Abstract
Objectives
Investigate associations of diffuse idiopathic skeletal hyperostosis (DISH) with self-reported and measured physical function in older adults.
Design
Cross-sectional analyses of data collected in 1992-96 from a longitudinal cohort.
Setting
Research clinic within a community.
Participants
Community-dwelling men (n=630) and women (n=961), mean age 71.5 years (SD=10.8), from the Rancho Bernardo Study.
Measurements
DISH assessed from lateral thoracic and lumbar spine radiographs; self-reported difficulty bending over to the floor, walking 2-3 level blocks, or climbing 1 flight of stairs; performance-based measures of grip strength and chair-stand testing (ability to stand up and sit down in a chair 5 times without using chair arms).
Results
DISH was present in 25.6% of men and 5.5% of women. In age and sex-adjusted models, those with DISH had 1.72-fold increased odds (95% CI: 1.13, 2.62) of self-reported difficulty bending; this remained significant after further adjustment for Cobb angle, weight, stroke, arthritis, and exercise, OR=1.69, (95% CI: 1.07, 2.66). In fully adjusted multivariate models, those with DISH had worse grip strength, -1.08kg, p=0.01, but did not differ from those without DISH on walking or climbing stairs. In sex-stratified, fully adjusted models, among men only, those with DISH were 2.17-times (95% CI: 1.04–4.52) more likely to be unable to complete 5 chair stands without using their arms.
Conclusions
DISH was less prevalent in women but affected almost one-quarter of older white men. Persons with DISH are more likely to experience physical functional impairment, suggesting that DISH has clinical correlations and is not an incidental radiographic finding.
Keywords: Aging, diffuse idiopathic skeletal hyperostosis (DISH), physical function, sex differences
Introduction
Diffuse idiopathic skeletal hyperostosis (DISH) is a non-inflammatory skeletal disease characterized by ligamentous ossification of the anterolateral spine, but very little is known about its clinical implications. Estimates of the prevalence of DISH range from 10% to over 40% depending upon the cohort.1-3 DISH is approximately twice as common in older men than women.4 The distinctive radiographic finding is flowing calcification and ossification along the anterolateral aspects of at least 4 contiguous vertebral bodies, with preservation of the affected levels' disc space. DISH can involve multiple vertebral levels and extend across the cervical and thoracolumbar regions of the spine. Similar ossification can be seen at the shoulder, iliac crest, ischial tuberosity, trochanters of the hip, tibial tuberosities, patellae, and bones of the hands and/or feet.5 Limited motion of the thoracic spine is the most commonly reported abnormality, and older adults with DISH report more overall physical and spinal disability compared to age-matched controls.6 DISH has also been associated with back pain in some, but not all, studies.2,6-8 Unfortunately, little is known about the clinical implications of DISH, in particular its impact on objective measures of physical function.
The characteristic ossification of the anterior longitudinal ligament in DISH may inhibit the ability to perform physical function tasks that require flexibility in the spine. Basic activities of daily living (ADLs) such as bathing, dressing, toileting, and physical function tasks such as standing up from a chair and reaching require flexibility in the spine that may become limited with DISH. For example, the spine may be unable to extend to shift the body weight appropriately during the transition from sit to stand. In cadaver studies, transection of the anterior longitudinal ligament resulted in a 16 degree mean increase in thoracic spine extension,9 supporting the potential role of DISH in limiting certain physical functional activities. Furthermore, spinal stiffness associated with DISH may have a negative impact on overall physical strength and physical activity, however this has not been well established.
Given the limited knowledge about the clinical implications of DISH in older populations, and that functional deficits associated with DISH have been limited to self-reported limitations in physical function, we conducted a cross-sectional study to investigate the association of DISH with self-reported and objectively measured physical function in a large community-dwelling cohort of older adults.
Methods
Participants
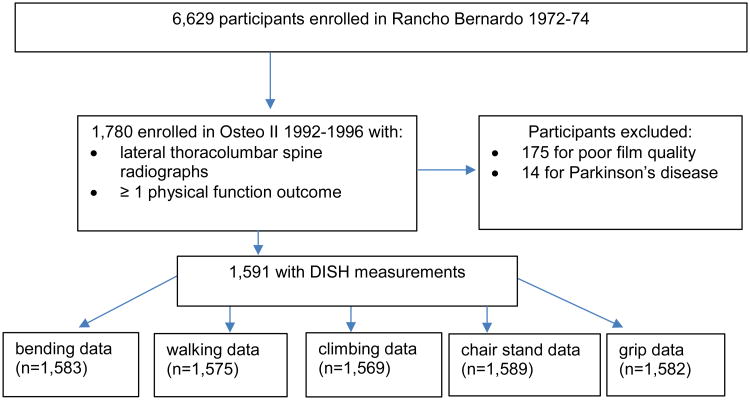
In 1972-74, 6,629 adults representing 82% of adults from the predominantly white and middle- to upper-middle class southern California community of Rancho Bernardo, were enrolled in a study of heart disease risk factors. These individuals have been followed ever since with periodic research clinic visits (approximately every 4 years) and yearly mailed surveys. In 1992-1996, 1,780 individuals aged 50 years and older, representing 80% of the original cohort, participated in a follow-up research clinic visit focused on skeletal assessment of osteoporosis (Osteo II). Bone mineral density (BMD) was measured at the hip and spine, lateral thoracolumbar spine radiographs, and measures of physical function were obtained at this visit. After excluding 175 lateral thoracic and lumbar spine radiographs of insufficient quality to measure DISH, and 14 reporting Parkinson's disease, there remained a total of 1,591 participants (630 men and 961 women) who were included in this cross-sectional study. Missing physical function and other covariate measures reduced the sample further so that analyses included 1,415 to 1,589 participants, depending upon the outcome (See Figure 1).
Figure 1. Flow chart of Study Sample Based Upon Each Physical Function Outcome.
This study was approved by Human Research Protections Program of the University of California, San Diego. All participants gave written informed consent prior to participation.
Measurements
Definition of DISH
Diffuse idiopathic skeletal hyperostosis (DISH) was assessed from lateral thoracic and lumbar spine radiographs obtained at the Osteo II visit using the standard Resnick radiologic criteria of: 1) the presence of flowing calcification and ossification along the anterolateral aspect of ≥ 4 contiguous vertebral bodies; 2) a relative preservation of disc height; and 3) absence of apophyseal joint bony ankylosis, sclerosis, or bony fusion.10 Radiographs were read once by an experienced radiologist. A previous study reported a kappa of 0.9 (95% CI: 0.8–0.9) for the intra-rater agreement in repeat assessments of DISH from the same radiograph.11
Physical functions
A hand held dynamometer (Therapeutic Instruments Hand Dynamometer, Clifton, NJ, USA) was used to measure grip strength (kg) in each hand. One practice trial and two test trials were performed, and the maximum grip strength value of the hand that was the highest was used in the analysis. Participants were timed performing the chair stand test where they were asked to stand up and sit down in a chair 5 times without using their arms.12 A categorical variable was created to classify subjects as never having to use their arms versus those having to use their arms at least some, or all of the time while performing the chair stand test. Participants were interviewed and asked whether they had difficulty (yes/no) bending over to the floor, walking 2 to 3 blocks on level ground, or climbing 1 flight of stairs.
Covariates
Questionnaire
Educational level was obtained at previous visits. At the Osteo II visit, self-administered surveys were used to obtain information on age, sex, and history of physician diagnosed medical conditions including stroke, hypertension, myocardial infarction, diabetes, Parkinson's disease, chronic obstructive pulmonary disease, osteoarthritis, and osteoporotic fractures. Reported hip, spine, wrist and clavicle fractures were confirmed by medical record review. Self-administered surveys were also used to obtain information regarding health behaviors including smoking (current/past/never), alcohol consumption (drinks/week, ml/week, and >12 drinks in the past year), back pain (no/yes) and exercise ≥three times/week (no/yes).
Examinations
During the clinic visit, bone mineral density (BMD) of the total hip, femoral neck, and lumbar spine were measured using dual-energy x-ray absorptiometry (DXA) (QDR 1000; Hologic, Inc., Waltham, MA, USA). Total hip BMD of the femoral neck, intertrochanter, and greater trochanter and spine BMD, the average BMD of the lumbar vertebrae L1-L4, were ascertained from the Hologic reports. Using a phantom standard, daily calibration of the DXA scanner yielded measurements precision of ≤ 1% for the spine and ≤ 1.5% for the hip. Height and weight were measured with participants in light clothing and without shoes; body mass index was used as an estimate of obesity and calculated as kg/m2.
Statistical Analysis
Comparisons of men and women, and of those with and without DISH, were performed with t-tests for continuous variables and chi-square analysis for categorical variables. Age- and sex-adjusted logistic regression analyses were performed to calculate the odds of self-reported difficulty in bending, walking, or climbing, and inability to perform the chair stand test without the use of arms by presence of DISH. For measured hand grip strength, multivariable linear regression was used to assess the association with DISH. Variables were examined as possible confounders using chi-square analyses for categorical variables and t-tests for continuous variables to test for differences by DISH and by poor physical function; variables with differences at p<0.10 were added to multivariable models and backward selection techniques (p< 0.10) were used to improve model fit. Because of observed sex differences, a sex by DISH interaction was added to these models. We performed sensitivity analyses with BMD (total hip and spine), and back pain included in the models to determine whether they had an effect on the associations, and to assess bias from missing data. Sex specific models were run examining the associations between DISH and poor physical function separately within men and women. SAS 9.4 software was used for all analyses (SAS Institute, Cary, NC).
Results
Characteristics of the sample overall, as well as sex specific means and proportions for men and women on selected characteristics, are shown in Table 1. The mean age of the overall cohort was 71.5 (SD=10.8) years; women comprised 61% of the sample. DISH was approximately five times more prevalent in men (25.6%) than women (5.5%). Men had approximately 5 degrees lower Cobb angle of kyphosis, weighed more and had higher BMI than women. A greater proportion of men reported having diabetes, whereas a greater proportion of women reported arthritis, less frequent exercise, and had lower measured hip BMD (Table 1).
Table 1. Characteristics of study participants.
| Characteristics | All (N = 1395 to 1591)a | Women (N = 850 to 961)a | Men (N = 545 to 630)a | P value |
|---|---|---|---|---|
| DISH (%)b | 13.5 | 5.5 | 25.6 | < 0.001 |
| Age (years) | 71.5 ± 10.8 | 71.7 ± 11.0 | 71.2 ± 10.5 | 0.35 |
| Cobb angle (degrees) | 46.5 ± 15.3 | 48.5 ± 16.2 | 43.4 ± 15.3 | < 0.001 |
| BMI (kg/m2)c | 25.3 ± 3.9 | 24.7 ± 4.1 | 26.3 ± 3.5 | < 0.001 |
| Weight (pounds) | 154.3 ± 32.0 | 139.7 ± 25.9 | 176.6 ± 27.3 | < 0.001 |
| Hip BMD | 0.86 ± 0.17 | 0.80 ± 0.14 | 0.96 ± 0.15 | < 0.001 |
| Stroke (%) | 3.0 | 2.5 | 3.7 | 0.18 |
| Diabetes (%) | 5.9 | 4.8 | 7.7 | 0.02 |
| Arthritis (%) | 20.1 | 23.5 | 14.8 | < 0.001 |
| Exercise (≥ 3 times/week) (%) | 70.8 | 68.1 | 75.0 | 0.003 |
| Current smoker (%) | 6.7 | 7.3 | 5.7 | 0.22 |
Sample size varied due to missing data for some covariates
the denominator used to estimate DISH prevalence was 1,591
kg/m2 = kilograms/meter2, kg=kilograms
Compared to those unaffected, those with DISH reported more diabetes and stroke. (Table 2). They were also slightly older, had significantly higher BMI, hip BMD, and weight. A significantly larger proportion of participants with DISH compared to those without DISH reported difficulty bending, and had difficulty with the chair stand test although they had higher grip strength. In women only, those with DISH reported more health limitations and a lower proportion reported exercise three or more times per week (data not shown).
Table 2. Selected characteristics among those with DISH compared to no DISH.
| Characteristics | No DISH (N = 1199 to 1377)a | DISH (N = 196 to 214)a | P-value |
|---|---|---|---|
| Age (years) | 70.7 ± 10.9 | 71.2 ± 10.5 | < 0.0001 |
| Men (%) | 34.1 | 75.2 | < 0.0001 |
| Cobb angle (degrees) | 46.3 ± 15.3 | 47.9 ± 15.6 | 0.17 |
| BMI (kg/m2)b | 25.2 ± 3.9 | 26.4 ± 3.9 | < 0.0001 |
| Weight (pounds) | 151.9 ± 32.4 | 169.7 ± 31.4 | < 0.0001 |
| Hip BMD | 0.86 ± 0.16 | 0.92 ± 0.18 | < 0.0001 |
| Stroke (%) | 2.6 | 5.2 | 0.04 |
| Diabetes (%) | 5.0 | 11.8 | 0.0001 |
| Arthritis (%) | 19.8 | 22.2 | 0.41 |
| Exercise (≥ 3 times/week) (%) | 71.3 | 67.9 | 0.32 |
| Current smoker (%) | 7.2 | 3.3 | 0.003 |
| Bending (% with difficulty) | 9.8 | 19.8 | < 0.0001 |
| Walking (% with difficulty) | 13.7 | 17.0 | 0.21 |
| Climbing (% with difficulty) | 19.2 | 20.4 | 0.69 |
| Chair stand (% with difficulty) | 7.9 | 12.2 | 0.04 |
| Grip Strength (kg) | 19.9 | 17.9 | < 0.001 |
Sample size varied due to missing data for some covariates
Kg/m2 = kilograms/meter2, kg=kilograms
The odds ratio was estimated from logistic regression models after controlling for age and sex (Table 3), and DISH was associated with a 1.72-fold increased odds of self-reported difficulty bending (95% CI: 1.13, 2.62). There were no associations between DISH and the other self-reported physical function measures of walking or climbing or the measured ability to complete 5 chair stands without the use of the arms after adjustment for age and sex. After additional adjustment for Cobb angle, weight, stroke, arthritis, and exercise, DISH remained significantly associated with increased odds of self-reported difficulty in bending, OR=1.69, (95% CI: 1.07, 2.66). DISH was not associated with measured grip strength after adjusting for age and sex (model 1, β estimate: -0.65 kg, p = 0.14), but in fully adjusted multivariable models lower grip strength was significantly associated with DISH (model 2, β estimate: -1.08 kg, p=0.01). We performed sensitivity analyses using total hip and spine BMD in the models, as well as using a restricted sample with no missing data for all physical functional outcomes (n = 1554), and our results did not appreciably change.
Table 3. Adjusted associations of DISH with measures of poor physical function.
| Physical Function Measure | Odds Ratio | 95% CI | p-value |
|---|---|---|---|
| Bending | |||
| Model 1a (n = 1583) | 1.72 | 1.13, 2.62 | 0.01 |
| Model 2b (n = 1386) | 1.69 | 1.07, 2.66 | 0.02 |
| Walking | |||
| Model 1a (n = 1575) | 1.06 | 0.69, 1.63 | 0.79 |
| Model 2b (n = 1378) | 0.96 | 0.60, 1.52 | 0.85 |
| Climbing | |||
| Model 1a (n = 1569) | 1.02 | 0.68, 1.52 | 0.92 |
| Model 2b (n = 1376) | 0.91 | 0.59, 1.41 | 0.68 |
| Chair Stand | |||
| Model 1a (n = 1589) | 1.33 | 0.79, 2.22 | 0.28 |
| Model 2b (n = 1385) | 1.34 | 0.78, 2.31 | 0.29 |
|
| |||
| Beta Coefficient | 95% CI | p-value | |
|
| |||
| Grip strength (kg) | |||
| Model 1a (n = 1589) | -0.65 | -1.51, 0.20 | 0.14 |
| Model 2b (n = 1385) | -1.08 | -1.92, -0.25 | 0.01 |
Model 1 - adjusted for age and sex
Model 2 - adjusted for age, sex, weight, stroke, arthritis, exercise (≥ 3 times/week), and Cobb angle.
Given the sex differences in the prevalence of DISH, we tested for effect modification and found significant interactions of DISH and sex for stair climbing (p = 0.02), chair stand (p = 0.08), and grip strength (p = 0.10) (Table 4). Therefore, analyses were repeated after stratification by sex (Table 4). Among men only, those with DISH were 2.17-times (95% CI: 0.1.04, 4.52) more likely to be unable to perform the chair stand test without using their arms (p=0.04) after adjustment for age, Cobb angle, weight, stroke, arthritis and exercise (Table 4). However, there were no significant associations with DISH for any of the other physical function measures in men and there were no significant associations of DISH with any of the physical function measures in women.
Table 4. Sex-stratified associations of DISH with poor physical function and gripa.
| Physical Function Measure | Odds Ratio | 95% CI | p-value | p-value for interactionb |
|---|---|---|---|---|
| Bending | 0.56 | |||
| Female | 1.58 | 0.74, 3.39 | 0.24 | |
| Male | 1.74 | 0.96, 3.14 | 0.07 | |
| Walking | 0.48 | |||
| Female | 0.82 | 0.38, 1.77 | 0.62 | |
| Male | 1.02 | 0.55, 1.90 | 0.94 | |
| Climbing | 0.02 | |||
| Female | 0.49 | 0.23, 1.05 | 0.07 | |
| Male | 1.29 | 0.73, 2.26 | 0.38 | |
| Chair Stand | 0.08 | |||
| Female | 0.71 | 0.28, 1.81 | 0.48 | |
| Male | 2.17 | 1.04, 4.52 | 0.04 | |
|
| ||||
| Beta Coefficient | 95% CI | p-value | p-value for interaction | |
|
| ||||
| Grip strength (kg) | 0.10 | |||
| Female | -0.40 | -1.63, 0.84 | 0.53 | |
| Male | -0.84 | -2.06, 0.37 | 0.17 | |
Adjusted for age, weight, stroke, arthritis, exercise (≥3 times/week) and Cobb angle
Interaction between DISH and sex
Discussion
In this cohort of community-dwelling older adults, we found DISH in approximately 25% of the men and 5% of the women, consistent with some but not all previous findings.1,2,4 DISH was associated with impairment of both objective (lower grip strength) and self-reported measures of physical function (ability to bend) in both men and women, and men with DISH had significantly more difficulty completing the chair stand test without using their arms than those without DISH.
These findings are in accord with those of a previous study that described self-reported physical and spinal disability among those with DISH.6 In contrast to that study, our results are independent of variables known to impact physical function such as weight, stroke, arthritis and exercise, and adjustment for them did not alter our results. Furthermore, to our knowledge, this is the first study that has reported associations of DISH with objective measures of physical function such as grip strength and chair stand.
The significant interactions of DISH and sex for the chair stand test, stair climbing and grip strength suggest that DISH may have different clinical implications for men and women. While the results were not significant in the sex-stratified analyses for stair-climbing and grip, sex did affect the ability to perform the chair stand test among men with DISH. In this study, more women than men had arthritis and exercised less than three times per week, both factors that can influence the ability to perform the chair stand test. It is possible that adding DISH to the equation did not confer any additional effect in women because they were already compromised by arthritis and poorer physical conditioning. We also cannot exclude the possibility that the low prevalence of DISH in this sample of women made effects too small to detect.
The results of this study suggest that DISH should be considered as a predictor of poor physical function. Grip strength is an indicator of general body strength and has been shown to predict falls in epidemiological studies of older men and women.13 Grip strength in midlife has also been reported to predict walking disability and self-care disability 25 years later.14 Moreover, the chair stand test is a reliable and valid measure that reflects an older person's lower extremity function,15 and is often used as a fall screening tool. Taken together, the physical function impairments that we found associated with DISH may increase their risk of falls, a possibility that warrants further study.
Several limitations and strengths of this study were considered. First, this older cohort was predominantly white, well-educated, and middle class; thus, results may not be generalizable to older adults with lower socio-economic status who are at increased risk for comorbidities. However, this homogeneity means that results are not confounded by differences in these factors or a lack of access to care. Second, the chair stand test was recorded as a categorical instead of continuous variable (i.e. time needed to complete 5 chair stands), and might not have been sensitive enough to detect differences between those with and without DISH in women; this could have affected our results in men as well. Third, we considered including BMD and back pain as potential covariates because they are known to affect physical function, however, they did not meet criteria during model selection. Furthermore, sensitivity analyses that included BMD and back pain showed that their presence in the models made no difference on the estimates. Fourth, while we might expect that poor physical function would increase with greater spinal involvement of DISH, we were unable to investigate this because our DISH data were categorical (yes/no), the films were never digitized and were no longer available for viewing. Fifth, our sample varied depending upon the variables included due to missing data. We did not want to restrict the sample in our analyses because we would have had to create a restricted sample of 1,554 due to missing data in any one of the 5 physical function outcomes. We did determine that there were no differences in the baseline characteristics in the restricted sample compared to the total sample of 1,591 and concluded that we did not introduce bias. This study has a number of strengths including the fact that this sample was from a large community-based cohort of older men and women, and there was a sufficiently large number of men and women to allow an investigation of sex interactions.
In conclusion, we found that DISH was common in this community-dwelling sample of older adults, affecting approximately 25% of the men. Results of this cross-sectional study show that older persons affected by DISH exhibit worse self-reported and objectively measured physical function, including self-reported difficulty bending and lower grip strength, and that older men with DISH had more difficulty rising from a chair. Given that DISH so commonly affects older men, prospective studies are warranted to further investigate the causes and clinical sequelae of DISH, and to determine how DISH affects physical function over time.
Acknowledgments
Funding sources: NIH AG007181-15, DK31801, and AR06828. Other grants supporting the researchers are P50 AR063043, RO1 AG041921, U01 AR45580, U01 AR45614, U01 AR45632, U01 AR45647, U01 AR45654, U01 AR45583, U01 AG18197, U01-AG027810, and UL1 RR024140.
Sponsor's Role: Indicate sponsor's role in the design, methods, subject recruitment, data collections, analysis and preparation of paper. If there is no sponsor, indicate “none”. None
Footnotes
Author Contributions: Indicate authors' role in study concept and design, acquisition of subjects and/or data, analysis and interpretation of data, and preparation of manuscript.
Katzman role: analysis and interpretation of data, preparation of manuscript, edited and approved final version of manuscript
Kado role: conceived of study question, designed analyses, interpreted data, edited and approved final version
Huang role: designed analyses, performed analyses, interpreted data, helped draft manuscript, edited and approved final version of manuscript
Silverstein role: acquisition of data, edited and approved final version of manuscript
Barrett-Connor role: obtained funding, interpreted data, edited and approved final version of manuscript
References
- 1.Yamada K, Toyoda H, Terai H, Takahashi S, Nakamura H. Spinopelvic alignment of diffuse idiopathic skeletal hyperostosis in lumbar spinal stenosis. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2014;23(6):1302–1308. doi: 10.1007/s00586-013-3154-1. [DOI] [PubMed] [Google Scholar]
- 2.Holton KF, Denard PJ, Yoo JU, et al. Diffuse idiopathic skeletal hyperostosis and its relation to back pain among older men: the MrOS Study. Seminars in arthritis and rheumatism. 2011;41(2):131–138. doi: 10.1016/j.semarthrit.2011.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Katzman WB, Parimi N, Mansoori Z, et al. Cross-sectional and Longitudinal Associations of Diffuse Idiopathic Skeletal Hyperostosis (DISH) and Thoracic Kyphosis in Older Men and Women. Arthritis care & research. 2016 doi: 10.1002/acr.23115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mader R. Diffuse idiopathic skeletal hyperostosis: a distinct clinical entity. The Israel Medical Association journal : IMAJ. 2003;5(7):506–508. [PubMed] [Google Scholar]
- 5.Bundrick TJ, Cook DE, Resnik CS. Heterotopic bone formation in patients with DISH following total hip replacement. Radiology. 1985;155(3):595–597. doi: 10.1148/radiology.155.3.3923552. [DOI] [PubMed] [Google Scholar]
- 6.Mata S, Fortin PR, Fitzcharles MA, et al. A controlled study of diffuse idiopathic skeletal hyperostosis. Clinical features and functional status. Medicine (Baltimore) 1997;76(2):104–117. doi: 10.1097/00005792-199703000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Mader R. Current therapeutic options in the management of diffuse idiopathic skeletal hyperostosis. Expert opinion on pharmacotherapy. 2005;6(8):1313–1318. doi: 10.1517/14656566.6.8.1313. [DOI] [PubMed] [Google Scholar]
- 8.Schlapbach P, Beyeler C, Gerber NJ, et al. Diffuse idiopathic skeletal hyperostosis (DISH) of the spine: a cause of back pain? A controlled study. British journal of rheumatology. 1989;28(4):299–303. doi: 10.1093/rheumatology/28.4.299. [DOI] [PubMed] [Google Scholar]
- 9.Birnbaum K, Siebert CH, Hinkelmann J, Prescher A, Niethard FU. Correction of kyphotic deformity before and after transection of the anterior longitudinal ligament--a cadaver study. Arch Orthop Trauma Surg. 2001;121(3):142–147. doi: 10.1007/s004020000193. [DOI] [PubMed] [Google Scholar]
- 10.Resnick D, Shapiro RF, Wiesner KB, Niwayama G, Utsinger PD, Shaul SR. Diffuse idiopathic skeletal hyperostosis (DISH) [ankylosing hyperostosis of Forestier and Rotes-Querol] Seminars in arthritis and rheumatism. 1978;7(3):153–187. doi: 10.1016/0049-0172(78)90036-7. [DOI] [PubMed] [Google Scholar]
- 11.Nardo L, Lane NE, Parimi N, et al. Diffuse Idiopathic Skeletal Hyperostosis Association With Thoracic Spine Kyphosis: A Cross-sectional Study for the Health Aging and Body Composition Study. Spine (Phila Pa 1976) 2014;39(24):E1418–1424. doi: 10.1097/BRS.0000000000000615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rossiter-Fornoff JE, Wolf SL, Wolfson LI, Buchner DM. A cross-sectional validation study of the FICSIT common data base static balance measures. Frailty and Injuries: Cooperative Studies of Intervention Techniques. J Gerontol A Biol Sci Med Sci. 1995;50(6):M291–297. doi: 10.1093/gerona/50a.6.m291. [DOI] [PubMed] [Google Scholar]
- 13.Pluijm SM, Smit JH, Tromp EA, et al. A risk profile for identifying community-dwelling elderly with a high risk of recurrent falling: results of a 3-year prospective study. Osteoporos Int. 2006;17(3):417–425. doi: 10.1007/s00198-005-0002-0. [DOI] [PubMed] [Google Scholar]
- 14.Rantanen T, Guralnik JM, Foley D, et al. Midlife hand grip strength as a predictor of old age disability. JAMA. 1999;281(6):558–560. doi: 10.1001/jama.281.6.558. [DOI] [PubMed] [Google Scholar]
- 15.Jones CJ, Rikli RE, Beam WC. A 30-s chair-stand test as a measure of lower body strength in community-residing older adults. Res Q Exerc Sport. 1999;70(2):113–119. doi: 10.1080/02701367.1999.10608028. [DOI] [PubMed] [Google Scholar]