Abstract
Background
Dietary recommendations for adults with diabetes are to follow a healthy diet in appropriate portion sizes. We determined recent trends in energy and nutrient intakes among a nationally representative sample of U.S. adults with and without type 2 diabetes.
Methods
Participants were adults age ≥20 years from the cross-sectional National Health and Nutrition Examination Surveys, 1988–2012 (N=49,770). Diabetes was determined by self-report of a physician diagnosis (n=4,885). Intake of energy and nutrients were determined from a 24 hour recall by participants of all food consumed. Linear regression was used to test for trends in mean intake over time for all participants and by demographic characteristics.
Results
Among adults with diabetes, overall total energy intake increased between 1988–1994 and 2011–2012 (1,689 kcals vs. 1,895 kcals, p-trend <0.001) with evidence of a plateau between 2003–2006 and 2011–2012. In 2007–2012, energy intake was greater for younger than older adults, men than women, and non-Hispanic whites vs. non-Hispanic blacks. There was no change in the percent of calories from carbohydrate, total fat, or protein. Percent of calories from saturated fat was similar across study periods but remained above recommendations (11.2% in 2011–2012). Fiber intake significantly decreased and remained below recommendations (p-trend=0.002). Sodium, cholesterol, and calcium intakes increased. There was no change in energy intake among adults without diabetes and dietary trends were similar to those with diabetes.
Conclusions
Future data are needed to confirm a plateau in energy intake among adults with diabetes but opportunity exists to increase fiber and reduce saturated fat.
Keywords: dietary intake, type 2 diabetes, energy intake, trends in dietary intake
Introduction
The prevalence of type 2 diabetes has increased substantially over the past several decades, which may lead to future growth in morbidity, mortality, and economic costs1. Given that the majority of persons with type 2 diabetes are overweight or obese, weight loss through nutritional therapy is often a first step to control diabetes 2. Modest reductions in weight loss can decrease insulin resistance and improve other health outcomes such as hypertension2. Furthermore, a nutritious diet that aids in weight loss or weight management may reduce the number of pharmacologic agents that are needed to control diabetes and may improve psychological health such that the patient is empowered to effectively manage their diabetes. The American Diabetes Association (ADA) advises that persons with diabetes to follow the dietary guidelines for the general population, the Dietary Guidelines for Americans3; there is no scientific evidence to support a specific diet for persons with type 2 diabetes. Thus, the ADA recommends following a healthy, nutrient dense diet in appropriate portion sizes to lose weight or maintain a healthy weight2.
In the U.S. general population, a significant increase in intake of total calories was found between 1971 and 20004. Since 2000, calorie intake has remained relatively stable5. In a national study of the general population, the percentage of energy from carbohydrate consumption increased, and the percent of energy from fat and protein decreased between 1971 and 2006; these trends were similar across normal-weight, overweight and obese groups6. There is less available data on trends in dietary intake among U.S. adults with type 2 diabetes. In a national study from 1988–2004 among adults with type 2 diabetes, about two-thirds consumed more fat and saturated fat than recommended with older adults eating a lower percentage of calories from fat7. In a previous study using the same national data between 1988 and 2004, total energy consumption among adults with diabetes remained stable, except for those age 45–64 years where consumption increased; for all adults with diabetes, carbohydrate consumption increased8. Finally, a national cross-sectional study conducted between 2005 and 2010 assessed whether knowledge of a diagnosis of diabetes made a difference in macronutrient intake; results indicated that men and women with diagnosed diabetes consumed more protein than their counterparts with undiagnosed diabetes; however, all participants consumed less fiber and more saturated fat than recommended 9.
There are several micronutrients that are known to be important for diabetes management. There is limited evidence that low vitamin D and calcium levels may negatively affect glycemic levels10,11. Nevertheless, calcium and vitamin D are important for bone health and persons with diabetes are at an increased risk of fractures12. Vitamin C and potassium are found in a variety of fruits and vegetables and potassium may influence insulin secretion13,14. In some studies, magnesium deficiency has been associated with type 2 diabetes15,16. Despite these associations, the ADA does not have specific micronutrient guidelines for persons with diabetes since the scientific evidence is insufficient to make any formal recommendations.
The main purpose of this study was to determine trends in energy and macro- and micro-nutrient intake among adults with type 2 diabetes using data from the National Health and Nutrition Examination Surveys, 1988–2012. In addition, current dietary intake among adults with type 2 diabetes was assessed by age, sex, and race/ethnicity and comparisons were made to those without diabetes. Results from this study provide new data on the nutritional status of U.S. adults with type 2 diabetes.
Methods
The National Health and Nutrition Examination Survey (NHANES) is a stratified multistage probability cluster survey conducted in the non-institutionalized U.S. population17. Participants are interviewed in their home for basic demographic and health information. Following the in-home interview, participants are scheduled to visit a mobile examination center (MEC) to complete a physical examination and a 24-hour dietary recall, and to obtain blood samples for laboratory measurement18,19. Between 1988–1994 and 2011–2012, the response rates for the interview ranged from 78.4% to 86.0%; for the examination, response rates ranged from 75.4% to 80.0%. Written informed consent was obtained from all participants and was approved by the National Center for Health Statistics Institutional Review Board.
Study participants
Participants were adults age ≥ 20 years (N=49,770). Diagnosed diabetes was determined if a participant answered “yes” when asked whether a physician had ever told them that they had diabetes, excluding during pregnancy (n=1,193 NHANES III, n=849 NHANES 1999–2002, n=910 NHANES 2003–2006, n=1,341 NHANES 2007–2010, n=592 NHANES 2011–2012). Participants likely to have type 1 diabetes were excluded (n=265) based on the criteria of diabetes diagnosis at age <30 years, current insulin use, and starting insulin treatment within one year of diagnosis20. Participants self-reported demographic characteristics, including age, sex and race/ethnicity. This study reports on non-Hispanic whites, non-Hispanic blacks, and Mexican Americans.
Dietary Intake
In the MEC, participants were asked to report all foods and beverages that were consumed in the past 24 hours. The approaches used to collect dietary data and the databases used to analyze energy and nutrient composition have changed slightly over time, however, estimates are known to be comparable and any effect would be non-differential21–23. In addition, the databases include foods and food products that are traditional to a variety of cultural backgrounds. In NHANES III, the recall was administered using a multiple-pass approach and coding system known as the NHANES III Dietary Data Collection (DDC) System23. The DDC system was developed for use in the survey by the University of Minnesota’s Nutrition Coordination Center (NCC) and total nutrients were based on the NCC nutrient database. In the continuous NHANES (1999—2012), dietary data were collected using a computer-assisted dietary interview (CADI) system. In NHANES 1999–2000, nutrient intake was based on the University of Texas Food Intake Analysis System (FIAS) database and the USDA 1994–1998 Survey Nutrient Database21. Beginning in 2001, the dietary intake data was an integration of two surveys: the USDA’s Continuing Survey of Food Intakes by Individuals (CSFII) and the DHHS’s National Health and Nutrition Examination Survey (NHANES). The integrated dietary survey was named ‘What We Eat in America’22. Since 2001, nutrient intake is based on the USDA’s Food and Nutrient Database for Dietary Studies (FNDDS).
Statistical Analysis
Means and percents (standard errors) were used to describe dietary intake in each survey period using the dietary recall from the MEC; 2-year survey cycles in the continuous 1999–2010 NHANES were combined into 4-year survey cycles as recommended by the National Center for Health Statistics24. Data from the 2011–2012 survey was released during the writing of this manuscript and the authors chose to include these data as a 2-year cycle to provide the most recent estimates available; in addition, the 2011–2012 survey cycle was combined with the 2007–2010 survey cycles for significance testing by demographic characteristics. Estimates of dietary intake included mean energy intake (kcals) in each survey period, percent of calories from consumption of carbohydrates, protein, total fat, saturated fat, polyunsaturated fat, monounsaturated fat; mean fiber intake (g/1,000 kcals); and mean intakes of sodium (mg), alcohol (g), cholesterol (mg), vitamin D (mcg), calcium (mg), vitamin C (mg), magnesium (mg), and potassium (mg). Overall estimates were age and sex standardized to the 2007–2010 NHANES diabetic population using age groups 20–44, 45–64, 65–74, and ≥75 years. In addition, dietary intake was stratified by age, sex, and race/ethnicity. Linear regression was used to test for a linear trend (p<0.01) in dietary intake with each dietary component as the dependent variable and the mid-point of each survey cycle as the independent variable. Trend testing for estimates that were age and sex standardized also included independent variables for age and sex. Two-sided t-tests (p<0.01) were used to determine differences in intake by demographic characteristics in 2007–2012. Finally, to provide a comparison to those with diabetes, overall dietary intake was assessed among those without diagnosed diabetes. Linear regression was used to test for an interaction between diabetes status and study period while adjusting for age, sex, race/ethnicity, education, and BMI. All statistical analyses used sample weights and accounted for the cluster sampling design using SUDAAN (SUDAAN User’s Manual, Release 9.2, 2008; Research Triangle Institute).
Results
Characteristics of Participants
There was no significant change in the age or the sex distribution over time (Table 1). The proportion who were non-Hispanic white significantly decreased and mean BMI significantly increased over time. The use of insulin was stable and the use of oral agents significantly increased.
Table 1.
Characteristics of participants age ≥20 years who self-reported type 2 diabetes in the National Health and Nutrition Examination Surveys, 1988–2012
| NHANES III, 1988–1994 (N=1,193) | NHANES 1999–2002 (N=849) | NHANES 2003–2006 (N=910) | NHANES 2007–2010 (N=1,341) | NHANES 2011–2012 (N=592) | |
|---|---|---|---|---|---|
| % (SE)† | % (SE) | % (SE) | % (SE) | % (SE) | |
| Age | |||||
| 20–44 | 15.3 (1.93) | 17.1 (2.11) | 13.2 (2.17) | 10.2 (1.17) | 10.8 (1.43) |
| 45–64 | 41.9 (2.25) | 45.9 (2.17) | 44.4 (2.35) | 46.9 (1.81) | 47.9 (2.85) |
| 65–74 | 24.8 (1.92) | 23.1 (1.79) | 26.7 (2.02) | 25.7 (1.35) | 22.7 (2.65) |
| ≥75 | 18.1 (1.44) | 13.8 (1.52) | 15.8 (1.95) | 17.3 (1.13) | 18.7 (1.17) |
| Sex, women | 56.0 (2.52) | 50.7 (2.29) | 53.4 (2.09) | 51.7 (2.33) | 51.2 (2.55) |
| Race/Ethnicity | |||||
| Non-Hispanic white | 77.9 (1.61) | 72.1 (3.08) | 71.7 (3.40) | 68.7 (3.45) | 69.0 (5.50)* |
| Non-Hispanic black | 15.9 (1.45) | 19.5 (3.04) | 19.4 (2.40) | 20.8 (2.49) | 21.6 (4.93) |
| Mexican American | 5.5 (0.47) | 8.4 (1.63) | 9.0 (2.02) | 10.5 (2.37) | 9.4 (3.24) |
| High school education | 56.0 (2.79) | 63.6 (2.79) | 71.3 (1.96) | 67.7 (1.46) | 73.1 (3.18) |
| BMI (kg/m2) (mean) | 30.4 (0.31) | 32.1 (0.45) | 32.6 (0.50) | 33.2 (0.33) | 32.8 (0.51)** |
| Taking insulin | 27.4 (1.42) | 25.7 (2.76) | 23.3 (1.81) | 27.6 (2.00) | 26.5 (2.36) |
| Taking oral agents | 47.9 (2.61) | 68.9 (2.49) | 70.8 (2.52) | 74.7 (1.90) | 73.2 (3.17)** |
p<0.01 for test of trends
p<0.001 for test of trends
Percent (standard error), unless otherwise noted in left column
Among adults without type 2 diabetes, there was a significant decrease in the proportion of adults age 20–44 years and an increase in the proportion age 45–64 years (Table S1). Similar to those with diabetes, mean BMI significantly increased.
Energy, Macronutrient, and Micronutrient Intake
Age and sex-standardized estimates of nutrient intake are presented in Table 2; Table S2 presents the estimates stratified by age, sex, and race/ethnicity.
Table 2.
Intake of energy, macronutrients, and micronutrients from a 24-hour dietary recall among adults with self-reported type 2 diabetes in the National Health and Nutrition Examination Surveys, 1988–2012
| NHANES III, 1988–1994 (N=1,193) | NHANES 1999–2002 (N=849) | NHANES 2003–2006 (N=910) | NHANES 2007–2010 (N=1,341) | NHANES 2011–2012 (N=592) | |
|---|---|---|---|---|---|
| Mean (SE)a | Mean (SE) | Mean (SE) | Mean (SE) | Mean (SE) | |
| Total Calories (kcals) | 1,689 (26.5) | 1,753 (35.1) | 1,888 (37.6) | 1,827 (31.0) | 1,895 (44.1)** |
| Macronutrients (%, SE): | |||||
| Carbohydrates | 48.5 (0.6) | 49.2 (0.8) | 47.1 (0.5) | 47.5 (0.4) | 47.4 (0.7) |
| Protein | 17.8 (0.3) | 17.5 (0.3) | 16.9 (0.3) | 17.2 (0.2) | 17.2 (0.4) |
| Total Fat | 34.1 (0.5) | 34.2 (0.7) | 36.1 (0.4) | 34.9 (0.4) | 35.2 (0.4) |
| Saturated Fat | 11.1 (0.2) | 10.4 (0.3) | 11.8 (0.2) | 11.4 (0.2) | 11.2 (0.2) |
| Polyunsaturated Fat | 7.3 (0.1) | 7.6 (0.2) | 7.9 (0.3) | 7.5 (0.1) | 8.5 (0.2)** |
| Monounsaturated Fat | 13.0 (0.2) | 12.6 (0.3) | 13.3 (0.2) | 12.8 (0.2) | 12.3 (0.3) |
| Fiber (g/1000 kcals) | 10.3 (0.3) | 9.6 (0.3) | 8.7 (0.2) | 9.0 (0.2) | 9.4 (0.4)* |
| Sodium (mg) | 3,037 (59.3) | 3,133 (88.5) | 3,226 (67.1) | 3,323 (60.8) | 3,376 (86.4)* |
| Alcohol (g) | 4.1 (1.0) | 3.0 (0.6) | 5.1 (0.9) | 5.9 (0.9) | 3.8 (0.8) |
| Cholesterol (mg) | 258 (10.7) | 279 (13.4) | 291 (13.1) | 282 (8.0) | 298 (12.1) |
| Vitamin D (mcg) | 4.4 (0.2) | 5.2 (0.6) | |||
| Calcium (mg) | 735 (20.2) | 697 (20.5) | 829 (23.5) | 869 (19.3) | 905 (33.1)** |
| Vitamin C (mg) | 102 (4.6) | 86 (4.1) | 82 (5.2) | 76 (3.3) | 80 (5.1)** |
| Magnesium (mg) | 281 (6.4) | 263 (7.3) | 275 (6.9) | 273 (4.6) | 285 (9.8) |
| Potassium (mg) | 2,743 (50.8) | 2,586 (59.8) | 2,650 (66.8) | 2,539 (46.0) | 2,643 (93.4) |
Estimates are age and sex standardized to the 2007–2010 NHANES diabetic population
p<0.01 for test of trends
p<0.001 for test of trends
Energy Intake
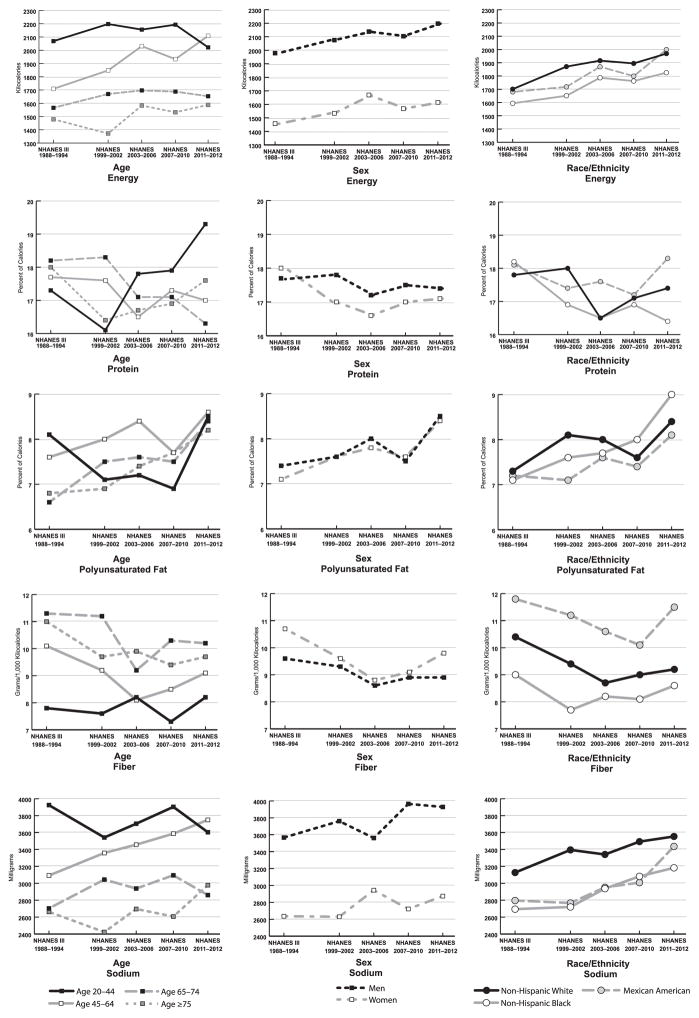
Among adults with diabetes, energy intake significantly increased between 1988–1994 and 2011–2012 (1,689 kcals vs. 1,895 kcals, respectively, p-trend<0.001) (Table 2). This increase in energy intake was most apparent in those age 45–64 years and among Mexican Americans (Figure 1, Table S2). There was little change in energy intake between 2003–2006 (1,888 kcals) and 2011–2012 (1,895 kcals). In 2007–2012, adults 20–44 years consumed more calories than adults age ≥ 65 years and men consumed more calories than women.
Figure 1.
Energy and nutrient intakes among adults with diabetes, NHANES 1988–2012. Trends were significant (p<0.01) for: energy, age 45–64 years and Mexican American; protein, age 65–74 years and non-Hispanic black; fiber, age 45–64 years, ≥75 years, women, and non-Hispanic white; polyunsaturated fat, age 65–74 years, ≥75 years, women, non-Hispanic white, and non-Hispanic black; fiber, age 45–64 years, ≥75 years, women, and non-Hispanic white; sodium, age 45–64 years, men, non-Hispanic white, and non-Hispanic black.
There was no significant increase in total energy intake between 1988–1994 and 2011–2012 among adults without type 2 diabetes (p-trend=0.975) (Table S3). There was a significant interaction between diabetes status and study period after adjusting for sociodemographic characteristics and BMI (p<0.001).
Percent of Calories from Macronutrients
For adults with diabetes, the percent of calories consumed from carbohydrates was stable between 1988–1994 (48.5%) and 2011–2012 (47.4%, p-trend=0.258) and there were no changes over time by demographic factors (Table 2 and Table S2). In 2007–2012, older adults and women consumed a greater percentage of calories from carbohydrates compared to younger adults and men. Overall, there was no change in the percent of calories from protein, but intake decreased for those age 65–74 years and non-Hispanic blacks (Figure 1, Table S2). There was no change in total fat, or saturated fat between 1988–1994 and 2011–2012. In 2007–2012, saturated fat was significantly higher for non-Hispanic whites compared to non-Hispanic blacks and Mexican Americans. The percent of calories from polyunsaturated fat significantly increased (Figure 1, Table S2) and there was no change in the percent of calories from monounsaturated fat (Table S2).
Among those without type 2 diabetes, there was a significant decrease in percent of calories consumed from saturated fat and monounsaturated fat which was accompanied by an increase in percent of calories from polyunsaturated fat (p-trend<0.001 for all) (Table S3). There was no change in percent of calories from carbohydrates, protein, or total fat. After adjusting for sociodemographic characteristics and BMI, there were significant interactions between diabetes status and study period for percent of calories from protein (p=0.007), total fat (p=0.009), and saturated fat (p=0.004).
Fiber Intake (g/1,000kcals)
Fiber intake significantly decreased between 1988–1994 (10.3 g/1,000 kcals) and 2011–2012 (9.4 g/1,000 kcals, p-trend=0.002) and this decrease was apparent for those age 45–64 years, ≥75 years, women, and non-Hispanic whites (Figure 1, Table 2). In 2007–2012, fiber intake was significantly lower among those age 20–44 years compared to adults ≥65 years (Table S2). Mexican Americans had the highest intake of fiber and non-Hispanic blacks had the lowest intake compared to non-Hispanic whites.
Fiber intake was stable between 1988–1994 and 2011–2012 (9.2 g/1,000 kcals) but remained low among adults without type 2 diabetes (Table S3). There was a significant interaction between diabetes status and study period after adjusting for sociodemographic characteristics and BMI (p=0.002).
Sodium
Overall, sodium intake increased between 1988–1994 (3,037 mg) and 2011–2012 (3,376 mg, p-trend=0.002) (Figure 1, Table 2). In 2007–2012, sodium intake was higher for younger adults, men, and non-Hispanic whites compared to non-Hispanic blacks and Mexican Americans.
Among adults without type 2 diabetes, sodium intake was stable between 1988–1994 and 2011–2012 (3,389 mg) (Table S3). There was a significant interaction between diabetes status and study period after adjusting for sociodemographic characteristics and BMI (p=0.009).
Alcohol
Alcohol intake remained stable between 1988–1994 (4.1 g) and 2011–2012 (3.8 g, p-trend=0.392) (Table 2). Alcohol intake significantly increased for adults age 20–44 years and non-Hispanic blacks (Table S2). In 2007–2012, alcohol intake was higher in younger adults and men. A standard drink in the U.S. contains 14 g of alcohol; thus, consumption was below the recommendations of ≤ 2 drinks per day for men and ≤ 1 drinks per day for women.
There was no change in alcohol intake among adults without type 2 diabetes (Table S3) and there was no significant interaction between diabetes status and study period.
Cholesterol
Cholesterol intake was stable between 1988–1994 (258 mg) and 2011–2012 (298 mg) (p-trend=0.012) (Table 2). However, there was a significant increase among those age ≥ 75 years and women (Table S2). In 2007–2012, cholesterol intake was lower for older adults age ≥ 65 years and women.
There was no change in cholesterol intake among adults without type 2 diabetes (Table S3) and there was no interaction between diabetes status and study period.
Micronutrients
In 2007–2012, vitamin D intake was similar by age but was significantly lower for women than men and for non-Hispanic blacks compared to non-Hispanic whites (Table S2). Vitamin D intake was not ascertained prior to 2007–2012. Mean calcium intake significantly increased between 1988–1994 and 2011–2012. Vitamin C intake significantly decreased between 1988–1994 and 2011–2012, but was relatively stable between 1999–2002 and 2011–2012 (Table 2). Overall, there was no change in magnesium or potassium intake.
Intake of calcium increased while intake of vitamin C and potassium decreased among those without diabetes (p-trend<0.001 for all) (Table S3). There was no interaction between diabetes status and study period.
Discussion
The ADA recommends that adults with diabetes follow a healthy, nutrient-dense, and balanced diet to manage their diabetes. In addition, persons with diabetes should be cognizant of any diabetes-related complications or comorbidities that may require modifications from the general Dietary Guidelines. Among adults with type 2 diabetes, energy intake significantly increased between 1988–1994 and 2011–2012, although there was little change between 2003–2006 and 2011–2012; supplemental analysis revealed that the observed increase in energy intake was not attenuated after controlling for BMI over time. These findings align with previous research in the general U.S. population showing that calorie intake increased between the 1970’s and 2000 but remained relatively stable through 20084,5. In addition, there were few changes in macronutrient composition over the study period for adults with type 2 diabetes. Carbohydrate intake was stable between 1988–1994 and 2011–2012; however, already low fiber intakes in 1988–1994 decreased further over time and were especially low among young adults. The Dietary Guidelines for Americans recommend at least 14 grams of fiber per 1,000 kcals; intake was 7.6 g/1,000 kcals for adults age 20–44 years and 9.4 g/1,000 kcals overall in 2011–20123. From this finding it can be assumed that a large proportion of carbohydrate consumption is coming from processed foods rather than whole grains, fruits, or vegetables25. Protein intake decreased for adults age 65–74 years and non-Hispanic blacks, but the ADA does not have specific recommendations for protein even among those with diabetic kidney disease. The percent of calories from saturated fat remained stable at 11% despite recommendations that <10% of calories come from saturated fat to reduce the risk of CVD; thus, it appears that adults with type 2 diabetes are not decreasing their consumption of saturated fat and that intake remains at the high end of recommended levels 3,26. Although saturated fat intake was similar by age in 2007–2012, intake among older adults significantly increased over the study period. Since older adults with diabetes already have a higher risk of diabetes-related complications, high levels of saturated fat intake may exacerbate their CVD risk; in fact, the American Heart Association recommends that dietary intake of saturated fat be <7.0% of total calories27. However, there was an increase in the percent of calories from polyunsaturated fat, which are known to be beneficial for reducing cholesterol when consumed instead of saturated fats, suggesting that adults with diabetes may be trying to improve the types of fat they consume.
It is important to highlight the suboptimal dietary intake among adults with type 2 diabetes age 45–64 years, the only age group that showed a significant increase in calorie intake between 1988–1994 and 2001–2012. A previous national study among persons with diabetes documented a similar trend in increased calorie consumption among this age group between 1988 and 20048. In addition to the increase in energy consumption, diabetic adults age 45–64 years continued to consume more saturated fat than recommended (11.5% of calories in 2007–2012), showed a decrease in already low fiber intakes to well below recommendations (8.7 g/1,000 kcals in 2007–2012), and demonstrated an increase in sodium intake to well above recommendations (3,647 mg/day in 2007–2012). The results in this age group are concerning given that the rate of muscle loss naturally increases around age 50 years and metabolic rate decreases; consequently, the likelihood of weight gain increases if energy consumption is not balanced28. For persons with type 2 diabetes, weight gain and a sub-par diet can further increase the risk of common comorbidities that often accompany a diagnosis of diabetes, such as hypertension and high cholesterol29.
The ADA recommends that persons with diabetes follow the general population Dietary Guidelines for micronutrient intakes3,26. Overall, adults with diabetes were within the recommended range for cholesterol (<300 mg); however, young diabetic adults, men, non-Hispanic blacks, and Mexican Americans had intakes just above recommendations. Furthermore, the Dietary Guidelines recommend a daily cholesterol intake of <200 mg for individuals at high risk of cardiovascular disease, which includes many persons with diabetes. Sodium intake remained stable but was about 1,000 mg greater than recommended levels (2,300 mg); intake was especially high for young diabetic adults and men. The ADA states that for persons with diabetes and hypertension, further reduction in sodium should be individualized to help manage blood pressure levels. Much of the sodium in the U.S. diet comes from processed foods, therefore, education on eating whole, unprocessed foods would naturally reduce the amount of sodium consumed in this population while also reducing saturated fat intake30. Nevertheless, there is current debate on whether sodium recommendations are too low31,32. Although intake of calcium increased over the study period, consumption was below recommended levels (1,000–1,200 mg). Persons with diabetes are at a higher risk of bone fractures, thus, calcium is an important nutrient for this population33,34. Current vitamin D intake was low for older diabetic adults, which is also important for bone health (15 mcg recommended). Intake of vitamin C, which is commonly found in a variety of fruits and vegetables, decreased over the study period but was within recommended dietary allowances (75–90 mg). Magnesium intake did not change over the study period but intakes were below recommended levels (300–400 mg); although magnesium deficiency has been associated with diabetes, levels were also low among those without diabetes15,16. Finally, potassium, which is also found in a variety of fruits and vegetables and may influence insulin secretion, decreased over the study period and was below recommended daily intake levels (4,700 mg per day)14; intake was also low among non-diabetic individuals. It is important to note that the vitamin intakes reported in this study only account for these nutrients consumed through food, and do not account for intake through supplements or multivitamins.
The prevalence of obesity in the U.S. population increased significantly between 1960 and 2000 with evidence that the epidemic plateaued between 2003 and 201035,36. This aligns with findings in the general population that have shown an increase in energy consumption between the 1970’s and 2000 and relatively stable energy intake between 2000 and 20084,5,35,37,38. The results from this study among persons with type 2 diabetes were similar in that energy consumption increased between 1988–1994 (1,689 kcals) and 2011–2012 (1,895 kcals) but the amount of calories consumed between 2003–2006 and 2011–2012 was unchanged (1,888 kcals vs. 1,895 kcals). Interestingly, recent research has suggested a plateau in the prevalence and incidence of diabetes between 2008 and 2012; however, future data is needed to confirm this trend to be able to make any association between changes in calorie intake and the prevalence of diabetes39. These findings are encouraging since weight control or loss is a major factor in determining future complications. However, the use of glycemic medications can make weight management particularly difficult for those with diabetes40. Diabetes medications can increase energy intake if patients are over medicated and, consequently, experience hypoglycemia; in addition, patients may think of their medications as a safety net and an excuse to consume excess energy. Nevertheless, in supplemental analysis we found no differences in energy intake by insulin use (1,871 kcals vs. 1,810 kcals for no insulin use), use of oral agents (1,817 kcals vs. 1,842 kcals for no oral agents), or BMI (1,716 kcals for normal weight vs. 1,851 kcals in obese) (data not shown). Further investigation with future data will help determine if energy intake has truly plateaued among persons with diabetes.
Unlike adults with type 2 diabetes, there was no significant change in energy consumption among adults without type 2 diabetes despite a roughly 100 calorie increase over the study period. Those without diabetes had a lower mean BMI compared to those with diabetes which may have resulted in smaller change in energy consumption. Energy consumption was higher among adults without diabetes but this finding is likely due to the diabetes population being older. Similar to adults with type 2 diabetes, among those without diabetes, intake of polyunsaturated fat and calcium increased while intake of vitamin C and potassium decreased; however, saturated fat and monounsaturated fat also decreased among those without diabetes.
A strength of this study was the nationally representative sample of U.S. adults with type 2 diabetes, thus, results can be generalized to the U.S., non-institutionalized population. The relatively consistent methods in the NHANES allowed for examining data over several decades and assessing trends. Although dietary intake was self-reported, the recall was interviewer assisted and computer-based to ensure that the most accurate information was collected. In addition, the food databases included a large number of foods and food products; any updates to the food databases over time would be expected to have a non-differential effect on the assessment of dietary intake by demographic characteristics. Dietary recalls are deemed reliable in a healthy normal weight population but those with diabetes or who are overweight may tend to underreport intake41. It is also possible that, regardless of weight status, adults may alter their eating habits if they know they will need to report on what they had eaten the following day41. Thus, the energy intake reported may be lower than actual intake. Only one dietary recall was used to estimate nutrient intake since not all NHANES survey years collected two recalls. However, nutrient intake based on one recall can be a reliable measure of usual intake in large population groups42. Sodium intakes were adjusted in NHANES 2002–2008 based on the use of salt in home food preparation but this adjustment was not used in NHANES III, NHANES 1999–2001, or NHANES 2009–2012, thus, estimates in NHANES 2007–2010 and NHANES 2011–2012 cycles may be slightly higher due to this change in methods43. Finally, diabetes was self-reported and not adjudicated; we focused on the dietary intake of adults with self-reported diabetes who are aware of their diabetes status and should, ideally, be conscientious of their diet. In addition, self-report of diabetes in survey data has been shown to be highly reliable44.
An optimal diet varies by a variety of factors including age, current health, medications, activity level, and metabolism. As recommended by the Dietary Guidelines, intake should focus on whole foods rich in whole grains, fruits, vegetables, healthy fats, and appropriate portion sizes for weight loss or management. The evidence for these recommendations are primarily based on research in the general population related to reducing CVD risk factors, many of which are relevant to those with diabetes; however, there is little scientific research on optimal dietary intake among those with diabetes. Given that there is a lack of evidence to endorse one specific type of diet, dietary intake should be individualized within the parameters of the major guidelines.
Conclusions
The ADA recommends that persons with type 2 diabetes follow the Dietary Guidelines for Americans and consume a healthy, nutrient dense diet in appropriate portion sizes to lose weight or maintain a healthy weight. Overall, there was a significant increase in energy intake between 1988–1994 and 2011–2012 for adults with diabetes in the U.S.; however, there was evidence that energy intake plateaued between 2003–2006 and 2011–2012. In addition, saturated fat and sodium intakes were high and fiber and calcium intakes were low across all age, sex, and race/ethnic groups. Thus, there is substantial opportunity for U.S. adults with type 2 diabetes to improve their dietary intake. Persons with diabetes, especially older adults who have a higher risk and prevalence of comorbidities, should carefully manage their diet. It is promising that energy intake among adults with diabetes may be plateauing, a finding that has also been found in the general U.S. population, but future data is needed to confirm this trend.
Supplementary Material
Acknowledgments
This study was supported by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) (GS-10F-0381L). The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the NIDDK. The authors have no conflicts of interest to report.
Footnotes
Author Roles: S.S. Casagrande formulated the research question, designed the study, analyzed the data, and wrote the manuscript. C.C. Cowie formulated the research question, designed the study, and edited and revised the manuscript.
References
- 1.Centers for Disease Control and Prevention; U.S. Department of Health and Human Services, editor. National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States 2011. Atlanta, GA: Centers for Disease Control and Prevention; 2011. [Google Scholar]
- 2.Evert AB, Boucher JL, Cypress M, et al. Nutrition therapy recommendations for the management of adults with diabetes. Diabetes Care. 2013 Nov;36(11):3821–3842. doi: 10.2337/dc13-2042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.U.S. Department of Agriculture and U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2010. 7. Washington, D.C: U.S. Government Printing Office; 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Trends in intake of energy and macronutrients--United States, 1971–2000. MMWR. Morbidity and mortality weekly report. 2004 Feb 6;53(4):80–82. [PubMed] [Google Scholar]
- 5.Wright JD, Wang CY. Trends in intake of energy and macronutrients in adults from 1999–2000 through 2007–2008. NCHS data brief. 2010 Nov;(49):1–8. [PubMed] [Google Scholar]
- 6.Austin GL, Ogden LG, Hill JO. Trends in carbohydrate, fat, and protein intakes and association with energy intake in normal-weight, overweight, and obese individuals: 1971–2006. The American journal of clinical nutrition. 2011 Apr;93(4):836–843. doi: 10.3945/ajcn.110.000141. [DOI] [PubMed] [Google Scholar]
- 7.Nelson KM, Reiber G, Boyko EJ. Diet and exercise among adults with type 2 diabetes: findings from the third national health and nutrition examination survey (NHANES III) Diabetes Care. 2002 Oct;25(10):1722–1728. doi: 10.2337/diacare.25.10.1722. [DOI] [PubMed] [Google Scholar]
- 8.Oza-Frank R, Cheng YJ, Narayan KM, Gregg EW. Trends in nutrient intake among adults with diabetes in the United States: 1988–2004. Journal of the American Dietetic Association. 2009 Jul;109(7):1173–1178. doi: 10.1016/j.jada.2009.04.007. [DOI] [PubMed] [Google Scholar]
- 9.Bardenheier BH, Cogswell ME, Gregg EW, Williams DE, Zhang Z, Geiss LS. Does knowing one’s elevated glycemic status make a difference in macronutrient intake? Diabetes Care. 2014 Dec;37(12):3143–3149. doi: 10.2337/dc14-1342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pittas AG, Lau J, Hu FB, Dawson-Hughes B. The role of vitamin D and calcium in type 2 diabetes. A systematic review and meta-analysis. The Journal of clinical endocrinology and metabolism. 2007 Jun;92(6):2017–2029. doi: 10.1210/jc.2007-0298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Krul-Poel YH, Westra S, ten Boekel E, et al. Effect of Vitamin D Supplementation on Glycemic Control in Patients With Type 2 Diabetes (SUNNY Trial): A Randomized Placebo-Controlled Trial. Diabetes Care. 2015 Aug;38(8):1420–1426. doi: 10.2337/dc15-0323. [DOI] [PubMed] [Google Scholar]
- 12.Shanbhogue VV, Mitchell DM, Rosen CJ, Bouxsein ML. Type 2 diabetes and the skeleton: new insights into sweet bones. The lancet. Diabetes & endocrinology. 2015 Sep 10; doi: 10.1016/S2213-8587(15)00283-1. [DOI] [PubMed] [Google Scholar]
- 13.U.S. National Library of Medicine. Vitamin C. [Accessed November 5, 2015];Health Topics. 2015 https://www.nlm.nih.gov/medlineplus/vitaminc.html.
- 14.Chatterjee R, Yeh HC, Shafi T, et al. Serum and dietary potassium and risk of incident type 2 diabetes mellitus: The Atherosclerosis Risk in Communities (ARIC) study. Archives of internal medicine. 2010 Oct 25;170(19):1745–1751. doi: 10.1001/archinternmed.2010.362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chaudhary DP, Sharma R, Bansal DD. Implications of magnesium deficiency in type 2 diabetes: a review. Biological trace element research. 2010 May;134(2):119–129. doi: 10.1007/s12011-009-8465-z. [DOI] [PubMed] [Google Scholar]
- 16.Tosiello L. Hypomagnesemia and diabetes mellitus. A review of clinical implications. Archives of internal medicine. 1996 Jun 10;156(11):1143–1148. [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention (CDC). National Center for Health Statistics (NCHS) National Health and Nutrition Examination Survey, 1999–2012. Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 1999–2012. [Google Scholar]
- 18.Centers for Disease Control and Prevention (CDC). National Center for Health Statistics (NCHS) National Health and Nutrition Examination Survey Examination Protocol, 1999–2012. Hyattsville, MD: Department of Health and Human Services, Centers for Disease Control and Prevention; 2008. [Google Scholar]
- 19.Centers for Disease Control and Prevention (CDC). National Center for Health Statistics (NCHS) National Health and Nutrition Examination Survey Laboratory Protocol: 1999–2012. Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2008. [Google Scholar]
- 20.Ng E, Vanderloo SE, Geiss L, Johnson JA. Concordance between self-report and a survey-based algorithm for classification of type 1 and type 2 diabetes using the 2011 population-based Survey on Living with Chronic Diseases in Canada (SLCDC)-Diabetes component. Canadian journal of diabetes. 2013 Aug;37(4):249–253. doi: 10.1016/j.jcjd.2013.05.007. [DOI] [PubMed] [Google Scholar]
- 21.National Center for Health Statistics; Department of Health and Human Services, editor. Dietary Interview- Total Nutrient Intakes. Hyattsville, MD: 1999–2000. [Google Scholar]
- 22.National Center for Health Statistics; Department of Health and Human Services, editor. Dietary Interview- Total Nutrient Intakes. Hyattsville, MD: 2002–2010. [Google Scholar]
- 23.National Center for Health Statistics. NHANES III Total Nutrient Intakes File Documentation. Hyattsville, MD: Department of Health and Human Services; 1998. [Google Scholar]
- 24.Johnson CL, Paulose-Ram R, Ogden CL, et al. National health and nutrition examination survey: analytic guidelines, 1999–2010. Vital and health statistics. Series 2, Data evaluation and methods research. 2013 Sep;(161):1–24. [PubMed] [Google Scholar]
- 25.Fryar CD, Ervin RB. U.S. Department of Health and Human Services, editor. NCHS Data Brief: Caloric Intake From Fast Food Among Adults, United States, 2007–2010. Vol. 114. Hyattsville, MD: National Center for Health Statistics; 2013. [PubMed] [Google Scholar]
- 26.Evert AB, Boucher JL, Cypress M, et al. Nutrition therapy recommendations for the management of adults with diabetes. Diabetes Care. 2013 Nov;36(11):3821–3842. doi: 10.2337/dc13-2042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.American Heart Association. Know Your Fats 2015. 2015 http://www.heart.org/HEARTORG/Conditions/Cholesterol/PreventionTreatmentofHighCholesterol/Know-Your-Fats_UCM_305628_Article.jsp#.Vl9EIVK5LCk.
- 28.Hobson K. US News & World Report. 2008. How To Avoid Losing Muscle as You Age. [Google Scholar]
- 29.Standards of medical care in diabetes--2015. Diabetes Care. 2014 Jan;37(Suppl 1):S14–80. doi: 10.2337/dc14-S014. [DOI] [PubMed] [Google Scholar]
- 30.Gillespie C, Maalouf J, Yuan K, et al. Sodium content in major brands of US packaged foods, 2009. The American journal of clinical nutrition. 2015 Feb;101(2):344–353. doi: 10.3945/ajcn.113.078980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Drewnowski A, Rehm CD, Maillot M, Mendoza A, Monsivais P. The feasibility of meeting the WHO guidelines for sodium and potassium: a cross-national comparison study. BMC Open. 2015:5. doi: 10.1136/bmjopen-2014-006625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zaraska M. Washington Post. Health & Science; May 4, 2015. Pass the salt, please. It’s good for you. [Google Scholar]
- 33.Meier C, Schwartz AV, Egger A, Lecka-Czernik B. Effects of diabetes drugs on the skeleton. Bone. 2015 Apr 23; doi: 10.1016/j.bone.2015.04.026. [DOI] [PubMed] [Google Scholar]
- 34.Yamamoto M. Insights into bone fragility in diabetes: the crucial role of bone quality on skeletal strength [Review] Endocrine journal. 2015 Apr 30;62(4):299–308. doi: 10.1507/endocrj.EJ15-0129. [DOI] [PubMed] [Google Scholar]
- 35.Flegal KM, Carroll MD, Kuczmarski RJ, Johnson CL. Overweight and obesity in the United States: prevalence and trends, 1960–1994. International journal of obesity and related metabolic disorders : journal of the International Association for the Study of Obesity. 1998 Jan;22(1):39–47. doi: 10.1038/sj.ijo.0800541. [DOI] [PubMed] [Google Scholar]
- 36.Flegal KM, Kruszon-Moran D, Carroll MD, Fryar CD, Ogden CL. Trends in Obesity Among Adults in the United States, 2005 to 2014. JAMA : the journal of the American Medical Association. 2016 Jun 7;315(21):2284–2291. doi: 10.1001/jama.2016.6458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA : the journal of the American Medical Association. 2012 Feb 1;307(5):491–497. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 38.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA : the journal of the American Medical Association. 2010 Jan 20;303(3):235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 39.Geiss LS, Wang J, Cheng YJ, et al. Prevalence and incidence trends for diagnosed diabetes among adults aged 20 to 79 years, United States, 1980–2012. JAMA : the journal of the American Medical Association. 2014 Sep 24;312(12):1218–1226. doi: 10.1001/jama.2014.11494. [DOI] [PubMed] [Google Scholar]
- 40.Standards of Medical Care in Diabetes-2015. Diabetes Care. 2015;38(S1) doi: 10.2337/dc19-Sint01. [DOI] [PubMed] [Google Scholar]
- 41.Moshfegh AJ, Rhodes DG, Baer DJ, et al. The US Department of Agriculture Automated Multiple-Pass Method reduces bias in the collection of energy intakes. The American journal of clinical nutrition. 2008 Aug;88(2):324–332. doi: 10.1093/ajcn/88.2.324. [DOI] [PubMed] [Google Scholar]
- 42.Basiotis PP, Welsh SO, Cronin FJ, Kelsay JL, Mertz W. Number of days of food intake records required to estimate individual and group nutrient intakes with defined confidence. The Journal of nutrition. 1987 Sep;117(9):1638–1641. doi: 10.1093/jn/117.9.1638. [DOI] [PubMed] [Google Scholar]
- 43.Sebastian RS, Wilkinson Enns C, Steinfeldt LC, Goldman JD, Moshfegh AJ. Monitoring sodium intake of the US population: impact and implications of a change in what we eat in America, National Health and Nutrition Examination Survey dietary data processing. Journal of the Academy of Nutrition and Dietetics. 2013 Jul;113(7):942–949. doi: 10.1016/j.jand.2013.02.009. [DOI] [PubMed] [Google Scholar]
- 44.Saydah SH, Geiss LS, Tierney E, Benjamin SM, Engelgau M, Brancati F. Review of the performance of methods to identify diabetes cases among vital statistics, administrative, and survey data. Annals of epidemiology. 2004 Aug;14(7):507–516. doi: 10.1016/j.annepidem.2003.09.016. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.