Abstract
The U.S. Mexican American population enjoys longer life expectancies relative to other racial/ethnic groups but is disproportionately affected by chronic conditions and functional limitations. Studying the impact of heterogeneity in age, time and other characteristics of migration among older Mexican Americans can inform our understanding of health disparities and health care needs in later-life. This research employed 20 years of data from the Hispanic Established Populations for the Epidemiologic Study of the Elderly to assess the proportion of life spent with functional limitations and one or more morbidity (by age of migration and gender) in the United States Mexican American population. Our results indicate early-life and late-life migrant women spend a larger number of years with performance-oriented mobility assessment (POMA) limitations than U.S.-born women. Conversely, mid-life migrant women were not statistically different from U.S.-born women in years spent disabled. Among men, mid-life migrants had longer life expectancies and spent more years disability-free than U.S.-born men. For morbidity, late-life migrant women spent a significantly smaller proportion of their elderly years with morbidity than U.S.-born women. However, late-life migrant men spent more years with morbidity than U.S.-born men. These findings illustrate that older Mexican Americans in the United States are heterogeneous in nativity and health outcomes. More years spent disabled/unhealthy may result in greater burden on family members and higher dependency on public resources. These findings have implications for the development of social and health policies to appropriately target the medical conditions and disabilities of older Mexican Americans entering late-life.
Keywords: Age of Migration, Mexican Americans, functional limitations, morbidity, life expectancy
Introduction
Despite a relatively disadvantaged socio-economic profile, Hispanics in the United States enjoy long life expectancies (1). At age 65 Hispanic men have a remaining life expectancy of 19 years and Hispanic women 21.7 years compared to 17.1 for non-Hispanic white men and 19.7 for non-Hispanic white women (2). However, higher life expectancy among Hispanic groups does not always coincide with overall favorable health since declines in mortality do not necessarily indicate that overall health has improved. Although longer life may be a goal in and of itself, the individual and social benefits of greater longevity may be undermined if the added years are characterized by high levels of chronic illness, functional limitations, and dependency (3). In fact, if mortality decreases while the incidence of chronic diseases increases or remains the same, the proportion of the population living in poor health will increase (4). For example, Mexican Americans (50 years and older) have been shown to have higher disability and functional limitations than non-Hispanic whites, even in the context of longer life expectancy among migrants (5, 6).
Despite a growing interest in Hispanic health by policy makers and researchers, most health studies focus broadly on nativity differences, and do not make distinctions among the foreign-born, thus downplaying potential health differentials (7). The U.S. Mexican American population is heterogeneous in regards to nativity; their health and functional status in later life may vary considerably depending on place of birth, gender, and socioeconomic status. For instance, migration selectivity is thought to shape the health profiles of Mexican migrants to the United States. Selective migration, is defined as the disproportionate migration by healthy individuals born in Mexico into the U.S. compared with those in poor health (8, 9). Following this interpretation, positive health selection may contribute in part to a health advantage for U.S. Mexican migrants. This phenomenon has been observed in a host of studies (8-10).
While previous research has found a “healthy immigrant effect” in mortality among foreign-born Hispanics (inclusive of Mexicans) in the United States, a growing body of evidence suggests U.S.-born Hispanics spend more years of life with functional limitations and chronic morbidity (3, 6, 11). For example, Cantu et al. document the mortality and health advantages in morbidity and physical functioning among older foreign-born Hispanics which are not shared by U.S.-born Hispanics (6). Conversely, Angel et al. using data from the Hispanic Established Populations for Epidemiologic Studies of the Elderly (H-EPESE), found foreign-born Mexican American women spent approximately two-thirds of their remaining years of life after age 65 with a functional limitation despite having longer life expectancies than Mexican American men and U.S.-born Mexican American women (11).
However, less research has focused on how positive health selection varies by migrant subgroups. Consequently, the purpose of this study was to assess whether the “healthy immigrant effect” that has been documented in mortality extended to physical functioning and morbidity by examining the number of years past 65 lived with functional limitations and chronic disease (1). We draw on 20-years of data from the H-EPESE to address the following question: to what extent does physical functioning and healthy life expectancy differ for Mexican Americans by nativity and age of migration? We employ a life course perspective to test the “healthy immigrant effect,” by age of migration, among foreign-born Mexican Americans. This framework aims to link migration and healthy aging. We argue that the life experiences of Mexican migrants are likely shaped by the age at which they migrated. The inclusion of age of migration is particularly important in order to gain a better understanding of why nativity differences exist among U.S.-born and foreign-born Mexican Americans (7). Health selection likely varies by gender and age of migration. For example, health selectivity may be strongest in young and middle ages when foreign-born Mexican Americans decide to migrate to pursue occupational opportunities in agriculture, construction, and the service sector in which jobs can be physically demanding (12). Labor migrants are by definition healthy enough to migrate, face potential challenges of migration, and work when they arrive (13). Conversely, Mexicans who migrated in early-life are likely to have been brought by their parents or to join family members already settled in the United States. These migrants have little or no selection since their migration reflects their parents' characteristics and they do not to meet the demands required for migration themselves (7, 13). Likewise, health selectivity may be weaker among late-life Mexican migrants who likely migrate for family reunification rather than occupational opportunities (3, 14). In addition, negative health selection may be observed among some late-life migrants who come to the United States to seek care from family members.
Methods
Data
We employed data from the Hispanic Established Populations for the Epidemiologic Study of the Elderly (H-EPESE) to estimate the proportion of life spent in a disabled/unhealthy state prior to death for U.S.-born and foreign-born Mexican Americans. The H-EPESE is an ongoing longitudinal cohort study of community-dwelling Hispanic elderly (65 years and older), residing in the five southwestern states of Arizona, California, Colorado, New Mexico, and Texas (15). These data provide detailed information on risk factors for physical illness and mortality for a sample of 3,050 individuals first interviewed in 1993-1994. This panel was re-contacted in 1995-96, 1998-99, 2000-01, 2004-05, 2007, 2010-11 and 2012-2013. A new cohort of 902 individuals (75 or older at the time) was added in 2004 to increase sample size. We used aggregated individual level data from 1993-2013 to obtain prevalence estimates across survey years with a mortality linkages through National Death Index (NDI) up to Dec. 31, 2015. Respondents ranged in age from 65-107 years. Individuals (n=563) missing data on covariates are omitted. The final analytic sample included 3,389 unique individuals totaling 35,701 person-years of data.
Measures
We used the performance-oriented mobility assessment (POMA) to assess functional mobility. The POMA is based on three tasks: standing balance (semi-tandem and side by side), a timed 8-ft walk at a normal pace (gait speed), and a timed test of five repetitions of rising from a chair and sitting down (16). Each assessment was coded (0) unable to complete task, (1) poor, (2) moderate, (3) good, and (4) best. Respondents who received a score of (0) on at least one POMA item were coded as having POMA limitations. Our assessment of morbidity is based on any occurrence of at least one of four self-reported items that asked whether the respondent had ever been told by a doctor that he/she ever had (a) diabetes, (b) heart attack, (c) a stroke, or (d) any cancer.
Socio-demographic Characteristics
To classify nativity, we used birth place information and categorized respondents born in the U.S. versus Mexico. Following previous research we created three groups to measure life course stage at migration: those who arrived in early-life (0–19 years); middle-life (20–49 years); and late-life (≥50 years) (11, 17-18). Recent research suggests age of migration can be useful for understanding migrant health in later-life by approximating type of migration (i.e. labor versus family), the degree of health selectivity upon arrival, and the ability to maintain good health among migrants (7, 18-19). In addition, the following sociodemographic variables are used in the descriptive analysis: gender, age, and years of education.
Statistical Analysis
The study combined age-specific mortality rates with age-specific prevalence of morbidity and POMA limitations to calculate Sullivan-based life table models of disabled/unhealthy life expectancy and disability-free/healthy life expectancy for each group (20). This technique is a prevalence-based method of estimating healthy life expectancy. This method divides total life expectancy into the different health states based on the age-specific prevalence of disabled/unhealthy (with POMA limitation and morbidity) and non-disabled and healthy (POMA limitation-free and morbidity-free) states. Non-disabled/disabled (healthy/unhealthy) life expectancy calculated by this method is the number of remaining years (at a specific age) which a population can expect to live in a non-disabled/disabled (healthy/unhealthy) state (21).
To evaluate whether nativity groups (U.S.-born and three age of migration groups) differed by gender, estimates of the total life expectancy, non-disabled/disabled life expectancy and healthy/unhealthy life expectancy and the corresponding standard errors were obtained through 300 bootstrapping life tables for each group by gender. The statistical significance was further assessed at significance level 0.05, 0.01, and/or 0.001.
Results
Table 1 presents descriptive characteristics for the study sample by nativity group and gender. In the overall population, 43.0% were foreign-born and 60.4% of respondents were females. Approximately one quarter of respondents had migrated in mid-life. In general, foreign-born Mexican Americans were slightly older than their U.S.-born counterparts, regardless of gender. Similarly, mean years of education was higher among U.S.-born respondents than foreign-born respondents. As expected, there are statistically significant differences in age and education by nativity for both females and males (p<.05).
Table 1. Socio-demographic Characteristics on Gender among Mexican-Origin Elders Age 65 and Older by Nativity and Age of Migration, 1993-2013a.
| Females | Males | |||||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| U.S.-Born | Foreign-Born (Age of Migration) |
U.S.-Born | Foreign-Born (Age of Migration) |
|||||
|
|
|
|||||||
| 0-19 | 20-49 | 50+ | 0-19 | 20-49 | 50+ | |||
|
|
|
|||||||
| N (%) | 5,019 | 857 | 1,923 | 844 | 3,137 | 583 | 1,442 | 494 |
| (58.1) | (9.9) | (22.3) | (9.8) | (55.5) | (10.3) | (22.5) | (8.7) | |
| Age b | 78.5 | 81.7* | 78.4 | 80.2* | 77.7 | 80.8* | 78.2* | 79.8* |
| (7.2) | (8.0) | (7.4) | (7.8) | (6.9) | (7.7) | (7.2) | (7.9) | |
| Education b | 6.1* | 4.9* | 4.5* | 3.1* | 6.6* | 4.3* | 3.8* | 2.3* |
| (4.1) | (3.5) | (3.5) | (3.2) | (4.5) | (3.7) | (3.4) | (2.6) | |
Total observations of females and males were 8,643 (60.4%) and 5,656 (39.6%) respectively; U.S.-born and foreign-born were 8,156 (57%) and 6,143 (43%) respectively; corresponding weighted percentages were shown within parentheses. For age and years of education, the weighted means were shown and the standard deviations were presented within parentheses.
For age and education,
represents a significant difference between age of migration group and U.S.-born (p.<.05).
Table 2 presents estimates of life expectancy for U.S.-born and three age of migration groups for Mexican American men and women at age 65, as well as the average number of years spent with and without POMA limitations and chronic morbidity. Overall, life expectancy for the foreign-born was higher than the U.S.-born regardless of gender. Foreign-born Mexican American women who migrated in early-life and late-life exhibited no health selectivity in later life and experienced a significantly higher number of elderly years spent with POMA limitations than U.S.-born Mexican American women (12.8 years and 12.9 years vs. 10.2 years, respectively) (see also Figure 1: Panel A). Moreover, the ratio of number of years lived without any POMA limitations to the total number of years lived was lower for late-life migrant when compared to U.S.-born women (0.34 vs. 0.42). Late-life migrant women were particularly disadvantaged in both years spent with any POMA limitation and the remaining years after age 65 in a disabled state. Out of the additional 3 years of life expectancy at age 65 (20.8 years vs. 17.8 years), early-life migrant women could expect to spend an additional 2.6 years with POMA limitations compared to U.S.-born women. Conversely, mid-life migrant women were not statistically different from U.S.-born women in years disabled-free. Among men, results showed no statistically significant differences by age of migration groups in the number of years spent with POMA limitations or in the ratio of years after 65 spent non-disabled compared to U.S.-born Mexican American men. However, mid-life migrant men exhibited positive health selectivity in both longer life expectancies (17.1 years vs. 15.4 years) and years spent non-disabled after age 65 (9.0 years vs. 7.6 years) compared to U.S.-born Mexican American men.
Table 2. POMA and Morbidity Life Expectancy Years at Age 65 by Gender, Nativity, and Age of Migration a, b.
| POMA c | ||||
|---|---|---|---|---|
|
|
||||
| Females | ||||
|
|
||||
| U.S.-Born | Foreign-Born (Age of Migration) | |||
|
|
||||
| 1-19 | 20-49 | 50+ | ||
|
|
||||
| TLE | 17.8 | 20.8*** | 18.9 | 19.5 |
| (0.34) | (0.81) | (0.49) | (0.83) | |
| DFLE | 7.5 | 8.0 | 8.0 | 6.6 |
| (0.23) | (0.60) | (0.37) | (0.50) | |
| DLE | 10.2 | 12.8*** | 10.9 | 12.9*** |
| (0.24) | (0.75) | (0.38) | (0.78) | |
| Ratio | 0.42 | 0.38 | 0.42 | 0.34*** |
| (0.01) | (0.03) | (0.02) | (0.02) | |
|
|
||||
| Males | ||||
|
|
||||
| U.S.-Born | Foreign-Born (Age of Migration) | |||
|
|
||||
| 1-19 | 20-49 | 50+ | ||
|
|
||||
| TLE | 15.4 | 16.0 | 17.1* | 16.1 |
| (0.31) | (1.09) | (0.61) | (0.89) | |
| DFLE | 7.6 | 7.5 | 9.0* | 7.8 |
| (0.28) | (0.62) | (0.47) | (0.51) | |
| DLE | 7.9 | 8.5 | 8.2 | 8.3 |
| (0.24) | (0.85) | (0.43) | (0.76) | |
| Ratio | 0.49 | 0.47 | 0.52 | 0.49 |
| (0.01) | (0.03) | (0.02) | (0.03) | |
|
|
||||
| Morbidity d | ||||
|
|
||||
| Females | ||||
|
|
||||
| U.S.-Born | Foreign-Born (Age of Migration) | |||
|
|
||||
| 1-19 | 20-49 | 50+ | ||
|
|
||||
| TLE | 17.8 | 20.8*** | 18.9 | 19.5 |
| (0.34) | (0.81) | (0.49) | (0.83) | |
| HLE | 9.6 | 12.1** | 11.4** | 12.6*** |
| (0.32) | (0.81) | (0.50) | (0.79) | |
| ULE | 8.2 | 8.7 | 7.5 | 6.9* |
| (0.27) | (0.76) | (0.38) | (0.52) | |
| Ratio | 0.54 | 0.58 | 0.60** | 0.65*** |
| (0.01) | (0.03) | (0.02) | (0.03) | |
|
|
||||
| Males | ||||
|
|
||||
| U.S.-Born | Foreign-Born (Age of Migration) | |||
|
|
||||
| 1-19 | 20-49 | 50+ | ||
|
|
||||
| TLE | 15.4 | 16.0 | 17.1* | 16.1 |
| (0.31) | (1.09) | (0.61) | (0.89) | |
| HLE | 8.5 | 9.5 | 11.0*** | 7.2 |
| (0.32) | (1.11) | (0.47) | (0.85) | |
| ULE | 7.0 | 6.5 | 6.1 | 9.0* |
| (0.25) | (0.67) | (0.39) | (0.74) | |
| Ratio | 0.55 | 0.59 | 0.64*** | 0.44* |
| (0.02) | (0.04) | (0.02) | (0.04) | |
POMA denoted performance-oriented mobility assessment.
denoted the statistical significance on P < .05.
denoted the statistical significance on P < .01.
denoted the statistical significance on P < .001.
The corresponding standard errors on life expectancy years were presented within parentheses.
TLE, DFLE, and DLE denoted total life expectancy, disabled-free life expectancy, and disabled life expectancy, respectively. Ratio denoted the ratio of non-disabled life expectancy and total life expectancy.
TLE, HLE, and ULE denoted total life expectancy, healthy life expectancy, and unhealthy life expectancy, respectively. Ratio denoted the ratio of healthy life expectancy and total life expectancy.
Figure 1.
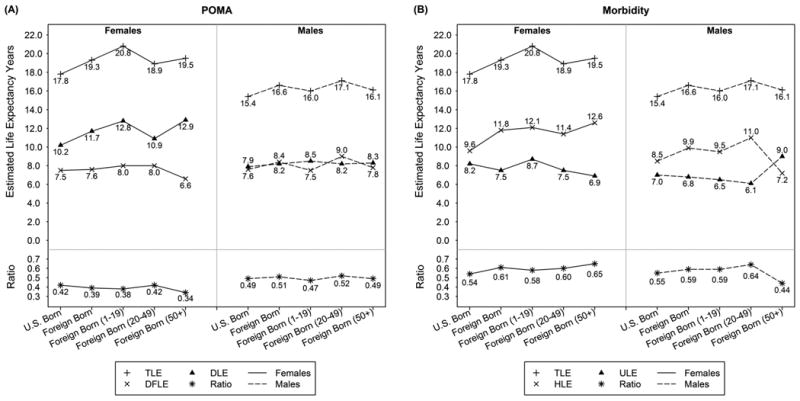
The estimated life expectancy years of POMA (performance-oriented mobility assessment) and morbidity at age 65 were shown by gender, nativity, and age of migration on foreign born (0-19, 20-49, and 50+). In POMA panel, TLE (+), DFLE (×), and DLE (▲) denoted total life expectancy, disabled-free life expectancy, and disabled life expectancy, respectively. Ratio denoted the ratio of non-disabled life expectancy and total life expectancy. The corresponding patterns on females and males were presented by solid and dashed lines, respectively. In morbidity panel, TLE (+), HLE (×), and ULE (▲) denoted total life expectancy, healthy life expectancy, and unhealthy life expectancy, respectively. Ratio denoted the ratio of healthy life expectancy and total life expectancy. The corresponding patterns on females and males were presented by solid and dashed lines, respectively.
For life expectancy with and without any morbidity (Figure 1: Panel B), late-life migrant women spent a statistically significant (p. <.001) shorter amount of their elderly years with morbidity when compared to U.S.-born women (6.9 years vs. 8.2 years) and exhibited the least amount of health selectivity in old age among migrant groups. Furthermore, the ratio of number of years lived with and without morbidity to the total number of years lived was higher in mid- and late-life foreign-born women when compared to U.S-born Mexican American women (0.60 and 0.65 vs. 0.54). However, among men late-life migrants spent a significantly larger number of years with morbidity when compared their U.S.-born counterparts (9.0 years vs. 7.0 years). Additionally, the ratio of number of elderly years lived without morbidity to the total number of years lived was higher for mid-life migrants but lower for late-life migrants when compared to U.S.-born Mexican American men (0.64 for mid-life migrants, 0.44 for late-life migrants, and 0.55 for U.S.-born Mexican Americans).
Discussion
Relative to non-Hispanics, older Hispanics exhibit longer life expectancies (2). Recent research suggests older Hispanics have both a higher life expectancy, and health advantages in physical functioning and morbidity in comparison to their U.S.-born counterparts (11). This analysis examined nativity and age of migration differences to assess whether the “healthy immigrant effect” that has been documented among migrants in mortality extends to functional capacity and morbidity among older Mexicans Americans. Prior studies reported that older late-life migrants had lower prevalence of certain chronic conditions including cancer, lung disease, and cardiovascular disease (22-23). Our results were consistent with past research, with evidence supporting a nativity advantage among older foreign-born Mexican Americans in morbidity, particularly among women. The results presented above advance prior research by demonstrating the heterogeneity among foreign-born Mexican Americans by age of migration. We documented how some foreign-born Mexican migrants are able to preserve their health into later life, while others experience negative health outcomes in physical functioning and morbidity relative to U.S.-born Mexican Americans. Specifically, we show that early-life and late-life migration among women significantly accounts for the nativity disadvantage in disabled/unhealthy life expectancy, while mid-life male migrants accounted for differences in total life expectancy, and retained significantly more years without any POMA limitation after age 65 among age of migration groups.
Some researchers have proposed that a health advantage among migrants of reduced late-life morbidity may partially be due to health selection, lifestyle factors, and selective return of ailing migrants to their country of origin (Salmon hypothesis) (24). Our findings are suggestive of a positive health selection for mid-life male migrants (in total life expectancy and years after 65 healthy/non-disabled), and supports the premise that healthy mid-life male migrants primarily migrate in search of work-related opportunities, while older migrant women mostly migrate for family reunion purposes (3, 13). There is a positive selection for migrants who leave in search of occupational opportunities, as a minimum amount of motivation and resources is necessary to make the move (25-26). Cultural and behavioral factors, along with strong social networks have been identified as protective factors among migrants (27). The deterioration of health outcomes with acculturation, time spent in the U.S., and over generations substantiates this assertion (27). Overall, our findings show gender and age of migration to be important predictors of morbidity and POMA limitations among older Mexican Americans and have great implications for long-term care in aging population.
There are plausible explanations for why foreign-born Mexican migrants experience high life expectancy and have high prevalence of functional limitations. First, positive health selectivity may be linked directly to the historical time period and government policy under which many Mexican individuals migrated to the United States. Over 50% of migrants in our analysis migrated to the U.S. during the era of the Bracero Program (1942-1964). This program was initiated by the U.S. government in response to wartime labor shortages in the agricultural industry, which led to legislation for the temporary migration for Mexican farmworkers (28). Second, this cohort of Mexican labor workers most likely spent decades performing physically taxing labor, with limited access to health care, and few labor laws to protect them (28). Thus, the higher rates of physical limitations are most likely tied to hazardous working conditions and not necessarily an exclusive result of poor health caused by chronic disease.
The current study findings should be viewed in light of several limitations. Although we utilized similar measures on chronic conditions in previous research, the limited number of morbidity indicators in the H-EPESE may weaken the predictive validity of our measure for morbidity (6). Among others, respiratory problems which can be important for older adults who have worked in agriculture and cognitive impairment/dementia (a common impairment among older adults) are excluded from the present analysis. In addition, data are based on self-report which may affect results due to recall bias. Furthermore, undiagnosed diseases among foreign-born Mexican Americans are higher than non-Hispanic whites and U.S.-born Mexican Americans due to lack of insurance (29). Although, nearly universal health care coverage through Medicare for older adults has shown self-reported medical conditions to be consistent with medical reports.
Studies examining healthy life expectancy by nativity and age of migration are scarce (17), and our study partially addressed this gap in the literature. To the best of our knowledge this is the first study in the U.S. to assess the effects of age of migration on morbidity and POMA limitations among older Mexican Americans. With aging Mexican Americans representing a large proportion of the ever-growing U.S. Hispanic population, a better understanding of how nativity and age of migration may be associated with health in later life is particularly important to gain a better understanding of why nativity differences exist among U.S.-born and foreign-born Mexican Americans. Such understanding can inform policy discussions regarding healthy aging and quality of life among older minority and migrant adults in the United States. The combination of long life expectancy and unfavorable socioeconomic and educational characteristics raises important questions regarding health and functionality among the older U.S. Hispanic population. What is the relationship between occupational hazards in early to mid-life on late-life incidence of cancer, stroke and other physical functioning but potentially preventable conditions? How does access to health insurance impact onset of high prevalence of functional limitations among the old-old of Mexican American women? Do workplace regulations and policy enacted over the last 50 years affect the occupation-related late life physical functioning among older men with limited education? All these are questions need to be addressed in future studies. The possibility of a longer life characterized by compromised health also underscores the potential burden on public health service and family caregiving; particularly for minority and migrant groups who report higher levels of time intensive caregiving than whites (30). Research on the timing of migration also has important health policy and health care forecasting implications for long-term care needs, caregiver burden, public health resources and culture-appropriate lifestyle interventions (including leveraging the protective Hispanic-specific social cultural factors) geared towards keeping older Hispanics independent and functional in their late years. With the rapid aging of the Mexican-American population, our findings underscore the need for development and implementation of culture appropriate public health programs aimed towards reducing negative late-life health outcomes and increasing access for patient-centered management of diabetes and other disabling diseases that are prevalent among older Hispanics.
Acknowledgments
Funding: This study was supported by the NIH National Institute of Minority Health and Health Disparities (R01 MD005894-01), National Institute on Aging (R01 AG10939-10 and 5T32AG270) and by the National Institutes of Health (R01-AG018016, R.W. [PI]) and by the UTMB Sealy Center on Aging. Dr. Valderrama-Hinds is a visiting scholar in the WHO/PAHO Collaborating Center on Aging and Health at UTMB during this study.
Footnotes
Conflict of Interest: The authors have no conflicts to declare.
Author Contributions: Garcia: study concept. Garcia, Chui: data acquisition. Garcia, Valderrama-Hinds, Chui, Chen: data analysis. Garcia, Valderrama-Hinds, Chen, Mutambudzi, Raji: manuscript preparation.
Sponsor's Role: No sponsor had a role in the design, methods, analysis, and preparation of the paper.
References
- 1.Markides KS, Eschbach K. Aging, migration, and mortality: Current status of research on the Hispanic paradox. J Gerontol B Psychol Sci Soc Sci. 2005;60:68–75. doi: 10.1093/geronb/60.special_issue_2.s68. [DOI] [PubMed] [Google Scholar]
- 2.Arias E. United States life tables by Hispanic origin. Vital Health Stat 2. 2010;152:1–33. [PubMed] [Google Scholar]
- 3.Markides KS, Eschbach K, Ray LA, et al. Census disability rates among older people by race/ethnicity and type of Hispanic origin. In: Angel JL, Whitfield KE, editors. The health of aging Hispanics. New York: Springer New York; 2007. pp. 26–39. [Google Scholar]
- 4.Crimmins EM. Trends in the health of the elderly. Annu Rev Public Health. 2004;25:79–98. doi: 10.1146/annurev.publhealth.25.102802.124401. [DOI] [PubMed] [Google Scholar]
- 5.Hayward MD, Hummer RA, Chiu C, et al. Does the Hispanic paradox in mortality extend to disability? Popul Res Policy Rev. 2014;33:81–96. doi: 10.1007/s11113-013-9312-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cantu PA, Hayward MD, Hummer RA, et al. New estimates of racial/ethnic differences in life expectancy with chronic morbidity and functional loss: evidence from the National Health Interview Survey. J Cross Cult Gerontol. 2013;28(3):283–97. doi: 10.1007/s10823-013-9206-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gubernskaya Z. Age at migration and self-rated health trajectories after age 50: Understanding the older immigrant health paradox. J Gerontol B Psychol Sci Soc Sci. 2014;70:279–290. doi: 10.1093/geronb/gbu049. [DOI] [PubMed] [Google Scholar]
- 8.Bostean G. Does selective migration explain the Hispanic paradox? A comparative analysis of Mexicans in the U.S. and Mexico. J Immigr Minor Health. 2013;15(3):624–635. doi: 10.1007/s10903-012-9646-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Riosmena F, Wong R, Palloni A. Migration selection, protection, and acculturation in health: a binational perspective on older adults. Demography. 2013;50(3):1039–1064. doi: 10.1007/s13524-012-0178-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Garcia MA, Angel JL, Angel RJ, et al. Acculturation, gender, and active life expectancy in the Mexican-origin population. J Aging Health. 2015;27(7):1247–1265. doi: 10.1177/0898264315577880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Angel RJ, Angel JL, Hill TD. Longer lives, sicker lives? Increased longevity and extended disability among Mexican-origin elders. J Gerontol B Psychol Sci Soc Sci. 2014;70(4):639–49. doi: 10.1093/geronb/gbu158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gubernskaya Z, Bean FD, Van Hook J. (Un)Healthy immigrant citizens: Naturalization and activity limitations in older age. J Health Soc Behav. 2013;54(4):427–443. doi: 10.1177/0022146513504760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Angel RJ, Angel JL, Díaz Venegas C, et al. Shorter stay, longer life: Age at migration and mortality among the older Mexican-origin population. J Aging Health. 2010;22(7):914–31. doi: 10.1177/0898264310376540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Treas J. Incorporating immigrants: Integrating theoretical frameworks of adaptation. J Gerontol B Psychol Sci Soc Sci. 2015;70:269–278. doi: 10.1093/geronb/gbu067. [DOI] [PubMed] [Google Scholar]
- 15.Markides KS, Rudkin L, Angel RJ, et al. Health status of Hispanic elderly. In: Martin LG, Soldo BJ, editors. Racial and Ethnic Differences in the Health of Older Americans. Washington (DC): National Academies Press (US); 1997. pp. 285–300. [PubMed] [Google Scholar]
- 16.Guralnik JM, LaCroix AZ, Branch LG, et al. Morbidity and disability in older persons in the years prior to death. Am J Public Health. 1991;81(4):443–447. doi: 10.2105/ajph.81.4.443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Garcia MA, Chiu CT. Age at migration and disability-free life expectancy among the elder Mexican-origin population. Demographic Research. 2016;35:1523–1536. doi: 10.4054/DemRes.2016.35.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Garcia MA, Reyes AM. Physical Functioning and Disability Trajectories by Age of Migration Among Mexican Elders in the United States. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2017 Jan 3; doi: 10.1093/geronb/gbw167. gbw167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Markides KS, Rote S. Emerging Trends in the Social and Behavioral Sciences. John Wiley & Sons Inc; 2015. Immigrant health paradox. [Google Scholar]
- 20.Sullivan DF. A single index of mortality and morbidity. HSMHA Health Rep. 1971;86(4):347–54. [PMC free article] [PubMed] [Google Scholar]
- 21.Jagger C, Cox B, Le Roy S. Health expectancy calculation by the Sullivan method. EHEMU Technical Report. 2006 [Google Scholar]
- 22.Colón-López V, Haan MN, Aiello AE, et al. The effect of age at migration on cardiovascular mortality among elderly Mexican immigrants. Ann Epidemiol. 2009;19(1):8–14. doi: 10.1016/j.annepidem.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Swallen KC. Do health selection effects last? A comparison of morbidity rates for elderly adult immigrants and US-born elderly persons. J Cross Cult Gerontol. 1997;12(4):317–39. doi: 10.1023/a:1006527615599. [DOI] [PubMed] [Google Scholar]
- 24.Thomson EF, Nuru-Jeter A, Rischardson D, et al. The Hispanic paradox and older adults' disabilities: Is there a healthy migrant effect? Int J Environ Res Public Health. 2013;10(5):1786–1814. doi: 10.3390/ijerph10051786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Palloni A, Arias E. Paradox lost: Explaining the Hispanic adult mortality advantage. Demography. 2004;41(3):385–415. doi: 10.1353/dem.2004.0024. [DOI] [PubMed] [Google Scholar]
- 26.Rubalcava LN, Teruel GM, Duncan T, et al. The healthy migrant effect: New findings from the Mexican Family Life Survey. Am J Public Health. 2008;98(1):78–84. doi: 10.2105/AJPH.2006.098418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kimbro RT, Bzostek S, Goldman N, et al. Race, ethnicity, and the education gradient in health. Health Aff. 2008;27(2):361–72. doi: 10.1377/hlthaff.27.2.361. [DOI] [PubMed] [Google Scholar]
- 28.Massey D, Durand J, Malone N. Beyond Smoke and Mirrors: Mexican Immigration in an Era of Economic Integration. Russell Sage Foundation. 2003 [Google Scholar]
- 29.Barcellos SH, Goldman DP, Smith JP. Undiagnosed disease, especially diabetes, casts doubt on some of reported health ‘advantage’of recent Mexican immigrants. Health Aff. 2012;31(12):2727–2737. doi: 10.1377/hlthaff.2011.0973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rote S, Moon H. Racial/Ethnic Differences in Caregiving Frequency: Does Immigrant Status Matter? The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2016 Aug 3; doi: 10.1093/geronb/gbw106. gbw106. [DOI] [PubMed] [Google Scholar]


