Abstract
Objective
To examine the association between life-space mobility and cognitive decline over a 5-year period among older Mexican Americans.
Design
Longitudinal study.
Setting
Hispanic Established Population for the Epidemiologic Study of the Elderly survey conducted in the southwestern of United States (Texas, Colorado, Arizona, New Mexico, and California).
Participants
Four hundred thirty-two Mexican Americans aged 75 and older with normal or high cognitive function at baseline.
Measurement
Socio-demographic factors, living arrangement, type of household, social support, financial strain, self-reported medical conditions, Mini-Mental State Examination (MMSE), depressive symptoms, activities of daily living (ADLs), and Short Physical Performance Battery. Life-space assessment (LSA) during the past 4 weeks was assessed during in-home interview. Scores ranged from 0 (daily restriction to the bedroom) to 120 (daily trips outside of their own town without assistance) and categorized as 0-20, 21-40, 41-60, 61-80, and 81-120. Because of the small sample size in the category of 81 to 120, the two highest categories were combined into a single group.
Results
The mean LSA score and MMSE score of participants at baseline was 44.6 [(Standard Deviation (SD), 20.7] and 25.7 (SD, 3.2), respectively. Mixed Model analyses showed that participants in the highest life-space category (≥ 61) experienced slower rates of cognitive decline over time compared to participants in the lowest category (0 to 20) [β = 1.03, Standard Error (SE) = 0.29, p=0.0004], after adjusting for all covariates.
Conclusion
Greater life-space mobility at baseline was predictor of slower rates of cognitive decline over 5-years in older Mexican Americans.
Keywords: Mobility, Life-Space, Cognition, Older Adults, Mexican Americans
Introduction
The rapid growth of the aging population globally has fueled the increased incidence of cognitive impairment, with more than 16 million people in the United States living with cognitive impairment 1, 2. Cognitive impairment in older adults, ranging from mild impairment to severe dementia, is a major contributor to the high incidence of institutionalization, caregiver burden, premature death, and high health care costs in this growing population 1.
Mobility directly influences the individual access to resources of daily needs, participation in social, cultural, recreational, and physical activities as well as the ability to live independently in the community 3. The maintenance of social networks and community participation have shown a protective effect on cognitive function in older adults 4, 5. For example, Crooks and colleagues found that larger social networks were associated with lower risk of dementia over 4-years of follow-up 4. Krueger and colleagues found that higher level of perceived social support and more frequent participation in social activities were associated with higher level of cognitive function in older adults without clinical signs of dementia 5.
Life-space mobility measured by a multidimensional self-reported instrument, refers to a person's ability to move in their environment within a specific time period (e.g., within a day, week or month), has been found to be associated with physical performance, disability, falls, fractures, physical activity, quality of life, and mortality 6-10. Several studies have examined the effect of life-space mobility and cognitive function in Non-Hispanic Whites and African Americans 11-13. For example, Crowe and colleagues found that greater life-space mobility was associated with reduced cognitive decline over 4-years of follow-up 11. James and colleagues found that constricted life-space was associated with increased risk of Alzheimer disease, mild cognitive impairment, and cognitive decline among older adults without dementia at baseline in a period of 8-years of follow-up12. Sartori and colleagues found a positive relationship between cognitive function and life-space, with memory, reasoning, and processing speed domains being strong independent predictors of life-space mobility 13.
The Hispanic population is known to have a higher prevalence of cognitive impairment than non-Hispanic whites and are about one and one-half times as likely to have Alzheimer's and other dementias as older whites 1. The objective of our study was to examine the relationship between life-space mobility assessment and cognitive decline among older Mexican Americans aged 75 years and older with normal or high cognition at baseline over a 5-year period. We studied life-space mobility and cognitive function in this population because: 1) resources and commodities to achieve high life-space mobility may be compromised by low educational attainments, limited disposable incomes, access to optimal transportation, residence in high stress neighborhoods, and language barriers 14-16; and 2) the high prevalence of factors associated with cognitive decline such as diabetes, stroke, hypertension, depression, and lower performance in physical function 17-20.
Methods
Sample and Procedures
Participants were from the Hispanic Established Population for the Epidemiologic Study of the Elderly (H-EPESE), an ongoing longitudinal study of Mexican Americans aged 65 and older residing in Texas, New Mexico, Colorado, Arizona, and California. The sampling plan and cohort characteristics have been described previously 15. Information and data for the H-EPESE are available at the National Archive of Computerized Data on Aging 21. The original H-EPESE sample consisted of 3,050 participants interviewed in 1993/94 at baseline and followed-up every two or three years. In 2005/06 a subsample aged 75 and older (n = 1,013) from the 2004/05 H-EPESE cohort was randomly selected to study frailty, and three follow-ups were conducted. The present study used data obtained from three waves of the frailty study (2008/09, 2010/11, and 2012/13) 6. Information from the first wave of the frailty study was not used because the Life-Space Assessment (LSA) was not administered. Data on LSA was introduced in 2008/09 to examine the mobility and community engagement of older Mexican American adults 6.
Of the 1,013 participants interviewed in the frailty study at first wave (2005-2006), 731 were interviewed in 2008/09 using LSA questionnaire. Of the 731 participants, we excluded 225 participants with a Mini-Mental State Examination (MMSE) less than 21 because we were interested in examining how life-space mobility influenced changes in cognitive function in individuals with normal or high cognition at baseline. Of the 506 with MMSE ≥ 21, 72 were excluded because of incomplete information on LSA and covariates. The final cohort included 432 participants aged 75 and older who had MMSE ≥ 21 and complete information on life space, MMSE, and all covariates in 2008/09 (hereafter referred to as baseline). At the end of follow-up (2012/13), 243 were re-interviewed, 123 were confirmed deceased through the National Death Index and reports from relatives, and 66 were lost to follow-up. Participants excluded were significantly more likely to be older, to have less education, to have more children living in the household, to report more financial strain, to report more depressive symptoms, ADL disability, and lower life-space mobility. Participants were interviewed and examined in their homes by interviewers employed by Nielsen Research Company (formerly Harris Interactive) and trained by H-EPESE investigators. The interviews were conducted in Spanish or English, depending on the respondent's preference. The study received approval from the university's institutional review board.
Measures
Independent variable
Life-space mobility was assessed with the Life-Space Assessment (LSA) questionnaire 22, 23 that assesses mobility during the month before the interview and involves a single interview instead of a record of activities in a diary. Participants were asked: “During the past 4 weeks have you: (1) been to other rooms in your home besides the room where you sleep (level 1); (2) been to an area outside of your home, such as your porch, deck or patio, hallway of an apartment building, or garage (level 2); (3) been to places in your neighborhood other than your own yard or apartment building (level 3); (4) been to places outside your neighborhood, but within your town (level 4); and (5) been to places outside your own town (level 5).” For each life-space level, participants were asked how often within the week (less than once a week, 1-3 times each week, 4-6 times each week, daily) they attained that level, and if they needed help from assistive devices or another person (“yes” vs. “no”) to move to that level. A composite score was calculated on the basis of life-space level, the frequency of attaining each level, and the degree of independence in achieving each level. The composite scores ranged from 0 to 120, with higher scores representing greater mobility. LSA mobility was analyzed as a continuous score and as a categorical variable using 20-point intervals for descriptive purposes as follows: category I (0 to 20, n=52), category II (21 to 40, n=149), category III (41 to 60, n=133), category IV (61 to 80, n=78) and category V (81 to 120, n=20). Because of the small sample size in the category of 81 to 120, the two highest categories were combined into a single group (category IV) 9, 22, 24-26.
Covariates
Baseline socio-demographic variables included age, sex, marital status (married vs. unmarried), and education. Living arrangement was assessed by asking how many people live in the household with the participant. Social support was assessed by two questions: 1) “In times of trouble, can you count on at least some of your family or friends most of the time, some of the time, or hardly ever?” and 2) “Can you talk about your deepest problems with at least some of your family or friends most of the time, some of the time, or hardly ever?”. Financial strain was assessed by asking participants: “How much difficulty do you have in meeting monthly payments on your bills – a great deal, some, a little, or none?”. Self-reported medical conditions included hypertension, diabetes mellitus, cancer, heart attack, stroke, and hip fracture. Falls were assessed by asking participants how many times they had fallen and landed on the floor or ground during the past 12 months. Depressive symptomatology was measured using the Center for Epidemiologic Study-Depression Scale (CES-D) 27. Disability was assessed by self-report, using 7 items from a modified version of the Katz Activities of Daily Living (ADL) scale (walking, bathing, grooming dressing, eating, transferring, and toileting) 28. ADL disability was dichotomized as no help needed versus needed help or unable to perform one or more of the 7 ADL activities. Physical function was measured with the Short Physical Performance Battery (SPPB), which includes three lower body extremity tests (standing balance, walking speed, and repeated chair-stands)29. Each test was scored from 0 to 4, with 0 reflecting the inability to complete the test and 1-4 reflecting quartiles relating to task completion (higher score indicating higher performance). The combined scores ranged from a low of 0 to a high of 12, with higher scores indicating better physical functioning. Type of household was assessed by interviewer observation as living in the community (more specifically, a single house, a multi-family house, or an apartment), and living in a facility (which included assisted living, congregate housing, and group quarters).
Outcome
Cognitive function was assessed using the 30-item Mini-Mental State Examination (MMSE) 30. The English and Spanish versions of the MMSE were adapted from the Diagnostic Interview Scale and have been used in prior community surveys 31. Similar to previous studies in populations with low educational attainment and low English literacy, only participants with MMSE scores of 21 or higher (normal or good cognition) at baseline were included in the analyses 32-35.
Statistical Analysis
Chi-square, Fisher exact, analysis of variance, and post hoc Tukey's tests were used to examine the distribution of covariates for participants by life-space category at baseline. General linear mixed models using the MIXED procedure were used to estimate change in cognitive function (MMSE score) over a 5-year period as a function of LSA 36. All variables were analyzed as time-dependent covariates (with the potential to change as time progresses) except age, gender, education, and the LSA. Two mixed models were constructed to test the relationship between life-space mobility and change in cognitive function (total MMSE score) over a 5-year period. Model 1, included time, age, gender, marital status, education, LSA categories (Category 1 was the reference), and the interaction between LSA categories and time. In Model 2, living arrangement, type of household, social support, financial strain, medical conditions (hypertension, diabetes, cancer, heart attack, stroke, and hip fracture), falls, depressive symptoms, SPPB, and ADL disability were added to the variables in Model 1. LSA was analyzed both as a categorical and a continuous variable. All analyses were performed using the SAS System for Windows, version 9.4 (SAS Institute, Inc., Cary, NC).
Results
The mean age of the 432 participants was 83.8 ± 3.9 years at baseline (2008-2009). Sixty-six percent were female and 36% were married. The mean years of education was 5.8± 4.0, the mean LSA score was 44.6 ± 20.7, and the mean MMSE score was 25.7 ± 3.2. Ninety-four percent lived in the community, 28% reported ADL disability and 16.7% reported high depressive symptoms. The most common medical conditions were hypertension (73.8%) and diabetes (30.1%). Table 1 presents the baseline descriptive characteristics of the sample by LSA category. Mean LSA scores were 13.1 ± 5.2 for those in Category I, 31.6 ± 5.9 for Category II, 49.9 ± 5.6 for Category III, and 73.9 ± 9.4 for Category 4. Participants in Category IV were significantly more likely to be younger, to be male, married, to report fewer depressive symptoms, to report less ADL disability, to report fewer falls, and to have fewer medical comorbidities (including stroke and hip fracture). Those in Category IV have higher SPPB scores compared with those in Category I or II, and those in Category IV have higher MMSE scores compared with those in Category I.
Table 1. Baseline characteristics of the sample by life-space assessment (LSA) category, N=432.
| Variables | Category I (0 to 20) N (%) | Category II (21 to 40) N (%) | Category III (41 to 60) N (%) | Category IV (≥ 61) N (%) | P-Value |
|---|---|---|---|---|---|
| Total | 52 (12.0) | 149 (34.5) | 133 (30.8) | 98 (22.7) | |
| LSA-continuous score, mean ± SD | 13.1 ± 5.2 | 31.6 ± 5.9 | 49.9 ± 5.6 | 73.9 ± 9.4 | < .0001 |
| Age (years), mean ± SD | 83.9 ± 4.6 | 84.8 ± 4.3 | 83.4 ± 3.8 | 82.7 ± 2.9 | 0.0004 |
| Gender (female) | 49 (94.2) | 106 (71.1) | 84 (63.2) | 47 (47.9) | < .0001 |
| Marital status (married) | 14 (26.9) | 52 (34.9) | 41 (30.8) | 49 (50.0) | 0.0081 |
| Education (years), mean ± SD | 5.1 ± 3.7 | 5.7 ± 4. | 6.0 ± 3.9 | 6.0 ± 4.2 | 0.5194 |
| Financial strain (great/some) | 33 (63.5) | 77 (52.0) | 69 (52.3) | 57 (58.2) | 0.4199 |
| Type of Housing (Community) | 47 (90.4) | 140 (93.9) | 127 (95.5) | 91 (92.9) | 0.6072 |
| Number of children living, mean ± SD | 2.0 ± 0.9 | 2.2 ± 1.4 | 2.0 ± 1.2 | 2.1 ± 1.2 | 0.4567 |
| Have someone to count on about problems | 38 (73.1) | 117 (78.5) | 102 (76.7) | 81 (82.7) | 0.5460 |
| Have someone to talk to about problems | 34 (65.4) | 98 (65.8) | 88 (66.2) | 65 (66.3) | 0.9993 |
| Hypertension | 45 (86.5) | 107 (71.8) | 98 (73.7) | 67 (68.4) | 0.1086 |
| Diabetes | 20 (38.5) | 44 (29.5) | 33 (24.8) | 33 (37.7) | 0.2494 |
| Cancer | 0 (0) | 3 (2.0) | 9 (6.8) | 2 (2.0) | 0.0656 |
| Heart Attack | 2 (3.9) | 3 (2.0) | 3 (2.3) | 1 (1.0) | 0.6980 |
| Stroke | 4 (7.7) | 3 (2.0) | 1 (0.8) | 0 (0) | 0.0117 |
| Hip Fracture | 3 (5.8) | 2 (1.4) | 0 (0) | 0 (0) | 0.0093 |
| Depression (CES-D) | 21 (40.4) | 28 (18.8) | 17 (12.8) | 6 (6.1) | < .0001 |
| Falls | 25 (48.1) | 46 (30.9) | 36 (27.1) | 14 (14.3) | 0.0002 |
| ADL Disability | 43 (82.7) | 55 (36.9) | 17 (12.8) | 4 (4.1) | < .0001 |
| SPPB, mean ± SD | 1.9 ± 2.4 | 5.1 ± 3.2 | 6.9 ± 2.8 | 7.7 ± 2.7 | < .0001 |
| Total MMSE, mean ± SD | 24.6 ± 3.2 | 25.7 ± 3.2 | 25.9 ± 3.1 | 26.1 ± 3.2 | 0.0515 |
Values are presented as mean ± standard deviation (SD) or N (%). CES-D = Center for Epidemiologic Studies Depression Scale; SPPB=Short Physical Performance Battery; ADL= Activities of Daily Living.
Table 2 displays the general linear mixed model estimates for total MMSE score as a function of LSA over the 5-year period. The adjusted rate of decline for total MMSE was 1.48 per year. The association between LSA category and MMSE score at baseline (intercept of total MMSE score) after adjusting for age, gender, marital status, education, and time (Model 1) was statistically significant for LSA Category III [(Estimate = 1.09, Standard Error (SE) = 0.49] and LSA Category IV (Estimate = 1.27, SE = 0.53) when compared with LSA Category I (lowest LSA). The interaction term between LSA categories and time of follow-up (slope of total MMSE score over 5-years) was statistically significant for LSA Category II (Estimate = 0.59, SE = 0.29), Category III (Estimate = 0.65, SE = 0.29), and Category IV (Estimate = 1.01, SE = 0.30). After adjusting for all covariates (Model 2) the associations between LSA Categories (II, III, and IV) and MMSE remained statistically significant. Other factors that were significantly associated with slower rates of decline in MMSE scores over time were being female (Estimate = 0.68, SE = 0.33), high level of education (Estimate = 0.25, SE = 0.04), and higher scores on the SPPB (Estimate = 0.10, SE = 0.04).
Table 2. General linear mixed models estimates for Total Mini Mental State Examination (MMSE) score as a function of baseline life-space assessment (LSA) over a 5-year period, N=432.
| Predictor variables | Model 1 Estimate (SE) | p-value | Model 2 Estimate (SE) | p-value |
|---|---|---|---|---|
| LSA category | ||||
| Intercept | 23.91 (3.19) | < .0001 | 25.87 (3.35) | < .0001 |
| Time | -1.48 (0.26) | < .0001 | -1.36 (0.25) | < .0001 |
| Main effect | ||||
| I (0 to 20) | Reference | Reference | ||
| II (21 to 40) | 0.99 (0.49) | .0422 | 0.37 (0.52) | .4824 |
| III (41 to 60) | 1.09 (0.50) | .0295 | -0.04 (0.56) | .9427 |
| IV (≥61) | 1.27 (0.53) | .0181 | -0.14 (0.61) | .8202 |
| Interaction with time | ||||
| I (0 to 20)*Time | Reference | Reference | ||
| II (21 to40)*Time | 0.59 (0.29) | .0436 | 0.56 (0.28) | .0471 |
| III (41 to 60)* Time | 0.65 (0.29) | .0236 | 0.85 (0.28) | .0026 |
| IV (≥61) * Time | 1.01 (0.30) | .0007 | 1.03 (0.29) | .0004 |
| LSA (continuous score) | ||||
| Intercept | 23.49 (3.22) | < .0001 | 25.81 (3.38) | < .0001 |
| Time | -1.44 (0.20) | < .0001 | -1.26 (0.19) | < .0001 |
| LSA - Main effect | 0.01 (0.01) | .0468 | -0.01 (0.01) | .4163 |
| LSA interaction with time | 0.01 (0.004) | .0005 | 0.01 (0.003) | .0002 |
Model 1: Adjusted for time, age, gender, marital status, education
Model 2: Adjusted for type of housing, living arrangement, social support, financial strain, medical conditions, depressive symptoms, activities of daily living, and Short Physical Performance Battery along with variables in Model 1
When LSA was analyzed as a continuous variable (Table 2), the parameter estimates for total MMSE score at baseline after adjusting for all covariates (intercept of total MMSE score) was -0.007 (SE = 0.01. p-value = .4163) and for the interaction term between LSA score and time of follow-up (slope of total MMSE over 5 years) was 0.01 (SE = 0.004, p-value = .0002).
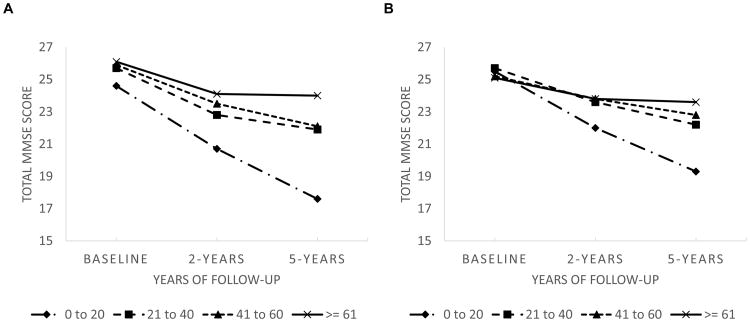
Figure 1 shows the unadjusted and adjusted mean distribution for total MMSE score over the 5-year period according to the LSA category at baseline. Participants in LSA Category I had a steeper decline in total MMSE score than those in higher LSA categories over the entire follow-up period.
Figure 1.
Unadjusted and adjusted means for total Mini-Mental-State-Examination (MMSE) score as a function of baseline life-space assessment (LSA) category over a 5-year follow-up period, N=432.
(A) Unadjusted
(B) Adjusted
Legend: 0-20 – LSA Category I
21-40 – LSA Category II
41-60 – LSA Category III
≥ 61 – LSA Category IV
Discussion
We examined the association between LSA mobility and cognitive function over time in older Mexican Americans aged 75 years and older with normal or high cognitive function at baseline. The rate of decline in the total MMSE score was 1.36 points per year over the 5-year period of follow-up after adjusting for all covariates. We found that the highest level of LSA at baseline (Category III and Category IV) was associated with a slower decline in MMSE scores over time.
The reasons why LSA is associated with cognitive function are not well understood. Studies have reported complex environments and leisure-time activities as protective factors against cognitive decline in later life 37, 38. Thus, keeping a person's life space large, such as leaving the home, attending religious services, and visiting family and friends may help provide the necessary stimulation to maintain cognitive skills. Moreover, because of its social dimension, life space has also been linked to social network size 39. Therefore, restricted life space mobility may decrease the social integration and engagement of individuals, both associated with a high risk of cognitive decline in older adults 40. Another important factor to take into account is the ability to drive in late life. Driving cessation which decreases life-space mobility accelerates cognitive decline over time 41.
Our findings are in line with previous studies conducted in African American and Caucasian older adults 11-13. Using data from a community-dwelling study of 624 African American and Caucasian older adults, Crowe and colleagues using the MMSE as a measure of cognitive function found that higher scores of LSA mobility were associated with decreased risk of cognitive decline 11. James and colleagues found that African American and Non-Hispanic white older adults with restricted life-space mobility were 1.6 times more likely to develop mild cognitive impairment (MCI) and 1.8 times more likely to develop Alzheimer disease than those with largest life-space 12. Examining the association between objective cognitive function and life-space in older adults with MMSE ≥ 23, Sartori and colleagues found that memory, reasoning, and processing speed composite tests were positively associated with larger life-space 13.
Our study has some limitations. First, measures of LSA were based on self-report. Mobility can be affected by various contextual factors including barriers in the environment (busy traffic, poor public transportation, safety) and facilitators in the environment (parks, sidewalks) within a neighborhood. Second, measures of environmental barriers were not collected in this study 39. Third, Information on season and weather were not included in this study, factors that may influence the life space mobility of older adults 42. Fourth, the use of the MMSE as measure for cognitive function underestimates mild cognitive impairment and cannot be used to diagnose dementia 30. However, the MMSE is the most frequently measure of cognitive screening used in aging research, and adaptations for those with low educational attainment and low English literacy has been made 31-33, 35. Fifth, is the possibility of reverse causation. It is possible that those participants who experienced cognitive impairment are more likely to have smaller life-space mobility than those who maintained normal or high cognition. However, we excluded those participants with MMSE < 21 at baseline. Additional analyses were conducted comparing those with MMSE < 21 and those with MMSE ≥ 21 and found that those with MMSE < 21 had smaller life-space at each follow-up when compared with those with MMSE ≥ 21 (37.4 vs 44.6, 31.9 vs 40.0 and 30.7 vs 41.1, respectively). Lastly, the participants in this study were from a subsample of the larger study and the results may not be generalizable to all older Mexican-Americans. Despite these few limitations, our study has several strengths. These include its large number of subjects 75 years and older from a well-defined, comprehensively studied sample from a minority community and under-served population, its prospective design, and the inclusion of a wide range of variables related to health and the social environment.
Conclusion
Constricted life-space may be an early marker of cognitive impairment. Our study findings highlight the importance of maintaining an optimal range of life-space and mobility in this population. Development and implementation of culturally appropriate interventions, targeting older Mexican Americans with high risk of cognitive decline and restricted life-space are needed to enhance mobility performance in daily life, and preserve and promote cognitive function.
Table 3. Conflict of Interest Disclosures.
| Elements of Financial/Personal Conflicts | *Author 1 SS | Author 2 AK | Author 3 MR | Author 4 KM | Author 5 KO | Author 6 SAS | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | |
| Employment or Affiliation | X | X | X | X | X | X | ||||||
| Grants/Funds | X | X | X | X | X | X | ||||||
| Honoraria | X | X | X | X | X | X | ||||||
| Speaker Forum | X | X | X | X | X | X | ||||||
| Consultant | X | X | X | X | X | X | ||||||
| Stocks | X | X | X | X | X | X | ||||||
| Royalties | X | X | X | X | X | X | ||||||
| Expert Testimony | X | X | X | X | X | X | ||||||
| Board Member | X | X | X | X | X | X | ||||||
| Patents | X | X | X | X | X | X | ||||||
| Personal Relationship | X | X | X | X | X | X | ||||||
Acknowledgments
This study was supported in part by grants R01-AG017638, R01-AG010939, R03 AG04640902, R01MD010355, and the UTMB Claude Pepper Center (P30-AG024832) from the National Institute of Aging. Seraina Silberschmidt was a Visiting Scholar in the Sealy Center on Aging. The content is solely the responsibility of the author(s) and does not represent the official views of this Institute or the National Institutes of Health. The authors acknowledge the assistance of Sarah Toombs Smith, PhD, ELS, in manuscript preparation.
Administrative, technical, or material support: Ottenbacher, Al Snih, and Markides.
Funding: Ottenbacher and Markides.
Study supervision: Al Snih.
Sponsor's Role: None.
Footnotes
Preliminary findings were presented at the annual meeting of the Gerontological Society of America (GSA), 2014.
Author Contributions: Data access: Kenneth J Ottenbacher, Kyriakos S Markides, and Soham Al Snih had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Seraina Silberschmidt and Soham Al Snih.
Acquisition, analysis, or interpretation of data: Seraina Silberschmidt and Soham Al Snih.
Drafting of manuscript: Seraina Silberschmidt, Amit Kumar, and Soham Al Snih.
Critical review: Seraina Silberschmidt, Amit Kumar, Kyriakos S Markides, Soham Al Snih, Mukaila A Raji, and Kenneth J Ottenbacher.
Statistical analysis: Seraina Silberschmidt and Soham Al Snih.
References
- 1.Alzheimer's Association. 2011 Alzheimer's Disease Facts and Figures. Alzheimer's & Dementia; Chicago, IL: 2011. [DOI] [PubMed] [Google Scholar]
- 2.U.S.Department of Health and Human Services Center for Disease Control and Prevention, editor. U.S.Department of Health and Human Services Center for Disease Control and Prevention. Cognitive impairment: a call for action, Now! 2011. [Google Scholar]
- 3.Rantanen T. Promoting mobility in older people. J Prev Med Public Health. 2013;46(1):S50–S54. doi: 10.3961/jpmph.2013.46.S.S50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Crooks VC, Lubben J, Petitti DB, Little D, Chiu V. Social network, cognitive function, and dementia incidence among elderly women. Am J Public Health. 2008;98:1221–1227. doi: 10.2105/AJPH.2007.115923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Krueger KR, Wilson RS, Kamenetsky JM, Barnes LL, Bienias JL, Bennett DA. Social engagement and cognitive function in old age. Exp Aging Res. 2009;35:45–60. doi: 10.1080/03610730802545028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Al Snih S, Peek KM, Sawyer P, Markides KS, Allman RM, Ottenbacher KJ. Life-space mobility in Mexican Americans aged 75 and older. J Am Geriatr Soc. 2012;60:532–537. doi: 10.1111/j.1532-5415.2011.03822.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bentley JP, Brown CJ, McGwin G, Jr, Sawyer P, Allman RM, Roth DL. Functional status, life-space mobility, and quality of life: a longitudinal mediation analysis. Qual Life Res. 2013;22:1621–1632. doi: 10.1007/s11136-012-0315-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lo AX, Brown CJ, Sawyer P, Kennedy RE, Allman RM. Life-space mobility declines associated with incident falls and fractures. J Am Geriatr Soc. 2014;62:919–923. doi: 10.1111/jgs.12787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mackey DC, Lui LY, Cawthon PM, Ensrud K, Yaffe K, Cummings SR. Life-Space Mobility and Mortality in Older Women: Prospective Results from the Study of Osteoporotic Fractures. J Am Geriatr Soc. 2016;64:2226–2234. doi: 10.1111/jgs.14474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tsai LT, Portegijs E, Rantakokko M, et al. The association between objectively measured physical activity and life-space mobility among older people. Scand J Med Sci Sports. 2015;25:e368–e373. doi: 10.1111/sms.12337. [DOI] [PubMed] [Google Scholar]
- 11.Crowe M, Andel R, Wadley VG, Okonkwo OC, Sawyer P, Allman RM. Life-space and cognitive decline in a community-based sample of African American and Caucasian older adults. J Gerontol A Biol Sci Med Sci. 2008;63:1241–1245. doi: 10.1093/gerona/63.11.1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.James BD, Boyle PA, Buchman AS, Barnes LL, Bennett DA. Life Space and Risk of Alzheimer Disease, Mild Cognitive Impairment, and Cognitive Decline in Old Age. Am J Geriatr Psychiatry. 2011;19:961–969. doi: 10.1097/JGP.0b013e318211c219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sartori AC, Wadley VG, Clay OJ, Parisi JM, Rebok GW, Crowe M. The relationship between cognitive function and life space: The potential role of personal control beliefs. Psychol Aging. 2011;27:364–3740. doi: 10.1037/a0025212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Eschbach K, Ostir GV, Patel KV, Markides KS, Goodwin JS. Neighborhood context and mortality among older Mexican Americans: is there a barrio advantage? American journal of public health. 2004;94:1807–1812. doi: 10.2105/ajph.94.10.1807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Markides KS, Black SA, S-B C, et al. The health of Mexican American elderly: selected findings from the Hispanic EPESE. In: Wykle ML, F A, editors. Serving Minority Elderly in the 21st Century. New York, NY: Springer Pub.; 1999. pp. 72–90. [Google Scholar]
- 16.Shell AM, Peek MK, Eschbach K. Neighborhood Hispanic composition and depressive symptoms among Mexican-descent residents of Texas City, Texas. Social science & medicine. 2013;99:56–63. doi: 10.1016/j.socscimed.2013.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Alfaro-Acha A, Al Snih S, Raji MA, Markides KS, Ottenbacher KJ. Does 8-foot walk time predict cognitive decline in older Mexicans Americans? J Am Geriatr Soc. 2007;55:245–251. doi: 10.1111/j.1532-5415.2007.01039.x. [DOI] [PubMed] [Google Scholar]
- 18.Downer B, Raji MA, Markides KS. Relationship between metabolic and vascular conditions and cognitive decline among older Mexican Americans. Int J Geriatr Psychiatry. 2016;31:213–221. doi: 10.1002/gps.4313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nguyen HT, Black SA, Ray LA, Espino DV, Markides KS. Predictors of decline in MMSE scores among older Mexican Americans. J Gerontol A Biol Sci Med Sci. 2002;57:M181–185. doi: 10.1093/gerona/57.3.m181. [DOI] [PubMed] [Google Scholar]
- 20.Raji MA, Reyes-Ortiz CA, Kuo YF, Markides KS, Ottenbacher KJ. Depressive symptoms and cognitive change in older Mexican Americans. J Geriatr Psychiatry Neurol. 2007;20:145–152. doi: 10.1177/0891988707303604. [DOI] [PubMed] [Google Scholar]
- 21.National Archive of Computarized Data on Aging. Inter-university Consortium for Political and Social Research. 2012;1907 [Google Scholar]
- 22.Baker PS, Bodner EV, Allman RM. Measuring life-space mobility in community-dwelling older adults. J Am Geriatr Soc. 2003;51:1610–1614. doi: 10.1046/j.1532-5415.2003.51512.x. [DOI] [PubMed] [Google Scholar]
- 23.Peel C, Sawyer BP, Roth DL, Brown CJ, Brodner EV, Allman RM. Assessing mobility in older adults: the UAB Study of Aging Life-Space Assessment. Phys Ther. 2005;85:1008–1119. [PubMed] [Google Scholar]
- 24.Mackey DC, Cauley JA, Barrett-Connor E, Schousboe JT, Cawthon PM, Cummings SR. Life-space mobility and mortality in older men: a prospective cohort study. J Am Geriatr Soc. 2014;62:1288–1296. doi: 10.1111/jgs.12892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sheppard KD, Sawyer P, Ritchie CS, Allman RM, Brown CJ. Life-space mobility predicts nursing home admission over 6 years. J Aging Health. 2013;25:907–920. doi: 10.1177/0898264313497507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Allman RM, Baker PS, Maisiak RM, Sims RV, Roseman JM. Racial similarities and differences in predictors of mobility change over eighteen months. J Gen Intern Med. 2004;19:1118–1126. doi: 10.1111/j.1525-1497.2004.30239.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Radloff LS. The CED-S Scale: A self-report depression scale for research in the general population. J Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 28.Katz s, Ford AB, Moscowitz RW, Jackson BA, Jaffe NM. The index of ADL: a standardized measure of biological and psychosocial function. JAMA. 1963;21:941–949. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 29.Guralnik JM, Ferrucci L, Pieper CF, et al. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci. 2000;55:M221–M231. doi: 10.1093/gerona/55.4.m221. [DOI] [PubMed] [Google Scholar]
- 30.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 31.Bird HR, Canino G, Stipec MR, Shrout P. Use of the Mini-mental State Examination in a probability sample of a Hispanic population. J Nerv Ment Dis. 1987;175:731–737. doi: 10.1097/00005053-198712000-00005. [DOI] [PubMed] [Google Scholar]
- 32.Crum RM, Anthony JC, Bassett SS, Folstein MF. Population-based norms for the Mini-Mental State Examination by age and educational level. JAMA. 1993;269:2386–2391. [PubMed] [Google Scholar]
- 33.Mulgrew CL, Morgenstern N, Shetterly SM, Baxter J, Baron AE, Hamman RF. Cognitive functioning and impairment among rural elderly Hispanics and non-Hispanic whites as assessed by the Mini-Mental State Examination. J Gerontol B Psychol Sci Soc Sci. 1999;54:223–230. doi: 10.1093/geronb/54b.4.p223. [DOI] [PubMed] [Google Scholar]
- 34.Padubidri A, Al SS, Samper-Ternent R, Markides KS, Ottenbacher KJ, Raji MA. Falls and cognitive decline in Mexican Americans 75 years and older. Clin Interv Aging. 2014;9:719–726. doi: 10.2147/CIA.S59448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Raji MA, Al Snih S, Ray LA, Patel KV, Markides KS. Cognitive status and incident disability in older Mexican Americans: findings from the Hispanic established population for the epidemiological study of the elderly. Ethnicity & disease. 2004;14:26–31. [PubMed] [Google Scholar]
- 36.Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42:121–130. [PubMed] [Google Scholar]
- 37.Milgram NW, Siwak-Tapp CT, Araujo J, Head E. Neuroprotective effects of cognitive enrichment. Ageing Res Rev. 2006;5:354–369. doi: 10.1016/j.arr.2006.04.004. [DOI] [PubMed] [Google Scholar]
- 38.Scarmeas N, Levy G, Tang MX, Manly J, Stern Y. Influence of leisure activity on the incidence of Alzheimer's disease. Neurology. 2001;57:2236–2242. doi: 10.1212/wnl.57.12.2236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rantakokko M, Iwarsson S, Portegijs E, Viljanen A, Rantanen T. Associations between environmental characteristics and life-space mobility in community-dwelling older people. J Aging Health. 2015;27:606–621. doi: 10.1177/0898264314555328. [DOI] [PubMed] [Google Scholar]
- 40.Zunzunegui MV, Alvarado BE, Del ST, Otero A. Social networks, social integration, and social engagement determine cognitive decline in community-dwelling Spanish older adults. J Gerontol B Psychol Sci Soc Sci. 2003;58:S93–S100. doi: 10.1093/geronb/58.2.s93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Choi M, Lohman MC, Mezuk B. Trajectories of cognitive decline by driving mobility: evidence from the Health and Retirement Study. Int J Geriatr Psychiatry. 2014;29:447–453. doi: 10.1002/gps.4024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Portegijs E, Iwarsson S, Rantakokko M, Viljanen A, Rantanen T. Life-space mobility assessment in older people in Finland; measurement properties in winter and spring. BMC Res Notes. 2014;7:323. doi: 10.1186/1756-0500-7-323. [DOI] [PMC free article] [PubMed] [Google Scholar]