Abstract
Background
Physical activity (PA) reduces the rate of mobility disability, compared with health education (HE), in at risk older adults. It is important to understand aspects of performance contributing to this benefit.
Objective
To evaluate intervention effects on tertiary physical performance outcomes.
Design, Setting and Participants
The Lifestyle Interventions and Independence for Elders (LIFE) randomized trial included older adults (n=1635, aged 78.9 ± 5.2 and 67.2% women) at risk for mobility disability (Short Physical Performance Battery [SPPB] score <10) from 8 centers throughout the United States.
Interventions
Moderate PA including walking, resistance and balance training compared with HE consisting of topics relevant to older adults.
Outcomes
Grip strength, SPPB score and its components (balance, 4m gait-speed, and chair-stands), as well as 400meter walking-speed.
Results
Total SPPB score was higher in PA vs. HE across all follow-up times (overall P=0.04) as was the chair-stand component (overall P<0.001). No intervention effects were observed for balance (overall p=0.12), 4meter gait-speed (overall P=0.78), or grip-strength (overall P=0.62). However, 400meter walking-speed was faster in PA vs. HE group (overall P=<0.001). In separate models, 29% of the rate reduction of mobility disability in the PA vs. HE group was explained by change in SPPB score, while 39% was explained by change in the chair-stand component.
Conclusion
Lower extremity performance (SPPB) was significantly higher in the PA compared with HE group. Changes in chair-stand score explained a considerable portion of the effect of PA on the reduction of mobility disability - consistent with the idea that preserving muscle strength/power may be important for the prevention of mobility disability.
Keywords: Randomized clinical trial, physical activity, physical function, gait speed
INTRODUCTION
Slow gait speed in older adults is associated with an increased risk for disability1–2, institutionalization1 and mortality1, 3. Poor muscle function (strength/power) is an important risk factor for slowed gait and is also associated with increased risk of disability4–7 and death4, 7–8. Balance is a major risk factor for falls9–10 and impaired mobility11. Both aerobic and resistance training are successful in improving balance, mobility and muscle function at older ages; however, most studies have been short-term, small or included relatively higher functioning participants12–23.
The LIFE study, a randomized trial of 1,635 adults aged 70–89 and older24, showed over 2.6 years that physical activity (PA) is more effective than health education (HE) at preventing major mobility disability in previously sedentary, at risk older adults25. However, it is also important to determine the effects of PA and HE on common physical performance measures, such as balance mobility and muscle function, to better understand mechanisms underlying the prevention of mobility disability. Functional limitations are known risk factors for disability; thus these performance measures could be used to track early benefits of future interventions aimed at preventing downstream outcomes in the disablement pathway.
The purpose of these pre-specified analyses was to compare the effects of PA with HE on the tertiary outcomes of 400m walking-speed, grip-strength, as well as total Short Physical Performance Battery (SPPB) score and its components: balance, 4m gait speed and repeated chair-stands24. Secondly, we examined the potential mediating role of these performance measures in preventing major mobility disability in at risk older adults. We hypothesized that PA would benefit these functional outcomes to a greater degree than the HE. We also hypothesized that improvements in lower extremity performance (SPPB score) would explain a significant proportion of the effect of the PA intervention compared with the HE intervention on major mobility disability.
METHODS
Clinical Trial Design and Participants
The LIFE Study was a multicenter, single-blind randomized trial of 1,635 sedentary older adults, aged 70–89, at high risk for mobility disability conducted between February 2010 and the predetermined end date of December 201324. LIFE was designed to assess the effect of PA compared with HE in preventing major mobility disability after an average of 2.6 years. Targeted mass mailings were the primary recruitment strategy26. Eligible participants were randomized to the PA or HE group using a permuted block algorithm (with random block lengths) stratified by field center and sex.
Primary results and detailed descriptions of the flow of participants, design, recruitment, and methods were published previously24–26. Briefly, inclusion criteria included, sedentary (reporting <20 min/week of regular exercise in the past month and <125 min/week of moderate PA), high risk for mobility disability (SPPB score <10 and 45% <8)27–28, able to walk 400m in <15min, no cognitive impairment (1.5 standard deviations below education and race-specific norms25 on the Modified Mini-Mental State Examination [3MSE])29; and able to safely participate in the interventions determined by medical history, physical examination, and resting electrocardiography.
Interventions
Both interventions have been described elsewhere24. Briefly, PA sessions were group based and consisted primarily of overground walking, with a goal of 150 min/week, supplemented with strength and balance training designed to be done at the center (2x/week) and at home24. Participants were instructed to walk at a “somewhat hard” intensity and perform strength training at a “hard” intensity30. Resistance training used ankle weights that were adjustable up to 20 lbs. in 0.5 lb. increments. The balance regimen consisted of five levels that progressed in difficulty. Following each session, participants completed several flexibility/stretching exercises.
The HE group consisted of weekly workshops for the first 26 weeks. From week 27 on, sessions were offered 2x/month, with required participation at least 1x/month. The topic of PA was purposefully avoided. The workshops concluded with 5–10 minutes of light, upper extremity stretching.
Clinic Measurements
Participants attended clinic visits every 6-months. Home, telephone and proxy assessments were offered if a participant was unable to attend. The assessment staff was blinded to intervention assignments. Self-reported PA was measured using the Community Healthy Activities Model Program for Seniors (CHAMPS) questionnaire31 and was administered by a separate set of unmasked staff.
Assessments included self-reported race, demographic information, medical and hospitalization history, electrocardiography, physical examination, cognitive testing using the 3MSE29,body height and weight. Activities of daily living (ADL) disability was measured with the Pepper Assessment Tool for Disability (PAT-D) and the average level of difficulty (0–5, 0= none and 5=unable to do) for each of the 7 ADL items was calculated24, 32. These measures were repeated during follow-up at varied intervals. Details of these measures and their frequency are described elsewhere24. Race and ethnicity were reported by the participants and were collected according to NIH categories.
Physical Performance Outcomes
The SPPB, measured at baseline, 6, 12, 24 and 36 months, is a well-validated measure of lower extremity performance and consists of a balance battery with side-by-side, semi-tandem and tandem positions, 4meter walk at usual pace and 5 repeated chair-stands27. Each component was assigned a categorical score ranging from 0 (unable to complete) to 4 (best) and a summary score (0–12) was calculated. Chair-stand score was considered a surrogate for lower extremity muscle function (strength and power)33.
Grip strength was measured with a dynamometer (Jamar Handheld Dynamometer, J.A. Preston Corporation, Clifton, NJ) at baseline and 12-months. Participants performed one practice trial and two tests from a seated position using their dominant hand. The higher value was defined as hand grip strength.
A usual pace 400meter walk was performed at baseline and every 6-months. The primary outcome of the LIFE study was major mobility disability, defined as the inability to complete the 400m walk in <15 minutes without sitting and without the help of another person or walker. In these analyses, 400m walk was also treated as a continuous outcome (m/s). The test consisted of completing 10 laps on a 20meter course (40 meters/lap). Participants were instructed to walk at their usual pace, without overexerting themselves and were allowed to stop for up to 1 minute. Participants were permitted to use single pronged, straight canes only.
Statistical Analysis
Baseline characteristics stratified by intervention group were summarized using means and standard deviations, or counts and percentages. Intervention adherence was the percentage of scheduled center-based intervention sessions attended. We compared the intervention effects, using an intention-to-treat approach, on grip strength, 400m walking speed, and the SPPB and its components, using repeated measures analysis of covariance (ANCOVA) with an unstructured parameterization matrix for longitudinal covariance. Models included the following variables: site, sex (both used to stratify randomization), baseline outcome variable, intervention, visit, and interaction between intervention and visit. The impact of the intervention on the outcome variables was determined by generating least square means from these models. Contrasts were used to estimate the average effects over time. To determine the intervention effects on the lowest functioning participants, we repeated these analyses in participants with baseline SPPB scores <9.
Walking speed for 400m walk failures was calculated by dividing the meters walked prior to stopping by time walked in seconds. We also conducted two sensitivity analyses: 1) evaluated changes in 400m walk after excluding failures and 2) calculated 400m walking speed for failures using an imputation approach, which assumed different distributions for the portion of the walk that went unfinished and estimated the rate of ‘slowing down34’. A sensitivity analysis for grip strength was also performed assigning a 0 to those who could not complete the test due to pain or other contraindication. Those unable to complete 5 repeated chair-stands were assigned a score of 0. A sensitivity analysis was performed in which the time to complete 5 repeated chair stands was treated as a continuous variable and those who could not complete test were assigned a time of 60s.
To determine the role of changes in the components of the SPPB and grip strength on the prevention of major mobility disability, we compared hazard ratios for the intervention effect before and after adjustment for these factors. The proportion of change in the association between intervention and major mobility disability after adjusting for the components of the SPPB, or grip strength, was calculated as: one minus {the regression coefficient of intervention from the adjusted proportional hazards model divided by the regression coefficient of intervention from the original model}. These analyses were only done for those components that showed overall significant differences in change between groups from baseline to 24-months.
No adjustments were made for multiple testing, as these were a priori tertiary aims. Nominal P-values are reported throughout as simple guides to possible associations. Statistical analyses were performed using SAS (SAS Institute), v9.4.
RESULTS
Intervention groups were similar in terms of baseline characteristics (Table 1).
Table 1.
Baseline Characteristics of LIFE Participants by Treatment Arm
| Treatment Arm | ||
|---|---|---|
| Physical Activity (N=818) |
Health Education (N=817) |
|
| Age-years | 78.7 ± 5.2 | 79.1 ± 5.2 |
| Female | 547 (67%) | 551 (67%) |
| Race/Ethnicity | ||
| Black | 163 (20.0%) | 125 (15.3%) |
| White | 604 (74%) | 635 (78%) |
| Hispanic | 31 (4%) | 30 (4%) |
| Other | 20 (3%) | 27 (3%) |
| Education, college and above | 515 (63%) | 529 (65%) |
| ADL disability, 0–5 | 1.3 ± 0.4 | 1.3 ± 0.4 |
| Number of Chronic Diseases, n | 0.5 ± 0.7 | 0.6 ± 0.7 |
| Body Mass Index, kg/m2 | 30.1 ± 5.7 | 30.3 ± 6.2 |
| Waist Circumference, cm | 101.6 ± 15.4 | 102.0 ± 15.7 |
| 3MSE Score, 0–100 | 91.5 ± 5.5 | 91.6 ± 5.3 |
| Balance Score, 0–4 | 2.8 ± 1.1 | 2.7 ± 1.1 |
| Gait Score, 0–4 | 3.0 ± 0.8 | 3.0 ± 0.8 |
| Chair Stand Test Score, 0–4 | 1.6 ± 1.0 | 1.5 ± 1.0 |
| SPPB Total Score, 0–12 | 7.4 ± 1.6 | 7.3 ± 1.6 |
| Gait speed during 400m, m/s | 0.83±0.2 | 0.82 ±0.2 |
| Hand Grip Strength, kg | 24.8 ± 10.1 | 24.5 ± 9.7 |
ADL disability was calculated as the average difficulty across 7 items (0=none – 5=unable to do). Abbreviations: ADL: activities of daily living; 3MSE: Teng Mini Mental State Examination; SPPB: Short Physical Performance Battery
Intervention Effects on Physical Performance Outcomes
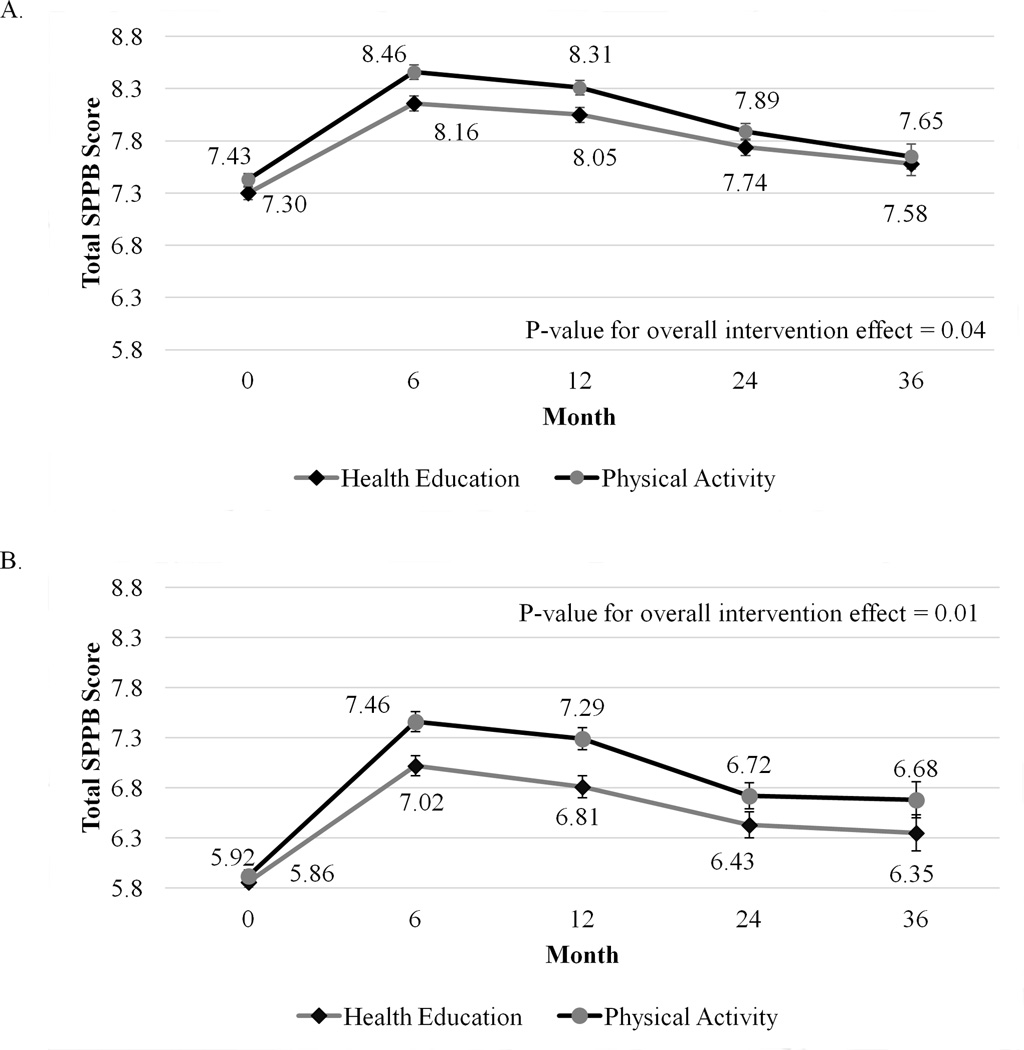
The PA intervention had a significantly more positive overall effect on the SPPB compared with HE (P=0.04, Figure 1). Specifically, PA had significantly higher total SPPB scores at 6-months than the HE group (8.5±0.1 vs. 8.2±0.1, P=0.001). The PA group maintained higher SPPB scores compared with HE at 12-months (8.3±0.1 vs. 8.1±0.1, P=0.01) but scores became more similar between groups at 24- (P=0.19) and 36-months (P=0.69).
Figure 1. Adjusted Least Square Mean for Total SPPB score at Baseline, 6- 12- 24- and 36 Months by Intervention Group in All (panel A) and Lower Functioning Participants (panel B).
Legend: The Physical Activity group had better lower extremity performance (SPPB score), compared with the Health Education group, over the course of the trial (Panel A). These effects were more pronounced in lower functioning participants (SPPB <9, Panel B). Error bars are standard errors. Abbreviations: SPPB: Short Physical Performance Battery.
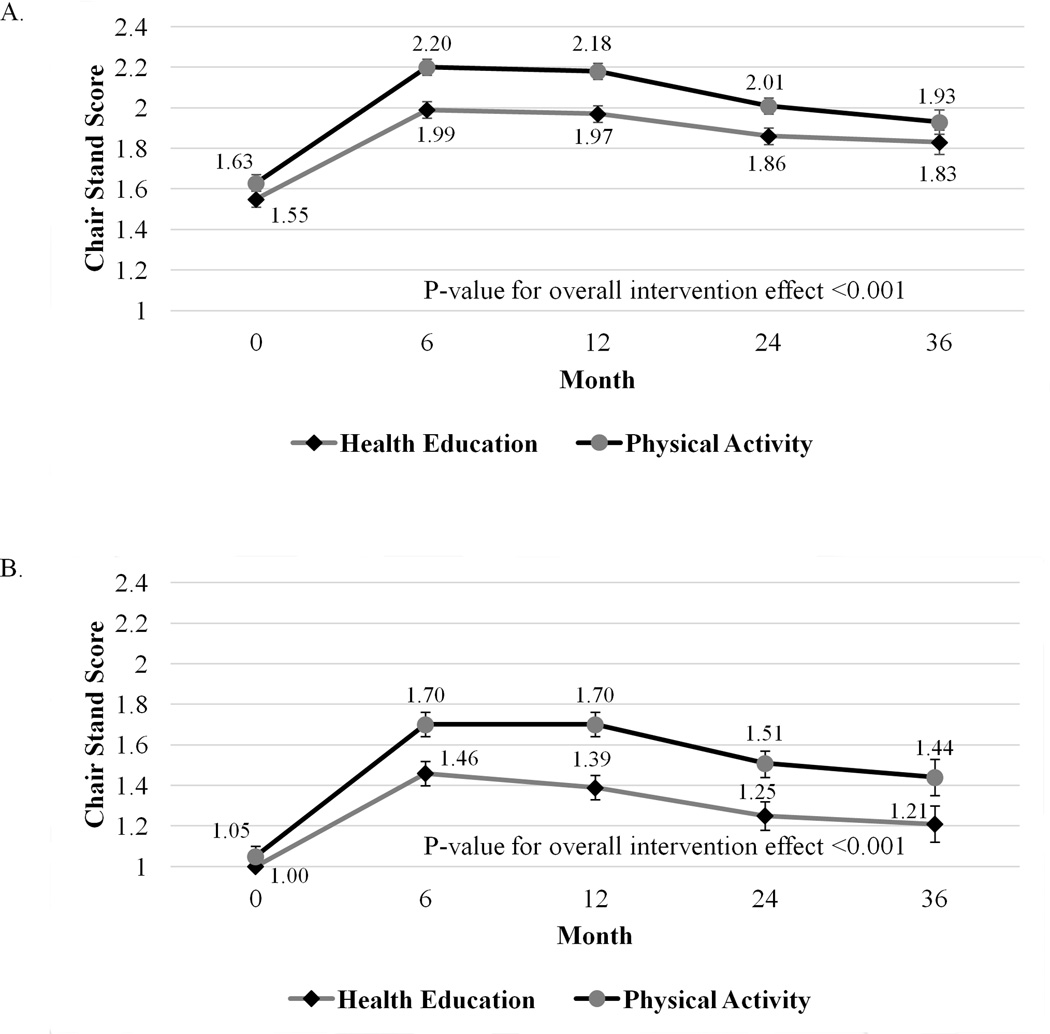
Chair-stand scores were significantly higher in PA compared to HE at 6- (2.2±0.1 vs. 2.0±0.1), 12- (2.2±0.1 vs. 2.0±0.1) and 24-months (2.0±0.1 vs. 1.9±0.1), with a significant overall intervention effect (P<0.001, Figure 2). Sensitivity analyses treating time to complete chair-stands as a continuous variable and assigning 60s to those who could not complete the test yielded nearly identical results. The balance score was higher in PA vs. HE at 6-months (P=0.01) but similar at all other follow-up times (overall effect, P=0.12, Table 2). There was no difference between study arms in 4m gait speed score (overall effect P=0.78, Table 2).
Figure 2. Adjusted Least Square Mean for Chair Stand Score at Baseline, 6- 12- 24- and 36-Months by Intervention Group in All (panel A) and Lower Functioning Participants (panel B).
Legend: The Physical Activity group had better timed chair-stand scores, compared with the Health Education group, over the course of the trial (Panel A). These effects were more pronounced in lower functioning participants (SPPB <9, Panel B). Error bars are standard errors.
Table 2.
Adjusted Mean Gait speed, Balance Score and Hand Grip Strength at each Follow-Up Time by Intervention Group in All and Lower Functioning Participants
| All Participants | Lower Functioning Participants (SPPB Score <8) |
||||||
|---|---|---|---|---|---|---|---|
| Physical Activity |
Health Education |
Physical Activity |
Health Education |
||||
| aMean ± SE | Mean ± SE | P-value | Mean ± SE | Mean ± SE | P-value | ||
|
Balance Score 0–4 |
|||||||
| 6-Months | 3.03±0.03 (N=770) |
2.91±0.03 (N=787) |
0.01 | 2.75±0.06 (N=330) |
2.56±0.05 (N=362) |
0.01 | |
| 12-Months | 2.94±0.04 (N=747) |
2.85±0.04 (N=766) |
0.09 | 2.67±0.06 (N=321) |
2.48±0.06 (N=354) |
0.02 | |
| 24-Months | 2.79±0.04 (N=700) |
2.78±0.04 (N=711) |
0.90 | 2.44±0.07 (N=291) |
2.41±0.06 (N=327) |
0.77 | |
| 36-Months | 2.77±0.06 (N=279) |
2.72±0.06 (N=283) |
0.52 | 2.57±0.10 (N=104) |
2.36±0.09 (N=114) |
0.12 | |
| Overall Effect | - | - | 0.12 | - | - | 0.03 | |
|
Usual gait speed score, 0–4 |
|||||||
| 6-Months | 3.25±0.02 (N=770) |
3.25±0.02 (N=787) |
0.83 | 3.00±0.04 (N=330) |
3.01±0.04 (N=362) |
0.92 | |
| 12-Months | 3.21±0.02 (N=747) |
3.23±0.02 (N=766) |
0.53 | 2.92±0.04 (N=321) |
2.95±0.04 (N=354) |
0.53 | |
| 24-Months | 3.12±0.03 (N=700) |
3.10±0.03 (N=711) |
0.67 | 2.78±0.05 (N=291) |
2.80±0.04 (N=327) |
0.77 | |
| 36-Months | 2.98±0.04 (N=279) |
3.04±0.04 (N=283) |
0.37 | 2.71±0.08 (N=104) |
2.78±0.07 (N=114) |
0.51 | |
| Overall Effect | - | - | 0.78 | - | - | 0.54 | |
|
400m walking- speed, m/s |
|||||||
| 6-Months | 0.84±0.00 (N=764) |
0.81±0.00 (N=775) |
<0.001 | 0.78±0.01 (N=326) |
0.73±0.01 (N=354) |
<0.001 | |
| 12-Months | 0.82±0.00 (N=734) |
0.80±0.00 (N=756) |
<0.001 | 0.74±0.01 (N=313) |
0.71±0.01 (N=345) |
<0.001 | |
| 18-Months | 0.81±0.00 (N=707) |
0.78±0.00 (N=723) |
<0.001 | 0.74±0.01 (N=299) |
0.69±0.01 (N=334) |
<0.001 | |
| 24-Months | 0.78±0.01 (N=690) |
0.76±0.01 (N=701) |
0.01 | 0.71±0.01 (N=286) |
0.67±0.01 (N=321) |
<0.001 | |
| Overall Effect | - | - | <0.001 | <0.001 | |||
|
Hand grip strength, kg |
|||||||
| 12-Months | 23.6±0.2 (N=688) |
23.8±0.2 (N=684) |
0.62 | 22.4±0.3 (N=292) |
22.7±0.3 (N=308) |
0.52 | |
All means are least squared means and adjusted for baseline value, clinic site and sex
The benefits of PA compared with HE on the SPPB and its components were more pronounced in older adults at highest risk for mobility disability (baseline SPPB <9, Table 2, Figures 1&2, panel B.). In this sub-group, PA conveyed significant overall benefits to total SPPB score (overall effect P=0.01), balance (overall effect P=0.03) and chair stand scores (overall effect P<0.01) but not gait speed (overall effect P=0.54).
Grip strength followed similar trajectories in both groups (overall effect P=0.62, Table 2). Sensitivity analyses assigning 0 kg to those who could not complete the test yielded similar results.
Walking-speed during the 400m walk was significantly higher in PA vs. HE, with more pronounced effects in the lower functioning sub-group, over the course of the study (both overall effect P<0.001, Table 2.). Both sensitivity analyses - excluding failures and imputing speed for failures - yielded similar results. The correlation between 400m and 4m gait speed at baseline was 0.49.
After adjustment for change in total SPPB score, the hazard ratio (95% confidence interval (CI)) for risk of major mobility disability in PA vs. HE was attenuated to non-significance from 0.82 (0.69–0.98) to 0.87 (0.73–1.04), Table 3. When SPPB score was replaced in the model by just the chair-stand component score, the hazard ratio (95% CI) for risk of major mobility disability in PA vs. HE was attenuated from 0.82 (0.69–0.98) to 0.89 (0.75–1.06). In other words, 29% of the PA effect on the prevention of major mobility disability was explained by total SPPB score, while 39% of the effect was explained by the chair-stand component. In other words, change in lower extremity performance, specifically chair-stand ability, appears to be a mechanism by which PA preserves major mobility disability to a greater degree than HE. Chair-stand score was the only SPPB component to show significant overall intervention effects, which was why chair-stands explained more of the effect of PA on major mobility disability than total SPPB score.
Table 3.
The Effect of Physical Activity compared with Health Education on the Prevention of Mobility Disability Adjusted for Change in Physical Performance
|
aCox Proportional Hazard Model for the development of Mobility disability |
|||
|---|---|---|---|
| Physical Activity vs. Health Education |
Adjusted for change in total SPPB score |
Adjusted for change in chair-stand score |
|
| HR (95% CI) |
0.82 (0.69 – 0.98) |
0.87 (0.73 – 1.04) |
0.89 (0.75 – 1.06) |
Physical performance measures treated as time-dependent variables in separate models
DISCUSSION
We showed that a long term (average 2.6 years), moderate intensity physical activity intervention focused on over ground walking supplemented with lower extremity resistance and balance exercises conveyed significant benefits to lower extremity function (SPPB score) and 400m walking-speed compared with a HE group. The benefit of PA on lower extremity function (SPPB) was mainly attributable to its effect on chair-stand performance, as PA and HE had similar effects on the other two SPPB components: 4m gait speed and balance. There was no difference in grip strength change between the two groups, likely because the PA intervention focused on the lower extremities.
The lower rate of major mobility in the PA group was largely attributable to improved chair-stand performance. Chair-stand performance was the most direct measure of lower extremity muscle strength/power employed in the LIFE study and although influenced by other factors, lower extremity muscle strength is the strongest determinant of chair-stand performance33. Therefore, lower extremity muscle function appears to be a mechanism by which PA prevents mobility disability and targeting this domain appears to be particularly important for preserving mobility in older adults at high risk for mobility disability. It should be noted that other unmeasured factors, such as cardio-respiratory fitness, may also account for the intervention affect on major mobility disability. In fact, the PA group performed better on the 400m walk, which has been shown to reflect fitness in older adults35–36. Interventions specifically aimed at comparing different modalities (strength vs. aerobic vs. a combination) on the prevention of downstream outcomes are needed to refine approaches for the prevention of mobility disability.
Notably, the differences between total SPPB score in the PA compared with HE groups were small despite being statistically significant. Specifically, an improvement of 0.5 points in SPPB score has been estimated to be a small meaningful change14, while the largest difference between the LIFE PA and HE groups was 0.3 points at 6-months. However, the differences in SPPB score in lower functioning participants (SPPB <8) approached the 0.5 threshold at 6- and 12-months. Additionally, despite the modest overall intervention effects, improved chair-stand and SPPB scores did explain a large proportion of the effect of PA compared with HE on the prevention of mobility disability. Thus, previously reported meaningful thresholds for change in SPPB may underestimate the impact of smaller improvements on downstream outcomes such as mobility disability. Finally, the largest benefits were observed for the chair-stand component; therefore, it is also possible that a 0.2 point in the chair-stand component is clinically meaningful despite small overall differences in total SPPB score. It is important to note that other exercise interventions studies of older adults that included more intensive training programs yielded larger changes in SPPB and similar performances measures. Thus, more intensive training may convey greater benefits on major mobility disability. Future studies are needed to determine if more intensive training programs can be tolerated by at risk older adults such as those enrolled in the LIFE study.
Similar to SPPB, the observed differences in 400m walking-speed between PA and HE was small; a 0.05 m/s difference in usual gait-speed has been estimated to be a small meaningful change. However, this estimate was determined using walking tests conducted over shorter distances (4 – 20m). Further, change in 400m walking-speed explained a considerable proportion of the effect of PA compared with HE on the prevention of mobility disability. Previous work may underestimate the benefits of smaller changes in gait speed, especially over longer distances. Notably, gait-speed measured over 4m remained nearly identical in PA vs. HE, thus gait-speed measured over a short distance may not be a good outcome or early indicator of the prevention of downstream outcomes in intervention trials.
The LIFE-Pilot (LIFE-P) study was able to directly measure isokinetic knee extensor strength in a small subset of participants (n=42) and showed that after 12-months, strength adjusted for muscle mass decreased in HE, whereas the loss of strength was completely prevented in the PA group37. However, the LIFE-Pilot study did observe greater differences between PA vs. HE at 6- and 12-months in total SPPB score. This may be attributable to the frequency of center-based exercise in LIFE-P, which was 3x/week for the first 6-months, 2x/week for months 7–10 and 1–2 optional center-based sessions for the remaining 2-months. Further, the behavioral component in LIFE-P employed structured, small group based behavior counseling, which was not done in LIFE. LIFE-P participants were also over 2 years younger at baseline compared with LIFE. Nevertheless, PA, compared to HE, conveyed significant benefits to lower extremity muscle function in both LIFE-P and LIFE. Further, change in SPPB weighted more strongly on change in 400m walking-speed than did 4m gait-speed in LIFE-P. This corroborates our hypothesis that change in lower extremity function is a better early indicator of the effectiveness of PA interventions on the prevention of major mobility disability than 4m gait speed.
Numerous smaller and shorter term studies have shown that PA is effective at improving or preventing declines in lower extremity muscle function and physical function at older ages12–13, 15–17, 19, 22–23. We have extended the literature by including a large sample of at-risk older adults, conducting a long-term intervention and showing the efficacy of exercise at improving physical function in at risk older adults. Further, these are the first data to directly show that improved lower extremity muscle function, is a key factor underlying the prevention of mobility disability. Studies that directly measure lower extremity muscle strength/power, cardiorespiratory fitness, muscle tissue properties as well as total and regional body composition are needed to examine specific pathways.
The LIFE study has the major strength of being a large randomized trial, and has numerous other strengths, including the inclusion of an active comparison group, long duration, with a high proportion of men and women as well as minorities. LIFE employed widely used and well validated physical performance measures that assessed many aspects of physical function. Key limitations include no direct measures of lower extremity muscle strength or power, fitness or body composition. These results are mainly generalizable to older adults at high risk (SPPB <10) for mobility disability.
In conclusion, compared with HE, a moderate intensity, structured PA intervention consisting primarily of walking, supplemented with lower extremity resistance training and balance regimens was effective at improving lower extremity function. PA had the strongest effects on chair-stand performance and walking-speed over 400m. The effect of PA was not evident when examining gait speed over a shorter distance (4m), suggesting shorter gait speed tests may not be a sensitive indicator of the effectiveness of PA on downstream outcomes in the disablement pathway. Importantly, a large proportion of the effect of PA, compared to HE, on the prevention of major mobility disability was explained by modest changes in lower extremity muscle function and 400m walking-speed. This suggests that interventions directly targeting lower muscle function and fitness would be especially effective at preventing mobility disability.
Supplementary Material
Acknowledgments
Sponsor’s role and funding sources for the LIFE Study:
The following funded design, methods, subject recruitment, data collection, analysis and/or preparation of paper: National Institutes of Health/National Institute on Aging Cooperative Agreement #UO1 AG22376 and a supplement from the National Heart, Lung and Blood Institute 3U01AG022376-05A2S, and sponsored in part by the Intramural Research Program, National Institute on Aging, NIH.
The research is partially supported by the Claude D. Pepper Older Americans Independence Centers at the University of Florida (1 P30 AG028740), Wake Forest University (1 P30 AG21332),Tufts University (1P30AG031679), University of Pittsburgh (P30 AG024827), and Yale University (P30AG021342) and the NIH/NCRR CTSA at Stanford University (UL1 RR025744),
Tufts University is also supported by the Boston Rehabilitation Outcomes Center (1R24HD065688-01A1).
Authors are also partially supported by the following:
Dr. Thomas Gill (Yale University) is the recipient of an Academic Leadership Award (K07AG3587) from the National Institute on Aging.
Dr. Roger Fielding (Tufts University) is partially supported by the U.S. Department of Agriculture, under agreement No. 58-1950-0-014. Any opinions, findings, conclusion, or recommendations expressed in this publication are those of the author(s) and do not necessarily reflect the view of the U.S. Dept of Agriculture.
Footnotes
Trial Registration: clinicaltrials.gov, Identifier: NCT01072500
Conflicts of Interest: Dr. Roger Fielding (Tufts University) is partially supported by the U.S. Department of Agriculture, under agreement No. 58-1950-0-014. Any opinions, findings, conclusion, or recommendations expressed in this publication are those of the author(s) and do not necessarily reflect the view of the U.S. Dept of Agriculture. All other authors have no conflicts to report.
Author contributions: NWG, SNB, RAF, TMG, JMG, ACK, ESS, TMM, APM, MMM, BHG, MP and ABN designed the research; all authors participated in interpretation of the data; LCL and FCH analyzed the data; AJS and ABN drafted the manuscript; all authors gave critical revisions of the manuscript for important intellectual content; NWG, SNB, RAF, TMG, JMG, ACK, TMM, APM, MMM, BHG, MP and ABN obtained funding; LCL and FCH performed statistical analyses; and all authors gave final approval of the manuscript.
Supplementary Appendix S1: LIFE Study Acknowledgments
A list of key LIFE Study personnel can be found online in Supplementary Appendix S1.
REFERENCES
- 1.Cesari M, Kritchevsky SB, Penninx BWHJ, et al. Prognostic Value of Usual Gait Speed in Well-Functioning Older People—Results from the Health, Aging and Body Composition Study. Journal of the American Geriatrics Society. 2005;53:1675–1680. doi: 10.1111/j.1532-5415.2005.53501.x. [DOI] [PubMed] [Google Scholar]
- 2.Guralnik JM, Ferrucci L, Pieper CF, et al. Lower Extremity Function and Subsequent Disability. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2000;55:M221–M231. doi: 10.1093/gerona/55.4.m221. [DOI] [PubMed] [Google Scholar]
- 3.Studenski S, Perera S, Patel K, et al. Gait Speed and Survival in Older Adults. JAMA: The Journal of the American Medical Association. 2011;305:50–58. doi: 10.1001/jama.2010.1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pahor M, Manini T, Cesari M. Sarcopenia: Clinical evaluation, biological markers and other evaluation tools. J Nutr Health Aging. 2009;13:724–728. doi: 10.1007/s12603-009-0204-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rantanen T, Guralnik JM, Foley D, et al. Midlife hand grip strength as a predictor of old age disability. JAMA. 1999;281:558–560. doi: 10.1001/jama.281.6.558. [DOI] [PubMed] [Google Scholar]
- 6.Mitchell WK, Atherton PJ, Williams J, et al. Sarcopenia, dynapenia and the impact of advancing age on human skeletal muscle size and strength; a quantitative review. Frontiers in Physiology. 2012:3. doi: 10.3389/fphys.2012.00260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Manini TM, Clark BC. Dynapenia and Aging: An Update. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2012;67A:28–40. doi: 10.1093/gerona/glr010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Newman AB, Kupelian V, Visser M, et al. Strength, But Not Muscle Mass, Is Associated With Mortality in the Health, Aging and Body Composition Study Cohort. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2006;61:72–77. doi: 10.1093/gerona/61.1.72. [DOI] [PubMed] [Google Scholar]
- 9.de Rekeneire N, Visser M, Peila R, et al. Is a fall just a fall: correlates of falling in healthy older persons. The Health, Aging and Body Composition Study. J Am Geriatr Soc. 2003;51:841–846. doi: 10.1046/j.1365-2389.2003.51267.x. [DOI] [PubMed] [Google Scholar]
- 10.Nevitt MC, Cummings SR, Kidd S, et al. Risk factors for recurrent nonsyncopal falls: A prospective study. JAMA. 1989;261:2663–2668. [PubMed] [Google Scholar]
- 11.Frank JS, Patla AE. Balance and mobility challenges in older adults: Implications for preserving community mobility. American Journal of Preventive Medicine. 2003;25:157–163. doi: 10.1016/s0749-3797(03)00179-x. [DOI] [PubMed] [Google Scholar]
- 12.Kukuljan S, Nowson CA, Sanders K, et al. Effects of resistance exercise and fortified milk on skeletal muscle mass, muscle size, and functional performance in middle-aged and older men: an 18-mo randomized controlled trial. J Appl Physiol. 2009;107:1864–1873. doi: 10.1152/japplphysiol.00392.2009. [DOI] [PubMed] [Google Scholar]
- 13.Liu CJ, Latham NK. Progressive resistance strength training for improving physical function in older adults. Cochrane Database Syst Rev. 2009:CD002759. doi: 10.1002/14651858.CD002759.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Perera S, Mody SH, Woodman RC, et al. Meaningful Change and Responsiveness in Common Physical Performance Measures in Older Adults. Journal of the American Geriatrics Society. 2006;54:743–749. doi: 10.1111/j.1532-5415.2006.00701.x. [DOI] [PubMed] [Google Scholar]
- 15.Villareal DT, Banks M, Sinacore DR, et al. Effect of Weight Loss and Exercise on Frailty in Obese Older Adults. Archives of internal Medicine. 2006;166:860–866. doi: 10.1001/archinte.166.8.860. [DOI] [PubMed] [Google Scholar]
- 16.Villareal DT, Chode S, Parimi N, et al. Weight Loss, Exercise, or Both and Physical Function in Obese Older Adults. New England Journal of Medicine. 2011;364:1218–1229. doi: 10.1056/NEJMoa1008234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Messier SP, Loeser RF, Miller GD, et al. Exercise and dietary weight loss in overweight and obese older adults with knee osteoarthritis: The arthritis, diet, and activity promotion trial. Arthritis & Rheumatism. 2004;50:1501–1510. doi: 10.1002/art.20256. [DOI] [PubMed] [Google Scholar]
- 18.Pahor M, Blair SN, Espeland M, et al. Effects of a physical activity intervention on measures of physical performance: Results of the lifestyle interventions and independence for Elders Pilot (LIFE-P) study. The journals of gerontology Series A, Biological sciences and medical Sciences. 2006;61:1157–1165. doi: 10.1093/gerona/61.11.1157. [DOI] [PubMed] [Google Scholar]
- 19.Avila J, Gutierres J, Sheehy M, et al. Effect of moderate intensity resistance training during weight loss on body composition and physical performance in overweight older adults. European Journal of Applied Physiology. 2010;109:517–525. doi: 10.1007/s00421-010-1387-9. [DOI] [PubMed] [Google Scholar]
- 20.Howe TE, Rochester L, Neil F, et al. Exercise for improving balance in older people. Cochrane Database Syst Rev. 2011:CD004963. doi: 10.1002/14651858.CD004963.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pamukoff DN, Haakonssen EC, Zaccaria JA, et al. The effects of strength and power training on single-step balance recovery in older adults: a preliminary study. Clin Interv Aging. 2014;9:697–704. doi: 10.2147/CIA.S59310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhuang J, Huang L, Wu Y, et al. The effectiveness of a combined exercise intervention on physical fitness factors related to falls in community-dwelling older adults. Clin Interv Aging. 2014;9:131–140. doi: 10.2147/CIA.S56682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gschwind YJ, Kressig RW, Lacroix A, et al. A best practice fall prevention exercise program to improve balance, strength / power, and psychosocial health in older adults: study protocol for a randomized controlled trial. BMC Geriatr. 2013;13:105. doi: 10.1186/1471-2318-13-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fielding RA, Rejeski WJ, Blair S, et al. The Lifestyle Interventions and Independence for Elders Study: Design and Methods. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2011;66A:1226–1237. doi: 10.1093/gerona/glr123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pahor M, Guralnik JM, Ambrosius WT, et al. Effect of structured physical activity on prevention of major mobility disability in older adults: the LIFE study randomized clinical trial. JAMA. 2014;311:2387–2396. doi: 10.1001/jama.2014.5616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Marsh AP, Lovato LC, Glynn NW, et al. Lifestyle Interventions and Independence for Elders Study: Recruitment and Baseline Characteristics. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2013;68:1549–1558. doi: 10.1093/gerona/glt064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Guralnik JM, Simonsick EM, Ferrucci L, et al. A Short Physical Performance Battery Assessing Lower Extremity Function: Association With Self-Reported Disability and Prediction of Mortality and Nursing Home Admission. Journal of Gerontology. 1994;49:M85–M94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 28.Guralnik JM, Ferrucci L, Simonsick EM, et al. Lower-Extremity Function in Persons over the Age of 70 Years as a Predictor of Subsequent Disability. New England Journal of Medicine. 1995;332:556–562. doi: 10.1056/NEJM199503023320902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Teng EL, Chui HC. The Modified Mini-Mental State (3MS) examination. The Journal of clinical psychiatry. 1987;48:314–318. [PubMed] [Google Scholar]
- 30.Borg G. Borg’s Perceived exertion and pain scales. Champaign, IL: Human Kinetics; 1998. [Google Scholar]
- 31.Stewart AL, Mills KM, King AC, et al. CHAMPS Physical Activity Questionnaire for Older Adults: outcomes for interventions. Medicine & Science in Sports & Exercise. 2001;33:1126–1141. doi: 10.1097/00005768-200107000-00010. [DOI] [PubMed] [Google Scholar]
- 32.Rejeski WJ, Ip EH, Marsh AP, et al. Measuring disability in older adults: the International Classification System of Functioning, Disability and Health (ICF) framework. Geriatr Gerontol Int. 2008;8:48–54. doi: 10.1111/j.1447-0594.2008.00446.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lord SR, Murray SM, Chapman K, et al. Sit-to-Stand Performance Depends on Sensation, Speed, Balance, and Psychological Status in Addition to Strength in Older People. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2002;57:M539–M543. doi: 10.1093/gerona/57.8.m539. [DOI] [PubMed] [Google Scholar]
- 34.Chen H, Quandt SA, Grzywacz JG, et al. A Bayesian multiple imputation method for handling longitudinal pesticide data with values below the limit of detection. Environmetrics. 2013;24:132–142. doi: 10.1002/env.2193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Simonsick EM, Fan E, Fleg JL. Estimating Cardiorespiratory Fitness in Well-Functioning Older Adults: Treadmill Validation of the Long Distance Corridor Walk. Journal of the American Geriatrics Society. 2006;54:127–132. doi: 10.1111/j.1532-5415.2005.00530.x. [DOI] [PubMed] [Google Scholar]
- 36.Lange-Maia B, Newman A, Strotmeyer E, et al. Performance on fast- and usual-paced 400-m walk tests in older adults: are they comparable? Aging Clin Exp Res. 2015;27:309–314. doi: 10.1007/s40520-014-0287-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Goodpaster BH, Chomentowski P, Ward BK, et al. Effects of physical activity on strength and skeletal muscle fat infiltration in older adults: a randomized controlled trial. J Appl Physiol. 2008;105:1498–1503. doi: 10.1152/japplphysiol.90425.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.