Abstract
Objective
The increased risk for poor physical and mental health outcomes for older parents in Mexico who have an adult child living in the United States may contribute to an increased risk for cognitive impairment in this population. The objective of this study was to examine if older adults in Mexico who have one or more adult children living in the United States are more or less likely to develop cognitive impairment over an 11-year period compared to older adults who do not have any adult children living in the United States.
Design
Data for this study came from Wave I (2001) and Wave III (2012) of the Mexican Health and Aging Study. The final sample included 2609 participants aged 60 and over who were not cognitively impaired in 2001 and had one or more adult children (age ≥15). Participants were matched using a propensity score that was estimated with a multivariable logistic regression model that included sociodemographic characteristics and migration history of the older parents.
Results
Having one or more adult children living in the United States is associated with lower socioeconomic status and higher number of depressive symptoms, but greater social engagement for older parents living in Mexico. No significant differences in the odds for developing cognitive impairment according to having one or more adult children living in the United States were detected.
Conclusion
In summary, having one or more adult children living in the United States was associated with characteristics that may increase and decrease the risk for cognitive impairment. This may contribute to the non-significant relationship between migration status of adult children and likelihood for cognitive impairment for older parents living in Mexico.
Keywords: Cognition, human migration, Mexico, aging
Introduction
Familism is an important construct of Latin American culture that describes the strong emotional attachment and feelings of loyalty and solidarity to immediate and extended family members (Marin and Marin 1991). Familism contributes to the greater involvement of family in the care of sick family members and to the expectation that adult children will provide care for their aging parents (Herrera et al. 2008). Adult children caring for aging parents is especially important in Mexico and other Latin American countries because of the underdeveloped health care system and limited public resources for old-age support and long-term care in these countries (Vazquez et al. 2009).
In 2012 there were an estimated 33.7 million people of Mexican origin living in the United States of which 11.4 million were born in Mexico and subsequently immigrated to the United States (Gonzalez-Barrera and Lopez 2013). Mexican immigrants are frequently working-aged males pursuing employment opportunities (Passel, D’Vera, and Gonzalez-Barrera 2012). The emigration of adult children from Mexico to the United States can have positive and negative implications for aging parents who remain in Mexico. Migrating to the United States may allow for adult children to send remittances to aging parents, which can be an important source of financial support in old age (Antman 2012), can help pay for household expenses (Durand et al. 1996), and may reduce household poverty (Acosta, Fajnzylber, and Lopez 2007). Remittances have also been reported to increase healthcare utilization by aging parents because they are able to pay for more expensive services (Lopez-Cevallos and Chi 2012). Conversely, the migration of an adult child from Mexico to the United States has been associated with an increased risk for adverse health events for older adults, including heart attack, stroke, and poor mental health (Antman 2016). Migration of adult children may also have negative effects on the social well-being of older parents. However, the results of a study using data from Thailand provide evidence that technological advances in communication and transportation enable aging parents and migrant children to maintain contact, potentially decreasing the negative impact of adult child migration on the social support and isolation of aging parents (Knodel and Saengtienchai 2007).
An extensive body of literature documents the effects of adult child migration on economic outcomes for aging parents, but there is limited research on the influence of adult child migration on physical and mental health outcomes of aging parents. Depression, stroke, and heart disease are all risk factors for cognitive impairment (Reitz, Brayne, and Mayeux 2011), and the increased rates of these conditions that have been observed among aging parents who have an adult child migrate to the United States (Antman 2010) may contribute to poor cognitive outcomes in this population. In addition, aging parents in Mexico often rely upon their children for social support and assistance with meeting financial or household needs (Antman 2012). Older adults who are socially engaged, have social support networks, and have friends or family nearby who can provide assistance are less likely to become cognitively impaired compared to older adults without these resources (Kuiper et al. 2015). Thus, when an adult child migrates to the United States, the aging parent loses a source of direct support, which may increase their risk for cognitive impairment. Finally, the added stress and worry of having an adult child in the United States, especially if the child is an undocumented migrant, may increase the risk for cognitive impairment for aging parents in Mexico.
Globally, in 2010, 58% of all adults aged 60 and over diagnosed with dementia were living in low- and middle-income countries (Prince et al. 2013). Furthermore, it is expected that rapid population aging in low- and middle-income countries will contribute to a greater increase in dementia prevalence compared to Western countries (Ferri et al. 2005). This is particularly true for Latin America, which is projected to experience a 120% increase in dementia prevalence from 2001 to 2020 compared to 49% for North America over the same time period (Ferri et al. 2005). To our knowledge, no research has been conducted on whether the potentially disruptive change in family structure due to migration of young adults from Mexico to the United States is related to cognitive outcomes of older parents who remain in Mexico. Studying the relationship between having an adult child living in the United States and cognitive outcomes of aging parents living in Mexico is necessary to gain a better understanding of the unique factors that may contribute to the expected increase of dementia in Mexico and other Latin American countries.
An adult child’s decision to migrate may be influenced by the health status of his or her older parent (Antman 2016). This presents a significant challenge to studying the effect that having an adult child migrate to the United States has on the health of an older parent because the observed relationship between adult child migration and outcomes of the older parent may be due to reverse causality. For example, adult children who have an older parent in poor health may migrate to the United States to pursue higher wages so that they can help pay for medical care or they may remain close to home so that they can provide direct care. Alternatively, an adult child may be more prone to migrate to the United States if his or her older parent is in good health and has strong social support networks because the parent will not rely upon the adult child for direct support. An additional challenge to investigators is that individuals who migrate to the United States from Mexico are selected into migration (Breslau et al. 2011) and these characteristics, such as a genetic predisposition for good health, personality characteristics, and financial resources, may also contribute to the overall better health of the older parent (Kuhn, Everett, and Silvey 2011). Not accounting for reverse causality and the non-random selection of migrants from the general population can lead to biased results of the impact of migration because the observed effect of migration may be confounded by the effect of factors that contributed to the decision to migrate (Antman 2013).
A randomized trial is the gold standard for estimating treatment effects because the random assignment of participants into treatment and control groups minimizes the potential for systematic differences in observed and unobserved pretreatment characteristics of participants. Data from migration lottery programs have allowed for randomized designs to be used in migration research (Stillman, Gibson, and McKenzie 2012), but this approach is often not feasible due to data limitations. An alternative approach to address the non-random selection of migrants in observational studies is propensity score analysis. This analytical approach allows for observational studies to adopt a pseudo-randomized design by estimating the likelihood of treatment assignment based on observable baseline characteristics and then matching participants in the treatment and control groups based on their propensity score.
Propensity score matching analysis was used in the present study to estimate the likelihood of an older parent having an adult child living in the United States. This propensity was based on parental sociodemographic and migration history variables, and then the score was used to match each study participant with one or more adult children in the United States to a study participant who reported having no adult children living in the United States. Additionally, we minimized the likelihood of reverse causality by using a longitudinal study design and excluding from the analytical sample the older parents who had evidence of cognitive impairment during the baseline observation.
Methods
Mexican Health and Aging Study
Data for the present study come from the Mexican Health and Aging Study (MHAS). The MHAS is an ongoing longitudinal study of aging in Mexico that includes a nationally representative sample of adults aged 50 and over in 2001 (Wong, Michaels-Obregon, and Palloni 2015). A total of 15,186 adults were interviewed during the baseline observation in 2001 (Wave I) and subsequent observations were completed in 2003 (Wave II) and 2012 (Wave III). Detailed information on participants’ sociodemographic characteristics, family structure, current self-reported health status and health conditions, lifestyle characteristics, history of migration to and from the United States, economic status, cognitive functioning, and participants’ childhood health and living conditions have been collected using direct and proxy interviews. Proxy interviews were given to a spouse or family member when the target participant was unable to complete the interview because of illness, hospitalization, or temporary absence. The primary analysis used data from Waves I and III because the two years that elapsed between Waves I and II is not a sufficient period of time for substantial changes in cognitive functioning to be detected.
Measures
The primary independent variable was having one or more adult children (defined as being aged ≥15 years) living in the United States during Wave I. This was a dichotomous variable coded as zero if the older parent reported that none of their adult children were currently residing in the United States, and as one if the older parent reported having one or more adult children currently residing in the United States. Measures for parental sociodemographic characteristics (age, gender, education, employment status, marital status, living in an urban or rural community, living in a high migration state, has ever lived/worked in the United States, and having a toilet in the household as a child), characteristics of adult children (number who completed high school, number who are married), parental health (diabetes, hypertension, heart attack, stroke, high depressive symptoms, having experienced a head injury as a child), and parental social engagement characteristics (number of visits with friends per month, having relatives who live in the neighborhood, having friends you can count on, and volunteering) were collected during the Wave I interview.
Cognitive functioning of participants who received a direct interview was assessed using the Cross-Cultural Cognitive Examination (CCCE) (Glosser et al. 1993). A detailed description of the scoring and implementation of the CCCE in the MHAS has been provided previously (Mejia-Arango, Wong, and Michaels-Obregon 2015). Wave I included measures for verbal learning (word list immediate recall), verbal memory (word list delayed recall), visuospatial abilities (figure drawing), visual memory (delayed recall of figure drawing), and attention (visual scanning). These five measures were included in Wave III plus measures for orientation (date naming), verbal fluency (animal naming), and numeracy (counting backward). Cognitive impairment for participants who were directly interviewed was defined as scoring 1.5 standard deviations or lower based on a participant’s age on two or more assessments (Mejia-Arango and Gutierrez 2011).
Cognitive functioning of participants who required a proxy to complete the Wave III interview was measured using an abbreviated version of the Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE) (Jorm 2004). The abbreviated IQCODE consists of 16 questions that are answered by an informant (e.g. family member or relative) with knowledge of changes in cognitive functioning of the participant over a two-year period. The informant answers each question on a 1 to 5 scale (1-much improved, 3- not much change, 5-much worse) and a summary score can be obtained by calculating the average of the 16 items. An average score of ≥3.4 was used to define cognitive impairment for participants who required the IQCODE (Jorm 2004). The cognitive domains assessed by the IQCODE are consistent with those assessed by the CCCE (e.g. memory, executive functioning, attention) and both instruments provide a general measure of cognitive functioning (Glosser et al. 1994; Jorm 2004).
Selection of final sample
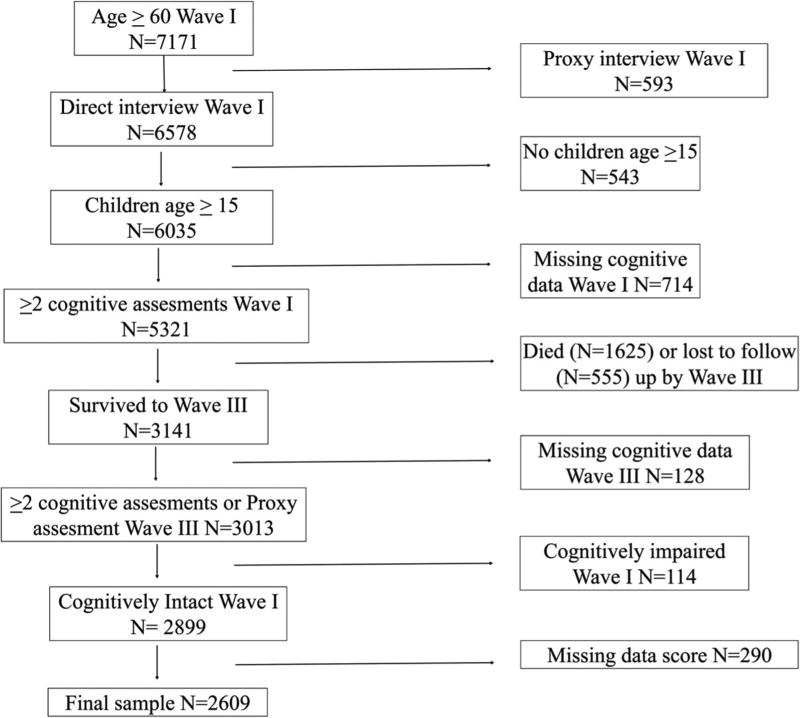
A visual description of the selection of the 2609 participants included in the final analytic sample is presented in Figure 1. The final sample included MHAS participants aged 60 and over who had one or more living children aged 15 and over at Wave I. We excluded participants who reported having no living children or only having living children younger than 15 years of age because these parents were not at risk of having an adult child living in the United States. A total of 114 participants who had cognitive impairment during Wave I were excluded from the final sample. We excluded older adults who required a proxy to complete the Wave I interview, and who completed one or zero cognitive assessments. Participants who required a proxy interview for Wave I were excluded because measures for high depressive symptoms were only collected from participants who received a direct interview. Participants included in the final sample were required to have completed ≥2 cognitive assessments or a proxy measure for cognition during the Wave III observation. Finally, 290 participants who had missing data for one or more covariates included in the propensity score or in the multivariable logistic regression models were excluded from the final sample. These 290 participants were significantly older and more likely to have no formal education, have experienced a stroke, not have had a toilet in the household as a child, not have friends in the neighborhood, not have friends they can count on, and have chatted or visited more times per month compared to the 2609 participants in the final sample.
Figure 1.
Selection of analytic sample.
Statistical methods
Propensity score analysis
Studies on variable selection to estimate the propensity score indicate that the number of matched pairs is maximized when confounding variables and variables related to the outcome are used (Patrick et al. 2011). Therefore, for our case, we selected variables related to parental sociodemographic characteristics and parental migration history because these variables influence the likelihood of having an adult child migrate and are plausibly associated with cognitive functioning of the parent. These variables included having completed at least one year of formal education, living in an urban community, having ever worked or lived in the United States, and having a toilet in the household as a child, which served as a proxy measure for the early life socioeconomic status of the parent (Beltran-Sanchez et al. 2011). Additional variables plausibly related to cognition included in the propensity score equation were current marital status (married, not married), gender, age, and having experienced a head injury as a child. The propensity score was estimated by including the selected variables as covariates in a multivariable logistic regression model with the dependent variable being having an adult child living in the United States at Wave I.
Matching procedure
The obtained propensity score was used to match a randomly selected participant from the treatment group (i.e. parents with one or more adult children living in the United States) to a participant in the control group (i.e. parents with no adult children living in the United States) whose propensity score was closest to that of the treated participant. If multiple participants in the control group had a propensity score that was equally close to that of the participant in the treatment group, then one of the participants from the control group was selected at random. Participants in the control group were no longer eligible to be matched once they had been matched to a participant in the treatment group. The logits of the propensity scores of the treatment and control groups were required to be within 0.20 standard deviations. Participants in the treatment group who could not be matched to a participant in the control group within 0.2 standard deviations were not included in the matched sample.
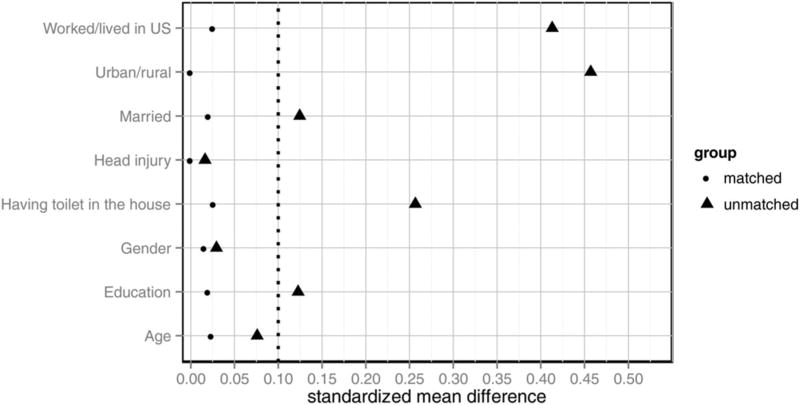
After the matching procedure was complete, 641 out of 673 participants in the treatment group were successfully matched to a participant in the control group. The distribution, frequencies, and standard mean differences of covariates in the unmatched and matched samples were examined to determine if the model used to calculate the propensity score was correctly specified and if the covariates were sufficiently balanced after the matching procedure was complete. A standard mean difference of 0 indicates the variable is perfectly balanced between the treatment and control groups. The closer the standard mean difference is to 0 the better the balance of the covariate in the matched sample. A standard difference of <0.1 was used as the threshold for determining if a covariate was sufficiently balanced in the matched sample.
Differences in the demographic, health, social, and adult child characteristics of participants of the unmatched sample according to having an adult child living in the United States were examined using independent t-tests for continuous variables, chi-squared tests for categorical variables, and Poisson regression for variables related to the number of adult children (total, completed high school, and married) and times per month chatting or visiting with friends. Logistic regression models were constructed using data from the matched sample to estimate the odds for cognitive impairment in 2012 as a function of having one or more adult children living the United States as of 2001. Unadjusted and adjusted models were used to account for potential mediating and confounding effects of sociodemographic, health, and social characteristics, and variables that influence the likelihood of having an adult child migrate. Hubert-White robust standard errors were used to calculate confidence intervals to account for the correlation between participants in the matched sample.
Results
Table 1 presents the distribution and frequencies of the covariates used to estimate the propensity score for the matched and unmatched samples. The distribution and frequencies of the covariates were much more balanced in the matched sample compared to the unmatched sample. This is indicated by the smaller standard mean differences in the matched sample compared to the unmatched sample (Figure 2).
Table 1.
Distribution and frequency of propensity score covariates in the unmatched and matched samples according to having an adult child living in the United States.
| Unmatched Sample
|
Matched Sample
|
|||||
|---|---|---|---|---|---|---|
| Adult child living in the United States | Adult child living in the United States | |||||
| Measure, n (%) | No (n = 1936) | Yes (n = 673) | P-value | No (n = 641) | Yes (n = 641) | P-value |
| Age, mean (SD) | 66.6 (5.5) | 66.2 (5.3) | 0.09 | 66.1 (5.4) | 66.2 (5.3) | 0.67 |
| Gender | 0.51 | 0.77 | ||||
| Male | 809 (73.5) | 291 (26.5) | 272 (50.5) | 267 (49.5) | ||
| Female | 1127 (74.7) | 382 (25.3) | 369 (49.7) | 374 (50.3) | ||
| Education | 0.01 | 0.72 | ||||
| 0 years | 489 (70.3) | 207 (29.7) | 204 (50.7) | 198 (49.3) | ||
| 1+ years | 1447 (75.6) | 466 (24.4) | 437 (49.7) | 443 (50.3) | ||
| Marital status | 0.01 | 0.71 | ||||
| Not married | 673 (77.5) | 195 (22.5) | 183 (49.2) | 189 (50.8) | ||
| Married | 1263 (72.5) | 478 (27.5) | 458 (50.3) | 452 (49.7) | ||
| Living in urban region | <0.01 | 1.0 | ||||
| No | 564 (62.2) | 343 (37.8) | 315 (50.0) | 315 (50.0) | ||
| Yes | 1372 (80.6) | 330 (19.4) | 326 (50.0) | 326 (50.0) | ||
| Worked/lived in the United States | <0.01 | 0.65 | ||||
| No | 1811 (77.1) | 537 (22.9) | 543 (50.3) | 537 (49.7) | ||
| Yes | 125 (47.9) | 136 (52.1) | 98 (48.5) | 104 (51.5) | ||
| Toilet in the home | <0.01 | 0.64 | ||||
| No | 1316 (71.2) | 533 (28.8) | 496 (49.6) | 503 (50.4) | ||
| Yes | 620 (81.6) | 140 (18.4) | 145 (51.2) | 138 (48.8) | ||
| Head injury | 0.72 | 1.0 | ||||
| No | 1861 (74.1) | 649 (25.9) | 618 (50.0) | 618 (50.0) | ||
| Yes | 75 (75.8) | 24 (24.2) | 46 (50.0) | 46 (50.0) | ||
Note: Differences in continuous and dichotomous variables determined using t-test and Chi-square test.
Not married included participants who reported being divorced, separated, or widowed.
Figure 2.
Standard mean difference in the unmatched and matched samples. Dashed vertical line at standardized mean difference equals 0.10 represents balance threshold. Values closer to zero are more balanced.
A total of 673 older adults in the final unmatched sample reported having one or more adult children living in the United States during Wave I. The average number of adult children living in the United States was 2.4 (range 1–9 children) and the average duration in the United States by the adult children was 8.8 (range 1–38.3). Of the 2609 participants in the final sample, 419 were classified as having developed cognitive impairment at Wave III. Only 14 additional participants were classified as cognitively impaired when using all 8 cognitive assessments administered during the Wave III interview compared to when using the 5 assessments that are consistent between Wave I and Wave III.
Statistically significant differences in the baseline characteristics of older adults in the unmatched sample according to having an adult child living in the United States were detected (Table 2). Older adults with one or more adult children living in the United States were more likely to have no formal education, to be married, to live in a less urbanized community, to not have had a toilet in the household as a child, to live in a high migration state, to have high depressive symptoms, to have friends in the neighborhood, to have friends they can count on, and to have visited or chatted more times per month with neighbors compared to older adults with no adult children living in the United States. Additionally, older adults with one or more adult children living in the United States had more adult children, had fewer adult children who completed high school, and had more adult children who were married.
Table 2.
Characteristics of older parents in the final sample according to having one or more adult children living in the United States (N = 2609).
| Measure | No adult children living in the United States (n = 1936) |
Adult child living in the United States (n = 673) |
P- Value |
|---|---|---|---|
| Age, mean (SD) | 66.6 (5.5) | 66.2 (5.3) | 0.09 |
| Gender, n (%) | 0.51 | ||
| Male | 809 (41.8) | 291 (43.2) | |
| Female | 1127 (58.2) | 382 (56.8) | |
| Education, n (%) | 0.01 | ||
| 0 years | 489 (25.2) | 207 (30.8) | |
| 1+ years | 1447 (74.7) | 466 (69.2) | |
| Currently married, n (%) | 0.01 | ||
| No | 673 (34.8) | 195 (29.0) | |
| Yes | 1263 (65.2) | 478 (71.0) | |
| Live in urban region, n (%) | <0.01 | ||
| No | 564 (29.1) | 343 (51.0) | |
| Yes | 1372 (70.9) | 330 (49.0) | |
| Currently employed, n (%) | 0.35 | ||
| No | 1216 (62.8) | 409 (60.8) | |
| Yes | 720 (37.2) | 264 (39.2) | |
| Toilet in the household, n (%) | <0.01 | ||
| No | 1316 (68.0) | 533 (79.2) | |
| Yes | 620 (32.0) | 140 (20.8) | |
| Number of kids 15 or older, mean (SD) | 5.4 (3.0) | 7.3 (2.9) | <0.01 |
| Number of kids who completed high school, mean (SD) | 1.8 (2.1) | 1.6 (2.1) | <0.01 |
| Number of kids married, mean (SD) | 4.1 (2.8) | 5.8 (2.7) | <0.01 |
| Live in a high migration state, n (%) | <0.01 | ||
| No | 1511 (78.0) | 413 (61.4) | |
| Yes | 425 (22.0) | 260 (38.6) | |
| Parent has lived/worked in the United States, n (%) | <0.01 | ||
| No | 1811 (93.4) | 537 (79.8) | |
| Yes | 125 (6.6) | 136 (20.2) | |
| Diabetes, n (%) | 0.21 | ||
| No | 1675 (86.5) | 595 (88.4) | |
| Yes | 261 (13.5) | 78 (11.6) | |
| Hypertension, n (%) | 0.42 | ||
| No | 1159 (59.9) | 391 (58.1) | |
| Yes | 777 (40.1) | 282 (41.9) | |
| Heart attack, n (%) | 0.27 | ||
| No | 1883 (97.3) | 649 (96.4) | |
| Yes | 53 (2.7) | 24 (3.6) | |
| Stroke, n (%) | 0.57 | ||
| No | 1897 (98.0) | 657 (97.6) | |
| Yes | 39 (2.0) | 16 (2.4) | |
| High depressive symptoms, n (%) | 0.01 | ||
| No | 1456 (75.2) | 471 (70.0) | |
| Yes | 480 (24.8) | 202 (30.0) | |
| Head injury as a child, n (%) | 0.72 | ||
| No | 1861 (96.1) | 649 (96.4) | |
| Yes | 75 (3.9) | 24 (3.6) | |
| Number of chats/visits with friends per month, mean (SD) | 13.0 (13.1) | 15.3 (13.4) | <0.01 |
| Have friends who live in the neighborhood, n (%) | 0.02 | ||
| No | 390 (20.1) | 109 (16.2) | |
| Yes | 1546 (79.9) | 564 (83.8) | |
| Have relatives who live in the neighborhood, n (%) | 0.71 | ||
| No | 599 (30.9) | 203 (30.2) | |
| Yes | 1337 (69.1) | 470 (69.8) | |
| Have friends you can count on, n (%) | <0.01 | ||
| No | 734 (37.9) | 202 (30.5) | |
| Yes | 1162 (60.1) | 461 (69.5) | |
| Volunteer in community, n (%) | 0.52 | ||
| No | 296 (15.3) | 96 (14.3) | |
| Yes | 1640 (84.7) | 577 (85.7) | |
| Cognitive status Wave III, n (%) | 0.54 | ||
| Not impaired | 1620 (83.7) | 570 (84.7) | |
| Impaired | 316 (16.3) | 103 (15.3) |
Note: Differences in continuous and dichotomous variables determined using t-test and Chi-square test. Poisson regression used for variables related to a number of children and times per month visiting with neighbors.
Not married included participants who reported being divorced, separated, or widowed.
Percentages are based on column totals.
The results from the unadjusted and adjusted logistic regression models using the matched sample are presented in Table 3. Having one or more adult children in the United States was not associated with cognitive impairment at Wave III in the unadjusted model (OR = 0.91, 95% CI = 0.68–1.23). These results were consistent in the demographic, migration, health, social, and fully adjusted models. In the fully adjusted model, advanced age and diabetes in Wave I were associated with higher odds for cognitive impairment at the 11-year follow-up, whereas having a greater number of children complete high school and participating in volunteer activities at Wave I were associated with lower odds for cognitive impairment at follow-up (Table 3).
Table 3.
Likelihood for cognitive impairment according to having one or more adult children living in United States.
| Unadjusted, OR (95% CI) | Demographics, OR (95% CI) | Migration, OR (95% CI) | Health, OR (95% CI) | Social, OR (95% CI) | Full model, OR (95% CI) | |
|---|---|---|---|---|---|---|
| Child in the United States | 0.91 (0.68, 1.23) | 0.90 (0.66, 1.22) | 0.85 (0.62, 1.17) | 0.90 (0.67, 1.22) | 0.91 (0.67, 1.22) | 0.86 (0.61, 1.21) |
| Age | 1.09* (1.06, 1.12) | 1.09* (1.06, 1.12) | ||||
| Female | 0.89 (0.61, 1.32) | 1.01 (0.65, 1.57) | ||||
| 1+ years Education | 0.82 (0.59, 1.14) | 0.89 (0.63, 1.26) | ||||
| Married | 0.73 (0.52, 1.04) | 0.74 (0.51, 1.08) | ||||
| Currently working | 0.71 (0.49, 1.04) | 0.71 (0.47, 1.06) | ||||
| Living in urban community | 0.85 (0.61, 1.17) | 0.87 (0.60, 1.24) | ||||
| Toilet in house during childhood | 0.72 (0.46, 1.11) | 0.84 (0.52, 1.33) | ||||
| Number of kids >15 | 0.95 (0.88, 1.03) | 0.97 (0.89, 1.05) | ||||
| Number of kids complete high school | 0.79* (0.72, 0.87) | 0.80* (0.71, 0.89) | ||||
| Number of kids married | 1.08 (0.99, 1.17) | 1.04 (0.95, 1.13) | ||||
| Living in high migration state | 1.22 (0.87, 1.69) | 1.19 (0.83, 1.70) | ||||
| Worked/lived in the United States | 1.30 (0.86, 1.91) | 1.52 (0.94, 2.43) | ||||
| Diabetes | 1.61* (1.05, 2.42) | 1.96* (1.24, 3.04) | ||||
| High depressive symptoms | 1.20 (0.86, 1.67) | 0.88 (0.61, 1.28) | ||||
| Heart attack | 0.77 (0.28, 1.78) | 0.72 (0.23, 1.88) | ||||
| Hypertension | 1.04 (0.77, 1.42) | 1.08 (0.77, 1.52) | ||||
| Stroke | 1.37 (0.49, 3.31) | 1.15 (0.36, 3.07) | ||||
| Head injury as a child | 1.16 (0.51, 2.36) | 1.05 (0.43, 2.31) | ||||
| Chat/visits with neighbors | 1.00 (0.99, 1.01) | 0.99 (0.98, 1.01) | ||||
| Friends in neighborhood | 1.22 (0.77, 1.97) | 1.08 (0.66, 1.78) | ||||
| Friends count on | 0.82 (0.58, 1.17) | 0.89 (0.61, 1.30) | ||||
| Relatives in neighborhood | 1.16 (0.77, 1.97) | 1.10 (0.76, 1.61) | ||||
| Volunteer | 0.50* (0.29, 0.83) | 0.56* (0.31, 0.94) |
P < 0.05.
Additional analyses were done to examine the relationship between having one or more adult children living in the United States and scores for verbal learning and memory, visuospatial learning and memory, and attention at Wave III. Scores on verbal learning and memory, visuospatial learning and memory, and attention at Wave I were included as covariates in these multivariable models to control for initial functioning in these cognitive domains. Having one or more adult children in the United States was not significantly associated with scores for verbal learning, verbal memory, visuospatial learning, visuospatial memory, or attention (results not shown).
Discussion
This study examined if older adults in Mexico who have one or more adult children living in the United States are more or less likely to develop cognitive impairment compared to older adults who do not have any adult children living in the United States. The findings from unadjusted and adjusted logistic regression models indicate that there is not a significant relationship between having one or more adult children living in the United States and the odds for cognitive impairment 11 years later. Furthermore, having one or more adult children living in the United States was not associated with scores at Wave III for verbal learning and memory, visuospatial learning and memory, or attention. Previous research using data from the MHAS suggests that having an adult child migrate to the United States is associated with poor physical and mental health of older parents living in Mexico (Antman 2016). Poor mental and physical health are risk factors for cognitive impairment (Whitmer et al. 2005; Heser et al. 2013), and this would suggest that having an adult child migrate to the United States may be detrimental to the cognitive functioning of older parents living in Mexico. Thus, the findings of the present study have important implications for the health and well-being of older parents living in Mexico because having an adult child migrate to the United States does not appear to be a risk factor for cognitive impairment.
There are many plausible explanations for the lack of significant findings. First, having one or more adult children living in the United States was associated with adverse and protective factors for cognitive impairment. We observed that older parents with one or more adult children living in the United States were more likely to report having low socioeconomic status and background and higher depressive symptoms compared to older parents with no adult children living in the United States. Conversely, older parents with one or more adult children living in the United States seemed to be more socially engaged as indicated by the greater likelihood to report having friends in the neighborhood, having friends that they could count on, and chatting or visiting more frequently with neighbors. Low educational attainment (Caamano-Isorna et al. 2006), socioeconomic disadvantages through the life course (Zeki Al Hazzouri et al. 2011), and depressive symptoms (Reitz, Brayne, and Mayeux 2011) are associated with an increased risk for cognitive impairment. Having friends in the neighborhood, having friends to count on, and chatting more frequently were not associated with cognitive impairment in the present analysis, but several other studies have reported that these measures of social engagement are associated with better cognitive outcomes for older adults (Kuiper et al. 2015). Thus, the potential negative effects of low education, low socioeconomic status, and high depressive symptoms may be partly counteracted by the positive effects of being more socially engaged.
A second explanation for the non-significant findings is the lack of detailed migration information in MHAS. This analysis was able to determine if an older parent had one or more adult children living in the United States at the time of the Wave I interview but could not account for the complex migration patterns of adult children, such as seasonal migration, and multiple out and return migration between the United States and Mexico. Many working-aged Mexican adults migrate to the United States seeking seasonal employment and subsequently return to Mexico (Passel and Cohn 2009). Circular migration by an adult child may decrease the potentially negative impact of the migration on the health of the older parent because the adult child is able to earn a greater income by working in the United States and still provide direct support to a parent when he or she returns to Mexico. However, in the present study, the average duration lived in the United States was relatively high (8.8 years) and only 12.7% of the final sample reported having an adult child that had lived in the United States for less than 2 years. This suggests that few older parents in the final sample have adult children with short US durations or with frequent trips between the United States and Mexico.
A third explanation is that this analysis was unable to account for the circumstances that motivated the decision of the adult child to migrate to the United States. It is possible that this decision was related to the characteristics of the older parent, such as available social support and health. We attempted to account for this potential confounding by using propensity score matching, but we could not control for measures not included in the MHAS, such as the age of diagnosis for health conditions.
The present study detected that advancing age and diabetes were associated with increased odds for cognitive impairment, but that participating in volunteer activities was associated with decreased odds for cognitive impairment. Age and diabetes are important risk factors for dementia (Mayeda, Whitmer, and Yaffe 2015) and older adults who participate in socially engaging activities, such as volunteering, have been observed to experience less cognitive decline than non-engaged older adults (James et al. 2011). A novel finding of this study was that having adult children who graduated from high school was associated with decreased odds for cognitive impairment for older parents. The educational attainment of the adult children is unlikely to have a direct effect on the cognitive functioning of older parents. Rather, greater child educational attainment may reflect greater financial resources (Kim and Sherraden 2011) and other socioeconomic factors of the older parent that contribute to the decreased odds for cognitive impairment.
A strength of this study is the use of a longitudinal study design, which allowed for older parents who were cognitively impaired during the baseline observation to be excluded from the analysis. This decreased the likelihood that the migration of the adult child was undertaken in response to his or her parent’s decline in cognition. Additionally, this study used propensity score analysis to account for the endogeneity of the migration selection process that may influence the relationship between having one or more adult children living in the United States and the likelihood for cognitive impairment among older parents living in Mexico.
This study also has limitations that need to be acknowledged. First, by excluding participants with missing data for variables included in the propensity score and in the multivariable logistic regression models, we may have induced bias into the analysis. Second, propensity score analysis fails to control for bias from unobserved variables that are related to having an adult child migrate to the United States and to cognitive functioning of older parents living in Mexico. We were limited in what variables could be used to estimate the propensity score because we could not determine the temporal relationship between when the migration of the adult child occurred and the onset of demographic, health, and social characteristics of the older parent that may influence an adult child to migrate. Determining the sequence of events becomes even more complicated when multiple adult children have migrated since one child could have migrated before the event (e.g. stroke, family moving to the neighborhood) and another child could have migrated after the event had occurred.
In summary, this study provides evidence that older parents who have one or more adult children living in the United States have sociodemographic and health characteristics that may place them at greater risk for cognitive impairment, but that these negative effects may be countered by greater social engagement. Thus, having one or more adult children living in the United States does not appear to be associated with increased odds for cognitive impairment of older parents living in Mexico. Additional research on the relationship between adult child migration and cognitive functioning of older parents living in Mexico and other Latin American countries is necessary before making definitive statements regarding this relationship.
Acknowledgments
Funding
This work was supported by National Institute of Child Health and Human Development: [grant number R01HD051764,R24HD041022]; National Institute on Aging: [grant number 5T32 AG00027017,R01AG018016].
Footnotes
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Acosta P, Fajnzylber P, Lopez JH. The Impact of Remittances on Poverty and Human Capital: Evidence from Latin American House-hold Surveys. Washington, DC: World Bank; 2007. [Google Scholar]
- Antman FM. Adult Child Migration and the Health of Elderly Parents Left Behind in Mexico. American Economic Review. 2010;100(2):205–208. doi: 10.1257/aer.100.2.205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antman FM. Elderly Care and Intrafamily Resource Allocation When Children Migrate. Journal of Human Resource. 2012;47(2):331–363. doi: 10.3368/jhr.47.2.331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antman FM. The Impact of Migration on Family Left Behind. In: Constant Amelie F, Zimmermann Klaus F., editors. In International Handbook on the economics of migration. Cheltenham: Edward Elgar Publishing Limited; 2013. pp. 293–308. [Google Scholar]
- Antman FM. Department of Economics. University of Colorado at Boulder; 2016. How Does International Migration Affect the Health of Elderly Parents Left Behind? Evidence from Mexico. http://spot.colorado.edu/~antmanf/AntmanMigration&ElderlyHealth.pdf. [Google Scholar]
- Beltran-Sanchez H, Crimmins EM, Teruel GM, Thomas D. Links between Childhood and Adult Social Circumstances and Obesity and Hypertension in the Mexican Population. Journal of Aging and Health. 2011;23(7):1141–1165. doi: 10.1177/0898264311422255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau J, Borges G, Tancredi DJ, Saito N, Anderson H, Kravitz R, Hinton L, Aguilar-Gaxiola S, Mora ME. Health Selection among Migrants from Mexico to the U.S.: Childhood Predictors of Adult Physical and Mental Health. Public Health Reports. 2011;126(3):361–370. doi: 10.1177/003335491112600310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caamano-Isorna F, Corral M, Montes-Martinez A, Takkouche B. Education and Dementia: A Meta-Analytic Study. Neuroepidemiology. 2006;26(4):226–232. doi: 10.1159/000093378. [DOI] [PubMed] [Google Scholar]
- Durand J, Kandel W, Parrado EA, Massey DS. International Migration and Development in Mexican Communities. Demography. 1996;33(2):249–264. [PubMed] [Google Scholar]
- Ferri CP, Prince M, Brayne C, Brodaty H, Fratiglioni L, Ganguli M, Hall K, et al. Global Prevalence of Dementia: A Delphi Consensus Study. The Lancet. 2005;366(9503):2112–2117. doi: 10.1016/S0140-6736(05)67889-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glosser G, Wolfe N, Albert ML, Lavine L, Steele JC, Calne DB, Schoenberg BS. Cross-cultural Cognitive Examination: Validation of a Dementia Screening Instrument for Neuroepidemiological Research. Journal of the American Geriatrics Society. 1993;41(9):931–939. doi: 10.1111/j.1532-5415.1993.tb06758.x. [DOI] [PubMed] [Google Scholar]
- Glosser G, Wolfe N, Kliner-Krenzel L, Albert ML. Cross-cultural Cognitive Examination Performance in Patients with Parkinson’s Disease and Alzheimer’s Disease. The Journal of Nervous and Mental Disease. 1994;182(8):432–436. doi: 10.1097/00005053-199408000-00002. [DOI] [PubMed] [Google Scholar]
- Gonzalez-Barrera A, Lopez MH. A Demographic Portrait of Mexican-origin Hispanics in the United States. Washington, DC: Pew Research Hispanic Center; 2013. [Google Scholar]
- Herrera AP, Lee J, Palos G, Torres-Vigil I. Cultural Influences in the Patterns of Long-term Care Use Among Mexican American Family Caregivers. Journal of Applied Gerontology. 2008;27(2) [Google Scholar]
- Heser K, Tebarth F, Wiese B, Eisele M, Bickel H, Kohler M, Mosch E, et al. Age of Major Depression Onset, Depressive Symptoms, and Risk for Subsequent Dementia: Results of the German Study on Ageing, Cognition, and Dementia in Primary Care Patients (AgeCoDe) Psychological Medicine. 2013;43(8):1597–1610. doi: 10.1017/S0033291712002449. [DOI] [PubMed] [Google Scholar]
- James BD, Wilson RS, Barnes LL, Bennett DA. Late-life Social Activity and Cognitive Decline in Old Age. Journal of the International Neuropsychological Society. 2011;17(6):998–1005. doi: 10.1017/S1355617711000531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jorm AF. The Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE): A Review. International Psychogeriatrics. 2004;16(3):275–293. doi: 10.1017/s1041610204000390. [DOI] [PubMed] [Google Scholar]
- Kim Y, Sherraden M. Do Parental Assets Matter for Children’s Educational Attainment?: Evidence from Mediation Tests. Children and Youth Services Review. 2011;33:969–979. [Google Scholar]
- Knodel J, Saengtienchai C. Rural Parents with Urban Children: Social and Economic Implications of Migration for the Rural Elderly in Thailand. Population, Space and Place. 2007;13:193–210. [Google Scholar]
- Kuhn R, Everett B, Silvey R. The Effects of Children’s Migration on Elderly Kin’s Health: A Counterfactual Approach. Demography. 2011;48(1):183–209. doi: 10.1007/s13524-010-0002-3. [DOI] [PubMed] [Google Scholar]
- Kuiper JS, Zuidersma M, Oude Voshaar RC, Zuidema SU, van den Heuvel ER, Stolk RP, Smidt N. Social Relationships and Risk of Dementia: A Systematic Review and Meta-Analysis of Longitudinal Cohort Studies. Ageing Research Reviews. 2015;22:39–57. doi: 10.1016/j.arr.2015.04.006. [DOI] [PubMed] [Google Scholar]
- Lopez-Cevallos DF, Chi C. Migration, Remittances, and Health Care Utilization in Ecuador. Revista Panamericana de Salud Pública. 2012;31(1):9–16. doi: 10.1590/s1020-49892012000100002. [DOI] [PubMed] [Google Scholar]
- Marin G, Marin BV. Research with Hispanic Populations. Newbury Park, CA: Sage; 1991. [Google Scholar]
- Mayeda ER, Whitmer RA, Yaffe K. Diabetes and Cognition. Clinics in Geriatric Medicine. 2015;31(1):101–115. doi: 10.1016/j.cger.2014.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mejia-Arango S, Gutierrez LM. Prevalence and Incidence Rates of Dementia and Cognitive Impairment no Dementia in the Mexican Population: Data from the Mexican Health and Aging Study. Journal of Aging and Health. 2011;23(7):1050–1074. doi: 10.1177/0898264311421199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mejia-Arango S, Wong R, Michaels-Obregon A. Normative and Standardized Data for Cognitive Measures in the Mexican Health and Aging Study. Salud Publica De Mexico. 2015;57(Suppl 1):S90–S96. doi: 10.21149/spm.v57s1.7594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Passel J, Cohn D. Mexican Immigrants: How Many Come? How Many Leave? Washington, DC: Pew Hispanic Center; 2009. [Google Scholar]
- Passel J, D’Vera C, Gonzalez-Barrera A. Net Migration from Mexico Falls to Zero—and Perhaps Less. Washington, DC: Pew Hispanic Center Report; 2012. [Google Scholar]
- Patrick AR, Schneeweiss S, Brookhart MA, Glynn RJ, Rothman KJ, Avorn J, Sturmer T. The Implications of Propensity Score Variable Selection Strategies in Pharmacoepidemiology: An Empirical Illustration. Pharmacoepidemiology and Drug Safety. 2011;20(6):551–559. doi: 10.1002/pds.2098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prince M, Bryce R, Albanese E, Wimo A, Ribeiro W, Ferri CP. The Global Prevalence of Dementia: A Systematic Review and Metaanalysis. Alzheimer’s & Dementia. 2013;9(1):63–75.e2. doi: 10.1016/j.jalz.2012.11.007. [DOI] [PubMed] [Google Scholar]
- Reitz C, Brayne C, Mayeux R. ‘Epidemiology of Alzheimer Disease.’ Nature Reviews. Neurology. 2011;7(3):137–152. doi: 10.1038/nrneurol.2011.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stillman S, Gibson J, McKenzie D. The Impact of Immigration on Child Health: Experimental Evidence from a Migration Lottery Program. Economic Inquiry. 2012;50(1):62–81. doi: 10.1111/j.1465-7295.2009.00284.x. [DOI] [PubMed] [Google Scholar]
- Vazquez ML, Vargas I, Unger JP, Mogollon A, Silva MR, de Paepe P. Integrated Health Care Networks in Latin America: Toward a Conceptual Framework for Analysis. Revista Panamericana de Salud Pública. 2009;26(4):360–367. doi: 10.1590/s1020-49892009001000012. [DOI] [PubMed] [Google Scholar]
- Whitmer RA, Sidney S, Selby J, Johnston SC, Yaffe K. Midlife Cardiovascular Risk Factors and Risk of Dementia in Late Life. Neurology. 2005;64(2):277–281. doi: 10.1212/01.WNL.0000149519.47454.F2. [DOI] [PubMed] [Google Scholar]
- Wong R, Michaels-Obregon A, Palloni A. Cohort Profile: The Mexican Health and Aging Study (MHAS) International Journal of Epidemiology. 2015 doi: 10.1093/ije/dyu263. epub ahead of print (January 27, 2015). http://www.ncbi.nlm.nih.gov/pubmed/25626437. [DOI] [PMC free article] [PubMed]
- Zeki Al Hazzouri A, Haan MN, Kalbfleisch JD, Galea S, Lisabeth LD, Aiello AE. Life-course Socioeconomic Position and Incidence of Dementia and Cognitive Impairment Without Dementia in Older Mexican Americans: Results from the Sacramento Area Latino Study on Aging. American Journal of Epidemiology. 2011;173(10):1148–1158. doi: 10.1093/aje/kwq483. [DOI] [PMC free article] [PubMed] [Google Scholar]