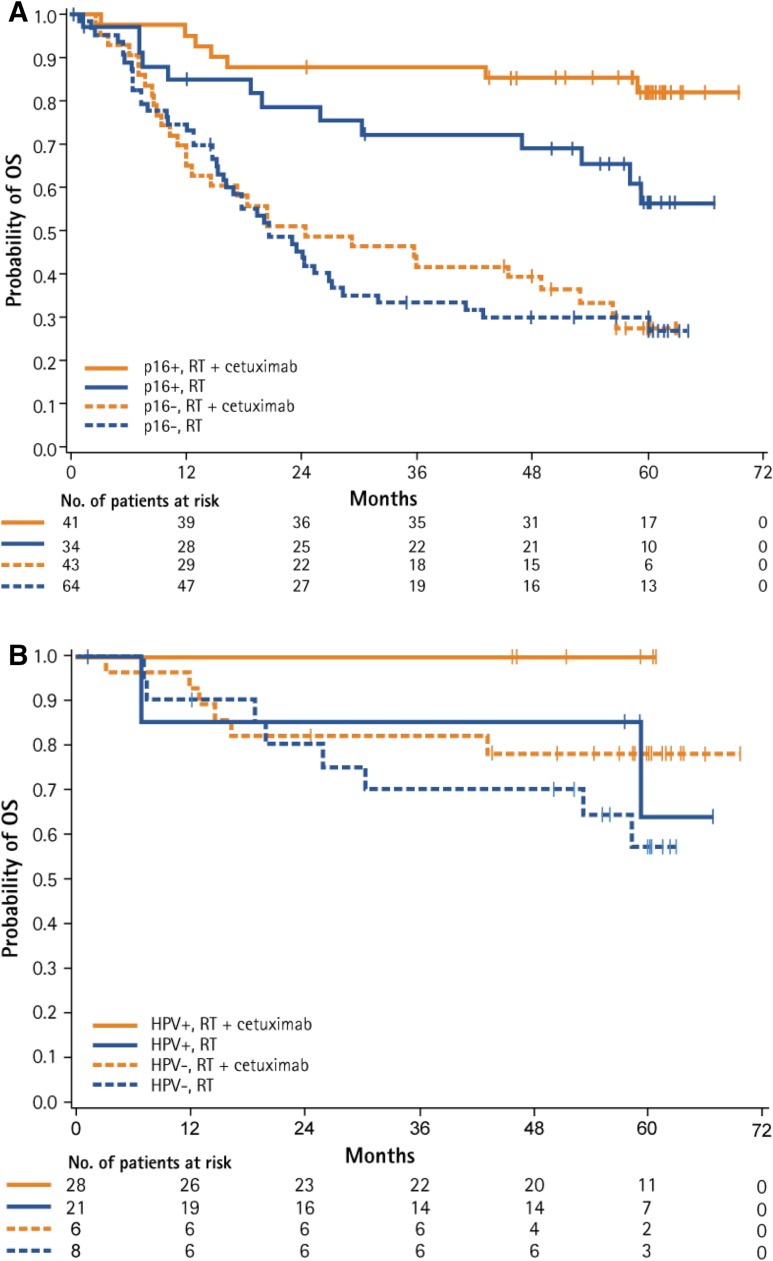
Within the IMCL‐9815 intention‐to‐treat (ITT) population, patients with p16‐positive tumors had superior LRC, OS, and PFS than those with p16‐negative tumors in both the cetuximab plus RT and RT alone treatment arms. The same observation was made for the OPC subgroup (Table 2, Fig. 1) [24], [61], [62], [63].
Table 2. Efficacy outcomes of the IMCL‐9815 trial by p16 status.
Abbreviations: CI, confidence interval; HR, hazard ratio; ITT, intention to treat; LRC, locoregional control; OPC, oropharyngeal carcinoma; OS, overall survival; PFS, progression‐free survival; RT, radiotherapy.
Figure 1.
Effect of p16 (A) and HPV (B) status on OS in patients with locoregionally advanced squamous‐cell carcinoma of the head and neck treated with RT ± cetuximab in the oropharyngeal carcinoma subgroup. Reprinted from [24] with permission © 2016 American Society of Clinical Oncology. All rights reserved.
Abbreviations: HPV, human papillomavirus; OS, overall survival; RT, radiotherapy.
p16 in R/M SCCHN.
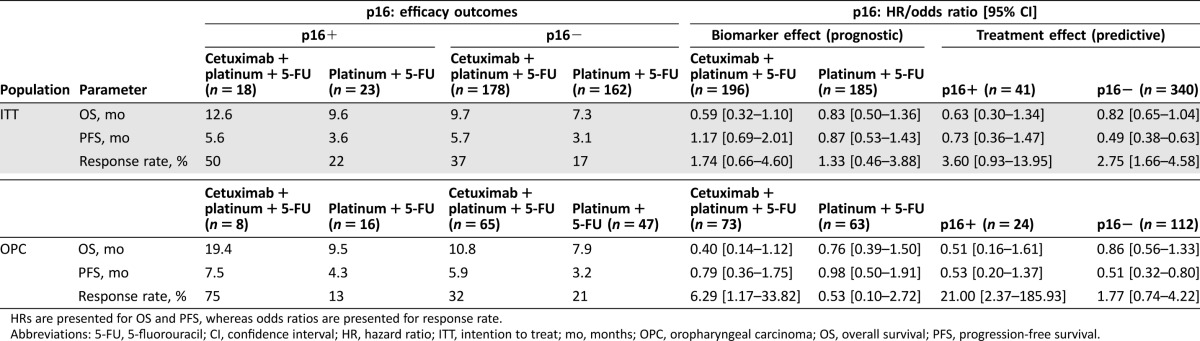
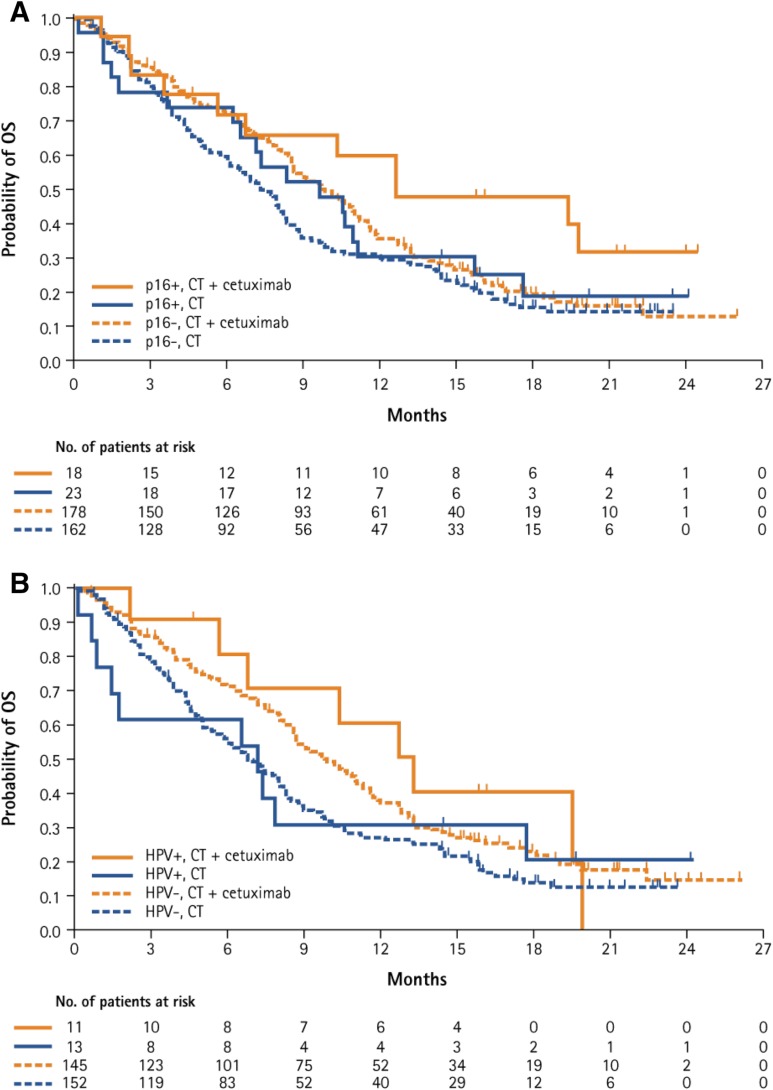
Analogously, in both the ITT population and the OPC subgroup of EXTREME, p16‐positive status was associated with better OS in both the cetuximab plus platinum plus 5‐FU and platinum plus 5‐FU treatment arms. In the ITT population, PFS and response rate favored p16‐positive status in the platinum plus 5‐FU arm, but did not unambiguously differ based on p16 status in the cetuximab plus platinum plus 5‐FU arm. Therefore, no clear and consistent prognostic role for p16 status in terms of its influence on PFS and response rate in the ITT population could be established. Due to the small number of patients with p16‐positive OPC in this trial, these data are insufficient for a definitive conclusion to be drawn (Table 3, Fig. 2) [25], [63].
Table 3. Efficacy outcomes of the EXTREME trial by p16 status.
HRs are presented for OS and PFS, whereas odds ratios are presented for response rate.
Abbreviations: 5‐FU, 5‐fluorouracil; CI, confidence interval; HR, hazard ratio; ITT, intention to treat; mo, months; OPC, oropharyngeal carcinoma; OS, overall survival; PFS, progression‐free survival.
Figure 2.
Effect of p16 (A) and HPV (B) status on OS in patients with recurrent and/or metastatic squamous‐cell carcinoma of the head and neck treated with platinum + 5‐fluorouracil ± cetuximab in the intention‐to‐treat population. Reprinted from [25] by permission of Oxford University Press and the European Society for Medical Oncology.
Abbreviations: CT, chemotherapy; HPV, human papillomavirus; OS, overall survival.
HPV in LA SCCHN.
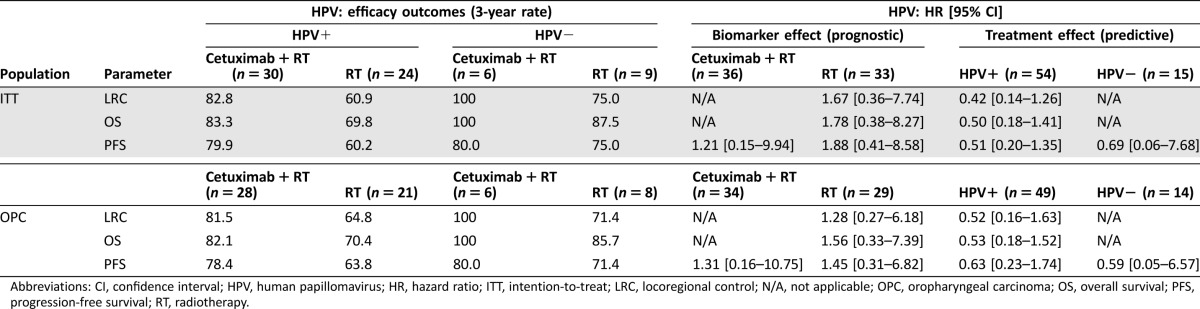
Given the small number of patients with p16‐positive but HPV‐negative tumors, it is difficult to draw firm conclusions regarding the putative prognostic role of HPV status in this group regarding the endpoints of LRC, OS, and PFS from either the IMCL‐9815 trial ITT population or OPC subgroup (Table 4, Fig. 1) [24], [61], [62], [63].
Table 4. Efficacy outcomes of the IMCL‐9815 trial by HPV status.
Abbreviations: CI, confidence interval; HPV, human papillomavirus; HR, hazard ratio; ITT, intention‐to‐treat; LRC, locoregional control; N/A, not applicable; OPC, oropharyngeal carcinoma; OS, overall survival; PFS, progression‐free survival; RT, radiotherapy.
HPV in R/M SCCHN.
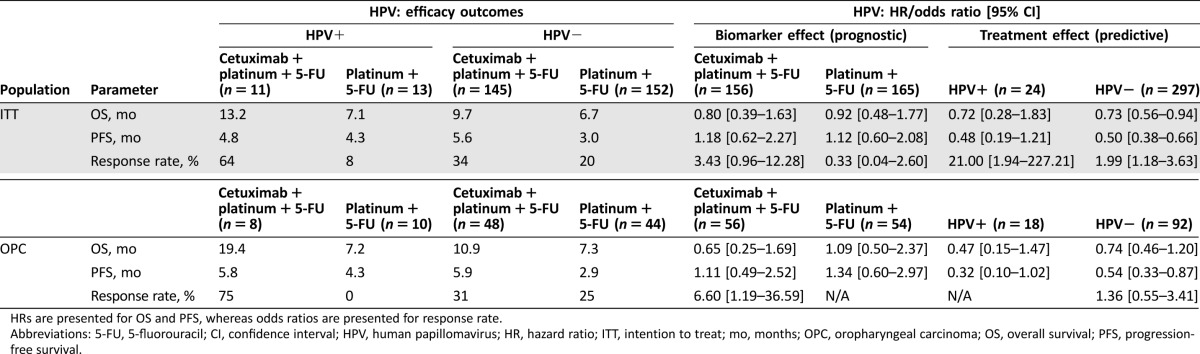
There was a trend toward longer OS in the HPV‐positive versus HPV‐negative subgroup of the EXTREME ITT population in both the cetuximab plus platinum plus 5‐FU and platinum plus 5‐FU treatment arms. This observation persisted in the cetuximab plus platinum plus 5‐FU arm, but not in the platinum plus 5‐FU arm of the OPC subgroup. Consistent with the p16 analysis, there was no clear and consistent prognostic effect on PFS and response rate for HPV status in the cetuximab plus platinum plus 5‐FU and platinum plus 5‐FU arms of the ITT population. An analogous conclusion was reached for the OPC subgroup (Table 5, Fig. 2) [25], [63].
Table 5. Efficacy outcomes of the EXTREME trial by HPV status.
HRs are presented for OS and PFS, whereas odds ratios are presented for response rate.
Abbreviations: 5‐FU, 5‐fluorouracil; CI, confidence interval; HPV, human papillomavirus; HR, hazard ratio; ITT, intention to treat; mo, months; OPC, oropharyngeal carcinoma; OS, overall survival; PFS, progression‐free survival.
p16 and HPV as Potential Predictive Biomarkers
p16 in LA SCCHN.
Within the IMCL‐9815 ITT population, adding cetuximab to RT resulted in superior 3‐year LRC, OS, and PFS in patients with both p16‐positive and p16‐negative tumors. The addition of cetuximab to RT also increased 3‐year LRC, OS, and PFS in patients with both p16‐positive and p16‐negative tumors within the OPC subgroup of IMCL‐9815. Although the treatment effects were stronger in the p16‐positive subgroup, interaction tests for LRC, OS, and PFS revealed no significant interaction between p16 status and treatment both in the ITT population (p = .098, p = .134, and p = .252, respectively) and the OPC subgroup (p = .087, p = .085, and p = .253, respectively; Table 2, Fig. 1) [24], [61], [62], [63].
Within the IMCL‐9815 ITT population, adding cetuximab to RT resulted in superior 3‐year LRC, OS, and PFS in patients with both p16‐positive and p16‐negative tumors. The addition of cetuximab to RT also increased 3‐year LRC, OS, and PFS in patients with both p16‐positive and p16‐negative tumors within the OPC subgroup of IMCL‐9815.
p16 in R/M SCCHN.
OS and PFS were numerically improved in patients treated with cetuximab plus platinum plus 5‐FU as compared with patients treated with platinum plus 5‐FU in both the p16‐positive and p16‐negative subgroups of the EXTREME trial ITT population. Interaction tests for OS (p = .482) and PFS (p = .430) further underlined that the treatment effect persisted regardless of p16 status. In addition, adding cetuximab to platinum plus 5‐FU improved the response rate in both patients with p16‐positive and p16‐negative disease. Similarly, within the OPC subgroup of EXTREME, there was a trend toward improved OS and PFS in cetuximab‐treated patients in both the p16‐positive and p16‐negative subgroups, and the addition of cetuximab to platinum plus 5‐FU improved—at least numerically—the response rate in both subgroups of patients with OPC. Interaction tests for OPC subgroups were not performed due to the very small sample sizes (Table 3, Fig. 2) [25], [63].
HPV in LA SCCHN.
Although the number of patients in the p16‐positive, HPV‐evaluable ITT subgroup from the IMCL‐9815 trial was small, 3‐year LRC, OS, and PFS data appeared to be consistent with those previously obtained during the p16 subgroup analysis for the HPV‐positive subgroup. The small size of the HPV‐negative subgroup precluded drawing meaningful conclusions. While similar statistical considerations apply to the IMCL‐9815 p16‐positive HPV‐evaluable OPC subgroup, 3‐year LRC, OS, and PFS again seemed similar to the findings reported in the p16 subgroup analysis for the HPV‐positive subgroup. The small size of the HPV‐negative subgroup did not permit drawing meaningful conclusions (Table 4, Fig. 1) [24], [61], [62], [63].
HPV in R/M SCCHN.
In consonance with the findings of the p16 subgroup analysis—although the OS and PFS difference between treatment arms only reached a p value smaller than .05 in the HPV‐negative subgroup—OS and PFS were longer in cetuximab‐treated patients regardless of HPV status. Furthermore, no clear interaction was suggested between HPV status and treatment for either OS (p = .824) or PFS (p = .975) in the ITT population. Analogously, the addition of cetuximab to platinum plus 5‐FU resulted in increased response rate in both the HPV‐positive and HPV‐negative subgroups of the ITT population. In the OPC subgroup of EXTREME, OS was numerically better and PFS was improved in patients receiving cetuximab in both the HPV‐positive and HPV‐negative subgroups. Additionally, adding cetuximab to platinum plus 5‐FU numerically improved the response rate in patients with HPV‐negative tumors; drawing meaningful conclusions regarding response rate in the HPV‐positive subgroup was not possible in light of the small number of patients. Interaction tests were not performed due to the very small sample size (Table 5, Fig. 2) [25], [63].
Key Conclusions From the p16 and HPV Subgroup Analyses of the IMCL‐9815 and EXTREME Trials
These subgroup analyses of the IMCL‐9815 and EXTREME trials evaluated the roles of p16 and HPV as potential prognostic and predictive biomarkers in patients with SCCHN (LA SCCHN and R/M SCCHN, respectively) [24], [25], [61], [62], [63]. In both trials, p16 was found to be a valid surrogate for HPV in OPC. Based on observations made in the EXTREME trial and the available literature, this may not be the case in non‐OPC SCCHN, although it should be noted that the high concordance between p16‐positivity and HPV‐positivity in the six‐patient non‐OPC subgroup of the IMCL‐9815 trial was not in line with these conclusions. Both studies suggested that p16 and HPV are prognostic biomarkers, with biomarker positivity associated with increased survival, particularly for OPC [24], [25], [61], [62], [63]. Additionally, both studies reported efficacy gains upon the addition of cetuximab to the control regimen (RT and platinum plus 5‐FU, respectively) and looked at the biomarker subgroups of p16‐positive, p16‐negative, HPV‐positive, and HPV‐negative OPC; interaction tests did not show a significant interaction between biomarker status and treatment effect [24], [25], [61], [62], [63]. Taken together, these observations suggest that, although p16 and HPV are prognostic biomarkers in patients with LA SCCHN and R/M SCCHN, it could not be shown that they are predictive for the response to the described cetuximab‐containing regimens in either indication [64]; consequently, the data suggest that the addition of cetuximab appears to provide benefit over the control arm regardless of p16 and HPV status in both LA SCCHN and R/M SCCHN.
Current Controversies and Future Outlook
Currently controversial is the extent to which the findings from the p16 and HPV subgroup analyses of IMCL‐9815 and EXTREME can be extrapolated to patients receiving cetuximab monotherapy. Although this topic lies beyond the scope of the present review, which is focused on combination regimens involving cetuximab plus either RT or platinum plus 5‐FU, it should be noted that very little information is presently available [44]. Our conclusions are derived from retrospective analyses of the two cetuximab registration trials, because HPV became relevant after the study completions. Further prospective validation is needed for definitive conclusions to be made.
Additionally, though further confirming the prognostic value of p16 and HPV status, ostensibly divergent results concerning the potential predictive impact of p16 and HPV status have been obtained from two studies involving the anti‐EGFR monoclonal antibody panitumumab. First, the CONCERT‐2 trial compared panitumumab plus RT with chemoradiotherapy (CRT) in patients with LA SCCHN. There was no significant difference between treatment arms in terms of 2‐year LRC in patients with p16‐positive disease, whereas 2‐year LRC favored the CRT arm in patients with p16‐negative tumors; the effect of HPV was very low, and outcomes favoring CRT were largely driven by patients with p16‐negative LA SCCHN [47]. Second, in the SPECTRUM trial, which investigated the effect of adding panitumumab to chemotherapy in patients with R/M SCCHN, panitumumab was more active in patients with p16‐negative tumors, and no benefit was observed upon the addition of panitumumab to chemotherapy in patients with p16‐positive disease [42]. However, neither CONCERT‐2 nor SPECTRUM met their primary endpoints in the ITT population, rendering biomarker‐defined subgroup analyses from these trials difficult to interpret. An added confounding variable when interpreting CONCERT‐2 and SPECTRUM is that both trials used a different p16 cutoff for positivity (10%) than did EXTREME and IMCL‐9815 (70%) [24], [42], [47]. Finally, it should be reiterated that cetuximab and panitumumab are not biologically identical; indeed, their different affinities for EGFR, as well as the distinct characteristics of cetuximab‐induced ADCC [39], may account for the observed apparent differences.
Because of their more favorable prognosis, a consideration for patients with HPV‐positive OPC concerns the extent to which it may be possible to reduce the collateral toxicities of anticancer treatments in this subgroup while maintaining treatment [14]. Indeed, treatment deintensification for patients with LA SCCHN represents a topic of major current clinical research interest, in light of the fact that current standard‐of‐care treatment with high‐dose CRT is associated with significant acute and late toxicities [65], [66], [67], [68], [69]. Accordingly, treatment regimens that reduce treatment‐related toxicities and, in particular, life‐threatening late side effects without compromising efficacy are urgently needed. This is particularly the case for patients with HPV‐positive OPC, who are likely to experience longer durations of treatment [11]. Strategies currently under study in patients with HPV‐positive SCCHN involve, but are not limited to, reducing the dose of RT and the use of bioradiation with cetuximab instead of CRT (RTOG 1016 [NCT01302834], De‐EscaLate [NCT 01874171], and TROG 12.01 [NCT 01855451]). As grade 3–4 mucositis and radiation dermatitis were not found to have significantly increased with cetuximab/RT compared with RT alone, and quality of life was not adversely affected in IMCL‐9815, cetuximab/RT could be a viable replacement for CRT in patients with HPV‐positive SCCHN, in the event of a positive outcome in the above‐mentioned trials [31], [70]. Furthermore, there is interest in using induction chemotherapy to differentiate between patients who will need more aggressive locoregional therapy and those for whom a lower RT dose approach (reduced RT dose from 69.3 to 54 Gy) may be an option based on patient responses to induction therapy (ECOG 1308 [NCT01084083]). Other studies are focused on evaluating the use of reduced‐dose CRT versus accelerated but lower‐dose RT alone (NRG‐002 [NCT02254278]). Finally, the ECOG 3311 trial (NCT01898494) employs transoral robotic surgery for eligible patients and uses a risk‐based adjuvant therapy approach to minimize RT application, RT dose, and the concurrency of chemotherapy. Finally, approximately 20% of patients with HPV‐positive SCCHN will experience disease recurrence [27]; more studies are needed to shed light on how patients with increased risk of relapse can be identified during the diagnosis and treatment of their first disease occurrence. It should also be noted that p16 continues to be widely accepted as a surrogate marker for HPV in OPC, including in scenarios such as during patient selection for enrollment into treatment de‐escalation trials. While the p16 assay is not 100% specific for HPV association, and approximately 10% of OPC tumors test as p16‐positive/HPV DNA‐negative, this assay remains an informative and practical tool for identifying patients with OPC with a good versus poor prognosis [50].
It should also be noted that p16 continues to be widely accepted as a surrogate marker for HPV in OPC, including in scenarios such as during patient selection for enrollment into treatment de‐escalation trials. While the p16 assay is not 100% specific for HPV association, and approximately 10% of OPC tumors test as p16‐positive/HPV DNA‐negative, this assay remains an informative and practical tool for identifying patients with OPC with a good versus poor prognosis.
Conclusion
In conclusion, available data from retrospective analyses suggest that, while p16 and HPV are prognostic biomarkers in patients with LA SCCHN and R/M SCCHN, it could not be shown that they are predictive for the described cetuximab‐containing regimens in either indication; consequently, although HPV testing provides important prognostic information, it is not a requirement for treating patients with SCCHN with cetuximab plus RT or platinum‐based chemotherapy. Additionally, the available evidence suggests that while p16 is a valid surrogate for HPV in OPC, this may not be the case in non‐OPC SCCHN. Collectively, the topics reviewed herein hold key implications for the clinical management of SCCHN and should be reviewed by oncologists before deciding how (and how not) to incorporate p16 and HPV testing into their practices. Data from ongoing prospective studies are anticipated to help resolve any remaining open questions (NCT01302834, NCT 01874171, NCT 01855451).
Acknowledgments
We thank Merck KGaA, Bristol‐Myers Squibb, and Eli Lilly & Co., the study sponsors. Medical writing assistance was provided by ClinicalThinking, Inc., Hamilton, New Jersey, USA, and funded by Merck KGaA, Darmstadt, Germany, Ina Nikolaeva, PhD.
Author Contributions
Conception and Design: David I. Rosenthal, Frank Beier, Jeltje Schulten, Jan B. Vermorken, James A. Bonner, Ricard Mesia, Jordi Giralt, Amanda Psyrri, Ulrich Keilholz
Provision of Study Material or Patients: David I. Rosenthal, Frank Beier, Jeltje Schulten, Jan B. Vermorken, James A. Bonner, Ricard Mesia, Jordi Giralt, Amanda Psyrri, Ulrich Keilholz
Collection and/or Assembly of Data: Frank Beier
Data Analysis and Interpretation: David I. Rosenthal, Frank Beier, Jeltje Schulten, Jan B. Vermorken, James A. Bonner, Ricard Mesia, Jordi Giralt, Amanda Psyrri, Ulrich Keilholz
Manuscript Writing: David I. Rosenthal, Frank Beier, Jeltje Schulten, Jan B. Vermorken, James A. Bonner, Ricard Mesia, Jordi Giralt, Amanda Psyrri, Ulrich Keilholz
Final Approval of Manuscript: David I. Rosenthal, Frank Beier, Jeltje Schulten, Jan B. Vermorken, James A. Bonner, Ricard Mesia, Jordi Giralt, Amanda Psyrri, Ulrich Keilholz
Disclosures
James A Bonner: Merck KGaA, Bristol‐Myers Squibb, Eli Lilly & Co (C/A); Ricard Mesia: Merck KGaA, Merck Sharp & Dohme, AstraZeneca (C/A, H); Amanda Psyrri: Merck Sharpe & Dolme, AstraZeneca, Merck KGaA, Merck Serono, Amgen (C/A); Ulrich Keilholz: Merck KgaA, Merck Serono, AstraZeneca, Pfizer (C/A), Merck KgaA, Merck Serono, AstraZeneca, Pfizer, Glycotope (H), Innate, Glycotope (RF); David I. Rosenthal: Merck Serono (C/A, RF); Frank Beier: Merck KGaA (E); Jeltje Schulten: Merck KGaA (E); Jan B. Vermorken: Merck KGaA, Amgen, AstraZeneca, Boerhinger‐Ingelheim, Merck Sharp & Dolme (SAB), PCI Biotech, Synthon Biopharmaceuticals, Innate Pharma, Vaccinogen (C/A), Merck KGaA, Sanofi (H). The other author indicated no financial relationships.
(C/A) Consulting/advisory relationship; (RF) Research funding; (E) Employment; (ET) Expert testimony; (H) Honoraria received; (OI) Ownership interests; (IP) Intellectual property rights/inventor/patent holder; (SAB) Scientific advisory board.
References
- 1.Cancer Genome Atlas Network. Comprehensive genomic characterization of head and neck squamous cell carcinomas. Nature 2015;517:576–582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ferlay J, Soerjomataram I, Ervik M et al. GLOBOCAN 2012 cancer incidence and mortality worldwide: IARC cancerbase No. 11. Lyon, France: International Agency for Research on Cancer, 2013.
- 3. Rischin D, Ferris RL, Le QT. Overview of advances in head and neck cancer. J Clin Oncol 2015;33:3225–3226. [DOI] [PubMed] [Google Scholar]
- 4. Sacco AG, Cohen EE. Current treatment options for recurrent or metastatic head and neck squamous cell carcinoma. J Clin Oncol 2015;33:3305–3313. [DOI] [PubMed] [Google Scholar]
- 5. Pignon JP, le Maitre A, Maillard E et al. Meta‐analysis of chemotherapy in head and neck cancer (MACH‐NC): An update on 93 randomised trials and 17,346 patients. Radiother Oncol 2009;92:4–14. [DOI] [PubMed] [Google Scholar]
- 6. Gregoire V, Lefebvre JL, Licitra L et al. Squamous cell carcinoma of the head and neck: EHNS‐ESMO‐ESTRO Clinical Practice Guidelines for diagnosis, treatment and follow‐up. Ann Oncol 2010;21(suppl 5): v184–v186. [DOI] [PubMed] [Google Scholar]
- 7. Ahn MJ, D'Cruz A, Vermorken JB et al. Clinical recommendations for defining platinum unsuitable head and neck cancer patient populations on chemoradiotherapy: A literature review. Oral Oncol 2016;53:10–16. [DOI] [PubMed] [Google Scholar]
- 8.National Comprehensive Cancer Network. Bone cancer (version 1.2016). Available at https://www.nccn.org/professionals/physician_gls/pdf/head-and-neck.pdf. Accessed May 20, 2016.
- 9. Ang KK, Harris J, Wheeler R et al. Human papillomavirus and survival of patients with oropharyngeal cancer. N Engl J Med 2010;363:24–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Granata R, Miceli R, Orlandi E et al. Tumor stage, human papillomavirus and smoking status affect the survival of patients with oropharyngeal cancer: An Italian validation study. Ann Oncol 2012;23:1832–1837. [DOI] [PubMed] [Google Scholar]
- 11. Bhatia A, Burtness B. Human papillomavirus‐associated oropharyngeal cancer: Defining risk groups and clinical trials. J Clin Oncol 2015;33:3243–3250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Chen ZW, Weinreb I, Kamel‐Reid S et al. Equivocal p16 immunostaining in squamous cell carcinoma of the head and neck: Staining patterns are suggestive of HPV status. Head Neck Pathol 2012;6:422–429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Chaturvedi AK, Engels EA, Pfeiffer RM et al. Human papillomavirus and rising oropharyngeal cancer incidence in the United States. J Clin Oncol 2011;29:4294–4301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Gillison ML, D'Souza G, Westra W et al. Distinct risk factor profiles for human papillomavirus type 16‐positive and human papillomavirus type 16‐negative head and neck cancers. J Natl Cancer Inst 2008;100:407–420. [DOI] [PubMed] [Google Scholar]
- 15. Gillison ML, Koch WM, Capone RB et al. Evidence for a causal association between human papillomavirus and a subset of head and neck cancers. J Natl Cancer Inst 2000;92:709–720. [DOI] [PubMed] [Google Scholar]
- 16. Gillison ML, Chaturvedi AK, Anderson WF et al. Epidemiology of human papillomavirus‐positive head and neck squamous cell carcinoma. J Clin Oncol 2015;33:3235–3242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hauck F, Oliveira‐Silva M, Dreyer JH et al. Prevalence of HPV infection in head and neck carcinomas shows geographical variability: A comparative study from Brazil and Germany. Virchows Arch 2015;466:685–693. [DOI] [PubMed] [Google Scholar]
- 18. Mehanna H, Beech T, Nicholson T et al. Prevalence of human papillomavirus in oropharyngeal and nonoropharyngeal head and neck cancer‐systematic review and meta‐analysis of trends by time and region. Head Neck 2013;35:747–755. [DOI] [PubMed] [Google Scholar]
- 19. Zandberg DP, Bhargava R, Badin S et al. The role of human papillomavirus in nongenital cancers. CA Cancer J Clin 2013;63:57–81. [DOI] [PubMed] [Google Scholar]
- 20. Ndiaye C, Mena M, Alemany L et al. HPV DNA, E6/E7 mRNA, and p16INK4a detection in head and neck cancers: A systematic review and meta‐analysis. Lancet Oncol 2014;15:1319–1331. [DOI] [PubMed] [Google Scholar]
- 21. Mork J, Moller B, Dahl T et al. Time trends in pharyngeal cancer incidence in Norway 1981‐2005: A subsite analysis based on a reabstraction and recoding of registered cases. Cancer Causes Control 2010;21:1397–405. [DOI] [PubMed] [Google Scholar]
- 22. Blomberg M, Nielsen A, Munk C et al. Trends in head and neck cancer incidence in Denmark, 1978‐2007: Focus on human papillomavirus associated sites. Int J Cancer 2011;129:733–741. [DOI] [PubMed] [Google Scholar]
- 23. Chung CH, Zhang Q, Kong CS et al. p16 protein expression and human papillomavirus status as prognostic biomarkers of nonoropharyngeal head and neck squamous cell carcinoma. J Clin Oncol 2014;32:3930–3938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Rosenthal DI, Harari PM, Giralt J et al. Association of human papillomavirus and p16 status with outcomes in the IMC‐9815 phase 3 registration trial for patients with locoregionally advanced oropharyngeal squamous cell carcinoma of the head and neck treated with radiotherapy with and without cetuximab. J Clin Oncol 2016;34:1300–1308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Vermorken JB, Psyrri A, Mesia R et al. Impact of tumor HPV status on outcome in patients with recurrent and/or metastatic squamous cell carcinoma of the head and neck receiving chemotherapy with or without cetuximab: Retrospective analysis of the phase III EXTREME trial. Ann Oncol 2014;25:801–807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Misiukiewicz K, Camille N, Gupta V et al. The role of HPV status in recurrent/metastatic squamous cell carcinoma of the head and neck. Clin Adv Hematol Oncol 2014;12:812–819. [PubMed] [Google Scholar]
- 27. Keck MK, Zuo Z, Khattri A et al. Integrative analysis of head and neck cancer identifies two biologically distinct HPV and three non‐HPV subtypes. Clin Cancer Res 2015;21:870–881. [DOI] [PubMed] [Google Scholar]
- 28. Hayes DN, Van Waes C, Seiwert TY. Genetic landscape of human papillomavirus‐associated head and neck cancer and comparison to tobacco‐related tumors. J Clin Oncol 2015;33:3227–3234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Bonner JA, Harari PM, Giralt J et al. Radiotherapy plus cetuximab for squamous‐cell carcinoma of the head and neck. N Engl J Med 2006;354:567–578. [DOI] [PubMed] [Google Scholar]
- 30. Bonner JA, Harari PM, Giralt J et al. Radiotherapy plus cetuximab for locoregionally advanced head and neck cancer: 5‐year survival data from a phase 3 randomised trial, and relation between cetuximab‐induced rash and survival. Lancet Oncol 2010;11:21–28. [DOI] [PubMed] [Google Scholar]
- 31. Bonner JA, Giralt J, Harari PM et al. Association of human papillomavirus and p16 status with mucositis and dysphagia for head and neck cancer patients treated with radiotherapy with or without cetuximab: Assessment from a phase 3 registration trial. Eur J Cancer 2016;64:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Vermorken JB, Mesia R, Rivera F et al. Platinum‐based chemotherapy plus cetuximab in head and neck cancer. N Engl J Med 2008;359:1116–1127. [DOI] [PubMed] [Google Scholar]
- 33. Vermorken JB, Remenar E, Hitt R et al. Platinum‐based chemotherapy (CT) plus cetuximab in recurrent or metastatic squamous cell carcinoma of the head and neck cancer (R/M‐SCCHN): 5‐year follow‐up data for the extreme trial. J Clin Oncol 2014;32:6021a. [Google Scholar]
- 34. Mesia R, Rivera F, Kawecki A et al. Quality of life of patients receiving platinum‐based chemotherapy plus cetuximab first line for recurrent and/or metastatic squamous cell carcinoma of the head and neck. Ann Oncol 2010;21:1967–1973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Huang SM, Bock JM, Harari PM. Epidermal growth factor receptor blockade with C225 modulates proliferation, apoptosis, and radiosensitivity in squamous cell carcinomas of the head and neck. Cancer Res 1999;59:1935–1940. [PubMed] [Google Scholar]
- 36. Huang SM, Harari PM. Modulation of radiation response after epidermal growth factor receptor blockade in squamous cell carcinomas: Inhibition of damage repair, cell cycle kinetics, and tumor angiogenesis. Clin Cancer Res 2000;6:2166–2174. [PubMed] [Google Scholar]
- 37. Han R, Huangfu H, Gao W et al. Synergistic lethal effects of cetuximab combined with chemotherapy and/or radiotherapy in laryngeal squamous carcinoma cells. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2013;27:1375–1380. [PubMed] [Google Scholar]
- 38. Zhang N, Erjala K, Kulmala J et al. Concurrent cetuximab, cisplatin, and radiation for squamous cell carcinoma of the head and neck in vitro. Radiother Oncol 2009;92:388–392. [DOI] [PubMed] [Google Scholar]
- 39. Sung FL, Poon TC, Hui EP et al. Antitumor effect and enhancement of cytotoxic drug activity by cetuximab in nasopharyngeal carcinoma cells. In Vivo 2005;19:237–245. [PubMed] [Google Scholar]
- 40. Ferris RL, Jaffee EM, Ferrone S. Tumor antigen‐targeted, monoclonal antibody‐based immunotherapy: Clinical response, cellular immunity, and immunoescape. J Clin Oncol 2010;28:4390–4399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Siu LL, Waladron JN, Chen BE et al. Phase III randomized trial of standard fractionation radiotherapy (SFX) with concurrent cisplatin (CIS) versus accelerated fractionation radiotherapy (AFX) with panitumumab (PMab) in patients (pts) with locoregionally advanced squamous cell carcinoma of the head and neck (LA‐SCCHN): NCIC Clinical Trials Group HN.6 trial. J Clin Oncol 2015;33:6000a. [Google Scholar]
- 42. Vermorken JB, Stöhlmacher‐Williams J, Davidenko I et al. Cisplatin and fluorouracil with or without panitumumab in patients with recurrent or metastatic squamous‐cell carcinoma of the head and neck (SPECTRUM): An open‐label phase 3 randomised trial. Lancet Oncol 2013;14:697–710. [DOI] [PubMed] [Google Scholar]
- 43. Vokes EE, Worden FP, Adkins D et al. A randomized phase II trial of the MET inhibitor tivantinib + cetuximab versus cetuximab alone in patients with recurrent/metastatic head and neck cancer. J Clin Oncol 2015;33:6060a. [Google Scholar]
- 44. Fayette J, Wirth L, Oprean C et al. Randomized phase II study of duligotuzumab (MEHD7945A) vs cetuximab in squamous cell carcinoma of the head and neck (MEHGAN study). Front Oncol 2016;6:232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Machiels J, Haddad RI, Fayette J et al. Afatinib versus methotrexate (MTX) as second‐line treatment for patients with recurrent and/or metastatic (R/M) head and neck squamous cell carcinoma (HNSCC) who progressed after platinum‐based therapy: Primary efficacy results of LUX‐Head & Neck 1, a phase III trial. Abstract presented at 2014 Congress of the European Society for Medical Oncology; September 26–30, 2014; Madrid, Spain.
- 46. Klussmann JP, Gultekin E, Weissenborn SJ et al. Expression of p16 protein identifies a distinct entity of tonsillar carcinomas associated with human papillomavirus. Am J Pathol 2003;162:747–753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Giralt J, Trigo J, Nuyts S et al. Panitumumab plus radiotherapy versus chemoradiotherapy in patients with unresected, locally advanced squamous‐cell carcinoma of the head and neck (CONCERT‐2): A randomised, controlled, open‐label phase 2 trial. Lancet Oncol 2015;16:221–232. [DOI] [PubMed] [Google Scholar]
- 48. Adelstein DJ, Ridge JA, Gillison ML. Head and neck squamous cell cancer and the human papillomavirus: Summary of a national cancer institute state of the science meeting, November 9‐10, 2008, Washington, D.C. Head Neck 2009;31:1393–1422. [DOI] [PubMed] [Google Scholar]
- 49. Rietbergen MM, Snijders PJ, Beekzada D et al. Molecular characterization of p16‐immunopositive but HPV DNA‐negative oropharyngeal carcinomas. Int J Cancer 2014;134:2366–2372. [DOI] [PubMed] [Google Scholar]
- 50. Zuo Z, Keck MK, Khattri A et al. Multimodality determination of HPV status in head and neck cancers (HNC) and development of an HPV signature. J Clin Oncol 2013;31:6008a. [Google Scholar]
- 51. Jordan RC, Lingen MW, Perez‐Ordonez B et al. Validation of methods for oropharyngeal cancer HPV status determination in US cooperative group trials. Am J Surg Pathol 2012;36:945–954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Lingen MW, Xiao W, Schmitt A et al. Low etiologic fraction for high‐risk human papillomavirus in oral cavity squamous cell carcinomas. Oral Oncol 2013;49:1–8. [DOI] [PubMed] [Google Scholar]
- 53. Seiwert TY. Ties that bind: p16 as a prognostic biomarker and the need for high‐accuracy human papillomavirus testing. J Clin Oncol 2014;32:3914–3916. [DOI] [PubMed] [Google Scholar]
- 54. Bratman SV, Bruce JP, O'Sullivan B. Human papillomavirus genotype association with survival in head and neck squamous cell carcinoma. JAMA Oncol 2016;2:823–826. [DOI] [PubMed] [Google Scholar]
- 55. Weinberger PM, Yu Z, Haffty BG et al. Molecular classification identifies a subset of human papillomavirus‐associated oropharyngeal cancers with favorable prognosis. J Clin Oncol 2006;24:736–747. [DOI] [PubMed] [Google Scholar]
- 56. Badaracco G, Rizzo C, Mafera B et al. Molecular analyses and prognostic relevance of HPV in head and neck tumours. Oncol Rep 2007;17:931–939. [PubMed] [Google Scholar]
- 57. Lim MY, Dahlstrom KR, Sturgis EM et al. Human papillomavirus integration pattern and demographic, clinical, and survival characteristics of patients with oropharyngeal squamous cell carcinoma. Head Neck 2016;38:1139–1144. [DOI] [PubMed] [Google Scholar]
- 58. Parfenov M, Pedamallu CS, Gehlenborg N, et al. Characterization of HPV and host genome interactions in primary head and neck cancers. Proc Natl Acad Sci USA 2014;111:15544–15549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Rusan M, Li YY, Hammerman PS. Genomic landscape of human papillomavirus‐associated cancers. Clin Cancer Res 2015;21:2009–2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Koshiol J, Rotunno M, Gillison ML et al. Assessment of human papillomavirus in lung tumor tissue. J Natl Cancer Inst 2011;103:501–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Rosenthal DI, Harari PM, Giralt J et al. Impact of p16 status on the results of the phase III cetuximab (cet)/radiotherapy (RT). J Clin Oncol 2014;32:6001a. [Google Scholar]
- 62. Bonner JA, Harari PM, Giralt J et al. PD‐036: Association of HPV/p16 status with efficacy and safety in pts with OPC in the phase 3 RT/cetuximab registration trial. Radiother Oncol 2014;114:21–22. [Google Scholar]
- 63. Bonner JA, Rosenthal DI, Mesia R et al. p16 and human papillomavirus (HPV) subgroup analyses of the IMCL‐9815 and EXTREME cetuximab registration trials in squamous cell carcinoma of the head and neck (SCCHN). EHN 2016;0222a. [Google Scholar]
- 64. Castellsagué X, Alemany L, Quer M et al. HPV involvement in head and neck cancers: Comprehensive assessment of biomarkers in 3,680 patients. J Natl Cancer Inst 2016;28;108:djv403. [DOI] [PubMed] [Google Scholar]
- 65. Brizel DM, Albers ME, Fisher SR et al. Hyperfractionated irradiation with or without concurrent chemotherapy for locally advanced head and neck cancer. N Engl J Med 1998;338:1798–1804. [DOI] [PubMed] [Google Scholar]
- 66. Bourhis J, Overgaard J, Audry H et al. Hyperfractionated or accelerated radiotherapy in head and neck cancer: A meta‐analysis. Lancet 2006;368:843–854. [DOI] [PubMed] [Google Scholar]
- 67. Adelstein DJ, Li Y, Adams GL et al. An intergroup phase III comparison of standard radiation therapy and two schedules of concurrent chemoradiotherapy in patients with unresectable squamous cell head and neck cancer. J Clin Oncol 2003;21:92–98. [DOI] [PubMed] [Google Scholar]
- 68. Pignon JP, Syz N, Posner M et al. Adjusting for patient selection suggests the addition of docetaxel to 5‐fluorouracil‐cisplatin induction therapy may offer survival benefit in squamous cell cancer of the head and neck. Anticancer Drugs 2004;15:331–340. [DOI] [PubMed] [Google Scholar]
- 69. Pignon JP, Bourhis J, Domenge C et al. Chemotherapy added to locoregional treatment for head and neck squamous‐cell carcinoma: Three meta‐analyses of updated individual data. MACH‐NC collaborative group. Meta‐analysis of chemotherapy on head and neck cancer. Lancet 2000;355:949–955. [PubMed] [Google Scholar]
- 70. Curran D, Giralt J, Harari PM, et al. Quality of life in head and neck cancer patients after treatment with high‐dose radiotherapy alone or in combination with cetuximab. J Clin Oncol 2007;25:2191–2197. [DOI] [PubMed] [Google Scholar]